SELECTED REVIEWS, DESCRIPTIVE ARTICLES
Many of these articles give an idea of the treatment and outlook at the time they were written – always remembering they were written by staff at CF Centres where the outlook would be much better than at a local general hospital paediatric department
1942 Wolman IJ. Cystic fibrosis of the pancreas. Am J Med Sci 1942; 203: 900-905.

Irving Wolman
A really excellent review by Irving Wolman of Philadelphia of the “great catch basket of intestinal disorders comprised in the term “celiac disease” noting that “a new and significant entity has crystallized out”.
Wolman considers that Passini (1919) was the first to describe an instance of faulty digestion due to pancreatic disease. Parmalee (1935) related steatorrhoea to pancreatic deficiency as had Harper (1932 and 1938), Andersen (1938) and Rauch Litvak and Steiner in 1939), all working independently, had succeeded to “throw this hitherto indefinite entity into sharp focus” i.e. cystic fibrosis.
1949 May CD, Lowe CU. Fibrosis of the pancreas in infants and children; illustrated review of certain clinical features with special emphasis on pulmonary and cardiac aspects. J Pediatr 1949; 34:663-687. [PubMed]
A very comprehensive study of 134 patients from Minneapolis (also described in Lowe & May, 1949 above). Virtually all had early onset of signs of malabsorption, 29 had meconium ileus and all had pulmonary involvement Staphylococcus aureus being the usual organism. Cardiac failure was observed in six patients. The authors considered that aerosol antibiotic (penicillin) inhalation, recently described by di Sant’Agnese (1946) was the first substantial advance in treatment. The authors believed that “the pulmonary process begins soon after birth, is most intense between 6 to 18 months and then subsides somewhat”. Even improved nutrition did not seem to halt the progress.
1952 Bodian ML. Fibrocystic Disease of the Pancreas. A Congenital Disorder of Mucus Production (Mucosis). London, W Heinemann, 1952.

Martin Bodian
The first substantial work on CF from the UK by Martin Bodian and his colleagues at the Hospital for Sick Children, Great Ormond Street, London (GOS). Dr. Martin Bodian (1910-1963),(figure 4 main text) had been appointed morbid anatomist at GOS in 1946. Dr Archie Norman (figure 5 main text) was the paediatrician in charge of the CF clinic at GOS and a leading figure in CF care in the UK for many years. Dr. Cedric Carter (1917-1984 figure 6 main text) was a clinical geneticist who started the first genetic counselling clinic at GOS in 1957.
In the preface of the book Martin Bodian notes the contents encompass almost a decade of work since Donald Paterson diagnosed the first child with CF at Great Ormond Street in 1943. The authors reviewed their own and previously published families and concluded there was a recessive mode of inheritance and suggested parents of a child with CF should be given a 1 in 4 risk of further children being affected; this confirmed the findings of Andersen & Hodges (1946 above) and the earlier suggestion of Howard (1944 above)
1954 May CD. Cystic Fibrosis of the Pancreas in Infants and Children. Charles C Thomas. Springfield, Illinois. 1954.
A 93 page monograph reviewing the current knowledge on cystic fibrosis. Charles May acknowledges many years of shared experience with Dr Charles Upton Lowe, at the time associate Professor of Pediatrics at Buffalo.
There is an interesting dedication at the beginning – “To the practitioners, Margaret Harper (1938) of Sydney, Australia and Arthur H Parmelee of Chicago, Illinois (1935) who recognised the salient clinical features of patients found to have cystic fibrosis of the pancreas, published the first papers indicating the frequency and importance of the disease, and clearly set it apart from celiac disease against the prevalent practice”. Interestingly Dorothy Andersen is not mentioned in this context!
Also May recalls how Blackfan was steadily preoccupied during the Thirties with the problem of recognising infants who had cystic fibrosis of the pancreas culminating in his report of 1938 (Blackfan & May, 1938).
In the Chapter III “Historical” of this book May writes “Thus the history of the discovery of cystic fibrosis of the pancreas in infants is a revealing example of the gradual accumulation of observations from a variety of independent sources which may be required to attain a clear conception of a disease, even though its manifestations clinically and pathologically are flagrant. That recognition of this disease was delayed until the most recent times should serve as a reminder of the continuing need for critical clinical observation in this age of overwhelming dependence on the laboratory” – this written in 1954!! However wise this advice, it was through observations in the laboratory of the characteristic pancreatic histological changes that CF was identified as a distinct clinical entity by Dorothy Andersen. It is interesting that there was no mention of Dorothy Andersen by May except that “Andersen’s original paper should be consulted for the most adequate illustrations of progressive stages in the development of this (pancreatic) lesion”.
In the Treatment chapter diet and the use of pancreatin precede the treatment of the chest. The important relationship between the activity of the chest infection and nutritional state is mentioned. There is a rather unenthusiastic approach to pancreatin therapy which is considered to dampen the appetite with only modest benefit on absorption so “if the infant or child does not accept pancreatin readily or if the expense is prohibitive one need not feel badly if this form of therapy must be abandoned”.
 |
| A illustration, from May’s 1954 book, of a typical child with CF in the Fifties. |
1954 McIntosh R. Cystic fibrosis of the pancreas. Patients over 10 years of age. Acta Paediatr 1954; (Supp.100): 467. [PubMed]

Rustin MacKintosh
From 1931 Rustin McIntosh (1894-1986 figure in main text) a distinguished general paediatrician, was Chairman of the Babies Hospital, New York where Dorothy Andersen and Paul di Sant’Agnese developed their CF service. Out of a large group of their patients McIntosh describes 27 who were over the age of 10 years (four of whom had died) from the Colombia Presbyterian Medical Center in New York. It is of note that all the patients already had severe respiratory involvement although all retained an optimistic outlook for the future. Fatty foods were avoided because of symptoms and only half took pancreatic enzymes and they did equally well without them.
The report was mentioned by Shwachman in 1958 as the largest series of older patients so far published.
1955 Shwachman H, Leubner H. Mucoviscidosis. Advan Pediat 1955; 7:249-323. [PubMed]

Harry Shwachman.
The paper contains the first detailed report of symptomatic diabetes mellitus and CF in a white boy aged 5 years from Kaloa,Hawaii – considered to be the superimposition of one serious disease on another. The authors note that “mucoviscidosis is so well established today that we seldom see individual case reports except in areas where interest in the disease is awakening (for example South Africa, Canada and Germany). Rather we look forward to monographs such as Bodian’s (1952 above) and May’s (May CD. Cystic fibrosis of the pancreas in infants and children. Springfield Ill: Charles C Thomas. Publisher, 1954 above) where accumulated experience is recorded”.
They note that in Bodian’s book Cedric Carter, the geneticist, combined the data from Andersen and Hodges, Lowe, May and Reed with his own to confirm the expected probability of 1 in 4 children being affected. The importance of di Sant’Agnese’s recent (1953) description of the sweat electrolyte abnormality is mentioned particularly its importance in the recognition of the 5 – 10% of people with CF without clinical pancreatic insufficiency – but the tryptic activity of duodenal juice was still of great importance in diagnosis. Shwachman describes their experience of inducing sweating in 300 children by placing the child in a plastic suit bag for 30-90 minutes with pieces of covered gauze on the back. Values of over 80 meq/l were considered diagnostic of cystic fibrosis.
The beneficial effect of controlling infection with antibiotics in contrast to the relatively unsuccessful attempts with various inhalations including trypsin and oral iodides was stressed – “early recognition of the disease and prompt antibiotic therapy may be so encouraging that parents as well as doctor begin to question the original diagnosis”!
Finally, Shwachman notes that the average age of death from 1940-48 was 12.8 months and from 1949-53 was 45.2 months – the broad spectrum antibiotics came into use in 1949 and were considered likely to be one of the reasons for the improvement.
This 74 page paper, with 142 references, is a very detailed review of the current knowledge of CF up to that time by Harry Shwachman, written with the assistance of Hugo Leubner of the WHO and Pincus Catzel, then a research fellow; it makes very interesting reading.
1958 Shwachman H, Kulczycki LL. Long-term study of 105 cystic fibrosis patients. Am J Dis Child 1958; 96:6-15. [PubMed]
This is a frequently-quoted paper of studies made over a five to fourteen year period after diagnosis –“survival beyond childhood is being noted with
Lucas Kulczycki
increasing frequency”. Ninety five patients were still living and 10 had died; 41 were over 10 years. Details of therapy are described and also the details of the Shwachman/Kulczycki clinical score which became the standard method of scoring a patients clinical condition. In the score equal weight given to the general activity, physical examination, nutritional status and X-ray chest. The authors emphasise “the value of pursuing a vigorous therapeutic programme in a disease which is still so little understood”. With regard to treatment, prior to 1948 sulphonamides, penicillin and streptomycin were the only agents available – the latter two used mainly for exacerbations. In September 1948 Aureomycin was used and very effective and Terramycin in early 1950 was equally effective. Chloramphenicol and erythromycin were used liberally since 1955 and novobiocin sparingly for one year. Wide spectrum agents in prophylactic dosage or in therapeutic dosage when pulmonary infection was well established. Complex mixtures of antibiotics, propylene glycol and detergents were used for short term inhalation therapy. A few patients were treated in mist tents at night. Patients received a liberal high protein diet with an effort to reduce the fat intake. All had pancreatin (Viokase) and vitamins.
These results were extraordinarily good for the time – certainly in most of the UK at this time there were only very exceptional patients who reached adolescence. There was no requirement for adult clinics as there were virtually no adults in most of the UK – the only clinic for adults with CF was at the Royal Brompton Hospital in London and this did not start until the early Sixties.
1958 Andersen DH. Cystic fibrosis of the pancreas. A review. J Chron Dis 1958; 7:58-90. [PubMed]

Dorothy Andersen
A wide ranging and very comprehensive review of CF by Dorothy Andersen containing 240 references. The text was kindly given to me by Dr Archie Norman who I suspect reviewed the original paper. Andersen writes “From obscure origins as an esoteric disease, cystic fibrosis of the pancreas has in twenty years become one of the most intensively studied and widely discussed maladies in pediatrics”.
The introduction sums up the situation at that time – “Cystic fibrosis of the pancreas can be defined as a congenital familial disease characterised by dysfunction of many of the exocrine glands. The most obvious effects are pancreatic deficiency with characteristic morphologic changes in that organ, susceptibility to chronic bronchitis, and a high concentration of electrolytes in the sweat. Other exocrine glands may give functional and morphological evidence of abnormality. The basic defect is unknown. Death occurs in infancy or childhood in the majority of cases”.
This paper provides a detailed review of CF up to that time, in particular, a very detailed review of the pathology. Andersen’s observation that “the disease has proved to be of varied expression requiring the informed attention of a number of branches of medicine including radiology, surgery, otolaryngology, obstetrics and internal medicine” has certainly proved to be correct – even more so as the average age of the CF population increases.
1959 Di Sant’Agnese PA, Andersen DH. Cystic fibrosis of the pancreas in young adults. Ann Intern Med 1959; 50:1321-1330. [PubMed]

Paul di Sant’Agnese.
A review article intended to bring CF to the attention of adult physicians. There are interesting statistics – between 1939 and 1958 there were 550 children with CF seen at the Babies Hospital, New York. One hundred and six survived beyond the age of 10 years, the oldest was aged 24 years and 85 were still alive. The authors mention abdominal masses in the right iliac fossa as being not infrequent; some explored surgically had proved to be of faecal in origin. Appendix abscesses, where the symptoms have been masked by antibiotics given for the chest, had been seen in two patients both of whom recovered – but “important to keep in mind”.
The authors conclude that “Cystic fibrosis is breaking out of the paediatric bounds to which it had been limited by its high mortality rate in infancy and childhood. It is now invading the domain of diseases of the adult individual.”
This paper has been quoted as containing first description of appendix abscesses in CF and the difficulties of their recognition in people with CF (also Holsclaw & Habboushe. J Pediatr Surg 1976; 11:217-221).
1959 di Sant’Agnese PA. Recent observations on the pathogenesis of cystic fibrosis of the pancreas. Pediatrics 1959; 24: 313-321. [PubMed]
An interesting review, by a leader in the field, on the possibilities – a deficiency in function of the autonomic nervous system (also mentioned by Shwachman as a possibility and obviously popular at the time), an absence of an enzyme or some other metabolic error or according to Gochberg & Cooke “a shortage of energy for secretory activity” (Pediatrics 1956; 18:701).
The author noted that the recognition of many variations in the clinical picture had been possible since the sweat tests became available after 1953. More than 550 patients had attended the Babies Hospital in New York since 1939 and only 9 (2%) had liver cirrhosis and these occurred in recent years as the age increased. Of 213 patients seen in last 5 years 34 (16.4%) had only reduced or normal pancreatic activity.
The proportion of patients who are “pancreatic sufficient” varies between 5% and 15% in various reports – in part, the variation will be related to the gene mutations present in the population described.
1960 Shwachman H. Therapy of cystic fibrosis of the pancreas. Pediatrics 1960; 25:155-163. [PubMed]
A review of management presented to the American Academy of Pediatrics in 1958 by Harry Shwachman, the most experienced CF clinician at the time, who urged caution “against discarding any form of therapy that offers relief” but avoiding “the use of harmful agents and needless operative procedures”.
The article is a pleasure to read and full of wise advice. For example, he stressed the importance of early and certain diagnosis, adequate education of the parents, seeing the patient at regular intervals, also being readily accessible for advice. On the last he comments – “clinic as well as private patients may call us on the phone whenever questions arise”.
Although often accused of advising severe fat restriction, Shwachman states that fat is allowed as tolerated. Iodides were thought to be helpful in thinning the viscid secretions, intramuscular or aerosol pancreatic trypsin were not recommended nor were carbon dioxide inhalations but the mist tent, with a 10% solution of propylene glycol and 3% saline, was helpful as were “English” methods of physiotherapy. Antibiotics were central to treatment but the parenteral route was rarely used – a major difference to present day treatment. Oral chlorotetracycline or oxytetracycline, at times were combined with erythromycin or a sulphonamide, and aerosol penicillin and streptomycin or neomycin and polymyxin.
It is interesting, in view of the present role of macrolides, that both Harry Shwachman and Margaret Mearns appeared to find erythromycin was helpful.
1960 Feigelson J. The treatment of mucoviscidosis or cystic fibrosis of the pancreas. Bull Mem Soc Med Paris 1960; 9:4-17.
Jean Feigelson of Paris is one of the pioneers of CF care and still, in 2011 attending CF conferences in Europe and North America. He trained in paediatrics at the Sick Children’s Clinic in Oslo in 1952. In a career spanning over 45 years he has treated over 250 people with cystic fibrosis.
This is Jean Feigelson’s first recorded paper on cystic fibrosis. His most recent is as a co-author, on partial splenectomy, and was published in 2007 (Louis D et al, Pediatr Pulmonol 2007; 42:1173-1180). He has 48 references noted in Medline produced steadily over 40 years.
1964 Cystic Fibrosis. A symposium. Report of a meeting on 28th May 1964 at the Wellcome Foundation London. Chest and Heart Association.
This was one of the first, if not the first, substantial CF meeting in the UK. Chaired by Professor Douglas Hubble of Birmingham. The contributors included most of those in the UK who had significant involvement with CF at the time including Drs Winifred Young, Archie Norman, Tony Jackson, John Batten, Cedric Carter, Lynne Reid and David Lawson.
Dr Lloyd Rusby, of the Chest and Heart Association, noted that the Cystic Fibrosis Research Foundation was started in 1962 to raise funds for further research; also a group of parents based in Somerset “devote largely to the exchange of emotive and dismal family news”.
Sir Robert Johnson describes how attempts were made to absorb this Somerset Group in the Chest and Heart Association and to make that the main Cystic Fibrosis organisation in the UK but fortunately that failed as the charity would have been concerned with too wide a range of disabilities to give adequate emphasis to cystic fibrosis. However, these efforts gave rise to considerable concern until the Cystic Fibrosis Research Trust was formed (1964 details below).

Archie Norman

Lynn Reid
Among the presentations at this meeting, Lynne Reid (scientist at the Brompton Hospital) implied that CF resulted in an abnormality of mucus which predisposed to infection and this abnormality could occur at an early stage but did not seem to be present at birth and “what is not so clear is why infection arises from impaction of uninfected mucus”. “Perhaps the proportion of the different cell types is abnormal; from this, differences in the final constitution of the final secretion may follow”.
Archie Norman (paediatrician, Great Ormond Street) gives a detailed account of the clinical features ending – “To sum up cystic fibrosis should be remembered as a possibility in a newborn baby who takes his feeds well and yet fails to thrive, in an older baby who develops whooping cough and in the toddler with rectal prolapse. It should be considered in any older child with clubbing of the fingers or with a cough that never quite clears up”.
John Emery (paediatric pathologist from Sheffield), discussing the laboratory aspects concluded – “I suggest that you do not send 24-hour specimens of stool to the laboratory for quantitative fat. A half minute scan of a drop of stool under the

John Emery
microscope will usually tell you much more”. 20% trichloracetic acid is advised to test meconium for the increased protein in meconium ileus and the X-ray plate method for tryptic activity. After a review of the various tests available
Winifred Young
including the sweat test Emery wisely observes “Cystic fibrosis is by no means an ‘all or none’ disease and in my opinion should never be diagnosed or excluded on a single test”.
Winifred Young (“research clinician” Queen Elizabeth Hospital Hackney, London) one of the leading CF paediatricians describes how their treatment at the Queen Elizabeth Hospital was intensified in 1955 due to their failure to arrest the incidence and progress of the pulmonary complications.
Tony Jackson
Tony Jackson,(consultant paediatrician, London), reviews the improvement in outlook that occurred following this change. Criteria for adequate antibiotic therapy were now considered to be –
1.Early treatment of the first lower respiratory infection with high doses of antibiotics by aerosol and other routes until clinical recovery and elimination of Staphylococcus aureus as judged by three negative swabs.
2.Continuous antibiotic prophylaxis for at least three months after lower respiratory infections.
3. Prophylaxis with antibiotics intermittently during subsequent upper respiratory infections.
4. Adequate treatment of all subsequent lower respiratory infections.
Considerable emphasis was placed on maintaining adequate nutrition and nearly half their patients were above the 25th centile
David Lawson
for weight.
David Lawson (paediatrician Carshalton, London) gave a thoughtful concluding talk on the future. As “there is as yet no wisp of smoke over the horizon of our knowledge” “we must deal with the problem as it is”.
This symposium gives an insight into the situation regarding CF as seen by the very few professionals in the UK who were familiar with the condition at that time.
1964 Matthews LW, Doershuk CF, Wise M, Eddy G, Nudelman H, Spector S. A therapeutic regimen for patients with cystic fibrosis. J Pediatr 1964; 65:558-575. [PubMed]
Dr Doershuk recalls that Dr William Wallace, Chairman of Paediatrics at the Babies and Children’s Hospital, Cleveland had been approached in 1957 by a parents’ organisation – the “Cousins Club” – one of whom had already lost a child with CF and had another deteriorating from the condition. They asked Dr Wallace to start a “research orientated treatment programme for CF” which they offered to fund. To develop this programme Dr Wallace appointed a young paediatrician, Dr Leroy Matthews (figure) to plan and initiate the “comprehensive and prophylactic (preventive) treatment programme” for the treatment of cystic fibrosis. The programme which developed eventually became the model for the CF Foundation CF centres programme (also Doershuk et al, 1964 & 1965 below).
 |
| Carl Doershuk. From Postgraduate Medicine 1966; 40:550-562. |
 |
| LeRoy Matthews. From Postgraduate Medicine 1966; 40:550-562. |
Three important areas of treatment were the obstructive pulmonary lesion, the secondary infections and the pancreatic deficiency and nutritional state. Treatment was early and comprehensive even started before symptoms – where this group differed from others and, as such, were far ahead of their time.
This paper describes the “comprehensive therapeutic regimen” which so influenced CF care in N America..
Veteran CF physician Dr Warren Warwick of Minnesota has “fond memories of two great stars – Harry Shwachman and Leroy Matthews”. Of Leroy Matthews he writes – “Leroy Matthews, the greatest genius CF has seen, single handedly established the value of Comprehensive Treatment, laid the ground work for Pediatric Pulmonology, organised and led the CF Centres as well as planning and directing excellent research. He made only two mistakes. He allowed his “Comprehensive Treatment” plan to be equated with “mist tent therapy” so when the mist tent was discredited many also felt the Comprehensive Care Program was discredited. And he tried too hard to control his diabetes and suffered hypoglycaemic brain injury and cardiovascular complications” (Warren Warwick in Doershuk CF (ed). Cystic fibrosis in the 20th Century. AM Publishing, Cleveland 2001:319)
1964 Doershuk CF, Matthews LW, Tucker AS, Nudelman H, Eddy G, Wise M, Spector S. A 5 year clinical evaluation of a therapeutic program for patients with cystic fibrosis. J Pediatr 1964; 65:677-93. [PubMed]
A detailed evaluation of the results of the Cleveland comprehensive therapeutic regimen. 96 consecutive patients were followed for 18 to 60 months (average 37 months) and evaluated using a modified Shwachman score. 82% improved, 11% remained the same, and 4% showed progression beyond their initial status and only 3% died – none were less than five years of age. Patients who were regarded as having reversible pulmonary changes were reviewed separately in 1965 (Doershuk et al, Pediatrics 1965; 36:675 below).
1965 Doershuk CF, Matthews LW, Tucker A, Spector S. Evaluation of a prophylactic and therapeutic program for patients with cystic fibrosis. Pediatrics 1965; 36:675-688. [PubMed]
Good results were reported in the group of children treated prophylactically with little progression over an average of 4.5 yrs. The early intervention and prophylactic approach was not the usual policy at this time and most clinicians waited until symptoms developed – even experts such as Paul di Sant’Agnese. In this study 98 consecutive patients had been followed for an average of 4.5 years and the clinical course of 49 were considered to be on prophylactic therapy was significantly different from the accepted natural course of the disease and from the 49 patients who had irreversible lung damage when first seen. No evidence of significant progression of the pulmonary state was seen in any of the prophylactic group. No deaths occurred in this group and the annual mortality rate was only 2% for the whole group. Their findings supported the need for early diagnosis and prophylactic treatment.
Sydney Gellis
Dr Sydney Gellis (always a sceptic regarding the treatment of cystic fibrosis!!) commenting in the Year Book of Pediatrics questioned whether more mild cases had been included; also whether the improved survival could not have been due entirely to antibiotics and to none of the other methods of treatment described such as mist tents, aerosols, segmental postural drainage. di Sant’Agnese also observed that in one series of older patients (Shwachman et al, 1965) the diagnosis had not been made in many until teen age years suggesting they had a milder form of CF.
Certainly patients with CF diagnosed later in childhood, who were included in some of the early adult series, undoubtedly more frequently would have had milder CF gene mutations as was confirmed in later studies (Gan K-H et al, 1995 below).
Rather surprisingly di Sant’Agnese questioned the need to start the full prophylactic programme in all patients as soon as the diagnosis is made and agrees with most other clinicians that treatment is not started “until there is indication of incipient pulmonary involvement”. This view regarding the start of treatment is interesting and in these days of neonatal screening, failure to start early microbiological monitoring, early eradication treatment of respiratory pathogens and early nutritional intervention, would nowadays be regarded as unacceptable.
1970 Shwachman H, Redmond A, Kon-Taik Khaw. Report of 130 patients diagnosed under 3 months of age over a 20-year period. Pediatrics 1970; 46:355-343. [PubMed]

Aileen Redmond
This was a classic paper from Harry Shwachman’s unit involving Aileen Redmond, a young paediatrician from Belfast who was working in Boston at the time and who later became director of the Northern Ireland Paediatric CF unit at the Belfast Children’s Hospital. Patients who had been diagnosed aged less than 3 months between 1949 to 1969. Group A – 63 before symptoms, Group B-13 with mild symptoms, and Group C – 54 diagnosed with symptoms requiring hospitalisation. There were 29 deaths – 11 (15%) in groups A and B and 18 (33%) in group C. Of the 101 survivors 14 were in excellent condition, 71 mildly affected and 12 moderately or severely ill. The calculated survival to 20 years was 77%. The authors mention that the first major treatment advance was chlortetracycline in 1948, pancreatin since 1951; mist tents from 1954; and physiotherapy since 1955.
Jim Littlewood & Margaret Mearns
The authors concluded that -”Better health and prolonged life result from early diagnosis and vigorous therapy”
1972 Mearns MB. Cystic fibrosis in infancy and early childhood. Arch Dis Child 1972; 47:5-11.[PubMed]
Margaret Mearns, at the Queen Elizabeth Hospital for Children, Hackney Rd, London was one of the few UK paediatricians with considerable experience in treating children with CF. She wrote “Most patients admitted in early infancy and treated since 1957 remain free of detectable lung damage up to the age of five years. Vigorous treatment and attempts to control and eradicate infection in infancy can prevent most of these patients from becoming chronic respiratory invalids in early childhood”. Of 76 patients between 1950 and 1964 – 30 were pre-1957 and 46 after 1957 and they had more vigorous treatment including continuous anti-Staphylococcal antibiotics for the first year and they were in better condition at five years.
None of Margaret Mearns children were treated with mist tents which were very popular throughout the Sixties in the USA (see Lawson D, 1972 below for comment). However, Carl Doershuk and others from Cleveland commented and emphasised that, although they believed mist tents to be beneficial, they had NEVER implied they were the main reason for the improved survival but emphasised their overall approach of early diagnosis, prompt and comprehensive care and wherever possible prophylactic (maintenance of normal hygiene) care. Their results were comparable with Mearns’s – continuous antibiotics and no mist tents (London) vs. mist tents and discontinuous antibiotics (Cleveland).
The final paragraph of these Cleveland paediatricians deserves a full quote exemplifying the attitude adopted by most successful CF paediatricians and physicians –
“The central issue seems to us to be not how little one can do in treating a progressive life-threatening disease; but rather how effective a programme one can develop and maintain for long term home management of these patients. In our opinion each measure recommended for long term management works best in conjunction with the other measures. However, the continued presence of a concerned and interested physician, routine regular outpatient visits and respiratory cultures cannot be replaced in any way and must be repeatedly emphasised”.
This central theme comes through from all the really successful CF centres and clinicians.
1972 Lawson D. Cystic fibrosis – Assessing the effects of treatment. Arch Dis Child 1972; 47:1-4. [PubMed]
Commenting on the preceding paper on CF treatment by Margaret Mearns (1972 above), David Lawson observes “The results are a remarkable tribute to the work of the clinical service led and inspired by the late Dr. Winifred Young and I do not think they can be matched in the literature of the period”.
David Lawson asked the interesting and really fundamental question – “How much is the course of the disease, as shown in its natural history untreated (i.e. rare survival beyond the second year), an inevitable peripheral result of the genetic defect? And how much is this due to the interaction of controllable environmental factors with these biochemical and structural remote effects of the gene?”
David Lawson’s question has been, in part, answered for over the years we have seen that the increasingly effective control of environmental factors and the secondary effects results in an impressive increase in survival before the genetic defect is amenable to treatment.
This editorial is a lengthy review of the situation at the time and of the 1971 meeting of the European Working Group for Cystic Fibrosis, was by one of the leading UK CF paediatricians who already saw the need for neonatal screening and treatment before symptoms become established. “Cases must be diagnosed before they come into trouble to a clinician: and sophisticated co-operative recording and analysis of prospective studies are necessary if future treatment is to be based upon emerging fact rather than upon disparate opinion”
1974 Crozier DN. Cystic fibrosis: a not so fatal disease. Pediatr Clin North Am 1974; 21:935-948. [PubMed]

Douglas Crozier presenting “Breath of Life Award” to Maureen McChesney (With permission)
This paper gives an idea of treatment at the Toronto CF clinic (figure 11 main text) in the early Seventies. Douglas Crozier, who started the Toronto CF clinic in 1958, stated that “success of treatment will depend on a complete assessment of the patient and then continuing attempts to obtain normal bodily function and maintain it”. He described how he advised his patients to abandon the traditional low fat diet and used of very high doses of pancreatic enzymes (up to 100 Cotazym capsules per day). Crozier believed that “to deprive a child with cystic fibrosis, who usually has very little subcutaneous fat, of this important nutrient seems ridiculous”. The superior nutritional state of the Toronto patients is believed to be the main reason for their better long term survival. In 1973, 428 people with CF were attending the Toronto clinic of whom 92 (21.4%) were 16 years or older – this was quite remarkable for that time.
I was profoundly influenced by this landmark paper from Toronto regarding the approach to management of people with CF – also by a later visit to Henry Levison at the Toronto CF clinic and attendance at the 8th International Cystic Fibrosis Congress there in 1980.
1974 Mearns MB. Cystic fibrosis. Brit J Hosp Med 1974; Oct: 497-506.
This is a detailed overview of the situation in the UK by Margaret Mearns one of the leading authorities on CF at the time at one of the few UK paediatric CF units at the Queen Elizabeth Hospital for Children in London. Warren Warwick and Pogue constructed life tables on these children attending the QE Hospital for Margaret Mearns. There was an estimated survival rate of 72% at 12 years and 45% at 20 years (figure 6).
These survival figures were a tribute to the excellent care the children received at the QE Children’s Hospital from Margaret Mearns and Winifred Young – results in sharp contrast to the outlook for children with CF in most of the UK most of whom did not attend a specialised CF clinic.
 |
| Fig. 6: Survival curve from article. With permission. |
1976 Stern R, Boat TF, Doershuk CF, Tucker AS, Primiano FP Jr, Matthews LW. Course of cystic fibrosis in 95 patients. J Pediatr 1976; 89:406-411. [PubMed]
Robert Stern
From the LeRoy Matthews and Carl Doershuk team at Cleveland reporting the long term results of their comprehensive system of management (Matthews et al. J Pediatr 1964; 65:558-575 above): these were the 95 patients they reported in 1964 after a mean follow up period of 14 years (minimum 13 years). Of the 45 diagnosed before extensive lung damage only one had died and none were disabled. Of the other 50 diagnosed after substantial lung damage 26 had died – mortality being greater in females.
Factors contributing to better prognosis were considered to be early diagnosis, aggressive management and comprehensive care, easy access to specialised care and improved antibiotic therapy.
The observations of this group on achieving successful treatment include – early inpatient treatment before significant lung damage in optimal facilities, as and when needed with flexible arrangements for daily absences, outpatient appointments throughout the week including Saturdays. Follow-up exclusively by a centre physician – usually the same physician each visit. All decisions are made by a CF centre physician.
1976 Wood RE, Boat TF, Doershuk CF. State of the Art. Cystic Fibrosis. Am Rev Respir Dis 1976; 113:833-878. [PubMed]

Robert Wood
Dr Robert Wood provides an excellent very detailed review (with 500 references) of the situation in 1976 in the USA when the 50% survival there was 15 years. The discussion of mist tent therapy, which was falling out of favour at the time, was particularly interesting. Woods mentions that early studies were encouraging (Doershuk et al, 1968 above; Matthews et al, 1967 above) but later studies had not shown a beneficial response (Motoyama et al, 1972 above; Chang et al, 1973 above). However, although studies of radioactive aerosols showed little radioactivity in the lungs (Wolsdorf J et al. Pediatrics 1969; 43:799; Bau SK, et al. Pediatrics 1971; 48:605). Woods suggests that significant deposition may have been masked by the rapid absorption of the radioactive aerosol which was known to occur. He questioned the techniques used in some of the aerosol studies and noted that, at bronchoscopy, he had observed large amounts of mist particles reaching at least the subsegmental bronchi even during nasal breathing. In fact he considers it possible that the radioactivity at any particular site may bare little relation to the amount of fluid deposited.
The implication of these observations was that the final word had not been said on mist tent therapy. This is all particularly relevant now in view of the present belief that the low salt theory and drying of the epithelial surfaces accounts for the increased viscosity and easy tendency to infection within the airways. It is worth recalling that highly experienced clinicians such as Shwachman, di Sant’Agnese and particularly Leroy Matthews all were impressed by the benefits of mist tent therapy as were some patients who took part in the Toronto studies (Chang et al. 1973). More recently inhaled hypertonic saline has shown significant benefit (Elkins et al. 2006 below) and is also tolerated by infants in whom a trial is to be undertaken.
1980 Mearns MB. Natural history of pulmonary infection in cystic fibrosis. In: Perspectives in Cystic Fibrosis. Ed: Sturgess JM. Toronto 1980; 325-334.
An interesting review, by one of the UK’s few paediatric CF experts, describing the gradual transition from Staphylococcus aureus infection and the gradual increase in Pseudomonas aeruginosa. This was considered to be due to an increasing use of antibiotic therapy and perhaps changes in the bacteria in the environment.
1981 Schiotz PO, Hoiby N, Flensborg EW. Cystic fibrosis in Denmark. In: Warwick WJ. Ed: 100 years of Cystic Fibrosis. Minnesota 1981:141-146
 |
| The Rigshospitalet in Copenhagen where the CF unit is based (from Wikipedia website) |
A report describing the Copenhagen regimen including the practice of giving 3-monthly IV anti-Pseudomonal antibiotics to patients who were chronically infected. This practice was not accepted by most CF clinicians but at that time there was a great discrepancy between the CF care and results in most parts of the UK and the intensive approach to care in the Copenhagen CF centre (figure 7). The regimen was introduced to anticipate and prevent the deterioration of lung function after a course of IV antibiotics (also Szaff et al. 1983 below).
It should be noted that regular inhaled anti-Pseudomonal antibiotics were not used in Copenhagen at this time to stabilise the chest infection between the courses of IV antibiotics. The use of regular inhaled antibiotics, largely influenced by Margaret Hodson’s 1981 paper (Hodson et al, 1981) had a favourable influence on stabilising the chest infection making 3 monthly courses of IV antibiotics less necessary in some patients.
1986 Littlewood JM. An overview of the management of cystic fibrosis. J R Soc Med 1986; 79 (Suppl. 12): 55-63. [PubMed]
A detailed review of treatment in 1985 at the first of many annual meetings on CF organised over more almost 30 years, at the Royal Society of Medicine, London by Prof. Tim David of Manchester.

Jim Littlewood
Although by now an experienced general paediatrician, I was a relative newcomer to CF compared with some of the audience. However, I had seen many new patients for full assessments over the previous five years from many different hospitals – well over a 100 new patients by 1984. Drawing from this experience and the literature, I tried to describe the areas where treatment appeared to make a significant difference to the long term outlook. A major problem was to communicate the established facts to the hundreds of clinicians each of whom is responsible for the long term management of only a few CF patients, and each of whom had numerous conflicting demands on his/her time ranging from neonatal intensive care to child abuse. Such paediatricians rarely had the opportunity to attend major CF meetings in Europe or North America as they had so few affected patients. So this was a very detailed account of modern CF care with a plea for some form of CF centre specialist care for all – either full care or shared with the local hospital as already recommended by the British Paediatric Association Working Party.
Surprisingly, there was still considerable opposition to the concept of CF centre care by many UK paediatricians.
I concluded at the time that “if the outlook for CF patients in the UK was similar to that expected in large CF centres both here and overseas, these suggestions (of some centre care for all) would be superfluous. However, it is not and until such time as it is we must give such an arrangement a trial for the sake of CF patients and their families”.
I felt very strongly about this issue having by this time seen so many children with CF referred to Leeds for Comprehensive Assessment during the preceding 5 years who had been severely under-treated by modern standards (Littlewood et al, Comprehensive clinical and laboratory assessment in cystic fibrosis. In: Lawson D, editor. Cystic Fibrosis: Horizons. Chichester: John Wiley, 1984:266; Littlewood et al, 1988 below; Littlewood 1993 below).
1987 Pedersen SS, Jensen T, Hoiby N, Koch C, Flensborg EW. Management of Pseudomonas aeruginosa lung infection in Danish cystic fibrosis patients. Acta Paediatr Scand 1987; 76:955-961. [PubMed]
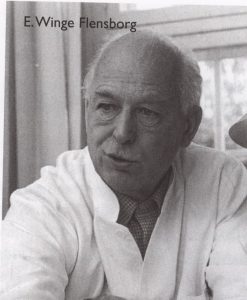
Erhard Flensburg

Christian Koch, Birgitte Frederikson, Niels Hoiby & Jim Littlewood. Copenhagen 1997
This is one of the main publications justifying the Danish policy of 3-monthly courses of intravenous antibiotics for patients chronically infected with Pseudomonas – a policy which has never been subjected to an acceptable clinical trial and as mentioned above was initiated before the advent of inhaled antibiotics.
The annual mortality rate of cystic fibrosis patients with chronic P. aeruginosa lung infection at the Danish CF-centre ranged from 10 to 20% in the years 1970-1975 – in this period the patients received anti-Pseudomonal chemotherapy only during acute exacerbations of infection. From 1976-1979 patients who acquired chronic P. aeruginosa infection were given regular and intensive anti-Pseudomonal treatment three to four times per year. The patients were followed for 6-12 patient-years; seven died and the 10-year survival rate after onset of P. aeruginosa infection was 90% (+/- 4%). The annual mortality rate is now only 1-2%. Although precipitating antibodies against P. aeruginosa increased significantly, pulmonary function did not deteriorate with duration of infection.
An unwelcome consequence was an increase in cross-infection between patients associated with more frequent hospitalisation and an increased incidence of new P. aeruginosa infection in 1976 which was steadily reduced, starting in the late Seventies, by improved hygienic measures and a new ward in the CF centre.
1988 Littlewood JM, Kelleher J, Rawson I, Gilbert J, Firth J, Morton S, Wall C. Comprehensive assessment of patients at a CF centre identifies suboptimal treatment and improves management, symptoms and conditions. 10th International Cystic Fibrosis Congress, Sydney 1988 Excerpta Medica Asia Pacific Services. 89-90.
This poster from Leeds reported the findings of the first 250 new patients with CF referred to our Leeds unit between May 1980 and September 1987 for what we termed “Comprehensive CF Assessments” and advice. It was because we offered to carry out Comprehensive Assessments on other paediatricians’ patients, without taking over the care of the majority of the patients, that the service we offered developed so rapidly during the Eighties.
During two day-long visits to the Leeds Regional CF Unit the patients underwent a detailed review of their past history, symptoms, treatment, physical state and diagnosis. There was a confirmatory sweat test, assessment by the dietitian (Clare Wall) and physiotherapist (Sue Morton), respiratory function tests (Jeanette Firth) chest and abdominal X-rays and abdominal ultrasound. Sputum culture, detailed haematology, biochemical and immunological blood tests including fat soluble vitamin levels and a faecal fat and chymotrypsin estimation were performed. The day finished with an hour with the CF consultant (Jim Littlewood) who by then had considerable detail about the patient available including the referral letter form their paediatrician, the extensive data obtained by our permanent CF clinic doctor, nurses, dietitian, physiotherapist, respiratory function tests and chest and abdominal x-rays (also Littlewood et al, 1984 above; Littlewood et al, 1993 below).
Both the treatment and the physical state were frequently found to be suboptimal and, it must be said, reflected treatment in many general hospitals in the UK during the Eighties. For example of our first 250 referred patients, the diagnosis was incorrect in 7 (3%), the chest was obviously under treated in 30%, physiotherapy was suboptimal or not preformed at all in 60%, the energy intake was inadequate and less than 120% of the recommended daily allowance in 75%, pancreatic supplements inadequate in 40% and vitamin supplements insufficient resulting in suboptimal plasma levels in 60%.
 |
| Clinical progress of a typical child referred at that time. |
 |
| Respiratory function peak expiratory flow rates of same patient as in Fig 45 during treatment. |
 |
| One hundred new referrals 1988 -1992. Previous 100 new referrals 1985-1987 bracketed.(Littlewood, 1993) |
A girl of 12 years who was admitted when referred for Comprehensive Assessment as the state of her chest was so bad. Before referral from her local hospital she had never had IV antibiotics although she was chronically infected with Pseudomonas aeruginosa. She was given 3 weeks intravenous anti-Pseudomonal antibiotics and physiotherapy with a dramatic response in clinical score, weight and laboratory findings (figure 8) and respiratory function (figure). This was the type of patient referred to as “under-treated.” Unfortunately, although such patients improve dramatically for a few years when treated, some then deteriorated despite treatment, as did this girl, who died aged 15 years.
1993 Littlewood JM. The value of comprehensive assessment and investigation in the management of cystic fibrosis. In Clinical Ecology of Cystic Fibrosis. H Escobar, CF Baquero Suarez (Eds). Elsevier Science Publishers. 1993:181-187.[Conference publication]
This was a report of the 427 new patients seen at the Leeds CF centre for a Comprehensive CF Assessment between 1980 and 1992, 364 of whom had at least one follow-up assessment. They were referred from 10 hospitals in Yorkshire and a further 26 hospitals in the UK. The details of their management and condition are recorded and a comparison made between a previous 100 referral between 1985 and 1987 and 100 new referral between 1988 and 1992 showing improvement in their condition in a number of areas reflecting the general improvement in CF care in the UK (figure 10). The details give an idea of the condition of the patients at the time. (See also Littlewood et al, 1984 above; Littlewood et al, 1988 above)
1997 Drittanti L, Masciovecchio MV, Gabbarini J, Vega M. Cystic fibrosis: gene therapy or preventive gene transfer? Gene Therapy 1997; 4:1001-1003. [PubMed]
I was very impressed by this, not widely known, paper for it accurately described the situation clinicians, who followed many patients year after year, had been observing in the clinic. Patients’ respiratory function tests are usually stable before chronic infection (usually Pseudomonas) becomes established but begin a slow deterioration after chronic Pseudomonas infection becomes established i.e. they pass the “point of no return” .
These authors suggested that before the onset of chronic infection people with CF can be considered to be in the phase of “CF Disease” i.e. they have various physicochemical alterations in the electrolyte and liquid composition of the airway fluid but no tissue damage. Although they get respiratory infections these can be eradicated, if treated early with antibiotics and their respiratory function remains stable. However, eventually a new respiratory infection is not eradicated and chronic infection of the tissues becomes established. At this stage the patient then enters the phase of “Lung disease” where infection and chronic inflammation become established, self perpetuating and progress independently of the basic CFTR abnormality – this change is referred to as the “Point of no return” and there follows a slow deterioration in their condition, the speed of which is determined by the type and intensity of treatment they receive.
So the aim of modern treatment is to avoid passing the “Point of no return” i.e. prevent or delay for as long as possible the onset of chronic infection of the airways. So it can be appreciated that if the airway cultures are repeatedly positive for Pseudomonas, even if the patient has few or even no symptoms (as in the paper by Konstan et al, above), he already has passed the “Point of No Return”.
1998 Mahadeva R, Webb K, Westerbeek RC, Carroll NR, Dodd ME, Bilton D. Clinical outcome in relation to care in centres specializing on cystic fibrosis: cross sectional study. BMJ 1998; 316:1771-1775. [PubMed]
This is one of the few papers which is accepted as supporting the superiority of CF Centre care to the care received at a general paediatric clinic in the local hospital. Patients at the adult cystic fibrosis centre were subdivided into three groups. Those who had received continuous care from paediatric and adult cystic fibrosis centres (group A), those who had received paediatric care at their local hospital then at an adult CF centre (group B) and those who had received neither paediatric nor adult specialist care (Group C). Body mass index was 21.3, 20.2 and 18.3 for Groups A B and C respectively (P<0.001) and the improved nutritional status was correlated with a higher FEV1 and better chest X-rays (P<0.001 for both).

Kevin Webb
These findings are widely quoted as providing the first direct evidence that management in cystic fibrosis centres resulted in a better clinical outcome. This had been appreciated for years by doctors dealing with people with CF, and indeed by patients and parents, but is still contested by a minority of general paediatricians and physicians.
Professor Kevin Webb started the first CF centre for adults at Monsall Hospital Manchester in 1982; the unit later moved to the purpose-built Bradbury Unit at Wythenshawe Hospital in 1994. The CF Centre is one of the largest in the UK and the staff have made major contributions to improving CF care in the UK.
2006 Lording A, McGraw J, Dalton A, Beal G, Everard M, Taylor CJ. Pulmonary infection in mild variant cystic fibrosis: implications for care. J Cyst Fibros 2006; 5:101-104. [PubMed]
Few reports document the condition of the airway in infants and young children with apparent “mild” disease. A retrospective cohort study was carried out comparing frequency of bacterial isolates and clinical outcomes in eleven compound heterozygotes for DeltaF508 and a second mild mutation, mainly R117H, with a matched group of DeltaF508 homozygotes. Staphylococcus aureus was isolated in 8 of the 11 patients with mild variant disease and Pseudomonas aeruginosa found in 7 (64%), although the frequency of positive cultures was significantly less (2.8/year) than the DeltaF508 homozygotes (6.1/year). Shwachman scores were significantly higher in patients with mild mutations (94(74-92) vs. 88 (77-91)); there was also a small but significant difference in chest radiograph (Chrispin-Norman) scores although little difference in lung function.
This is a timely paper from Sheffield UK stressing that most patients with so-called “mild variant CF” will nonetheless have bacterial isolates from their airway cultures requiring antibiotic therapy three to four times a year. Infection with both S. aureus and P. aeruginosa is common. Also they are slowly deteriorating with respect to respiratory function. Anti-staphylococcal prophylaxis for the first three years should be considered. It is vitally important these “mild” patients are followed carefully by a team experienced in CF care and treated vigorously to prevent their changing into “severe cases”. They deserve just as careful treatment and follow-up as those with more obvious symptoms and signs.
2009 Ouyang L, Grosse SD, Amendah DD, Schechter MS. Healthcare expenditure for privately insured people with cystic fibrosis. Pediatr Pulmonol 2009; 44:989-996. [PubMed]
The authors estimated medical care expenditures, including both insurance reimbursements and patient out-of-pocket expenses, for privately insured people with CF and investigated how those expenditures varied with certain complications of CF during 2004 to 2006. They were compared with a matching group of people who did not have CF and examined the effect of age and certain complications of CF on these expenditures. The annual medical care expenditure for a person with actively managed CF averaged $48,098 in 2006 dollars, which was 22 times higher than for a person without CF. This ratio is high relative to other chronic disorders. Outpatient prescription medications made up the largest component of total expenditures for people with CF (39%). Those who were recorded in claims data as having a liver or lung transplant, malnutrition, diabetes, or a chronic Pseudomonas aeruginosapulmonary infection incurred much higher expenditures than people without these conditions. People with CF will incur high medical expenditures throughout their life span. These findings will assist in the development of economic evaluations of future CF screening and management initiative
This is one of a number of studies recording the very high cost of modern CF care which is some circumstances seriously interferes with the provision of optimal treatment even in the UK NHS where treatment is free. It is likely that cost will become an increasingly difficult problem as more treatments for the basic defect become available. in 2012/13 this became a major problem with regard to the cost of ivacaftor.
2016 Massie J; Robinson PJ; Cooper PJ. The story of cystic fibrosis 1965-2015 J Paediatr Child H 2016 Sep 1. [PubMed] There have been dramatic changes in the care of children with cystic fibrosis (CF) from 1965 to 2015. The initial improvements were the result of incremental gains in medical knowledge and better use of available therapies. Some CF-specific drugs were developed (recombinant human DNase and purified tobramycin for inhalation), but these simply delayed the progression of the lung damage. The discovery of the CF transmembrane conductance regulator gene in 1989 created an explosion of knowledge of airway biology and CF pathophysiology. Now mutation-specific therapy to potentiate mutated CF transmembrane conductance regulator is available for some patients with CF and is transforming their lives. Further advances are eagerly anticipated to benefit all patients with CF.
Marco Zampoli, Janine Verstraete, Marlize Frauendorf, Reshma Kassanjee, Lesley Workman, Brenda M Morrow, Heather J Zar Cystic fibrosis in South Africa: spectrum of disease and determinants of outcome. ERJ Open Res 2021 Aug 2;7(3):00856-2020.doi: 10.1183/23120541.00856-2020.eCollection 2021 Jul. 34350279 Free PMC article

Marco Zampoli
Introduction: Little is known about cystic fibrosis (CF) in low- to middle-income settings. This study aimed to describe the spectrum and outcomes of CF in South Africa (SA) from the recently established SA CF registry (SACFR).
Methods: Demographic, diagnosis and clinical data were extracted from the SACFR. Cross-sectional univariable and multivariable regression analysis of best forced expiratory volume in 1 s (FEV1; age≥6 years) and nutrition (all ages) in 2018 was conducted to investigate factors associated with severe lung disease (SLD; FEV1 ≤3.0 z-score) and undernutrition.
Results: By December 2018, ancestry of 447 individuals included in the SACFR was Caucasian (315; 70%), mixed (87; 19%) and black African (41; 9%). Median diagnosis age was 7.6 months (IQR 2.7-37.1). Genotype was p.Phe508del homozygous (220; 49%); p.Phe508del heterozygous (144; 32%) and neither p.Phe508del or unknown Cystic Fibrosis Transmembrane Conductance Regulator (CFTR) variant in 83 (19%); the second most frequent CFTR variant was 3120+1G>A, common in black Africans. Median age of patients in 2018 was 14.7 years (IQR 7.4-24.4). SLD was independently associated with chronic methicillin-resistant Staphylococcus aureus (MRSA) (adjusted odds ratio( aOR) 16.75; 95% CI 1.74-161.50), undernutrition (aOR 5.20; 95% CI 2.23-12.13) and age (aOR 2.23 per 10 years; 95% CI 1.50-3.31). Undernutrition was associated in univariable analysis with low weight at diagnosis, non-Caucasian ancestry, chronic P. aeruginosa infection and lower socioeconomic status.
Conclusion: Interventions targeting MRSA infection and nutrition are needed to improve CF outcomes in SA. Most people with CF in SA are eligible for highly effective CFTR modulator therapy.
Dr Marco Zampoli is a paediatric pulmonologist in the Dept. of Paediatrics and Child Health, University of Cape Town, Cape Town, South Africa.
South African MRC Unit for Child and Adolescent Health, University of Cape Town, Cape Town, South Africa.
Ratjen F, VanDevanter D R. Retracing changes in cystic fibrosis understanding and management over the past twenty years. J Cyst Fibros. 2021 Sep 30:S1569-1993(21)01420-X. doi: 10.1016/j.jcf.2021.09.015. Online ahead of print.PMID: [Pubmed]

Donald R VanDevanter

Felix Ratjen
This is a very interesting article describing the quite remarkable changes which have occurred in the understanding of and outlook for cystic fibrosis since the Journal of Cystic Fibrosis was launched twenty years ago.
The state of CF art in 2002 was described. Important milestones between 2002 and 2020 were described as follows. Building of a clinical research infrastructure, encounter based registries, wide adoption of CF newborn screening, consensus treatment guidelines and Cochrane Database analyses, alternate measures of lung physiology and function, improvements in delivery of inhaled therapies, improved knowledge of airway microbiology, cf animal models, newer therapies particularly the CFTR modulators but also use of azithromycin and hypertonic saline, aztreonam and inhaled levofloxacin, efficacy studies in paediatric CF populations with mild lung disease.
The authors conclude “CF is a multi organ disease and CF research and care and compass a broad variety of disciplines, from basic science to epidemiology to drug development. The Journal of Cystic Fibrosis, which is established 20 years ago to provide coverage of this diversity in a single multidisciplinary setting, was established at a fortuitous time: as CF research productivity started and exponential increase. It is perhaps not surprising that the JCF has enjoyed a consistent growth in both interest and quality as it has mirrored and supported the expansion of our understanding of CF itself”
Felix Ratjen is Professor in the Division of Respiratory Medicine, Department of Paediatrics, Hospital for Sick Children, University of Toronto, Canada
Donald R VanDevanter is Adjunct Professor of Pediatrics in the Department of Pediatrics, Case Western Reserve University School of Medicine, Cleveland OU USA.
Kris De Boeck, J Stuart Elborn, Isabelle Fajac, Niels Hoiby. The journal of cystic fibrosis’ 20th anniversary. J Cyst Fibros 2021 Dec 11;S1569-1993(21)02157-3.doi: 10.1016/j.jcf.2021.11.016. Online ahead of print. [Pubmed]

Kris De Boeck
A very interesting account of the outstanding success of first 20 years of the Journal of Cystic Fibrosis. The Journal of Cystic Fibrosis (JCF) celebrates 20 years since its first edition and has gone from strength to strength under the leadership of exceptional Editors-in-Chief and their editorial boards. The JCF was first published in January 2002 and was the result of many discussions within the board of the relatively newly constituted European Cystic Fibrosis Society (ECFS). The vision for the journal came from then President, Prof Gerd Döring, and Prof Harry Heijerman, an ECFS board member at that time. Their vision is deeply appreciated.
– The full text of the editorial is very informative including a large table listing the Journal of Cystic Fibrosis published guidelines and consensus statements: Search on archives of the Journal (January 2002-October 2021) for ‘guideline’ or ‘consensus’ in title.
H L Barr, T Bihouee, A M Zwitserloot. A year in review: Real world evidence, functional monitoring and emerging therapeutics in 2021. J Cyst Fibros 2022 Mar;21(2):191-196.doi: 10.1016/j.jcf.2022.02.014.Epub 2022 Mar 7. Free PMC article [Pubmed]

Helen Barr
This is a comprehensive and extensively referenced review of significant areas of change and new knowledge during 2021. The Free PMC article is available and strongly recommended.
There are joint first authors. The correspondiing author is Dr Helen Barr consultant respiratory physician at the Nottingham University Hospitals NHS Trust, Nottingham, United Kingdom; Nottingham Respiratory Biomedical Research Centre, University of Nottingham, Nottingham, United Kingdom.
Adrienne P Savant. Cystic fibrosis year in review 2021. Pediatr Pulmonol 2022 May 2.doi: 10.1002/ppul.25948.Online ahead of print.[Pubmed]

Adrienne P Savant
People with cystic fibrosis (CF) have an amazing outlook with the treatment availability of highly effective modulators. Unfortunately, not all PwCF are eligible for modulators leading to continued pulmonary exacerbations and advanced lung disease. Additionally, optimizing diagnosis and evaluation for CF in the newborn period continues to be an area of focus for research. This review article will work to cover articles published in 2021 with high clinical relevance related to the above topics, however due to the extensive body of research published, this review will not be comprehensive. This article is protected by copyright. All rights reserved.
Adrienne P Savant is a paediatric pulmonologist at the Department of Pediatrics, Children’s Hospital of New Orlea
