Lung Function – See also Chest topic
1954 West JR, Levin MS, di Sant’Agnese PA. Studies of pulmonary function in cystic fibrosis of the pancreas. Pediatrics 1954; 13:155-164. [PubMed]
These were the first pulmonary function tests reported in children with cystic fibrosis. Most children find pulmonary function tests using a spirometer difficult to perform before the age of six years or so. But as more patients survived through early childhood to an age when they could perform lung function, of a number of studies were reported. The findings in six patients aged 12 to 14 years clearly identified most of the important features of impaired lung function found in cystic fibrosis i.e. essentially there was difficulty moving air in and out of the lungs.
These abnormalities in respiratory function were confirmed in later studies e.g. the increase in residual volume in relation to total lung capacity as early changes and reduced total lung capacity and CO2 retention as late features; also noted were abnormal pulmonary gas mixing and other features of non-uniform distribution of alveolar ventilation as a result of bronchial obstruction (also West JR, di Sant’Agnese PA. Am J Dis Child 1953; 86:496-498).
1957 White R Jr, Dent JH, Derbes VJ. Asthmatic states caused by mucoviscidosis. J Louisiana St Med S 1957; 109:299-302. [PubMed]
Thirty eight of 66 children with CF from New Orleans had some degree of wheezing. The authors comment “It has been the common experience of mature pediatricians that administration of epinephrine in such circumstances has led to prompt, albeit transient, alleviation. The mechanical factors that cause impairment of pulmonary function in asthma – bronchospastic contraction, edema of the mucous membrane and excessive secretion and retention of mucus, are present both in CF and asthma”.
The authors’ wise message from their paper being – “it is the responsibility of all physicians who treat wheezing children to exclude this disorder (i.e. cystic fibrosis)”.
1959 Gandevia B, Anderson CM. The effect of bronchodilator aerosol on ventilatory capacity in fibrocystic disease of the pancreas. Arch Dis Child 1959; 34:511-515. [PubMed]
An early report, from the Royal Children’s Hospital Melbourne, of the favourable effect of bronchodilators in some people with cystic fibrosis. A 1/1000 solution of isoprenaline was used for its potency and rapidity of action. One third of 16 children with CF showed impressive improvement in their respiratory function tests after the bronchodilator, most marked in the moderately affected group rather than the severely or mildly affected patients. The authors note that there are only two previous references to bronchodilator therapy in CF – West et al, 1954 (above) who found no improvement in six patients during their early respiratory function studies and Royce 1956 (above) who noted improvement in one child. White et al, 1957 (above) reported some degree of wheezing in 38 of 66 children with CF which was relieved by epinephrine. Subsequently Landau & Phelan measured the maximum expiratory flow volumes and cautioned on the use of bronchodilators as they may impair respiratory function (Landau & Phelan. Pediatr 1973; 82:863, below).
– Note this present paper is by Charlotte Anderson – a paediatrician from Melbourne, Australia where she started the CF clinic. She eventually was appointed Professor of Paediatrics in Birmingham, UK – not Dorothy Andersen the pathologist from New York who described the disease in 1938.
1959 Cook CD, Helliesen PJ, Kulczycki L, Barrie H, Freidlander L, Agathon S, Harris GB, Shwachman H. Studies of respiratory physiology in children. II. Lung volumes and mechanics of respiration in 64 patients with cystic fibrosis of the pancreas. Pediatrics 1959; 24:181-193.[PubMed]
Detailed respiratory function on 64 patients aged 6 to 25 years. (Previous reports of West et al, 1954 above and Royce et al, 1958 are mentioned). Tidal volume and respiratory rate were abnormal in only the worst affected patients. The most frequent finding was an increased residual volume (46%) and functional residual capacity (21%). Vital capacity was reduced in 34%. The RV/TLC ratio was increased in 70%.
There was a definite correlation between respiratory function tests and clinical condition of the patients.
1959 Wright BM, McKerrow CB. Maximum expiratory flow rate as a measure of ventilatory capacity – with a description of a new portable instrument for measuring it. Brit Med J 1959; 2:1041-1947. [PubMed]
-
Martin Wright
- Martin Wright writing about this original paper later in 1981 Dr Martin Wright says “I think the paper has been cited so much because it describes a test and an instrument which are practical and useful. In those days there was also room to put in a decent historical review and quite a bit of useful discussion and useful detail. Some years ago I noticed that although the peak flow meter (PFM) was mentioned and as often the key to the whole work, there was no longer any reference to our paper. It was evidently assumed that the PFM had been created by God. I have never got any award or honour but the Minimeter, a sort of paperback version (BMJ 1978; 2:1627-8), got a design award and is selling hundreds of thousands because it can be used by patients at home. My reward is knowing that I have made a substantial contribution to clinical medicine”. Dr Wright says that “physiologists were a bit sniffy about the PFM holding that the proper way to measure flow is by volume and time but Colin McKerrow and Margery McDermott kindly did a very thorough calibration study”.
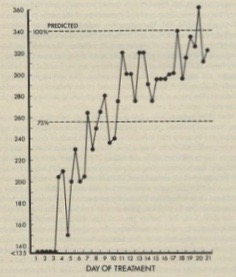
Twice daily peak flow rates during treatment of a severe exacerbation of chest infection
Undoubtedly the Wright Peak Flow Meter was a major advance in that useful repeated measurements of the patient’s respiratory function were possible at any time and anywhere without the use of a large spirometer (figure) . Standard values of peak flow rates were available for adults and children. Subsequently the advent of the Minimeter allowed patients to use it in the home and chart their own respiratory function. This was a major step forward in the management of both asthma, cystic fibrosis and other respiratory conditions.
George Polgar
1962 Polgar G, Denton R. Cystic fibrosis in adults. Studies in pulmonary function and some physical properties of bronchial mucus. Am Rev Respir Dis 1962; 85:319-327. [PubMed]
At this time only 2% of people with CF were over 20 years of age. Two of the 4 adults studied died and were autopsied. In all the recognition of CF had been only after years of illness. Interestingly the use of hypertonic saline was mentioned as causing “symptomatic improvement” – eventually, some 40 years later, this was confirmed in a large trial (Elkins et al, 2006 below). Functional abnormalities were: airway obstruction, stiffening of the lungs, increased arterial carbon dioxide and reduced arterial oxygen saturation.
The authors concluded the primary cause of the respiratory disease was obstruction of the airways secondary to impaired flow of abnormal bronchial mucus. They suggested that the practical conclusion would be to search for methods that could be used for mobilisation of the mucus from the airways.
Subsequently such treatments as hypertonic saline or rhDNase (Pulmozyme) proved to be an effective means of improving and preserving lung function
George Polgar (1918-2015), who founded a pediatric hospital in Nazi-occupied Budapest where he helped Hungarian Jews escape the death camp trains, led his family on a daring escape from Hungary following the failed revolution to overthrow the Soviet-controlled government, subsequently became a leading researcher in paediatric pulmonary at the Children’s Hospital of Philadelphia.
1968 Mearns MB. Simple tests of ventilatory capacity in children with cystic fibrosis. Arch Dis Child 1968; 4:528-539. [PubMed]
The first reports of respiratory function tests in children with CF had been performed by West et al, 1954 (above). In Margaret Mearns’s study from
-

Margaret Mearns
- London the results of respiratory function tests were correlated with clinical and radiological findings. Thirty three of 85 patients had normal FEV1 and FVC but the day to day variability were considered to limit the value of the respiratory function tests. Reversibility in response to bronchodilators was described. Twenty eight had minimal X-ray change, stable and normal; 16 with localised damage had greater reduction in FEV1 than FVC; extensive damage was associated with significant reductions in both. The tests were a valuable aid to clinical assessment especially in those patients with no or little radiological changes.
Margaret Mearns observed that “the present study shows that without the mist tent (given such prominence by Leroy Matthews and others in the USA during the Sixties), but using intensive treatment for acute respiratory illness and very close follow up from the time of diagnosis, children presenting without permanent lung damage can remain well and maintain good respiratory function over a period of years”.
These were early days for respiratory function tests in many paediatric clinics in the UK. The Vitalograph was the first widely available bellows spirometer for non-specialist use. But most general paediatricians in the UK did not have a Vitalograph although most eventually used the Wright
-
Peter Phelan at the time of this research
peak flow meter. Few children treated in general paediatric clinics lived to an age when the results would have been reliable – say over six year
1969 Phelan PD, Gracey M, Williams HE, Anderson CM. Ventilatory function in infants with cystic fibrosis. Physiological assessment of inhalation therapy. Arch Dis Child 1969; 44: 393-400. [PubMed]
An early (possibly the first?) study of respiratory function in CF infants (figure 33 main text). Total gas volume, dynamic compliance and mean pulmonary resistance were measured in 18 infants less than 9 months old. Nine infants with no infection and others with infections all returned to normal when treated with intermittent inhalations of propylene glycol 10%, glycerine 2%, in 0.9% saline 2ml + 0.25 ml of 2% orciprenaline 1-4 x daily.
More recent studies of infant respiratory function show a mild but consistent degree of airways obstruction and hyperinflation even in uninfected young infants with cystic fibrosis (Ranganathan SC et al, Lancet 2001; 358:1964-1965.[PubMed]).
1971 Godfrey S, Mearns M. Pulmonary function and response to exercise in cystic fibrosis. Arch Dis Child 1971; 46:144-151. [PubMed]
In 41 patients with CF, aged between five and 21 years, there was a linear relationship between FEV1 and maximum voluntary ventilation and the
-
Simon Godfrey
general clinical grading. The authors suggested that “the pattern of physiological disturbance is so characteristic that it could well serve as an aid to diagnosis in doubtful cases and can be revealed by steady state exercise without the use of cardiac or arterial catheterisation”.
This may have been so in the authors’ experience but these physiological studies have never been made generally available to most people with CF in the UK nor have they made a significant contribution to clinical management or the understanding of the basic CF defect. Simon Godfrey, an academic respiratory paediatrician working at the Hammersmith Hospital, London, and Margaret Mearns at the Queen Elizabeth Hospital, Hackney combined on a number of interesting studies.
1973 Day G, Mearns MB. Bronchial lability in cystic fibrosis. Arch Dis Child 1973; 48:355-359.[PubMed]
The authors comment that Heimlich EM et al, in an abstract (J Allerg 1966; 37:103) surprisingly had failed to show a difference in bronchial lability between normal children and those with cystic fibrosis. However, the exercise had been more gentle. In the present study only 14 (27%) of the 52 children with CF had normal results; 50% had abnormal bronchodilatation on exercise and 46% had abnormal bronchoconstriction after exercise.
– Bronchial lability is commonly present in people with CF and can be seen to gradually lessen as the bronchial infection is treated with intravenous antibiotics during an exacerbation.
1973 Landau LI, Phelan PD. The variable effect of a bronchodilating agent on pulmonary function in cystic fibrosis. J Pediatr 1973; 82:863-868. [PubMed]
An important paper from the Royal Children’s Hospital, Melbourne. Nine (18%) of 50 patients with CF had measurable response to bronchodilators as judged by the maximum expiratory flow-volume curve which demonstrates the maximum expiratory flow rate throughout the forced vital capacity manoeuvre (figure 1). The changes were complex. In 5 (10%) the changes were typical of asthma. Four had a fall in Vmax thought to be due to airway compression during forced expiration as had been reported previously. The authors note that previous reports indicate no effect or minimal improvement with bronchodilators (Cook CD et al. Pediatrics 1959; 24;181; Gandevia B & Anderson C. Arch Dis Child 1959; 34:511; Polgar G & Barbero GJ. Am J Dis Child 1960; 100:733; Zaptetal A et al. Pediatrics 1971; 48:64). Most people with CF have no changes, a few will show typical asthmatic response and will benefit from bronchodilators, BUT some develop reduced maximum expiratory flow rates possibly from compression of the larger airways (figure 2) – this could impair coughing and sputum clearance.
– This is a paper from two experts with a clear message that bronchodilators can sometimes make the situation worse. The authors suggest that MEFV curve should be performed before bronchodilators are prescribed. Despite this and other studies, bronchodilators are prescribed for many people with CF and usually their effect on the MEFV is not checked – usually just the effect on FEV1 and FVC by simple spirometry – and also how the patient feels after the bronchodilator should be noted!! This approach seems to work well for most people with cystic fibrosis.
 |
| Maximum expiratory flow curves. From paper with permission. |
 |
| Maximum expiratory flow curve from patient before and after bronchodilator. From paper with permission. |
1979 Price JF, Weller PH, Harper SA, Matthews DJ. Response to bronchial provocation and exercise in children with cystic fibrosis. Clin Allerg 1979; 9:563-570. [PubMed]
Ten of 15 children with CF who had positive skin prick tests to allergens had an immediate reaction to the allergen inhaled; five had late reactions also but only one had a history of asthma. The most common positive skin reaction was to Aspergillus fumigatus – inhalation of the allergen was negative in two, immediate in one and dual in three. None showed the typical reaction to exercise of asthmatic children. Although the bronchial allergy did not totally explain the tendency for children with CF to have asthma and anti-allergy treatment may have a place.
1994 Beardsmore CS, Thompson JR, Williams A, McCardle EK, Gregory GA, Weaver LT, Simpson H. Pulmonary function in infants with cystic fibrosis: effect of antibiotic treatment. Arch Dis Child 1994; 71:133-137. [PubMed]
Children from the East Anglian neonatal screening programme (1985-1992) who were included in the flucloxacillin trial
-

Carolyn Beardsmore
(Weaver et al, 1994 above) underwent infant respiratory function tests at three to four months and one year of age (measurements of thoracic gas volume and airway conductance using an infant whole body plethysmograph and maximum expiratory flow by the “squeeze” technique). There was no difference in lung function between the flucloxacillin treated infants and the control CF infants at any age.
Dr Carolyn Beardsmore was one of the few experts in infant lung testing at the time in the UK and since has published widely on a variety of paediatric respiratory topics.
Periodically studies are published on infant respiratory function testing but the techniques are so complicated and time-consuming that they are usually only performed by the authors of the papers. Although valuable for research they have never been of great practical value in the clinic for most patients. In the present study it is not surprising that there was no difference between the treated and control infants as some hyperinflation is present in all CF infants from early infancy whether they are infected or not. Hyperinflation in most CF infants was confirmed in subsequent studies (Ranganathan et al, 2001 below).
2001 Ranganathan SC, Dezateux C, Bush A, Carr SB, Castle RA, Madge S, Price J, Stroobant J, Wade A, Wallis C, Stocks J. Airway function in infants newly diagnosed with cystic fibrosis. Lancet 2001; 358:1964-5. [PubMed]
-

Somnath Ranganathan
The airway function of 33 infants with CF was significantly reduced compared with 87 healthy controls, even in those without clinically recognised previous lower respiratory illness.
– Some degree of airway obstruction, increased residual volume and hyperinflation from an early age has been recognised for many years (Keats TE. Generalized pulmonary emphysema as an isolated manifestation of early cystic fibrosis of the pancreas. Radiology 1955; 65:223-226. [PubMed] above and subsequent studies). This present study confirms this fact. A follow up study was performed by Ranganathan et al. (Am J Resp Crit Care Med 2004; 169:928-933. [PubMed]) FEV 0.5 was measured soon after diagnosis (median age of 28 weeks) and 6 months later in subjects with CF and in healthy infants on two occasions 6 months apart using the raised-volume technique. The mean FEV 0.5 was significantly lower in infants with CF both shortly after diagnosis and at the second test with 72% of infants having a value less than the fifth percentile. So the airway function is already diminished soon after diagnosis in infants with CF and does not catch up during infancy and early childhood. These findings have important implications for early interventions in CF.
2005 Fischer R, Lang SM, Brückner K, Hoyer HX, Meyer S, Griese M, Huber RM. Lung function in adults with cystic fibrosis at altitude: impact on air travel. Eur Respir J 2005; 25:718-724. [PubMed]
Current guidelines for air travel state that patients with chronic respiratory diseases are required to use oxygen if their in-flight arterial oxygen tensions (Pa,O2) drop below 6.6 kPa. This recommendation may not be strictly applicable to cystic fibrosis patients, who may tolerate lower Pa,O2 for several hours without clinical symptoms. Lung function, symptoms, blood gas levels and signs of pulmonary hypertension were studied in 36 cystic fibrosis patients at altitudes of 530 m and, after 7 h, 2,650 m. A hypoxia inhalation test (inspiratory oxygen fraction 0.15) was performed at low altitude in order to predict high-altitude hypoxaemia. Median Pa,O2 dropped from 9.8 kPa at low altitude to 7.0 kPa at high altitude. Mild exercise at a workload of 30 W further decreased Pa,O2. Two-thirds of all patients exhibited Pa,O2 of <6.6 kPa during exercise and, except for one patient, were asymptomatic. Patients were significantly less obstructed at an altitude of 2,650 m. Low forced expiratory volume in one second at baseline was associated with a low Pa,O2 at altitude. The authors concluded that cystic fibrosis patients with baseline arterial oxygen tensions of >8.0 kPa safely tolerate an altitude of 2,650 m for several hours under resting conditions. The risk assessment of low in-flight oxygenation should encompass the whole clinical situation of cystic fibrosis patients, with special attention being paid to the presence of severe airway obstruction.
2005 Aurora P, Bush A, Gustafsson P, Oliver C, Wallis C, Price J, Stroobant J, Carr S, Stocks J. London Cystic Fibrosis Collaboration. Multiple-breath washout as a marker of lung disease in preschool children with cystic fibrosis. Am J Resp Crit Care 2005; 171:249-256.[PubMed]
-

Paul Aurora
- Sensitive measures of lung function applicable to young subjects are needed to detect early cystic fibrosis (CF) lung disease. Forty children with CF aged 2 to 5 years and 37 age-matched healthy control subjects performed multiple-breath inert gas washout, plethysmography, and spirometry. Thirty children in each group successfully completed all measures, with success on first visit being between 68 and 86% for all three measures. Children with CF had significantly higher lung clearance index (mean [95% CI] difference for CF control 2.7 [1.9, 3.6], p < 0.001) and specific airway resistance (1.65 z-scores [0.96, 2.33], p < 0.001), and significantly lower forced expired volume in 0.5 seconds (-0.49 z-scores [-0.95, -0.03], p < 0.05). Abnormal lung function results were identified in 22 (73%) of 30 children with CF by multiple-breath washout, compared with 14 (47%) of 30 by plethysmography, and 4 (13%) of 30 by spirometry. Children with CF who were infected with Pseudomonas aeruginosa had significantly higher lung clearance index, but no significant difference in other lung function measures, when compared with non infected children. Most preschool children can perform multiple-breath washout, plethysmography, and spirometry at first attempt. Multiple-breath washout detects abnormal lung function in children with CF more readily than plethysmography or spirometry
Dr Paul Aurora is Consultant Paediatrician at Great Ormond Street Hospital for Children, London. He subsequently further developed this test for use in children with early lung disease (Aurora P. Thorax 2010; 65:373-374.[PubMed]). He also has a major involvement in the paediatric transplantation programme at Great Ormond Street.
2008 Linnane BM, Hall GL, Nolan G, Brennan S, Stick SM, Sly PD, Robertson CF, Robinson PJ, Franklin PJ, Turner SW, Ranganathan SC. AREST-CF. Lung function in infants with cystic fibrosis diagnosed by newborn screening. Am J Resp Critical Care 2008; 178:1238-1244.[PubMed]
A study to measure lung function in infants with CF diagnosed by newborn screening and describe its association with pulmonary infection and inflammation. Lung function, measured by forced expiration, is normal in infants with CF at the time of diagnosis by newborn screening but is diminished in older infants. These findings suggest that in CF the optimal timing of therapeutic interventions aimed at preserving lung function may be within the first 6 months of life.
2008 Gustafsson PM, De Jong PA, Tiddens HA, Lindblad A. Multiple-breath inert gas washout and spirometry versus structural lung disease in cystic fibrosis. Thorax 2008; 63:129-134. [PubMed].
The lung clearance index (LCI) from multiple-breath washout (MBW) is known to detect abnormal lung function more readily than spirometry in children and teenagers with CF, but its relationship to structural lung abnormalities is unknown. The authors concluded that LCI is a more sensitive indicator than FEV1 or FEF75 for detecting structural lung disease in CF, and a normal LCI almost excludes HRCT abnormalities. The finding of an abnormal LCI in some patients with normal HRCT scans suggests that LCI may be even more sensitive than HRCT scanning for detecting lung involvement in CF.
– The lung clearance index is gaining increasing support as a measure of early non-invasive lung function also useful in young children.
2009 Fuchs SI, Eder J, Ellemunter H. Gappa M. Lung clearance index: normal values, repeatability, and reproducibility in healthy children and adolescents. Pediatr Pulmonol 2009; 44:1180-1185.[PubMed]
The aim of this prospective study was to assess within-test repeatability, short term reproducibility and long term reproducibility, and to establish normal values for the LCI in healthy children and adolescents using the sidestream ultrasonic flow sensor (EasyOne Pro, MBW Module, ndd Medical Technologies, Switzerland).This study confirms the reliability and robustness of equipment, protocol and analysis and the reliability of the MBW technique in general. The present data will help to interpret the effect of therapeutic interventions and interpretation of longitudinal data in patients with pulmonary diseases.
– Further evidence that this test does seem to be an extremely useful.
2009 Horsley A. Lung clearance index in the assessment of airways disease. Respir Med 2009; 103:793-799. [PubMed]
In the last few years there has been a growing interest in lung clearance index (LCI), a measure of lung physiology derived from multiple breath washout tests. This resurgence of interest was initially driven by the recognition that such assessments were capable of detecting early airways disease in children, and are more sensitive and easier to perform in this population than conventional lung function tests [Aurora P, Kozlowska W, Stocks J. Gas mixing efficiency from birth to adulthood measured by multiple-breath washout. Respir Physiol Neurobiol, 2005;148(1-2):125-39]. With an appreciation of the importance of earlier identification of airways dysfunction, and prevention of irreversible structural airway changes, methods of following airways disease in these “silent years” are especially important. LCI has now been reported in studies involving all age groups, from infants to adults [Lum S, Gustafsson P, Ljungberg H, Hulskamp G, Bush A, Carr SB, et al. Early detection of cystic fibrosis lung disease: multiple-breath washout versus raised volume tests. Thorax, 2007;62(4):341-7; Horsley AR, Gustafsson PM, Macleod K, Saunders CJ, Greening AP, Porteous D, et al. Lung clearance index is a sensitive, repeatable and practical measure of airways disease in adults with cystic fibrosis. Thorax, 2008;63:135-40], and has a narrow range of normal over this wide age range, making it especially suitable for long-term follow-up studies. In cystic fibrosis (CF) particularly, there is a pressing need for sensitive and repeatable clinical endpoints for therapeutic interventions [Rosenfeld M. An overview of endpoints for cystic fibrosis clinical trials: one size does not fit all. Proc Am Thorac Soc, 2007;4(4):299-301], and LCI has been proposed as an outcome measure in future CF gene therapy studies [Davies JC, Cunningham S, Alton EW, Innes JA. Lung clearance index in CF: a sensitive marker of lung disease severity. Thorax, 2008;63(2):96-7]. This review will consider how LCI is derived, how it differs from conventional lung function testing, and its applications and limitations.
This is an detailed review of lung clearance index with many useful references so the abstract has been included in full. Does seem to be an important applicable advance in respiratory function testing.
2010 Ellemunter H, Fuchs SI, Unsinn KM, Freund MC, Waltner-Romen M, Steinkamp G, Gappa M. Sensitivity of Lung Clearance Index and chest computed tomography in early CF lung disease. Resp Med 2010; 104:1834-1842. [PubMed].
The aim of this study was to prospectively investigate the diagnostic accuracy of the lung clearance index (LCI) measured by multiple Breath Washout (MBW) in comparison to chest computed tomography (CT) in CF patients with early lung disease and normal FEV(1) (>80% pred. ). The diagnostic accuracy of the LCI for detecting CF lung disease in patients with normal FEV(1) was good when compared to CT. Results indicate that structural changes are unlikely if a normal LCI is measured. The authors suggest that serial measurements of the LCI for assessing ventilation inhomogeneity may help to identify early structural lung disease and help to reduce the individual cumulative radiation dose.
– Further evidence that LCI is a sensitive measure of even mild lung involvement in CF. It has the advantage of reducing the radiation to which people with CF are exposed over a lifetime. The technique appears to be a significant advance particularly as chest involvement is less gross in children but even so the early detection of abnormalities is crucial to avoid permanent progressive damage. LCI does seem to represent a significant advance. Paul Aurora from Great Ormond Street, London has published extensively in support of the technique.
2010 Amin R, Subbarao P, Jabar A, Balkovec S, Jensen R, Kerrigan S, Gustafsson P, Ratjen F. Hypertonic saline improves the LCI (lung clearance index) in paediatric patients with CF with normal lung function. Thorax 2010; 65:379-383. [PubMed]
The authors objective was to study the ability of the lung clearance index (LCI), a measure of ventilation inhomogeneity, to detect a treatment response to hypertonic saline inhalation in paediatric patients with CF with normal spirometry. In a crossover trial, 20 patients with CF received 4 weeks of hypertonic saline (HS) and isotonic saline (IS) in a randomised sequence separated by a 4 week washout period. The primary end point was the change in the LCI due to HS versus IS. Four weeks of twice-daily HS inhalation significantly improved the LCI compared with IS (1. 16, 95% CI 0. 26 to 2. 05; p=0. 016), whereas other outcome measures such as spirometry and quality of life failed to reach statistical significance. Randomisation order had no significant impact on the treatment effect. The LCI, but not spirometry was able to detect a treatment effect from HS inhalation in patients with CF with mild disease and may be a suitable tool to assess early intervention strategies in this patient population.
– The early administration of hypertonic saline has a definite effect on improving lung function as measured by the lung clearance index – a sensitive test that is steadily gaining in popularity particularly as more children with CF have normal spirometry.
2011 Kieninger E, Singer F, Fuchs O, Abbas C, Frey U, Regamey N, Casaulta C, Latzin P. Long-term course of lung clearance index between infancy and school-age in cystic fibrosis subjects. J Cyst Fibros 2011; 10:487-490. [PubMed]
Multiple breath washout (MBW) measurements have recently been shown to be sensitive for detection of early cystic fibrosis (CF) lung disease, with the lung clearance index (LCI) being the most common measure for ventilation inhomogeneity. The aim of this observational study was to describe the longitudinal course of LCI from time of clinical diagnosis during infancy to school-age in eleven children with CF. Elevated LCI during infancy was present in seven subjects, especially in those with later clinical diagnosis. Tracking of LCI at follow-up was evident only in the four most severe cases. These are the first longitudinal data describing the long-term course of LCI in a small group of infants with CF. Our findings support the clinical usefulness of MBW measurements to detect and monitor early lung disease in children with CF already present shortly after clinical diagnosis.
– See later study from Australia, mentioned below, which seems to cast doubt on the value of this tests in the first 2 years (Hall GL, et al. Air trapping on chest CT is associated with worse ventilation distribution in infants with cystic fibrosis diagnosed following newborn screening. PLoS ONE [Electronic Resource].2011; 6:e23932. [PubMed]).
2011 Aurora P, Stanojevic S, Wade A, Oliver C, Kozlowska W, Lum S, Bush A, Price J, Carr SB, Shankar A, Stocks J. London Cystic Fibrosis Collaboration. Lung clearance index at 4 years predicts subsequent lung function in children with cystic fibrosis. Am J Respir Crit Care 2011; 183:752-758. [PubMed]
There is an urgent need for alternative surrogates that detect early lung disease and track through early childhood. This study aimed to determine whether multiple-breath washout (MBW) results at preschool age can predict subsequent abnormal lung function. Preschool children (3-5 yr) with CF and healthy control subjects underwent spirometry and MBW with testing repeated during early school age (6-10 yr). Primary outcomes were FEV1 from spirometry and lung clearance index (LCI) from MBW. Forty-eight children with CF and 45 healthy children completed testing. Thirty-five (73%) children with CF had abnormal LCI at preschool age, whereas only five had abnormal FEV1. The positive predictive value of preschool LCI for predicting any abnormal school-age result was 94%, with a negative predictive value of 62%. Only one child with abnormal FEV1 at school age had had a normal preschool LCI. In contrast, for preschool FEV1 the positive predictive value was 100%, but negative predictive value was only 25%. The authors concluded that their study demonstrates that an abnormal preschool LCI predicts subsequent lung function abnormalities, whereas a normal preschool LCI usually remains normal. MBW has potential as a clinical and research outcome in young children with CF.
The fact that 35/48 (73%) of preschool CF children had an abnormal lung clearance index but only 5/45 (11%) had an abnormal FEV1 attests to the sensitivity of the LCI. An abnormal LCI in preschool children with CF predicts later abnormalities.
2011 Hall GL, Logie KM, Parsons F, Schulzke SM, Nolan G, Murray C, Ranganathan S, Robinson P, Sly PD, Stick SM, Berry L, Garratt L, Massie J, Mott L, Poreddy S, Simpson S. Air trapping on chest CT is associated with worse ventilation distribution in infants with cystic fibrosis diagnosed following newborn screening. PLoS ONE [Electronic Resource].2011; 6:e23932.[PubMed]
The primary objective of this analysis was to determine the relationships between ventilation distribution outcomes and the presence and extent of structural damage as assessed by chest CT in infants and young children with CF. The findings suggest that in early CF lung disease there are weak associations between ventilation distribution and lung damage from chest CT. These finding are in contrast to those reported in older children.
These findings suggest that assessments of lung clearance index could not be used to replace a chest CT scan for the assessment of structural lung disease in the first two years of life.
Further research is required to assess the role of ventilation distribution in tracking the progression of lung damage in infants with CF.
– The detection of even minor abnormalities in infants is of importance and the presence and severity correlated with later progressive damage. This paper lends caution to the suggestion that lung clearance index would be a useful method to follow lung involvement in the early years.
2012 Belessis Y, Dixon B, Hawkins G, Pereira J, Peat J, Macdonald R, Field P, Numa A, Morton J, Lui K, Jaffe A. Early cystic fibrosis lung disease detected by bronchoalveolar lavage and lung clearance index. Am J Resp Crit Care 2012; 185:862-873. [PubMed]
A study to determine whether the lung clearance index (LCI) is a sensitive and repeatable noninvasive measure of airway infection and inflammation in newborn-screened children with CF. Methods: Forty-seven well children with CF (mean age, 1.55 yr) and 25 healthy children (mean age, 1.26 yr) underwent multiple-breath washout testing. LCI within and between-test variability was assessed. Children with CF also had surveillance bronchoalveolar lavage performed.
Measurements and Main Results: The mean (SD) LCI in healthy children was 6.45 (0.49). The LCI was higher in children with CF (7.21 [0.81]; P < 0.001). The upper limit of normal for the LCI was 7.41. Fifteen (32%) children with CF had an elevated LCI. LCI measurements were repeatable and reproducible. Airway infection was present in 17 (36%) children with CF, including 7 (15%) with Pseudomonas aeruginosa. Polymicrobial growth was associated with worse inflammation. The LCI was higher in children with Pseudomonas (7.92 [1.16]) than in children without Pseudomonas (7.02 [0.56]) (P = 0.038). The LCI correlated with bronchoalveolar lavage IL-8 (R(2) = 0.20, P = 0.004) and neutrophil count (R(2) = 0.21, P = 0.001). An LCI below the upper limit of normality had a high negative predictive value (93%) in excluding Pseudomonas.
The authors concluded that the LCI is elevated (abnormal) early in children with CF, especially in the presence of Pseudomonas and airway inflammation. They suggest that LCI is a feasible, repeatable, and sensitive noninvasive marker of lung disease in young children with CF. The lung clearance index seems to be emerging as practical and accurate measure of airway function particularly useful in very young patients.
2012 Pittman JE, Johnson RC, Davis SD. Improvement in pulmonary function following antibiotics in infants with cystic fibrosis. Pediatr Pulmonol 2012; 47:441-446. [PubMed]
While pulmonary function testing (PFT) is often used to follow progression of lung disease and guide treatment in older children with CF, little data is available on change in infant PFTs in young children with CF. Pre- and post-antibiotics PFT data was available on 11 infants with CF, with a mean age of 102 weeks at time of first PFT. The majority of infants were symptomatic prior to antibiotics, and showed statistically significant improvement in clinical parameters following treatment. Prior to antibiotics, PFTs showed evidence of substantial obstructive disease. Following antibiotics, all of the parameters showed statistically significant improvement. The authors have shown a statistically significant improvement in infant PFT measures following antibiotic therapy in a cohort of 11 infants with CF, which paralleled improvement in clinical parameters. Though infant PFTs showed improvement, they remained abnormal in the majority of subjects, with persistent air-trapping and hyperinflation after antibiotic therapy. So these findings suggest that infant PFTs are sensitive to acute clinical changes in children with CF, and may be a useful tool in managing infants with CF.
These findings are to be expected but the increasing use of more accurate objective measurement in young CF infants is an important advance particularly as the emphasis is increasingly on very early intervention with treatment such as antibiotics, rhDNase and hypertonic saline. Once again the significant proportion of CF infants who already have changes in their respiratory function, even after antibiotic therapy, is apparent.
2012 Haidopoulou K, Lum S, Turcu S, Guinard C, Aurora P, Stocks J, Sonnappa S. Alveolar LCI vs. standard LCI in detecting early CF lung disease. Respir Physiol Neurobiol 2012; 180:247-251. [PubMed]
Multiple breath washout (MBW) is a sensitive technique that detects early airways disease. However in very young children, large equipment and physiological dead space relative to lung volumes may result in a higher Lung Clearance Index (LCI). The authors investigated whether alveolar LCI (aLCI) is a more sensitive index than standard LCI in children. MBW data-sets from children aged 0.1-10.7 years [97 healthy controls and 93 with cystic fibrosis (CF)] were analysed. LCI is traditionally calculated by dividing the cumulative expired volume (CEV) by functional residual capacity (FRC) after correcting for equipment dead space. aLCI was calculated similarly, but after correcting the CEV and FRC for Langley’s physiological dead space. There was a significant correlation between LCI and aLCI in health (r(2): 0.993; p<0.0001) and disease (r(2): 0.984; p<0.0001). Sensitivity of both LCI and aLCI in detecting abnormal lung function in CF was 39% during infancy, which increased to 77% and 83% respectively in older children. However, the difference in sensitivity (aLCI vs. LCI) was not significant (p=0.36).
The authors conclude that LCI is minimally affected by airway deadspace, or relative equipment deadspace, and is an appropriate measure of lung function in infancy.
– Further evidence supporting the use of lung clearance index in young children
2012 Hoo AF, Thai LP, Nguyen TT, Bush A, Chudleigh J, Lum S, et al. London Cystic Fibrosis Collaboration. Lung function is abnormal in 3-month-old infants with cystic fibrosis diagnosed by newborn screening. Thorax 2012; 67:874-881. [PubMed].(http://dx.doi.org/10.1136/thoraxjnl-2012-201747 for full text)
Long-term benefits of newborn screening (NBS) for cystic fibrosis (CF) have been established with respect to nutritional status, but effects on pulmonary health remain unclear. Lung clearance index (LCI) and functional residual capacity (FRC) using multiple breath washout (MBW), plethysmographic (pleth) FRC and forced expirations from raised lung volumes were measured in 71 infants with CF (participants in the London CF Collaboration) and 54 contemporaneous healthy controls age ∼3 months.
Compared with controls, and after adjustment for body size and age, LCI, FRC(MBW) and FRC(pleth) were significantly higher in infants with CF (mean difference (95% CI): 0.5 (0.1 to 0.9), p=0.02; 0.4 (0.1 to 0.7), p=0.02 and 0.9 (0.4 to 1.3), p<0.001, z-scores, respectively), while forced expiratory volume (FEV(0.5)) and flows (FEF(25-75)) were significantly lower (-0.9 (-1.3 to -0.6), p<0.001 and -0.7 (-1.1 to -0.2), p=0.004, z-scores, respectively). 21% (15/70) of infants with CF had an elevated LCI (>1.96 z-scores) and 25% (17/68) an abnormally low FEV(0.5) (below -1.96 z-scores). While only eight infants with CF had abnormalities of LCI and FEV(0.5), using both techniques identified abnormalities in 35% (24/68). Hyperinflation (FRC(pleth) >1.96 z-scores) was identified in 18% (10/56) of infants with CF and was significantly correlated with diminished FEF(25-75) (r=-0.43, p<0.001) but not with LCI or FEV(0.5).
The authors concluded that despite early diagnosis of CF by NBS and protocol-driven treatment in specialist centres, abnormal lung function, with increased ventilation inhomogeneity and hyperinflation and diminished airway function, is evident in many infants with CF diagnosed through NBS by 3 months of age.
– This is an important study from the UK’s leading paediatric respiratory group confirming that many screened CF infants already have abnormal lung function – 61% of the screened infants had had some respiratory symptoms (52% mild, 9% severe), 23% a positive cough swab and 73% had received antibiotics in addition to their routine prophylactic medication. With the exception of a significantly lower FEV0.5 in those who had received additional antibiotics for symptoms or positive cough swab, there was no significant association between LF outcomes and the infant’s genotype, clinical status, growth trajectory or treatment prior to the LFTs at 3 months of age.
It is perhaps encouraging that many infants who had been treated aggressively for respiratory exacerbations in the first few months had entirely normal LF by 3 months, whereas others with no prior symptoms or cause for concern had evidence of early lung disease. So damage from very early infection is not inevitable but does support the view that early specialised management is essential to achieve the maximum benefit from newborn CF screening.
2012 Vandenbranden SL, McMullen A, Schechter MS, Pasta DJ, Michaelis RL, Konstan MW, Wagener JS, Morgan WJ, McColley SA. Investigators and Coordinators of the Epidemiologic Study of Cystic Fibrosis. Lung function decline from adolescence to young adulthood in cystic fibrosis. Pediatr Pulmonol 2012; 47:135-143. [PubMed].
The authors identified 4,680 patients in the Epidemiologic Study of Cystic Fibrosis 1994-2005 with data in both adolescence (age 14.0-17.4 years) and young adulthood (age 18.5-22.0 years) and analyzed 2,267 who had >=5 encounters and >=5 measurements of forced expiratory volume in 1 second (FEV(1) ) spanning >=1 year during both adolescence and young adulthood, and >=1 encounter with weight and height and >=1 FEV(1) measurement age 17.5-18.5 years. They compared the annualized rates of decline in FEV(1) during adolescence and young adulthood stratified by best FEV(1) around age 18. Logistic regression was used to identify risk factors associated with substantial decline (>20 points) in FEV(1) % predicted in young adulthood.
The annual rate of decline was greater in young adulthood than in adolescence. Risk factors for substantial decline included slower rate of FEV(1) decline, greater FEV(1) variability, faster body mass index (BMI) decline, male sex, chronic inhaled antibiotics, Hemophilus influenzae detection, and absence of multidrug-resistant Pseudomonas aeruginosa in adolescence, and lower than expected FEV(1) and BMI around age 18.
The authors concluded that decline in lung function accelerates in young adults with CF, especially in those with early stage lung disease. Adolescents at risk for substantial decline in lung function in young adulthood have higher FEV(1) and worse nutritional status, among other identifiable risk factors.
2013 Horsley AR. Davies JC. Gray RD. Macleod KA. Donovan J. Aziz ZA. Bell NJ. Rainer M. Mt-Isa S. Voase N. Dewar MH. Saunders C. Gibson JS. Parra-Leiton J. Larsen MD. Jeswiet S. Soussi S. Bakar Y. Meister MG. Tyler P. Doherty A. Hansell DM. Ashby D. Hyde SC. Gill DR. Greening AP. Porteous DJ. Innes JA. Boyd AC. Griesenbach U. Cunningham S. Alton EW. Changes in physiological, functional and structural markers of cystic fibrosis lung disease with treatment of a pulmonary exacerbation. Thorax 2013; 68:532-9. [PubMed]
A study by members of the UK Gene Therapy Consortium to evaluate a range of conventional and novel biomarkers of CF lung disease in a multicentre setting as a contributing study in selecting outcome assays for their 2013-2014 clinical trial of CFTR gene therapy. Measurements were performed at commencement and immediately after a course of intravenous antibiotics. Disease activity was assessed using 46 assays across five key domains: symptoms, lung physiology, structural changes on CT, pulmonary and systemic inflammatory markers.
Statistically significant improvements were seen in forced expiratory volume in 1 s (p<0.001, n=32), lung clearance index (p<0.01, n=32), symptoms (p<0.0001, n=37), CT scores for airway wall thickness (p<0.01, n=31), air trapping (p<0.01, n=30) and large mucus plugs (p=0.0001, n=31), serum C-reactive protein (p<0.0001, n=34), serum interleukin-6 (p<0.0001, n=33) and serum calprotectin (p<0.0001, n=31).
The authors identified the key biomarkers of inflammation, imaging and physiology that alter alongside symptomatic improvement following treatment of an acute CF exacerbation. These data, in parallel with their study of biomarkers in patients with stable CF, provide important guidance in choosing optimal biomarkers for novel therapies. Further, they highlight that such acute therapy predominantly improves large airway parameters and systemic inflammation, but has less effect on airway inflammation.
The UK Gene Therapy Consortium commenced their multi-dose major gene therapy trial in June 2012 (Alton EW et al. Pediatr Pulmonol 2013; Suppl 36: Poster 245). This study helped to determine the parameters which would be used in the trial. The primary outcome chosen was the FEV1 and secondary outcomes the lung clearance index, CT changes and CFQ questionnaire. The trial will be completed around June 2014.
The Cystic Fibrosis Trust provided substantial funding for these studies and many other studies during the decade leading up to the gene therapy trial but was unable to fund the trial itself for which the GTC, due to the excellence of their work, were successful in achieving funding from the Medical Research Council Efficacy and Mechanism Evaluation (EME) funding.
2013 Adam RJ. Michalski AS. Bauer C. Abou Alaiwa MH. Gross TJ. Awadalla MS. Bouzek DC. Gansemer ND. Taft PJ. Hoegger MJ. Diwakar A. Ochs M. Reinhardt JM. Hoffman EA. Beichel RR. Meyerholz DK. Stoltz DA. Air trapping and airflow obstruction in newborn cystic fibrosis piglets. Am J Resp Crit Care 2013; 188:1434-41.[PubMed]
Air trapping and airflow obstruction are being increasingly identified in infants with cystic fibrosis. These findings are commonly attributed to airway infection, inflammation, and mucus build up. This study was to determine if air trapping and airflow obstruction are present before the onset of airway infection and inflammation in cystic fibrosis. On the day they are born, piglets with CF lack airway infection and inflammation so the authors used newborn wild-type piglets and piglets with CF to assess air trapping, airway size, and lung volume with inspiratory and expiratory X-ray computed tomography scans. Micro-computed tomography scanning was used to assess more distal airway sizes. Airway resistance was determined with a mechanical ventilator. Mean linear intercept and alveolar surface area were determined using stereologic methods.
On the day they were born, piglets with cystic fibrosis exhibited air trapping more frequently than wild-type piglets (75% vs. 12.5%, respectively). Moreover, newborn piglets with CF had increased airway resistance that was accompanied by luminal size reduction in the trachea, mainstem bronchi, and proximal airways. In contrast, mean linear intercept length, alveolar surface area, and lung volume were similar between both genotypes. The authors conclude that the presence of air trapping, airflow obstruction, and airway size reduction in newborn piglets with cystic fibrosis before the onset of airway infection, inflammation, and mucus accumulation indicates that cystic fibrosis impacts airway development. They suggest their findings suggest that early airflow obstruction and air trapping in infants with cystic fibrosis might, in part, be caused by congenital airway abnormalities.
– This is a fascinating study showing what has been suspected previously – that the airways of the newborn with CF are anatomically abnormal. Anatomical abnormalities have already been described in airways of CF piglets (Meyerholz DK et al, 2010. [PubMed] 20622026). The trachea and mainstem bronchi had a uniformly small calibre and cross-sections of trachea were less circular than in controls, the trachealis smooth muscle had an altered bundle orientation and increased transcripts in a smooth muscle gene set, the submucosal glands were hypoplastic and had global reductions in tissue-specific transcripts. To learn whether any of these changes occurred in young patients with CF, they examined CT scans from children 2 years of age and younger, and found that CF tracheas were less circular in cross-section, but lacked differences in lumen area. However, analysis of previously published morphometric data showed reduced tracheal lumen area in neonates with CF.
Occasionally the lower airway abnormalities are such that a young infant presents a clinical picture resembling tracheomalacia with intractable expiratory wheezing which gradually improves through infancy.
2013 Rosenfeld Mj, Arets BH, Aurora P, Beydon N, Calogero C, Castile RG, Davis SD, Fuchs S, Gappa M, Gustaffson PM, Hall GL, Jones MH, Kirkby JC, Kraemer R, Lombardi E, Lum S, Mayer OH, Merkus P, Nielsen KG, Oliver C, Oostveen E, Ranganathan S, Ren CL,, Robinson PD, Seddon PC, Sly PD, Sockrider MM, Sonnappa S, Stocks J, Subbarao P, Tepper RS, Vilozni D. American Thoracic Society Assembly on Pediatrics Working Group on Infant and Preschool Lung Function Testing. An official American Thoracic Society workshop report: optimal lung function tests for monitoring cystic fibrosis, bronchopulmonary dysplasia, and recurrent wheezing in children less than 6 years of age. Annals of the American Thoracic Society 2013; 10:S1-S11. [PubMed]
Official American Thoracic Society workshops were convened in 2009 and 2010 to review six lung function tests based on a comprehensive review of the literature (infant raised-volume rapid thoracic compression and plethysmography, preschool spirometry, specific airway resistance, forced oscillation, the interrupter technique, and multiple-breath washout). In these proceedings, the current state of the art for each of these tests is reviewed as it applies to the clinical management of infants and children under 6 years of age with cystic fibrosis, bronchopulmonary dysplasia, and recurrent wheeze, using a standardized format that allows easy comparison between the measures. Although insufficient evidence exists to recommend incorporation of these tests into the routine diagnostic evaluation and clinical monitoring of infants and young children with cystic fibrosis, bronchopulmonary dysplasia, or recurrent wheeze, they may be valuable tools with which to address specific concerns, such as ongoing symptoms or monitoring response to treatment, and as outcome measures in clinical research studies
As it is realised that very early treatment and monitoring are of crucial importaance to identify infection and reduce early lung damage this review is timely. Previously unavailable to many infants it appears feasible to use the newer techniques such as multiple breath washouts even infants.
2013 Singer F. Kieninger E. Abbas C. Yammine S. Fuchs O. Proietti E. Regamey N. Casaulta C. Frey U. Latzin P. Practicability of nitrogen multiple-breath washout measurements in a pediatric cystic fibrosis outpatient setting. Pediat Pulmonol 2013; 48:739-46. [PubMed]
Although lung clearance index (LCI) is a sensitive indicator of mild cystic fibrosis (CF) lung disease, it is rarely measured due to lengthy protocols and the commercial unavailability of multiple-breath washout (MBW) setups and tracer gases. We used a newly validated, commercially available nitrogen (N2 ) MBW setup to assess success rate, duration, and variability of LCI within a 20min timeframe, during clinical routine. We also evaluated the relationship between LCI and other clinical markers of CF lung disease. METHODS: One hundred thirty six children (83 with CF) between 4 and 16 years were studied in a pediatric CF outpatient setting. One hundred eighteen out of 136 children were naive to MBW. Within 20min, each child was trained, N2 MBW was performed, and LCI was analyzed. We assessed intra- and between-test reproducibility in a subgroup of children. RESULTS: At least one LCI was feasible in 123 (90%) children, with a mean (range) of 3.3 (1.2-6.4) min per test. Two or more measurements were feasible in 56 (41%) children. Comparing LCI in CF versus controls, LCI mean (SD) was 12.0 (3.9) versus 6.1 (0.9), and the intra- and inter-test coefficient of repeatability was 1.00 versus 0.81 and 0.96 versus 0.62, respectively. LCI was correlated with spirometry, blood gases, and Pseudomonas aeruginosa infection.
The authors concluded that using available N2 MBW equipment, LCI measurements are practical and fast in children. LCI is correlated with markers of CF lung disease.
2013 Subbarao P. Stanojevic S. Brown M. Jensen R. Rosenfeld M. Davis S. Brumback L. Gustafsson P. Ratjen F. Lung clearance index as an outcome measure for clinical trials in young children with cystic fibrosis. A pilot study using inhaled hypertonic saline. Am J Respir Crit Care 2013; 188:456-60. [PubMed]
To study the feasibility of using LCI to assess treatment effect outcomes in CF trials of infants and preschoolers. The Infant Study of Inhaled Saline trial was a multicenter, randomized, controlled trial of hypertonic (7%) versus isotonic (0.9%) saline inhaled twice daily for 48 weeks in children with CF under 6 years of age.
LCI measurements were performed in a single-center pilot substudy at baseline and 48 weeks using a respiratory mass spectrometer and sulfur hexafluoride as the tracer gas. LCI measurements were standardized using published normative data (zLCI) to account for height-related changes in LCI during early childhood. A generalized estimating equation model with an interaction between treatment group and test occasion was used to estimate a treatment effect.
A total of 27 participants were randomized; 25 participants, aged (median [range]) 2.6 (0.34-4.95) years, had acceptable baseline and follow-up LCI measures. On average, LCI decreased in the hypertonic saline group (n = 12) by 1.19 z-scores units (95% confidence interval [CI] = -2.46 to 0.06), and remained stable in the isotonic saline group (n = 13) at 0.81 (95% CI = -0.40 to 2.02).
A significant treatment effect was observed for zLCI (2.01; 95% CI = 0.26 to 3.76; P = 0.025)
The authors concluded that multiple breath washout (MBW) testing is feasible in an interventional study in infants and preschool children with CF. These pilot findings support the development of MBW and LCI as an objective outcome measure in interventional trials in young children with CF, and provide estimates for sample size calculations for future studies.
– The lung clearance index appears to be deservedly gaining general acceptance as a measure of respiratory function in prescchool children – such an important age group as the need for early intervention and its effects become increasingly apparent.
2014 Kent L. Reix P. Innes JA. Zielen S. Le Bourgeois M. Braggion C. Lever S. Arets HG. Brownlee K. Bradley JM. Bayfield K. O’Neill K. Savi D. Bilton D. Lindblad A. Davies JC. Sermet I. De Boeck K. European Cystic Fibrosis Society Clinical Trial Network (ECFS-CTN) Standardisation Committee. Lung clearance index: evidence for use in clinical trials in cystic fibrosis. J Cyst Fibros 2014;13(2):123-38. [PubMed]
The ECFS-CTN Standardisation Committee has undertaken this review of lung clearance index as part of the group’s work on evaluation of clinical endpoints with regard to their use in multicentre clinical trials in CF. It was concluded that LCI has an attractive feasibility and clinimetric properties profile and is particularly indicated for multicentre trials in young children with CF and patients with early or mild CF lung disease.
This is the first article to collate the literature in this manner and support the use of LCI in clinical trials in CF. This is a method of respiratory function testing, applicable to all age groups, has undoubtedly been one of the major advaces in recent years.
2014 Nguyen TT. Thia LP. Hoo AF. Bush A. Aurora P. Wade A. Chudleigh J. Lum S. Stocks J. London Cystic Fibrosis Collaboration (LCFC). Evolution of lung function during the first year of life in newborn screened cystic fibrosis infants. Thorax 2014; 69:910-7.[PubMed]
A study to assess changes in pulmonary function during the first year of life in CF infants detected by newborn screening. CF NBS infants and healthy controls were recruited between 2009 and 2011. Lung Clearance Index (LCI), plethysmographic lung volume (plethysmographic functional residual capacity (FRCpleth)) and forced expired volume (FEV 0.5) were measured at 3 months and 1 year of age.
Paired measurements were obtained from 72 CF infants and 44 controls. At 3 months, CF infants had significantly worse lung function for all tests. FEV 0.5 improved significantly (0.59 (95% CI 0.18 to 0.99) z-scores; p<0.01) in CF infants between 3 months and 1 year, and by 1 year, FEV 0.5 was only 0.52 (0.89 to 0.15) z-scores less than in controls. LCI and FRCpleth remained stable throughout the first year of life, being on average 0.8 z-scores higher in infants with CF. Pulmonary function at 1 year was predicted by that at 3 months. Among the 45 CF infants with entirely normal LCI and FEV 0.5 at 3 months, 80% remained so at 1 year, while 74% of those with early abnormalities remained abnormal at 1 year.
This is the first study reporting improvements in FEV 0.5 over time in stable NBS CF infants treated with standard therapy. Milder changes in lung function occurred by 1 year than previously reported. Lung function at 3 months predicts a high-risk group, who should be considered for intensification of treatment and enrolment into RCTs. A very interesting study from the London CF Collaboration with implications for early management. The importance of early involvement and of identifying this early at risk group at 3 months, who may require more intensive treatment and supervision (at a specialist centre rather than care shared with a local hospital), is emphasised.
2014 Rodriguez Hortal MC. Hjelte L. Time point to perform lung function tests evaluating the effects of an airway clearance therapy session in cystic fibrosis. Respir Care 2014; 59:1537-41.2014.[PubMed]
The authors found that performing spirometry 30 min after a session in adults and immediately after in children appeared to be optimal if individual peak time values cannot be used.
2014 Welsh L, Robertson C F, Ranganathan SC. Increased rate of lung function decline in Australian adolescents with cystic fibrosis. Pediatr Pulmonol 2014; 49:873-7. [PubMed]

Liam Welsh
Although baseline lung function as measured by spirometry in children with cystic fibrosis has improved, the annual rate of decline has not changed significantly during the critical period of adolescence. The aim of this study was to describe factors associated with longitudinal decline in lung function in a contemporary cohort of children with CF.
The authors confirmed that FEV(1) declines at its sharpest rate during adolescence even in the presence of newborn screening. Genotype, increasing age, CFRD, PsA infection, pancreatic insufficiency and a greater number of respiratory hospitalizations are all associated with an increased rate of lung function decline in Australian children and adolescents with cystic fibrosis.
– This data from Melbourne confirms the tendency for decline in respiratory function to be a frequent occurrence during adolescence.
Liam Welsh (figure) is Senior Scientist in the Respiratory Unit at the Royal Children’s Hospital Melborne.
2015 Banton GL, Hall GL, Tan M, Skoric B, Ranganathan SC, Franklin PJ, Pillow JJ, Schulzke SM, Simpson SJ. Multiple breath washout cannot be used for tidal breath parameter analysis in infants. Pediatr Pulmonol. 2015 Oct 5. doi: 10.1002/ppul.23326. [Epub ahead of print][PubMed]
Multiple breath washout (MBW) testing with SF6 gas mixture is routinely used to assess ventilation distribution in infants. It is currently unknown whether SF6 changes tidal breathing parameters during MBW in infants. We investigated if SF6 does change tidal breathing parameters in infants and whether a separate tidal breathing trace prior to MBW testing is necessary.
The authors found differences in tidal breathing parameters during MBW testing with SF6 in infants. It is, therefore, important to measure a separate tidal breathing trace in room air, prior to MBW testing to ensure rigour of tidal breath indices derived from analysis.
2015 Davis SD, Ratjen F, Brumback LC, Johnson RC, Filbrun AG, Kerby GS, Panitch HB, Donaldson SH, Rosenfeld M; ISIS Study Group. Infant lung function tests as endpoints in the ISIS multicenter clinical trial in cystic fibrosis. J Cyst Fibros. 2015 Nov 4. pii: S1569-1993(15)00249-0. doi: 10.1016/j.jcf.2015.10.007. [Epub ahead of print] [PubMed]
The Infant Study of Inhaled Saline (ISIS) in CF was the first multicenter clinical trial to utilise infant pulmonary function tests (iPFTs) as an endpoint. However, the authors concluded iPFTs are, as yet, not appropriate primary endpoints for multicenter clinical trials due to challenges of obtaining acceptable data and near-normal average raised volume measurements. However, they suggest raised volume measures have potential to serve as secondary endpoints in future clinical CF trials.
2013 Davies J, Sheridan H, Bell N, Cunningham S, Davis SD5, Elborn JS, Milla CE, Starner TD, Weiner DJ, Lee PS, Ratjen F. Assessment of clinical response to ivacaftor with lung clearance index in cystic fibrosis patients with a G551D-CFTR mutation and preserved spirometry: a randomised controlled trial. Lancet Respir Med. 2013 Oct;1(8):630-8. doi: 10.1016/S2213-2600(13)70182-6. Epub 2013 Sep 10. [PubMed]
Lung clearance index (LCI) using multiple-breath washout might be an alternative to and more sensitive method than forced expiratory volume in 1 s (FEV1) to assess treatment response in the growing number of children and young adults with cystic fibrosis who have normal spirometry. The aim of the study was to assess the treatment effects of ivacaftor on LCI in patients with cystic fibrosis, a G551D-CFTR mutation, and an FEV1 >90% predicted.
This phase 2, multicentre, placebo-controlled, double-blind 2×2 crossover study of ivacaftor treatment was conducted in patients with cystic fibrosis, at least one G551D-CFTR allele, and an FEV1 >90% predicted. Patients also had to have an LCI higher than 7·4 at screening, age of 6 years or older, and a weight higher than or equal to 15 kg. Eligible patients were randomly allocated to receive one of two treatment sequences (placebo first followed by ivacaftor 150 mg twice daily [sequence 1] or ivacaftor 150 mg twice daily first followed by placebo [sequence 2]) of 28 days’ treatment in each period, with a 28-day washout between the two treatment periods. Randomisation (ratio 1:1) was done with block sizes of 4, and all site personnel including the investigator, the study monitor, and the Vertex study team were masked to treatment assignment. The primary outcome measure was change from baseline in LCI.
Between February and November, 2011, 21 patients were enrolled, of which 11 were assigned to the sequence 1 group, and 10 to the sequence 2 group. 20 of these patients received treatment and 17 completed the trial (eight in sequence 1 group and 9 in sequence 2 group).
Treatment with ivacaftor led to significant improvements compared with placebo in LCI (difference between groups in the average of mean changes from baseline at days 15 and 29 was -2·16 [95% CI -2·88 to -1·44]; p<0·0001). Adverse events experienced by study participants were similar between treatment groups; at least one adverse event was reported by 15 (79%) of 19 patients who received placebo and 13 (72%) of 18 patients who received ivacaftor.
The authors concluded that in patients with cystic fibrosis aged 6 years or older who have at least one G551D-CFTR allele, ivacaftor led to improvements in Lung Clearance Index. They suggest that LCI might be a more sensitive alternative to FEV1 in detecting response to intervention in these patients with mild lung disease.
2015 Lenherr N, Lurà M, Trachsel D, Latzin P, Hammer J. Ivacaftor in a young boy with the rare gating mutation S549R – use of lung clearance index to track progress: a case report. BMC Pulm Med. 2015 Oct 16;15:123. doi: 10.1186/s12890-015-0120-1. Free PMC article [PubMed]
S549Ris a rare gating mutation considered to be less sensitive to potentiators such as ivacaftor than all other gating mutations. An 8-year-old boy with the rare S549R gating mutation treated with ivacaftor had subjective clinical improvements, the sweat chloride level and the lung clearance index decreased impressively within a few weeks of treatment while forced expiratory volume in the first and second values remained in normal range.
– The authors emphasise the value of measuring small airway function by lung clearance index as an outcome measure for new interventions targeting the correction of the CFTR defect at an age before traditional lung function parameters start to deteriorate.
2015 Matecki S, Kent L, de Boeck K, Le Bourgeois M, Zielen S, Braggion C, Arets HG, Bradley J, Davis S, Sermet I, Reix P; respiratory function group of the European Cystic Fibrosis Society Clinical Trial Network. Is the raised volume rapid thoracic compression technique ready for use in clinical trials in infants with cystic fibrosis? J Cyst Fibros. 2015 Apr 15. pii: S1569-1993(15)00070-3. doi: 10.1016/j.jcf.2015.03.015. [Epub ahead of print][PubMed]
The aim of this article is to present a review of literature on clinimetric properties of the infant raised-volume rapid thoracic compression (RVRTC) technique in the context of CF, to summarise the consensus amongst the group on feasibility and answer key questions regarding the promotion of this technique to surrogate endpoint status.
The ECFS-CTN Working Group considers that RVRTC cannot be used as a primary outcome in clinical trials in infants with CF before universal standardization of this measurement is achieved and implementation of inter-institutional networking is in place. They advise its use currently in phase I/II trials and as a secondary endpoint in phase III studies and emphasise the need for (1) more short-term variability and longitudinal ‘natural history’ studies, and (2) robust reference values for commercially available devices.
2014 Ramsey KA, Ranganathan S, Park J, Skoric B, Adams AM, Simpson SJ, Robins-Browne RM, Franklin PJ, de Klerk NH, Sly PD, Stick SM, Hall GL; AREST CF. Early respiratory infection is associated with reduced spirometry in children with cystic fibrosis. Am J Respir Crit Care Med 2014; 190(10):1111-6. doi: 10.1164/rccm.201407-1277OC.
Lung function (forced expiratory volume in the first three-quarters of a second [FEV0.75], FVC) was assessed in individuals with cystic fibrosis diagnosed after newborn screening and healthy subjects during infancy (0-2 yr) and again at early school age (4-8 yr). Individuals with cystic fibrosis underwent annual bronchoalveolar lavage fluid examination, and chest computed tomography. They determined which clinical outcomes (pulmonary inflammation, infection, structural lung disease, respiratory hospitalisations, antibiotic prophylaxis) measured in the first 2 years of life were associated with reduced lung function in infants and young children with cystic fibrosis, using a mixed effects model.
Children with cystic fibrosis (n = 56) had 8.3% (95% confidence interval [CI], -15.9 to -6.6; P = 0.04) lower FEV0.75 compared with healthy subjects (n = 18). Detection of pro-inflammatory bacterial pathogens in bronchoalveolar lavage fluid was associated with clinically significant reductions in FEV0.75 (ranging between 11.3 and 15.6%).
The onset of lung disease in infancy, specifically the occurrence of lower respiratory tract infection, is associated with low lung function in young children with cystic fibrosis. Deficits in lung function measured in infancy persist into childhood, emphasising the need for targeted therapeutic interventions in infancy to maximise functional outcomes later in life.
– More evidence that intervention against infection must be very early in CF infants if the decline in respiratory function is to be minimised or hopefully even avoided. The UK CF Trust Antibiotic Working Group’s recommendation of longterm flucloxacillin for CF infants from birth for at least the first 3 years seems to be supported by recent studies of this type.
2015 Subbarao P; Milla C; Aurora P; Davies JC; Davis SD; Hall GL; Heltshe S; Latzin P; Lindblad A; Pittman JE; Robinson PD; Rosenfeld M; Singer F; Starner TD; Ratjen F; Morgan W. Multiple-Breath Washout as a Lung Function Test in Cystic Fibrosis. A Cystic Fibrosis Foundation Workshop Report. Ann Amer Thorac Soc 2015; 12(6):932-9. [PubMed]
This workshop, of distinguished attendees, concluded that the Multiple Brehttp://www.sickkids.ca/images/Staff%20profiles/9748-011549.jpgath Washout (MBW) test is a valuable potential outcome measure for CF clinical trials in preschool-aged patients and in older patients
with FEV1 in the normal range. However, gaps in knowledge about the choice of device, gas, and standardisation across systems are key issues precluding its use as a clinical trial end point in infants. Based on the current evidence, they concluded there are insufficient data to support the use of Lung Clearance Index or MBW parameters in the routine clinical management of patients with CF.
– This attractive, non-invasive, test has received considerable attention and evaluation in recent years, particularly as a measure of respiratory function in young children. It is likely to gain general acceptance as a measure of respiratory function in young patients and represents a major advance
2015 Sonneveld N, Stanojevic S, Amin R, Aurora P, Davies J, Elborn JS, Horsley A, Latzin P, O’Neill K, Robinson P, Scrase E, Selvadurai H, Subbarao P, Welsh L, Yammine S, Ratjen F. Lung clearance index in cystic fibrosis subjects treated for pulmonary exacerbations. Eur Respir J. 2015 Oct; 46(4):1055-64. doi: 10.1183/09031936.00211914. Epub 2015 Jul 9. [PubMed]
A systematic literature search was performed to identify prospective observational studies. Factors predicting the relative change in LCI and spirometry were evaluated while adjusting for within-study clustering. Six previously reported studies and one unpublished study, which included 176 pulmonary exacerbations in both paediatric and adult patients, were included. Overall, LCI significantly decreased by 0.40 units (95% CI −0.60– −0.19, p=0.004) or 2.5% following treatment. The relative change in LCI was significantly correlated with the relative change in forced expiratory volume in 1 s (FEV1), but results were discordant in 42.5% of subjects (80 out of 188). Higher (worse) baseline LCI was associated with a greater improvement in LCI (slope: −0.9%, 95% CI −1.0– −0.4%). LCI response to therapy for pulmonary exacerbations is heterogeneous in CF patients; the overall effect size is small and results are often discordant with FEV1. A retrospective analysis of pooled LCI data to assess treatment with intravenous antibiotics for pulmonary exacerbations in CF and to understand factors explaining the heterogeneous response.
The study confirms that LCI does decrease significantly in patients with CF treated for a pulmonary exacerbation. However the overall effect size was smaller for LCI than for FEV1, and there was discordance between FEV1 and LCI.
The authors suggest future studies should assess how treatment response assessed by LCI is linked to the subsequent course of lung disease as well as long-term outcomes.
2015 Sanders B, Emerson J, Ren CL, Schechter MS, Gibson RL, Morgan W, Rosenfeld M; EPIC Study Group. Early Childhood Risk Factors for Decreased FEV1 at Age Six to Seven Years in Young Children with Cystic Fibrosis. Ann Am Thorac Soc. 2015; 12(8):1170-6. doi: 10.1513/AnnalsATS.201504-198OC.
To evaluate early childhood predictors of lung function at age 6-7 in a large U.S. CF cohort in the current era of widespread early eradication therapy for P. aeruginosa. Participants were children with CF enrolled before age 4 in the Early Pseudomonas Infection Control (EPIC) Observational Study, a multicenter, longitudinal study that enrolled P. aeruginosa-negative children not exceeding 12 years of age. Linear regression was used to estimate the association between potential early childhood risk factors and the best FEV1% predicted at age 6-7 years.
Four hundred and eighty-four children (of 1,797 enrolled in the EPIC Observational Study) met the eligibility criteria for this analysis. Mean (SD) age at enrolment was 2.0 (1.3) years.
In a multivariable model adjusted for age at enrolment, the following risk factors were significantly associated with lower mean (95% confidence interval) FEV1% predicted at age 6-7: weight percentile less than 10% during the year of enrolment (-5.3 [-9.1, -1.5]), P. aeruginosa positive during the year of enrolment (-2.8 [-5.7, 0.0]), crackles or wheeze during the year of enrolment (-5.7 [-9.4, -1.9]), mother’s education of high school or less (-4.2 [-7.3, -1.2]), and mother smoked during pregnancy (-4.4 [-8.8, 0.1]).
In this large U.S. cohort, the authors identified several early childhood risk factors for lower FEV1 at age 6-7 years, most of which are modifiable.
– Most of the factors identified are predictable and have been suggested in previous studies but it is good to have them clearly documented in a alrge population.
2015 Schultz A, Stick S. Early pulmonary inflammation and lung damage in children with cystic fibrosis. Respirology 2015 Mar 30. doi: 10.1111/resp.12521. [Epub ahead of print]
Individuals with cystic fibrosis (CF) suffer progressive airway inflammation, infection and lung damage. Airway inflammation and infection are present from early in life, often before children are symptomatic. CF gene mutations cause changes in the CF transmembrane regulator protein that result in an aberrant airway microenvironment including airway surface liquid (ASL) dehydration, reduced ASL acidity, altered airway mucin and a dysregulated inflammatory response. This review discusses how an altered microenvironment drives CF lung disease before overt airway infection, the response of the CF airway to early infection, and methods to prevent inflammation and early lung disease.
– Already there are a number of significant structural changes in the CF infant by the time of birth as evidenced by the often severe pancreatic changes (figure: neonatal CF pancreas). These changes permitted Dorothy Andersen to recognise CF as a distinct entity among the many marasmic infants that came to postmortem in New York during the Thirties. These changes are likely to be irreversible as may also be the case with the prenatal changes in the lung where early structural and inflammatory changes, even in the fetus, have been described and reviewed (Verhaeghe C et al. J Cyst Fibros 2007; 6:304-308. [PubMed] Full text of an interesting review), the possibility of inflammatory changes being related to ion channel abnormalities was suggested.
2015 Sanders B, Emerson J, Ren CL, Schechter MS, Gibson RL, Morgan W, Rosenfeld M; EPIC Study Group. Early Childhood Risk Factors for Decreased FEV1 at Age Six to Seven Years in Young Children with Cystic Fibrosis. Ann Am Thorac Soc. 2015; 12(8):1170-6. doi: 10.1513/AnnalsATS.201504-198OC. [PubMed]
To evaluate early childhood predictors of lung function at age 6-7 in a large U.S. CF cohort in the current era of widespread early eradication therapy for P. aeruginosa. Participants were children with CF enrolled before age 4 in the Early Pseudomonas Infection Control (EPIC) Observational Study, a multicenter, longitudinal study that enrolled P. aeruginosa-negative children not exceeding 12 years of age. Linear regression was used to estimate the association between potential early childhood risk factors and the best FEV1% predicted at age 6-7 years.
Four hundred and eighty-four children (of 1,797 enrolled in the EPIC Observational Study) met the eligibility criteria for this analysis. Mean (SD) age at enrolment was 2.0 (1.3) years.
In a multivariable model adjusted for age at enrolment, the following risk factors were significantly associated with lower mean (95% confidence interval) FEV1% predicted at age 6-7: weight percentile less than 10% during the year of enrolment (-5.3 [-9.1, -1.5]), P. aeruginosa positive during the year of enrolment (-2.8 [-5.7, 0.0]), crackles or wheeze during the year of enrolment (-5.7 [-9.4, -1.9]), mother’s education of high school or less (-4.2 [-7.3, -1.2]), and mother smoked during pregnancy (-4.4 [-8.8, 0.1]).
In this large U.S. cohort, the authors identified several early childhood risk factors for lower FEV1 at age 6-7 years, most of which are modifiable.
– Most of the factors identified are predictable and have been suggested in previous studies but it is good to have them clearly documented in such a large population.
2015 Hall H; Gadhok R; Alshafi K; Bilton D; Simmonds NJ. Eradication of respiratory tract MRSA at a large adult cystic fibrosis centre. Respir Med 2015; 109(3):357-63. [PubMed]
This is an observational cohort study from the Royal Brompton Hospital of all patients with MRSA positive sputum, 2007-2012. All eradication attempts with subsequent culture results were reviewed. Single vs. dual antibiotic regimens were compared for both new and chronic infections.
37 patients (median FEV1 58.7 (27.6-111.5)% predicted) were identified, of which 67.6% (n = 25) had newly acquired MRSA. Compared with single regimens, a high proportion of dual regimens achieved MRSA eradication (84.6% vs. 50%; p = 0.1) for new infections. Rifampicin/Fusidic acid was associated with high success rates (100% vs. 60% for other dual regimens (p = 0.13)). Compared with new infections, chronic MRSA was much less likely to be eradicated (18.2%, p = 0.01).
The authors concluded combined antibiotic therapy, particularly Rifampicin/Fusidic acid, is a well-tolerated and effective means of eradicating MRSA in patients with cystic fibrosis.
2016 Amin R; Stanojevic S; Kane M; Webster H; Ratjen F. A randomized controlled trial to evaluate the lung clearance index as an outcome measure for early phase studies in patients with cystic fibrosis. Resp Med 2016; 112:59-64. [PubMed]
T he authors investigated whether the lung clearance index (LCI) measured by multiple breath washout (MBW) can detect a treatment effect of hypertonic saline (HS) inhalation after single dosing within a 24 h period. In this cross over trial CF patients received inhalation of HS and isotonic saline (IS). MBW and spirometry were performed at 5 time points over 24 h. LCI was measured using both a nitrogen washout technique (LCIN2) and sulfur hexafluoride as a tracer gas (LCISF6). The primary endpoint was the change in the LCIN2 between baseline and 24 h. Secondary endpoints included change in LCISF6 and spirometry outcomes.
Twenty-one patients were randomized. Sixteen completed all study visits and all time point measurements. Eighteen patients contributed to the intention to treat analysis. Significant changes were not detected for either LCI or the spirometry outcomes. However, the primary outcome parameter (change in LCI between the baseline visits and 24 h after inhalation) demonstrated a trend towards improved LCI, in the HS treatment arm compared with the IS treatment arm, -0.60 LCIN2 (SE 0.32), p = 0.08); similar trends were not observed for spirometric measures. The overall effect size of HS was smaller than in previous studies of longer duration. The authors concluded these data suggest that LCI may potentially be used as an outcome measure in early phase trials with therapeutic agents that have a larger treatment effects than a single inhalation of HS.
2016 Davis SD, Ratjen F, Brumback LC, Johnson RC, Filbrun AG, Kerby GS, Panitch HB, Donaldson SH, Rosenfeld M; ISIS Study Group. Infant lung function tests as endpoints in the ISIS multicenter clinical trial in cystic fibrosis. J Cyst Fibros 2016; 15(3):386-91.[PubMed]

Stephanie Davis
The Infant Study of Inhaled Saline (ISIS) in CF was the first multicenter clinical trial to utilise infant pulmonary function tests (iPFTs) as an endpoint. Secondary analysis of ISIS data was conducted in order to assess feasibility of iPFT measures and their associations with respiratory symptoms. The authors concluded iPFTs are not appropriate primary endpoints for multicenter clinical trials due to challenges of obtaining acceptable data and near-normal average raised volume measurements. However, raised volume measures have potential to serve as secondary endpoints in future clinical CF trials
Dr Stephanie Davis (figure) is a Paediatric Pulmonologist and Professor of Pediatrics at Indiana School of Medi
2016 Ellemunter H; Eder J; Fuchs S; Gappa M; Steinkamp G. Long-term improvement of lung clearance index in patients with mild cystic fibrosis lung disease: Does hypertonic saline play a role?. J Cyst Fibros 2016; 15(1):123-6. [PubMed]

Gratiana Steinkamp

H Ellemunter
To assess whether long-term inhalation with hypertonic saline is able to halt the progression of mild CF lung disease, we analysed longitudinal data of lung clearance index (LCI) and spirometry. A total of 34 patients with mild lung disease (FEV1 > 70% of predicted) had at least one LCI result before and >2 LCI measurements after start of hypertonic saline (HS) therapy. After a mean follow-up of 39.7 (SD 7.4) months after starting HS, LCI improved significantly from 7.89 (SD 1.35) at baseline to 6.96 (SD 1.03), and 19/34 patients had a normal LCI value at the last measurement. No decrease in mean FEV1 was observed. Thus, ventilation inhomogeneity can improve in patients with mild lung disease
The authors, whilst admitting the drawbacks of the study, in particular the retrospective file evaluation of longitudinal MBW and spirometry measurements, observed a statistically significant and clinically relevant improvement in LCI over three years of hypertonic saline inhalation, in parallel with stable FEV1 results. This was in sharp contrast to the one percent yearly decline in FEV1 observed before starting HS. They suggest that the deterioration of lung disease can be halted in mildly affected patients, provided that early lung disease is detected with sensitive methods and treatment is adjusted accordingly.
– A number of previous publications have reported normal LCI values for children (Fuchs SI et al 2009 [PubMed]). Mean LCI (SD) on three occasions was 6.2 (0.4), 6.3 (0.4), and 6.0 (0.4) at the 1st, 2nd, and 3rd test. The upper limit of normal was 7.0 for all subjects. Within-test repeatability was 5.1%. Short-term reproducibility (1st test vs. 2nd test) was 4.2% with a mean difference of -0.13 (95% CI -0.350; 0.087). Long-term reproducibility (1st test vs. 3rd test) was 5.1%, with a mean difference of 0.017 (95% CI -0.016; 0.348).
– This record of experience is certainly valuable and encouraging although essentially “real world” rather than a clinical trial.
Dr. med. Gratiana Steinkamp (figure) is a self-employed medical writer and free scientist with a focus on lung diseases. She has been working with cystic fibrosis patients since 1983. In 1986 she started a position at Hannover Medical School as the first full-time CF physician in Germany. During the following years, the Hannover CF-Centre became one of the three largest specialized institutions in Germany.
2016 Levine H; Cohen-Cymberknoh M; Klein N; Hoshen M; Mussaffi H; Stafler P; Breuer O; Kerem E; Blau H. Reversible airway obstruction in cystic fibrosis: Common, but not associated with characteristics of asthma. J Cyst Fibros 2016; 15(5):652-9. [PubMed

Hagit Levine
As asthma-like symptoms are common in CF, the authors evaluated reversible airway obstruction and associated characteristics by a retrospective analysis of charts including spirometry and bronchodilator response.Of 190 CF patients (103 at Schneider’s, 87 at Hadassah clinic), aged 14.4 (4-76) years, median (range), 39% had reversible obstruction (DELTAFEV1% predicted >12%), associated with younger age (p=0.01) and severe genotype (p=0.02). There was no association with family history of asthma, serum IgE, blood eosinophils, pancreatic status, FEV1<40% predicted, Aspergillus or Pseudomonas infection.Of the 39% of patients with reversible obstruction, 74% were on bronchodilator and 68% on inhaled corticosteroid therapy but 54% and 57% respectively receiving these therapies did not have reversible obstruction.
The authors confirmed that reversible airway obstruction is common in CF, more frequent in younger patients and those with severe genotype, with no correlation to markers of atopy or CF clinical severity. Bronchodilator and inhaled corticosteroid therapies are commonly prescribed even for patients without reversible obstruction.
– During the treatment of an exacerbation if twice daily respiratory function is performed (even with a simple peak flow meter) before and after a bronchodilator, the degree of reversibility lessens each day during the course of IV antibiotic treatment as the inflammation is controlled and respiratory function improves. So in this situation the reversibility certainly does appear to be related to the severity of the inflammation. Ian Balfour Lynn has described the frequent, and at times apparently unnecessary, use of inhaled corticosteroids in the UK even in those patients with no reversibility (Balfour-Lynn IM et al. Am J Respir Crit Care Med 2006; 173(12): 1356-62). However, it is important to recognise the minority of CF patients who do respond impressively to inhaled steroids – presumably those in Balfour—Lynn’s study whose parents refused to enter the steroid withdrawal trial.
Dr Hagit Levine (figure)) is Paediatric Pulmonologist at Schneiders Children’s Hospital. Israel.
2016 Matecki S; Kent L; de Boeck K; Le Bourgeois M; Zielen S; Braggion C; Arets HG; Bradley J; Davis S; Sermet I; Reix P; respiratory function group of the European Cystic Fibrosis Society Clinical Trial Network. Is the raised volume rapid thoracic compression technique ready for use in clinical trials in infants with cystic fibrosis?. [Review] J Cyst Fibros 2016; 15(1):10-20[PubMed]
The European Cystic Fibrosis Society Clinical Trial Network (ECFS-CTN) has established a Standardization Committee to undertake a rigorous evaluation of promising outcome measures with regard to use in multicentre clinical trials in cystic fibrosis (CF). The aim of this article is to present a review of literature on clinimetric properties of the infant raised-volume rapid thoracic compression (RVRTC) technique in the context of CF, to summarise the consensus amongst the group on feasibility and answer key questions regarding the promotion of this technique to surrogate endpoint status.
2016 Nielsen AO; Qayum S; Bouchelouche PN; Laursen LC; Dahl R; Dahl M. Risk of asthma in heterozygous carriers for cystic fibrosis: A meta-analysis. J Cyst Fibros 2016; 15(5):563-7. [PubMed]
The authors screened the medical literature from 1966 to 2015 and performed a meta-analysis to determine the risk of asthma in CF heterozygotes vs. non-carriers. Aggregating data from 15 studies, the odds ratio for asthma in CF heterozygotes compared with non-carriers was significantly elevated at 1.61 (95% CI: 1.18-2.21) showing that heterozygous carriers for CF have a higher risk of asthma than non-carriers.
– There are similar findings by Schultz and Tummler
2016 Schulz A; Tummler B. Non-allergic asthma as a CFTR-related disorder. J Cyst Fibros 2016; 15(5):641-4. [PubMed].
Subjects with cystic fibrosis-like disease, equivocal sweat chloride concentrations and no or one disease-causing CFTR mutation were investigated by intestinal current and/or nasal potential difference measurements. A subgroup of 7 female patients who had been diagnosed to suffer from non-allergic asthma showed intermediary chloride concentrations in sweat test, normal chloride secretory responses in the intestine and an abnormal nasal potential difference with Sermet scores in the cystic fibrosis range.
The authors concluded non-allergic asthma is a clinical entity that may be associated with CFTR dysfunction of the respiratory epithelium. Nasal potential difference is a rapid reliable and cost effective CFTR biomarker to identify subjects with CFTR related disorder among patients with non-allergic asthma or idiopathic bronchiectasis.
2016 O’Neill K; Tunney MM; Johnston E; Rowan S; Downey DG; Rendall J; Reid A; Bradbury I; Elborn JS; Bradley JM. Lung clearance index in adults and children with cystic fibrosis. Chest. , 2016 Jul 6 [PubMed]
Lung clearance index (LCI) has good clinimetric properties and an acceptable feasibility profile as a surrogate endpoint in Cystic Fibrosis (CF). Although most studies to date have been in children, increasing numbers of adults with CF also have normal spirometry. Further study of LCI as an endpoint in CF adults is required. Therefore, the purpose of this study was to determine the clinimetric properties of LCI over the complete age range of people with CF.Clinically stable adults and children with CF and age matched healthy controls were recruited. LCI and spirometry data for 110 CF subjects and 61 controls were collected at a stable visit. CF Questionnaire-Revised (CFQ-R) was completed by 80/110 CF subjects. Fifty-six CF subjects completed a second stable visit. The LCI CV% was 4.1% in adults and 6.3% in children with CF. The coefficient of repeatability of LCI was 1.2 in adults and 1.3 in children. In both adults and children, LCI (AUC(ROC)=0.93 and 0.84) had greater combined sensitivity and specificity to discriminate between people with CF and controls compared to FEV1 (AUC(ROC)=0.88 and 0.60) and FEF25-75 (AUC(ROC)=0.87 and 0.68). LCI correlated significantly with the CFQ-R treatment burden in adults (r=-0.37; p<0.01) and children (r=-0.50; p<0.01). Washout tests were successful in 90% of CF subjects and were perceived as comfortable and easy to perform in both adults and children.
The authors consider these data support the use of LCI as a surrogate outcome measure in CF clinical trials in adults as well as children.
2016 Ramsey KA, Rosenow T, Turkovic L, Skoric B, Banton G, Adams AM, Simpson SJ, Murray C, Ranganathan SC, Stick SM, Hall GL; AREST CF. Lung Clearance Index and Structural Lung Disease on Computed Tomography in Early Cystic Fibrosis. Am J Respir Crit Care Med. 2016 Jan 1;193(1):60-7. doi: 10.1164/rccm.201507-1409OC. [PubMed

Sally Ramsay
The lung clearance index is a measure of ventilation distribution derived from the multiple-breath washout technique. It has been suggested as a surrogate for chest computed tomography to detect structural lung abnormalities in individuals with cystic fibrosis; however, the associations between lung clearance index and early structural lung disease are unclear. The authors assessed the ability of the lung clearance index to reflect structural lung disease on the basis of chest computed tomography across the entire pediatric age range. dr kathryn RamseyrDRDrDd
In infants with CF, lung clearance index is insensitive to structural disease (κ = -0.03 [95% confidence interval, -0.05 to 0.16]). In preschool children with CF, lung clearance index correlates with total disease extent. In school-age children, lung clearance index correlates with extent of total disease, bronchiectasis, and air trapping. In preschool and school-age children, lung clearance index has a good positive predictive value (83-86%) but a poor negative predictive value (50-55%) to detect the presence of bronchiectasis.
The authors observe these data suggest that lung clearance index may be a useful surveillance tool to monitor structural lung disease in preschool and school-age children with CF. However, lung clearance index cannot replace chest computed tomography to screen for bronchiectasis in this population.
Dr Kathryn Ramsey (figure) is Ambizone Research fellow , Inelspital, Universitatsspital, Bern.
Comment–Florian Singer, Carmen Casaulta, and Philipp Latzin “How to Monitor Early Cystic Fibrosis Lung Disease. By Multiple-Breath Washout, Chest Computed Tomography, or Both?” American Journal of Respiratory and Critical Care Medicine, Vol. 193, No. 1 (2016), pp. 7-8. [PubMed]
2016 Stanojevic S, Davis SD, Retsch-Bogart G, Webster H, Davis M, Johnson RC, Jensen R, Pizarro ME, Kane M, Clem CC, Schornick L, Subbarao P, Ratjen FA. Progression of Lung Disease in Preschool Patients with Cystic Fibrosis. Am J Respir Crit Care Med. 2016 Dec 12. [Epub ahead of print] [PubMed]
Implementation of intervention strategies to prevent lung damage in early cystic fibrosis (CF) requires objective outcome measures that capture and track lung disease. A study to define the utility of the Lung Clearance Index (LCI), measured by Multiple Breath Washout (MBW), as a means to track disease progression in preschool children with CF.
CF children between the ages of 2.5 and 6 years with a confirmed diagnosis of CF and age-matched healthy controls were enrolled at three North American CF centres. MBW tests were performed at baseline 1, 3, 6 and 12 months to mimic time points chosen in clinical care and interventional trials; spirometry was also conducted. A generalised linear mixed-effects model was used to distinguish LCI changes associated with normal growth and development (i.e. healthy children) from the progression of CF lung disease.
Data were collected on 156 participants with 800 LCI measurements. While both LCI and spirometry discriminated health from disease, only the LCI identified significant deterioration of lung function in CF over time. The LCI deteriorated worsened during cough episodes as well as pulmonary exacerbations, whereas similar symptoms in healthy children were not associated with increased LCI values.
The authors concluded that LCI is a useful marker to track early disease progression and may serve as a tool to guide therapies in young patients with cystic fibrosis.
2016 Tepper LA; Caudri D; Rovira AP; Tiddens HA; de Bruijne M. The development of bronchiectasis on chest computed tomography in children with cystic fibrosis: can pre-stages be identified?. Eur Radiol 2016 Apr 23. [PubMed]

Leonie Tepper
Bronchiectasis is an important component of cystic fibrosis (CF) lung disease but little is known about its development. We aimed to study the development of bronchiectasis and identify determinants for rapid progression of bronchiectasis on chest CT. Forty-three patients with CF with at least four consecutive biennial volumetric CTs were included. Areas with bronchiectasis on the most recent CT were marked as regions of interest (ROIs). These ROIs were generated on all preceding CTs using deformable image registration. Observers indicated whether: bronchiectasis, mucus plugging, airway wall thickening, atelectasis/consolidation or normal airways were present in the ROIs.
They identified 362 ROIs on the most recent CT. In 187 (51.7 %) ROIs bronchiectasis was present on all preceding CTs, while 175 ROIs showed development of bronchiectasis. In 139/175 (79.4 %) no pre-stages of bronchiectasis were identified. In 36/175 (20.6 %) bronchiectatic airways the following pre-stages were identified: mucus plugging (17.7 %), airway wall thickening (1.7 %) or atelectasis/consolidation (1.1 %). Pancreatic insufficiency was more prevalent in the rapid progressors compared to the slow progressors (p=0.05).
Most bronchiectatic airways developed within 2 years without visible pre-stages, underlining the treacherous nature of CF lung disease. Mucus plugging was the most frequent pre-stage.In conclusion the authors observed the development of bronchiectasis in cystic fibrosis lung disease on CT. Most bronchiectatic airways developed within 2 years without pre-stages. The most frequently identified pre-stage was mucus plugging. They emphasise their study underlines the treacherous nature of CF lung disease.
– With the widespread introduction of neonatal CF screening increasing attention has been given to the recognition and treatment of early lung infection and damage. This study indicates the difficulty in identifying early damage from infection. Possibly combining clinical symptoms, bacteriological, biochemical and hematological data would perhaps improve recognition. For example the value of a persisting, even if mild, new cough is a valuable sign of unwelcome activity in the lower airways and should be treated aggressively!
Dr. Leonie Tepper (figure) is a member of the CF team at Erasmus MC Sophia , Rotterdam.
2016 Wielputz MO; Eichinger M; Biederer J; Wege S; Stahl M; Sommerburg O; Mall MA; Kauczor HU; Puderbach M. Imaging of Cystic Fibrosis Lung Disease and Clinical Interpretation.Rofo: Fortschritte auf dem Gebiete der Rontgenstrahlen und der Nuklearmedizin. 188(9):834-45, 2016 Sep. [PubMed]
Chest X-ray (CXR), computed tomography (CT) and magnetic resonance imaging (MRI) are now available as routine modalities, each with individual strengths and drawbacks, which need to be considered when choosing the optimal modality adapted to the clinical situation of the patient. CT stands out with the highest morphological detail and has often been a substitute for CXR for regular severity monitoring at specialized centers. Multidetector CT data can be post-processed with dedicated software for a detailed measurement of airway dimensions and bronchiectasis and potentially a more objective and precise grading of disease severity. However, changing to CT was inseparably accompanied by an increase in radiation exposure of CF patients, a young population with high sensitivity to ionizing radiation and lifetime accumulation of dose. MRI as a cross-sectional imaging modality free of ionizing radiation can depict morphological hallmarks of CF lung disease at lower spatial resolution but excels with comprehensive functional lung imaging, with time-resolved perfusion imaging currently being most valuable.
KEY POINTS:* Hallmarks are bronchiectasis, mucus plugging, air trapping, perfusion abnormalities, and emphysema.* Imaging is more sensitive to disease progression than lung function testing.* CT provides the highest morphological detail but is associated with radiation exposure.* MRI shows comparable sensitivity for morphology but excels with additional functional information.* MRI sensitively depicts reversible abnormalities such as mucus plugging and perfusion abnormalities.
2017 Fidler MC, Beusmans J, Panorchan P, Van Goor F. Correlation of sweat chloride and percent predicted FEV1 in cystic fibrosis patients treated with ivacaftor. J Cyst Fibros. 2017 Jan;16(1):41-44. doi: 10.1016/j.jcf.2016.10.002. Epub 2016 Oct 20.[Pubmed]
Several previous analyses have reported no statistical correlation between change from baseline in ppFEV1 and reduction in sweat chloride levels for individuals treated with ivacaftor. The objective of the post hoc analysis described here was to expand upon previous analyses and evaluate the correlation between sweat chloride levels and absolute ppFEV1 changes across multiple cohorts of patients with different CF-causing mutations who were treated with ivacaftor. The goal of the analysis was to help define the potential value of sweat chloride as a pharmacodynamic biomarker for use in CFTR modulator trials.
The authors concluded that for any given study, reductions in sweat chloride levels and improvements in absolute ppFEV1 were not correlated for individual patients. However, when the data from all studies were combined, a statistically significant correlation between sweat chloride levels and ppFEV1changes was observed (p<0.0001). Thus, sweat chloride level changes in response to potentiation of the CFTR protein by ivacaftor appear to be a predictive pharmacodynamic biomarker of lung function changes on a population basis but are unsuitable for the prediction of treatment benefits for individuals.
– See also two articles by Vermeulen F in these 2017 abstracts and the Editorial by Burkhard Tummler.
2017 P, Le Bourgeois M, Chiron R, Molinari N, Saguintaah M, Amsallem F, Matecki S. Early follow-up of lung disease in infants with cystic fibrosis using the raised volume rapid thoracic compression technique and computed tomography during quiet breathing. Pediatr Pulmonol. 2017 Oct;52(10):1283-1290. doi: 10.1002/ppul.23786. Epub 2017 Sep 1.[Pubmed]
Among the different techniques used to monitor lung disease progression in infants with CF diagnosed by newborn screening (NBS), raised volume-rapid thoracic compression (RVRTC) remains a promising tool. However, the need for sedation and positive pressure ventilation considerably limits its clinical use. The authors recently described a semi-quantitative method to evaluate air trapping by chest tomography during quite breathing without sedation (CTqb score). This parameter is the radiological sign of airway obstruction and could be also used for lung disease follow-up in infants with CF. However, its discriminative power compared with RVRTC and correlation with lung function parameters are not known.
The aim of this study was to compare the discriminative powers of the CTqb score and RVRTC parameters and to determine their correlation during the first year of life of infants with CF. In this multicentre longitudinal study, infants with CF diagnosed by NBS underwent RVRTC and CT during quite breathing at 10 ± 4 weeks (n = 30) and then at 13 ± 1 months of age (n = 28).
All RVRTC parameters and the CTqb score remained stable between evaluations. The CTqb score showed a higher discriminative power than forced expiratory volume in 0.5 s (FEV0.5 ; the main RVRTC parameter) at both visits (66% and 50% of abnormal values vs 30% and 28%, respectively). No correlation was found between CTqb score and, the different RVRTC parameters or the plethysmographic functional residual capacity, indicating that they evaluate different aspect of CF lung disease.
~ This is a multi centre study from France. Dr Remi Gauthier is from the Pediatric Functional Exploration Unit, Hôpital Nord, Amiens University Hospital, Amiens, France.
2016 O’Neill K; Tunney MM; Johnston E; Rowan S; Downey DG; Rendall J; Reid A; Bradbury I; Elborn JS; Bradley JM. Lung Clearance Index in Adults and Children With Cystic Fibrosis. Chest. 150(6):1323-1332, 2016 Dec. [Pubmed]

Katherine O’Neill
Lung clearance index (LCI) has good clinimetric properties and an acceptable feasibility profile as a surrogate end point in cystic fibrosis (CF). Although most studies to date have been in children,increasing numbers of adults with CF also have normal spirometric findings. Further study of LCI as an end point in adults with CF is required. Therefore, the purpose of this study was to determine the clinimetric properties of LCI across the age range of people with CF. Clinically stable adults and children with CF and age-matchedhealthy control subjects were recruited. LCI and spirometry data for 110 subjects with CF and 61 control subjects were collected at a stable visit. The CF Questionnaire-Revised (CFQ-R) was completed by 80 of 110 subjects with CF. Fifty-six subjects with CF completed a second stable visit. The LCI coefficient of variation percent was 4.1% in adults and 6.3% in children with CF. The coefficient of repeatability of LCI was 1.2 in adults and 1.3 in children. In both adults and children, LCI (area under the receiving operator characteristic curve [AUCROC] = 0.93 and 0.84, respectively) had greater combined sensitivity and specificity to discriminate between people with CF and control subjects when compared with FEV1 (AUCROC = 0.88 and 0.60,respectively) and forced expiratory flow at 25% to 75% of the curve (AUCROC = 0.87 and 0.68, respectively). LCI correlated significantly with the CFQ-R treatment burden in adults (r = -0.37; P < .01) and children (r= -0.50; P < .01). Washout tests were successful in 90% of subjects with CF and were perceived as comfortable and easy to perform in both adults and children. The authors suggest these data support the use of LCI as a surrogate outcome measure in CF clinical trials in adults as well as in children.
2017 O’Neill K, Moran F, Tunney MM, Elborn JS, Bradbury I, Downey DG, Rendall J, Bradley JM. Timing of hypertonic saline and airway clearance techniques in adults with cystic fibrosis during pulmonary exacerbation: pilot data from a randomised crossover study. Open Respir Res. 2017 Jan 12;4(1):e000168. doi: 10.1136/bmjresp-2016-000168. eCollection 2017.[Pubmed]
The optimal timing of treatment with hypertonic saline (HTS) and airway clearance techniques (ACT) is unknown. This study hypothesised that HTS before ACT would be more effective than HTS during ACT as measured by Lung Clearance Index (LCI). Thirteen adults with CF providing written informed consent were randomised to a crossover trial of HTS before ACT or HTS during ACT on consecutive days. ACT treatment consisted of Acapella Duet.
In this pilot study, HTS before ACT was no more effective than HTS during ACT as measured by LCI.
– One would imagine that taking the hypertonic saline before rather than after ACT would be more effective but this appears not to be the case. Interestingly, it is also the case that rhDNase is just as effective whether taken before or after airway clearance; in fact in one study those chronically infected with P. aeruginosa derived more benefit when administered after physiotherapy (Dentice R, Elkins M. Timing of dornase alpha inhalation for cystic fibrosis. Cochrane Database Syst Rev 2011;(5):Cd007923). Dentice and Elkins most recent advice is –“in the absence of strong evidence to indicate that one timing regimen is better than another, the timing of dornase alpha inhalation can be largely based on pragmatic reasons or individual preference with respect to the time of airway clearance and time of day. They suggest further research is warranted ‘[Pubmed]
~ Although the usual conclusion of Cochrane Reviewers is that “further research is warranted” it would seem reasonable to take their present advice and time the hypertonic saline according to the benefit and life style of the patient.
2017 Stahl M, Wielpütz MO, Graeber SY, Joachim C, Sommerburg O, Kauczor HU, Puderbach M, Eichinger M, Mall MA. Comparison of Lung Clearance Index and Magnetic Resonance Imaging for Assessment of Lung Disease in Children with Cystic Fibrosis. J Respir Crit Care Med. 2017 Feb 1;195(3):349-359. doi: 10.1164/rccm.201604-0893OC.[Pubmed]

Mirjam Stahl
A study to correlate the LCI with abnormalities detected by MRI and compare the sensitivity of the two techniques to detect responses to therapy for pulmonary exacerbations in children with CF.
LCI determined by age-adapted multiple breath washout techniques and MRI studies were performed in 97 clinically stable children with CF across the pediatric age range (0.2-21.1 yr). Furthermore, LCI (n = 26) or MRI (n = 10) were performed at the time of pulmonary exacerbation and after antibiotic therapy. MRI was evaluated using a dedicated morphofunctional score.
The LCI correlated with the global MRI score as well as MRI-defined airway wall abnormalities, mucus plugging, and abnormal lung perfusion in infants and toddlers (P < 0.05 to P < 0.001) and in older children (P < 0.001) with CF. LCI and MRI were sensitive to detect response to antibiotic therapy for pulmonary exacerbations.
Their results indicate that LCI and MRI may be useful complementary tools for noninvasive monitoring and as quantitative endpoints in early intervention trials in children with CF. In this context, MRI enables detection of disease heterogeneity, including regional mucus plugging associated with abnormal lung perfusion in early CF lung disease.
Dr Mirjam Stahl (figure) is Principal Investigator of the Translational Lung Research Center Heidelberg and the German Center for Lung Research.
2017 Stanojevic S; Davis SD; Retsch-Bogart G; Webster H; Davis M; Johnson RC; Jensen R; Pizarro ME; Kane M; Clem CC; Schornick L; Subbarao P; Ratjen FA. Progression of Lung Disease in Preschool Patients with Cystic Fibrosis. Am J Respir Crit Care Med 2017; 195(9):1216-1225, 2017 May 01.[Pubmed]
A study to define the utility of the Lung Clearance Index (LCI), measured by multiple breath washout, as a means to track disease progression in preschool children with CF. Children with CF between the ages of 2.5 and 6 years with a confirmed diagnosis of CF and age-matched healthy control subjects were enrolled at three North American CF centers. Multiple breath washout tests were performed at baseline, 1, 3, 6, and 12 months to mimic time point chosen in clinical care and interventional trials; spirometry was also conducted. A generalised linear mixed-effects model was used to distinguish LCI changes associated with normal growth and development (i.e., healthy children) from the progression of CF lung disease.
Data were collected on 156 participants with 800 LCI measurements.
Although both LCI and spirometry discriminated health from disease, only the LCI identified significant deterioration of lung function in CF over time. The LCI worsened during cough episodes and pulmonary exacerbations, whereas similar symptoms in healthy children were not associated with increased LCI values.
The authors concluded that LCI is a useful marker to track early disease progression and may serve as a tool to guide therapies in young patients with CF.
2017 Stephen MJ, Long A, Bonsall C, Hoag JB, Shah S, Bisberg D, Holsclaw D, Varlotta L, Fiel S, Du D, Zanni R, Hadjiliadis D. Daily spirometry in an acute exacerbation of adult cystic fibrosis patients. Chron Respir Dis. 2017 Jan 1:1479972317743756. doi: 10.1177/1479972317743756. [Epub ahead of print] [Pubmed]
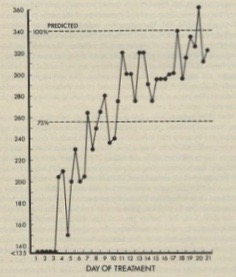
Twice daily peak flow rates during treatment of a severe exacerbation of chest infection
To help answer the question of length of intravenous antibiotics during an acute exacerbation of cystic fibrosis (CF), we had subjects to follow daily home spirometry while on intravenous antibiotics. CF patients, 18 and older, with an acute exacerbation requiring intravenous antibiotics had a daily FEV1. The average time to a 10% increase over their initial sick FEV1 was calculated, as well as the time to a new baseline. A total of 25 subjects completed the study. Ten of the 25 subjects did not have a sustainable 10% increase in FEV1. Of the 15 subjects with a sustainable 10% increase in FEV1, it took 5.2 days (±4.5) after day 1, while a new baseline was achieved on average at 6.6 days (±4.8) after day 1. Given the wide range of time to a 10% improvement and new baseline, it is recommended there should be flexibility in length of intravenous antibiotics in CF, not by a pre-set number
– This seems to be a helpful approach as, for a variety of reasons, patients differ in their response to antibiotic treatment. For many years in the Leeds Regional CF Centre we recorded the twice-daily Peak Expiratory Flow rates of children undergoing a course of IV antibiotic treatment (figure) ; this was continued until the values plateaued. Failure to improve each day would prompt a search for the reason/s. The twice-daily PFRs would usually be measured before and after a bronchodilator to note the usual reduction in bronchial lability that occurs during effective treatment.
2018 Korten I, Kieninger E, Yammine S, Cangiano G, Nyilas S, Anagnostopoulou P, Singer F, Kuehni CE, Regamey N, Frey U, Casaulta C, Spycher BD, Latzin P; SCILD; BILD study group Respiratory rate in infants with cystic fibrosis throughout the first year of life and association with lung clearance index measured shortly after birth. J Cyst Fibros. 2018 Jul 27. pii: S1569-1993(18)30696-9. doi: 10.1016/j.jcf.2018.07.002. [Epub ahead of print] 30060960 [Pubmed]

Philippe Latin
Lung impairment in cystic fibrosis (CF) starts in infancy. However,tools to monitor early lung disease are limited. Respiratory rate (RR) as a key vital sign is easy to assess during sleep and is elevated during acute respiratory disease. Thus, elevated RR could indicate early lung impairment and potentially serve as a diagnostic tool in disease monitoring. In a prospective cohort of infants with CF diagnosed by newborn screening and healthy controls RR was measured and respiratory symptoms reported weekly throughout infancy. Infants performed a lung function measurement within the first weeks of life. The analyses included 5656 measurements from 153 infants (43 with CF). RR declined from 43.2 (40.5)/min at 6 weeks of age to 28.3 (24.6)/min at 50 weeks in infants with CF (healthy controls). Infants with CF had consistently higher RR than controls (mean difference: 4.15/min; (95% CI 2.86-5.44); p < .001). In both study groups, RR was increased throughout the study period in infants with higher lung clearance indices (LCI) and during episodes of respiratory infections
The authors concluded infants with CF have a higher RR compared to healthy controls during the first year of life. The association with early LCI measurements, the current gold standard to assess physiology of peripheral airways, persisted throughout the study period. This may indicate tracking of lung function by RR. It might thus be an early subtle sign of functional respiratory deficit. Further studies will show if RR can be used as a sensitive and promising marker to monitor early CF lung disease.
The corresponding author, Philippe Latzin is Head of Paediatric Pulmonology at University of Berne Children’s Hospital.
2018 Kim SO, Corey M, Stephenson AL, Strug LJ. Reference percentiles of FEV1 for the Canadian cystic fibrosis population: comparisons across time and countries.Thorax. 2018 Feb 6. pii: thoraxjnl-2017-210899. doi: 10.1136/thoraxjnl-2017-210899. [Epub ahead of print][Pubmed
Forced expiratory volume in 1 s (FEV1) indicates lung health in cystic fibrosis (CF). FEV1 is commonly communicated as a per cent predicted of a healthy individual sharing the same age, sex, race and height. CF-specific reference equations are complementary and calibrate a patient’s FEV1 to that of their CF peers. Objectives were
(1) To derive Canadian CF-specific FEV1 reference percentiles (FEV1%iles), (2) characterize how they have changed over time and (3) compare the Canadian FEV1%iles to those for USA and European CF populations. CF FEV1%iles are calculated using the Canadian CF Registry and quantile regression. The Canadian FEV1%iles demonstrated better lung function in more recent time periods within Canada, especially below the 50% percentile and in males. When compared to USA and European FEV1%iles for the same time period, Canadian FEV1%iles were higher. The authors concluded CF-specific FEV1%iles can provide useful information about changes in lung health. An online calculator (available at cfpercentilesickkids.ca) makes these FEV1%iles accessible.
Dr S O Kim Division of Biostatistics, Dalla Lana School of Public Health, University of Toronto, Toronto, Canada.
2018 Foong RE, Harper AJ, Skoric B, King L, Turkovic L, Davis M, Clem CC, Rosenow T, Davis SD, Ranganathan S, Hall GL, Ramsey KA.The clinical utility of lung clearance index in early cystic fibrosis lung disease is not impacted by the number of multiple-breath washout trials. ERJ Open Res. 2018 Feb 16;4(1). pii: 00094-2017. doi: 10.1183/23120541.00094-2017. eCollection 2018 Jan [Pubmed] Free PMC Article

Rachel E Foong
The lung clearance index (LCI) from the multiple-breath washout (MBW) test is a promising surveillance tool for pre-school children with cystic fibrosis (CF). Current guidelines for MBW testing recommend that three acceptable trials are required. However, success rates to achieve these criteria are low in children aged <7 years and feasibility may improve with modified pre-school criteria that accepts tests with two acceptable trials. This study aimed to determine if relationships between LCI and clinical outcomes of CF lung disease differ when only two acceptable MBW trials are assessed. Healthy children and children with CF aged 3-6 years were recruited for MBW testing. Children with CF also underwent bronchoalveolar lavage fluid collection and a chest computed tomography scan. MBW feasibility increased from 46% to 75% when tests with two trials were deemed acceptable compared with tests where three acceptable trials were required. Relationships between MBW outcomes and markers of pulmonary inflammation, infection and structural lung disease were not different between tests with three acceptable trials compared with tests with two acceptable trials. This study indicates that pre-school MBW data from two acceptable trials may provide sufficient information on ventilation distribution if three acceptable trials are not possible.
Dr Rachel E Foong is an NHMRC Early Research Career Fellow with the Children’s Health Team, Telethon Kids Institute
2018 Newsome SJ, Daniel RM, Carr SB, Bilton D, Keogh RH.Investigating the effects of long-term dornase alfa use on lung function using registry data.J Cyst Fibros. 2018 Aug 29. pii: S1569-1993(18)30747-1. doi: 10.1016/j.jcf.2018.08.004. [Epub ahead of print]30172681 Full text available. [Pubmed]

Simon Newsome
Dornase alfa (DNase) is one of the commonest cystic fibrosis treatments and is often used for many years. However, studies have not evaluated the effectiveness of its long-term use. The authors aimed to use UK CF Registry data to investigate the effects of one-, two-, three-, four- and five-years of DNase use on lung function to see if the benefits of short-term treatment use are sustained long term. They analysed data from 4,198 people in the UK CF Registry from 2007 to 2015 using g-estimation. By controlling for time-dependent confounding they estimated the effects of long-term DNase use on percent predicted FEV1 (ppFEV1) and investigated whether the effect differed by ppFEV1 Considering the population as a whole, there was no significant effect of one-year’s use of DNase; change in ppFEV1 over one year was -0.1% in the treated compared to the untreated (p = 0.51) and this did not change with long-term use. However, treatment was estimated to be more beneficial in people with lower lung function (p < 0.001); those with ppFEV1 < 70% at treatment initiation, showed an increase in lung function over one year that was sustained out to five years. The estimated effect of DNase did not depend on age (p = 0.35).
They concluded DNase improved lung function in individuals with reduced lung function, bringing a step-change in lung function, but no change in the slope of decline. There was no evidence for a benefit in lung function in those initiating treatment with ppFEV1 > 70%.
Simon Newsome is a Research Degree Student in Medical Statistics at the London School of Hygiene and Tropical Medicine. He has published previously on cardiovascular topics and the UK CF Registry.
2017 Ronan NJ, Einarsson GG, Twomey M, Mooney D, Mullane D, NiChroinin M, O’Callaghan G, Shanahan F, Murphy DM, O’Connor OJ, Shortt CA, Tunney MM, Eustace JA, Maher MM, Elborn JS, Plant BJ. CORK Study in Cystic Fibrosis: Sustained Improvements in Ultra-Low-Dose Chest CT Scores After CFTR Modulation With Ivacaftor. Chest. 2018 Feb;153(2):395-403.doi: 10.1016/j.chest.2017.10.005. Epub 2017 Oct 14[Pubmed]
Ivacaftor produces significant clinical benefit in patients with cystic fibrosis (CF) with the G551D mutation. Prevalence of this mutation at the Cork CF Centre is 23%. This study assessed the impact of cystic fibrosis transmembrane conductance regulator modulation on multiple modalities of patient assessment. Thirty-three patients with the G551D mutation were assessed at baseline and prospectively every 3 months for 1 year after initiation of ivacaftor. Change in ultra-low-dose chest CT scans, blood inflammatory mediators, and the sputum microbiome were assessed. Significant improvements in FEV1, BMI, and sweat chloride levels were observed post-ivacaftor treatment. Improvement in ultra-low-dose CT imaging scores were observed after treatment, with significant mean reductions in total Bhalla score (P < .01), peribronchial thickening (P = .035), and extent of mucous plugging (P < .001). Reductions in circulating inflammatory markers, including interleukin (IL)-1β, IL-6, and IL-8 were demonstrated. There was a 30% reduction in the relative abundance of Pseudomonas species and an increase in the relative abundance of bacteria associated with more stable community structures. Post treatment community richness increased significantly (P = .03).
The authors concluded early and sustained improvements on ultra-low-dose CT scores suggest it may be a useful method of evaluating treatment response. It paralleled improvement in symptoms, circulating inflammatory markers, and changes in the lung microbiota
2018 Stahl M, Wielpütz MO, Ricklefs I, Dopfer C, Barth S, Schlegtendal A, Graeber SY, Sommerburg O, Diekmann G, Hüsing J, Koerner-Rettberg C, Nährlich L, Dittrich AM, Kopp MV, Mall MA.Preventive Inhalation of Hypertonic Saline in Infants with Cystic Fibrosis (PRESIS): A Randomized, Double-Blind, Controlled Study.Am J Respir Crit Care Med. 2018 Nov 9. doi: 10.1164/rccm.201807-1203OC. [Epub ahead of print] [Pubmed]
Cystic fibrosis (CF) lung disease starts in early infancy suggesting that preventive treatment may be most beneficial. Lung clearance index (LCI) and chest magnetic resonance imaging (MRI) have emerged as promising endpoints of early CF lung disease, however, randomized controlled trials testing the safety and efficacy of preventive therapies in infants with CF are lacking. This study was to determine feasibility, safety and efficacy of preventive inhalation with hypertonic saline (HS) compared to isotonic saline (IS) in infants with CF including LCI and MRI as outcome measures.
In this randomized, double-blind, controlled trial 42 infants with CF less than 4 months of age were randomized across 5 sites to twice daily inhalation of 6% HS (n=21) or 0.9% IS (n=21) for 52 weeks. Inhalation of HS and IS was generally well tolerated by CF infants and the number of adverse events did not differ between groups (P=0.49). The change in LCI from baseline to week 52 was larger in CF infants treated with HS (-0.6) compared to IS (-0.1, P<0.05). In addition, weight gain was improved in CF infants treated with HS (P<0.05), whereas pulmonary exacerbations and chest MRI scores did not differ in the HS vs. IS group.
The authors concluded preventive inhalation with HS initiated in the first months of life was safe and well tolerated, and resulted in improvements in LCI and weight gain in infants with CF. Their results support feasibility of LCI as endpoint in randomized controlled trials in infants with CF..
Dr M Stahl from the Division of Pediatric Pulmonology & Allergy and Cystic Fibrosis Centre, Department of Pediatrics and Department of Translational Pulmonology, Translational Lung Research Centre Heidelberg (TLRC). (image above).
2019 Fretzayas A, Douros K, Moustaki M, Loukou I. Applications of lung clearance index in monitoring children with cystic fibrosis. World J Clin Pediatr. 2019 Apr 9;8(2):15-22. doi: 10.5409/wjcp.v8.i2.15. eCollection 2019 Apr 9. [Pubmed]

Andreas Fretzayas
A sensitive, reproducible and feasible measure of lung function for monitoring the respiratory health is a prerequisite for the optimization of management of the patients with cystic fibrosis (CF). Spirometry has been considered the method of choice, although it is applicable only in children older than 6 years of age, as good cooperation is necessary for its proper performance. However, over the last 15 years, scientific interest in gas dilution techniques and particularly in multiple breath wash out (MBW) method has been revived. The most commonly reported index of MBW is lung clearance index (LCI). The aim of this review is to present the most recent developments in the application of LCI as a monitoring index of respiratory status of CF patients. LCI is a sensitive and reproducible marker of ventilation inhomogeneity. It is more sensitive than spirometry and, unlike spirometry; it can be performed across the whole pediatric age range. Since it is dependent on body size, until at least the age of 6 years, the relative and not the absolute changes are more appropriate for providing clinically meaningful conclusion on ventilation inhomogeneity. Until now, MBW has been mainly used as a research tool. Based on the currently available data LCI cannot safely predict high-resolution computed tomography findings in children with CF, especially in infants. It can be used as an end-point measure for the assessment of beneficial effect of interventions. However, its utility as an outcome measure for the efficacy of therapeutic interventions seems to be dependent on the pathophysiologic mechanisms that underlie each intervention. It seems that more studies, especially longitudinal ones, are required in order to fully clarify the clinical usefulness of LCI, not only in the research setting, but also in every day practice of CF clinic.
Dr Andreas Fretzayas is Professor of Paediatrics, School of Medicine,Athens, Greece
2019 Lombardi E, Gambazza S, Pradal U, Braggion C. Lung clearance index in subjects with cystic fibrosis in Italy. Ital J Pediatr. 2019 May 2;45(1):56. doi: 10.1186/s13052-019-0647-5. [Pubmed]
The Lung Clearance Index (LCI) is an index derived from washout recordings, able to detect early peripheral airway damage in subjects with cystic fibrosis (CF) with a greater sensitivity than spirometry.LCI is a marker of overall lung ventilation inhomogeneity; in fact, as pulmonary ventilation worsens, the number of tidal breaths and the expiratory volumes required to clear the lungs of a marker gas are increased, as documented by a greater value.In the field of CF, LCI allows indirect investigation of the small airways (< 2 mm) the site where, from a pathophysiologic point of view, the disease begins due to the defect of the CF transmembrane-conductance regulator (CFTR) protein. Infant pulmonary function changes seem to occur before clinically overt symptoms of lower respiratory illness occur.When performing the test, it is important to refer to the American Thoracic Society and European Respiratory Society consensus statements and apply a strict standardization.In Italy the first tests were carried out in 2014 for research purpose and now approximately 10 centers are collecting data and are experiencing a consistency in repeating exams.Currently in Italian centers children at pre-school age are the main target: in this population it is important to have a sensitive and feasible test, non-invasive, that can be performed at tidal volume without sedation, and requiring minimal cooperation and coordination, and that can be used longitudinally over time. Another target could be the transplanted subjects to detect early signs of lung function decline.The content of this paper captures the experience and discussions among some of the Italian centers where LCI is currently used for research and/or in clinical practice about the method and the need to have a common approach.The aim of this paper is not to describe the methodology of MBW, but to inform the pediatric community about the possible application of LCI in CF.
Dr Enrico Lombardi is Head of Paediatric Pulmonology, Paediatric University Hospital, Florence, Italy.
2016 Shawcross A, Murray CS, Goddard N, Gupta R, Watson S, Horsley. Accurate lung volume measurements in vitro using a novel inert gas washout method suitable for infants. Pediatr Pulmonol. 2016 May;51(5):491-7. doi: 10.1002/ppul.23348. Epub 2015 Dec 1 [Pubmed]
Multiple breath washout (MBW) in infants presents a number of technical challenges. Conventional MBW is based on simultaneous measurement of flow and gas concentrations. These two signals are aligned and combined to derive expired gas volumes from which lung volumes and measures of ventilation inhomogeneity are calculated. Accuracy of measurement becomes increasingly vulnerable to errors in gas signal alignment at fast respiratory rates. In this paper we describe an alternative method of performing MBW in infants. Expired gas is collected and analyzed to derive functional residual capacity (FRC) and lung clearance index (LCI). This eliminates the need for simultaneous measurement of flow, and integration of flow and gas signals, and significantly reduces deadspacee. A highly accurate lung model incorporating BTPS conditions was used to generate realistic infant breathing parameters: FRC of 100-250 mls with respiratory rate of 20-60 min(-1) . In vitro accuracy of FRC measurement using the novel MBW method was assessed using the model.
Overall mean error (standard deviation) of FRC measurement was -1.0 (3.3)% with 90% of tests falling within ±5%. FRC measurement using the novel method has superior accuracy in vitro than previously described systems. By uncoupling the measurement of gas volumes from real-time flow and gas measurement, this system offers an alternative method of MBW which is well suited to infants.
2019 Shawcross A, Murray CS, Pike K, Horsley A. A novel method for infant multiple breath washout: First report in clinical practice. Pediatr Pulmonol. 2019 Jun 18. doi: 10.1002/ppul.24384. [Epub ahead of print] [Pubmed]
Lung clearance index (LCI), measured using multiple breath inert gas washout (MBW) is a potentially useful test in infants with respiratory disease, particularly cystic fibrosis (CF). Clinical use is limited however by the need for specialist staff and equipment. We have previously described a novel method for infant MBW suitable for use outside of specialist laboratories. This study describes its performance in vivo in infants with CF and healthy controls, including a limited comparison with the respiratory mass spectrometer.
Children aged less than 2 years with CF and controls underwent MBW testing on a single occasion. The practical applicability of the system was determined by the number of successful duplicate tests and within-subject repeatability.
Twenty-five children (seven with CF, 18 healthy controls, all sedated with chloral hydrate) attempted MBW. Twenty patients (seven with CF) successfully underwent duplicate testing (80% success rate). Mean within-subject coefficient of variation for functional residual capacity (FRC) was 7.2% and for LCI 5.9%. Comparison of LCI with the mass spectrometer was limited but gave very similar values for LCI and FRC in those patients who underwent technically adequate tests with both methods.
We have described a new MBW method that is feasible and reproducible in sedated infants. Results fall within the expected range, and well within accuracy limits set by international guidelines. This could provide a more accessible alternative to previously described systems for infant MBW, and overcomes many of the technical challenges inherent in conventional MBW
Dr Anna Shawcross is Clinical Research Fellow and Specialist Tainee in Paedaitric Respiratory Medicine, Manchester
Department of Paediatric Respiratory Medicine, Royal Manchester Children’s Hospital, Manchester, UK.
Logie K, Welsh L, Ranganathan SC. Telehealth spirometry for children with cystic fibrosis. Arch Dis Child. 2019 Nov 6. pii: archdischild-2019-317147. doi: 10.1136/archdischild-2019-317147. [Epub ahead of print]. [Pubmed]

SpiroUSB (Vyaire) spirometer in foreground.
The authors assessed the feasibility of Telehealth spirometry assessments for children with cystic fibrosis (CF) living in a regional setting. Patients with acceptable computer hardware at home were provided with a SpiroUSB (Vyaire) spirometer. Spirometry was performed during ‘home admissions’ or for ongoing home monitoring in children living outside metropolitan Melbourne. At the end of the session, the family forwarded the data to the Royal Children’s Hospital, Melbourne.
Twenty-two patients aged 7 to 17 years participated, with spirometry successful in 55 of 59 (93%) attempted sessions according to American Thoracic Society/European Respiratory Society criteria. The median distance between the subject’s home and the hospital was 238 km (range 62-537 km) which equated to a travel time saving of 5 hours and 34 min per hospital visit.
The authors concluded Home-based Telehealth spirometry is feasible in children with CF and can support the CF team during home-based admissions and for ongoing outpatient monitoring.
Dr Karla Logie, Respiratory Scientist and Research Assistant in the Dept. of Respiratory Medicine, Royal Childrens Hospital Melbourne, Parkville, Victoria, Australia.
Poncin W, Lebecque P.[Lung clearance index in cystic fibrosis]. Rev Mal Respir. 2019 Jan 24. pii: S0761-8425(18)31015-5. doi: 10.1016/j.rmr.2018.03.007. [Epub ahead of print] (French) [Pubmed]
-

William Poncin
- The multiple breath washout (MBW) test is affordable and non-invasive. Lung clearance index (LCI), which is the most used derived parameter, is reproducible and much more sensitive than spirometry in detecting small airways disease. However, MBW is operator dependent. The recent commercialization of devices assessing LCI launches MBW as a potential tool in routine clinical care, although its use currently remains mostly dedicated to research purposes. However, important differences in LCI between various equipment settings raise a number of theoretical questions. Specific algorithms should be refined and more transparent. Standardization of MBW is still an on going process. Whether other MBW derived indices can prove superior over LCI deserves further study.
The authors conclude that in CF, LCI is now a well-established outcome in research settings to detect early lung function abnormalities and new treatment effects, especially in patients with mild lung disease. In these patients, LCI seems an attractive tool for clinicians too. Yet, further investigation is needed to define clinically significant changes in LCI and to which extent this index can be useful in guiding clinical decisions remains to be studied.
Dr William Poncin is an expert on respiratory physiology at Universite Catholique de Louvain.
Papale M, Parisi GF, Spicuzza L, Licari A, Bongiovanni A, Mulè E, Rotolo N, Manti S, Leonardi S. Lung clearance index evaluation in detecting nocturnal hypoxemia in cystic fibrosis patients: Toward a new diagnostic tool. Respir Med. 2020 Apr;164:105906. doi: 10.1016/j.rmed.2020.105906. Epub 2020 Feb 19. [Pubmed]
Nocturnal hypoxemia adversely affects outcomes in patients with cystic fibrosis (CF). Although an early detection of this abnormality may be desirable, still its predictability remains uncertain. The Lung Clearance Index (LCI) is a measure of lung ventilation distribution obtained from a multiple-breath washout technique (MBW), recently implemented in patients with CF. This study aimed to establish whether the LCI predicts nocturnal hypoxemia in patients with stable CF, with mild to moderate disease, and normal diurnal gas exchange.
31 stable patients (15 males, mean age 17.4 ± 5.2 years) with mild to moderate CF, normoxic when awake, were enrolled. In all patients we performed nocturnal cardio-respiratory polygraphy, lung function measurement, and MBW test to derive LCI values.
LCI was abnormal in most of the patients and inversely correlated with mean nocturnal SpO2 (r = -0.880 p < 0.01). A receiver operating characteristic (ROC) analysis, performed to assess whether LCI predicted nocturnal hypoxemia, revealed a high predictive accuracy of LCI for nocturnal desaturation (AUC = 0.96; Youden index = 0.79). Forced expiratory volume in 1 s (FEV1) was predictive only in patients with more severe airway obstruction, with a moderate degree of accuracy (AUC 0.71).
The authors concluded the LCI showed a high effectiveness in predicting nocturnal hypoxemia in stable patients with CF, particularly when compared with a traditional parameter of lung function such as FEV1.
From the Respiratory Unit, AOU Policlinico-Vittorio Emanuele, Department of Clinical and Experimental Medicine, University of Catania, Via Santa Sofia 78, I-95123, Catania, Italy.
L Caley, L Smith, H White, D G Peckham. Average Rate of Lung Function Decline in Adults With Cystic Fibrosis in the United Kingdom: Data From the UK CF Registry. J Cyst Fibros 2020 May 4;S1569-1993(20)30121-1. doi: 10.1016/j.jcf.2020.04.008.Online ahead of print.[Pubmed]
Rate of change in lung function is used as a measure of disease progression and a predictor of mortality in individuals with cystic fibrosis (CF). The aim of this study was to determine the national rate of decline in percent predicted Forced Expiratory Volume in 1 second (ppFEV1) in adults in the UK accounting for age, sex and pancreatic status.
Data on ppFEV1 for adults with CF, excluding those post lung transplantation, was extracted from the UK CF registry between 2015 and 2017. Multilevel modelling was conducted to calculate the annual rate of change in ppFEV1 accounting for age, sex and pancreatic status. The overall annual ppFEV1 decline was -1.52% (95% CI: -1.66 to -1.38%) and -0.55% (95% CI: -0.86 to -0.23%) in pancreatic insufficient (PI) and sufficient (PS) adults respectively. In PI individuals, females had a greater rate of decline in ppFEV1. There were differences between age groups. The fastest rate of decline was observed in the 18-28 years group, declining -1.76% (95% CI: -2.06 to -1.46) and -1.61% (95% CI: -1.91 to -1.31) per year in PI females and males respectively. The pattern between the sexes and age categories was more inconsistent in the PS group.
The average annual rates of decline in lung function in adults with CF in the UK are similar to reports from other large international cohorts. Pancreatic status has a marked impact on average rate of decline. Younger adults, especially females, have a faster rate of decline and need close monitoring.
Laura Caley is in the School of Medicine, Clinical Sciences Building, St James’s University Hospital, Leeds, LS9.
Clare Saunders , Renee Jensen, Paul D Robinson, Sanja Stanojevic, Michelle Klingel, Christopher Short, Jane C Davies, Felix Ratjen. Integrating the multiple breath washout test into international multicentre trials. J Cyst Fibros 2020 Jul;19(4):602-607.doi: 10.1016/j.jcf.2019.11.006. Epub 2019 Nov 24. [Pubmed]
The lung clearance index (LCI), derived from the Multiple Breath Washout (MBW) test, is sensitive to treatment effects and compared with spirometry has higher feasibility in younger children and requires smaller sample sizes. As a result, the LCI has been endorsed by the European CF Society Clinical Trials Network for use as a primary outcome measure in CF clinical trials.
Here the authors describe the implementation of standardised protocols for MBW test performance, data collection and quality control to successfully incorporate LCI as a novel outcome measure in a large multicentre phase III clinical trial.
Dr Clare Saunders is at the Royal Brompton & Harefield NHS Foundation Trust, London, United Kingdom; National Heart and Lung Institute, Imperial College London.
L Caley, L Smith, H White, D G Peckham. Average Rate of Lung Function Decline in Adults With Cystic Fibrosis in the United Kingdom: Data From the UK CF Registry. J Cyst Fibros 2020 May 4;S1569-1993(20)30121-1. doi: 10.1016/j.jcf.2020.04.008.Online ahead of print.[Pubmed]
Rate of change in lung function is used as a measure of disease progression and a predictor of mortality in individuals with cystic fibrosis (CF). The aim of this study was to determine the national rate of decline in percent predicted Forced Expiratory Volume in 1 second (ppFEV1) in adults in the UK accounting for age, sex and pancreatic status.
Data on ppFEV1 for adults with CF, excluding those post lung transplantation, was extracted from the UK CF registry between 2015 and 2017. Multilevel modelling was conducted to calculate the annual rate of change in ppFEV1 accounting for age, sex and pancreatic status. The overall annual ppFEV1 decline was -1.52% (95% CI: -1.66 to -1.38%) and -0.55% (95% CI: -0.86 to -0.23%) in pancreatic insufficient (PI) and sufficient (PS) adults respectively. In PI individuals, females had a greater rate of decline in ppFEV1. There were differences between age groups. The fastest rate of decline was observed in the 18-28 years group, declining -1.76% (95% CI: -2.06 to -1.46) and -1.61% (95% CI: -1.91 to -1.31) per year in PI females and males respectively. The pattern between the sexes and age categories was more inconsistent in the PS group.
The average annual rates of decline in lung function in adults with CF in the UK are similar to reports from other large international cohorts. Pancreatic status has a marked impact on average rate of decline. Younger adults, especially females, have a faster rate of decline and need close monitoring.
Laura Caley is in the School of Medicine, Clinical Sciences Building, St James’s University Hospital, Leeds, LS9.
From the University of Edinburgh, Centre for Genomic and Experimental Medicine, University of Edinburgh and Institute of Genetics & Molecular Medicine, Western General Hospital, Edinburgh UK; UK Cystic Fibrosis Gene Therapy Consortium, UK
Calthorpe RJ, Smith S, Gathercole K, Smyth AR. Using digital technology for home monitoring, adherence and self-management in cystic fibrosis: a state-of-the-art review.
Thorax. 2020 Jan;75(1):72-77. doi: 10.1136/thoraxjnl-2019-213233. Epub 2019 Oct 8.[Pubmed]

Rebecca Calthorpe
Digital healthcare is a rapidly growing healthcare sector. Its importance has been recognised at both national and international level, with the WHO recently publishing its first global strategy for digital health. The use of digital technology within cystic fibrosis (CF) has also increased. CF is a chronic, life-limiting condition, in which the treatment burden is high and treatment regimens are not static. Digital technologies present an opportunity to support the lives of people with CF. We included 59 articles and protocols in this state-of-the-art review, relating to 48 studies from 1999 until 2019. This provides a comprehensive overview of the expansion and evolution of the use of digital technology. Technology has been used with the aim of increasing accessibility to healthcare, earlier detection of pulmonary exacerbations and objective electronic adherence monitoring. It may also be used to promote adherence and self-management through education, treatment management Apps and social media
Davies G, Thia LP, Stocks J, Bush A, Hoo AF, Wade A, Nguyen TTD, Brody AS, Calder A, Klein NJ, Carr SB, Wallis C, Suri R, Pao CS, Ruiz G, Balfour-Lynn IM; London Cystic Fibrosis Collaboration (LCFC). Minimal change in structural, functional and inflammatory markers of lung disease in newborn screened infants with cystic fibrosis at one year. J Cyst FIBROS 2020 Feb 7. pii: S1569-1993(20)30031-X.doi: 10.1016/j.jcf.2020.01.006. [Epub ahead of print] [Pubmed[]
With the widespread introduction of newborn screening for cystic fibrosis(CF), there has been considerable emphasis on the need to develop objective markers of lung health that can be used during infancy. We hypothesised that in a newborn screened (NBS) UK cohort, evidence of airway inflammation and infection at one year would be associated with adverse structural and functional outcomes at the same age.
Infants underwent lung function testing, chest CT scan and bronchoscopy with bronchoalveolar lavage (BAL) at 1 year of age when clinically well. Microbiology cultures were also available from routine cough swabs.
65 infants had lung function, CT and BAL. Mean (SD) lung clearance index and forced expiratory volume in 0.5 s z-scores were 0.9(1.2) and -0.6(1.1) respectively; median Brody II CF-CT air trapping score on chest CT =0 (interquartile range 0-1, maximum possible score 27). Infants isolating any significant pathogen by 1 yr of age had higher LCI z-score (mean difference 0.9; 95%CI:0.4-1.4; p = 0.001) and a trend towards higher air trapping scores on CT (p = 0.06). BAL neutrophil elastase was detectable in 23% (10/43) infants in whom BAL supernatant was available. This did not relate to air trapping score on CT.
The authors concluded that in this UK NBS cohort at one year of age, lung and airway damage is much milder and associations between inflammation, abnormal physiology and structural changes were at best weak, contrary to our hypothesis and previously published reports. Continued follow-up will clarify longer term implications of these very mild structural, functional and inflammatory changes.
Dr Gwyneth Davies is a Research Associate Respiratory, Critical Care and Anaesthesia section, UCL Great Ormond Street Institute of Child Health (GOS ICH), London,
-This is a comprehensive review of the use of technology in various aspects of CF care. The fully referenced Thorax draft of the paper is available on the internet (R J Calthorpe) and is an excellent source of information for anyone looking in depth into this area.
Dr Rebecca J Calthorpe Division of Child Health, Obstetrics and Gynaecology, University of Nottingham,
FitzMaurice TS, McNamara PS, Nazareth D, McCann C, Bedi R, Shaw M, Walshaw M. Utility and validity of dynamic chest radiography in cystic fibrosis(dynamic CF): an observational, non-controlled, non-randomised, single-centre, prospective study. BMJ Open Respir Res. 2020 Mar;7(1). pii: e000569. doi: 10.1136/bmjresp-2020-000569. Free full text[Pubmed]
Dynamic chest radiography (DCR) uses novel, low-dose radiographic technology to capture images of the thoracic cavity while in motion. Pulmonary function testing is important in cystic fibrosis (CF). The tolerability, rapid acquisition and lower radiation and cost compared with CT imaging may make DCR a useful adjunct to current standards of care.
This is an observational, non-controlled, non-randomised, single-centre, prospective study. This study is conducted at the Liverpool Heart and Chest Hospital (LHCH) adult CF unit. Participants are adults with CF. This study reviews DCR taken during routine CF Annual Review (n=150), validates DCR-derived lung volumes against whole body plethysmography (n=20) and examines DCR at the start and end of pulmonary exacerbations of CF (n=20). The primary objectives of this study are to examine if DCR provides lung function information that correlates with PFT, and lung volumes that correlate whole body plethysmography.
Dr Thomas FitzMaurice is a Clinical Fellow at the Adult CF Unit, Liverpool Heart and Chest Hospital NHS Trust, and the Institute of Translational Medicine, University of Liverpool, Liverpool, UK
Clare Saunders , Renee Jensen, Paul D Robinson, Sanja Stanojevic, Michelle Klingel, Christopher Short, Jane C Davies, Felix Ratjen. Integrating the multiple breath washout test into international multicentre trials. J Cyst Fibros 2020 Jul;19(4):602-607.doi: 10.1016/j.jcf.2019.11.006. Epub 2019 Nov 24. [Pubmed]
The lung clearance index (LCI), derived from the Multiple Breath Washout (MBW) test, is sensitive to treatment effects and compared with spirometry has higher feasibility in younger children and requires smaller sample sizes. As a result, the LCI has been endorsed by the European CF Society Clinical Trials Network for use as a primary outcome measure in CF clinical trials.
Here the authors describe the implementation of standardised protocols for MBW test performance, data collection and quality control to successfully incorporate LCI as a novel outcome measure in a large multicentre phase III clinical trial.
Dr Clare Saunders is at the Royal Brompton & Harefield NHS Foundation Trust, London, United Kingdom; National Heart and Lung Institute, Imperial College London
L Caley, L Smith, H White, D G Peckham. Average Rate of Lung Function Decline in Adults With Cystic Fibrosis in the United Kingdom: Data From the UK CF Registry. J Cyst Fibros 2020 May 4;S1569-1993(20)30121-1. doi: 10.1016/j.jcf.2020.04.008.Online ahead of print.[Pubmed]
Rate of change in lung function is used as a measure of disease progression and a predictor of mortality in individuals with cystic fibrosis (CF). The aim of this study was to determine the national rate of decline in percent predicted Forced Expiratory Volume in 1 second (ppFEV1) in adults in the UK accounting for age, sex and pancreatic status.
Data on ppFEV1 for adults with CF, excluding those post lung transplantation, was extracted from the UK CF registry between 2015 and 2017. Multilevel modelling was conducted to calculate the annual rate of change in ppFEV1 accounting for age, sex and pancreatic status. The overall annual ppFEV1 decline was -1.52% (95% CI: -1.66 to -1.38%) and -0.55% (95% CI: -0.86 to -0.23%) in pancreatic insufficient (PI) and sufficient (PS) adults respectively. In PI individuals, females had a greater rate of decline in ppFEV1. There were differences between age groups. The fastest rate of decline was observed in the 18-28 years group, declining -1.76% (95% CI: -2.06 to -1.46) and -1.61% (95% CI: -1.91 to -1.31) per year in PI females and males respectively. The pattern between the sexes and age categories was more inconsistent in the PS group.
The average annual rates of decline in lung function in adults with CF in the UK are similar to reports from other large international cohorts. Pancreatic status has a marked impact on average rate of decline. Younger adults, especially females, have a faster rate of decline and need close monitoring.
Laura Caley is in the School of Medicine, Clinical Sciences Building, St James’s University Hospital, Leeds, LS9.
Christian Voldby, Kent Green, Thomas Kongstad, Astrid Madsen Ring, Rikke Mulvad Sandvik, Marianne Skov, Frederik Buchvald, Tacjana Pressler, Kim Gjerum Nielsen. Lung clearance index-triggered intervention in children with cystic fibrosis – A randomised pilot study. J Cyst Fibros 2020 Jun 20;S1569-1993(20)30755-4. doi: 10.1016/j.jcf.2020.06.010.Online ahead of print. [Pubmed]
Kim Gjerum Nielsen
Using increase in the lung clearance index (LCI) as a trigger for bronchoalveolar lavage (BAL) and associated antimicrobial treatment might benefit clinical outcomes in children with cystic fibrosis (CF).
Methods: A 2-year, longitudinal, interventional, randomized, controlled pilot study with quarterly visits in 5-18 years old children with CF. LCI and z-scores for the forced expired volume in 1 s (zFEV1) and body mass index (zBMI) were obtained at every visit, CF Questionnaire-revised (CFQ-R) yearly and BAL and chest computed tomography at first and last visit. Children in the intervention group had BAL performed if LCI increased >1 unit from a fixed baseline value established at first visit. If the presence of a pathogen was documented in the BAL fluid, treatment was initiated/altered accordingly.
Results: Twenty-nine children with CF were randomized to the control (n = 14) and intervention group (n = 15). The median (interquartile range) number of BAL procedures per child was 2.5 (2.0; 3.0) and 6.0 (4.0; 7.0) in the control and intervention group, respectively. There was no significant difference between groups in slope for the primary outcome LCI; difference was 0.21 (95% confidence interval: -0.45; 0.88) units/year. Likewise, there was no significant difference between groups in slope for the secondary outcomes zFEV1, zBMI, CFQ-R respiratory symptom score and the proportion of total disease and trapped air on chest computed tomography.
Conclusions: LCI-triggered BAL and associated antimicrobial treatment did not benefit clinical outcomes in a small cohort of closely monitored school-age children with CF.
Dr Christian Voldby is at the CF Centre Copenhagen, Paediatric Pulmonary Service, Department of Paediatrics and Adolescent Medicine, Copenhagen University Hospital, Rigshospitalet, Copenhagen, Denmark.
Professor Kim G Nielsen at the CF Centre Copenhagen, Paediatric Pulmonary Service, Department of Paediatrics and Adolescent Medicine, Copenhagen University Hospital, Rigshospitalet Copenhagen, Denmark
M Pollak , M Shaw , S Balkovec , D Wilson , K Kowalik , P Subbarao, F Ratjen Infant spirometry as a predictor of lung function at early childhood in cystic fibrosis patients. J Cyst Fibros. 2020 Sep 17;2116. doi: 10.1016/j.jcf.2020.09.005. Online ahead of print. [Pubmed]
Infant pulmonary function testing using the raised volume rapid thoracoabdominal compression (RVRTC) technique requires sedation and is time consuming. Many cystic fibrosis (CF) centers do not have access to equipment and the utility of routine testing remains to be determined. The authors aimed to assess whether RVRTC tests performed during infancy predict spirometry at early school age.
The RVRTC-based forced expiratory flow measures in infants were compared to the first adequately performed spirometry at school age. All tests were carried out during routine clinic visits and expressed as age related z-scores; only test occasions where patients were considered stable were included in the analysis
The infant RVRTC measures were not predictive of pulmonary function in early school age, likely due to the high proportion of measures of forced expiratory flows within the normal range at both time points.
Dr M Pollak is in the Division of Respiratory Medicine Hospital for Sick Children, Toronto, ON, Canada.
Lucy Perrem , Sanja Stanojevic , Michelle Shaw , Renee Jensen , Nancy McDonald , Sarah M Isaac , Miriam Davis , Charles Clem , Julia Guido, Sylvia Jara, Lisa France, Melinda Solomon , Hartmut Grasemann , Valerie Waters, Neil Sweezey, Don B Sanders, Stephanie Davis, Felix Ratjen. Lung Clearance Index to Track Acute Respiratory Events in School-age Children with Cystic Fibrosis. Am J Respir Crit Care Med 2020 Oct 8. doi: 10.1164/rccm.202006-2433OC.Online ahead of print.[Pubmed]
Objective: The lung clearance index (LCI) is responsive to acute respiratory events in preschool children with cystic fibrosis (CF) but its’ utility to identify and manage these events in school-age children with CF is not well defined.
Methods: In a multisite prospective observational study, LCI and forced expiratory volume in 1 second (FEV1) were measured quarterly and during acute respiratory events. Linear regression was used to compare relative changes in LCI and FEV1 % predicted at acute respiratory events. Logistic regression was used to compare the odds of a significant worsening in LCI and FEV1 % predicted at acute respiratory events. Generalized estimating equation models were used to account for repeated events in the same subject.
Results: A total of 98 children with CF were followed for two years. There were 265 acute respiratory events. Relative to a stable baseline measure, LCI (+8.9%; 95% CI 6.5 to 11.3) and FEV1% predicted (-6.6%; 95% CI -8.3 to -5.0) worsened with acute respiratory events. A greater proportion of events had a worsening in LCI compared to a decline in FEV1% predicted (41.7% vs 30.0%; p=0.012); 53.9% events were associated with worsening in LCI or FEV1. Neither LCI nor FEV1 recovered to baseline values at the next follow-up visit.
Conclusions: In school-age children with CF, LCI is a sensitive measure to assess lung function worsening with acute respiratory events and incomplete recovery at follow-up. LCI and FEV1 in combination capture a higher proportion of events with functional impairment.
Dr Lucy Perrem is at The Hospital for Sick Children, Toronto, Ontario, Canada
Rikke Mulvad Sandvik, Thomas Kongstad, Kent Green, Christian Voldby, Frederik Buchvald, Marianne Skov Tacjana Pressler, Kim Gjerum Nielsen Prospective longitudinal association between repeated multiple breath washout measurements and computed tomography scores in children with cystic fibrosis. J Cyst Fibros. 2020 Oct 4;2121 doi: 10.1016/j.jcf.2020.09.010. Online ahead of print. [Pubmed]

Rikke Mulvad Sandvik
Background: Progression of structural lung disease (SLD) is a major risk factor for morbidity in patients with cystic fibrosis (CF). We studied changes in SLD and correlations with spirometry and nitrogen multiple breath washout (N2MBW) outcomes to explore associations in contemporary evolution between structural and functional abnormalities in CF lung disease.
Methods: Spirometry-controlled chest-CTs using PRAGMA-CF for scoring extent of SLD, spirometry, and N2MBW were performed at two-year intervals in school-age children with CF
Results: Fifty-seven children aged 6-18 years were included. No significant progression in mean PRAGMA-CF scores was observed. Half of the children showed improvement in the proportion of bronchiectasis (%Bx). Lung Clearance Index (LCI) and the second moment ratio (M2) increased significantly and baseline values correlated significantly with SLD at follow-up (p ≤ 0.0002). The correlation between the change in M2 (∆M2) and the change in total SLD was R = 0.27 (p = 0.048). We found high negative predictive values (100%) for ∆M2<10% to exclude progression in SLD. For stable or improving values of LCI and M2, the predicted probability for progression in SLD was 16% and 14%, respectively (upper 95% confidence limit: 33%). Evolution in N2MBW and CT outcomes was discordant in half of the children.
Conclusions: We found no progression in structural lung disease (SL) over 2 years in school-age children with CF, in contrast to both LCI and M2, which along with discordant outcomes in half of the children underlines that N2MBW and CT assess different aspects of CF lung disease. However, stable outcomes from N2MBW were associated with stable structural lung disease.
Rikke Mulvad Sandvik is a PHD student at the Danish PCD & CHILD Centre, CF Centre Copenhagen, Paediatric Pulmonary Service, ERN Accredited, Department of Paediatrics and Adolescent Medicine, Copenhagen University Hospital, Rigshospitalet, Denmar
Matthew M Willmering, David J Roach, Elizabeth L Kramer, Laura L Walkup, Zackary I Cleveland , Jason C Woods. Sensitive structural and functional measurements and 1-year pulmonary outcomes in pediatric cystic fibrosis. J Cyst Fibros 2020 Dec 4;S1569-1993(20)30929-2. doi: 10.1016/j.jcf.2020.11.019.Online ahead of print. [Pubmed]

Matthew Willmering
Background: Two functional measurements (multiple breath washout [MBW] and hyperpolarized 129Xe ventilation magnetic resonance imaging [129Xe MRI]) have been shown to be more sensitive to cystic fibrosis (CF) lung obstruction than traditional spirometry. However, functional techniques may be sensitive to different underlying structural abnormalities. The purpose of this study was to determine relationships between these functional markers, their pathophysiology, and 1-year clinical outcomes.
Methods: Spirometry, MBW, 129Xe MRI, and ultrashort echo-time (UTE) MRI were obtained in a same-day assessment of 27 pediatric CF patients (ages 11.5±5.0) who had not begun CFTR modulator therapies. UTE MRI was scored for structural abnormalities and functional metrics obtained via spirometry, MBW and 129Xe MRI. 1-year outcomes (ΔFEV1 and pulmonary exacerbations), during which ≈50% initiated modulator therapy, were obtained from the electronic medical record.
Results: MBW, 129Xe MRI, and UTE MRI detected clinically significant disease in more subjects (>78%) compared to spirometry (<30%). UTE MRI suggests increased odds of bronchial changes when mucus plugging is present in the same lobe. MBW and 129Xe MRI correlated best with mucus plugging, while spirometry correlated best with consolidations. Bronchial abnormalities were associated with future pulmonary exacerbations.
Conclusions: MBW, 129Xe MRI, and UTE MRI are more sensitive for detection of pediatric CF lung disease when compared to spirometry. MBW and 129Xe MRI correlated with structural abnormalities which occur in early CF disease, suggesting MBW and 129Xe MRI are valuable tools in mild CF lung disease that can guide clinical decision making.
Matthew M Willmering is at the Center for Pulmonary Imaging Research, Cincinnati Children’s Hospital Medical Center, Cincinnati, OH 45229, United States; Division of Pulmonary Medicine, Cincinnati Children’s Hospital Medical Center, Cincinnati, OH 45229, United States
Mirjam Stahl , Cornelia Joachim, Ines Kirsch , Tatjana Uselmann , Yin Yu , Nadine Alfeis , Christiane Berger , Rebecca Minso, Isa Rudolf, Cornelia Stolpe, Xenia Bovermann, Lena Liboschik, Alena Steinmetz , Dunja Tennhardt, Friederike Dörfler , Jobst Röhmel, Klaudia Unorji-Frank, Claudia Rückes-Nilges , Bianca von Stoutz, Lutz Naehrlich, Matthias V Kopp, Anna-Maria Dittrich, Olaf Sommerburg, Marcus A Mall. Multicentre feasibility of multiple-breath washout in preschool children with cystic fibrosis and other lung diseases. ERJ Open Res 2020 Oct 26;6(4):00408-2020. doi: 10.1183/23120541.00408-2020.eCollection 2020 Oct. Free PMC article [Pubmed]

Mirjam Stahl
Background: Multiple-breath washout (MBW)-derived lung clearance index (LCI) detects early cystic fibrosis (CF) lung disease. LCI was used as an end-point in single- and multicentre settings at highly experienced MBW centres in preschool children. However, multicentre feasibility of MBW in children aged 2-6 years, including centres naïve to this technique, has not been determined systematically.
Methods: Following central training, 91 standardised nitrogen MBW investigations were performed in 74 awake preschool children (15 controls, 46 with CF, and 13 with other lung diseases), mean age 4.6±0.9 years at investigation, using a commercially available device across five centres in Germany (three experienced, two naïve to the performance in awake preschool children) with central data analysis. Each MBW investigation consisted of several measurements.
Results: Overall success rate of MBW investigations was 82.4% ranging from 70.6% to 94.1% across study sites. The number of measurements per investigation was significantly different between sites ranging from 3.7 to 6.2 (p<0.01), while the mean number of successful measurements per investigation was comparable with 2.1 (range, 1.9 to 2.5; p=0.46). In children with CF, the LCI was increased (median 8.2, range, 6.7-15.5) compared to controls (median 7.3, range 6.5-8.3; p<0.01), and comparable to children with other lung diseases (median 7.9, range, 6.6-13.9; p=0.95).
Conclusion: This study demonstrates that multicentre MBW in awake preschool children is feasible, even in centres previously naïve, with central coordination to assure standardised training, quality control and supervision. Our results support the use of LCI as multicentre end-point in clinical trials in awake preschoolers with CF
Dr Mirjam Stahl is in the Dept of Pediatric Pulmonology, Immunology and Critical Care Medicine, Charité – Universitätsmedizin Berlin, Berlin, Germany; Division of Pediatric Pulmonology and Allergy and Cystic Fibrosis Center, Dept of Pediatrics, University of Heidelberg, Heidelberg, Germany; Dept of Translational Pulmonology, Translational Lung Research Center Heidelberg (TLRC), German Center for Lung Research (DZL), University of Heidelberg, Heidelberg, Germany. DZL associated partner, Berlin, Germany.
Papale M, Parisi GF, Spicuzza L, Licari A, Bongiovanni A, Mulè E, Rotolo N, Manti S, Leonardi S. Lung clearance index evaluation in detecting nocturnal hypoxemia in cystic fibrosis patients: Toward a new diagnostic tool. Respir Med. 2020 Apr;164:105906. doi: 10.1016/j.rmed.2020.105906. Epub 2020 Feb 19. [Pubmed]
Nocturnal hypoxemia adversely affects outcomes in patients with cystic fibrosis (CF). Although an early detection of this abnormality may be desirable, still its predictability remains uncertain. The Lung Clearance Index (LCI) is a measure of lung ventilation distribution obtained from a multiple-breath washout technique (MBW), recently implemented in patients with CF. This study aimed to establish whether the LCI predicts nocturnal hypoxemia in patients with stable CF, with mild to moderate disease, and normal diurnal gas exchange.
31 stable patients (15 males, mean age 17.4 ± 5.2 years) with mild to moderate CF, normoxic when awake, were enrolled. In all patients we performed nocturnal cardio-respiratory polygraphy, lung function measurement, and MBW test to derive LCI values.
LCI was abnormal in most of the patients and inversely correlated with mean nocturnal SpO2 (r = -0.880 p < 0.01). A receiver operating characteristic (ROC) analysis, performed to assess whether LCI predicted nocturnal hypoxemia, revealed a high predictive accuracy of LCI for nocturnal desaturation (AUC = 0.96; Youden index = 0.79). Forced expiratory volume in 1 s (FEV1) was predictive only in patients with more severe airway obstruction, with a moderate degree of accuracy (AUC 0.71).
The authors concluded the LCI showed a high effectiveness in predicting nocturnal hypoxemia in stable patients with CF, particularly when compared with a traditional parameter of lung function such as FEV1.
Dr Maria Papale is at the Respiratory Unit, AOU Policlinico-Vittorio Emanuele, Department of Clinical and Experimental Medicine, University of Catania, Via Santa Sofia 78, I-95123, Catania, Italy.
Ajay S Kasi, Choo Phei Wee, Thomas G Keens, Danieli B Salinas. Abnormal Lung Clearance Index in Cystic Fibrosis Children with Normal FEV 1 and Single-Breath Nitrogen Washout Test. Lung 2021 Jan 3.doi: 10.1007/s00408-020-00412-8. Online ahead of print. [Pubmed]

Ajay S Kasi
Single- and multiple-breath washout tests (SBW and MBW) measure ventilation inhomogeneity, but the relationship between them is unclear.
Forty-three subjects with cystic fibrosis (CF) and healthy controls (HC) 8-21 years of age were recruited (CF = 30 and HC = 13) and performed nitrogen MBW, vital capacity SBW, spirometry, and plethysmography. Mean phase III slope from SBW (SIII) and lung clearance index (LCI) were significantly different between CF and HC (p = 0.017 and p < 0.0001, respectively). Based on Pearson correlation, SIII and LCI showed strong correlation (ρ = 0.81, p < 0.0001). Both SIII and LCI significantly correlated with spirometry (all p < 0.05). Among CF subjects with normal FEV1 (≥ 80%; n = 17), 76% (n = 13) had normal SIII but abnormal LCI.
We conclude that LCI can be abnormal despite normal SIII and FEV1 in CF children. Although LCI and SIII showed strong correlation, our results suggest that LCI is a better test to detect ventilation inhomogeneity in CF children with normal FEV1.
Dr Ajay S Kasi is in the Division of Pediatric Pulmonology, Department of Pediatrics, Children’s Hospital Los Angeles, Keck School of Medicine, University of Southern California, Los Angeles, CA, USA.
Beth L Laube, Kathryn A Carson, Christopher M Evans, Melis A Aksit , Joseph M Collaco, Vanessa L Richardson, Gail Sharpless, Pamela L Zeitlin, Garry R Cutting, Peter J Mogayzel. Characterizing mucociliary clearance in young children with cystic fibrosis. Pediatr Res 2021 Mar 22.doi: 10.1038/s41390-021-01453-2. Online ahead of print. [Pubmed]

Beth L Laube
Background: This research characterized mucociliary clearance (MCC) in young children with cystic fibrosis
Methods: Fourteen children (5-7 years old) with CF underwent: two baseline MCC measurements (Visits 1 and 2); one MCC measurement approximately 1 year later (Visit 3); and measurements of lungTwo shirts as well clearance index (LCI), a measure of ventilation inhomogeneity.
Results: Median (range) percent MCC through 60 min (MCC60) was similar on Visits 1 and 2 with 11.0 (0.9-33.7) and 12.8 (2.7-26.8), respectively (p = 0.95), and reproducible (Spearman Rho = 0.69; p = 0.007). Mucociliary clearance did not change significantly over 1 year with median percent MCC60 on Visit 3 [12.8 (3.7-17.6)] similar to Visit 2 (p = 0.58). Lower percent MCC60 on Visit 3 was significantly associated with higher LCI scores on Visit 3 (N = 14; Spearman Rho = -0.56; p = 0.04).
Conclusions: Tests of MCC were reproducible and reliable over a 2-week period and stable over a 1-year period in 5-7-year-old children with CF. Lower MCC values were associated with increased ventilation inhomogeneity. These results suggest that measurements of MCC could be used in short-term clinical trials of interventions designed to modulate MCC and as a new, non-invasive test to evaluate early lung pathology in children with CF.
Impact: This is the first study to characterize mucociliary clearance (MCC) in children with cystic fibrosis (CF) who were 5-7 years old. Measurements of mucociliary clearance were reproducible and reliable over a 2-week period and stable over a 1-year period. Variability in MCC between children was associated with differences in ventilation homogeneity, such that children with lower MCC values had increased ventilation inhomogeneity.
These results suggest that measurements of MCC could be used in short-term clinical trials of interventions designed to modulate MCC and as a new, non-invasive test to evaluate early lung pathology in children with CF
Dr Beth L Laube is a professor of pediatrics in the Department of Pediatrics, Johns Hopkins University School of Medicine, Baltimore, MD, USA. She is an aerosol scientist.
Alex R Horsley, John Belcher, Katie Bayfield, Brooke Bianco, Steve Cunningham, Catherine Fullwood, Andrew Jones, Anna Shawcross, Jaclyn A Smith, Anirban Maitra, Francis J Gilchrist. Longitudinal assessment of lung clearance index to monitor disease progression in children and adults with cystic fibrosis. Thorax 2021 Jul 22;thoraxjnl-2021-216928.doi: 10.1136/thoraxjnl-2021-216928.Online ahead of print. [Pubmed]

Alex Horsley
Background: Lung clearance index (LCI) is a valuable research tool in cystic fibrosis (CF) but clinical application has been limited by technical challenges and uncertainty about how to interpret longitudinal change. In order to help inform clinical practice, this study aimed to assess feasibility, repeatability and longitudinal LCI change in children and adults with CF with predominantly mild baseline disease.
Methods: Prospective, 3-year, multicentre, observational study of repeated LCI measurement at time of clinical review in patients with CF >5 years, delivered using a rapid wash-in system.
Results: 112 patients completed at least one LCI assessment and 98 (90%) were still under follow-up at study end. The median (IQR) age was 14.7 (8.6-22.2) years and the mean (SD) FEV1 z-score was -1.2 (1.3). Of 81 subjects with normal FEV1 (>-2 z-scores), 63% had raised LCI (indicating worse lung function). For repeat stable measurements within 6 months, the mean (limits of agreement) change in LCI was 0.9% (-18.8% to 20.7%). A latent class growth model analysis identified four discrete clusters with high accuracy, differentiated by baseline LCI and FEV1. Baseline LCI was the strongest factor associated with longitudinal change. The median total test time was under 19 min.
Conclusions: Most patients with CF with well-preserved lung function show stable LCI over time. Cluster behaviours can be identified and baseline LCI is a risk factor for future progression. These results support the use of LCI in clinical practice in identifying patients at risk of lung function decline.
Dr Alex Horsley is in the Division of Infection, Immunity and Respiratory Medicine, The University of Manchester Faculty of Biology, Medicine and Health, Manchester, UK and Manchester Adult Cystic Fibrosis Centre, Manchester University NHS Foundation Trust, Manchester, UK.
Eline Lauwers, Annemiek Snoeckx , Kris Ides , Kim Van Hoorenbeeck, Maarten Lanclus , Wilfried De Backer, Jan De Backer, Stijn Verhulst. Functional respiratory imaging in relation to classical outcome measures in cystic fibrosis: a cross-sectional study. BMC Pulm Med 2021 Aug 4;21(1):256.doi: 10.1186/s12890-021-01622-3. Free PMC article [Pubmed]

Eline Lauwers
Background: Functional Respiratory Imaging (FRI) combines HRCT scans with computational fluid dynamics to provide objective and quantitative information about lung structure and function. FRI has proven its value in pulmonary diseases such as COPD and asthma, but limited studies have focused on cystic fibrosis (CF). This study aims to investigate the relation of multiple FRI parameters to validated imaging parameters and classical respiratory outcomes in a CF population.
Methods: CF patients aged > 5 years scheduled for a chest CT were recruited in a cross-sectional study. FRI outcomes included regional airway volume, airway wall volume, airway resistance, lobar volume, air trapping and pulmonary blood distribution. Besides FRI, CT scans were independently evaluated by 2 readers using the CF-CT score. Spirometry and the 6-Minute Walk Test (6MWT) were also performed. Statistical tests included linear mixed-effects models, repeated measures correlations, Pearson and Spearman correlations.
Results: 39 CT scans of 24 (17M/7F) subjects were analyzed. Patients were 24 ± 9 years old and had a ppFEV1 of 71 ± 25% at the time of the first CT. All FRI parameters showed significant low-to-moderate correlations with the total CF-CT score, except for lobar volume. When considering the relation between FRI parameters and similar CF-CT subscores, significant correlations were found between parameters related to airway volume, air trapping and airway wall thickening. Air trapping, lobar volume after normal expiration and pulmonary blood distribution showed significant associations with all spirometric parameters and oxygen saturation at the end of 6MWT. In addition, air trapping was the only parameter related to the distance covered during 6MWT. A subgroup analysis showed considerably higher correlations in patients with mild lung disease (ppFEV1 ≥ 70%) compared to patients with moderate to severe lung disease (ppFEV1 < 70%) when comparing FRI to CF-CT scores.
Conclusions: Multiple structural characteristics determined by FRI were associated with abnormalities determined by CF-CT score. Air trapping and pulmonary blood distribution appeared to be the most clinically relevant FRI parameters for CF patients due to their associations with classical outcome measures. The FRI methodology could particularly be of interest for patients with mild lung disease, although this should be confirmed in future research.
Dr Eline Lauwers is a PhD researcher at the Laboratory of Experimental Medicine and Pediatrics, Faculty of Medicine and Health Sciences, University of Antwerp, Universiteitsplein 1, 2160, Wilrijk, Belgium and the Infla-Med Research Consortium of Excellence, University of Antwerp, Antwerp, Belgium.
Philippe Reix, Aurélie Tatopoulos, Iulia Ioan, Muriel Le Bourgeois, Stéphanie Bui, Marie Luce Choukroun, Katia Bessaci-Kabouya, Michele Gerardin, Plamen Bokov, Jennifer Da Silva, Jean-Louis Paillasseur, Pierre Regis Burgel, French Cystic Fibrosis Reference Network study group. Real-world assessment of LCI following lumacaftor-ivacaftor initiation in adolescents and adults with cystic fibrosis. J Cyst Fibros 2021 Jun 25;S1569-1993(21)01286-8.doi: 10.1016/j.jcf.2021.06.002.Online ahead of print. [Pubmed]
Lung clearance index (LCI) is a biomarker of ventilation inhomogeneity. Data are scarce on its usefulness in daily practice for monitoring the effects of treatments in older children and adults with CF. In this French observational study of lumacaftor-ivacaftor, 63 of 845 patients (7.5%) had available LCI performed at baseline and at six (M6; n=34) or 12 months (M12; n=46) after lumacaftor-ivacaftor initiation. At inclusion, median [IQR] age was 16 years [13-17], ppFEV1 was 72.8 [59.6-80.7], and LCI was 12.3 [10.3-15.0].
At both M6 and M12, non statistically significant LCI increases of 0.13 units or 1.34% (95% CI: -4.85-7.53) and 0.6 units or 6.66% (95% CI: -0.03-13.5) were observed. Discordant results between LCI and ppFEV1 were observed in one-third of the patients.
In daily practice, LCI monitoring in adolescents and young adults with moderate lung disease gives results that are more heterogenous than those reported in children with milder disease.
Dr Philippe Reix is at the Cystic Fibrosis Center, Hospices Civils de Lyon, Lyon, France; UMR 5558 CNRS Equipe EMET Université Claude Bernard Lyon 1 Lyon, France.
Elisabeth Kieninger, Corin Willers, Katrin Röthlisberger, Sophie Yammine, Orso Pusterla, Grzegorz Bauman, Enno Stranzinger, Oliver Bieri , Philipp Latzin, Carmen Casaulta. Effect of Salbutamol on Lung Ventilation in Children with Cystic Fibrosis: Comprehensive Assessment Using Spirometry, Multiple-Breath Washout, and Functional Lung Magnetic Resonance Imaging. Respiration 2021 Nov 22;1-10.doi: 10.1159/000519751. Online ahead of print. [Pubmed]

Elisabeth Kieninger
Background: Inhalation therapy is one of the cornerstones of the daily treatment regimen in patients with cystic fibrosis (CF). Recommendations regarding the addition of bronchodilators, especially salbutamol are conflicting due to the lack of evidence. New diagnostic measures such as multiple-breath washout (MBW) and functional magnetic resonance imaging (MRI) have the potential to reveal new insights into bronchodilator effects in patients with CF.
Objective: The objective of the study was to comprehensively assess the functional response to nebulized inhalation with salbutamol in children with CF.
Methods: Thirty children aged 6-18 years with stable CF performed pulmonary function tests, MBW, and matrix pencil-MRI before and after standardized nebulized inhalation of salbutamol.
Results: Lung clearance index decreased (improved) by -0.24 turnover (95% confidence interval [CI]: -0.53 to 0.06; p = 0.111). Percentage of the lung volume with impaired fractional ventilation and relative perfusion decreased (improved) by -0.79% (CI: -1.99 to 0.42; p = 0.194) and -1.31% (CI: -2.28 to -0.35; p = 0.009), respectively. Forced expiratory volume (FEV1) increased (improved) by 0.41 z-score (CI: 0.24-0.58; p < 0.0001). We could not identify specific clinical factors associated with a more pronounced effect of salbutamol.
Conclusions: There is a positive short-term effect of bronchodilator inhalation on FEV1 in patients with CF, which is independent of ventilation inhomogeneity. Heterogeneous response between patients suggests that for prediction of a therapeutic effect this should be tested by spirometry in every patient individually.
Elisabeth Kieninger is a Fellow in the Division of Paediatric Respiratory Medicine and Allergology, Department of Paediatrics, Inselspital, Bern University Hospital, University of Bern, Bern, Switzerland
Katarzyna Walicka-Serzysko,Magdalena Postek, Justyna Milczewska, Dorota Sands.Lung Clearance Index in Children with Cystic Fibrosis during Pulmonary Exacerbation. J Clin Med we 2021 Oct 23;10(21):4884. doi: 10.3390/jcm10214884 Free PMC article [Pubmed]

Katarzyna-Walicka-Serzysko
Background: Pulmonary exacerbation (PEx) is one of the main factors affecting the quality of life and life expectancy in patients with cystic fibrosis (CF). Our study aimed to evaluate the change in selected pulmonary function parameters, including lung clearance index (LCI), in patients with CF diagnosed with PEx.
Methods: We enrolled 40 children with CF aged 6-17. They performed spirometry and multiple breath nitrogen washout (MBNW) tests during a stable condition period at the beginning and the end of intravenous antibiotic treatment.
Results: LCI increased by 65% and FEV1 decreased by ≥10% in 40% of patients with CF during PEx. An absolute change in LCI between a stable condition period and PEx was 1.05 (±1.92) units, which corresponds to a relative change of 11.48% (±18.61) of the baseline. The relative decrease in FEV1was -9.22% (±12.00) and the z-score was -0.67 (±1.13). After the PEx treatment, FEV1 increased by 11.05% (±9.04) on average, whereas LCI decreased by 1.21 ± 1.59 units on average, which represented 9.42% ± 11.40 compared to the value at the beginning of PEx.
Conclusions: The change in LCI captures a higher proportion of events with functional impairment than FEV1 in school-age children with CF.
Dr Katarzyna Walicka-Serzysko is in the Cystic Fibrosis Department, Institute of Mother and Child and the Cystic Fibrosis Centre, Pediatric Hospital, 05-092 Warsaw, Poland.
Rikke M Sandvik, Per M Gustafsson, Anders Lindblad, Frederik Buchvald, Hanne Vebert Olesen, Jørgen Hovland Olsen, Marianne Skov, Marika N Schmidt, Mette R Thellefsen, Paul D Robinson, Sune Rubak, Tacjana Pressler, Kim G Nielsen. Contemporary N 2 and SF 6 multiple breath washout in infants and toddlers with cystic fibrosis. Pediatr Pulmonol 2022 Jan 13.doi: 10.1002/ppul.25830.Online ahead of print.[Pubmed]

Rikke Sandvik
Introduction:Multiple breath washout (MBW) is used for early detection of cystic fibrosis (CF) lung disease, with SF6 MBW commonly viewed as the reference method. The use of N2 MBW in infants and toddlers has been questioned for technical and physiological reasons, but a newly correction of the N2 -signal has minimized the technical part. The present study aimed to assess the remaining differences and the contributing mechanisms for the differences between SF6 and N2 MBW,corrected – such as tidal volume reduction during N2 washout with pure O2 .
Method:This was a longitudinal multicenter cohort study. SF6 MBW and N2 MBW were performed prospectively at three CF centres in the same visits in 154 test occasions across 62 children with CF (mean age 22.7 months). Offline analysis using identical algorithms to the commercial available program provided outcomes of N2,original and N2,corrected for comparison with SF6 MBW.
Results:Mean FRCN2,corrected was 14.3% lower than FRCN2,original , and 1.0% different from FRCSF6. LCIN2,corrected was 25.2% lower than LCIN2,original , and 7.3% higher than LCISF6 . Mean (SD) tidal volume decreased significantly during N2 MBW,corrected compared to SF6 MBW (-13.1mL [-30.7; 4.6], p<0.0001, equal to -12.0% [-25.7; 1.73]), but this tidal volume reduction did not correlate to the differences between LCIN2,corrected and LCISF6 . The absolute differences in LCI increased significantly with higher LCISF6 (0.63/LCISF6 ) and (0.23/LCISF6 ) respectively for N2,original and N2,corrected , but the relative differences was stable across disease severity for N2,corrected , but not for N2,original .
Conclusion:Only minor residual differences between FRCN2,corrected and FRCSF6 remained showing that the two methods measure gas volumes very similar in this age range. Small differences in LCI were found. Tidal volume reduction during N2 MBW did not affect differences. The corrected N2 MBW can now be used with confidence in young children with CF, although not interchangeably with SF6 .
Dr Rikke M Sandvik is a researcher in the CF Centre Copenhagen, Danish Paediatric Pulmonary Service, Copenhagen University Hospital, Rigshospitalet, Copenhagen, Denmark.
Magdalena Postek, Katarzyna Walicka-Serzysko, Justyna Milczewska, Dorota Sands. What Is Most Suitable for Children With Cystic Fibrosis-The Relationship Between Spirometry, Oscillometry, and Multiple Breath Nitrogen Washout. Front Pediatr 2022 Jan 14;9:692949.doi: 10.3389/fped.2021.692949. eCollection 2021. Free PMC article [Pubmed]

Dorota Sands

Magdalena Postek
Introduction: In cystic fibrosis (CF), pathological lung changes beginearly in life. The technological progress currently gives many diagnostic possibilities. However, pulmonary function testing in children remains problematic.
Objectives: Our study aimed to correlate the results of impulse oscillometry (IOS) with those of multiple breath nitrogen washout (MBNW) in our pediatric CF population. We also compared those parameters between the groups with and without spirometric features of obturation.
Methods: We collected 150 pulmonary function test sets, including spirometry, IOS, and MBNW in patients with CF aged 12.08 ± 3.85 years [6-18]. The study group was divided into two subgroups: IA (without obturation) and IB (with obturation). We also compared Sacin, Scond, and oscillometry parameters of 20 patients aged 14-18 years who reached the appropriate tidal volume (VT) during MBNW.
Results: Statistical analysis showed a negative correlation between lung clearance index (LCI) and spimoetric parameters. Comparison of subgroups IA (n = 102) and IB (n = 48) indicated a statistically significant difference in LCI (p < 0.001) and FEV1z-score (p < 0.001), FEV1% pred (p < 0.001), MEF25z-score (p < 0.001), MEF50 z-score (p < 0.001), MEF75 z-score (p < 0.001), R5% pred (p < 0.05), and R20% pred (p < 0.01). LCI higher than 7.91 was found in 75.33% of the study group, in subgroup IB-91.67%, and IA-67.6%.
Conclusions: LCI derived from multiple breath nitrogen washout (MBNW) may be a better tool than impulse oscillometry (IOS) for assessing pulmonary function in patients with CF, particularly those who cannot perform spirometry.
Dr Magdalena Postek is in the Cystic Fibrosis Department, Institute of Mother and Child, Warsaw, Poland and the Cystic Fibrosis Centre, Pediatric Hospital, Dziekanów Leśny, Poland.
Marcus Svedberg, Henrik Imberg, Per Gustafsson, Mela Brink, HåkanCaisander, Anders Lindblad. Chest x-rays are less sensitive than multiple breath washout examinations when it comes to detecting early cystic fibrosis lung disease. Acta Paediatr 2022 Feb 18.doi: 10.1111/apa.16302. Online ahead of print. [Pubmed]

Marcus Svedberg
Aim: Annual chest x-ray is recommended as routine surveillance to track cystic fibrosis (CF) lung disease. The aim of this study was to investigate the clinical utility of chest x-rays to track CF lung disease.
Methods: Children at Gothenburg’s CF centre who underwent chest x-rays, multiple breath washouts and chest computed tomography examinations between 1996-2016 were included in the study. Chest x-rays were interpreted with Northern Score (NS). We compared NS to lung clearance index (LCI) and structural lung damage measured by computed tomography using a logistic regression model.
Results: A total of 75 children were included over a median period of 13 years (range: 3.0-18.0 years). The proportion of children with abnormal NS was significantly lower than the proportion of abnormal LCI up to the age of 4 years (p<0.05). A normal NS and a normal LCI at age 6 years, were associated with a median (10-90th percentile) total airway disease of 1.8% (0.4-4.7%) and bronchiectasis of 0.2% (0.0-1.5%).
Conclusion: Chest x-rays were less sensitive than multiple breath washout examinations to detect early CF lung disease. The combined results from both methods can be used as an indicator to perform chest computed tomography less frequently.
Marcus Svedberg is at the Department of Pediatrics, Institute of Clinical Science at The Sahlgrenska Academy, University of Gothenburg, Gothenburg, Sweden. and the Department of Pediatrics, Queen Silvia’s Children Hospital, Gothenburg, Sweden
Jobst F Roehmel, Friederike J Doerfler, Cordula Koerner-Rettberg, Folke Brinkmann, Anne Schlegtendal, Martin Wetzke, Isa Rudolf, Simone Helms, Joerg Große-Onnebrink, Yin Yu, Thomas Nuesslein, Irena Wojsyk-Banaszak, Sebastian Becke, Olaf Eickmeier, Olaf Sommerburg, Heymut Omran, Mirjam Stahl, Marcus A Mall Comparison of the Lung Clearance Index in Preschool Children with Primary Ciliary Dyskinesia and Cystic Fibrosis Chest. 2022 Mar 7;S0012-3692(22)00421-4.doi: 10.1016/j.chest.2022.02.052.Online ahead of print. [Pubmed]

Jobst Roshmel
Background: Previous studies have shown that the lung clearance index (LCI) determined by multiple-breath washout (MBW) is sensitive to detect early lung disease in preschool children with cystic fibrosis (CF). In preschool children with primary ciliary dyskinesia (PCD), data on the onset and severity of lung disease and on the sensitivity of the LCI as a noninvasive quantitative outcome measure remain limited.
Research and study question: Is MBW feasible and sensitive to detect ventilation inhomogeneity in preschool children with PCD?
Study design and methods: This was a prospective cross-sectional multicenter study and included preschoolers with PCD and preschoolers with CF and healthy controls. LCI was determined using nitrogen MBW, and compared between the three groups.
Results: LCI was determined in 27 children with PCD, 34 children with CF and 30 healthy controls (mean age, 4.8 years; range, 2.2 – 6.9 years). The LCI in preschool children with PCD was increased (median, 9.1; CI 95%, 8.6-10.3) compared to healthy controls (median, 7.0; CI 95%, 6.7-7.1), (P < 0.0001), but did not differ from preschool children with CF (median, 8.6; CI 95%, 8.4-9.7), (P = 0.71). The feasibility in the PCD group was 93.1% and was similar to that in the CF group (91.9%) and in healthy controls (85.7%), (P = 0.55).
Interpretation: This study demonstrates early onset of lung disease in preschool children with PCD and indicates that lung disease severity in PCD may be similar to that in CF during preschool years. These data support a need for early diagnostic monitoring and therapy and suggest the LCI as a noninvasive diagnostic tool and as a potential endpoint in clinical trials testing early interventions in children with PCD.
Dr Jobst F Roehmel is consultant paediatrician in the Department of Pediatric Respiratory Medicine, Immunology and Critical Care Medicine, Charité – Universitätsmedizin Berlin, corporate member of Freie Universität Berlin and Humboldt-Universität zu Berlin, Berlin, Germany.
Elisabeth Kieninger, Corin Willers, Katrin Röthlisberger, Sophie Yammine, Orso Pusterla, Grzegorz Bauman, Enno Stranzinger, Oliver Bieri, Philipp Latzin, Carmen Casaulta. Effect of Salbutamol on Lung Ventilation in Children with Cystic Fibrosis: Comprehensive Assessment Using Spirometry, Multiple-Breath Washout, and Functional Lung Magnetic Resonance Imaging. Respiration 2022;101(3):281-290. doi: 10.1159/000519751. Epub 2021 Nov 22. [Pubmed]

Dr Elisabeth Kieninger
Background: Inhalation therapy is one of the cornerstones of the daily treatment regimen in patients with cystic fibrosis (CF). Recommendations regarding the addition of bronchodilators, especially salbutamol are conflicting due to the lack of evidence. New diagnostic measures such as multiple-breath washout (MBW) and functional magnetic resonance imaging (MRI) have the potential to reveal new insights into bronchodilator effects in patients with CF.
Objective: The objective of the study was to comprehensively assess the functional response to nebulized inhalation with salbutamol in children with CF.
Methods: Thirty children aged 6-18 years with stable CF performed pulmonary function tests, MBW, and matrix pencil-MRI before and after standardized nebulized inhalation of salbutamol.
Results: Lung clearance index decreased (improved) by -0.24 turnover (95% confidence interval [CI]: -0.53 to 0.06; p = 0.111). Percentage of the lung volume with impaired fractional ventilation and relative perfusion decreased (improved) by -0.79% (CI: -1.99 to 0.42; p = 0.194) and -1.31% (CI: -2.28 to -0.35; p = 0.009), respectively. Forced expiratory volume (FEV1) increased (improved) by 0.41 z-score (CI: 0.24-0.58; p < 0.0001). We could not identify specific clinical factors associated with a more pronounced effect of salbutamol.
Conclusions: There is a positive short-term effect of bronchodilator inhalation on FEV1 in patients with CF, which is independent of ventilation inhomogeneity. Heterogeneous response between patients suggests that for prediction of a therapeutic effect this should be tested by spirometry in every patient individually.
Elisabeth Kieninger is a Fellow in the Division of Paediatric Respiratory Medicine and Allergology, Department of Paediatrics, Inselspital, Bern University Hospital, University of Bern, Bern, Switzerland.
Lucy Perrem, Sanja Stanojevic, Melinda Solomon, Hartmut Grasemann, Neil Sweezey, Valerie Waters, Don B Sanders, Stephanie D Davis, Felix Ratjen. Evaluation of clinically relevant changes in the lung clearance index in children with cystic fibrosis and healthy controls. Thorax. 2022 Apr 15;thoraxjnl-2021-218347.doi: 10.1136/thoraxjnl-2021-218347.Online ahead of print. [Pubmed]

Lucy Perrem
Background:The limits of reproducibility of the lung clearance index (LCI) are higher in children with cystic fibrosis (CF) compared with healthy children, and it is currently unclear what defines a clinically meaningful change.
Methods:In a prospective multisite observational study of children with CF and healthy controls (HCs), we measured LCI, FEV1% predicted and symptom scores at quarterly visits over 2 years. Two reviewers performed a detailed review of visits to evaluate the frequency that between visit LCI changes outside ±10%, ±15%, ±20% represented a clinically relevant signal. In the setting of acute respiratory symptoms, we used a generalised estimating equation model, with a logit link function to determine the ability of LCI worsening at different thresholds to predict failure of lung function recovery at follow-up.
Results:Clinically relevant LCI changes outside ±10%, ±15% and ±20% were observed at 25.7%, 15.0% and 8.3% of CF visits (n=744), respectively. The proportions of LCI changes categorised as noise, reflecting biological variability, were comparable between CF and HC at the 10% (CF 9.9% vs HC 13.0%), 15% (CF 4.3% vs HC 3.1%) and 20% (CF 2.4% vs HC 1.0%) thresholds. Compared with symptomatic CF visits without a worsening in LCI, events with ≥10% LCI increase were more likely to fail to recover baseline LCI at follow-up.
Conclusion:The limits of reproducibility of the LCI in healthy children can be used to detect clinically relevant changes and thus inform clinical care in children with CF.
Dr Lucy Perrem is involved with the Division of Respiratory Medicine, The Hospital for Sick Children, Toronto, Ontario, Canada, Postgraduate Medical Education, Royal College of Surgeons in Ireland, Dublin, Ireland. National Children’s Research Centre, Dublin, Ireland. Department of Paediatrics, The University of Toronto, Toronto, Ontario, Canada. Translational Medicine Program, SickKids Research Institute, Toronto, Ontario, Canada.
Vaclav Koucky, Arnost Komarek, Petr Pohunek. Repeatability of lung clearance index in infants with cystic fibrosis and recurrent wheeze. Pediatr Pulmonol 2022 Apr 13.doi: 10.1002/ppul.25921. Online ahead of print. [Pubmed]

Vaclav Koucky
Objectives: To describe the short- and medium-term repeatability of lung clearance index (LCI2.5) in infants and calculate the number of patients needed to enrol in a study (N) using LCI2.5 as a primary outcome.
Methods: An 8-month follow-up observational study was employed for assessing short-term [coefficient of repeatability (CR) and intraclass correlation (ICC)] and medium-term repeatability (Bland-Altman method) of LCI2.5 in infants with cystic fibrosis (CF) or recurrent wheeze (RW) measured by the nitrogen multiple-breath washout test (N2 -MBW). Using these variability data, the N to reach 90% test power at the level of statistical significance (0.05) was calculated.
Results: Forty infants with CF and 21 with RW were enrolled. Initial N2 -MBW testing was successful in 33 and 17 patients, respectively. Follow-up data were available for 23 and 11 infants, respectively. Short-term repeatability of LCI2.5 was high (CR = 1.10 and 1.04 in CF and RW patients, respectively; ICC = 0.88 and 0.83 in CF and RW patients, respectively). The between-subject standard deviation was <13% of the actual LCI2.5 value. In clinically stable patients, LCI2.5did not significantly change during the 8-month follow-up. Mean LCI2.5 change was -0.08 (1% of baseline) in CF and -0.05 (0.6%) in RW, with 95% limits of agreement being (-1.70; 1.53) in CF and (-1.51; 1.40) in RW patients. N = 23 infants if both intra-group differences of LCI2.5 and minimal difference to be detected would be 2.0.
Conclusion: N2 -MBW may be a reproducible tool with reasonable test power to detect differences in infant studies. This article is protected by copyright. All rights reserved.
Dr Vaclav Koucky is a paediatric pulmonologist in the Department of Paediatrics, 2nd Faculty of Medicine, Charles University and University Hospital Motol, Prague, Czech Republic.
Amy Macdougall, Deborah Jarvis, Ruth H Keogh, Cole Bowerman, Diana Bilton, Gwyneth Davies, Siobhán B Carr, Sanja Stanojevic Trajectories of early growth and subsequent lung function in cystic fibrosis: An observational study using UK and Canadian registry data. J Cyst Fibros 2022 Sep 7;S1569-1993(22)00658-0.doi: 10.1016/j.jcf.2022.09.001.Online ahead of print. Free article pubmed.ncbi.nlm.nih.gov

Amy Macdougall Linked in
Background: Understanding the pulmonary impact of changes in early life nutritional status over time in a paediatric CF population may help inform how to use nutritional assessment to guide clinical care. National registry data provides an opportunity to study patterns of weight gain over time at the level of the individual, and thus to gain detailed understanding of the relationship between early weight trajectories and later lung function in children with Cystic Fibrosis (CF).
Methods: Using data from the United Kingdom (UK) and Canadian CF Registries, a mixed effects linear regression model was used to describe children’s weight and BMI z-score trajectories from age 1 to 5 years. The intercept (weight-for-age at age 1) and slope (weight-for-age trajectory) from this model were then used as covariates in a linear regression of first lung function measurement at age 6 years.
Results: In both the UK and Canadian data, greater weight-for-age z-score at age 1 year and greater change in weight-for-age over time were associated with higher FEV1% predicted. A greater weight-for-age z-score at age 1 year was associated with a higher FEV1% predicted (UK: 3.78% (95% CI: 1.76; 4.70); Canada: 3.20% (95%CI: 1.76, 4.70)). These associations were reproduced for BMI z-scores and FVC% predicted.
Conclusions: Early weight-for-age, specifically at age 1 year, and weight-for-age trajectories across early childhood are associated with later lung function. This relationship persists after adjustment for potential confounders. Current guidelines may need to be updated to place less emphasis on a specific cut-off (such as the 10th percentile) and encourage tracking of weight-for-age over time
Dr Amy Macdougall is a research fellow is at the National Heart and Lung Institute, Imperial College London, London, United Kingdom.
Emma Raywood , Harriet Shannon , Nicole Filipow , Gizem Tanriver , Sanja Stanojevic , Kunal Kapoor , Helen Douglas , Rachel O’Connor , Nicky Murray , Bridget Black , Eleanor Main. Quantity and quality of airway clearance in children and young people with cystic fibrosis. J Cyst Fibros. 2022 Oct 6;S1569-1993(22)00686-5. doi: 10.1016/j.jcf.2022.09.008. Online ahead of print. pubmed.ncbi.nlm.nih.gov/36210322/]

Emma Raywood crunchable.com
Children and young people with CF (CYPwCF) get advice about using positive expiratory pressure (PEP) or oscillating PEP (OPEP) devices to clear sticky mucus from their lungs. However, little is known about the quantity (number of treatments, breaths, or sets) or quality (breath pressures and lengths) of these daily airway clearance techniques (ACTs) undertaken at home. This study used electronic pressure sensors to record real time breath-by-breath data from 145 CYPwCF (6-16y) during routine ACTs over 2 months. ACT quantity and quality were benchmarked against individual prescriptions and accepted recommendations for device use. In total 742,084 breaths from 9,081 treatments were recorded. Individual CYPwCF maintained consistent patterns of ACT quantity and quality over time. Overall, 60% of CYPwCF did at least half their prescribed treatments, while 27% did fewer than a quarter. About 77% of pre-teens did the right number of daily treatments compared with only 56% of teenagers. CYPwCF usually did the right number of breaths. ACT quality (recommended breath length and pressure) varied between participants and depended on device. Breath pressures, lengths and pressure-length relationships were significantly different between ACT devices. PEP devices encouraged longer breaths with lower pressures, while OPEP devices encouraged shorter breaths with higher pressures. More breaths per treatment were within advised ranges for both pressure and length using PEP (30-31%) than OPEP devices (1-3%). Objective measures of quantity and quality may help to optimise ACT device selection and support CYPwCF to do regular effective ACTs.
Emma Raywood is a physiotherapist at UCL Great Ormond Street Institute of Child Health, London
Jobst F Roehmel, Friederike J Doerfler, Cordula Koerner-Rettberg, Folke Brinkmann, Anne Schlegtendal, Martin Wetzke, Isa Rudolf, Simone Helms, Joerg Große-Onnebrink, Yin Yu, Thomas Nuesslein, Irena Wojsyk-Banaszak, Sebastian Becke, Olaf Eickmeier, Olaf Sommerburg, Heymut Omran, Mirjam Stahl, Marcus A Mall Comparison of the Lung Clearance Index in Preschool Children with Primary Ciliary Dyskinesia and Cystic Fibrosis Chest. 2022 Mar 7;S0012-3692(22)00421-4.doi: 10.1016/j.chest.2022.02.052.Online ahead of print. [Pubmed]

Jobst Roshmel
Background:Previous studies have shown that the lung clearance index (LCI) determined by multiple-breath washout (MBW) is sensitive to detect early lung disease in preschool children with cystic fibrosis (CF). In preschool children with primary ciliary dyskinesia (PCD), data on the onset and severity of lung disease and on the sensitivity of the LCI as a noninvasive quantitative outcome measure remain limited.
Research and study question:Is MBW feasible and sensitive to detect ventilation inhomogeneity in preschool children with PCD?
Study design and methods:This was a prospective cross-sectional multicenter study and included preschoolers with PCD and preschoolers with CF and healthy controls. LCI was determined using nitrogen MBW, and compared between the three groups.
Results:LCI was determined in 27 children with PCD, 34 children with CF and 30 healthy controls (mean age, 4.8 years; range, 2.2 – 6.9 years). The LCI in preschool children with PCD was increased (median, 9.1; CI 95%, 8.6-10.3) compared to healthy controls (median, 7.0; CI 95%, 6.7-7.1), (P < 0.0001), but did not differ from preschool children with CF (median, 8.6; CI 95%, 8.4-9.7), (P = 0.71). The feasibility in the PCD group was 93.1% and was similar to that in the CF group (91.9%) and in healthy controls (85.7%), (P = 0.55).
Interpretation:This study demonstrates early onset of lung disease in preschool children with PCD and indicates that lung disease severity in PCD may be similar to that in CF during preschool years. These data support a need for early diagnostic monitoring and therapy and suggest the LCI as a noninvasive diagnostic tool and as a potential endpoint in clinical trials testing early interventions in children with PCD.
Dr Jobst F Roehmel is consultant paediatrician in the Department of Pediatric Respiratory Medicine, Immunology and Critical Care Medicine, Charité – Universitätsmedizin Berlin, corporate member of Freie Universität Berlin and Humboldt-Universität zu Berlin, Berlin, Germany.
Bettina S Frauchiger , Kathryn A Ramsey , Jakob Usemann , Elisabeth Kieninger, Carmen Casaulta, Daniel Sirtes, Sophie Yammine , Ben Spycher , Alexander Moeller , Philipp Latzin.Variability of clinically measured lung clearance index in children with cystic fibrosis. Pediatr Pulmonol. 2022 Oct 17. doi: 10.1002/ppul.26180. Online ahead of print. https://pubmed.ncbi.nlm.nih.gov/36251441

Bettina Frauchiger Linkedin
Rationale: The lung clearance index (LCI) is increasingly being used in the clinical surveillance of patients with cystic fibrosis (CF). However, there are limited data on long-term variability and clinically relevant changes in LCI during routine clinical surveillance
Objectives: To evaluate long-term variability of LCI and propose a threshold for a physiologically relevant change.
Methods: Children with CF aged 4-18 years performed LCI measurements every three months as part of routine clinical surveillance during 2011-2020 in two centers. The variability of LCI during periods of clinical stability was assessed using mixed-effects models and was used to identify thresholds for clinically relevant changes.
Results: Repeated LCI measurements of acceptable quality (N= 858) were available in 100 patients with CF, for 74 patients 399 visits at clinical stability were available. Variability of repeated LCI measurements over time expressed as coefficient of variation (CV%) was 7.4%. The upper limit of normal (ULN) for relative changes in LCI between visits was 19%.
Conclusion: We report the variability of LCI in children and adolescents with CF during routine clinical surveillance. According to our data, a change in LCI beyond 19% may be considered physiologically relevant. These findings will help guide clinical decisions according to LCI changes.
Bettina S Frauchiger is in the Respiratory Medicine, Department of Pediatrics, Inselspital, Bern University Hospital, University of Bern, Bern, Switzerland.
Alex R Horsley, John Belcher, Katie Bayfield, Brooke Bianco, Steve Cunningham, Catherine Fullwood , Andrew Jones, Anna Shawcross, Jaclyn A Smith, Anirban Maitra, Francis J Gilchrist. Longitudinal assessment of lung clearance index to monitor disease progression in children and adults with cystic fibrosis. Thorax 2022 Apr;77(4):357-363.doi: 10.1136/thoraxjnl-2021-216928. Epub 2021 Jul 22. Free PMC article [Pubmed]

Alex Horsley researchgate.net
Background: Lung clearance index (LCI) is a valuable research tool in cystic fibrosis (CF) but clinical application has been limited by technical challenges and uncertainty about how to interpret longitudinal change. In order to help inform clinical practice, this study aimed to assess feasibility, repeatability and longitudinal LCI change in children and adults with CF with predominantly mild baseline disease.
Methods: Prospective, 3-year, multicentre, observational study of repeated LCI measurement at time of clinical review in patients with CF >5 years, delivered using a rapid wash-in system
Results: 112 patients completed at least one LCI assessment and 98 (90%) were still under follow-up at study end. The median (IQR) age was 14.7 (8.6-22.2) years and the mean (SD) FEV1z-score was -1.2 (1.3). Of 81 subjects with normal FEV1 (>-2 z-scores), 63% had raised LCI (indicating worse lung function). For repeat stable measurements within 6 months, the mean (limits of agreement) change in LCI was 0.9% (-18.8% to 20.7%). A latent class growth model analysis identified four discrete clusters with high accuracy, differentiated by baseline LCI and FEV1. Baseline LCI was the strongest factor associated with longitudinal change. The median total test time was under 19 min.
Conclusions: Most patients with CF with well-preserved lung function show stable LCI over time. Cluster behaviours can be identified and baseline LCI is a risk factor for future progression. These results support the use of LCI in clinical practice in identifying patients at risk of lung function decline.
Dr Alex Horsley is in the Division of Infection, Immunity and Respiratory Medicine, The University of Manchester Faculty of Biology, Medicine and Health, Manchester, UK and the Manchester Adult Cystic Fibrosis Centre, Manchester University NHS Foundation Trust, Manchester, UK.
Elisabeth Kieninger, Corin Willers, Katrin Röthlisberger, Sophie Yammine, Orso Pusterla, Grzegorz Bauman, Enno Stranzinger, Oliver Bieri, Philipp Latzin, Carmen Casaulta. Effect of Salbutamol on Lung Ventilation in Children with Cystic Fibrosis: Comprehensive Assessment Using Spirometry, Multiple-Breath Washout, and Functional Lung Magnetic Resonance Imaging. Respiration 2022;101(3):281-290. doi: 10.1159/000519751. Epub 2021 Nov 22. pubmed.ncbi.nlm.nih.gov/34808631/

Elisabeth Kieninger kinderklinik.insel.ch
Background: Inhalation therapy is one of the cornerstones of the daily treatment regimen in patients with cystic fibrosis (CF). Recommendations regarding the addition of bronchodilators, especially salbutamol are conflicting due to the lack of evidence. New diagnostic measures such as multiple-breath washout (MBW) and functional magnetic resonance imaging (MRI) have the potential to reveal new insights into bronchodilator effects in patients with CF.
Objective: The objective of the study was to comprehensively assess the functional response to nebulized inhalation with salbutamol in children with CF.
Methods: Thirty children aged 6-18 years with stable CF performed pulmonary function tests, MBW, and matrix pencil-MRI before and after standardized nebulized inhalation of salbutamol.
Results: Lung clearance index decreased (improved) by -0.24 turnover (95% confidence interval [CI]: -0.53 to 0.06; p = 0.111). Percentage of the lung volume with impaired fractional ventilation and relative perfusion decreased (improved) by -0.79% (CI: -1.99 to 0.42; p = 0.194) and -1.31% (CI: -2.28 to -0.35; p = 0.009), respectively. Forced expiratory volume (FEV1) increased (improved) by 0.41 z-score (CI: 0.24-0.58; p < 0.0001). We could not identify specific clinical factors associated with a more pronounced effect of salbutamol.
Conclusions: There is a positive short-term effect of bronchodilator inhalation on FEV1 in patients with CF, which is independent of ventilation inhomogeneity. Heterogeneous response between patients suggests that for prediction of a therapeutic effect this should be tested by spirometry in every patient individually.
Elisabeth Kieninger is a Fellow in the Division of Paediatric Respiratory Medicine and Allergology, Department of Paediatrics, Inselspital, Bern University Hospital, University of Bern, Bern, Switzerland.
Bettina S Frauchiger , Kathryn A Ramsey , Jakob Usemann , Elisabeth Kieninger, Carmen Casaulta, Daniel Sirtes, Sophie Yammine , Ben Spycher , Alexander Moeller , Philipp Latzin.Variability of clinically measured lung clearance index in children with cystic fibrosis. Pediatr Pulmonol. 2022 Oct 17. doi: 10.1002/ppul.26180. Online ahead of print. https://pubmed.ncbi.nlm.nih.gov/36251441

Bettina Frauchiger Linkedin
Rationale: The lung clearance index (LCI) is increasingly being used in the clinical surveillance of patients with cystic fibrosis (CF). However, there are limited data on long-term variability and clinically relevant changes in LCI during routine clinical surveillance
Objectives: To evaluate long-term variability of LCI and propose a threshold for a physiologically relevant change.
Methods: Children with CF aged 4-18 years performed LCI measurements every three months as part of routine clinical surveillance during 2011-2020 in two centers. The variability of LCI during periods of clinical stability was assessed using mixed-effects models and was used to identify thresholds for clinically relevant changes.
Results: Repeated LCI measurements of acceptable quality (N= 858) were available in 100 patients with CF, for 74 patients 399 visits at clinical stability were available. Variability of repeated LCI measurements over time expressed as coefficient of variation (CV%) was 7.4%. The upper limit of normal (ULN) for relative changes in LCI between visits was 19%.
Conclusion: We report the variability of LCI in children and adolescents with CF during routine clinical surveillance. According to our data, a change in LCI beyond 19% may be considered physiologically relevant. These findings will help guide clinical decisions according to LCI changes.
Bettina S Frauchiger is in the Respiratory Medicine, Department of Pediatrics, Inselspital, Bern University Hospital, University of Bern, Bern, Switzerland.
Jennifer L Goralski , Sang Hun Chung , Agathe S Ceppe , Margret Z Powell, Muthu Sakthivel, Brian D Handly, Yueh Z Lee , Scott H Donaldson.Dynamic Perfluorinated Gas MRI Shows Improved Lung Ventilation in People with Cystic Fibrosis after Elexacaftor/Tezacaftor/Ivacaftor: An Observational Study. J Clin Med. 2022 Oct 19;11(20):6160. doi: 10.3390/jcm11206160. pubmed.ncbi.nlm.nih.gov/36294480/

Jennifer Goralski UNC School of medicine
The availability of highly effective CFTR modulators is revolutionizing the treatment of cystic fibrosis (CF) and drastically improving outcomes. MRI-based imaging modalities are now emerging as highly sensitive endpoints, particularly in the setting of mild lung disease. Adult CF patients were recruited from a single center prior to starting treatment with E/T/I. The following studies were obtained before and after one month on treatment: spirometry, multiple breath nitrogen washout (MBW), 1H UTE MRI (structural images) and 19F MRI (ventilation images). Changes between visits were calculated, as were correlations between FEV1, lung clearance index (LCI), MRI structural scores, and MRI-based ventilation descriptors. Eight subjects had complete datasets for evaluation. Consistent with prior clinical trials, FEV1 and LCI improved after 28 days of E/T/I use. 1H UTE MRI detected improvements in bronchiectasis/airway wall thickening score and mucus plugging score after 28 days of therapy. 19F MRI demonstrated improvements in fractional lung volume with slow gas washout time (FLV↑tau2) and ventilation defect percentage (VDP). Improvements in FLV↑tau2 and VDP correlated with improvement in FEV1 (r = 0.81 and 0.86, respectively, p < 0.05). This observational study establishes the ability of 19F MRI and 1H UTE MRI to detect improvements in lung structure and function after E/T/I treatment. This study supports further development of 19F MRI and 1H UTE MRI as outcome measures for cystic fibrosis research and drug development.
Dr Jennifer Goralski is at Division of Pulmonary and Critical Care Medicine, University of North Carolina at Chapel Hill, Chapel Hill, NC 27599, ; the Marsico Lung Institute/UNC Cystic Fibrosis Center, University of North Carolina at Chapel Hill, Chapel Hill, NC 27599, and the Division of Pediatric Pulmonology, University of North Carolina at Chapel Hill, Chapel Hill, NC 27599, USA.
Carmen Streibel, Corin C Willers , Orso Pusterla , Grzegorz Bauman, Enno Stranzinger, Ben Brabandt , Oliver Bieri, Marion Curdy, Marina Bullo, Bettina Sarah Frauchiger , Insa Korten, Linn Krüger, Carmen Casaulta, Felix Ratjen, Philipp Latzin, Elisabeth Kieninger. Effects of elexacaftor/tezacaftor/ivacaftor therapy in children with cystic fibrosis – a comprehensive assessment using lung clearance index, spirometry, and functional and structural lung MRI . J Cyst Fibros. 2023 Jan 10;S1569-1993(22)01432-1. doi: 10.1016/j.jcf.2022.12.012. Online ahead of print. pubmed.ncbi.nlm.nih.gov/36635199/

Carmen Streibel
Background: With improvement in supportive therapies and the introduction of cystic fibrosis transmembrane conductance regulator (CFTR)-modulator treatment in patients with cystic fibrosis (CF), milder disease courses are expected. Therefore, sensitive parameters are needed to monitor disease course and effects of CFTR-modulators. Functional lung MRI using matrix-pencil decomposition (MP-MRI) is a promising tool for assessing ventilation and perfusion quantitatively. This study aimed to assess the treatment effect of elexacaftor/tezacaftor/ivacaftor combination regimen (ELX/TEZ/IVA) on measures of structural and functional lung abnormalities.
Methods: 24 children with CF underwent lung function tests (multiple breath washout, spirometry), functional and structural MRI twice (one year apart) before and once after at least two weeks (mean 4.7 ± 2.6 months) on ELX/TEZ/IVA. Main outcomes were changes (Δ) upon ELX/TEZ/IVA in lung function, defect percentage of ventilation (VDP) and perfusion (QDP), defect distribution index of ventilation and perfusion (DDIV, DDIQ), and Eichinger score. Statistical analyses were performed using paired t-tests and multilevel regression models with bootstrapping.
Results: We observed a significant improvement in lung function, structural and functional MRI parameters upon ELX/TEZ/IVA treatment (mean; 95%-CI): ΔLCI2.5 (TO) -0.84 (-1.62 to -0.06); ΔFEV1 (z-score) 1.05 (0.56 to 1.55); ΔVDP (% of impairment) -6.00 (-8.44 to -3.55); ΔQDP (% of impairment) -3.90 (-5.90 to -1.90); ΔDDIV -1.38 (-2.22 to -0.53); ΔDDIQ -0.31 (-0.73 to 0.12); ΔEichinger score -3.89 (-5.05 to -2.72).
Conclusions: Besides lung function tests, functional and structural MRI is a suitable tool to monitor treatment response of ELX/TEZ/IVA therapy, and seems promising as outcome marker in the future.
Carmen Streibel is in the Dept of Paediatric Respiratory Medicine and Allergology, Department of Paediatrics, Inselspital, Bern University Hospital, University of Bern, Switzerland.Division of Paediatric Respiratory Medicine and Allergology, Department of Paediatrics, Inselspital, Bern University Hospital, University of Bern, Switzerland.
