PHYSIOTHERAPY – INCLUDES EXERCISE, INHALATION TREATMNTS
In 2011 the UK Cystic Fibrosis Trust published the Association of Chartered Physiotherapists in Cystic Fibrosis (ACPCF) “Standards of Care and Good Clinical Practice for Physiotherapy Management Cystic Fibrosis” edited by Penney Argent, Lisa Morrison and Ammani Prasad; it is an excellent review of the subject and available on the CF Trust website (www.cysticfibrosis.org.uk) or the ACPCF website (www.csp.org.uk/professional-networks/acpcf).
1959 Doyle B. Physical therapy in treatment of cystic fibrosis. Phys Therapy Rev 1959; 39:24 – 27. (Prepared under the direction of Harry Shwachman). [PubMed]
Barbara Doyle
An early report of physical therapy for the chest in cystic fibrosis. Shwachman mentions that active physical therapy was instituted in his clinic in 1957 and considers it to be one of the more important introductions into the treatment regimen. Barbara Doyle (figure ) was a physical therapist from Eire who received her physical therapy preparation at Dublin School of Physiotherapy and was a member of the Chartered Physiotherapy Society of Great Britain. From 1956-1958 she was an exchange visitor in the United States and worked at the Children’s Medical Center, Boston. She used the so-called “English” methods (Reid JMW in Physiotherapy for Chest Diseases. In Marshall G, Perry KMA. (Eds.) Diseases of the Chest. St Louis: Butterworth & Company. 1952; 2:395-413). This report describes the current physiotherapy treatment for people with CF as done in Shwachman’s clinic in Boston and based on the experience with various chest conditions at the Hospital for Sick Children, Great Ormond Street, London.
Lannefors L et al. (J R Soc Med 2004; 97 (Suppl 44):8-25) in an excellent review of CF physiotherapy note the first reference to the use of postural drainage was by Ewart in 1901 (Ewart W. Lancet 1901; ii: 70) who referred to it as “empty bronchus treatment by posture in bronchiectasis of children”. Although few children with CF would have survived infancy at that time, bronchiectasis as an after effect of pneumococcal pneumonia, whooping cough or measles was relatively common in the pre-antibiotic era. Ewart advocated continuous drainage for hours at a time with the patient sleeping in the various positions. Later the detailed anatomy of the various lobes was described (Nelson HP. BMJ 1934; 11:251-255) and in 1949 the nomenclature of the anatomy was agreed (Anonymous. Nomenclature of broncho-pulmonary anatomy; an international nomenclature accepted by the Thoracic Society. Thorax 1950; 5: 222-228).
1962 Denton R. Bronchial secretions in cystic fibrosis. The effects of treatment with mechanical percussion vibration. Am Rev Respir Dis 1962; 86:41-6. [PubMed]
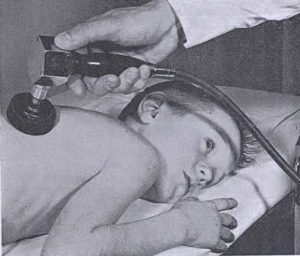
Chest percussor
One of many publications by Dr Robert Denton from Philadelphia. As the effect of chest clapping and vibrations was considered to be helpful in moving bronchial secretions, the effect of rapid repetitive percussion with a mechanical device was examined in 23 patients with CF who had moderate and marked pulmonary involvement.
The study with a mechanical percussor (figure ) is complex and impressive, even involving a “control percussor” that did not vibrate. Over a 12 minute period, there was a significant increase in secretions produced with the percussor + vibrations compared to percussor with simulated vibrations and unassisted postural drainage; this was significant in 19 of the 23 patients although the vital capacity did not change significantly.
This was the first of a number of papers on mechanical percussion as an aid to chest physiotherapy. Some years later in the UK the “Salford percussor” (Maxwell & Redmond, 1979 below; Flowers et al, 1979 below) received a cool reception from the UK physiotherapists. However, the delivery of vibrations by a jacket or vest eventually became part of standard approved therapy in the USA thanks to the work of Warren Warwick (Warwick & Hansen, 1991 below). Again this more recent mechanical aid, “the Vest”, was slow to find favour with physiotherapists in the UK!
1979 Pryor JA, Webber BA, Hodson ME, Batten JC. Evaluation of the use of forced expiration technique as an adjunct to postural drainage in treatment of cystic fibrosis. BMJ 1979; 2:417-418. [PubMed]
The classic paper on forced expiratory technique (FET) from the Brompton Hospital, London comparing conventional physiotherapy with FET without the involvement of an assistant. The latter was both more efficient (producing 45.6 g vs. 63.1 g sputum per day) and quicker (358.5 vs. 652.1 mg sputum per minute) than conventional physiotherapy and was not improved by involving an assistant. The authors concluded – “Patients with cystic fibrosis who had to rely on the help of others for their home treatment may now perform more effective treatment without help”.
The value of chest physiotherapy in clearing bronchial secretions in conjunction with postural drainage in patients producing more than 30ml of sputum per day was established first by Cochrane GM et al, (BMJ 1977; 2:1181-1183) who studied the specific airways conductance (SGAW) of 23 patients with copious sputum production and airflow obstruction before and after physiotherapy to determine the effect of bronchial secretions on pulmonary function. Chest physiotherapy to remove these secretions had the effect of reducing airflow obstruction, as measured by SGAW. These findings were taken to suggest that sputum has a detrimental effect on pulmonary function and that physiotherapy can reduce airways obstruction. Physiotherapy for children with CF had been introduced into Shwachman’s clinic in 1957 by Barbara Doyle (Doyle et al, 1959 above). This forced expiratory technique represented a significant advance allowing the patient more independence and less reliance on others.
1979 Flower KA, Eden RI, Lomax L, Mann NM, Burgess J. New mechanical aid to physiotherapy in cystic fibrosis. BMJ 1979; 2:630-631. [PubMed]
The authors analysed the effects of the percussion provided by professional physiotherapists for the first time and reproduced in the small portable “Salford Percussor”. Although initially popular with a few parents there was no subsequent work on the device and it was not accepted by UK physiotherapists who, as a group generally, have not been enthusiastic about mechanical aids to physiotherapy – as evidenced by their more recent lack of enthusiasm for the mechanical vest!!! (also Denton, 1962 above; Maxwell & Redmond, 1979 below)
1979 Maxwell M, Redmond A. Comparative trial of manual and mechanical percussion technique with gravity-assisted bronchial drainage in patients with cystic fibrosis. Arch Dis Child 1979; 54:542-544. [PubMed]
Here 14 patients with CF were studied by measuring sputum volumes and respiratory function. The results with the mechanical percussor (figure 22)

Aileen Redmond
were comparable with those with manual percussion. All the patients and parents preferred the mechanical percussor.
However, there is no further mention of the mechanical percussor by either the Manchester group (Flower et al, 1979 above) or Belfast group (Maxwell & Redmond) and they did not gain the support of he majority of UK physiotherapists who seem, as a group, to be unimpressed by mechanical aids for physiotherapy. Mechanical methods had been reported previously in an excellent trial by Robert Denton (Am Rev Respir Dis 1962; 86:41-46 above).
Aileen Redmond was paediatrician at the Belfast paediatric CF unit and had worked with Harry Shwachman in Boston – one of the first centres to use physiotherapy. She published on a wide variety of subjects including CF and was one of the few UK experts in CF at the time and one of the first to introduce neonatal IRT CF screening in Northern Ireland in the early Eighties. Her CF unit at the Belfast Children’s Hospital was highly regarded and she eventually achieved a purpose built CF unit – Cherry Tree House in Belfast.
1983 Desmond KJ, Schwenk WF, Thomas E, Beaudry PH, Coates AL. Immediate and long term effects of chest physiotherapy in patients with cystic fibrosis. J Pediatr 1983; 103:538-542. [PubMed]
Spirometric and plethysmographic evaluations were performed before chest physiotherapy (CPT) and at five and 30 minutes post-CPT. The pre-CPT measurements after a three-week period with no CPT were compared with the values while receiving CPT on a regular twice daily basis. Their findings showed that although there may be little immediate functional improvement when CPT is received on a regular basis, a three-week period without CPT resulted in a worsening of respiratory function which was reversed with renewal of regular chest physiotherapy.
This is one of the few studies evaluating the efficacy of chest physiotherapy. Previously Pryor et al, (1979 above) had evaluated the forced expiratory technique. Subsequently Reisman et al, (1988 below) performed a trial of physiotherapy in Toronto which also showed the benefit of routine physiotherapy. Considering the huge time commitment of the patients and their families to physiotherapy there were surprisingly few publications evaluating the efficacy of physiotherapy treatment.
1984 Falk M, Kelstrup M, Anderson JB, Kinoshita T, Falk P, Stovring S, Gothgen I. Improving the ketchup bottle method with positive expiratory pressure, PEP, in cystic fibrosis. Eur J Resp Dis 1984; 65:423-432. [PubMed]
The first report of the Positive Expiratory Pressure (PEP mask) for physiotherapy from Copenhagen that proved to be a popular and effective method of treatment. The mechanics of this method had been evaluated by one of the authors using parts of excised human lungs (Andersen J B et al. Scand J Respir Dis 1979; 60:260-266. [PubMed]. Falk et al studied the acute effects of four different chest physical therapy regimens using a randomised cross-over design in 14 patients with cystic fibrosis. PEP was well accepted by the patients, who preferred treatment with PEP, and the authors suggested PEP be incorporated in chest physical therapy regimens. (Tyrell et al, 1986 below for the first UK study of PEP from Nottingham; also Murray JF. The ketchup-bottle method. [Editorial] N Eng J Med 1979; 300:1155-1157). A trail of PEP from George Davidson’s unit in Vancouver had a significant influence on physiotherapy practice in N. America (McIlwaine PM et al. J Pediatr 1997; 131:506-508.below).
1986 Tyrrell JC, Hiller EJ, Martin J. Face mask physiotherapy in cystic fibrosis. Arch Dis Child 1986; 61:598-611. [PubMed]
This paper was from Dr Joan Hiller’s Paediaitric CF Unit at Nottingham City Hospital. Dr Joan Hiller (figure) founded the Nottingham CF Unit having previously worked in the USA with Dr Nancy Huang in Philadelphia.
This study was coordinated by Dr Jenny Tyrell, then the CF Research Fellow in Nottingham, and evaluated the use of the ‘PEP’ mask with forced expiratory coughing which was compared with conventional physiotherapy over a one month period. No difference was shown in symptom scores, sputum production, or simple lung function tests. The mask was well accepted and allowed independent treatment by older patients.
The PEP mask became a popular method physiotherapy giving some degree of independence to the patient (also Falk et al, 1984 above and many subsequent papers supporting the use of the PEP).
1988 Reisman JJ, Rivington-Law B, Corey M, Marcotte J, Wannamaker E, Levison H J. Role of conventional physiotherapy in cystic fibrosis. Pediatr 1988; 113:632-636. [PubMed]
A frequently quoted paper from Toronto of a 3-year prospective study to compare the long-term effects of postural drainage accompanied by percussion and the forced expiratory technique with the effects of the forced expiratory technique alone. Patients who performed the forced expiratory technique alone had mean annual rates of decline that were significantly different from zero for forced expiratory volume in 1 second (p <0.001), forced expiratory flow between 25% and 75% of vital capacity (p <0.001), and Shwachman clinical score (p< 0.004). In the group performing conventional physiotherapy with percussion and postural drainage, only the mean annual rate of decline for forced expiratory flow between 25% and 75% of vital capacity was significantly different from zero (p<0.03), and it was significantly different from the mean rate of decline associated with the forced expiratory technique alone (p<0.04). The authors concluded that conventional chest physiotherapy should remain a standard component of therapy in cystic fibrosis.
Physiotherapy is a major and time-consuming component of therapy and the worst part of treatment for many patients and parents. This frequently quoted study was one of the few to demonstrate that the time was well spent and so the paper was useful and was quoted widely for this reason (also Pryor et al, 1979 above; also Desmond et al, 1983; Tyrell et al, 1986 below).
1991 Warwick WJ, Hansen LG. The long-term effect of high frequency chest compression therapy on pulmonary complications of cystic fibrosis. Pediatr Pulmonol 1991; 11:265-271. [PubMed]
A high-frequency chest compression (HFCC) device for clearance of mucous secretions from airways was tested in 16 patients with CF with significant improvement in pulmonary function for the HFCC period, which averaged 22 months per patient. The device consists of a variable air pulse delivery system and a non-stretch inflatable vest worn by the patient to cover the entire torso. Ninety-four percent of patients’ regression line slopes for percent predicted forced vital capacity (FVC) and forced expiratory volume in 1 second (FEV1) became more positive during self-administered HFCC therapy as compared to slopes before HFCC therapy, when manual chest physical therapy was used.
Although this device (figure main text) has never found favour amongst physical therapist in the UK, over the next 15 years “the vest” became popular and widely used in North America by some 60% of people with CF and by many others with chronic respiratory disorders. The device has been pioneered by veteran CF centre director Warren Warwick (figure 21 main text) from Minnesota and has been the subject of many subsequent publications showing comparative efficiency with other forms of physiotherapy and improvements with alterations in the wave form created. The first reports on high frequency chest wall compression were from King M et al.(Am Rev Respir Dis 1983; 128:511-515.[PubMed]; Am Rev Respir Dis 1984; 130:703-706.[PubMed]).
1994 Arens R, Gozal D, Omlin KJ, Vega J, Boyd KP, Keens TG, Woo MS. Comparison of high frequency chest compression and conventional physiotherapy in hospitalized patients with cystic fibrosis. Am J Res Crit Care 1994; 150:1154-1157. [PubMed]
A study of 50 people with CF admitted for acute pulmonary exacerbations that were randomly allocated to receive either high frequency chest compression (HFCC) or conventional physiotherapy (CPT) three times a day. After seven and 14 days of treatment, improvements were similar in the two study groups, leading to patient discharge after similar periods of hospitalization.
The authors concluded that HFCC and CPT are equally safe and effective when used during acute pulmonary exacerbations in CF patients. They suggested that HFCC may provide an adequate alternative in management of CF patients in a hospital setting. (Also Warwick WJ, Hansen LG, 1991 above)
1997 Button BM, Heine RG, Catto-Smith AG, Phelan PD, Olinsky A. Postural drainage and gastro-oesophageal reflux in infants with cystic fibrosis. Arch Dis Child 1997; 76:148-150.[PubMed]

Brenda Button
First of series of papers from Brenda Button (figure 43 main text), a physiotherapist from Melbourne, Australia, noting the possible dangers of inhalation when infants with CF were in the head down position during postural drainage; infants with CF were known to have an increased incidence of gastro-oesophageal (GO) reflux. Physiotherapy with and without head down tilt were compared using 24 hour pH oesophageal monitoring. Standard physiotherapy with head down tilt was associated with a significant increase in GO reflux in the infants with CF.
This was an important study and, with Brenda Button’s subsequent publications, certainly had a major influence on the techniques of physiotherapy recommended for CF infants (see also Malfroot & Dab, 1991 above for earlier studies on reflux in CF infants). Button et al, 2004 also confirmed GO reflux as common and important in adults with CF.
1997 McIlwaine PM, Wong LT, Peacock D, Davidson AG. Long-term comparative trial of conventional postural drainage and percussion versus positive expiratory pressure physiotherapy in the treatment of cystic fibrosis. J Pediatr 1997; 131:506-508. [PubMed]

Maggie Mcllwaine
Forty patients were randomised to receive either postural drainage and percussion or PEP mask physiotherapy over one year. Those using the PEP mask had significantly better respiratory function after 1 year and the authors concluded that this was the more effective method of physiotherapy.
This study from Professor George Davidson’s CF centre in Vancouver, Canada had a significant influence on physiotherapy practice in North America. A subsequent study from this unit, comparing PEP and Flutter methods, showed PEP to be superior in maintaining pulmonary function and reducing the need for hospital admissions (McIlwaine et al. J Pediatr 2001; 138:845-850).
2000 Schneiderman-Walker J, Pollock SL, Corey M, Wilkes DD, Canny GJ, Pedder L, Reisman JJ. A randomized controlled trial of a 3-year home exercise program in cystic fibrosis. J Pediatr 2000; 136:304-310. [PubMed]).
To evaluate the effects of a 3-year home exercise program on pulmonary function and exercise tolerance in mildly to moderately impaired patients with CF and to assess whether regular aerobic exercise is a realistic treatment option. An improved sense of well-being was reported with exercise and pulmonary function declined more slowly in the exercise group than in the control group, suggesting a benefit for patients with CF participating in regular aerobic exercise (percentage predicted decline in FVC 2.42 vs. 0.25 and FEV1 3.47 vs. 1.46).
This is one of a number of studies that confirmed exercise was good for people with CF. It was always apparent following patients in the clinic that those people with CF who were very active seemed to remain in better condition which is really not surprising.
2003 Button BM. Heine RG. Catto-Smith AG. Olinsky A. Phelan PD. Ditchfield MR. Story I. Chest physiotherapy in infants with cystic fibrosis: to tip or not? A five-year study. Pediatr Pulmonol 2003; 35:208-213. [PubMed]
There is controversy about the need for postural drainage physiotherapy in asymptomatic infants with cystic fibrosis (CF). In this study Brenda Button and her colleagues compared the effectiveness of standard postural drainage chest physiotherapy (SPT) with a modified physiotherapy regimen without head-down tilt (MPT) in 20 young infants with CF. Patients receiving SPT had more days with upper respiratory tract symptoms than those on MPT (70 +/- 32.8 vs. 37 +/- 24.9 days; P = 0.04) and required longer courses of antibiotics (23 +/- 28.5 vs. 14 +/- 11.2 days; P = 0.05). Chest x-ray scores were similar at diagnosis but were worse at 2(1/2) years for those receiving SPT (P = 0.03). Forced vital capacity and forced expired volume in 1 sec (FEV(1)) at 5-6 years was lower for SPT than for MPT (P < 0.05). In conclusion, MPT was associated with fewer respiratory complications than SPT in infants with CF.
Brenda Button’s work has been largely influential in many physiotherapists omitting the head down position in the physiotherapy recommendations for infants with cystic fibrosis.
2004 Warwick WJ. Wielinski CL. Hansen LG. Comparison of expectorated sputum after manual chest physical therapy and high-frequency chest compression. Biomed Instru Tech 2004; 38:470-475. [PubMed]
Warren Warwick
These results show that sputum production by subjects with CF who receive CPT by certified respiratory therapists can be as great as the sputum produced by the same subjects who receive HFCC. The results also suggest that unknown factors attributed to the therapists may produce different levels of effort from time to time that may decrease the respiratory therapists’ effectiveness, whereas the HFCC therapy may be more consistently effective because it is entirely machine based.
A helpful practical paper from Warren Warwick on the use of the vest compared with manual physiotherapy.
2004 Phillips GE. Pike SE. Jaffé A. Bush A. Comparison of active cycle of breathing and high-frequency oscillation jacket in children with cystic fibrosis. Pediatr Pulmonol 2004; 37:71-75.[PubMed] Comparison of the active cycle of breathing techniques (ACBT) with the Hayek Oscillator Cuirass, performing HFCC on secretion clearance in children with CF during an exacerbation. Ten children (7 males; median age, 14 years; range, 9-16) received either two supervised sessions using HFCC or two self-treatment ACBT sessions in random order on successive days. Baseline pulmonary function was similar prior to treatments. Sputum weight increased significantly with ACBT compared with HFCC during treatment (5.2 g vs. 1.1 g, P < 0.005, morning; 4.1 g vs. 0.7 g, P < 0.01, afternoon). Pulmonary function improved significantly after morning ACBT (forced vital capacity (FVC): 2.67 l to 2.76 l, P < 0.03; forced expiratory volume in 1 sec (FEV1): 1.59 l to 1.62 l, P < 0.03). Following afternoon ACBT, there was a significant increase in FVC (2.64 to 2.79, P < 0.02), but no significant change in FEV1. Pulmonary function did not change at any time following HFCC. Compared with ACBT, HFCC by Hayek Cuirass is not an effective airway clearance treatment modality for children with CF during an infective exacerbation.
These are small numbers and small volumes of sputum. The findings reinforce the lack of enthusiasm from UK physiotherapists for the “vest” which is used by many people with CF in the USA apparently with satisfactory results.
2005 Button BM, Roberts S, Kotsimbos TC, Levvey BJ, Williams TJ, Bailey M, Snell GI, Wilson JW. Gastroesophageal reflux (symptomatic and silent): a potentially significant problem in patients with cystic fibrosis before and after lung transplantation. J Heart Lung Transpl 2005; 24:1522-9.
Gastroesophageal reflux (GER) may contribute to declining lung function both before and after lung transplantation. Twenty-four patients were studied – GER, both symptomatic and silent, is a frequent and significant problem in people with CF after lung transplantation. The advice was that this condition should be aggressively treated and if necessary by surgery if GER persists.
2006 Balfour-Lynn IM, Carr SB, Madge SL. A comparison of prevalence of urinary incontinence in girls. Pediatr Pulmonol 2006; 41:1065-1068.
Another study on urinary incontinence – this time on younger patients. The physiotherapists have taken an increasing interest in bladder dysfunction in cystic fibrosis. Girls with CF aged 11 to 17 years were studied and urinary incontinence was present in 17 (33%) of 51 girls, compared with only 4 (16%) of 25 of those with asthma and 2 (7%) of 27 healthy controls. The problem was associated with increasing severity of lung disease (also in adults with CF Cornacchia et al, 2001 above; Orr A et al. BMJ; 322:1521).
2007 Kempainen RR, Williams CB, Hazelwood A, Rubin BK, Milla CE. Comparison of high-frequency chest wall oscillation with differing waveforms for airway clearance in cystic fibrosis. Chest 2007; 132:1227-1232.
Using the vest device single-session sputum production is comparable with sine and triangular waveform high-frequency chest wall oscillation devices.
There is a steady output of work on the Vest physiotherapy device and although some seems to be related to companies competing for sales, it does seem to be a major advance particularly in convenience for all concerned – particularly the patients. The use of the Vest is one of a number of major differences between treatment in the UK and USA where over 50% of people with CF use the Vest but virtually no patients in the UK use it. Two obvious reasons are the cost of the equipment (£10K in the UK) and the undoubted lack of enthusiasm of UK CF physiotherapists for the technique!
2004 Button BM, Heine RG, Catto-Smith AG, Phelan PD, Olinsky. Chest physiotherapy, gastro-oesophageal reflux and arousal in infants with cystic fibrosis. Arch Dis Child 2004; 89:435-439. [PubMed]
This is similar to Brenda Button’s 1997 study (above) comparing standard physiotherapy (SPT) and modified physiotherapy without the head down position (MPT). The Melbourne team monitored the cardio-respiratory state during the procedures. It was confirmed that more episodes of gastro-oesophageal reflux occurred when the head down position was used; the left lateral position was associated with fewer episodes than the others. There were more episodes in supine and prone in the SPT head down and the infants were more likely to cry. Oxygen saturation was lower in SPT but improved with non-nutritive sucking (i.e. a dummy). The authors concluded that the SPT is associated with gastroesophageal reflux, distressed behaviour and lower oxygen saturation.
These studies certainly influenced the physiotherapy recommendations for CF infants particularly as screened infants often have very little in the way of respiratory secretions to remove, although their respiratory function tests are usually significantly below normal (Ranganathan et al, 2001 above). Not all physiotherapists and paediatricians initially accepted that reflux was increased in the head down position. For example the Brompton CF team in London refuted the need to change physiotherapy routines in infants with CF (Phillips GE et al. Holding the baby: head downwards positioning for physiotherapy does not cause gastro-oesophageal reflux. Eur Resp J 1998; 12:954-957. 9817174).
2005 Button BM, Roberts S, Kotsimbos TC, Levvey BJ, Williams TJ, Bailey M, Snell GI, Wilson JW. Gastroesophageal reflux (symptomatic and silent): a potentially significant problem in patients with cystic fibrosis before and after lung transplantation. J Heart Lung Transpl 2005; 24:1522-9. [PubMed]
Gastroesophageal reflux (GER) may contribute to declining lung function before and after lung transplantation. Twenty-four patients were studied. GER, both symptomatic and silent, is a frequent and significant problem in people with CF after lung transplantation. The advice was that this condition should be aggressively treated and if necessary by surgery if GER persists.
2005 Barak A, Wexler ID, Efrati O, Bentur L, Augarten A, Mussaffi H, Avital A, Rivlin J, Aviram M, Yahav Y, Kerem E. Trampoline use as physiotherapy for cystic fibrosis patients. Pediatr Pulmonol 2005; 39:70-73. [PubMed]
Physicians and physiotherapists who care for CF patients have recommended the use of trampolines as a methods of improving cardiopulmonary performance, encouraging sputum production, and improving general well-being. Despite some therapeutic and recreational benefits associated with trampoline use, papers in the paediatric literature mostly document an increased incidence of injuries, ranging from minor trauma to spinal cord injuries and even death!
This review examined the accumulated published data regarding the use of trampolines, to assess their potential contributions and disadvantages for CF patients, and to define whether trampoline use should be recommended. There were approximately 60 articles that primarily dealt with trampolines, out of which only two dealt with CF. Unfortunately most of these articles are reports pertaining to injuries related to the use of trampolines, with only a few describing the medical, physiologic, and/or psychological benefits of trampolines.
Based on the accumulated data, the presumed benefits of trampoline use for CF patients are not proven. Furthermore, the suggested benefits could be acquired using other types of exercise. Weighing the known definite risks of trampolines against the potential benefits that are not unique to this modality suggests that the use of trampolines for CF should not be recommended. In fact the main outcome of trampoline use appeared to be injury!! Subsequently support came from Ireland where daily trampoline use in half the patients had resulted in no injuries requiring medical treatment (Currant & Mahony, 2008). [PubMed]
2005 Dodd ME. Prasad SA. Physiotherapy management of cystic fibrosis. Chron Respir Dis 2005; 2:139-149. [PubMed]
This is a review by Mary Dodd (figure) and Armmani Prasad (figure) recognised experts on the subject. They notes that “for many years physiotherapy for cystic fibrosis (CF) was synonymous with a daily routine of postural drainage and percussion. Improved longevity and a desire for independence, together with a clearer understanding of the pathophysiology of the disease, has led to the development of many airway clearance techniques. The contribution of ‘chest’ physiotherapy remained unchallenged until recent times when lack of robust evidence and the presentation of asymptomatic infants and adults led some physiotherapists to question this traditional approach. As survival increases into the fourth and fifth decade unique complications have evolved and physiotherapy management is challenged with non-respiratory aspects of treatment. This review considers the evidence for, and current practice of airway clearance, the value of exercise and the emerging problems of musculoskeletal complications and urinary incontinence.
Mary Dodd (figure) is consultant physiotherapist in the Manchester Adult CF centre. She was the co-founder along with Prof. Kevin Webb of the Bradbury Adult CF Centre in Manchester. Mary has been closely involved in CF clinical care and research for many years since starting working with CF with the late Dr Holzel in Manchester. She has published on most aspects of physiotherapy for people with CF and is a leading authority on the subject both in the UK and internationally.
2006 Prasad SA, Balfour-Lynn IM, Carr SB, Madge SL. A comparison of prevalence of urinary incontinence in girls with cystic fibrosis, asthma and healthy controls. Pediatr Pulmonol 2006; 41:1065-1068. [PubMed]
Another study on urinary incontinence – this time on younger patients. In recent years the physiotherapists have

Ammani Prasad
taken an increasing interest in bladder dysfunction in CF. Girls with CF aged 11 to 17 years were studied and urinary incontinence was reported by 17/51 (33%) girls, compared with only 4/25 (16%) of those with asthma and 2/27 (7%) healthy controls. The problem was associated with increasing severity of lung disease. (also described in adults with CF by Cornacchia et al, 2001 above; Orr A et al. BMJ; 322:1521).
Armmani Prasad is the senior Physiotherapist at the CF Unit Great Ormond Street Hospital for Children, London and one the leading CF physiotherapists in the UK and internationally. She has written extensively on CF and also been an invited speaker at many conferences both in the UK and abroad and regularly advises the CF Trust on matters relating to CF care. She is now also manager of the Great Ormond Street CF centre.
2007 Kempainen RR, Williams CB, Hazelwood A, Rubin BK, Milla CE. Comparison of high-frequency chest wall oscillation with differing waveforms for airway clearance in cystic fibrosis. Chest 2007; 132:1227-1232. [PubMed] Using the vest device, single-session sputum production is comparable with the sine and the triangular waveform high-frequency chest wall oscillation devices.
There is a steady output of work on the various physiotherapy vest devices and although some seems to be related to companies competing for sales, it does seem to be a major advance particularly in convenience for all concerned. The use of the Vest is one of a number of major differences between treatment in the UK and USA where over 50% of people with CF use the Vest in contrast to the very few in the UK. Two obvious reasons are the cost of the equipment (approximately £10K in the UK) and the undoubted lack of enthusiasm of UK CF physiotherapists for the technique!
2008 Prasad SA, Main E, Dodd ME; Association of Chartered Physiotherapists. Finding consensus on the physiotherapy management of asymptomatic infants with cystic fibrosis. Pediatr Pulmonol 2008; 43:236-244. [PubMed]
This study aimed to provide expert consensus regarding the physiotherapy management of asymptomatic infants with CF using a Delphi consensus method. Twenty-five senior paediatric physiotherapists from Specialist CF Centres throughout the UK participated in the study. Consensus was high but consensus could not be achieved on whether routine daily chest physiotherapy is necessary in ‘asymptomatic’ babies. An agreed amendment to the original statement allows professionals to modify or change traditional practice with the sanction of their senior colleagues.
There had been a considerable amount of discussion as to the practice of tipping infants which Brenda Button and colleagues from Melbourne found caused oesophageal reflux in a significant proportion.
2009 Flume PA, Robinson KA, O’Sullivan B, Finder JD, Vender RL, Willey-Courand DB, White TB, Marshall BC. Cystic fibrosis pulmonary guidelines: airway clearance therapies. Clinical Practice Guidelines for Pulmonary Therapies Committee. Respiratory Care 2009; 54:522-537.[PubMed]
A CF Foundation committee found no evidence that one method of airway clearance was superior to the others and although the evidence for benefit was not strong, recommended daily airway clearance be performed and regular exercise taken by all patients.
A number of studies have failed to show one method of airway clearance better than the others although physiotherapy is better than no physiotherapy.
2009 Heijerman H. Westerman E. Conway S. Touw D. Döring G. Consensus working group. Inhaled medication and inhalation devices for lung disease in patients with cystic fibrosis: A European consensus. J Cyst Fibros 2009; 8:295-315. [PubMed]
In this European consensus document the authors review the current status of inhaled medication in CF, including the mechanisms of action of the various drugs, their modes of administration and indications, their effects on lung function, exacerbation rates, survival and quality of life, as well as side effects.
A detailed consensus document with no less than 249 references.
2010 Mislaying M, Wong LT, Chillers M, Davidson GF. Long-term comparative trial of two different physiotherapy techniques; postural drainage with percussion and autogenic drainage, in the treatment of cystic fibrosis. Pediatr Pulmonol 2010; 45:1064-1069. [PubMed]
In N. America, over the past decade, various airway clearance techniques (ACT) have been introduced for the treatment of cystic fibrosis (CF). These Canadian authors hypothesized that autogenic drainage (AD), an ACT developed in Belgium, would be as effective as postural drainage with percussion (PD) in treating patients with CF. They were similar similar but the patients preferred the autogenic drainage as 10 of 17 receiving autogenic drainage refused to change to postural drainage after a year.
2010 Osman LP, Roughton M, Hodson ME, Pryor JA. Short-term comparative study of high frequency chest wall oscillation and European airway clearance techniques in patients with cystic fibrosis. Thorax 2010; 65:196-200. [PubMed]
High frequency chest wall oscillation (HFCWO) is standard treatment for airway clearance in the USA and has recently been introduced in the UK and Europe. There is little published research comparing HFCWO with airway clearance techniques (ACTs) frequently used in the UK and Europe.
The aim of this study was to compare the short-term effects of HFCWO with usual ACTs in patients with cystic fibrosis hospitalised with an infective pulmonary exacerbation. A 4-day randomised crossover design was used. Patients received either HFCWO on days 1 and 3 and usual ACTs on days 2 and 4 or vice versa. Wet weight of sputum, spirometry and oxygen saturation were measured. Perceived efficacy, comfort, incidence of urinary leakage and preference were assessed. Data were analysed by mixed model analysis.
RESULTS: 29 patients (72% male) of mean (SD) age 29. 4 (8. 4) years and mean (SD) forced expiratory volume in 1 s (FEV(1)) percentage predicted (FEV(1)%) 38 (16. 7) completed the study. Significantly more sputum was expectorated during a single treatment session and over a 24 h period (mean difference 4. 4 g and 6. 9 g, respectively) with usual ACTs than with HFCWO (p<0. 001). No statistically significant change in FEV(1)% or oxygen saturation was observed after either HFCWO or usual ACTs compared with baseline. 17 patients (55%) expressed a preference for their usual ACT. The authors concluded during both a finite treatment period and over 24 h, less sputum was cleared using HFCWO than usual ACT. HFCWO does not appear to cause any adverse physiological effects and may influence adherence.
This study from the Royal Brompton exemplifies the lack of enthusiasm for the HFCWO method shown by UK physiotherapists!!! The fact that that the majority of US patients use HFCWO and virtually no UK patients do is interesting. Undoubtedly the cost of the apparatus (c. £10,000) is a major deterrent – presumably a cost shouldered by the medical insurance in the USA; also the lack of enthusiasm of the UK physiotherapists is another significant factor. Certainly individual UK patients who have used “the vest” at home have been quite enthusiastic.
2010 Denyer J, Prince I, Dixon E, Agent P, Pryor J, Hodson M. Evaluation of the Target Inhalation Mode (TIM) breathing maneuver in simulated nebulizer therapy in patients with cystic fibrosis. J Aero Med Pulmon Drug Deliver 2010; 23 Suppl 1:S29-36. [PubMed]
Adaptive Aerosol Delivery (AAD) systems provide efficient drug delivery and improved lung deposition over conventional nebulizers by combining real-time analyses of patient breathing patterns and precisely timed aerosol delivery. Delivery and deposition are further enhanced by breathing techniques involving slow, deep inhalations.
This exploratory study assessed the acceptability of slow, deep inhalations in 20 patients with cystic fibrosis (CF) during up to eight simulated nebulizer treatments with the I-neb AAD System. The breathing maneuver, Target Inhalation Mode (TIM) breathing, involved the lengthening of the patient’s inhalation time over successive breaths with guidance from auditory and tactile (vibratory) feedback from the device.
At the end of the first treatment, most patients felt that the instructions were easy to understand (90%) and that the vibratory feedback was pleasant (65%). Half of the patients found the procedure to be comfortable. At the end of the final treatment, most patients felt that the breathing maneuver was easy to understand (90%) and use (80%), but that the duration of the breath was too long (100%). Logged data revealed that 90% of patients were able to comply with the breathing maneuver. The two patients unable to comply had a forced vital capacity of <1.75 L. The average treatment time decreased from 288.4 to 141.6 sec during the first and final treatments, respectively.
The authors conclude that their study provides preliminary evidence of the acceptability of the TIM breathing maneuver in patients with CF and their ability to perform repeated TIM breathing during simulated nebulizer therapy with the I-neb AAD System.
The Adaptive Aerosol is another advance in making routine inhalation therapy more acceptable to patients by increasing efficiency and reducing time spent.
2011 Association of Chartered Physiotherapists in Cystic Fibrosis (ACPCF) “Standards of Care and Good Clinical Practice for Physiotherapy Management Cystic Fibrosis” edited by Penney Argent, Lisa Morrison and Ammani Prasad

Lisa Morrison

Penney Argent
This is an excellent review of the subject and available on the CF Trust website (www.cysticfibrosis.org.uk) or the ACPCF website (www.csp.org.uk/professional-networks/acpcf).
Penney Argent (figure) is deputy Director of Rehabilitation and Therapies at the Royal Brompton and Harefield Hospitals, London and a professional lead for physiotherapy.Her directorate has about 100 staff members and includes an adult cystic fibrosis team.
Lisa Morrison (figure) has worked in cystic fibrosis for the past 19 years, first at the Regional CF Centre in Leeds with the last 12 as Clinical Specialist Physiotherapist in the adult CF centre at the Gartnavel Hospital Glasgow. She is particularly interested in exercise management and has presented locally and nationally on this topic. Lisa is involved both nationally and internationally with various aspects of CF physiotherapy.
Ammani Prasad (figure in 2006). Following qualification Ammani specialised in paediatric respiratory care, working extensively in the fields of paediatric intensive care and paediatric respiratory medicine, particularly cystic fibrosis. More recently Ammani has been involved in coordinating the work within the Cystic Fibrosis Unit at GOSH. She is extensively involved in joint work with the Cystic Fibrosis Trust and Department of Health regarding clinical pathways, commissioning of cystic fibrosis care and Peer Review. She now manages the Cystic Fibrosis Unit at GOSH.
2011 McCormack P, McNamara PS, Southern KW. A randomised controlled trial of breathing modes for adaptive aerosol delivery in children with cystic fibrosis. J Cyst Fibros 2011;. 10:343-349. [PubMed]
Modern nebulisers have reduced treatment times by utilising mesh technology for aerosol production. A further modification (target inhalation mode (TIM)) that may reduce treatment delivery times further. Following a baseline period on tidal breathing mode (TBM), children with CF on long-term aerosol therapy were randomly allocated to either TIM, which optimises patient inhalations through a direct feedback mechanism, or to continue TBM. The primary outcome was nebuliser treatment times with secondary outcomes being adherence and patient preference.
The ten children allocated TIM reduced their mean (SD) treatment times from 6.9(2.9) to 3.7(2.3) minutes (p<0.001). In contrast, treatment times were unchanged in the ten children allocated TBM. Mean adherence was maintained in the TIM group but declined in patients allocated TBM by >5%. All children preferred TIM to TBM.
The authors concluded that TIM reduces nebuliser treatment times and may positively impact on adherence, although longer duration studies are required to examine this.
This seems to be a definite advance in improving the efficiency and acceptability of inhalation therapy which is central to modern treatment of CF. Previous evaluation in adults with CF also provided evidence of acceptability and efficacy (Denyer J et al. J Aerosol Med Pulm Drug Deliv 201023 Suppl 1:S29-S36). [PubMed]
2011 Coates AL, Green M, Leung K, Chan J, Ribeiro N, Ratjen F, Charron M. A comparison of amount and speed of deposition between the PARI LC STAR nebulizer and an investigational eFlow nebulizer. J aeros med pulmon drug del 2001; 24:157- 163. [PubMed]
The potency and physical properties of many of the drugs used in the treatment of cystic fibrosis necessitates the use of nebulization, a relatively time-consuming pulmonary delivery method. Newer, faster and more efficient delivery systems are being proposed. The purposes of this study was to compare the length of time it took to deliver the equivalent of normal saline nebulized for 10 min in a PARI LC STAR nebulizer to that of an investigational PARI eFlow.The investigational eFlow delivered 8.6 +/- 1.0 mg, approximately 90% of the lung dose compared to the LC STAR , 9.6 +/- 1.0 mg, but did in less than half the time (p < 0.02 for both). There were no differences in central versus peripheral distribution for either device. The authors concluded the investigational eFlow was both faster and more efficient than the LC STAR nebuliser.
One of many studies from Professor Coates and his colleagues at Toronto aimed at improving the efficiency of inhalation therapy in people with CF confirming the superiority of the eFlow nebuliser.
2012 O’Clock GD. Lee YW. Lee J. Warwick WJ. High-frequency and low-frequency chest compression: effects on lung water secretion, mucus transport, heart rate, and blood pressure using a trapezoidal source pressure waveform. IEEE Transactions on Biomedical Engineering 2012; 59:106-114. [PubMed]
High-frequency chest compression (HFCC), using an appropriate source (pump) waveform for frequencies at or above 3 Hz, can enhance pulmonary clearance for patients with cystic fibrosis (CF) and chronic obstructive pulmonary disease (COPD). Using a trapezoidal HFCC source pressure waveform, secretion of water from epithelial tissue and transport of mucus through lung airways can be enhanced for patients with CF and COPD. At frequencies below 3 Hz, low-frequency chest compression (LFCC) appears to have a significant impact on the cardiovascular system. For a trapezoidal source pressure waveform at frequencies close to 1 Hz, LFCC produces amplitude or intensity variations in various components of the electrocardiogram time-domain waveform, produces changes at very low frequencies associated with the electrocardiogram frequency spectra (indicating enhanced parasympathetic nervous system activity), and promotes a form of heart rate synchronization. It appears that LFCC can also provide additional cardiovascular benefits by reducing peak and average systolic and diastolic blood pressure for patients with hypertension
The latest publication from Warren Warwick and colleagues. High frequency chest compression which Warren described in the earl Nineties has been validated in a number of studies and is now widely used particularly in the USA. Now here is evidence of additional cardiovacular effects.
2013 Bradley JM, Blume SW, Balp MM, Honeybourne D, Elborn JS. Quality of life and healthcare utilisation in cystic fibrosis: a multicentre study. Eur Respir J 2013; 41:571-7.[PubMed]

Judy Bradley
The aim of this study was to discover the health status and healthcare utilisation associated with pulmonary exacerbations in cystic fibrosis (CF) and chronic Pseudomonas aeruginosa infection.
Patients with CF from five UK CF centres attended two visits, 8-12 weeks apart. They were classified at visit 1 as being in one of the three health states: no current pulmonary exacerbation; “mild” (no hospitalisation) pulmonary exacerbation; and “severe” (hospitalisation) pulmonary exacerbation. All patients completed the Cystic Fibrosis Questionnaire-Revised (CFQ-R) and EuroQol (EQ-5D) and a clinical form, and forced expiratory volume in 1 s (FEV1) was measured at visits 1 and 2. Annual healthcare utilisation data were collected. 94 patients of mean±sd age 28.5±8.2 yrs and FEV1 58.7±26.8% were recruited. 60 patients had no pulmonary exacerbation, 15 had a mild and 19 had a severe pulmonary exacerbation at visit 1. EQ-5D and CFQ-R data showed that the worse the exacerbation, the poorer the health-related quality of life (HRQoL). There were strong relationships between the CFQ-R and EQ-5D domain scores. The mean rate of pulmonary exacerbations per patient per year was 3.6 (1.5 in hospital and 2.2 at home). The mean length of stay per hospital pulmonary exacerbation was 9 days. As exacerbation status worsens, patients experience worse HRQoL. The authors confirmed that there is a significant healthcare burden associated with treatment of pulmonary exacerbation and long-term prophylaxis.
Judy Bradley (figure) is Professor of Physiotherapy at the University of Ulster. She has had a distinguished career in respiratory diseases particularly cystic fibrosis both nationally and internationally. She was presented with the Award of Distinguished Research Fellowship by the University in 2004 in recognition of her contribution to research in the area of respiratory physiotherapy. She was subsequently promoted to a Reader Joint Appointment at the University of Ulster/Belfast Health and Social Care Trust in 2005 and Professor in 2013.
2013 Kriemler S. Kieser S. Junge S. Ballmann M. Hebestreit A. Schindler C. Stussi C. Hebestreit H. Effect of supervised training on FEV1 in cystic fibrosis: a randomised controlled trial. J Cyst Fibros 2013; 12:714-720. [PubMed] A study to determine the positive effects of long-term exercise training on FEV1. 39 Swiss patients with CF were randomly divided into strength training (ST, n=12), endurance training (AT, n=17) and controls (CON(CH), n=10), and also compared with age-matched Swiss (n=35) and German (n=701) CF registry data. A partially supervised training of 3×30 min/week for 6 months took place with measurements at baseline and after 3, 6, 12 and 24 months. Primary outcome was FEV1 at 6 months.
The FEV1 increased significantly in both training groups compared with the controls (AT:+5.8+0.95, ST:+7.4+2.5, CON(CH):-11.5+2.7% predicted, p<0.001) and both registry groups at 6 months. At 24 months, changes in favour of the training groups persisted marginally compared with controls, but not compared with registry data.
The authors concluded partially supervised training over 6 months improved FEV1 but effects were basically gone 18 months off training. They suggest regular long-term training should be promoted as essential part of treatment in CF.
2013 Ledger SJ. Owen E. Prasad SA. Goldman A. Willams J. Aurora P. A pilot outreach physiotherapy and dietetic quality improvement initiative reduces IV antibiotic requirements in children with moderate-severe cystic fibrosis. J Cyst Fibros 2013; 12:766-772.[PubMed]
The current model of care for children with moderate-severe CF is focused on intensive inpatient intervention, regular outpatient clinic review and specialist outreach care as required. An alternative model providing more regular physiotherapy and dietetic outreach support, in addition to these specialist services, may be more effective. Introduction of such a policy resulted in a 23% reduction in inpatient IV antibiotic requirement and 20% reduction in home IV antibiotic requirement during the intervention year. The authors concluded that this pilot programme demonstrated a reduction in IV and admission requirements with a cost benefit in a small group of children with moderate-severe CF.
The confirmation of benefit from this more intensive approach is to be expected and welcome. It is doubtful if such a finding would warrant a full scale trial however.
2013 McIlwaine MP. Alarie N. Davidson GF. Lands LC. Ratjen F. Milner R. Owen B. Agnew JL. Long-term multicentre randomised controlled study of high frequency chest wall oscillation versus positive expiratory pressure mask in cystic fibrosis. Thorax 2013; 68:746-751. [PubMed]
Positive expiratory pressure (PEP) is the most commonly used method of airway clearance (AC) in Canada for patients with cystic fibrosis (CF) whereas, in some countries, high frequency chest wall oscillation (HFCWO) is the preferred form of airway clearance. There have been no long-term studies comparing the efficacy of HFCWO and PEP in the CF population. This study was to determine the long-term efficacy of HFCWO compared with PEP mask therapy in the treatment of CF as measured by the number of pulmonary exacerbations (PEs). A randomised controlled study was performed in 12 CF centres in Canada. After a 2-month washout period, subjects were randomised to perform either HFCWO or PEP mask therapy for 1 year.
RESULTS: 107 subjects were enrolled in the study; 51 were randomised to PEP and 56 to HFCWO. There were 19 dropouts within the study period, of which 16 occurred prior to or at the time of randomisation. There were significant differences between the groups in the mean number of PEs (1.14 for PEP vs 2.0 for HFCWO) and time to first PE (220 days for PEP vs 115 days for HFCWO, p=0.02). There was no significant difference in lung function, health-related quality of life scores or patient satisfaction scores between the two groups. PEP mask therapy required a shorter treatment time.
The results of this study favour PEP and do not support the use of HFCWO as the primary form of AC in patients with CF. Apparently the previous study on PEP from Vancouver by Maggie McIlwaine and her colleagues had a major influence on the introduction of the PEP mask into N. America (McIlwaine PM et al. J Pediatr 2001; 138:845-850. [PubMed]).
2014 Schneiderman JE, Wilkes DL, Atenafu EG, Nguyen T, Wells GD, Alarie N, Tullis E, Lands LC, Coates AL, Corey M, Ratjen F. Longitudinal relationship between physical activity and lung health in patients with cystic fibrosis. Eur Respir J. 2014 Mar;43(3):817-23. doi: 10.1183/09031936.00055513. Epub 2013 Oct 31. [PubMed] Free full text
Exercise is beneficial for patients with cystic fibrosis (CF) but long-term effects of physical activity on lung function evolution are unknown. We evaluated the longitudinal relationship between changes in habitual physical activity (HPA) and rate of decline in lung function in patients with CF. We tracked HPA using the Habitual Activity Estimation Scale, forced expiratory volume in 1 s (FEV₁) and Stage I exercise tests in 212 patients with CF over a 9-year period. Adjusting for sex, baseline age and FEV₁, mucoid Pseudomonas aeruginosa and CF-related diabetes, mean ± sd FEV₁ % predicted decreased by 1.63 ± 0.08% per year (p<0.0001) while mean ± sd HPA increased by 0.28 ± 0.03 h·day(-1) per year (p<0.0001) over the study period. A greater increase in HPA was associated with a slower rate of decline in FEV₁ (r=0.19, p<0.0069). Dividing subjects into “high” and “low” activity (above or below the mean rate of change of activity, respectively), a steeper rate of FEV₁ decline was observed for low (-1.90% per year) compared to high (-1.39% per year) (p=0.002). Increases in HPA are feasible despite progression of lung disease and are associated with a slower rate of decline in FEV₁, highlighting the benefit of regular physical activity, and its positive impact on lung function in patients with CF.
2015 Doumit M; Jaffe A. Use of the Lung Flute for sputum induction in children with cystic fibrosis: a pilot study. Pediatr Pulmonol 2015; 50(4):340-3. [PubMed]
This study aimed to assess the effectiveness of the Lung Flute in obtaining a sputum sample from children with cystic fibrosis (CF) that were not productive of sputum with coughing alone. Children attending an outpatient CF clinic who were not able to provide a sample with coughing alone were eligible. Each child used the Lung Flute on two occasions at least one month apart. The primary outcome was expectoration of a sputum sample. The authors found the lung flute to be clinically useful and an easy device for sputum induction in children with CF. They suggested further research comparing its effectiveness to other sputum induction methods is warranted.
– The lung flute is a medical device used to clear mucus from congested lungs with low-frequency sound waves. The device consists of a mouthpiece and a plastic reed which vibrates within a chamber to create sound waves in the chest cavity. These sound waves vibrate and break up mucus deposits in the lungs, allowing cilia to more easily move these deposits from the lungs to the throat. The lung flute was granted approval by the FDA in 2010 for use in patients with chronic obstructive pulmonary disease
2015 Freitas DA; Dias FA; Chaves GS; Ferreira GM; Ribeiro CT; Guerra RO; Mendonca KM. Standard (head-down tilt) versus modified (without head-down tilt) postural drainage in infants and young children with cystic fibrosis. Cochrane Database of Systematic Reviews. 3:CD010297, 2015. [PubMed]
Postural drainage is used primarily in infants with cystic fibrosis from diagnosis up to the moment when they are mature enough to actively participate in self-administered treatments. However, there is a reported risk of gastroesophageal reflux associated with this technique. The authors eventually concluded that the use of a postural regimen with a 30 degree head-up tilt is associated with a lower number of gastroesophageal reflux episodes and fewer respiratory complications in the longterm. The 20 head-down postural drainage position was not found to be significantly different from the 20 head-up tilt modified position. Nevertheless, the fact that the majority of reflux episodes reached the upper oesophagus should make physiotherapists carefully consider their treatment strategy.
– There have been a number of publications on the most suitable form of physiotherapy for infants and young children since Brenda Button’s first important report of the head down position causing more frequent episodes of oesophageal reflux (Button BM et al, 1997.[PubMed]). In 2008, 25 senior physiotherapists from the Association of Chartered Physiotherapists in the UK were unable to reach a consensus on the need for physiotherapy in asymptomatic CF infants (Prasad SA et al, 2008). Recent Standards from the UK CF Trust advise, “If gastro-oesophageal reflux has been identified consider using modified postural drainage avoiding a head down tilt” (Agent P, Morrison L, Prasad A, last updated 2013). (See also Topics -> Physiotherapy). In practice experienced physiotherapists use their clinical judgment in each individual infant conscious of the fact that GO reflux is a a possibility.
2015 Sawicki GS, Chou W, Raimundo K, Trzaskoma B, Konstan MW. Randomized trial of efficacy and safety of dornase alfa delivered by eRapid nebulizer in cystic fibrosis patients. J Cyst Fibros. 2015 Nov;14(6):777-83. doi: 10.1016/j.jcf.2015.04.003. Epub 2015 Apr 25. [PubMed]
Efficacy and safety of dornase alfa via an electronic nebulizer with vibrating membrane technology have not been formally assessed in randomized clinical trials. 87 CF patients (≥6years) were randomized in a crossover study to receive dornase alfa 2.5mg/d in 2-week periods with the Pari eRapid and Pari LC Plus jet nebulizers. The primary end point was comparison of forced expiratory volume in the first second. Safety, quality of life, and treatment satisfaction/preference were also compared between devices.
Lung function was equivalent between nebulizers. Most domain scores from the Cystic Fibrosis Questionnaire-Revised and Treatment Satisfaction Questionnaire for Medication instruments were similar but patients strongly preferred the eRapid. Mean patient-reported administration times were shorter with the eRapid vs the LC Plus (2.7 vs 10.2min). Adverse events were similar between devices.
Administration of dornase alfa via the eRapid nebulizer resulted in comparable efficacy and safety, shorter nebulization times, and higher patient preference.
2016 Button BM, Wilson C, Dentice R,et al. Physiotherapy for cystic fibrosis in Australia and New Zealand: A clinical practice guideline. Respirology. 2016 May;21(4):656-67. doi: 10.1111/resp.12764. Epub 2016 Apr 18. [PubMed] Free PMC Article
The aim of this guideline is to optimise the physiotherapy management of people with CF in Australia and New Zealand. A systematic review of the literature in key areas of physiotherapy practice for CF was undertaken. Recommendations were formulated based on National Health and Medical Research Council (Australia) guidelines and considered the quality, quantity and level of the evidence; the consistency of the body of evidence; the likely clinical impact; and applicability to physiotherapy practice in Australia and New Zealand.
A total of 30 recommendations were made for airway clearance therapy, inhalation therapy, exercise assessment and training, musculoskeletal management, management of urinary incontinence, managing the newly diagnosed patient with CF, delivery of non-invasive ventilation, and physiotherapy management before and after lung transplantation. These recommendations can be used to underpin the provision of evidence-based physiotherapy care to people with CF in Australia and New Zealand.
– This is a comprehensive review of physiotherapy for CF in Australia and New Zealand and the free article is a valuable review of present best practice.
2016 Dentice RL; Elkins MR; Middleton PG; Bishop JR; Wark PA; Dorahy DJ; Harmer CJ; Hu H; Bye PT. A randomised trial of hypertonic saline during hospitalisation for exacerbation of cystic fibrosis. Thorax. 71(2):141-7, 2016 Feb. [PubMed] To determine the effects of hypertonic saline inhalation during hospitalisation for exacerbation of CF. 132 adults with an exacerbation of CF were randomised to inhale three nebulised doses a day of either 4 mL 7% saline or a taste-masked control of 0.12% saline, throughout the hospital admission. The primary outcome measure was length of hospital stay.The authors concluded the addition of hypertonic saline to the management of a CF exacerbation did not reduce the length of hospital stay but hypertonic saline speeds the resolution of exacerbation symptoms and allows patients to leave hospital with greater symptom resolution.
– The authors do not state whether they have adopted the use of hypertonic saline as part of their regime for treating pulmonary exacerbations; they suggest that other centres should examine the possibility.
2017 Barry PJ, Flume PA*. Bronchodilators in cystic fibrosis: a critical analysis. Expert Rev Resp Med 11(1):13-20, 2017 Jan.[Pubmed] The use of bronchodilators in CF remains commonplace “despite the lack of solid evidence”. The authors suggest further studies should define key endpoints to determine a role for bronchodilators in light of a substantial treatment burden endured by people with CF.
– It would seem sensible to use N=1 test and, with the patient, judge if they are obtaining benefit. Do we really need a trial for everything?
2016 Lee AL; Rawlings S; Bennett KA; Armstrong D. Pain and its clinical associations in individuals with cystic fibrosis: A systematic review. Chro Respir Dis 13(2):102-17, 2016 May.[Pubmed]

Ann Marie Lee
Pain is recognized as a clinical complication in cystic fibrosis (CF), but the prevalence, characteristics and clinical associations of this co-morbidity have not been systematically reviewed. Electronic searches of six databases were performed. The pooled prevalence of pain in adults with CF was 77% (95% confidence interval (CI): 57%-92%) and in children was 42% (95% CI: 0%-91%). Common regions of pain included back, abdomen, chest and limbs. In children and adults, pain was associated with a poorer quality of life (QOL) and significant interference with treatments.
Pain is a surprisingly common problem in both children and adults with CF. It has negative clinical associations with QOL and the ability to successfully undertake treatment.
Anne Marie Lee (figure) is post doctoral research fellow at West Park Healthcare Centre Canada. She is a physiotherapist and has published extensively on co-morbidities in chronic respiratory disorders.
2017 Ranganathan SC, Hall GL, Sly PD, Stick SM, Douglas TA; Australian Respiratory Early Surveillance Team for Cystic Fibrosis (AREST-CF). Early Lung Disease in Infants and Preschool Children with Cystic Fibrosis. What Have We Learned and What Should We Do about It? Am J Respir Crit Care Med. 2017 Jun 15;195(12):1567-1575. doi: 10.1164/rccm.201606-1107CI.[Pubmed]
The past decade has seen significant advances in understanding of the pathogenesis and progression of lung disease in cystic fibrosis (CF). Pulmonary inflammation, infection, and structural lung damage manifest very early in life and are prevalent among preschool children and infants, often in the absence of symptoms or signs. Early childhood represents a pivotal period amenable to intervention strategies that could delay or prevent the onset of lung damage and alter the longer-term clinical trajectory for individuals with CF. This review summarises what we have learned about early lung disease in children with CF and discusses the implications for future clinical practice and research.
– This is an excellent article reviewing the present situation regarding the need for more effective early monitoring and treatment to prevent the development of bronchiectasis in up to 80% of children by the age of 5 years with the long-term consequences. The author considers an “attitudinal change within CF clinics in important with increased attention of the early years in the establishment of lung disease’ with “policies and guidelines that lead to a more unified proactive approach care in asymptomatic and apparently healthy young children rather than an acceptance of a casual or reactive approach”.
The author discuses in some detail the options which are already available multidisciplinary care at a CF centre modifiable psychological risk factors, home treatment, and adherence. Antibiotics for CF pathogens detected in both symptomatic and asymptomatic individuals. Early eradication of of P. aeruginosa. Mucolytic and the anti-inflammatory actions of macrolides and antibiotics targeting eradication of S. aureus and H. influenzae even in the absence of symptoms. Bronchoscopy is indicated when response to treatment is suboptimal. Introduction of mucolytics at an early stage. Nutritional strategies for the rapid regain of birth weight and normalising fat-soluble vitamin levels. Increased frequency of clinical review and a lower threshold for intensive multidisciplinary review and a lower threshold for admissions for intensive multidisciplinary therapy. He then discusses moving treatments into the preschool period and assessing the CFTR modulators in young children.
Associate Professor Sarath Ranganathan is a full-time specialist in paediatric respiratory medicine and director of Respiratory Medicine at the Royal Melbourne Children’s Hospital. He is an expert in the field of clinical respiratory physiology and early lung disease.
2017 Weir E; Burns PD; Devenny A; Young D; Paton JY. Cardiopulmonary exercise testing in children with cystic fibrosis: one centre’s experience. Arch Dis Child 102(5):440-444, 2017 May. [Pubmed] While exercise testing is increasingly used as a prognostic indicator in cystic fibrosis (CF), it is reported to be underused in UK CF centres, particularly in children. Here, the authors evaluated the cardiopulmonary exercise testing (CPET) results in children and young people with CF at CF annual review and its possible clinical value.
An observational study comparing CPET results using a cycle ergometer ramp test (peak oxygen uptake (Vo2peak)) and pulmonary function (forced expiratory volume in 1 s (FEV1)) was performed with body mass index (BMI) used as a disease severity marker. Data were identified from clinical case notes and our CF database. Thirty-eight children and young people (mean age 11+/-2.4, range 7-14 years; 17 males and 21 females) completed at least one CPET with 95% achieving technically satisfactory tests allowing measurement of Vo2peak. Mean Vo2peak was 107 +/-17.6% predicted, range 74%-150% predicted, with 8% having a reduced Vo2peak of <85% of predicted. Mean FEV1 z-score was -0.77+/-1.24, range -4.42 to 2.24. We did not demonstrate a significant correlation between Vo2peak % predicted and FEV1 z-score (r=0.25, p=0.13), or between Vo2peak % predicted and BMI z-score (r=-0.05, p=0.77).Twenty-eight of 38 completed a second CPET the following year with 71% showing a decline in Vo2peak (mean decline of 8% of predicted value, equivalent to 3.8 mL/kg/min).
The authors concluded that CPET is feasible with 95% of children and young people achieving technically satisfactory assessments starting from age 7. In this group with relatively mild CF, mean Vo2peak was normal with no significant correlation between Vo2peak and FEV1 or BMI, as markers of disease severity. The majority demonstrated a normal Vo2peak. However, 71% showed a downward trend on repeat testing 12-18 months later.
– It is true there that formal exercise testing is not a routine in most paediatric CF centres. In the present study, the majority of the children and young people with CF had BMI and pulmonary function within the normal range. The majority also had Vo2peak measurements within the normal range although most showed a decline in Vo2peak over time. The authors state it remains to be shown if these declines are clinically significant or are part of normal biological variation. The paper provides a useful review of the subject but certainly would not encourage one to add exercise testing to the already crowded routine for children with CF.
Dr. Elise Wier is a respiratory paediatrician at the Glasgow Children’s Hospital.
2017 White H, Shaw N, Denman S, Pollard K, Wynne S, Peckham DG. Variation in lung function as a marker of adherence to oral and inhaled medication in cystic fibrosis. Eur Respir J. 2017 Mar 8;49(3). pii: 1600987. doi: 10.1183/13993003.00987-2016. Print 2017 Mar. [Pubmed]

Helen White
The aim of this study was to characterise adherence in an adult population with cystic fibrosis (CF) and to investigate if variation in lung function was a predictor of adherence to treatment. The coefficient of variation of weight and C-reactive protein were not predictive of adherence. The coefficient of variation of FEV1 was identified as an objective predictor of adherence. The authors suggested further evaluation of this potential marker of adherence is now required
Dr. Helen White (figure) is a Principal Lecturer within the Nutrition and Dietetic Group and course leader for MSc Nutrition. She is Postgraduate Lead within the Group, and collaborates with NHS partners on a numbers of research projects incorporating adherence, nutrition and patient experience.
Goldenberg RB. Singing Lessons for Respiratory Health: A Literature Review. J Voice. 2018 Jan;32(1):85-94. doi: 10.1016/j.jvoice.2017.03.021. Epub 2017 Apr 29. 28461167 Open access to article in J. Voice

Rachel Goldenberg
Several studies have explored the role of music and singing as a treatment for respiratory symptoms. The objective of this paper was to review the current body of literature in regard to the use of singing as both a physiological and a psychological therapy for respiratory disease and assess the role the singing teacher might play in this treatment. This is a literature review, discussion of results and directions for further research. Multiple databases were searched using keywords such as “respiratory,” “physiotherapy,” and “pulmonary” in conjunction with “singing.” Studies that met selection criteria
Seventeen studies pertaining to multiple conditions including chronic obstructive pulmonary disease, asthma, cystic fibrosis, cancer, Parkinson disease, quadriplegia, and multiple sclerosis were analysed. All studies reported trends of positive physical and/or quality of life outcomes after a series of singing lessons, regardless of statistical significance. Several noted improvements in maximum expiratory pressure and overall breathing technique. Many studies included open-ended interviews revealing participants’ perception of singing as an effective therapy that was fun, improved mood, taught breathing and breath control, was a good exercise for the lungs, and had improved physical functioning.
The author concluded that singing can be used as an adjunctive treatment for respiratory disease, with the best results occurring after long-term study. Group lessons and a strong teacher relationship feed the need for social interaction and support, which can facilitate treatment compliance. Further research is warranted.
– This is an interesting extensive review of the previous literature by Rachel Goldenberg of the Department of Music, Ambrose University, Calgary, Canada. The publications concerning CF in both children and adults are reviewed in some detail concluding there appeared to be overall benefit. Dr. Rachel (Brager) Goldenberg is a distinguished Canadian soprano whose doctoral thesis was focused on the use of singing lessons as an adjunctive airway clearance technique for Cystic Fibrosis. She has presented her dissertation research and continuing research in the use of singing for respiratory ailments across the United States, Canada and Europe
Dentice R, Elkins MR, Verschuer J, Eberl S, Dwyer G, Bye PTP. Side lying during nebulisation can significantly improve apical deposition in healthy adults and adults with mild cystic fibrosis lung disease: a randomised crossover trial. BMC Pulm Med. 2019 Jul 16;19(1):128. doi: 10.1186/s12890-019-0886-7. [Pubmed]
In people with and without Cystic Fibrosis (CF), does side lying during nebulisation change: the proportion of the dose loaded in the nebuliser that is deposited in the lungs; the uniformity of deposition throughout the lungs; or the apical drug density as a percentage of the drug density in the remaining lung? Do these effects differ depending on the degree of lung disease present?
A randomised crossover trial with concealed allocation, intention-to-treat analysis and blinded assessors, involving 39 adults: 13 healthy, 13 with mild CF lung disease (FEV1 > 80%pred), and 13 with more advanced CF lung disease (FEV1 < 80%pred). In random order, 4 mL of nebulised radioaerosol was inhaled in upright sitting and in alternate right and left side lying at 2-min intervals, for 20 min.
Compared to sitting upright, lung deposition and the uniformity of deposition were not significantly altered by side lying in any of the three groups. In sitting, the density of the deposition was significantly less in the apical regions than in the rest of the lung in all participants. Side lying significantly improved apical deposition in healthy adults (MD, 13%; 95% CI, 7 to 19), and in minimal CF lung disease (MD, 4%; 95% CI, 1 to 7) but not in advanced disease (MD, 4%; 95% CI, - 2 to 9).
The authors concluded alternating between right and left side lying during nebulisation significantly improves apical deposition in healthy adults and in adults with mild CF lung disease, without substantial detriment to overall deposition.
Ruth Dentice is physiotherapist at the Royal Prince Alfred Hospital, Sydney, Australia.
Irons JY, Petocz P, Kenny DT, Chang AB. Singing as an adjunct therapy for children and adults with cystic fibrosis. Cochrane Database Syst Rev. 2019 Jul 12;7:CD008036. doi: 10.1002/14651858.CD008036.pub5. [Epub ahead of print][Pubmed]

J Yoon Irons
Anecdotal reports suggest that singing may provide both appropriate exercise for the whole respiratory system and a means of emotional expression which may enhance quality of life. This is an update of a previously published review.
To evaluate the effects of singing as an adjunct therapy to standard treatment on the quality of life, morbidity, respiratory muscle strength and pulmonary function of children and adults with cystic fibrosis.
Only one small study (n = 40) was included, so no meta-analysis could be performed. The included randomised controlled study was of parallel design and undertaken at two paediatric hospitals in Australia. The study evaluated the effects of a singing program on the quality of life and respiratory muscle strength of hospitalised children with cystic fibrosis (mean age 11.6 years, 35% male). While the singing group received eight individual singing sessions, the control group participated in preferred recreational activities, such as playing computer games or watching movies. This study was limited by a small sample size (51 participants) and a high drop-out rate (21%). There were no differences between the groups at either post-intervention or follow-up; although by the end of treatment there were some improvements in some of the domains of the quality of life questionnaire Cystic Fibrosis Questionnaire-Revised (e.g. emotional, social and vitality domains) for both singing and control groups.
The conclusion was there is insufficient evidence to determine the effects of singing on quality of life or on the respiratory parameters in people with cystic fibrosis. However, there is growing interest in non-medical treatments for cystic fibrosis and researchers may wish to investigate the impact of this inexpensive therapy on respiratory function and psychosocial well-being further in the future.
Dr J Yoon Irons qualified PhD at University of Sydney and is now a Research Fellow at the Department of Health and Social Care Research Centre, University of Derby, Derby, UK. She is interested in exploring health and wellbeing benefits from participating in arts such as singing, music, dance and visual arts.
See also Goldenberg RB. Singing lessons for respiratory health; a literature review. J Voice 2018; 32(1):85-94. In 2017 section and also Physiotherapy Topic section
Ward N, Stiller K, Holland AE; Australian Cystic Fibrosis Exercise Survey group. Collaborators (18) Exercise is commonly used as a substitute for traditional airway clearance techniques by adults with cystic fibrosis in Australia: a survey. J Physiother. 2019 Jan;65(1):43-50. doi: 10.1016/j.jphys.2018.11.006. Epub 2018 Dec 14. Free Full Text [Pubmed]

Nathan Ward
A cross-sectional survey at 13 CF centres in Australia, using a purpose-designed questionnaire.
More details in PubMed abstract.
The authors concluded exercise is commonly used as a substitute for traditional airway clearance techniques. Physiotherapists should advise patients that whilst there is some research suggesting a possible mechanism for exercise as a form of airway clearance, there are currently no medium-term to long-term data supporting exercise as a stand-alone form of airway clearance. These results suggest that future research to investigate the clinical effectiveness of exercise as a substitute for traditional airway clearance techniques should be a priority.
Nathan Ward is a physiotherapist in the Cystic Fibrosis Service, Royal Adelaide Hospital, Adelaide, Australia.
Rowbotham NJ, Smith SJ, Davies G, Daniels T, Elliott ZC, Gathercole K, Rayner OC, Smyth AR. Can exercise replace airway clearance techniques in cystic fibrosis? A survey of patients and healthcare professionals. J Cyst Fibros. 2019 Nov 15. pii: S1569-1993(19)30962-2. doi: 10.1016/j.jcf.2019.10.026. [Epub ahead of print] [Pubmed]
Nicola Rowbotham
Airway clearance techniques (ACTs) are recommended in cystic fibrosis (CF) to prevent accumulation of secretions and lung infection. “Can exercise replace chest physiotherapy for people with CF?” is one of the CF community’s top 10 research questions. We conducted an online survey of the CF community to gather data on current ACT use, recommendations, reported adherence levels and exercise strategies used. There were 488 respondents: 194 (40%) people with CF (pwCF), 141 (29%) family and 153 (31%) healthcare professionals (HCPs) (mostly physiotherapists). Only 10/285 (4%) of pwCF do no exercise at present and 163/303 (54%) already incorporate exercise into ACTs. ACTs were omitted by 128/267 (48%) of pwCF when they exercised. Nearly all (110/129, 93%) of HCPs currently recommend exercise to support ACTs. A trial replacing some or all ACTs with exercise, was supported by 80/110 (73%) of HCPs, with an additional 9/110 (8%) willing to consider in selected patients.
Dr Nicola J Rowbotham is in the University of Nottingham, Evidence Based Child Health Group, Division of Child Health, Obstetrics & Gynaecology, Queens Medical Centre, Nottingham, UK
Nicola J Rowbotham is at the University of Nottingham, Evidence Based Child Health Group, Division of Child Health, Obstetrics & Gynaecology, Queens Medical Centre, Nottingham31774149 31774149 31774149
McIlwaine M, Button B, Nevitt SJ. Positive expiratory pressure physiotherapy for airway clearance in people with cystic fibrosis. Cochrane Database Syst Rev. 2019 Nov 27;2019(11). doi: 10.1002/14651858.CD003147.pub5. [Pubmed]

Brenda Button

Maggie McIlwaine
To determine the effectiveness and acceptability of PEP devices compared to other forms of physiotherapy as a means of improving mucus clearance and other outcomes in people with CF. A total of 28 studies (involving 788 children and adults) were included in the review; 18 studies involving 296 participants were cross-over in design.
The study is a valuable review described in full detail in the abstract by these highly experienced authors who suggest that all techniques and devices described may have a place in the clinical treatment of people with CF. Following meta-analyses of the effects of PEP versus other airway clearance techniques on lung function and patient preference, this Cochrane Review demonstrated that there was high-quality evidence that showed a significant reduction in pulmonary exacerbations when PEP using a mask was compared with HFCWO. It is important to note that airway clearance techniques should be individualised throughout life according to developmental stages, patient preferences, pulmonary symptoms and lung function. This also applies as conditions vary between baseline function and pulmonary exacerbations
Maggie McIlwaine is senior physiotherapist at BC Children’s Hospital Vancouver and has done important research on PEP
Brenda Button is physiotherapist at Alfred Hospital Victoria Australia and widely experienced in CF physical therapy
Alberto Montero-Ruiz, Laura A Fuentes, Estela Pérez Ruiz, Nuria García-Agua Soler, Francisca Rius-Diaz, Pilar Caro Aguilera , Javier Pérez Frías, Elisa Martín-Montañez Effects of music therapy as an adjunct to chest physiotherapy in children with cystic fibrosis: A randomized controlled trial. PLoS One 2020 Oct 30;15(10):e0241334.doi: 10.1371/journal.pone.0241334. eCollection 2020. [Pubmed] Free PMC article

Alberto Montero-Ruiz
Airway clearance therapy (ACT) is considered an important approach to improve airway clearance in children with cystic fibrosis (CF). Daily ACT administration requires substantial commitments of time and energy that complicate ACT and reduce its benefits. It is crucial to establish ACT as a positive routine. Music therapy (MT) is an aspect of integrative strategies to ameliorate the psycho-emotional consequences of chronic diseases, and a MT intervention could help children with CF between the ages of 2 and 17 develop a positive response.
The aim of this randomized controlled trial was to evaluate the effects of specifically composed and recorded instrumental music as an adjunct to ACT. We compared the use of specifically composed music (Treated Group, TG), music that the patient liked (Placebo Group, PG), and no music (Control Group, CG) during the usual ACT routine in children with CF aged from 2 to 17.
The primary outcomes, i.e., enjoyment and perception of time, were evaluated via validated questionnaires. The secondary outcome, i.e., efficiency, was evaluated in terms of avoided healthcare resources. Enjoyment increased after the use of the specifically composed music (children +0.9 units/parents +1.7 units; p<0.05) compared to enjoyment with no music (0 units) and familiar music (+0.5 units). Perception of time was 11.1 min (±3.9) less than the actual time in the TG (p<0.05), 3.9 min (±4.2) more than the actual time in the PG and unchanged in the CG. The potential cost saving related to respiratory exacerbations was €6,704.87, while the cost increased to €33,524.35 in the CG and to €13,409.74 in the PG.
In conclusion, the specifically composed, played and compiled instrumental recorded music is an effective adjunct to ACT to establish a positive response and is an efficient option in terms of avoided costs. Trial registered as ISRCTN11161411. ISRCTN registry (www.isrctn.com)
Christophe Marguet, Véronique Houdouin, Isabelle Pin, Philippe Reix Frédéric Huet, Marie Mittaine, Sophie Ramel , et al. Chest physiotherapy enhances detection of Pseudomonas aeruginosa in nonexpectorating children with cystic fibrosis. ERJ Open Res. 2021 Mar 8;7(1):00513-2020.doi: 10.1183/23120541.00513-2020.eCollection 2021 Jan. Free PMC article [Pubmed]

Christophe Marguet
This prospective multicentre study compared three successive methods for sampling airway secretions applied through the same session: 1) an oropharyngeal swab (OP), 2) a chest physiotherapy session followed by a provoked cough to obtain sputum (CP-SP) and 3) a second oropharyngeal swab collected after chest physiotherapy (CP-OP). Haemophilus influenzae, Staphylococcus aureus and P. aeruginosagrowth cultures were assessed. Accuracy tests and an equivalence test were performed to compare the three successive methods of collection.
300 non-expectorating children with CF were included. P. aeruginosa was detected cumulatively in 56 (18.9%) children, and according to the different collection methods in 28 (9.8%), 37 (12.4%) and 44 (14.7%) children by using OP, CP-OP and CP-SP, respectively. Compared with OP, the increased detection rate was +22% for CP-OP (p=0.029) and +57% for CP-SP (p=0.003). CP-SP had the best positive predictive value (86.3%) and negative predictive value (96.0%) for P. aeruginosa compared with the overall detection.
The results of this adequately powered study show differences in the rates of pathogens detected according to the sampling method used. Chest physiotherapy enhanced detection of P. aeruginosa in non-expectorating children with CF.
Professor Christophe Marguet is at the CF Centre, Dept of Paediatrics and Adolescent Medicine, University Hospital Charles Nicolle, CIC INSERM 1404, EA 2656, Rouen University, Rouen, France.
Alberto Montero-Ruiz, Departamento de Farmacología y Pediatría, Universidad de Málaga, Instituto de Investigación Biomédica de Málaga, Facultad de Medicina, Málaga, Spain and Consejería de Educación, Junta de Andalucía, Delegación Territorial de Málaga, Málaga, Spain.
Paul Burnham, Gemma Stanford, Ruth Stewart.Autogenic drainage for airway clearance in cystic fibrosis. Cochrane Database Syst Rev. 2021 Dec 15;12:CD009595.doi: 10.1002/14651858.CD009595.pub3.[Pubmed]

Ruth Stewart

Gemma Stanfo
Background: Autogenic drainage is an airway clearance technique that was developed by Jean Chevaillier in 1967. The technique is characterised by breathing control using expiratory airflow to mobilise secretions from smaller to larger airways. Secretions are cleared independently by adjusting the depth and speed of respiration in a sequence of controlled breathing techniques during exhalation. The technique requires training, concentration and effort from the individual, but it has previously been shown to be an effective treatment option for those who are seeking techniques to support and promote independence. However, at a time where the trajectory and demographics of the disease are changing, it is important to systematically review the evidence demonstrating that autogenic drainage is an effective intervention for people with cystic fibrosis (Full details in the PubMed abstract)
Authors’ conclusions: Autogenic drainage is a challenging technique that requires commitment from the individual. As such, this intervention merits systematic review to ensure its effectiveness for people with cystic fibrosis, particularly in an era where treatment options are changing rapidly. From the studies assessed, autogenic drainage was not found to be superior to any other form of airway clearance technique. Larger studies are required to better evaluate autogenic drainage in comparison to other airway clearance techniques in view of the relatively small number of participants in this review and the complex study designs. The studies recruited a range of participants and were not powered to assess non-inferiority. The varied length and design of the studies made the analysis of pooled data challenging.
Paul Burnham is with the Servicio de Medicina Fisica y Rehabilitacion, Hospital La Paz, Madrid, Spain.
Gemma Stanford is in the Department of Cystic Fibrosis, Royal Brompton & Harefield NHS Foundation Trust, London, UK and the National Heart and Lung Institute, Imperial College London, London, UK.
Ruth Stewart is at the Royal Hospital for Children and Young People, Edinburgh, UK.
Beth L Laube, Kathryn A Carson, Christopher M Evans, Melis A Aksit, Joseph M Collaco, Vanessa L Richardson, Gail Sharpless, Pamela L Zeitlin, Garry R Cutting, Peter J Mogayzel. Characterizing mucociliary clearance in young children with cystic fibrosis. Pediatr Res 2022 Feb;91(3):612-620.doi: 10.1038/s41390-021-01453-2. Epub 2021 Mar 22. Free PMC article [Pubmed]

Bethe Laube johnshopkinscf.org
Background: This research characterized mucociliary clearance (MCC) in young children with cystic fibrosis (CF).
Methods: Fourteen children (5-7 years old) with CF underwent: two baseline MCC measurements (Visits 1 and 2); one MCC measurement approximately 1 year later (Visit 3); and measurements of lung clearance index (LCI), a measure of ventilation inhomogeneity.
Results: Median (range) percent MCC through 60 min (MCC60) was similar on Visits 1 and 2 with 11.0 (0.9-33.7) and 12.8 (2.7-26.8), respectively (p = 0.95), and reproducible (Spearman Rho = 0.69; p = 0.007). Mucociliary clearance did not change significantly over 1 year with median percent MCC60 on Visit 3 [12.8 (3.7-17.6)] similar to Visit 2 (p = 0.58). Lower percent MCC60 on Visit 3 was significantly associated with higher LCI scores on Visit 3 (N = 14; Spearman Rho = -0.56; p = 0.04).
Conclusions: Tests of MCC were reproducible and reliable over a 2-week period and stable over a 1-year period in 5-7-year-old children with CF. Lower MCC values were associated with increased ventilation inhomogeneity. These results suggest that measurements of MCC could be used in short-term clinical trials of interventions designed to modulate MCC and as a new, non-invasive test to evaluate early lung pathology in children with CF.
Impact: This is the first study to characterize mucociliary clearance (MCC) in children with cystic fibrosis (CF) who were 5-7 years old. Measurements of mucociliary clearance were reproducible and reliable over a 2-week period and stable over a 1-year period. Variability in MCC between children was associated with differences in ventilation homogeneity, such that children with lower MCC values had increased ventilation inhomogeneity.
These results suggest that measurements of MCC could be used in short-term clinical trials of interventions designed to modulate MCC and as a new, non-invasive test to evaluate early lung pathology in children with CF.
Dr Beth Laube is a professor and aerosol scientist in the Department of Pediatrics, Johns Hopkins University School of Medicine, Baltimore, MD, USA.
Katie D Heinz, Adam Walsh, Kevin W Southern Zoe Johnstone, Kate H Regan. Exercise versus airway clearance techniques for people with cystic fibrosis. Cochrane Database Syst Rev 2022 Jun 22;6(6):CD013285.doi: 10.1002/14651858.CD013285.pub2. [Pubmed]
Background: There are many accepted airway clearance techniques (ACTs) for managing the respiratory health of people with cystic fibrosis (CF); none of which demonstrate superiority. Other Cochrane Reviews have reported short-term effects related to mucus transport, but no evidence supporting long-term benefits. Exercise is an alternative ACT thought to produce shearing forces within the lung parenchyma, which enhances mucociliary clearance and the removal of viscous secretions. Recent evidence suggests that some people with CF are using exercise as a substitute for traditional ACTs, yet there is no agreed recommendation for this. Additionally, one of the top 10 research questions identified by people with CF is whether exercise can replace other ACTs. Systematically reviewing the evidence for exercise as a safe and effective ACT will help people with CF decide whether to incorporate this strategy into their treatment plans and potentially reduce their treatment burden. The timing of this review is especially pertinent given the shifting landscape of CF management with the advent of highly-effective small molecule therapies, which are changing the way people with CF are cared for.[OBJECTS AND METHODS ETC ARE OMITTED but on PubMed link]
Authors’ conclusions: As one of the top 10 research questions identified by clinicians and people with CF, it is important to systematically review the literature regarding whether or not exercise is an acceptable and effective ACT, and whether it can replace traditional methods. We identified an insufficient number of trials to conclude whether or not exercise is a suitable alternative ACT, and the diverse design of included trials did not allow for meta-analysis of results. The evidence is very low-certainty, so we are uncertain about the effectiveness of exercise as an ACT. Longer studies examining outcomes that are important to people with CF are required to answer this question.
Katie D Heinz is in the Department of Medicine, Glasgow Royal Infirmary, Glasgow, UK.
-It is difficult to see how “longer studies examining outcomes” would answer the question or be the best use of patients’ or the researchers’ time. It would seem that trials of both methods on each individual patient would be more useful than ever larger longer trials of groups of patients – the results of which would apply to groups rather than individuals? (A personal view of this reviewer)
Crystal Bourke , Sunalene Devadason, William Ditcham, Julie Depiazzi, Mark L Everard. Controlled inhalation improves central and peripheral deposition in cystic fibrosis patients with moderate lung disease. J Paediatr Child Health 2022 Feb 17. doi: 10.1111/jpc.15909. Online ahead of print. pubmed.ncbi.nlm.nih.gov/35174574/
Aim: With progressive impairment of lung function, deposition of inhaled drug in the lungs becomes progressively more central, limiting its effectiveness. This pilot study explored the possibility that long slow inhalations might improve delivery of aerosol to the lung periphery in cystic fibrosis patients with moderate lung disease.
Methods: Five subjects aged 12-18 years (mean FEV1 72%; range 63-80%) inhaled a radiolabelled aerosol from a jet nebuliser on two occasions. Two inhalation techniques were compared: breathing tidally from a standard continuous output nebuliser and using long slow inhalations from the AKITA® JET system.
An example of one participant’s gamma scintigraphy images (anterior view) showing significantly decreased deposition in the orogastric regions with long slow inhalations. (a) Standard delivery with tidal breathing. (b) Dosimetric delivery with long slow inhalation – (advise see free full article via Pubmed link(
Results: Long slow breaths resulted in much lower oropharyngeal deposition with higher lung doses. Importantly, the peripheral lung increased proportionately. The increased lung dose is attributable to more of the larger inhaled droplets passing into the lower airways. This would be expected to increase the central deposition unless significantly more of the smaller droplets were able to penetrate deeper into the lungs. The data support improved delivery of drug to the distal lung when compared with tidal breathing.
Conclusion: These pilot data suggest that this approach may prove to be clinically relevant in improving the efficacy of inhaled medication in those with moderate-severe lung disease.
Crystal Bourke is in the Physiotherapy Department, Perth Children’s Hospital, Perth, Western Australia, Australia.
Emma Raywood , Harriet Shannon , Nicole Filipow , Gizem Tanriver , Sanja Stanojevic , Kunal Kapoor , Helen Douglas , Rachel O’Connor , Nicky Murray , Bridget Black , Eleanor Main. Quantity and quality of airway clearance in children and young people with cystic fibrosis. J Cyst Fibros. 2022 Oct 6;S1569-1993(22)00686-5. doi: 10.1016/j.jcf.2022.09.008. Online ahead of print. pubmed.ncbi.nlm.nih.gov/36210322/]

Emma Raywood crunchable.com
Children and young people with CF (CYPwCF) get advice about using positive expiratory pressure (PEP) or oscillating PEP (OPEP) devices to clear sticky mucus from their lungs. However, little is known about the quantity (number of treatments, breaths, or sets) or quality (breath pressures and lengths) of these daily airway clearance techniques (ACTs) undertaken at home. This study used electronic pressure sensors to record real time breath-by-breath data from 145 CYPwCF (6-16y) during routine ACTs over 2 months. ACT quantity and quality were benchmarked against individual prescriptions and accepted recommendations for device use. In total 742,084 breaths from 9,081 treatments were recorded. Individual CYPwCF maintained consistent patterns of ACT quantity and quality over time. Overall, 60% of CYPwCF did at least half their prescribed treatments, while 27% did fewer than a quarter. About 77% of pre-teens did the right number of daily treatments compared with only 56% of teenagers. CYPwCF usually did the right number of breaths. ACT quality (recommended breath length and pressure) varied between participants and depended on device. Breath pressures, lengths and pressure-length relationships were significantly different between ACT devices. PEP devices encouraged longer breaths with lower pressures, while OPEP devices encouraged shorter breaths with higher pressures. More breaths per treatment were within advised ranges for both pressure and length using PEP (30-31%) than OPEP devices (1-3%). Objective measures of quantity and quality may help to optimise ACT device selection and support CYPwCF to do regular effective ACTs.
Emma Raywood is a physiotherapist at UCL Great Ormond Street Institute of Child Health, London
The Role of the Physical Therapist in Cystic Fibrosis Care.2022 Oct 4;pzac136.doi: 10.1093/ptj/pzac136. Online ahead of print. pubmed.ncbi.nlm.nih.gov/36193006/

Gemma Stanford
In looking back on 2020 and 2021, this Perspective reflects on the monumental impacts of the rollout of cystic fibrosis (CF) transmembrane conductance regulator highly effective modulator therapies and the COVID-19 pandemic on the management of CF. Advancements in the clinical management of people with CF have been both enormous and rapid, and physical therapists specializing in the care of people with CF have been at the forefront of driving this evolution in care. This year sees the thirtieth anniversary of the UK Association of Chartered Physiotherapists in Cystic Fibrosis and, as is inevitable in reaching such milestones, thoughts have turned to origins, role, impacts, and the future. With the changing demographics of the population of people with CF after the introduction of highly effective modulator therapies, potentially with fewer secondary complications, the future role of the physical therapist who specializes in CF is in question. This Perspective reflects upon and highlights the role of physical therapy within CF and provides insights into how physical therapists and respiratory therapists can evolve their roles to ensure relevance for the future.
and Harefield Hospitals, Guys and St. Thomas’ NHS Foundation Trust, Sydney Street, London, SW3 6NP, UK.; National Heart and Lung Institute, Imperial College, Guy Scadding Building, Dovehouse St, Chelsea, London SW3
Sandra Gursli, Alexandra Quittne , Reidun Birgitta Jahnsen , Bjørn Skrede , Britt Stuge, Egil Bakkeheim. Airway clearance physiotherapy and health-related quality of life in cystic fibrosis. PLoS One. 2022 Oct 18;17(10):e0276310. doi: 10.1371/journal.pone.0276310. eCollection 2022. Free PMC article pubmed.ncbi.nlm.nih.gov/36256673/

Sandra Gursli www.Linkedin
Objective: Airway clearance physiotherapy is recommended in cystic fibrosis, but limited evidence exists to suggest how much treatment is enough. As a secondary analysis of a prior study investigating the safety, efficacy, and participants’ perceptions of a novel airway clearance technique, specific cough technique (SCT) compared to forced expiration technique (FET), we aimed to evaluate whether the intervention was associated with changes in health-related quality of life (HRQoL).
Methods: We conducted randomised, controlled individual trials with six adults (N-of-1 RCTs). Each trial included eight weeks of treatment, twice a week, using saline inhalation in horizontal positions, one with SCT and one with FET, in random order. Efficacy was measured by sputum wet weight (g) after each session. Perceived usefulness and preference were self-reported at the end of the study. Lung function was assessed at baseline and at the end of study. HRQoL was measured using the Cystic Fibrosis Questionnaire-Revised (CFQ-R) at baseline (week 1) and at completion of the study (week 8). Individual HRQoL scores (0-100) were coded and analysed using CFQ-R Software Program, version 2.0.
Results: Patient-reported outcomes were completed by all subjects. Individual CFQ-R-Respiratory Symptoms Scores (CFQ-R-RSS) showed a positive change, meeting the minimal important difference (MID) ≥ 4 points in five participants and a negative change in one individual. A strong correlation (r = 0.94 (p<0.01) was found between total sputum weight (g) and the positive changes in CFQ-R-RSS, and between changes in lung function and CFQ-R-RSS (r = 0.84 (p = 0.04).
Conclusion: The airway clearance intervention was associated with clinically meaningful changes in patient-reported symptoms on the CFQ-R in the majority of the participants. This finding warrants further investigation regarding treatment, duration and frequency. A long-term study may reveal beneficial effects on other clinically meaningful endpoints, such as pulmonary exacerbations, high-resolution computed tomography scores and HRQoL.
Sandra Gursli is a specialist physiotherapist at the Resource Centre for Cystic Fibrosis, Oslo University Hospital, Oslo, Norway.
6LY,; UK.Association of Chartered Physiotherapists in Cystic Fibrosis (ACPCF) c/o ACPCF Secretary, Infection, Immunity & Inflammation Dept, University College London Great Ormond Street Institute of Child Health, Faculty of Population Health Sciences, University College London, Gower Street, London, WC1E 6BT, UK.
Máire Curran , Audrey C Tierney , Louise Collins , Lauren Kennedy , Ciara McDonnell , Andrew J Jurascheck , Ali Sheikhi , Cathal Walsh , Brenda Button , Brian Casserly , Roisin Cahalan . Steps Ahead: Optimising physical activity in adults with cystic fibrosis: A pilot randomised trialusing wearable technology, goal setting and text message feedbackJ Cyst Fibros. 2022 Nov 16;S1569-1993(22)01411-4. doi: 10.1016/j.jcf.2022.11.002. Online ahead of print pubmed.ncbi.nlm.nih.gov/36402730/

Maire Curran
Background: Regular participation in physical activity (PA) is encouraged for people with Cystic Fibrosis (CF). This study aimed to assess the effectiveness of an intervention using wearable technology, goal setting and text message feedback on PA and health outcomes in people with CF.
Methods: This was a pilot randomised trial conducted at University Hospital Limerick. Participants were randomly assigned to the intervention (INT) or active comparator (AC). The 12-week intervention consisted of wearable technology (Fitbit Charge 2) which was remotely monitored, and participants set step count goals. Participants were sent a one-way text message once a week over 12 weeks to positively reinforce and encourage PA participation. The AC group received the wearable technology alone. Follow up was assessed at 24 weeks. Outcomes assessed were PA, aerobic capacity, lung function, sleep, quality of life and wellbeing.
Results: Step count increased significantly for the INT group over 12 weeks when compared to the AC group (p=0.019). The INT group had a 28% week-to-week percentage change (Weeks 1-12), while the AC group reduced by 1%, p=0.023. Within group changes demonstrated that VO2 peak (ml/kg/min) significantly increased for the INT group at 12 weeks (24.4 ±7.65 to 26.13 ±7.79, p=0.003) but not at 24 weeks (24.45 ±7.05, p=0.776). There were no significant differences observed for VO2 peak (ml/kg/min) for the AC group. There was no significant effect on lung function, sleep, well-being, or quality of life for either group.
Conclusions: A personalised PA intervention using wearable technology, goal setting and text message feedback increased PA and aerobic capacity in people with CF. Integration of this intervention into usual care may encourage regular PA participation for people with CF.
Maire Curran is a specialist physiotherapist at School of Allied Health, University of Limerick, Limerick, Ireland; University Hospital Limerick, Limerick, Ireland; Health Research Institute, University of Limerick, Limerick, Ireland.
