NUTRITION – GROWTH – DIETARY FACTORS
INCLUDING NUTRITIONAL STATUS, GUIDELINES, ENERGY BALANCE AND REQUIREMENTS, MEGESTROL (APPETITE STIMULANT), PROBIOTICS, DIETARY SUPPLEMENTS, ENTERAL FEEDING, ARTIFICIAL DIET, VITAMINS (SEE ALSO VITAMIN SECTION), SODIUM CHLORIDE, ZINC, ESSENTIAL ELEMENTS, GROWTH HORMONE, OBESITY, LIPIDS, FATTY ACIDS
The early classic papers on nutrition are reviewed in detail as there are no summaries on PubMed but only a few of the vast number of more recent papers are summarised. See also Fatty Acids, Malabsorption, Vitamins in Gastroenterology section.
1946 West CD, Wilson JL, Eyles R. Blood amino nitrogen levels: changes in blood amino nitrogen levels following ingestion of protein hydrolysate in infants with normal and with deficient pancreatic function. Am J Dis Child 1946; 72:251-273.
The absorption of whole protein and casein hydrolysate was compared. There was a significantly smaller rise in blood amino acids after a whole protein meal in infants with CF but similar increases in blood amino acids after casein hydrolysate in both normal and CF children. Authors suggested that substitution of the hydrolysate for whole protein should benefit CF children.
This was further confirmation of the suggestion of Shohl et al, 1943 (above) and subsequently shown to be useful in practice (Allan et al, 1970 & 1973 below and the “Allan diet”) that protein hydrolysate was better absorbed than whole protein by children with cystic fibrosis..
1959 Hsia DY. Birth weight in cystic fibrosis of the pancreas. Ann Hum Genet 1959; 23:289-299. [PubMed]
The mean birth weight of CF infants of 2.9kg was below that for the USA which was 3.3 kg. It was suggested that this was due to the “intrauterine insult” of the condition.
John Lloyd-Still found a similar reduction in the birth weight of CF infants (Pediatrics 1974; 54:306-311. [PubMed]). Margaret Mearns (In Hodson et al.(eds.) Cystic Fibrosis. Bailliere Tindall, London 1983;183-196) found the mean birth weight of her 257 patients to be 3.18kg boys and 3.04kg for girls – below the 3.37 and 3.25kg for unaffected infants. This was not evident in Leeds screened infants with CF whose mean birth weight of 3.3 kg was similar to that of the general local North of England population (Simmonds EJ et al. A review of infant feeding practices at a regional cystic fibrosis unit. J Hum Nutr Diet 1994; 7:31-38.). Also Holliday K& Allen J found the birth weights to be normal (J Pediatr 1991; 118:77-79.[PubMed]). However, a more recent report, in addition to noting that CF infants had a significantly lower length (-1.24SD) and weight (-0.72 SD) than normal, also noted they had a smaller head circumference (-1.82 SD) than controls( Ghosal s et al. Arch Dis Child 1995; 72:150-152. [PubMed]). However, this series was from Sheffield Children’s Hospital and contained 34.6% who had meconium ileus, for which the hospital was a referral centre. Meconium ileus may have been associated with poor intrauterine growth for which there is some evidence. For example in Toronto, 158 patients with meconium ileus had lower birth weight (3026 +/- 610 gm) than patients with no meconium ileus (3169 +/- 534 gm; p< 0.008) (Kerem E, et al. J Pediatr 1989; 114:767-73. [PubMed]).
1961 Shahidi NT, Diamond LK, Shwachman H. Anemia associated with protein deficiency. A study of 2 cases with cystic fibrosis. J Pediatr 1961; 59:533-42. [PubMed]
There was a fall in serum albumin from 4.0 to 2.6 g/dl over 30 days in an infant with CF fed a soy formula. The normal half life of 131I-labelled albumin excluded an exudative protein loosing enteropathy. The authors suggested that in CF infants soy protein absorption is more affected than cow’s milk protein.
Usually serum albumin is, rather surprisingly, within the normal range in CF unless there is significant liver involvement. However, it became apparent in a number of subsequent reports that soya based milk preparations were particularly likely to be associated with hypoproteinaemia in infants with cystic fibrosis (Fleisher et al, 1964 below).
1962 Kuo PT, Huang NN, Bassett DR. The fatty acid composition of the serum chylomicrons and adipose tissue of children with cystic fibrosis of the pancreas. J Pediatr 1962; 60:394-403. [PubMed]
The first study of fatty acids in blood and tissue lipids of patients with CF. The fatty acid composition of chylomicrons and adipose tissue from children with CF who had variable degrees of fat malabsorption was compared with the values from controls. There was a relative decrease in linoleic acid and increased palmitoleic and oleic acids. Subsequently the abnormalities have been explained as related to liver disease, the basic defect and the intestinal malabsorption.
Prof. Bob Elliott and colleagues from New Zealand published several papers showing improvement in the clinical state with supplements of medium chain triglycerides even to the extent of returning the sweat electrolytes to nearer normal values (Elliott RB. Aust Paediatr J 1972; 8:217; Elliott RB, Robinson PG. Arch Dis Child 1975; 50:75-78.[PubMed]; Elliot RB. Pediatrics 1976; 57:474-479. [PubMed]). However, subsequent studies failed to substantiate their findings (Davidson GP et al. Aust Paediatr J 1978; 14:80-82.[PubMed]; Chase HP et al. Pediatrics 1979; 64:207-213. [PubMed]); 1979 Chase HP, Long MA, Lavin MH. Cystic fibrosis and malnutrition. J Pediatr 1979; 95:337-347.[PubMed]).
1964 Fleisher DS, DiGeorge AM, Barness LA, Cornfeld D. Hypoproteinaemia and edema in infants with cystic fibrosis of the pancreas. J Pediatr 1964; 64:341-348. [PubMed]
Four infants with CF fed either human milk or soya milk had severe hypoproteinemia. The onset of oedema was around two months. Death was usually between 8-16 weeks. Soya was definitely contraindicated in infants thought to have CF. Subsequent studies showed less nitrogen absorption from soya feed than from one based on evaporated milk (Fleisher et al. J Pediatr 1964; 64:349).
An earlier instance was mentioned in a reported by Menten ML et al. in 1944 (above). and the first detailed report being that of Wissler & Zollinger in 1945 (above) according to Fleisher et al – the present authors. A further example was reported by Shahidi NT et al, 1961[PubMed] (above).
Soya based feeds definitely seem to be contraindicated for infants with cystic fibrosis.
1964 Sproul A, Huang N. Growth patterns in children with cystic fibrosis. J Pediatr 1964; 65:664-676.[PubMed]
An early detailed report of the poor nutritional state and growth of 50 children with CF studied serially. The significant retardation of weight gain and
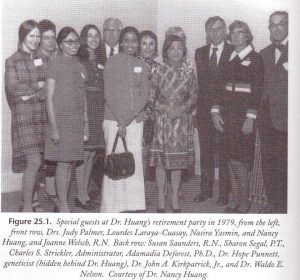
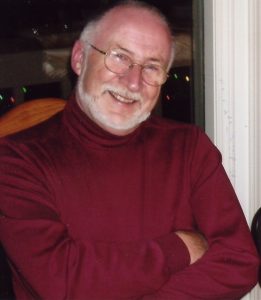
Nancy Huang’s retirement party – with some well-known guests
growth particularly in adolescent and pre-adolescent children was severe with the medians for height and weight being only between the third and tenth centiles for age. Skeletal development was delayed in 38% of children. Not surprisingly there was a significant relation between the severity of the malnutrition and the pulmonary status. Better weight gain and growth occurred when the chest was treated – improvement being most marked in infants.
Presumably a number of previously under-treated children were referred to this clinic and so the initial improvement was impressive. This was also our experience in Leeds during the Eighties but unfortunately, many children deteriorated after a short period of improvement, succumbing to their advanced pulmonary disease which had been a major factor in the first place.
1970 Allan JD, Milner J, Moss D. Therapeutic use of an artificial diet. Lancet 1970; i: 785-786. [PubMed]
The first report from Jimmy Allan, a general paediatrician from Macclesfield in the North of England, on the use of an artificial diet to improve nutrition in children with cystic fibrosis – a nutritional supplement consisting of beef serum protein hydrolysate, a glucose polymer and medium chain triglycerides.
At this time more children with CF were reaching adolescence with adverse nutritional effects of their poorly controlled malabsorption and increasingly severe chest infection which made normal weight gain and growth impossible in the majority. So understandably there was great interest in this publication (Allan et al, 1973 below).
1970 Keating JP, Feigin RD. Increased intracranial pressure associated with probable vitamin A deficiency in cystic fibrosis. Pediatrics 1970; 46:41-46. [PubMed]
Two infants with CF aged four months had signs of raised intracranial pressure associated with vitamin A deficiency. One infant had xerophthalmia and keratomalacia; one had a cranial nerve injury with facial paralysis (also Abernathy 1976 below). Raised intracranial pressure has been described by a number of authors in young infants with CF and also in non-CF infants with vitamin A deficiency examples of which are reviewed in this paper. (see also CNS Topic).
1970 Torstenson OL, Humphrey GB, Edson JR, Warwick WJ. Cystic fibrosis presenting with severe hemorrhage due to vitamin K malabsorption: A report of 3 cases. Pediatrics 1970; 45:857-861. [PubMed]
Three infants with CF presented with severe bleeding secondary to vitamin K deficiency at one, three and four months of age . The authors mention that Shwachman had observed CF infants with prothrombin deficiency one of whom developed a subdural bleed (Shwachman et al. Pediatrics 1960; 25:155). Also di Sant’Agnese noted vitamin K deficiency leading to occasional bleeding (di Sant’Agnese & Vidaurreta JAMA 1960; 172:2065-72. [PubMed]) and later four infants aged one to four months were reported by Walters TR & Koch F. (Am J Dis Child 1972; 124:641-642.[PubMed]).
1973 Weber A, Roy CC, Morin CL, Lasalle R. Malabsorption of bile acids in children with cystic fibrosis. New Engl J Med 1973; 289:1001. [PubMed]
Total faecal bile acid excretion had been reported to be increased (Leyland C. Arch Dis Child 1970; 45:714). This study of 26 children with CF aged two months to nine years from Prof. Roy’s unit in Montreal confirmed that faecal bile acid levels may reach seven times the normal level.
1973 Allan JD, Mason A, Moss AD. Nutritional supplementation in treatment of cystic fibrosis of the pancreas. Am J Dis Child 1973; 126:2-26. [PubMed]
The definitive publication of the “Allan Diet” of beef serum protein hydrolysate, glucose polymer and medium chain triglyceride. There had been great interest following the first report of this diet improving and maintaining the nutritional state of children with CF (Allan et al, Lancet 1970; i: 785-786. above). More children were surviving for longer but with increasingly severe chest involvement, which drastically increased their energy requirements. As the chest involvement worsened their energy requirement increased, so attempting to maintain a reasonable nutritional state became an increasingly common, difficult and often insoluble problem in the days before more effective pancreatic enzyme preparations became available in the early Eighties. It is not surprising therefore that the Allan diet received considerable attention from CF families (Berry et al, 1975 below; Yassa et al, 1979 below). Had not the new acid resistant pancreatic enzyme preparations (Pancrease and Creon) become available in the late Seventies/early Eighties the diet may have been used more widely.
1973 Rucker RW. Harrison GM. Vitamin B 12 deficiency in cystic fibrosis. N Engl J Med 1973; 289:329. [PubMed]
Some malabsorption of vitamin B12 has been demonstrated in a number of later studies but absorption is much improved when pancreatic extract is added although not in all patients. However, in practice, a deficiency of the vitamin is very rare in CF even though supplements are not usually given (also Deren JJ et al. NEJM 1973; 288:949-950; Gueant JL et al. Pancreas 1990; 5: 559-567).
1975 Elliott RB, Robinson PG. Unusual course in a child with cystic fibrosis treated with fat emulsion. Arch Dis Child 1975; 50:76-78.

Bob Elliot
A child with CF received regular intravenous infusions of soya oil emulsion from the first weeks. The authors state that “Sweat tests improved, pancreatic achylia was relieved and the child at present remains entirely well. Correction of fatty acid found in cystic fibrosis may prevent some of the manifestations of the disease”.
Elliott and colleagues from Auckland, New Zealand published several papers on this subject the first showing improvement in the clinical state with supplements of medium chain triglycerides even to the extent of returning the sweat electrolytes to nearer normal values (Elliott RB. Aust Paediatr J 1972; 8:217; Elliot RB. 1976; 57:474-479). Unfortunately, subsequent studies failed to substantiate their earlier findings (Davidson GP et al. Aust Paediatr J 1978; 14:80-82; Chase et al. Pediatrics 1979; 59:428-432 below)
1975 Berry HK, Kellog FW, Hunt MM, Ingberg RL, Richter L, Gutjahr C. Dietary supplement and nutrition in children with cystic fibrosis. Am J Dis Child 1975; 129:165-171. [PubMed]
Fifteen patients improved over 1 year with the Allan Diet (beef serum hydrolysate, glucose polymer and MCT) with >0.5 SD gain in weight, increase in clinical scores and serum albumin and drop in white blood count. The authors commented that “Changes that occurred following the use of the nutritional supplement are in sharp contrast to our earlier attempts to induce weight gain in patients with CF”. (also Allan et al, 1973 above; Yassa et al, 1979 below).
Nonetheless this depressing weight chart (figure 1) shows the typical weight progress of children with CF at the time showing the inexorable decline from the age of 10 years as the chest infection worsened.
1978 Kraemer R, Rudeberg A, Hadorn B, Rossi E. Relative underweight in cystic fibrosis and its prognostic value. Acta Paediatr Scand 1978; 67:33-37. [PubMed]

Richard Kraemer
This paper from Berne is often quoted as confirming the importance of the nutritional state as an indicator of prognosis. Observations on 117 children with CF from Jan 1956 to June 1976 showed that relative under weight (weight loss corrected for height) is most pronounced when chest is bad and correlates closely with survival.
1979 Yassa JG, Prosser R, Dodge JA. Effects of an artificial diet on growth of patients with cystic fibrosis. Arch Dis Child 1978; 53:777-783. [PubMed]
A controlled trial to test the Allan Diet by Jeanette Yassa working with John Dodge in Cardiff. Twenty eight children were treated but the diet significantly improved the nutritional state of only ten. The authors concluded that “such an unpleasant and expensive diet should be restricted to a few selected cases, rather than given as routine treatment”. Shortly after this paper was published the new acid resistant microsphere pancreatic enzymes (Pancrease and later Creon) were introduced and they totally revolutionised the treatment of malabsorption so much more efficient were they than the older preparations, so most patients no longer needed this type of artificial diet
1979 Chase HP, Long MA, Lavin MH. Cystic fibrosis and malnutrition. J Pediatr 1979; 95:337-347. [PubMed]
One of a number of important detailed nutritional studies of patients with CF around this time showing many patients had an inadequate energy intake even for non-CF individuals. As more children survived to adolescence the maintenance of a reasonable nutritional state and growth rate became increasingly difficult both from the inadequately controlled malabsorption and the progressive chest involvement . In this study the authors comment that the importance of the malnutrition in the disease process remains unknown, as does much information about specific nutritional deficiencies in cystic fibrosis. They advised that supplements for children with CF should include extra energy as fat or carbohydrate, a form of linoleic acid that can be absorbed, hydrolyzed protein, fat-soluble vitamins with vitamins A and E in a water emulsion, vitamin B12, probably B vitamins and vitamin C, and trace minerals. Routine measurements of nutritional status, particularly in children with growth failure, should be made at regular intervals and should include a three-day diet record and a simultaneous 72-hour stool fat determination. If fat malabsorption is not controlled even with pancreatic enzymes, the use of antacids or cimetidine should be considered. (also Hubbard & Magnum, 1982; Parsons et al, 1983)
1979 Bradley JA, Axon AT, Hill GL. Nocturnal elemental diet for retarded growth in a patient with cystic fibrosis. Brit Med J 1979; Jan 20th: 167. [PubMed]
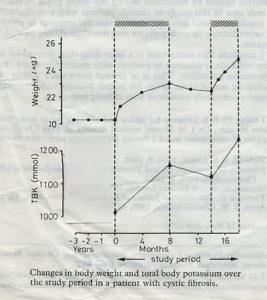
Bradley et al, 1979
The first report of continuous nocturnal nasogastric feeding in a child with CF – interestingly not from a CF centre as this child was referred by her

Tony Axon
general paediatrician to Dr Tony Axon’s adult gastroenterology unit in Leeds. A girl of 13 years with CF used a 8F nasogastric tube for overnight feeding with an elemental diet (Vivonex) infused over 10 hours each night to provide 600 kcal using an infusion pump for eight months then 6 months off then a further 2 months of treatment. There was a 12% increase in body weight in the first six months and overall 20% increase from pre-treatment values (figure).
The authors mention Andrassy RJ et al. (Surgery 1977; 82:205. [PubMed]) as having given continuous elemental diet by catheter to children with a large variety of illnesses and found the method easy to institute and free from side effects.
Intermittent tube feeding was routine practice in premature baby units but not by continuous feeds – suitable infusion pumps were not yet available. The overnight nasogastric feeding methods and then gastrostomy feeding gradually became widely used in the nutritional treatment of people with CF and a number of studies appeared over the next few years (Shepherd et al, 1980 below; Levy et al, 1985 below; Shepherd et al, 1986 below).
1980 Shepherd R, Cooksley WGF, Cooke WD. Improved growth and clinical, nutritional and respiratory changes in response to nutritional therapy in cystic fibrosis. J Pediatr 1980; 7:351-357.[PubMed] One of the early papers by Ross Shepherd of Brisbane on the use of parenteral nutrition in cystic fibrosis. Twelve malnourished children with CF were studied from six months before to six months after a period of supplemental parenteral nutrition. After parenteral nutritional therapy, providing a balanced consistent hyper caloric intake for 21 days, catch-up weight gain occurred by one month and continued at six months; catch-up in linear growth was observed by three months and continued at six months; also there were fewer respiratory infections.Here was further evidence, from Ross Shepherd, of the impressive benefits of this new aggressive nutritional intervention with parenteral feeds. Subsequently there were further studies from Brisbane on nutritional rehabilitation.

Ross Shepherd
1981 Congden PJ, Bruce G, Rothburn MM, Clarke PCN, Littlewood JM, Kelleher J, Losowsky MS. Vitamin status in treated patients with cystic fibrosis. Arch Dis Child 1981; 56:708-714. [PubMed]

Congden et al 1981
This was our first nutritional research study from Seacroft and St James University Hospital, Leeds collaborating with the University Department of Medicine at St James’s. The data was presented at the 1980 Toronto CF Conference. It was the first of many studies on the nutritional and gastrointestinal aspects of CF carried out in collaboration with Dr. Jerry Kelleher and members of Professor Monty Losowsky’s Department of Medicine. This study was coordinated by the late Dr. Peter Congden. Many of our patients, and those of some of our paediatric colleagues who were also included, had unexpectedly low fat-soluble vitamin levels and suboptimal control of intestinal absorption despite what we considered to be adequate enzyme and vitamin supplements; but the water soluble vitamin levels were satisfactory.
The collaboration with Professor Monty Losowsky and members of his department at St James’s University Hospital was crucial to the development of our CF service. This was the first of many studies where we combined to study various aspects of cystic fibrosis.
Monty Losowsky
These disappointing results, reflecting our suboptimal treatment in the late Seventies, prompted us to start annual Comprehensive CF Assessments in May 1980 along the lines suggested by Crozier in 1974; he stated that “success of treatment will depend on a complete assessment of the patient and then continuing attempts to obtain normal bodily function and maintain it”.
Our so-called “Comprehensive CF Assessments” proved so useful in identifying areas where we could improve treatment of our own patients, that in 1981 we offered the service to paediatric colleagues in the Yorkshire Region for their patients. It was through this offer, to accept patients for assessment and advice that the Leeds Regional CF Service developed.
Paul Pencharz
1984 Pencharz P, Hill R, Archibald E, Levy L, Newth C. Energy needs and nutritional rehabilitation in undernourished adolescents and young adult patients with cystic fibrosis. J Pediatr Gastroenterol Nutr 1984; 3 (Suppl 1): S147-S153. [PubMed] The energy needs, nutritional status and body composition of six undernourished adolescents and young adults with CF were shown to be 25-80% higher than in healthy individuals of the same age, sex and size. There was significant wasting of adipose tissue. During the short period of refeeding, body weight, fat and potassium all increased significantly, while fat-free body mass and total body nitrogen did not change.
This was the first report from Toronto documenting increased energy expenditure in people with CF. The increased energy expenditure was related to the severity of the chest infection and the increased requirements were lessened when the chest infection was treated. These facts were confirmed in many subsequent studies (Vaisman et al, J Pediatr 1987; 11:496-500; Buchdahl et al, J Appl Physiol 1988; 64:1810-1816; Bowler et al, Arch Dis Child 1993; 68:754-759 all below).
Professor Paul Pencharz is a gastroenterologist and nutritional expert in the Departments of Nutritional Sciences and Paediatrics in Toronto. He has published widely on the nutritional aspects of CF and many other conditions. This present report was the first to clearly document the increased resting energy expenditure in people with cystic fibrosis.
1984 Reardon MC, Hammond KB, Accurso FJ, Fisher CD, McCabe ER, Cotton EK, Bowman CM. Nutritional deficits exist before 2 months of age in some infants with cystic fibrosis identified by screening test. J Pediatr 1984; 105:271-274. [PubMed]
Keith Hammond
Data on the first 20 infants identified in the Colorado neonatal CF screening programme. Although birth weights were normal, by a mean age of 5.5 weeks nine infants had a weight more than 20 percentile points less than birth although their dietary intake was normal. Albumin and pre-albumin levels were low in thirteen. Eight had elevated alkaline phosphatase levels; five had low cholesterol levels and stool trypsin was undetectable in nine, low in four and normal in three.
The very early onset of nutritional and weight gain problems, even when diagnosed early by neonatal screening, has been observed in a number of series of screened CF infants. Also the catch up growth period may last for the whole of the first year even with expert dietetic support (Wolfe et al, 2005
Kieth Hammond, the biochemist and one of the pioneers of neonatal CF screening, kindly provided the image in his retirement.
1985 Levy LD, Durie PR, Pencharz PB, Corey ML. Effects of long-term nutritional rehabilitation on body composition and clinical status in cystic fibrosis. J Pediatr 1985; 107:225-230.[PubMed]

Peter Durie
One of a number of papers reporting effects of enteral feeding around this time. Fourteen patients aged 4.9 to 21.5 years with CF who had moderate to severe lung disease, malnutrition, or growth failure were given nocturnal supplemental feeding by gastrostomy tube. Mean follow-up was for 1.1 years (range 0.8 to 2.78 years). Patients were studied to observe the effect of nutritional support on body composition, growth, pulmonary function, and quality of life. A contemporary group of patients with CF was retrospectively pair-matched to the study group. The supplemental feeding resulted in positive changes in body composition and in growth velocity. Weight, as a percentage of standard in the control group, declined by 3% over 1 year, whereas it increased by 2% in the treatment group (p< 0.05). Pulmonary function, assessed as a percent of predicted FVC and FEV1, did not change significantly in the treatment group over 1.1 years, whereas FVC declined by 12% (P<0.01) and FEV1 declined by 13% (P<0.01) in the control group (this is rather alarming decline and far greater than one would expect). There was a marked increase in patient ability to participate in activities of daily living, even in those patients in whom pulmonary function deteriorated during the study
1986 Kelleher J, Goode HF, Field HP, Walker BE, Miller MG, Littlewood JM. Essential element nutritional status in cystic fibrosis. Human Nutr: Applied Nutrition 1986; 40A: 79-84.[PubMed]
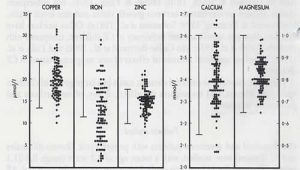
Kelleher et al, 1986
In this present study (figure 5) calcium, magnesium, iron, copper and zinc were measured in 117 patients with CF of wide age range. All the minerals were normal except the iron which was frequently low. There was no evidence that the degree of malabsorption, clinical grading or degree of pulmonary involvement influenced the essential element status as assessed by serum levels.
A later paper recording the iron status of 165 patients with CF attending Leeds for Comprehensive Assessment confirmed that 41 (32%) had low serum ferritin levels although the iron status did not correlated with the clinical features (Ehrhardt P et al. Arch Dis Child 1987; 62:185-187.[PubMed]).
Jerry Kelleher
1988 Buchdahl RM, Cox M, Fulleylove C, Marchant AL, Tomkins AM, Brueton MJ, Warner JO. Increased resting energy expenditure in cystic fibrosis. J Appl Physiol 1988; 64:1810-1816. [PubMed]

Roger Buchdahl
Roger Buchdahl at the Brompton Hospital measured resting energy expenditure (REE) by indirect calorimetry in 23 subjects with CF in a stable clinical state and in 42 normal control subjects. In subjects with CF the REE was found to be elevated by an average of 9.2% above expected values derived from the control subjects. There were significant correlations between increased values and poor pulmonary function. However; the correlations were low, suggesting that other factors may contribute to the increased resting energy expenditure, possibly including the putative metabolic defect in cystic fibrosis.
This study provided confirmation of previous original observations from Toronto (Pencharz et al, J Pediatr Gastroenterol Nutr 1984; Suppl 1:S147-53 above; Vaisman et al, J Pediatr 1987; 111:496-500. [PubMed]) that most children with CF have increased resting energy expenditure which appears to be related to and correlated with the severity of the chest infection. Also CF infants have some 25% greater energy expenditure than controls (Shepherd RW, et al. Lancet 1988; i: 1300-1303. [PubMed]; also Bowler et al, 1993 below).
1988 Corey M, McLaughlin FJ, Williams M, Levison H. A comparison of survival growth and pulmonary function in patients with cystic fibrosis in Boston and Toronto. J Clin Epidemiol 1988; 41:588-591. [PubMed]

Mary Corey
A classic and oft-quoted study comparing survival curves between 1972-1981 of 499 Boston patients and 534 Toronto patients (figure 6). The Toronto patients were taller and heavier than the Boston patients but had similar respiratory function. Median age of survival in Boston was 21 years and in Toronto 30 years with divergence occurring from the age of 10 years.
The authors concluded “The differences in growth and survival in these two patient groups, with very similar age specific pulmonary function, suggest further examination of nutritional guidance and intervention in CF especially regarding the traditional restriction of dietary fat”.
Douglas Crozier in Toronto had recommended a normal or high fat intake with very large doses of Cotazym since the early Seventies, at a time when many clinicians advised a fat-restricted diet (Crozier, 1974 above).
1988 MacDonald A, Kelleher J, Littlewood JM. A normal fat diet for cystic fibrosis: is a dietitian still needed? Scand J Gastroenterol 1988; 23 (Suppl 143):157-159. [PubMed]

Anita MacDonald
In this paper the dietary intakes of 90 people with CF who came to Leeds for Comprehensive Assessment; they had received various degrees of dietetic support at their local hospitals. They were assessed by a 7-day dietary history. Patients who had contact with a dietitian at least twice a year achieved higher energy and protein intakes than patients with little or no dietetic help. Patients who had one intensive interview with a specialist CF dietitian but had little local dietetic support attained better nutrient intakes than patients with no dietetic support. At that time dietary misconceptions, which still led to restriction of fat and even sugar, were still relatively common in the UK particularly when patients or parents of children with CF received little dietary advice. Only 8% of patients receiving no dietary advice achieved energy intakes of more than 120% of the recommended daily allowance compared with 50% of those seeing a dietitian – the difference being largely related to the fat intake. So it seemed a dietitian was still needed!
Anita MacDonald, at the time of this study was the senior dietitian at the Leeds Paediatric CF Centre, reported experience with patients referred to Leeds for our so-called Comprehensive Assessment. Anita made a major and quite exceptional contribution to the nutritional management of children with CF attending the Leeds centre and to the development of the regional CF service. Eventually she became Chief Dietitian at the Birmingham Children’s Hospital but left a legacy of expertise which was continued and further built on Sue Wolfe and Alison Morton our two present chief dietitians. Anita flourished at Birmingham Children’s Hospital where she became Professor and was awarded the OBE.
1989 Rayner RJ, Tyrell JC, Hiller EJ, Marenah C, Neugebauer MA, Vernon SA, Brimlow G. Night blindness and conjunctival xerosis due to vitamin A deficiency in cystic fibrosis. Arch Dis Child 1989; 64:1151-1156. [PubMed]

Joan Hiller
Rosie Rayner, then the CF Research Fellow at Nottingham and now paediatrician in Wolverhampton, studied 43 patients with CF aged 8 to 44 years (median 16 years), for evidence of vitamin A deficiency. Eight had abnormal dark adaptation tests and three had conjunctival xerosis. Serum vitamin A and retinol binding protein concentrations were significantly lower in the affected patients who were also more likely to have abnormal liver function tests. Five patients were treated with 100,000-200,000 IU water miscible vitamin A orally and their daily vitamin supplements were increased to maintain normal concentrations. In four patients dark adaptation tests were repeated. Three were normal, but one patient required three further doses of water miscible vitamin A and a daily supplement of 12,000 IU vitamin A before her dark adaptation threshold returned to normal. Adolescents with cystic fibrosis are liable to develop night blindness and conjunctival xerosis, particularly if they have liver disease or fail to take daily vitamin supplements.
One of the papers reporting objective evidence of the clinical effects vitamin deficiency rather than merely reduced plasma levels. Obviously very important if adults with CF, of which there were increasing numbers, were driving at night. Histological evidence of vitamin A deficiency was evident in many of the early post-mortem studies – in fact, for some time it was regarded by Dorothy Andersen as a major factor in the pathogenesis of the condition.
1989 Hill S, Phillips A, Mearns M, Walker-Smith JA. Cows’ milk sensitive enteropathy in cystic fibrosis. Arch Dis Child 1989; 64:1251-1255. [PubMed]

John Walker-Smith
Over 12 years, proximal small intestinal mucosal biopsies were carried out in children with CF who had diarrhoea and failed to thrive in spite of adequate treatment, including pancreatic supplements. Histological examination of eight of the 17 biopsies taken over a period of 12 years from children with CF showed evidence of enteropathy, and accounted for one in 13 (8%) children with cystic fibrosis under 3 years of age attending Margaret Mearns’s CF clinic. Seven children clearly responded to a cows’ milk free diet; the diarrhoea stopped and weight gain increased. One of these responded only when gluten was also excluded from his diet. The eighth child remained on a normal diet and his symptoms did not improve. The enteropathy had resolved in all five patients who had further biopsies taken while receiving treatment, and from 15 months to 3 years of age all the children tolerated a normal diet and continued to thrive.
Cows’ milk sensitive enteropathy is an important cause of failure to thrive in a minority of children with cystic fibrosis – usually not revealed by allergy tests such as IgE or RAST. Small intestinal biopsy is an important investigation in younger children with CF who fail to thrive and have diarrhoea despite adequate treatment for they may have cow’s milk intolerance or even coeliac disease.
1989 Choonara IA, Winn MJ, Park BK, Littlewood JM. Plasma vitamin K1 concentrations in cystic fibrosis. Arch Dis Child 1989; 64:732-734. [PubMed]
One of the first studies on vitamin K from the Leeds CF centre when Prof. Choonara worked there. Plasma concentrations in 37 patients mean age 10.6 years (2-23yrs) median 46ng/l and 16 controls 49ng/l. No relation found between an increase in prothrombin time and vitamin K plasma concentration.
However, subsequent studies using more efficient tests showed vitamin K was deficient in many patients and possibly related to later osteoporosis (Conway et al, 2005 below).
1989 Sokol RJ. Reardon MC. Accurso FJ. Stall C. Narkewicz M. Abman SH. Hammond KB. Fat-soluble-vitamin status during the first year of life in infants with cystic fibrosis identified by screening of newborns. Am J Clin Nutr 1989; 50:1064-1071. [PubMed]

Ronald Sokol
Another report on infants diagnosed in the Colorado neonatal screening programme. Fat-soluble vitamin status during the first year of life in 36 infants with CF was examined; biochemical evidence of fat-soluble-vitamin deficiency is common before the age 3 months in CF infants.
A further report on these 36 infants (Sokol RJ, et al. Pediatr Pulmonol 1991; Suppl 7:52-55) after treatment with pancreatic enzymes, a multiple vitamin preparation, and additional vitamin E was associated with normalization of serum albumin, retinol, and 25-hydroxyvitamin D and negative PIVKA testing (for vitamin K) at six and 12 months of age. Several patients remained vitamin E deficient, but this was felt to be due to poor adherence to the treatment.
These studies from Denver of some of the earlier screened CF infants were important as they drew attention to the very early onset of nutritional deficiencies in the infants. Biochemical evidence of fat-soluble vitamin deficiency is common before three months of age and responds to adequate supplementation in the first year of life. Also the initial fall off in weight gain may take many months to recover.
1993 Phillips RJ, Crock CM, Dillon MJ, Clayton PT, Curran A, Harper JI. Cystic fibrosis presenting as kwashiorkor with florid skin rash. Arch Dis Child 1993; 69:446-448. [PubMed]
Two infants with a florid erythematous rash and generalised oedema, hypoalbuminaemia, and anaemia were found to have cystic fibrosis. This rare presentation is associated with false negative sweat tests, delays in diagnosis, and a considerable mortality. The authors suggested that this presentation represents a manifestation of kwashiorkor secondary to intestinal malabsorption.
1993 Bowler IM, Green JH, Wolfe SP, Littlewood JM. Resting energy expenditure and substrate oxidation rates in cystic fibrosis. Arch Dis Child 1993; 68:754-759. [PubMed]

Ian Bowler during the study
The resting energy expenditure (REE) and substrate oxidation rates in 16 patients with CF who had mild chest disease and 11 healthy controls were measured using indirect calorimetry. The mean REE (% predicted) in the patients with CF was 11% greater than in the controls. Five patients with CF were hypermetabolic but only one of these had a clinically significant reduction of respiratory function. A greater proportion of REE was derived from carbohydrate oxidation in the CF patients (43.5% v 29.9%). However, the 24 hour dietary intake of carbohydrate was greater in the cystic fibrosis group (49.6 v 45.8% of energy intake).
These data suggest that a high dietary intake of carbohydrate may contribute to the increased oxidation of carbohydrate in these CF patients.
1994 Wilfond BS, Farrell PM, Laxova A, Mischler E. Severe hemolytic anemia associated with vitamin E deficiency in infants with cystic fibrosis. Implications for neonatal screening. Clin Pediatr 1994; 33:2-7. [PubMed]

Philip Farrell
Three infants with CF and malnutrition leading to severe anemia beginning as early as six weeks of age. They had high reticulocyte counts, negative Coombs’ tests, abnormal peroxide haemolysis test results, and biochemical evidence of vitamin E deficiency. Oral administration of alpha-tocopherol resulted in rapid correction of the laboratory abnormalities.
Phillip Farrell has published extensively on vitamin E deficiency both in premature infants and those with CF (see Farrell et al, J Clin Invest 1977; 60:233-241 above). This report emphasises the early onset of fat soluble vitamin deficiencies in infants with CF as also found in the Colorado screened infants (Sokol et al, 1991 above).
1995 Ghosal S, Taylor CJ, Pickering M, McGraw J, Beckles-Wilson, Wales JKH. Disproportionate head

Shamik Ghosal
growth retardation in cystic fibrosis. Arch Dis Child 1995; 72:150-152.[PubMed]
Fifty children with CF (18 diagnosed with meconium ileus, four by post natal screening, 30 by clinical diagnosis) were followed over four years. The length SD scores improved from -1.24 at birth to -0.15 at four years and the weight SD scores from -1.37 at 6 months to -0.53 at four years. In contrast the head circumference SD score reached a plateau of -1.0 from the age of 1.5 to four years and remained significantly low throughout the four years of measurement being -1.05 at four years. (also Lloyd-Still JD et al, Pediatrics 1974; 54:306-311 – “malnutrition in infancy can affect intellectual development in the first five years”).
This was the first report that the head circumference of children with CF may be slightly smaller than expected. The high proportion of infants with meconium ileus (34%) in the series probably was due to Sheffield Children’s Hospital being a regional centre for neonatal surgery. The authors suggested that the data may support the expression of CFTR in the choroid plexus and ependyma. There is very little in the literature on head circumference in CF although in the Wisconsin screening data on cognitive score index (CSI) – “the highest proportion of CSI scores >84 occurred in the control <300E group (41%). Patients in this group also had the lowest mean head circumference z-scores at diagnosis” (Koscik RL et al. J Pediatr 2005; 147(3 Suppl):S51-6). A further study of screened CF infants from Sheffield confirmed that head growth appeared to lag behind somatic growth supporting the functional expression of CFTR in the brain (Ghosal S et al. Arch Dis Child 1996; 75:191-193. [PubMed]).
1995 Morkeberg JC, Edmund C, Prause JU, Lanng S, Koch C, Michaelsen KF. Ocular findings in cystic fibrosis patients receiving vitamin A supplementation. Graefe’s Arch Clin Exp Ophthalmol 1995; 233:709-713. [PubMed]
Only 26% of 35 patients examined in the Copenhagen clinic had normal vitamin A status as measured by serum retinol and light sensitivity but reduced contrast sensitivity. Conjunctival imprints showed dry eye in 42%; decreased tear stability in 49% and other abnormalities of low tear production (31%) and increased numbers of dying cells (23%). In fact 26% were considered to have the criteria for “keratoconjunctivitis sica”. The authors even suggested that the high incidence of dry eye could be a primary manifestation of CF.
These findings are more likely the result of suboptimal vitamin A status particularly as only 26% had normal vitamin A levels. In studies where vitamin A status is regularly monitored to maintain normal serum levels, only reduced contrast sensitivity is found (Ansari et al. 1999 below) and the cause of this is unexplained.
1999 Ansari EA, Sahni K, Etherington C, Morton A, Conway SP, Moya E, Littlewood JM. Ocular signs and symptoms and vitamin A status in patients with cystic fibrosis treated with daily vitamin A supplements. Br J Ophthalmol 1999; 83:688-691.[PubMed]
Since the first Leeds studies on vitamin levels in 1978 (Congden et al, 1981 above), oral supplementation has been guided by annual monitoring of vitamin levels; also all patients are seen regularly by a CF specialist dietitian and most have a comprehensive annual dietary assessment. None of the 28 patients in this study had vitamin A deficiency, the median value of serum retinol being 48 microg/dl, range 31-80 microg/dl (normal range 30-80 microg/dl). Dark adaptation was normal in all patients compared with the control group where the mean value was 3.4 log units of threshold luminance (95% confidence interval 2.4-4.0). None of the test group had a value of threshold luminance 2 SD above the mean value for the control group. Eight patients had reduced contrast sensitivity. The median value for serum zinc was 14.2 micromol/ l, range 13-81 micromol/l (normal range 8-23 micromol/l) and the median value for retinol binding protein was 36 mg/l, range 13-81 mg/l (normal range 35-58 mg/l). There was no correlation between dark adaptation and serum retinol, zinc, or retinol binding protein. Two patients had clinical evidence of dry eye.
So regular estimates of plasma vitamin A, together with appropriate supplementation and expert dietetic review, can maintain normal dark adaptation in patients with cystic fibrosis. The occurrence of reduced contrast sensitivity function is well documented in CF and confirmed in this study but remains an unexplained phenomenon (also Morkeberg et al, 1995 above).
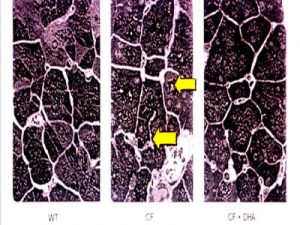
1999 Freedman SD Katz MH, Parker EM, Laposata M, Urman MY, Alvarez JG. A membrane lipid imbalance plays a role in the phenotypic expression of cystic fibrosis in cftr-/-mice. PNAS 1999; 96:13995-14000. [PubMed]
A deficiency in essential fatty acid metabolism has been reported previously in plasma from patients with cystic fibrosis. The objective of this present study was to determine whether alterations in fatty acid metabolism were specific to CF-regulated organs and whether they played a role in the expression of disease. A membrane lipid imbalance was found in ileum, pancreas, and lung from cftr(-/-) mice characterized by an increase in phospholipid-bound arachidonic acid and a decrease in phospholipid-bound docosahexaenoic acid (DHA). This lipid imbalance was observed in organs pathologically affected by CF including lung, pancreas, and ileum and was not secondary to impaired intestinal absorption or hepatic biosynthesis of DHA. As proof of concept, oral administration of DHA to cftr (-/-) mice corrected this lipid imbalance and reversed the observed pathological manifestations in the pancreas. The authors considered these results strongly suggest that certain phenotypic manifestations of CF may result from remediable alterations in phospholipid-bound arachidonic acid and DHA levels (figure 7).
This paper, caused considerable interest in medical circles and in the media at the 1999 CF Conference in Seattle, as Dr Freedman of the Beth Israel Deaconess Medical Centre Boston, suggested that essential fatty acid imbalance, affected the phenotypic expression of the CF defect and hence implied that the CF phenotype could be modified by correction of the imbalance. This latest revival in interest in essential fatty acids was made possible by the availability of CF mice and the opportunity to examine their pancreatic tissue.
Unfortunately subsequent studies by this group failed to confirm the fundamental importance of these findings (Beharry et al, 2007 below) but did suggest that DHA therapy may release endogenous inhibitors of inflammation (below) although it is fair to say that the initial enthusiasm has waned (Freedman SD et al, 2004; Beharry et al, 2007 both described out of chronological order for convenience below).
[next two references are out of sequence as they relate to above article]
2004 Freedman SD, Blanco PG, Zaman MM, Shea JC, Ollero M, Hopper IK, Weed DA, Gelrud A, Regan MM, Laposata M, Alvarez JG, O’Sullivan BP. Association of cystic fibrosis with abnormalities in fatty acid metabolism. N Eng J Med 2004; 350:560-569. [PubMed]
Freedman et al, 2004
The authors previously demonstrated that arachidonic acid levels are increased and docosahexaenoic acid levels are decreased in affected tissues from cystic fibrosis-knockout mice (Freedman et al, 1999 above). In this present study of fatty acids from nasal- and rectal-biopsy specimens, nasal epithelial scrapings, and plasma were analyzed from 38 subjects with CF and compared with results in 13 obligate heterozygotes, 24 healthy controls, 11 subjects with inflammatory bowel disease, 9 subjects with upper respiratory tract infection, and 16 subjects with asthma. The ratio of arachidonic to docosahexaenoic acid was increased in mucosal and submucosal nasal-biopsy specimens (P<0.001) and rectal-biopsy specimens (P=0.009) from subjects with CF compared with the healthy control subjects. In nasal tissue, this change reflected an increase in arachidonic acid levels and a decrease in docosahexaenoic acid levels. In cells from nasal mucosa, the ratio of arachidonic to docosahexaenoic acid was increased in subjects with cystic fibrosis (P<0.001), as compared with healthy controls, with values in obligate heterozygotes intermediate between these two groups (P<0.001). The authors concluded that these data indicated that alterations in fatty acids similar to those in cystic fibrosis-knockout mice are present in CFTR-expressing tissue from subjects with cystic fibrosis.
– Despite considerable published work, up to 2008, EFA therapy has not been established as beneficial in people with CF; nor has this work had a major impact on the understanding of or treatment of cystic fibrosis as was hoped when first reported in 1999.
2007 Beharry S, Ackerley C, Corey M, Kent G, Heng YM, Christensen H, Luk C, Yantiss RK, Nasser IA, Zaman M, Freedman SD, Durie PR. Long-term docosahexaenoic acid therapy in a congenic murine model of cystic fibrosis. Am J Physiol – Gastr L 2007; 292:G839-48. [PubMed]
A congenic C57Bl/6J cystic fibrosis transmembrane conductance regulator (Cftr)(-/-) mouse model, which develops cystic fibrosis (CF)-like pathology in all organs, was used to evaluate the short- and long-term therapeutic effects of dietary docosahexaenoic acid (DHA). Thirty-day-old Cftr (-/-) mice and wild-type littermates were randomized to receive a liquid diet with or without DHA (40 mg/day). Animals were killed for histological and lipid analysis after 7, 30, and 60 days of therapy. DHA had no significant therapeutic or harmful effect on the lung, pancreas, or ileum of the Cftr (-/-) mice or their wild-type littermates. In contrast, dietary DHA resulted in highly significant amelioration of the severity of liver disease in the Cftr (-/-) mice, primarily a reduction in the degree of peri-portal inflammation. The authors concluded that inhibition of cytokines and/or eicosanoid metabolism and release of endogenous inhibitors of inflammation by the DHA may account for the anti-inflammatory effects in the liver of this congenic murine model of CF. The potential therapeutic benefits of DHA in severe CF-associated liver disease remain to be explored.
So the EFA story continues and although dietary DHA supplements had no effect on many organs of the Cftr (-/-) mouse including the pancreas as had been suggested in 1999, there was considerably less hepatic inflammation in the treated mice.
2000 Marchand V, Baker SS, Stark TJ, Baker RD. Randomized, double-blind, placebo-controlled pilot trial of megestrol acetate in malnourished children with cystic fibrosis. J Pediatr Gastroenterol Nutr 2000; 31:264-269. [PubMed]
Megestrol, an appetite stimulant, caused increased weight gain in the 6 of the 12 children with CF who completed the trial. Three withdrew for unrelated reasons and three developed diabetes.
So megestrol acetate appeared to improve appetite but the side effects were a problem including adrenal suppression, glucose intolerance and diabetes.
2000 Krebs NF, Westcott JE, Arnold TD, Kluger BM, Accurso FJ, Miller LV, Hambidge KM. Abnormalities in zinc homeostasis in young infants with cystic fibrosis. Pediatr Res 2000; 48:256-261. [PubMed]
Low plasma zinc concentrations have been reported in approximately 30% of young infants with CF identified by newborn screening. This study examined zinc homeostasis in this population by application of stable isotope methodology. Faecal zinc losses correlated with faecal fat excretion, suggesting interference with the normal conservation of endogenously secreted zinc suggesting impaired zinc homeostasis and suggest an explanation for the reported suboptimal zinc status in many young infants with CF prior to diagnosis and treatment.
The results of many studies on zinc status are conflicting. In 1986 the late Jerry Kelleher reported the zinc status of 117 children with CF in Leeds and found their levels, except for two children, to be quite normal (Kelleher J et al. Hum Nutr-Appl Nutr 1986;40A:79-84). In a later study Ansari et al.1999 (above) in a study of vitamin A also found the zinc levels were normal in Leeds patients.
2000 Keevil B, Rowlands D, Burton I, Webb AK. Assessment of iron status in cystic fibrosis patients. Ann Clin Biochem 2000; 37:662-665. [PubMed]
The use of soluble transferrin receptor (sTfR), together with more traditional measurements such as iron, transferrin and ferritin, were used to assess iron status in 70 adult CF patients. Sixty nine percent of subjects as determined by transferrin saturation had iron deficiency, but only 29% as determined by sTfR and only 11% as determined by ferritin. There was a significant correlation between C-reactive protein (CRP) and both ferritin and transferrin saturation. In addition, because the CRP concentration was elevated in 64% of subjects, it may be that the transferrin saturation was overestimating, and the ferritin underestimating, iron deficiency in these patients. The sTfR concentration, on the other hand, is unaffected by the acute-phase response and was therefore thought to be the most useful test for detecting iron deficiency in this group of patients.
There is an extensive literature on iron in cystic fibrosis dating back to the early Sixties since Davis and Badenoch reported increased iron absorption in pancreatitis (Lancet 1962; 2:6), a finding confirmed in children with CF (Smith RS. BMJ 1964; 1:608-609. [PubMed]). Subsequently a number of studies found low iron status in people with CF including those in Leeds where 41 (32%) of 165 patients had low ferritin levels (Ehrhardt P et al. Arch Dis Child 1987; 62:185-187. [PubMed]). More recently Fischer R et al (Pediatr Pulmonol 2007; 42:1193-1197[PubMed]) found no benefit from iron supplementation and concluded that chronic inflammation was the main cause of the low iron status. This seems to be the most likely explanation although it seems the matter is still unresolved.
2002 Proesmans M, De Boeck K. Evaluation of dietary fiber intake in Belgian children with cystic fibrosis: is there a link with gastrointestinal complaints?. J Pediatr Gastr Nutr 35(5):610-4, 2002 [PubMed]

Marijke Proesmans
A low fiber intake is suspected to be an underlying factor in gastrointestinal complaints of people with CF. In this study the overall fiber intake was adequate in the cystic fibrosis population. There was no relation between low fiber intake and gastrointestinal problems in the patients with cystic fibrosis.
2002 Sinaasappel M, Stern M, Littlewood J, Wolfe S, Steinkamp G, Heijerman H, Robberecht E, Döring G.

Marten Sinassappel
Nutrition in patients with cystic fibrosis: a European Consensus. J Cyst Fibros 2002; 1:51-75. 15463811
The outcome of a European CF Society Consensus Group at Artimino, Italy in March 2001 involving 33 experts on nutrition in patients with cystic fibrosis. The contents give an idea of the current nutritional management of people with CF. The full text is available on the European CF Society website (www.ecfsoc.org). Although now somewhat dated there are useful references.
2004 Parker EM. O’Sullivan BP. Shea JC. Regan MM. Freedman SD. Survey of breast-feeding practices and outcomes in the cystic fibrosis population. Pediatr Pulmonol 2004; 37:362-367. [PubMed]
Three thousand, two hundred questionnaires were sent to 30 accredited CF centers for anonymous completion. Eight hundred and sixty-three questionnaires were returned. Fifty-three percent of those who breast-fed exclusively > or = 6 months had FEV1% values > 90%, compared to 47% of those not breast-fed. This is a suggestive but not statistically significant difference. In conclusion, breast-feeding for > or = 6 months is associated with decreased use of intravenous antibiotics in the 2 years prior to administering the questionnaire.
This survey indicates that breast-feeding is not harmful to children with CF, and may be beneficial.
2006 Poustie VJ, Russell JE, Watling RM, Ashby D, Smyth RL. CALICO Trial Collaborative Group. Oral protein energy supplements for children with cystic fibrosis: CALICO multicentre randomised controlled trial. BMJ 2006; 332(7542):632-636. [PubMed]

Venessa Poustie
In 102 children with cystic fibrosis, aged between 2 and 15 years, who were moderately malnourished, the effects of oral protein energy supplements in addition to their usual dietary advice were compared with dietary advice alone, for 12 months. The authors concluded that the long term use of oral protein energy supplements did not result in a significantly better improvement in nutritional status or other clinical features and so oral protein energy supplements should not be regarded as an essential part of the management of children with CF.
This multi centre trial was supported by the UK CF Trust. At the time over 50% of children with CF in the UK were taking regular (expensive) proprietary dietary supplements with only sparse evidence of their efficacy. Although this trial showed that dietary advice to increase the intake of normal food was of equivalent value, the supplements were still widely used as one way of dealing with the eating problems so common in small children with CF and in improving energy intake in adults (White et al, J Cyst Fibros 2004; 3:1-7. [PubMed]). So the outcome of the trial appeared to have only minimal effect on reducing the use of the supplements.
2007 Wiedemann B, Paul KD, Stern M, Wagner TO, Hirche TO. German CFQA Group. Evaluation of body mass index percentiles for assessment of malnutrition in children with cystic fibrosis. Eur J Clin Nutr 2007; 61:759-768. [PubMed].
To compare the performance of recently released body mass index percentiles (BMIp) with standard anthropometric indexes, including height-for-age percentile (HAP), weight-for-age percentile (WAP) and percent ideal body weight (%IBW), as measures for nutritional failure in children with cystic fibrosis (CF). Cross-sectional analysis of growth and lung function data from 4577 children with CF reported to the German CF quality assurance (CFQA) project from 1995 to 2004 were used. . BMIp predicts nutritional failure more sensitively and accurately than conventional anthropometric indexes, at least in children with CF. Consequently, less CF children were identified with nutritional failure according to %IBW method (male 20.5%; female 22.7%) compared with BMIp method (male 30.4%; female 28.7%). The clinical relevance of these findings was confirmed by stronger correlation of BMIp with impaired %forced expiratory volume/s, a marker for disease progression in CF. Screening of CF patients by BMIp could provide an early warning sign and allow for timely therapeutic intervention.
This is a useful paper confirming the increased sensitivity of the BMIp with the previously used anthropomorphic values for children with CF
Khalid S, McGrowder D, Kemp M, Johnson P. The use of soluble transferrin receptor to assess iron deficiency in adults with cystic fibrosis. Clin Chim Acta 2007; 378:194-200. [PubMed].
Iron deficiency (ID) is common in cystic fibrosis (CF) and the soluble transferrin receptor (sTfR) is a sensitive, quantitative measurement of tissue iron deficiency. The study investigated the use of sTfR together with serum iron, transferrin saturation (TS) and serum ferritin, in assessing iron status in adult CF patients. The patient population consisted of 127 CF patients which consisted of 51 inpatients with infected exacerbation (IE) and 76 outpatients at the time of their annual review (AR). Serum sTfR was measured using a particle-enhanced immunoturbidimetric assay on the Beckman Coulter LX20. RESULTS: Sixty five percent (65%) of CF patients in the IE group and 28% in the AR group had ID as determined by TS, but only 18% (IE group) and 20% (AR group) as determined by ferritin. Serum sTfR detected 20% in the IE group and 12% in the AR group. We found significant correlation between C-reactive protein and TS (r=-0.56; P<0.01) but not with ferritin (r=0.22; P=0.380) in the IE group. The authors concluded that iron status of patients with CF can be accurately assessed by sTfR which is unaffected by the acute phase response and can be used in conjunction with serum ferritin.
Studies on iron and CF have appeared regularly since the 1960s and would continue to appear after this article! (Gifford A H et al. [PubMed]). The general view is that iron deficiency is common in CF and correlates with lung function and general health.
2007 Bruzzese E, Raia V, Spagnuolo MI, Volpicelli M, De Marco G, Maiuri L, Guarino A. Effect of Lactobacillus GG supplementation on pulmonary exacerbations in patients with cystic fibrosis. Clinical Nutrition 2007; 26:322-328. [PubMed]
Nineteen children with CF received a probiotic Lactobacillus GG (LGG) for 6 months and then changed to a placebo of oral rehydration solution (ORS) for 6 months; in parallel nineteen received ORS and then changed to LGG. Patients treated with LGG showed a reduction of pulmonary exacerbations (Median 1 vs. 2) and of hospital admissions (Median 0 vs. 1, range 3 vs. 2,). LGG resulted in a greater increase in FEV1 (3.6% +/- 5.2 vs. 0.9% +/- 5; p=0.02) and body weight (1.5 kg +/- 1.8 vs. 0.7 kg +/- 1.8; p=0.02). The authors concluded that Lactobacillus GG reduces pulmonary exacerbations and hospital admissions in patients with CF, that probiotics may delay respiratory impairment and that a relationship exists between intestinal and pulmonary inflammation.
There is an increasing interest on the part of patients, parents and doctors in the role probiotics in treating people with CF (Borowitz D et al, J Pediatr Gastroenterol Nutr 2005; 41:273-285. [PubMed]); however, as yet, few CF clinics advise their routine use – perhaps because the evidence of their value is still sparse but also there are so many other components to treatment that there is reluctance to add yet another medicine to gain a marginal benefit.
2009 Coates AJ, Crofton PM, Marshall T. Evaluation of salt supplementation in CF infants. J Cyst Fibros 2009; 8:382-385. [PubMed]
Alan Coates
CF infants may be at increased risk of sodium depletion which may lead to impaired growth. The objective of this study was to evaluate their sodium supplementation requirements. Ten CF infants had serial measurements of weight and plasma/urine sodium and creatinine. Sodium supplementation was adjusted with the aim of maintaining fractional excretion (FENa) between 0.5% and 1.5% and urinary sodium > 10 mmol/L. The urine sodium:creatinine (UNa:Cr) ratio strongly correlated with FENa [UNa:Cr (mmol/mmol)=35.0 x FENa (r=0.99)]. The FENa target range corresponded to UNa:Cr 17-52 mmol/mmol. All infants required sodium supplementation to achieve UNa:Cr > 17 mmol/mmol. Sodium supplement requirements (mean+/-SD) at ages 0-3, 3-6, 6-9 and 9-12 months were 1.9+/-0.5, 1.8+/-0.8, 1.9+/-0.9 and 0.8+/-0.4 mmol/kg/d. No infant required calorie supplementation to achieve expected weight gain. The authors concluded that using current UK CF Trust and European CFS guidelines many cases of sodium depletion may be overlooked. Some infants require more than the recommended 1-2 mmol/kg/d. The UNa:Cr ratio is a useful non-invasive measure to monitor sodium supplementation.
This is a particularly useful paper as most infants are diagnosed after neonatal screening and the advice in the UK and European CF Society consensus documents suggested that routine sodium supplementation was unnecessary.
2009 Switzer M, Rice J, Rice M, Hardin DS. Insulin-like growth factor-I levels predict weight, height and protein catabolism in children and adolescents with cystic fibrosis. J Pediatr Endocrinol 2009; 22:417-424. [PubMed]

Dana Hardin
There was also a strong relationship between leucine rate of appearance (a measure of protein catabolism) and IGF-I. These results suggest a strong correlation between IGF-I and height, weight and protein catabolism and emphasize the need to normalize IGF-I levels in children with cystic fibrosis.
Hardin has written a number of papers on the use of growth hormone. Here they analyse the IGF-1 levels in the patients studied previously studied. It is interesting that in recent animal studies involving CF pigs there seems to be a relationship between IGF-1 and the growth potential of the animals (Rogan MP et al. 2010.[PubMed]).
2011 Haupt ME, Kim EE, Prestridge AL. Successful prolonged use of recombinant human insulin-like growth factor-1 in a child with cystic fibrosis. Pediatr Pulmonol 2011; 46:1137-41. [PubMed]
These authors report the successful prolonged use of recombinant human insulin-like growth factor-1 in an adolescent boy with CF, who demonstrated significant clinical benefits from the therapy.
Growth failure is a common and complicated process in children with cystic fibrosis. Growth hormone, which is becoming a more commonly used agent in such patients, has demonstrated beneficial effects aside from increased growth velocity. Recently, insulin-like growth factor-1 has gained significant attention in the understanding of growth failure in children with CF. This present report is the first of its use in a child with CF
2012 Stalvey MS, Anbar RD, Konstan MW, Jacobs JR, Bakker B, Lippe B, Geller DE. A multi-center controlled trial of growth hormone treatment in children with cystic fibrosis. Pediatr Pulmonol 2012; 47:252-263. [PubMed]

Michael Stalvey
A multicenter, open-label, controlled clinical trial comparing outcomes in prepubertal children <14 years with CF, randomized in a 1:1 ratio to receive daily rhGH (Nutropin AQ) or no treatment (control) for 12 months, followed by a 6-month observation (month 18). Sixty-eight subjects were randomized (control 32 and rhGH 36). Changes in glucose tolerance for the two groups were similar over the 12-month study period, with three subjects developing IGT and one CFRD in each group. One rhGH-treated patient developed increased intracranial pressure. The treatment with rhGH in prepubertal children with CF was effective in promoting growth, weight, LBM, lung volume, and lung flows, and had an acceptable safety profile.
Another study on the use of human growth hormone for which there is now ample evidence for effect – but whether clinicians will use it and whether children will object to the daily injections over a long period of treatment is not clear. Previous studies have come to similar conclusions.
2012 Smith C, Winn A, Seddon P, Ranganathan S. A fat lot of good: balance and trends in fat intake in children with cystic fibrosis. J Cyst Fibros 2012; 11:154-157. [PubMed]
The fundamental nutritional treatment of a high fat diet for cystic fibrosis (CF) is established and essentially unchanged in the last 25 years. However, recent concerns have emerged regarding the potential risks of such a diet. The authors investigated the diets of children with CF to determine the source of energy, energy imbalance, and changing trends of fat intake. Macronutrient intakes did not change significantly in our population of CF children, but there was a consistent imbalance of fat-sources with over-dependence on saturated fats which, in the context of increased survival in CF may potentially increase risk of cardiovascular disease. The authors suggested that further studies are needed to confirm their findings, investigate consequences of fat imbalance and guide clearer advice regarding appropriate proportions of sources of fat for CF patients.
There is increasing interest in the long term effects of various treatment in people with CF and this is becoming more relevant as the length of survival increases. It was many years ago that autopsy studies showed the arteries of people with CF were relatively free of atheroma and this was attributed to the impaired fat absorption. Controls had 4 times the amount of atheroma than people with CF (Holman RL, Blanc WA, Andersen D. Decreased aortic atherosclerosis in cystic fibrosis of the pancreas. Pediatrics 1959; 24:34-39. [PubMed]
2011 Jadin SA, Wu GS, Zhang Z, Shoff SM, Tippets BM, Farrell PM, Miller T, Rock MJ, Levy H, Lai HJ. Growth and pulmonary outcomes during the first 2yr of life of breast fed and formula-fed infants diagnosed with cystic fibrosis through the Wisconsin Routine Newborn Screening Program. Am J Clin Nutr 2011; 93:1038-47. [PubMed]
The optimal feeding (breast milk, formula, or a combination) for infants with cystic fibrosis (CF) is unknown. Recommendations from the CF Foundation are based on limited data. The authors compared growth and pulmonary outcomes between breast-fed and formula-fed infants through the age of 2 yrs. A total of 103 CF infants born in 1994-2006 and diagnosed through newborn screening in Wisconsin were studied. Breast fed infants were classified by the duration of exclusive breast feeding (ExBF). Exclusive formula-feeding (ExFM) was classified by the formula’s caloric density (i.e., standard [0.67 kcal/mL (20 kcal/oz) (ExFM20)] throughout infancy or high density [>=0.74 kcal/mL (22 kcal/oz) (ExFM22+)] for some duration of infancy). RESULTS: Fifty-three infants (51% of infants) were breast fed and 50 infants (49% of infants) were ExFM. In breast fed infants, the duration of ExBF was <1 mo (53% of infants), 1-1.9 mo (21% of infants), 2-3 mo (17% of infants), and 4-9 mo (9% of infants). In ExFM infants, 23 infants (46%) received a formula with a high caloric density; approximately half (n = 13) of the ExFM infants received the formula by 6 mo of age. Proportionately more infants with pancreatic sufficiency (n = 9) were ExBF >=1 mo (44% of infants), and none of the infants were ExFM22+, compared with infants with meconium ileus (n = 24; 13% of infants were ExBF >=1 mo, and 38% of infants were ExFM22+) or pancreatic insufficiency (n = 70; 25% of infants were ExBF >=1 mo, and 20% of infants were ExFM22+) (P = 0.02). In infants with pancreatic insufficiency, weight z scores declined from birth to 6 mo (P < 0.0001) in infants who were ExBF >=2 mo, and the number of Pseudomonas aeruginosa infections through the age of 2 y was fewer in breast fed than in ExFM infants (P = 0.003) but did not differ by the duration of ExBF.
The authors concluded that for infants with CF, exclusive breast feeding for less than 2 months does not compromise growth and is associated with a respiratory benefit.
Early nutrition of CF infants is obviously very important and this paper contains useful information. One striking feature of screened CF infants is the degree of weight loss in the first few weeks before treatment is started and the time required to regain a reasonable nutritional state. It had been suggested that exclusive breast feeding did not provide suffcient energy to support maximal growth.
Our own experience of feeding screened CF infants in Leeds did suggested that exclusive breast feeding is adequate for some CF infants (Wolfe et al J Cyst Fibros 2005; 4(S1):S94).See entry of Reardon et al 1984 above for figure of weights of Leeds screened infants. Obviously an individual approach is required supervised by an experienced dietitian.
2013 Yen EH, Quinton H, Borowitz D. Better nutritional status in early childhood is associated with improved clinical outcomes and survival in patients with cystic fibrosis. J Pediatr 2013; 162:530-535. [PubMed]
To evaluate the relationship between nutritional status early in life and the timing and velocity of height growth, lung function, complications of cystic fibrosis, and survival using data from the Cystic Fibrosis Foundation Registry (US) for patients born between 1989 and 1992 (n=3142). For the population studied, greater weight at age 4 years is associated with greater height, better pulmonary function, fewer complications of cystic fibrosis, and better survival through age 18 years. Furthermore, greater weight-for-age in the peripubertal period is associated on average with improved tempo and timing of pubertal height growth.
This data confirms, yet again, the now well established observation that improved survival correlates with a better nutritional state, first clearly shown by Richard Kraemer and colleagues in 1978 (above) [PubMed]
2015 Schall JI, Mascarenhas MR, Maqbool A, Dougherty KA, Elci O, Wang DJ, Altes TA, Hommel KA, Shaw W, Moore J, Stallings VA. Choline Supplementation with a Structured Lipid in Children with Cystic Fibrosis: A Randomized Placebo-Controlled Trial. J Pediatr Gastroenterol Nutr. 2015 Oct 9. [Epub ahead of print][PubMed]
Choline depletion is seen in cystic fibrosis (CF) and pancreatic insufficiency (PI) in spite of enzyme treatment and may result in liver, fatty acid and muscle abnormalities. This study evaluated the efficacy and safety of an easily absorbed choline-rich structured lipid (LYM-X-SORB [LXS]) to improve choline status.
Children with CF and PI were randomised to LXS or placebo in a 12-month double blind trial. 110 subjects were enrolled (age 10.4 ± 3.0 years). LXS had improved choline intake, plasma choline status and muscle choline stores, compared with placebo. The choline-rich supplement was safe, accepted by participants and improved choline status in children with CF.
– The metabolism and significance of choline in CF and other conditions has been reviewed recently (Hollebeck CB. Cent Nerv Syst Agents Med Cham 2012; 12(2):100-13. [PubMed]). In the present study there is no mention that there was any change in the clinical condition commensurate with the improved choline status.
2015 Morton A; Wolfe S. Enteral tube feeding for cystic fibrosis. Cochrane Database of Systematic Reviews. 4:CD001198, 2015. [PubMed]

Alison Morton & Sue Wolfe
The authors identified 38 trials; however, they considered none were eligible for inclusion in this review. Reported use of enteral tube feeding suggests that it does result in nutritional and respiratory improvement; but, the efficacy has not been fully assessed by randomised controlled trials. They do acknowledge, however, that performing a randomised controlled trial would be difficult due to the ethics of withholding an intervention in a group of patients whose nutritional status necessitates it
– This review by two very experienced Leeds dietitians, Sue Wolfe and Alison Morton, notes that, although there are no controlled trials, reports do support the use of enteral tube feeding. Fortunately the authors do not make the frequent closing plea of many Systematic Reviewers for more controlled trials! They consider a controlled trial of enteral feeding would be unethical – so, quite correctly, clinical judgment of the professional carers, and discussion with the patient/parents, should determine who requires and who receives this nutritional treatment.
2016 Sarah Collins (Chair), Joanne Barrett, Caroline Elston, Alison Morton, Ruth Watling, Sue Wolfe.(Section Leads). Nutritional Management of Cystic Fibrosis. Second Edition, September 2016. Nutrition Working Group of the Cystic Fibrosis Trust. Full document available on the CF Trust website (www,cystic fibrosis .org.uk)

Sarah Collins
A detailed up to date account of nutritional management published by the UK CF Trust. Written by UK experts of great experience in this field, the document contains almost 400 references. The document updates the CF Trust’s previous 2002 guidelines. It represents what the current Nutrition Consensus Working Group and those who have contributed to the document consider to be the best clinical practice. The document has been reviewed by relevant experts in addition to peer review.
Sarah Collins (figure) is specialist CF Dietitian at Kings College London.
Forrester DL, Knox AJ, Smyth AR, Barr HL, Simms R, Pacey SJ, Pavord ID, Honeybourne D, Dewar J, Clayton A, Fogarty AW. Glutamine supplementation in cystic fibrosis: A randomized placebo-controlled trial. Pediatr Pulmonol. 2016 Mar;51(3):253-7. doi: 10.1002/ppul.23370. Epub 2015 Dec 27. [PubMed] A study to test the hypothesis that oral glutamine supplementation (21 g/day) for 8 weeks in adults with cystic fibrosis would decrease pulmonary inflammation and improve clinical status.There was no effect of glutamine supplementation on markers of pulmonary inflammation in the intention-to-treat analysis.
Konstan MW, Pasta DJ, Wagener JS, VanDevanter DR, Morgan WJ. BMI fails to identify poor nutritional status in stunted children with CF. J Cyst Fibros. 2016 Dec 1. pii: S1569-1993(16)30663-4. doi: 10.1016/j.jcf.2016.11.005. [PubMed]
Body mass index (BMI) is currently emphasized for evaluating nutritional status in children with cystic fibrosis (CF). Weight for age (WFA) and height for age (HFA) may get less attention. Data from the Epidemiologic Study of Cystic Fibrosis were used to compare patient WFA, HFA, and BMI percentiles for children age 2 to 18years.
For children with BMI between the 25th and 50th percentiles, 16.8% had WFA <10th percentile and 26.6% had HFA <10th percentile.
So the BMI fails to identify a substantial proportion of children with CF who have stunting or potentially poor nutritional status as measured by WFA and/or HFA.
2016 Turck D; Braegger CP; Colombo C; Declercq D; Morton A; Pancheva R; Robberecht E; Stern M; Strandvik B; Wolfe S; Schneider SM; Wilschanski M. ESPEN-ESPGHAN-ECFS guidelines on nutrition care for infants, children, and adults with cystic fibrosis. Clin Nutr 2016; 35(3):557-77. [Full text from Clinical Nutrition website] [PubMed]
ESPEN, ESPGHAN and ECFS recommended guidelines to cover nutritional management of patients with CF. The guidelines were developed by an international multidisciplinary working group in accordance with officially accepted standards. The GRADE system was used for determining grades of evidence and strength of recommendation. Statements were discussed, submitted to Delphi rounds, reviewed by ESPGHAN and ECFS and accepted in an online survey among ESPEN members.
The Working Group recommends that initiation of nutritional management should begin as early as possible after diagnosis, with subsequent regular follow up and patient/family education. Exclusive breast feeding is recommended but if not possible a regular formula is to be used. Energy intake should be adapted to achieve normal weight and height for age. When indicated, pancreatic enzyme and fat-soluble vitamin treatment should be introduced early and monitored regularly. Pancreatic sufficient patients should have an annual assessment including fecal pancreatic elastase measurement. Sodium supplementation is recommended and a urinary sodium:creatinine ratio should be measured, corresponding to the fractional excretion of sodium. If iron deficiency is suspected, the underlying inflammation should be addressed. Glucose tolerance testing should be introduced at 10 years of age. Bone mineral density examination should be performed from age 8-10 years. Oral nutritional supplements followed by polymeric enteral tube feeding are recommended when growth or nutritional status is impaired. Zinc supplementation may be considered according to the clinical situation. Further studies are required before essential fatty acids, anti-osteoporotic agents, growth hormone, appetite stimulants and probiotics can be recommended.Nutritional care and support should be an integral part of management of CF. Obtaining a normal growth pattern in children and maintaining an adequate nutritional status in adults are major goals of multidisciplinary CF centers.
– An authoritative 30-page document outlining the present recommended nutritional management for people with cystic fibrosis.
Usatin D, Yen EH, McDonald C, Asfour F, Pohl J, Robson J. Differences between WHO AND CDC early growth measurements in the assessment of Cystic Fibrosis clinical outcomes. J Cyst Fibros. 2016 Dec 15. pii: S1569-1993(16)30670-1. doi: 10.1016/j.jcf.2016.12.001. [PubMed]
Adulthood CF outcomes based on early weight-for-length (WFL) measurements, using either World Health Organization (WHO) or Centers for Disease Control (CDC) scales, have not been compared. Cystic Fibrosis Foundation registry patients were studied (n=3014). Participants were categorised at age two years as WFL <50th percentile on both WHO and CDC scales, ≥50th percentile on WHO but not CDC, or ≥50th percentile on both. Pulmonary function and overall survival were assessed at age 18years. Results: Stepwise gains in pulmonary function and lung transplant-free survival were noted across the three increasing WFL categories. Children with CF who achieve higher WFL at age two years have improved pulmonary and survival outcomes into adulthood. The authors advise CF providers to continue to utilize current early growth recommendations, with goal WFL ≥50th percentile on CDC growth charts before age two. Data from article -<50th WHO >50th WHO >50th WHO and CDC not CDC and CDCFEV1%86.3 (77.8-89.4) 87(80.9-95.4) 89.7(85-95.4)Transplant-free survival 83.8% 88.7% 92.3%
– An interesting study from the CFF Patient Registry confirming the importance of early progress on later outlook.
Konstan MW, Pasta DJ, Wagener JS, VanDevanter DR, Morgan WJ. BMI fails to identify poor nutritional status in stunted children with CF. J Cyst Fibros. 2017 Jan;16(1):158-160. doi: 10.1016/j.jcf.2016.11.005.[Pubmed] Body mass index (BMI) is currently emphasised for evaluating nutritional status in children with cystic fibrosis (CF). Weight for age (WFA) and height for age (HFA) may get less attention. Data from the Epidemiologic Study of Cystic Fibrosis were used to compare patient WFA, HFA, and BMI percentiles for children age 2 to 18years. For children with BMI between the 25th and 50th percentiles, 16.8% had WFA <10th percentile and 26.6% had HFA <10th percentile.
The authors concluded the BMI fails to identify a substantial proportion of children with CF who have stunting or potentially poor nutritional status as measured by WFA and/or HFA.
– It is good the authors have re-emphasised the well-known limitations of the BMI as a measure of nutritional status in children.
Smyth RL; Rayner O. Oral calorie supplements for cystic fibrosis. [Review][Update of Cochrane Database Syst Rev. 2014 Nov 03;(11):CD000406; PMID: 25363148] Cochrane Database of Systematic Reviews. 5:CD000406, 2017 05 04.[Pubmed] The authors of this Cochrane review concluded that oral calorie supplements do not confer any additional benefit in the nutritional management of moderately malnourished children with cystic fibrosis over and above the use of dietary advice and monitoring alone. While nutritional supplements may be used, they should not be regarded as essential. They suggest further randomised controlled trials are needed to establish the role of short-term oral protein energy supplements in people with cystic fibrosis and acute weight loss and also for the long-term nutritional management of adults with cystic fibrosis or advanced lung disease, or both.
– Professor Ros Smyth was a co-author in the original CALICO trial in 2006 where the conclusion was “Long term use of oral protein energy supplements did not result in an improvement in nutritional status or other clinical outcomes in children with cystic fibrosis who were moderately malnourished. Oral protein energy supplements should not be regarded as an essential part of the management of this group of children”.At that time over 50% of children with CF in the UK were taking regular (expensive) proprietary dietary supplements with only sparse evidence of their efficacy. The original trial showed that dietary advice to increase the intake of normal food was of equivalent value, the supplements were still widely used as one way of dealing with the eating problems so common in small children with CF and in improving energy intake in adults (see original comment in 2006 section of this History – Poustie V J et al, 2006)
Stalvey MS, Pace J, Niknian M, Higgins MN, Tarn V, Davis J, Heltshe SL, Rowe SM. Growth in Prepubertal Children With Cystic Fibrosis Treated With Ivacaftor. Pediatrics 2017 Feb;139(2). pii: e20162522. doi:10.1542/peds.2016-2522.[Pubmed]
The authors hypothesised that targeting the biological defect in the CF transmembrane conductance regulator (CFTR) protein may affect growth outcomes. In this post hoc analysis, the authors assessed linear growth and weight in 83 children (aged 6-11 years) enrolled in 2 clinical trials, the longitudinal-observation GOAL study and the placebo-controlled ENVISION study, to evaluate the effects of ivacaftor, a CFTR potentiator. They calculated height and weight z scores and height and weight growth velocities (GVs).
In ivacaftor-treated children in GOAL, height and weight z scores increased significantly from baseline to 6 months (increases of 0.1 [P < .05] and 0.26 [P < .0001], respectively); height GV increased significantly from 3 to 6 months (2.10-cm/year increase; P < .01). In ivacaftor-treated children in ENVISION, height and weight z scores increased significantly from baseline to 48 weeks (increases of 0.17 [P < .001] and 0.35 [P < .001], respectively). Height and weight GVs from baseline to 48 weeks were also significantly higher with ivacaftor than with placebo (differences of 1.08 cm/year [P < .05] and 3.11 kg/year [P < .001], respectively).
The authors suggest Ivacaftor treatment in prepubescent children may help to address short stature and altered GV in children with CF; results from these analyses support the existence of an intrinsic defect in the growth of children with CF that may be ameliorated by CFTR modulation.
– It is difficult to say whether this favourable effect is on “an intrinsic defect in growth of children with CF” or a beneficial effect ivacaftor has on factors such as infection, respiratory function, intestinal absorption, and insulin production.
Usatin D, Yen EH, McDonald C, Asfour F, Pohl J, Robson J. Differences between WHO AND CDC early growth measurements in the assessment of Cystic Fibrosis clinical outcomes. J Cyst Fibros. 2017 Jul;16(4):503-509. doi: 10.1016/j.jcf.2016.12.001. Epub 2016 Dec 15. [Pubmed]
Early childhood growth status has been used to predict long-term clinical outcomes in CF patients. Adulthood CF outcomes based on early weight-for-length (WFL) measurements, using either World Health Organisation (WHO) or Centers for Disease Control (CDC) scales, have not been compared.
Cystic Fibrosis Foundation registry patients were studied (n=3014). Participants were categorised at age two years as WFL <50th percentile on both WHO and CDC scales, ≥50th percentile on WHO but not CDC, or ≥50th percentile on both. Pulmonary function and overall survival were assessed at age 18years. Stepwise gains in pulmonary function and lung transplant-free survival were noted across the three increasing WFL categories.
The authors concluded children with CF who achieve higher weight for length (WFL) at age two years have improved pulmonary and survival outcomes into adulthood. CF providers should continue to utilise current early growth recommendations, with goal WFL ≥50th percentile on CDC growth charts before age two.
– This long-term study is interesting and valuable even though the result was to be expected. In the past the long-term effect of various new interventions was unknown although predicted. For example, it was not until 2001 that the positive long-term favourable effect on growth following diagnosis by neonatal screening was established by Phillip Farrell’s group (Farrell PM et al, Pediatrics 2001; 107:1-13).
Dr. Danielle Usatin a paediatric gastroenterologist in San Francisco
2017 Woestenenk JW, Gulmans VA, van der Ent CK, Houwen RH. Height Assessment in the Dutch-Origin Pediatric Cystic Fibrosis Population. Nutr Clin Pract. 2017 Feb;32(1):130-132. doi: 10.1177/0884533616639109. Epub 2016 Jul 10. [Pubmed
Height evaluation is an integral part of cystic fibrosis care. Height is compared with reference values by converting it to height-for-age (HFA) z scores. However, HFA z scores do not adjust for genetic potential (ie, target height [TH]), which could result in an incorrect estimation of the height. To evaluate the magnitude of this potential problem, the authors assessed the agreement between HFA and HFA-adjusted-for-TH (HFA/TH) z scores in 474 Dutch children with CF.
In this study sample, HFA z scores were -0.07 (95% confidence interval, -0.02 to -0.12) lower than HFA/TH z scores. When HFA and HFA/TH z scores were subdivided into 4 categories (≥0, <0 and ≥-1, <-1 and ≥-2, and ≤-2), a moderate agreement was found. HFA z scores were classified lower than HFA/TH z scores in 21% of the measurements and higher in 15% of the measurements.
– The authors concluded in clinical routine, height evaluation based on height-for-age may result in underestimation or overestimation of height growth, which may induce inappropriate nutrition interventions. Seems there is still a place for clinical judgment of the state of nutrition!
Quon BS, Sykes J, Stanojevic S, Marshall BC, Petren K, Ostrenga J, Fink A, Elbert A, Faro A, Goss CH, Stephenson AL.Clinical characteristics of cystic fibrosis patients prior to lung transplantation: An international comparison between Canada and the United States.Clin Transplant. 2018 Jan 2. doi: 10.1111/ctr.13188. [Epub ahead of print] [Pubmed]

Bradley Quon
Between 1986 and 2013, 607 (10.2%) CF patients underwent lung transplantation in Canada and 3428 (7.5%) in the United States. A lower proportion of recipients had growth of B. cepacia complex prior to transplant in the United States compared to Canada (0.8% vs 4.3%). Lung function was similar between recipients from the two countries. The proportion of patients classified as underweight was significantly higher in the United States compared to Canada (39.8% vs 28.0%; SD 26.1) despite higher rates of feeding tube use (42.5% vs 28.6%; SD 29.0).
CF lung transplant recipients from the United States have similar lung function, lower rates of B. cepacia complex, and worse nutritional parameters prior to transplant compared to counterparts in Canada. Future studies are necessary to evaluate the impact of these differences on post-transplant survival.
Dr. Bradley S Quon is Assistant Professor in the Department of Medicine University of British Columbia. He is a Staff Respirologist and CF Physician at St. Paul’s Hospital in Vancouver
– Presumably the better nutrition and higher B. cepacia rates are a reflection of the patients’ previous experience – the Canadians being better nourished for decades from the time of Douglas Crozier in the Seventies but more likely to have B. cepacia which became a common pathogen in Toronto patients from the Eighties.
Munck A, Boulkedid R, Weiss L, Foucaud P, Wizla-Derambure N, Reix P, Bremont F, Derelle J, Schroedt J, Alberti C; Gastroenterology and Nutrition Société française de la Mucoviscidose (SFM) Working Group and the ALIMUDE Study Group. Nutritional Status the First Two Years of Life in Cystic Fibrosis Diagnosed by Newborn Screening. J Pediatr Gastroenterol Nutr. 2018 Mar 14. doi: 10.1097/MPG.0000000000001956. [Epub ahead of print][Pubmed]

Anne MunckA
A prospective longitudinal multi-centre study assessing nutritional status according to pancreatic status, feeding modalities, prescriptions, pulmonary outcome and biological nutritional parameters.
One-hundred-and-five infants were recruited and 99 completed the study. Nutritional care management prevented under nutrition and stunting in those with exocrine pancreatic sufficiency (EPS), but affected (13/87) 15% and (21/86) 24%, respectively, of infants with exocrine pancreatic insufficiency (EPI). The logistic regression model found a positive association between both weight and length z-scores “at risk” at month 24, and initial pulmonary symptoms (OR 0.06, p < 0.01 and OR 0.08, p < 0.01, respectively); these symptoms were less frequent when age at first visit was earlier than 1.2 months (33% versus 67%, p = 0.02); stunting was also associated with high-calorie density intake and Staphylococcus aureus (OR: 0.05, p = 0.01 and OR: 0.17, p < 0.01). Pulmonary outcome did not differ according to pancreatic status; breast-feeding for at least 3 months delayed first acquisition of Pseudomonas aeruginosa. Despite sodium and fat-soluble vitamin supplementation, half of both cohorts had low urinary sodium output and half of the EPI cohort had low vitamin D levels.
The authors’ data shed light on the fact that stunting was more frequent than undernutrition, while both parameters involved only patients with pancreatic insufficiency. Modalities of feeding were not associated with nutritional status; breast-feeding may provide some protection against acquisition of Pseudomonas aeruginosa.
– Presumably the significant proportion of infants who are stunted is a manifestation of the intrinsic growth problem reported in a number of previous publications.
Stallings VA, Sainath N, Oberle M, Bertolaso C, Schall JI. Energy Balance and Mechanisms of Weight Gain with Ivacaftor Treatment of Cystic FibrosisGating Mutations. J Pediatr. 2018 Oct;201:229-237.e4. doi: 10.1016/j.jpeds.2018.05.018. Epub 2018 Jul 18. [Pubmed]

Virginia Stallings
A study to determine if ivacaftor treatment results in weight gain and improved pulmonary function in people with cystic fibrosis transmembrane conductance regulator gating mutations. Children and adults with cystic fibrosis and at least 1 cystic fibrosis transmembrane conductance regulator gating mutation were evaluated in this observational study before and after 3 months of ivacaftor treatment. Body size and composition, total energy expenditure, resting energy expenditure (REE%) as percent predicted, coefficient of fat absorption (CFA%), fecal calprotectin, fecal elastase, and quality of life were assessed. Some outcomes were explored by pancreatic status.
There were 23 patients (5-61 years of age) who completed the study; 70% had pancreatic insufficiency (PI). Patients gained 2.5 ± 2.2 kg (P < .001) with increased (P < .05) fat-free mass (0.9 ± 1.9 kg) and fat mass (1.6 ± 1.5 kg). REE% decreased by 5.5 ± 12.0% (P < .05), fecal calprotectin decreased by 30 ± 40 µg/g stool (P < .01), and total energy expenditure was unchanged. Improvements were greater for PI than patients who were pancreatic-sufficient. CFA% increased significantly only with PI. The change (Δ) in weight was positively correlated with the percent change in forced expiratory volume at 1 second (r = 0.46; P = .028) and ΔCFA% (r = 0.47; P = .032) and negatively with ΔREE% (r = -0.50; P = .017). Together, ΔREE%, ΔCFA%, and the percent change in forced expiratory volume at 1 second explained 58% of the variance in weight gain (adjusted R2 = 0.579; P = .0007). Growth status and muscle strength improved, as did quality of life in several domains. Fecal elastase increased in most patients with pancreatic sufficiency, with no change in those with PI.
The authors’ identified mechanisms for ivacaftor-associated weight gain were decreased resting energy expenditure, gut inflammation, and fat malabsorption.
Dr Virginia A Stallings is a nutrition paediatrician and Jean A. Cortner Endowed Chair in the Division of Gastroenterology, Hepatology and Nutrition at Children’s Hospital of Philadelphia. She is the Research Director in the Nutrition Center.
Van Biervliet S, Declercq D, Somerset S.Clinical effects of probiotics in cystic fibrosis patients: A systematic review. Clin Nutr ESPEN. 2017 Apr;18:37-43. doi: 10.1016/j.clnesp.2017.01.007. Epub 2017 Feb 22. [Pubmed]
This study investigated the current evidence for probiotics as an adjunct to usual therapy for CF. Electronic clinical databases were interrogated for human randomised, controlled, intervention trials (1985-2015) testing the effects of probiotics on clinical endpoints in CF were reviewed. From 191 articles identified in initial searches, six studies met the critical inclusion criteria, and were reviewed in detail. These studies varied in size (n = 22 to 61) but were generally small and showed substantial diversity in protocol, specific probiotic species used and range of clinical outcomes measured. Probiotic administration showed beneficial effects on fecal calprotectin levels, pulmonary exacerbation risk, and quality of life indicators. In one study, such changes were associated with variations in gut microbiota composition.
Despite encouraging preliminary results, the limited number of small and highly varied studies to date do not justify the addition of probiotics as an adjunct to current CF treatment protocols. Importantly, very minimal adverse effects of probiotics have been reported
Sutherland R, Katz T, Liu V, Quintano J, Brunner R, Tong CW, Collins CE, Ooi CY. Dietary intake of energy-dense, nutrient-poor and nutrient-dense food sources in children with cystic fibrosis. J Cyst Fibros. 2018 Nov;17(6):804-810. doi: 10.1016/j.jcf.2018.03.011. Epub 2018 May 1. Free article. [Pubmed]
This interesting and timely study confirms that the energy- and fat-dense CF diet is primarily achieved by overconsumption of energy -dense nutrition-poor foods, rather than nutrient dense sources. The authors suggest this dietary pattern may not be optimal for the future health of children with CF, who are now expected to survive well into adulthood.
Rosie Sutherland is at the Discipline of Paediatrics, School of Women’s and Children’s Health, University of New South Wales, Sydney, NSW 2052, Australia.
Van Biervliet S, Hauser B, Verhulst S, Stepman H, DelangheJ, Warzee JP, Pot B, Vandewiele T, Wilschanski M.Probiotics in cystic fibrosis patients: A double blind crossover placebo controlled study: Pilot study from the ESPGHAN Working Group on Pancreas/CF. Clin Nutr ESPEN. 2018 Oct;27:59-65. doi: 10.1016/j.clnesp.2018.06.008. Epub 2018 Jul 20 [Pubmed]

Stephanie Van Biervliet
A potential positive effect of probiotics in cystic fibrosis (CF) on fecal calprotectin (FCP), pulmonary exacerbations and weight has been described in small controlled trials. A double-blind multicenter cross-over study (2 × 4 m) was performed looking at abdominal pain, nutritional status, pulmonary function, pulmonary exacerbation, FCP and lactulose/mannitol gut permeability test. Patients kept a diary with daily scoring of abdominal pain, stool frequency and consistency as well as treatment changes.
31 CF patients entered the study of which 25 finished it. At start patients aged 9.3yrs (6.9-12.2), had a median BMI z-score of -0.5 (-1.5-0.08), height z-score of -0.4 (-1.1-0.05) and FEV1% of 100% (87.2-106.6). Median FCP at start was 61 μg/g (17-108) and gut permeability 0.079 (0.051-0.122). No significant changes were observed in the clinical parameters (BMI, FEV1%, abdominal pain, exacerbations). Despite being frequently abnormal (17/28 (61%) >50 mg/kg), FCP did not change significantly with probiotics. The proportion of patients with normal permeability was 8% during placebo and 32% during probiotic treatment (p = 0.031). FCP correlated to BMI z-score (p = 0.043) and gut permeability to abdominal pain (p = 0.015). The microbiome revealed a high predominance of Actinobacteria and Proteobacteriae. Probiotic supplementation did not result in a shift at the phylum nor at phylogenetic level.
The authors concluded that normalization of gut permeability was observed in 13% of patients during probiotic treatment. However, none of the previously described effects on fecal calprotectin (FCP), pulmonary exacerbations and weight, which have been described in previous small controlled trials, could be confirmed.
Prof.dr.Stephanie Van Biervliet works in the Department of Paediatrics and Medical Genetics Ghent University Hospital and is coordinator of the CF centre
2018 Sagel SD, Khan U, Jain R, Graff G, Daines CL, Dunitz JM, Borowitz D, Orenstein DM, Abdulhamid I, Noe J, Clancy JP, Slovis B, Rock MJ, McCoy KS, Strausbaugh S, Livingston FR, Papas KA, Shaffer ML. Effects of an Antioxidant-enriched Multivitamin in Cystic Fibrosis. A Randomized, Controlled, Multicenter Clinical Trial. Am J Respir Crit Care Med. 2018 Sep 1;198(5):639-647. doi: 10.1164/rccm.201801-0105OC. [Pubmed]
Scott Segal
A study to evaluate the effects of an oral antioxidant-enriched multivitamin supplement on antioxidant concentrations, markers of inflammation and oxidative stress, and clinical outcomes. In this investigator-initiated, multicenter, randomized, double-blind, controlled trial, 73 pancreatic-insufficient subjects with CF 10 years of age and older with an FEV1 between 40% and 100% predicted were randomized to 16 weeks of an antioxidant-enriched multivitamin or control multivitamin without antioxidant enrichment. Endpoints included systemic antioxidant concentrations, markers of inflammation and oxidative stress, clinical outcomes (pulmonary exacerbations, anthropometric measures, pulmonary function), safety, and tolerability.
[The antioxidant enriched vitamin supplement(AquADEKs-2) – contains standard amounts of fat-soluble vitamins (A, D, E, K) that are contained in typical CF multivitamin supplements plus several antioxidants including beta-carotene, mixed tocopherols (different forms of vitamin E), coenzyme Q10 (CoQ10), mixed carotenoids (lutein, lycopene and zeaxanthin), and the minerals zinc and selenium.
Dietary Supplement: control multivitamin – The control multivitamin contains standard (standard for CF multivitamin supplements) amounts of vitamins A, B, D, E, and K without added antioxidants].
Change in sputum myeloperoxidase concentration over 16 weeks, the primary efficacy endpoint, was not significantly different between the treated and control groups. Systemic antioxidant (β-carotene, coenzyme Q10, γ-tocopherol, and lutein) concentrations significantly increased in the antioxidant-treated group (P < 0.001 for each), whereas circulating calprotectin and myeloperoxidase decreased in the treated group compared with the control group at Week 4. The treated group had a lower risk of first pulmonary exacerbation requiring antibiotics than the control group (adjusted hazard ratio, 0.50; P = 0.04). Lung function and growth endpoints did not differ between groups. Adverse events and tolerability were similar between groups.
The authors concluded antioxidant supplementation was safe and well tolerated, resulting in increased systemic antioxidant concentrations and modest reductions in systemic inflammation after 4 weeks. Antioxidant treatment was also associated with a lower risk of first pulmonary exacerbation.
Dr Scott D Segal Department of Pediatrics, Children’s Hospital Colorado, University of Colorado School of Medicine, Aurora, Colorado. He is President and Co-founder of Segal’s Trials
Altman K, McDonald CM, Michel SH, Maguiness K. Nutrition in cystic fibrosis: From the past to the present and into the future. Pediatr Pulmonol. 2019 Nov;54 Suppl 3:S56-S73. doi: 10.1002/ppul.24521. [Pubmed]

Kimberly Altman
Nutritional management is an integral part of multidisciplinary care for persons with cystic fibrosis. This review will look at how nutrition care has evolved over time. In addition, they will look at how some newer therapies impact nutrition care.
– This is a long, detailed and very interesting account of nutritional management in CF. In the summary the authors note there has been a shift from focus on the pulmonary components of CF care to an emphasis on diet and nutrition aspects of care. This may be so in recent years and in adult units (where emphasis on the chest was the rule), however in the early years after Dorothy Andersen described CF in 1938, when there were no adults, CF was considered by Andersen to be primarily a nutritional disorder with other organ involvement such as the chest as secondary to the nutritional problems. It is worth remembering that Dr Douglas Crozier of Toronto led the way in abandoning the traditional low fat diet in the Seventies and was ultimately responsible for the superior Canadian results reported by Mary Corey in 1988 (Corey et al, J Clin Epidemiol 1988; 41:588-591).
Kimberly Altman is a Cystic Fibrosis Dietitian at the Gunnar Esiason Adult Cystic Fibrosis and Lung Center, New York Presbyterian/Columbia University Medical Center, New York. Her co-authors are from Salt Lake City, South Carolina and Indiana.
Harindhanavudhi T, Wang Q, Dunitz J, Moran A, Moheet A. revalence and factors associated with overweight and obesity in adults with cystic fibrosis: A single-center analysis. J Cyst Fibros. 2019 Nov 11. pii: S1569-1993(19)30922-1. doi: 10.1016/j.jcf.2019.10.004. [Epub ahead of print] [Pubmed]

Tasma
Harindhanaudhi
The relation between malnutrition and pulmonary death in patients with cystic fibrosis (CF) has resulted in intensive nutritional intervention over the last few decades, leading to a significant decline in underweight and the emergence of overweight/obesity as a potential new problem. The authors performed a cross-sectional database analysis of 484 adults with CF seen at the University of Minnesota CF Center between January 2015-January 2017, to determine the prevalence and pulmonary/cardiovascular risk factors associated with overweight and obesity in this population.
Mean age was 35.2 ± 11.6 years. 5.2% were underweight (BMI<18.5 kg/m2), 62.6% normal weight (BMI ≥ 18.5-24.9 kg/m2), 25.6% overweight (BMI ≥ 25-29.9 kg/m2) and 6.6% obese (BMI ≥ 30 kg/m2). In the subgroup with severe genotypes, 25% had BMI ≥ 25 kg/m2. In the entire cohort, overweight/obese were likely to be older (OR = 1.04, p < 0.0001) and to have a mild CFTR genotype (OR = 3.33, p = 0.0003) and modestly elevated triglyceride levels (OR = 1.008, p < 0.0001). The prevalence of hypertension was higher in overweight (25%) and obese (31%) than normal (17%) or underweight (16%), p = 0.01. Total cholesterol levels were higher in overweight/obese versus normal/underweight (144-147 vs 123-131 mg/dL, p = 0.04) as were LDL levels (70-71 vs 53-60 mg/dL, p = 0.02), but all were within the normal range. Percent predicted FEV1 was higher in overweight/obese (78-81%) versus underweight (59%) and normal (70%), p < 0.0001, and overweight/obese experienced significantly fewer acute pulmonary exacerbations.
The authors concluded that overweight/obesity is common in adults with CF including those with severe genotypes. Lung function is better in the overweight/obese and lipid levels are within the normal range, albeit higher than in normal/underweight.
Dr Tasma Harindhanavudhi is an endocrinologist in the Division of Diabetes and Endocrinology, Department of Medicine, University of Minnesota, Minneapolis,
Bonhoure A, Boudreau V, Litvin M, Colomba J, Bergeron C, Mailhot M4, Tremblay F, Lavoie A, Rabasa-Lhoret R. Overweight, obesity and significant weight gain in adult patients with cystic fibrosis association with lung function and cardiometabolic risk factors. Clin Nutr. 2020 Jan 10. pii: S0261-5614(20)30005-4. doi: 10.1016/j.clnu.2019.12.029. [Epub ahead of print] [Pubmed]

Anne Bonhoure
Given therapy improvements, some CF patients are now overweight, obese or present rapid weight gain. However, the impact of being overweight on clinical outcomes (e.g. FEV1 & metabolic complications) remains unknown.
Baseline data from 290 adult CF patients and observational follow-up (3.5 years; n = 158) were collected. BMI categories: underweight (UW < 18.5 kg/m2), normal (NW 18.5-26.9 kg/m2), and overweight/obese (OW ≥ 27 kg/m2). Follow-up data (weight change over time): weight loss (WL>10%), stable (WS), and weight gain (WG>10%). BMI categories and follow-up data were compared to FEV1 and cardiometabolic parameters: glucose tolerance, estimated insulin resistance (IR), blood pressure (BP), and lipid profile.
For BMI categories, 35 patients (12.1%) were UW, 235 (81.0%) NW, and 20 (6.9%) OW. Compared to UW and NW patients, OW patients are older (p < 0.001), had less pancreatic insufficiency (p = 0.009), a higher systolic BP (p = 0.004), higher LDL (p < 0.001), and higher IR (p < 0.001). Compared to UW patients, OW patients had a better FEV1 (p < 0.001). For weight change, WL was observed in 7 patients (4.4%), WS in 134 (84.8%) and WG in 17 patients (10.8%). Compared to WL and WS patients, WG patients had a 5% increase in FEV1 accompanied by higher IR (p = 0.017) and triglycerides (p < 0.001). No differences were observed for glucose tolerance for neither BMI nor weight change.
The authors concluded a higher weight or weight gain over time are associated with a better FEV1 but also some unfavourable cardio-metabolic trends.
Dr A Bonhoure is at the Institut de Recherches Cliniques de Montréal (IRCM), Montréal, Canada; McGill University, Faculty of Medicine, Division of Experimental Medicine, Montréal, Canada.
Mingione A, Dei Cas M, Bonezzi F, Caretti A, Piccoli M, Anastasia L, Ghidoni R, Paroni R, Signorelli P.Inhibition of Sphingolipid Synthesis as a Phenotype-Modifying Therapy in Cystic Fibrosis. Cell Physiol Biochem. 2020 Jan 31;54(1):110-125. doi: 10.33594/000000208. Free full text [Pubmed]
Cystic Fibrosis (CF) is an inherited disease associated with a variety of mutations affecting the CFTR gene. A deletion of phenylalanine 508 (F508) affects more than 70% of patients and results in unfolded proteins accumulation, originating a proteinopathy responsible for inflammation, impaired trafficking, altered metabolism, cholesterol and lipids accumulation, impaired autophagy at the cellular level. Lung inflammation has been extensively related to the accumulation of the lipotoxin ceramide. We recently proved that inhibition of ceramide synthesis by Myriocin reduces inflammation and ameliorates the defence response against pathogens infection, which is downregulated in CF. Here, we describe the mechanisms of Myriocin therapeutic effects in Cystic Fibrosis broncho-epithelial cells.
Cystic Fibrosis bronchial epithelia accumulate lipids, exacerbating inflammation. Myriocin administration: i) activates the transcriptions of genes involved in enhancing autophagy-mediated stress clearance; ii) reduces the content of several lipid species and, at the same time, iii) enhances mitochondrial lipid oxidation. Silencing the expression of Sptlc1 reproduces Myriocin induced autophagy and transcriptional activities, demonstrating that the inhibition of sphingolipid synthesis drives a transcriptional program aimed at addressing cell metabolism towards lipid oxidation and at exploiting autophagy mediated clearance of stress. They speculate that regulating sphingolipid de novo synthesis can relieve from chronic inflammation, improving energy supply and anti-oxidant responses, indicating an innovative therapeutic strategy for CF.
From the Biochemistry and Molecular Biology Laboratory, Health Sciences Department, University of Milan, Italy.
Gettle LS, Harden A, Bridges M, Albon D. Prevalence and Risk Factors for Iron Deficiency in Adults With Cystic Fibrosis. Nutr Clin Pract. 2020 Jan 29. doi: 10.1002/ncp.10454. [Epub ahead of print] [Pubmed]
Iron deficiency is common in cystic fibrosis (CF), but previous prevalence studies often reported results confounded by acute exacerbations. This single-center retrospective study aimed to identify the prevalence of iron deficiency in a stable adult CF population, identify the risk factors associated with iron deficiency, and compare common laboratory indicators of iron status. Medical charts of 105 patients aged 18-67 were reviewed to determine the prevalence of anaemia. Of these patients, a subgroup of 67 were included.
In this stable CF population, the prevalence of iron deficiency was 41.8% (n = 67), and the prevalence of anaemia was 33.3% (n = 105). Iron deficiency was associated with presence of anemia (P < .001), vitamin A deficiency (P = .012), and moderate (P = .047) and severe lung disease (P = .045) compared with mild lung disease. Transferrin agreed poorly with other iron status indicators.
The authors concluded iron deficiency is common in CF, although prevalence rates can vary widely depending on the laboratory parameters used. They suggest CF centers should consider routine screening for iron deficiency.
From the Department of Nutrition Services, University of Virginia Health System, Charlottesville, Virginia, USA
Coffey MJ, Garg M, Homaira N, Jaffe A, Ooi CY. Probiotics for people with cystic fibrosis. Cochrane Database Syst Rev. 2020 Jan 22;1:CD012949. doi: 10.1002/14651858.CD012949.pub2. [Pubmed]

Michael J Coffey
The conclusions of this review were that probiotics significantly reduce faecal calprotectin (a marker of intestinal inflammation) in children and adults with CF, however the clinical implications of this require further investigation. Probiotics may make little or no difference to pulmonary exacerbation rates, however, further evidence is required before firm conclusions can be made. Probiotics are associated with a small number of adverse events including vomiting, diarrhoea and allergic reactions. In children and adults with CF, probiotics may be considered by patients and their healthcare providers. Given the variability of probiotic composition and dosage, further adequately-powered multicentre RCTs of at least 12 months duration are required to best assess the efficacy and safety of probiotics for children and adults with CF.
Dr Michael Jonathon Coffey is a researcher at the University of New South Wales, School of Women’s and Children’s Health,
Atteih SE, Raraigh KS, Blackman SM, Cutting GR, Collaco JM. Predictive effects of low birth weight and small for gestational age status on respiratory and nutritional outcomes in cystic fibrosis.
J Cyst Fibros. 2020 Feb 12. pii: S1569-1993(20)30048-5. doi: 10.1016/j.jcf.2020.02.003. [Epub ahead of print] [Pubmed]

Michael Collaco
Prior literature shows that neonates with cystic fibrosis (CF) are more likely to be born low birth weight (LBW, <2500 grams) and/or small for gestational age (SGA, <10thpercentile for weight) than non-CF counterparts. There is limited literature exploring the predictive effects of birth parameters on long-term outcomes.The study population (CF Twin and Sibling Study) was recruited between 2000-2013 (n = 1677). Relationships between FEV1 percent predicted at 6, 12, or 18 years or BMI z-score at 2, 6, 12, or 18 years, and predictor variables (LBW or SGA status) were assessed using adjusted linear regressions.
Mean birth weight was 3.3 ± 0.7 kg (Females: 3.2 ± 0.7kg; males: 3.4 ± 0.7kg) and mean gestational age was 38.4 ± 2.6 weeks, with 10.2% of participants classified as SGA. Predictors of LBW included female sex, pancreatic insufficiency, and prematurity. Predictors of SGA included female sex. After adjustment, LBW was associated with lower BMI at ages 2-12 years and SGA was associated with lower BMI at age 2 years. LBW was associated with lower FEV1 percent predicted only at age 6 years. SGA was not associated with FEV1.
We did not observe higher rates of LBW or SGA in full term infants compared to the general population. We observed associations particularly between LBW and BMI or FEV1, but these associations decreased with age, suggesting that alternate factors contribute to outcomes over time. In lieu of the ability to target growth during gestation, efforts could be considered to optimize infant nutritional status, which may improve later life outcomes.
Dr Samar Atteih is a Third-Year Resident ta Johns Hopkins Children’s Center, Baltimore, MD, USA.
Dr J Michael Collaco is Associate Professor of Pediatrics at Johns Hopkins
Chevalier B, Hinzpeter A. The influence of CFTR complex alleles on precision therapy of cystic fibrosis.
J Cyst Fibros. 2020 Mar;19 Suppl 1:S15-S18. doi: 10.1016/j.jcf.2019.12.008. Epub 2019 Dec 26.[Pubmed] CFTR is an extensively studied gene and multiple sequence variants have been identified, many of which still need to be defined as neutral or disease causing. Complex alleles are defined when at least two variants are identified on the same allele. Each pathogenic variant can affect distinct steps of the CFTR biogenesis. As CFTR modulators are being developed to alleviate specific defects, pathogenic variants need to be characterized to propose adequate treatments. Conversely, cis-variants can affect treatment response when defects are additive or if they alter the binding or efficacy of the modulator. Hence, complex alleles increase the complexity of CFTR variant classification and need to be assigned as neutral, disease causing or modulating treatment efficacy. This review was based on a symposium session presented at the 16th ECFS Basic Science Conference, Dubrovnik, Croatia, 27 to 30 March, 2019.
Both authors from INSERM U1151, Institut Necker Enfants Malades, Paris, France; Université Paris Descartes, Paris, France. Electronic address: benoit.chevalier@inserm.fr
Lavi E, Gileles-Hillel A, Zangen D. Somatic growth in cystic fibrosis. Curr Opin Endocrinol Diabetes Obes. 2020 Feb;27(1):38-46. doi: 10.1097/MED.0000000000000522. [Pubmed]

Alex Gileles-Hillel

David Zangen
Cystic fibrosis (CF) is commonly associated with compromised growth especially in severe cases when the pulmonary function (PFT) deteriorates. As growth optimization is an important aspect of CF management, this review will summarize the current knowledge on the prevalence of growth failure in CF patients, and focus on the mechanisms leading to poor growth, on the association of poor linear growth with reduced PFT and on recombinant human growth hormone (rhGH) therapy in CF patients.
Despite the improvement in CF care in the last 2 decades, compromised linear growth is still quite prevalent. The pathophysiology of growth failure in CF is multifactorial. Malnutrition due to decreased energy intake increased energy expenditure and malabsorption of ingested nutrients secondary to pancreatic insufficiency, all probably play a major role in growth restriction. In addition, chronic inflammation characteristic of CF may contribute to growth failure via alteration in the GH-insulin-like growth factor 1 signaling and other changes in the growth plate. rhGH and new CFTR modulators may improve some growth parameters.
Beyond optimizing nutrition and malabsorption, and controlling chronic inflammation, children with CF may benefit from the anabolic effects of rhGH therapy to improve their anthropometric parameters. Whether this translates into better PFT and improved long-term outcomes is yet to be determined.
Prof David Zangen is Head of the Division of Pediatric Endocrinology and Juvenile Diabetes Unit, Pediatric Endocrinology Unit. Dr Alex Gileles-Hillel a member of the Pediatric Pulmonology and CF Unit, Department of Pediatrics. The Wohl Institute for Translational Medicine, Hadassah Hebrew University Medical Center, Jerusalem, Israel.
– There is a considerable research on the use of growth hormone in children with CF
Zofia N Zysman-Colman, Marissa J Kilberg, Victor S Harrison, Alessandra Chesi, Struan F A Grant , Jonathan Mitchell, Saba Sheikh, Denis Hadjiliadis, Michael R Rickels, Ronald C Rubenstein, Andrea Kelly. Genetic Potential and Height Velocity During Childhood and Adolescence Do Not Fully Account for Shorter Stature in Cystic Fibrosis. Pediatr Res 2020 May 9.doi: 10.1038/s41390-020-0940-4. Online ahead of print. 32386398 [Pubmed]

Zofia N Zysman-Colman
Despite improved health, shorter stature is common in cystic fibrosis (CF). The authors aimed to describe height velocity (HV) and contribution of height-related genetic variants to height (HT) in CF. Methods: HV cohort: standard deviation scores (-Z) for HT, mid-parental height-adjusted HT (MPAH), and HV were generated using our Pediatric Center’s CF Foundation registry data. HV-Z was compared with population means at each age (5-17 y), the relationship of HV-Z with HT-Z assessed, and HT-Z compared with MPAH-Z. GRS cohort: HT genetic risk-Z (HT-GRS-Z) were determined for pancreatic exocrine sufficient (PS) and insufficient (PI) youth and adults from our CF center and their relationships with HT-Z assessed.
Results: HV cohort: average HV-Z was normal across ages in our cohort but was 1.5× lower (p < 0.01) for each SD decrease in HT-Z. MPAH-Z was lower than HT-Z (p < 0.001). GRS cohort: HT-GRS-Z more strongly correlated with HT-Z and better explained height variance in PS (rho = 0.42; R2= 0.25) vs. PI (rho = 0.27; R2 = 0.11).
Conclusions: Despite shorter stature compared with peers and mid-parental height, youth with CF generally have normal linear growth in mid- and late childhood. PI tempered the heritability of height. These results suggest that, in CF, final height is determined early in life in CF and genetic potential is attenuated by other factors.
The authors comment this manuscript is a clinical study: Children with CF remain shorter than their healthy peers despite advances in care. Our study demonstrates that children with CF have persistent shorter stature from an early age and fail to reach their genetic potential despite height velocities comparable to those of average maturing healthy peers and similar enrichment in known height increasing single-nucleotide polymorphisms (SNPs). Genetic risk scores better explained variability in pancreatic sufficient than in pancreatic insufficient individuals, suggesting that other modifying factors are in play for pancreatic insufficient individuals with CF. Given the CF Foundation’s recommendation to target not only normal body mass index, but normal height percentiles as well, this study adds valuable insight to this discussion.
Zofia N Zysman-Colman is in the Division of Pulmonary Medicine, Children’s Hospital of Philadelphia, Philadelphia, PA, USA.
Virginia A Stallings, Alyssa M Tindall, Maria R Mascarenhas , Asim Maqbool, Joan I Schall. Improved Residual Fat Malabsorption and Growth in Children With Cystic Fibrosis Treated With a Novel Oral Structured Lipid Supplement: A Randomized Controlled Trial. PLoS One 2020 May 8;15(5):e0232685.doi: 10.1371/journal.pone.0232685. eCollection 2020.[Pubmed]

Virginia Stallings
In the primary analysis of a 12-month double-blind randomized active placebo-controlled trial, treatment of children with cystic fibrosis (CF) and pancreatic insufficiency (PI) with a readily absorbable structured lipid (Encala™, Envara Health, Wayne, PA) was safe, well-tolerated and improved dietary fat absorption (stool coefficient of fat absorption [CFA]), growth, and plasma fatty acids (FA). [Full details in PubMed abstract above] Findings: Subjects with CF, PI and more severe fat malabsorption experienced greater improvements in CFA, FA and growth after three months of Encala™ treatment. Encala™ was safe, well-tolerated and efficacious in patients with CF and PI with residual fat malabsorption and improved dietary energy absorption, weight gain and FA status in this at-risk group
Dr Virginla Stallings is in the Division of Gastroenterology, Hepatology and Nutrition and Department of Pediatrics, University of Pennsylvania Perelman School of Medicine, Philadelphia.
Helmut Ellemunter, Markus Dumke, Gratiana Steinkamp. Reference Values Matter: Fewer Patients with Malnutrition using American Compared to more Recent German Growth Charts. J Pediatr Gastroenterol Nutr 2021 Feb 24.doi: 10.1097/MPG.0000000000003095.Online ahead of print. [Pubmed]

Helmut Ellemunter
Reference values are important for patient care as well as for comparisons between different centres or countries. We investigated two anthropometric reference datasets, the US Centers for Disease Control (CDC) growth charts and the German Health Interview and Examination Survey for Children and Adolescents Study (KiGGS) percentiles, which were established in Germany between 2003 and 2006. A smaller proportion of children with cystic fibrosis had decreased z-scores <-2 with CDC (5.0% for weight and 3.0% for height) compared to KiGGS (7.4% for weight and 6.3% for height) values (p<0.0001). Median z-scores were higher using the CDC reference data. Thus, the choice of growth reference is important, may influence clinical management and must be considered when comparing outcomes of different institutions.
Dr Helmut Ellemunter is Assistant Professor at the Cystic Fibrosis Centre at the Medical University of Innsbruck, Department of Child and Adolescent Health, Paediatrics III, Austria. STAT-UP Statistical Consulting & Services, Munich, Germany Clinical Research and Medical Scientific Writing, Schwerin, Germany.
Molly Bozic , Christopher H Goss , Rabindra M Tirouvanziam, Arthur Baines, Margaret Kloster, Liebe Antoine, Drucy Borowitz, Sarah Jane Schwarzenberg, GROW study group. Oral Glutathione and Growth in Cystic Fibrosis: A Multicenter, Randomized, Placebo-controlled, Double-blind Trial J Pediatr Gastroenterol Nutr 2020 Dec;71(6):771-777.doi: 10.1097/MPG.0000000000002948. [Pubmed]

Molly Bozic
Objectives: The nutritional status of children with cystic fibrosis (CF) is associated with mortality and morbidity. Intestinal inflammation may contribute to impaired digestion, absorption, and nutrient utilization in patients with CF and oral glutathione may reduce inflammation, promoting improved nutritional status in patients with CF.
Methods: The GROW study was a prospective, multicenter, randomized, placebo-controlled, double-blind, phase II clinical trial in pancreatic insufficient patients with CF between the ages of 2 and 10 years. Patients received reduced glutathione or placebo orally daily for 24 weeks. The primary endpoint was the difference in change in weight-for-age z-scores from baseline through week 24 between treatment groups. Secondary endpoints included other anthropometrics, serum, and fecal inflammatory markers in addition to other clinical outcomes.
Results: Fifty-eight participants completed the study. No significant differences were seen between glutathione (n = 30) and placebo (n = 28) groups in the 6-month change in weight-for-age z-score (-0.08; 95% CI: -0.22 to 0.06; P = 0.25); absolute change in weight (kg) (-0.18; 95% CI: -0.55 to 0.20; P = 0.35); or absolute change in BMI kg/m (-0.06; 95% CI: -0.37 to 0.25; P = 0.69). There were no significant differences in other secondary endpoints. Overall, glutathione was safe and well tolerated.
Conclusions: Oral glutathione supplementation did not impact growth or change serum or fecal inflammatory markers in pancreatic insufficient children with CF when compared with placebo.
Dr Molly Bozic is Associate Professor of Pediatrics at the Indiana University School of Medicine, Indianapolis, IN.
Meghana Sathe, Preeti B Sharma, Adrienne P Savant. Year in review 2020: Nutrition and gastrointestinal disease in cystic fibrosis. Pediatr Pulmonol. 2021 Jul 26.doi: 10.1002/ppul.25587. Online ahead of print. [Pubmed]
The multisystemic manifestations of cystic fibrosis (CF) involve all parts of the gastrointestinal (GI) system, including the pancreas, intestine, and liver. As providers who care for people with CF, knowledge of the manifestations, treatment, and research related to nutrition and GI disease are important. This review is the last instalment of the CF year in review 2020 series, focusing on nutritional, GI, and hepatobiliary articles from Pediatric Pulmonology and other journals of particular interest to clinicians..
– A useful review of the many contributions in these areas during the year. Summarised by the authors in the article as follows – “The lessons from 2020 for nutrition include 1) reminders to assess pancreatic status via genotype/phenotype correlation; 2) apps can help optimize PERT dosing 3) a new nutritional supplement can aid fat malabsorption 4) Nutritional deficiencies are common 5) obesity is not uncommon and associated with a plateau effect on FEV1. The intestinal microbiome is altered early in life with specific environmental tobacco smoke exposure and antibiotics, leading to more pathogenic bacteria while no microbial alterations are seen with acid blocking agents. The low length was shown to be associated with differences in the intestinal microbiome, allowing for the possibility of intestinal microbiome treatment to improve growth. Liver disease can be assessed with biomarkers and images with GGT being a key biomarker. Ultrasound findings of a heterogenous liver were nine times more likely to predict progression to nodular disease. Liver stiffness measurements have the ability to define the degree of fibrosis.”
Meghana Sathe is in the Division Gastroenterology, Hepatology, and Nutrition, Department of Pediatrics, University of Texas Southwestern and Children’s Health, Dallas, Tex
Clark T Bishop Case report: Three adult brothers with cystic fibrosis (delF508-delF508) maintain unusually preserved clinical profile in the absence of standard CF care. Respir Med Case Rep 2021 Apr 15;33:101413.doi: 10.1016/j.rmcr.2021.101413. eCollection 2021. Free PMC article [Pubmed]

Clark T Bishop
We present three cases in this report. Three adult brothers, homozygous for the delF508 cystic fibrosis mutation, have maintained an unusually preserved clinical condition even though they did not attend a CF Clinic during their childhood, do not attend a CF Clinic now, and do not follow standard CF care guidelines. The brothers use an alternative CF treatment regimen on which they have maintained normal lung function, height/weight, and bloodwork, and they utilize less than half the recommended dosage of pancreatic enzymes. The brothers culture only methicillin-sensitive Staphylococcus aureus, and have never cultured any other bacteria. Highly effective modulator therapies, such as elexacaftor/tezacaftor/ivacaftor, do not substantially reduce infection and inflammation in vivo in CF patients, and thus these three case reports are of special note in terms of suggesting adjunct therapeutic approaches. Finally, these three cases also raise important questions about standard CF care guideline
Advise read the Free article where the detailed treatment of these patients is described. Dr Clark has long time been an advocate of importance of glutathione’
Sarah E Bauer, HuiChuan J Lai, Catherine M McDonald, Fadi Asfour, James E Slaven, Clement L Ren. Zinc status and growth in infants and young children with cystic fibrosis. Pediatr Pulmonol. 2021 Sep 9.doi: 10.1002/ppul.25666. Online ahead of print. [Pubmed]
Background: Zinc deficiency is associated with poor growth in children without cystic fibrosis (CF), but its impact on growth in children with CF is unknown.
Objective: To determine the prevalence of low serum Zn (sZn) and its relationship with growth in the first 3 years of life in children with CF.
Methods: We utilized data from infants with CF who were enrolled in a longitudinal study of nutrition and lung health and had sZn measured as part of clinical care. Cross-sectional correlations between sZn levels and growth z scores were assessed by Pearson’s correlation coefficient. To identify factors associated with sZn status and its association to longitudinal growth patterns, multiple regression analysis with repeated measures were performed using generalized estimating equations.
Results: A total of 106 sZn measurements from 53 infants were identified. Seventeen infants (32%) had intermittent Zn insufficiency, defined as at least one sZn <70 mcg/dl in their first 3 years of life. There were no significant cross-sectional associations between sZn and growth z scores. However, analysis of longitudinal growth patterns revealed that weight- and length-for-age z scores in children with intermittent Zn insufficiency were lower during early infancy and their weight-for-length z scores at age 3 years were also lower compared to those who were always Zn sufficient.
Conclusion: Low sZn occurs in one-third of children with CF in the first 3 years of life. Cross-sectional and longitudinal analyses revealed discrepant associations between sZn and growth. Therefore, prospective studies are needed to understand the role of Zn in growth in CF.
Dr Sarah E Bauer is a paediatric pulmonologist in the Department of Pediatrics, Indiana University School of Medicine, Indianapolis, Indiana, USA
Deanne H Hryciw , Courtney A Jackson, Nirajan Shrestha, David Parsons, Martin Donnelley, Andrew J McAinch. Role for animal models in understanding essential fatty acid deficiency in cystic fibrosis. Cell Mol Life Sci. 2021 Nov 5.doi: 10.1007/s00018-021-04014-2.Online ahead of print. [Pubmed]

Deanne H Hryciw
Essential fatty acid deficiency has been observed in most patients with Cystic Fibrosis (CF); however, pancreatic supplementation does not restore the deficiency, suggesting a different pathology independent of the pancreas. At this time, the underlying pathological mechanisms are largely unknown. Essential fatty acids are obtained from the diet and processed by organs including the liver and intestine, two organs significantly impacted by mutations in the cystic fibrosis transmembrane conductance regulator gene (Cftr). There are several CF animal models in a variety of species that have been developed to investigate molecular mechanisms associated with the CF phenotype. Specifically, global and systemic mutations in Cftr which mimic genotypic changes identified in CF patients have been generated in mice, rats, sheep, pigs and ferrets. These mutations produce CFTR proteins with a gating defect, trafficking defect, or an absent or inactive CFTR channel. Essential fatty acids are critical to CFTR function, with a bidirectional relationship between CFTR and essential fatty acids proposed. Currently, there are limited analyses on the essential fatty acid status in most of these animal models. Of interest, in the mouse model, essential fatty acid status is dependent on the genotype and resultant phenotype of the mouse. Future investigations should identify an optimal animal model that has most of the phenotypic changes associated with CF including the essential fatty acid deficiencies, which can be used in the development of therapeutics.
Dr Deanne H Hryciw is a Senior Lecturer at the School of Environment and Science, Griffith University, Nathan, QLD, Australia. Centre for Planetary Health and Food Security, Griffith University, Nathan, QLD, Australia. Institute for Health and Sport, Victoria University, Melbourne, VIC, Australia.
Megan E Gabel, Claudia K Fox, Rachel A Grimes, John D Lowman, Catherine M McDonald, Virginia A Stallings, Suzanne H Michel. Overweight and cystic fibrosis: An unexpected challenge. Pediatr Pulmonol 2021 Nov 5.doi: 10.1002/ppul.25748. Online ahead of print. [Pubmed]

Megan E Gabel
Achieving a healthy weight balance has been a central focus of care for people who have cystic fibrosis (CF). Over the years, the emphasis has primarily been on promoting weight gain to optimize pulmonary outcomes. With continued improvements in CF care, including highly effective CF modulators available for many people, the CF community is now experiencing a new challenge: addressing the concern that some people are gaining weight excessively. While at this time, we do not know to what extent overweight and obesity will affect health outcomes for people with CF, it is likely that excessive weight gain may have negative health impacts similar to those seen in the general population. In this paper, we review the history of nutritional guidelines for people with CF, as well as more recent trends toward overweight and obesity for some. A multidisciplinary approach is needed to collaboratively start the oftentimes difficult conversation regarding excessive weight gain, and to identify resources to help people achieve and maintain a healthy weight through diet, exercise, and behavioral modification.
Dr Megan E Gabel is Associate Professor in the Department of Pediatrics, University of Rochester Medical Center, Rochester, New York, USA.
Sarah Soltman, Rebecca A Hicks, Farah Naz Khan, Andrea Kelly. Body composition in individuals with cystic fibrosis. J Clin Transl Endocrinol. 2021 Oct 30;26:100272 doi: 10.1016/j.jcte.2021.100272.eCollection 2021 Dec. Free PMC article .[Pubmed]

Sarah Soltman
Because nutritional status is intimately linked with pulmonary function and survival, nutrition has been at the mainstay of cystic fibrosis (CF) care. Body Mass Index (BMI) is traditionally used to define nutritional status because of the ease with which it can be calculated, but it has a number of limitations including its inability to differentiate fat mass (FM) from lean body mass (LBM), the latter thought to confer health advantage.
A number of tools are available to quantify body composition including dual-energy x-ray absorptiometry (DXA), bioelectrical impedance, MRI, CT, air displacement plethysmography, and stable isotopes, and these have been used to varying degrees in studies of CF.
In CF, LBM tends to be lower for a given BMI, particularly at lower BMI. In adults, lower fat-free mass (FFM) correlates with greater CF disease severity, lower pulmonary function and higher inflammatory markers. FFM is also positively associated with greater bone mineral density, while greater FM is associated with greater loss of lumbar spine bone mineral density over 2 years. In youth, LBM is positively associated with pulmonary function. The predictive value of body composition for functional and clinical outcomes and the role of improving LBM on these outcomes remain undefined. With improvements in BMI accompanying highly-effective modulator therapy, closer evaluations of body composition may inform risk for more traditional, non-CF adult outcomes in CF.
All the authors are associated with Oregon Health & Science University Division of Endocrinology, Diabetes and Clinical Nutrition 3181 Southwest Sam Jackson Park Road, L607 Portland, OR 97239, USA. David Geffen School of Medicine, UCLA, Division of Pediatric Endocrinology, US University of Washington Division of Metabolism, Endocrinology and Nutrition, USA. Children’s Hospital of Philadelphia Division of Endocrinology & Diabetes, USA. Perelman School of Medicine of University of Pennsylvania, USA.
Max C Petersen, Lauren Begnel, Michael Wallendorf, Marina Litvin. Effect of elexacaftor-tezacaftor-ivacaftor on body weight and metabolic parameters in adults with cystic fibrosis. J Cyst Fibros 2021 Nov 30;S1569-1993(21)02153-6. doi: 10.1016/j.jcf.2021.11.012.Online ahead of print. [Pubmed]

Max Petersen
Background: Though weight gain has been reported in some clinical trials of CFTR modulators, the effect of elexacaftor-tezacaftor-ivacaftor on body weight, body mass index (BMI), blood pressure, lipids and glycemic control in the real-world setting remains incompletely described.
Methods: We performed a single-center, retrospective, observational analysis of the effect of elexacaftor-tezacaftor-ivacaftor on body weight and cardiometabolic parameters in 134 adult CF patients of the Washington University Adult Cystic Fibrosis Center. Body weight, BMI, and blood pressure were extracted from outpatient clinic visits for the year preceding and the period following the initiation of elexacaftor-tezacaftor-ivacaftor. Other metabolic parameters were extracted at baseline and at latest available follow-up.
Results: A mean of 12.2 months of follow-up data was available for analysis. The mean rate of change in BMI was 1.47 kg/m2/yr (95% CI, 1.08 to 1.87) greater after initiation of elexacaftor-tezacaftor-ivacaftor. Significant increases in blood pressure were observed. In those without CFRD, random blood glucose and hemoglobin A1c were decreased after elexacaftor-tezacaftor-ivacaftor initiation. In those with CFRD, elexacaftor-tezacaftor-ivacaftor increased serum total cholesterol, HDL-cholesterol, and LDL-cholesterol.
Conclusions: In this single-center, retrospective, observational study of 134 adults with CF, initiation of elexacaftor-tezacaftor-ivacaftor was associated with increases in BMI at a mean follow up of 12.2 months. Changes in other cardiometabolic risk factors were also observed. Widespread use of elexacaftor-tezacaftor-ivacaftor may be expected to increase the incidence of overnutrition in the CF population.
Max C Petersen is in the Division of Endocrinology, Metabolism, & Lipid Research, Department of Medicine, Washington University, St. Louis, Missouri, USA.
Margaret P Marks , Sonya L Heltshe, Arthur Baines, Bonnie W Ramsey, Lucas R Hoffman, Michael S Stalvey. Most Short Children with Cystic Fibrosis Do Not Catch Up by Adulthood. Nutrients 2021 Dec 10;13(12):4414.doi: 10.3390/nu13124414. Free PMC article [Pubmed]
Poor linear growth is common in children with cystic fibrosis (CF) and predicts pulmonary status and mortality. Growth impairment develops in infancy, prior to pulmonary decline and despite aggressive nutritional measures. We hypothesized that growth restriction during early childhood in CF is associated with reduced adult height. We used the Cystic Fibrosis Foundation (CFF) patient registry to identify CF adults between 2011 and 2015 (ages 18-19 y, n = 3655) and had height for age (HFA) records between ages 2 and 4 y. We found that only 26% CF adults were ≥median HFA and 25% were <10th percentile. Between 2 and 4 years, those with height < 10th percentile had increased odds of being <10th percentile in adulthood compared to children ≥ 10th percentile (OR = 7.7). Of HFA measured between the 10th and 25th percentiles at ages 2-4, 58% were <25th percentile as adults. Only 13% between the 10th and 25th percentile HFA at age 2-4 years were >50th percentile as adults. Maximum height between ages 2 and 4 highly correlated with adult height. These results demonstrate that low early childhood CF height correlates with height in adulthood. Since linear growth correlates with lung growth, identifying both risk factors and interventions for growth failure (nutritional support, confounders of clinical care, and potential endocrine involvement) could lead to improved overall health.
Dr Margaret P Marks is a paediatrician in the Department of Pediatrics, University of Alabama, and the Cystic Fibrosis Research Center, University of Alabama, Birmingham, AL 35233, USA.
Dirk Westhölter FabianSchumacher, Nuria Wülfinghoff, SivagurunathanSutharsan, Svenja Strassburg, Burkhard Kleuser, Peter A Horn, Sebastian Reuter, Erich Gulbins, Christian Taube, Matthias Welsner. CFTR modulator therapy alters plasma sphingolipid profiles in people with cystic fibrosis. J Cyst Fibros 2022 Feb 12;S1569-1993(22)00037-6.doi: 10.1016/j.jcf.2022.02.005.Online ahead of print. [Pubmed]

Dirk Westholter
Background: Sphingolipids, in particular ceramides, play an important role in the pathogenesis of cystic fibrosis (CF) lung disease. Ceramides seem to be dysregulated in people with CF (PWCF): An elevated ratio of ceramides C16Cer/ C24Cer has been linked to inflammation and disease severity. CFTR modulators might influence sphingolipid dysregulation in PWCF.
Methods: Sphingolipid profiles were retrospectively analyzed in serum from 112 PWCF and 96 healthy controls as well as in plasma from 25 PWCF before and after treatment with the CFTR modulator elexacaftor/tezacaftor/ivacaftor (ELX/TEZ/IVA) using liquid chromatography-tandem mass spectrometry (LC-MS/MS). Lipid data were correlated with clinical parameters.
Results: There were significantly higher levels of long-chain ceramides C18Cer and C20Cer and of the very long-chain ceramide C24:1Cer in PWCF versus healthy controls. Sphingosine levels were significantly reduced and accurately distinguished PWCF from healthy controls. Treatment with ELX/TEZ/IVA was associated with a decrease in levels of long-chain ceramides C16Cer, C18Cer and C20Cer and very long-chain ceramide C24:1Cer. Plasma levels of the most abundant very long-chain ceramide C24Cer as well as sphingosine-1-phosphate increased. Consequently, the ratio of ceramides C16Cer/ C24Cer decreased. Sphingolipid levels showed weak correlations with clinical parameters.
Conclusions: These findings highlight the existence of a distinctive sphingolipid profile in blood from PWCF, which appears to be altered by ELX/TEZ/IVA therapy. Thus, strategies for sphingolipid remodeling need to be reassessed and adjusted in the light of highly effective CFTR modulator therapies.
Dirk Westhölter is in the Department of Pulmonary Medicine, University Hospital Essen- Ruhrlandklinik, Tüschener Weg 40, Essen 45239, Germany. Electronic address: dirk.westhoelter@uk-essen.de.
Birgitta Strandvik. Nutrition in Cystic Fibrosis-Some Notes on the Fat Recommendations. Nutrients 2022 Feb 18;14(4):853.doi: 10.3390/nu14040853. Free PMC article [Pubmed]

Birgitta Strandvik
Nutrition is important in cystic fibrosis (CF) because the disease is associated with a higher energy consumption, special nutritional deficiencies, and malabsorption mainly related to pancreatic insufficiency. The clinical course with deterioration of lung function has been shown to relate to nutrition. Despite general recommendation of high energy intake, the clinical deterioration is difficult to restrain suggesting that special needs have not been identified and specified. It is well-known that the CF phenotype is associated with lipid abnormalities, especially in the essential or conditionally essential fatty acids.
This review will concentrate on the qualitative aspects of fat metabolism, which has mainly been neglected in dietary fat recommendations focusing on fat quantity. For more than 60 years it has been known and confirmed that the patients have a deficiency of linoleic acid, an n-6 essential fatty acid of importance for membrane structure and function. The ratio between arachidonic acid and docosahexaenoic acid, conditionally essential fatty acids of the n-6 and n-3 series, respectively, is often increased. The recently discovered relations between the CFTR modulators and lipid metabolism raise new interests in this field and together with new technology provide possibilities to specify further specify personalized therapy.
Professor Birgitta Strandvik is in the Department of Biosciences and Nutrition, Karolinska Institutet, Huddinge, 14183 Stockholm, Sweden.
-Professor Strandvik has been and remains a leading European authority on cystic fibrosis since the Sixties. This paper deals with one of her favourite areas, lipid metabolism in the era of CFTR modulators.
Aliye Uc , Birgitta Strandvik, Jianrong Yao, Xiaoming Liu, Yaling Yi , Xingshen Sun 3 , Ruth Welti , John F Engelhardt, Andrew W Norris. The Fatty Acid Imbalance of Cystic Fibrosis Exists at Birth Independent of Feeding, in Pig and Ferret Models. Clin Sci (Lond). 2022 Nov 23;CS20220450. doi: 10.1042/CS20220450. Online ahead of print. pubmed.ncbi.nlm.nih.gov/36416119/

Aliye Uc
Persons with cystic fibrosis (CF) exhibit a unique alteration of fatty acid composition, marked especially among polyunsaturates by relative deficiency of linoleic acid and excess of Mead acid. Relative deficiency of docosahexaenoic acid is variably found. However, the initial development of these abnormalities is not understood. We examined fatty acid composition in young CF ferrets and pigs, finding abnormalities from the day of birth onward including relative deficiency of linoleic acid in both species. Fatty acid composition abnormalities were present in both liver and serum phospholipids of newborn CF piglets even prior to feeding, including reduced linoleic acid and increased Mead acid. Serum fatty acid composition evolved over the first weeks of life in both non-CF and CF ferrets, though differences between CF and non-CF persisted. Although red blood cell phospholipid fatty acid composition was normal in newborn animals, it became perturbed in juvenile CF ferrets including relative deficiencies of linoleic and docosahexaenoic acids and excess of Mead acid. In summary, fatty acid composition abnormalities in CF pigs and ferrets exist from a young age including at birth independent of feeding and overlap extensively with the abnormalities found in humans with CF. That the abnormalities exist prior to feeding implies that dietary measures alone will not address the mechanisms of imbalance.
Aliye Uc, MD, is director of the division of pediatric gastroenterology at University of Iowa Stead Family Children’s Hospital.
