Statistics, Survival, Type of care
There are excellent Patient Registries published annually by the CF Foundation, the Cystic Fibrosis Trust, the European CF Society and other national CF organisations
In this section there are a limited selection of publications relating to survival figures which have received attention over the years
With regard to interpretation of the survival data, the late Dr Sarah Walters has written a very clear article dealing with survival statistics which can be recommended to non-statisticians (“Survival in cystic fibrosis – what do the statistics mean?”) the full text of which is on the CF Trust website (www.cysticfibrosis.org.uk).
1966 Mantle DJ, Norman AP. Life tables for cystic fibrosis. BMJ 1966; 2:1238-1241. [PubMed]
First of a number of publications on survival in the UK from Dr. Archie Norman’s unit at Great Ormond Street, London. Life tables for 1943-1964 showed that 80% died by 5 years and 90% by 10 years. Infants with meconium ileus, 25% died by 1 week and 75% by 3 months.
Sydney Gellis, in an editorial comment in the corresponding Year Book of Pediatrics, observed that “Despite claims to the contrary, cystic fibrosis of the pancreas continues to carry a gloomy prognosis. Present day therapy is helpful but offers relatively little, and a realistic alteration of the course of the disease will require a major breakthrough in discovering the aetiology”. Gellis, although a distinguished pediatrician was not an expert on CF and in this prediction was obviously quite wrong for the outlook improved steadily over the years long before the aetiology was identified during the Eighties.
1967 Pugh RJ, Pickup JD. Cystic fibrosis in the Leeds region: incidence and life expectancy. Arch Dis Child 1967; 42:544-545. [PubMed]
Richard Pugh
This paper is included as it is one of the few reports from the UK of a survey between 1952 and 1962 from the North of England by Yorkshire paediatricians Richard Pugh of Hull and Douglas Pickup of Pontefract on behalf of the Leeds Regional Paediatric Club. During this decade 132 infants were confirmed as having CF among total of 546,764 births over 13 years – an incidence of 1/4142. Fifty six infants (42%) died in the first year.
The findings would be typical of the situation in the UK at the time where virtually all children with CF were treated at local hospitals and there were no specialised CF clinics in most towns and cities – or even in most provincial teaching hospitals. So few patients survived childhood. A significant number of affected infants must have gone unrecognised in this study for the incidence in this part of the UK is around 1/2400 births.
1967 Young WF, Jackson AD. The prognosis of cystic fibrosis. Bibliotheca Paediatrica 1967;86:350-352.
Winifred Young and Tony Jackson were paediatricians at the Queen Elizabeth Hospital Hackney where there was one of the few CF clinics in the UK which was started by Winifred Young in 1950. Margaret Mearns joined the staff there soon after.
Further data from these authors is described above in Cystic Fibrosis. A symposium. Report of a meeting on 28th May 1964 at the Wellcome Foundation London. Chest and Heart Association.
1967 Warwick WJ, Manson S. Life table studies of mortality. In Cystic Fibrosis Part I. Physiology and pathophysiology of serum secretion clinical investigation and therapy. Proc 4th Int Conf on CF. Geigy Symposium Berne/Grundewald 1966 (Modern Problems in Pediatrics Vol 10) PFI p353 Ed. Rossi E, Stoll E. Karger: Basle and New York. [Conference report]
Warren Warwick
In 2001 Warren Warwick commented “After 10 years of grants funding the US CF Patient Registry and indirectly supporting the Canadian CF Patient Registry and the beginning of the International Registry, the CF Foundation decided the Registry should become the property of the CF Foundation. When the CF Foundation took over the operation they discovered what a bargain the $10,000 annual grant was. So after spending over $100,000 and still not finishing the analysis, they decided to give up the analysis as too expensive. They were shamed into doing the analysis when the Canadian Foundation provided funds and manpower to complete the analysis. The fallout was that the Canadian Foundation went its own way and beginning the International Registry was abandoned. All the data from the first 10 years of the US Registry, including the magnetic tapes, were transferred to the CF Foundation
1968 Warwick W, Pogue RE. Computer studies in cystic fibrosis. In Lawson D (ed). Proceedings of 5th international Cystic Fibrosis Conference, Cambridge 1969; 320-330. London. Cystic Fibrosis Research Trust. [Conference]
Warren Warwick has pioneered databases in CF and was responsible for starting the CF Foundation Patient Registry. He maintains that US paediatricians initially agreed to cooperate with his first CF database as they did not believe Leroy Matthews excellent results and thought the data may confirm their suspicion! (also Warwick & Manson, 1967).
1971 George L, Norman AP. Life tables for cystic fibrosis. Arch Dis Child 1971; 46:139-143.[PubMed]
Archie Norman and colleagues produced a number of life tables for people with CF in the UK. Here 128 infants without meconium ileus (MI) and 43 with MI from 1964 for five years are compared with tables for previous 20 years showing obvious improvement in survival – suggested as being due to early diagnosis and treatment. The one year survival was 34% compared with 93%, and at five years 19% vs. 89% between the two periods.
1973 Taussig LM, Kattwinkel J, Friedewald WT, di Sant’Agnese PA. A new prognostic score and clinical evaluation system for cystic fibrosis. J Pediatr 1973; 82:380-390. [PubMed]

Lynn Taussig
Often referred to as the NIH Score, this system by Lynn Taussig (figure 3.1) and colleagues stood up to evaluation well and apparently Shwachman and Kulczycki realised that a “more accurate method of assessment might become available” than their score. Respiratory function tests were included also complications that affected prognosis such as haemoptysis, cor pulmonale and pneumothorax. Some considered that the nutritional state was under represented. This and a number of subsequent scoring systems have been discussed by a number of authors (Cystic Fibrosis Clinical Scoring Systems. Conway SP, Littlewood JM. In Cystic Fibrosis – Current Topics. Volume 3. Dodge JA. Brock DJH, Widdicombe JH, editors Chichester: John Wiley & Sons Ltd, 1996:339-358.
Dr Lynn Taussig worked with Paul di Sant’Agnese at the NIH, then as Professor at the Arizona College of Medicine for 20 years and then at the National Jewish Research Center in Denver. He was particularly active in CF care and research during the Seventies and Eighties. In 1984 he edited one of the major textbooks on the CF (Cystic Fibrosis. Lynn Taussig. New York Theime-Stratton Inc. 1984). In the introduction to the book Charles Lobeck describes Lynn Taussig, Thomas Boat and Robert Schwartz as the professional descendants of Paul di Sant’Agnese who had in turn influenced their colleagues from Cleveland, Tuscon, Rochester and other academic locations. The book contains notable chapters on the gastrointestinal system, the pancreas and the hepatobiliary system by Paul di Sant’Agnese. There many other distinguished contributors who have made significant contributions to our knowledge of CF.
1976 Stern R, Boat TF, Doershuk CF, Tucker AS, Primiano FP Jr, Matthews LW. Course of cystic fibrosis in 95 patients. J Pediatr 1976; 89:406-411. [PubMed]
Robert Stern
From the LeRoy Matthews and Carl Doershuk team at Cleveland reporting the long term results of their comprehensive system of management (Matthews et al. J Pediatr 1964; 65:558-575 above): these were the 95 patients they reported in 1964 after a mean follow up period of 14 years (minimum 13 years). Of the 45 diagnosed before extensive lung damage (Figure 18 Group1) only one had died and none were disabled. Of the other 50 diagnosed after substantial lung damage (Figure 18 Group 2) 26 had died – mortality being greater in females. Factors contributing to better prognosis were considered to be early diagnosis, aggressive management and comprehensive care, easy access to specialised care and improved antibiotic therapy.
The observations of this group on achieving successful treatment include – early inpatient treatment before significant lung damage in optimal facilities, as and when needed with flexible arrangements for daily absences, patient appointments throughout the week including Saturdays. Follow-up exclusively by a centre physician – usually the same physician each visit. All decisions are made by a CF centre physician.
1979 Phelan PD, Allan JL, Landau LI, Barnes GL. Improved survival of patients with cystic fibrosis. Med J Australia 1979; 1:261-263. [PubMed]

Peter Phelan
Three hundred and twenty patients with CF born after 1958 who were treated at Royal Children’s Hospital, Melbourne had an 80% survival to 11 yrs and a 64% survival to 18 yrs. Those managed between 1973-77, 91% survival to 12 yrs and 80% to 17 yrs. These were really excellent results for the time and were attributed, almost certainly correctly, to all patients having received Specialist CF Centre care as was later discussed in a very influential subsequent paper from Melbourne the contents of which prompted the formation of the UK Working Party on Cystic Fibrosis in 1982 (Phelan and Hey, 1984 below).
1984 Phelan P, Hey E. Cystic fibrosis mortality in England & Wales and in Victoria Australia. Arch Dis Child 1984; 59:71-83. [PubMed]
The contents of this paper had a major influence on CF treatment in the UK. In Victoria, Australia one death in 125 between the ages of 1 and 14 years was in a child with CF – in England and Wales the frequency was 1 in 44. A newborn child with CF had an 80% chance of surviving to 9 years in England and Wales and to 20 years in Victoria (figure 1 ). The better survival in Victoria during the Seventies was attributed to the Australian patients being treated at CF Centres rather than at by general paediatricians at their local hospitals. During the Seventies most UK children with CF were treated at their local hospital by general paediatricians all of whom saw only a few children with cystic fibrosis.
The authors note “It has been claimed in North America that management in a specialist centre, as in Victoria, is essential for optimal care and recent data from Denmark indicate a much better survival among patients attending a specialist clinic compared with those looked after by their local paediatrician, as happens for most children in England and Wales”.
The data in this report was available before publication through John Dodge who had visited Australia before its publication and the availability of the data was directly responsible for the formation of the British Paediatric Association’s Working Party on Cystic Fibrosis in 1982 whose terms of reference were “to assess the advantages and disadvantages of regional centres for cystic fibrosis”. For summary of the Working Party Report see Jackson 1986 (below).
John Dodge comments that he considers the original data in this report were seriously flawed because they compared mean age at death (UK) with standard survival calculations (Australia), but the point they erroneously made was of great value in setting up not only CF centres in the UK but also a CF registry, without which any data are totally unreliable!

Edmund Hey
Dr Edmund Hey, the co-author, is a UK consultant paediatrician with previous experience in neonatal physiology and paediatrics who, in 1973, became the first full time consultant respiratory paediatrician at Great Ormond Street Hospital, London; there he met Peter Phelan (figure 26) who spent a six month sabbatical there. In 1978, on the death of Gerald Neligan (the neonatal paediatrician in Newcastle, UK), Hey was invited to return to Newcastle, as neonatologist which he did. Later in 1982, Phelan invited Hey back to Melbourne to cover the sabbatical leave of a colleague; it was during this six months that Hey was involved in the present paper. When he returned to Newcastle, Hey concentrated on developing neonatal services there but later said to me (2008) “but I did watch the slow transformation of CF care across the UK with some knowledge that I had probably helped to nudge it into an important change of direction.” This is undoubtedly true!
1988 Wood RE, Piazza F. Survival in cystic fibrosis: correlation with treatment in three cystic fibrosis centres. 10th International Cystic Fibrosis Congress, Sydney 1988 Excerpta Medica Asia Pacific Services 74:79.

Robert Wood
An impressive and important, if disturbing, study presented as a poster at the 1988 Sydney CF meeting. The medical records of three US CF Centres for the years 1971-1980 were reviewed including 24,000 outpatient visits and 2000 hospitalisations. Median survival ages at the three centres were 9.5, 18.1 and 22.8 years for centres A, B and C respectively. No differences in the content of treatment between centres correlated with group survival. But for each patient year in A, B and C the mean number of outpatient visits was 4.4, 8.0 and 12.1 and the number of hospital days was 4.7, 5.0 and 9.5. – usually hospitalisations would be for IV antibiotics. Hospitalisation was considered necessary in 19.3, 20.9 and 31.2% of patients at least once a year. There was strong correlation between group survival and the use of oral and aerosolized antibiotics, vitamins E and K, and aerosols of epinephrine. When the data was separated into 1971-1975 and 1976-1980, changes in antibiotic use correlated well with improved survival. The authors concluded “more frequent outpatient visits, more aggressive use of antibiotics and more frequent hospitalisation correlate well with increasing survival”.
It is disappointing that this excellent study was never published. I suspect the marked differences between the CF centres were unacceptable and too sensitive data for publication at that time. Interestingly similar studies, some very recent, repeatedly show patients are better when seen more frequently and receive more antibiotics – which is exactly what one would expect!
1988 Dodge JA, Goodall J, Geddes D, Littlewood JM, Mearns MB, Owen JR, Russell G. Cystic fibrosis in the United Kingdom 1977-85: an improving picture. British Paediatric Association Working Party on Cystic Fibrosis. BMJ 1988; 297:1599-1602. [PubMed]
A further publication from the Working Party on Cystic Fibrosis chaired by Prof. John Dodge. The national survey included all patients with CF known to paediatricians, chest physicians and others between 1977 and 1985 or whose deaths were reported through death certification authorities in the United Kingdom. The number indicated an incidence of 1 in 2500 live births. Mortality was 7.6% in the first year and greater for females than males under 20 years of age. Survival improved through the study particularly in the first five years with 100 more births than deaths each year. In particular, death from meconium ileus was increasingly less frequent. It was estimated that there were some 5000 people with CF in 1985. (1982 Formation of UK CF Working Party above; Jackson 1986 for summary of the initial Working Party report, above; Dodge et al, 2007 final data, below)
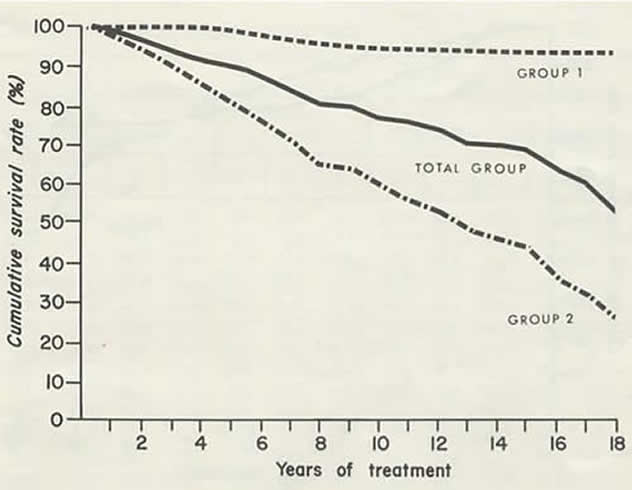
Figure 1: Survival curve from the paper by Phelan and Hey 1984. With permission from the BMJ Publishing Group.
1991 Littlewood AE, Bowler IM, Littlewood JM. A method of data collection and computerisation in use at a regional CF unit. 17th European Cystic Fibrosis Conference Denmark. June 1991. Poster 94.

Ann Littlewood
Much of the clinical research data and the smooth running of the Leeds CF clinic were dependent on the Administrator

Ian Bowler
Mrs Christine Silburn, and the clerks and secretaries.
The computer data management had been in operation since the early Eighties using first a computer funded by the Variety Club of Great Britain. Ann Littlewood (figure 25) a state registered nurse (and my wife!), was responsible for the running of our data service from the early Eighties until we both retired from clinical work in 1997.
The introduction of a Comprehensive CF Assessment service in Leeds from 1981 generated such vast amounts of data on every patient that computerisation became essential and was introduced in 1982. The system, initially using an Epson PC AX with 80Mb hard disk and 640K using Symantec Q&A software, provided a database and word processing facilities. By 1991 four databases were in use – a patient register, clinic visit database, an inpatient database and an assessment database for the results of Comprehensive Assessments. The system had been repeatedly modified and adapted over the next eight years by interested colleagues and professional computer programmers. The Leeds CF units are now totally computerised for both clinical and research purposes – a system developed by Dr Daniel Peckham, Respiratory Physician on the Adult CF Unit.
1996 Frederiksen B, Lanng S, Koch C, Hoiby N. Improved survival in the Danish center-treated cystic fibrosis patients: results of aggressive treatment. Pediatr Pulmonol 1996; 21:153-158. [PubMed]

Birgitte Frederiksen
Survival data for Danish center-treated CF patients, covering the period 1974-1993. The annual mortality rate for 1989-1993 was 0-1.2%. Using the age-specific mortality rate for 1989-1993, it was impossible to calculate the median survival probability because the curve did not fall below 50% (age up to 45 years); however, it was possible to show that the survival probability for a newborn CF child to reach his 45th birthday was 80.4% (confidence interval 76.5-84.6%). The median age at diagnosis was 0.63 years with no sex difference (surprisingly there was and is no neonatal CF screening in Denmark). The probability of surviving 40 years after the diagnosis of CF was made was 83.3% (confidence interval 80.1-86.6%).
These survival figures are considerably better than any other published survival probability at the time. The only item that I would not agree with the Danish CF centre is their policy of not screening neonates for CF.
2000 Fogarty A, Hubbard R, Britton J. International comparison of median age at death from cystic fibrosis. Chest 2000; 117:1656-1660. [PubMed]
Data from ten countries in North America, Europe, and Australasia of all persons registered as having died of CF from 1980 to 1994 were analysed by Prof. John Britton and his colleagues from Nottingham, England. The overall median age at death increased from 8 years in 1974 to 21 years in 1994. Median age at death also increased within all countries and was consistently highest in the United States. Women were significantly more likely to die at a younger age than men.
The median age of death is one of the basic indicators of survival. It is encouraging that the median age of death steadily increases each year as the effect of better treatment is reflected in better survival. The relatively recent figures for median age of death for patients registered with the UK CF Patient Registry are encouraging – in 2002 the median age of death was 23 yrs, in 2003 24.2 yrs and in 2004 25.6 years and in 2008 it had risen to 27 years.
The late Dr Sarah Walters has written a very clear article dealing with survival statistics which can be recommended to non-statisticians (Survival in cystic fibrosis – what do the statistics mean?) the full text of which is on her website (www.cfstudy.com) and also on the CF Trust website (www.cftrust.org.uk).
2000 Cheng K. Smyth RL. Motley J. O’Hea U. Ashby D. Randomized controlled trials in cystic fibrosis (1966-1997) categorized by time, design, and intervention. Pediatr Pulmonol 2000; 29:1-7. [PubMed]
Ros Smyth, Deborah Ashby and colleagues developed a register of RCTs in CF and have studied when they were performed, their design, and what interventions were investigated. They identified 506 RCTs; 37.5% were identified solely as abstract reports in conference proceedings. There has been about a 30-fold increase in the number of RCTs in CF since 1966. A high proportion of the RCTs (72.7%) had a sample size of 30 or less, and only 8.7% were multicenter trials. Reporting of study design was poor: in 51.4% the report did not state whether there was any blinding in the trial design; 53.6% of studies were of crossover design. The most common interventions studied were antibiotic treatments and physiotherapy, but a number of commonly used therapies had been evaluated only in a small number of patients. Although the number of RCTs of interventions in CF patients has increased over the last 25 years, the sample sizes of these trials are generally too small to indicate whether the intervention was effective, and very few were multicenter. Future RCTs in CF are more likely to provide clinically useful answers if higher numbers of patients are recruited into large, well-designed multicenter trials. This should be a priority of the organization of future research in CF.
2007 Dodge JA, Lewis PA, Stanton M, Wilsher J. Cystic fibrosis mortality and survival in the UK: 1947-2003. Eur Respir J 2007; 29:522-526. [PubMed]

John Dodge
Data up to 1995 on the survival of 3-yr cohorts of patients with CF born in the UK in the period 1968-1992 had previously been published (Dodge et al. Arch Dis Child 1997; 77:493-496. 9496181). The present study, coordinated by John Dodge and the last from the original Survey of the UK CF Working party, reports survival data up to the end of 2003 together with a 2003 population estimate. All subjects with CF born in the UK in the period 1968-1992 were identified up to 1997 and information from the death certification authorities up to the end of 2003 was added.
The observed survival up to 2003 of CF patients born in 1978 was 55% for males and 49% for females. For 1988 and 1992 the data were 91 and 88%, and 97 and 96%, respectively. The estimated 2003 mid-year CF population was 8,284. The continuing improvement in survival of cystic fibrosis patients in successive cohorts means that the previous prediction of median survival of >50 yrs of age for individuals born in 2000 continues to look realistic, even in the absence of proven effective therapy aimed at correcting the basic cystic fibrosis defect.
2010 Hult G, Li Z, Scotet V, Dugueperoux I, Ferec C, Roussey M, Laxova A, Farrell PM. Participating CF centres of Brittany, France. Pulmonary outcome differences in U. S. and French cystic fibrosis cohorts diagnosed through newborn screening. J Cyst Fibros 2010; 9:44-50. [PubMed] A comparison of the longitudinal progression of lung disease in cystic fibrosis patients identified through newborn screening (NBS) in cohorts located in two different countries is a “first”.
The study included 56 patients in Brittany diagnosed through NBS between 1989 and 1994 and 69 similar patients in Wisconsin between 1985 and 1994. The onset and progression of lung disease was radiographically quantified using the Wisconsin Chest X-ray (WCXR) scoring system. A single pediatric pulmonologist blinded to all identifiers scored the films. RESULTS: Generalized estimating equation analyses adjusted for age, genotype, sex, pancreatic insufficiency, and meconium ileus showed worse WCXR scores in Brittany patients compared to Wisconsin patients (average score difference=4. 48; p<0. 001). Percent predicted FEV1 was also worse among Brittany patients (p<0. 001). The finding of milder radiographically-quantified lung disease using the WCXR scoring system, as well as better FEV1 values, may be explained by variations in nutrition, environmental exposures, or health care delivery.
This is the first long term comparison of children diagnosed by neonatal screening in two different countries. The clearly worse condition of the Brittany children compared to those born in Wisconsin is not explained. Although the suggestion was made that the French children had less rigorous infection avoidance and more hospitalizations, the bacteriological data was said to be not suitable for comparison which is unfortunate for it is likely to be relevant.
2011 George PM, Banya W, Pareek N, Bilton D, Cullinan P, Hodson ME, Simmonds NJ. Improved survival at low lung function in cystic fibrosis: cohort study from 1990 to 2007. BMJ 2011; 342:d1008. [PubMed] To evaluate the survival of patients with cystic fibrosis whose lung function has deteriorated to a forced expiratory volume in one second (FEV(1)) below 30% predicted in the recent treatment era and to explore factors associated with any change in survival. 276 patients (147 (53%) male) attending the Brompton whose FEV(1) was first observed to be less than 30% predicted between 1 January 1990 and 31 December 2003. The median survival improved from 1.2 years in the 1990-1 group to 5.3 years in the 2002-3 group, with a marked improvement in survival from 1994. The use of nebulised recombinant human DNase was significantly associated with a reduced risk of death (hazard ratio 0.59, 95% confidence interval 0.44 to 0.79). Significantly increased risks were associated with a body mass index under 19 (hazard ratio 1.52, 1.10 to 2.10), long term oxygen therapy (3.52, 2.49 to 4.99), and nebulised antibiotics (1.84, 1.05 to 3.22). The authors concluded that a marked improvement has occurred in the survival of patients with cystic fibrosis with an FEV(1) less than 30% predicted. Secondary analyses suggest that some of this improvement may be due to use of recombinant human DNase.
This is interesting and encouraging data from the UKs major adult CF centre showing a much improved survival for these severely affected patients, presumably related to improved treatment. For some years a survival;- in this study the authors suggest that the use of DNase may be a significant factor.
2011 Reid DW, Blizzard CL, Shugg DM, Flowers C, Cash C, Greville HM. Changes in cystic fibrosis mortality in Australia, 1979-2005. Med J Australia 2011; 195:392-395.[PubMed]
Between 1979 and 2005, the mean age at death increased from 12.2 years to 27.9 years for males and from 14.8 years to 25.3 years for females. Overall, female deaths in childhood (0-14 years) occurred at an age-standardised rate of 0.40 per 100,000 (95% CI, 0.34-0.45) during 1979-2005, which exceeded the corresponding rate for males of 0.24 (95% CI, 0.20-0.28) per 100,000. Among 0-14-year-old boys, event rates declined markedly after 1989, but they declined later and more gradually for girls, with the result that the age-standardised rate for girls was 2.38 times that of boys during 1989-2005 (95% CI, 1.69-3.36). The authors concluded that the pattern of CF mortality in Australia has changed substantially. Mortality rates continue to be higher for girls than for boys, but death in childhood has become uncommon. Survival has increased since 1979, but females continue to have reduced length of life.
2011 Barr HL, Britton J, Smyth AR, Fogarty AW. Association between socioeconomic status, sex, and age at death from cystic fibrosis in England and Wales (1959 to 2008): cross sectional study. BMJ 2011; 343:d4662.[PubMed] Free full version available
Series of annual cross sectional studies of all registered deaths with a diagnosis of cystic fibrosis in England and Wales, from 1959 to 2008. From 2001 onwards, the National Statistics Socioeconomic Classification was implemented and socioeconomic status was split into three groups: professional and managerial, intermediate, and routine and manual. The authors calculated median age at death for every study year and the effects of sex and socioeconomic status on the odds of death above the median age at death for every study decade using logistic regression. From 1959 to 2008, 6750 deaths were attributed to cystic fibrosis in England and Wales. Males were more likely to die above the annual median age at death than females (from 1959 to 1999, adjusted odds ratio for socioeconomic status 1.28, 95% confidence intervals 1.13 to 1.45; from 2000 to 2008, 1.57, 1.18 to 2.08). Individuals in the highest socioeconomic class were also more likely to die above the median age of death than those in the lowest socioeconomic class (from 1959 to 2000, adjusted odds ratio for sex 2.50, 2.16 to 2.90; from 2001 to 2008, 1.89, 1.20 to 2.97).
The authors comment that socioeconomic status and sex remain strong determinants of survival from cystic fibrosis in England and Wales, and the magnitude of these effects does not appear to have substantially reduced over time.
2011 Stern M, Niemann N, Wieddemann B, Wenzlaff P, on behalf of the German CFQA Group. Benchmarking improves quality in cystic fibrosis care: a pilot project involving 12 centres. Int J Qual health Care 2011; 23:349-56.[PubMed] (Full text is available to download via PubMed entry)

Martin Stern
A group of 12 CF centres in Germany, treating a total of 1200 patients of all ages, enrolled in a nationwide pilot benchmarking project from 2004 to 2007. Key nutritional and respiratory parameters were used as quality indicators. Numerical benchmarks were set and used for ranking. Applying the plan-do-check-act cycle, quality improvement interventions were introduced, such as harmonization of definitions and references, improvement of measurement standards, data quality, completion of missing data, enforcement of early aggressive antibiotic treatment and individual adaptation of dietary counselling. Ranking alone was not sufficient for identification of the best performing centres unless it was accompanied by longitudinal follow-up. Improvement was possible in the 3 years’ period as shown by benchmarking for single centres that introduced new interventions in nutritional and antibiotic treatment most consequently.
CF provides a model of the link between processes of health care delivery and health outcomes of patients. Quality improvement is a continuous goal in CF care with realistic potential as exemplified by our data. Accountability was introduced and transparency was improved by our pilot benchmarking project. Using the benchmarking procedure, our long-term project will reinforce standards, programmes, and individual attitudes and principles to ensure continuous quality improvement in CF health care.
Professor Martin Stern (figure 5) is Head of the Paediatric Department at the University Children’s Hospital, University of Tubingen, Germany. He is involved in many aspects of CF care and research both nationally and internationally.
2011 Bell SC, Bye PT, Cooper PJ, Martin AJ, McKay KO, Robinson PJ, Ryan GF, Simms GC. Cystic fibrosis in Australia, 2009: results from a data registry. Med J Aust 2011; 195:396-400.[PubMed]

Scott Bell
In 2009, data were submitted on 2986 people (48% female). Median age was 17.6 years and 49% of people were aged 18 years or over. Seventy-eight people were newly diagnosed. Fourteen people died and 14 people underwent lung transplantation in the year. Lung function and nutrition were relatively normal among children but deteriorated (more rapidly) among adolescents. With increasing age, progressive respiratory disease was apparent, and the frequency of CF-related complications and use of health care resources increased. In all age groups, there was a wide range in severity of lung disease and nutritional status. CF remains a progressive respiratory disease and is associated with multisystem complications. The acceleration in disease severity in adolescence and early adulthood suggests that better treatment at these stages is required to further improve survivalA total of 53 national cystic fibrosis (CF) patient registry studies published between July 2008 and November 2011 have been reviewed, focusing on the following topics: CF epidemiology, nutrition, microbiology, clinical complications, factors influencing diagnosis and lung disease, effects of socioeconomic status, therapeutic strategy evaluation, clinical trial methodology. The studies describe the clinical characteristics of CF patients, the incidence and prevalence of disease and role of gender gap, as well as the influence of socioeconomic status and environmental factors on clinical outcomes, covering a variety of countries and ethnic groups. Original observations describe patients as they get older, with special reference to the adult presentation of CF and long-term survival. Methodological aspects are discussed, covering the design of clinical trials, survival analysis, auxometry, measures of quality of life, follow up of lung disease, predictability of disease progression and life expectancy. Microbiology studies have investigated the role of selected pathogens, such as Burkholderia species and MRSA. Pulmonary exacerbations are discussed both as a factor influencing morbidity and an endpoint in clinical trials. Finally, some studies give insights on complications, such as CF-related diabetes and hemoptysis, and emerging problems, such as chronic nephropathy.
A comprehensive review supporting the value of patient registries which yield so much important information.
2012 Rowe SM, Borowitz DS, Burns JL, Clancy JP, Donaldson SH, Retsch-Bogart G, Sagel SD, Ramsey BW. Progress in cystic fibrosis and the CF Therapeutics Development Network. Thorax 2012; 67:882-890.[PubMed] Full text available
Cystic fibrosis (CF), the most common life-shortening genetic disorder in Caucasians, affects approximately 70 000 individuals worldwide. In 1998, the Cystic Fibrosis Foundation (CFF) launched the CF Therapeutics Development Network (CF-TDN) as a central element of its Therapeutics Development Programme. Designed to accelerate the clinical evaluation of new therapies needed to fulfil the CFF mission to control and cure CF, the CF-TDN has conducted 75 clinical trials since its inception, and has contributed to studies as varied as initial safety and proof of concept trials to pivotal programmes required for regulatory approval. This review highlights recent and significant research efforts of the CF-TDN, including a summary of contributions to studies involving CF transmembrane conductance regulator (CFTR) modulators, airway surface liquid hydrators and mucus modifiers, anti-infectives, anti-inflammatories, and nutritional therapies. Efforts to advance CF biomarkers, necessary to accelerate the therapeutic goals of the network, are also summarised.
This is an excellent update of the growing points in CF clinical research; full text is available online.
2012 Doull I, Evans H. South and Mid Wales Paediatric Cystic Fibrosis Network. Full, shared and hybrid paediatric care for cystic fibrosis in South and Mid Wales. Arch Dis Child 2012; 97:17-20. [PubMed]

Iolo Doull
Although care for children with cystic fibrosis (CF) is increasingly shared between CF centres and local CF clinics, the optimal model is unclear. The authors compared three models of care within a well established CF network in Wales: full centre care; local clinic based care with annual review by the CF centre; and hybrid care, where the child is usually reviewed at least three times a year by the specialist CF centre.
Of 199 children and young people with CF in South and Mid-Wales, 77 were receiving full care, 102 shared care and 20 hybrid care. There were no significant differences in baseline characteristics, nutritional outcomes or use of chronic therapies. There was however a statistically significant difference between full, shared and hybrid care in mean forced expiratory volume in 1 s (FEV(1)) per cent predicted (89.2% vs 74.5% vs 88.9%; p=0.001).
These differences in pulmonary function are likely to reflect the model of care received, and may affect long term outcomes.
This important study shows an advantage for children who received all their care at the Wales CF Centre in Cardiff however the results were not accepted by all Iolo Doull’s colleagues in Wales and drew a vigorous response from paediatricians working in two of the local CF clinics involved – in Newport (Bowler I, Pierrepoint M, Evans R. Arch Dis Child 2012; 97:88) and Lanarkshire (Dryden C et al. Arch Dis Child 2012; 97: 88-89). So the discussion continues in the UK as to whether CF centre care is superior to care shared between a CF Centre and a local hospital clinic.
2012 Martin B, Schechter MS, Jaffe A, Cooper P, Bell SC, Ranganathan S. Comparison of the US and Australian cystic fibrosis registries: the impact of newborn screening. Pediatrics 2012; 129:e348-55. [PubMed]
The authors compared the 2003 US and Australian registries. Data on 12994 US and 1220 Australian patients aged <=18 years were analyzed. A significant difference was noted in the proportion who had been diagnosed after newborn screening (Australian 65.8% vs United States 7.2%; P < .001). Australian children had significantly greater mean height percentile (41.0 vs 32.6; P < .001) and weight percentile (43.5 vs 36.1; P = .028) than US children. Mean forced expiratory volume in 1 second (FEV(1)) percent predicted adjusted for age, gender, and genotype was similar in the 2 countries (P = .80). Patients diagnosed after newborn screening had higher mean FEV(1) (5.3 [95% confidence interval (CI): 3.6-7.0]) percent predicted and BMI (0.26 [95% CI: 0.09-0.43]). Mean FEV(1) of Australian patients diagnosed after newborn screening was lower by 5.2 (95% CI: 2.8-7.6) percent predicted compared with US children.
CONCLUSIONS: Children diagnosed with CF after newborn screening benefited from better lung function and BMI than those diagnosed clinically. The benefit of newborn screening on lung function was significantly less in Australian children compared with US children. Statistical comparisons between CF registries are feasible and can contribute to benchmarking and improvements in care
2012 Scotet V, Dugueperoux I, Saliou P, Rault G, Roussey M, Audrezet MP, Ferec C. Evidence for decline in the incidence of cystic fibrosis: a 35-year observational study in Brittany, France. Orphanet J Rare Dis 2012; 7:14. [PubMed]
This study assessed time trends in the birth incidence of CF over a long period (35 years: 1975-2009) in an area where CF is frequent (Brittany, France) and where NBS has been implemented for more than 20 years. The average number of patients born each year declined from 18.6 in the late 1970’s (period 1975-79) to 11.6 nowadays (period 2005-09). The corresponding incidence rates dropped significantly from 1/1983 to 1/3268, which represented a decline close to 40% between these two periods A clear breakpoint in incidence rate was observed at the end of the 1980’s (p < 0.0001). However, the incidence rate has remained quite stable since that time. The authors observed a 40% drop in incidence which seems consecutive to the availability of prenatal diagnosis.
In other areas where neonatal screening (UK, Australia, Italy) and indeed antenatal screening (Edinburgh) have been introduced there has been a significant reduction in the incidence of infants born with CF. Theoretically the means are now available to prevent all CF births (carrier detection, antenatal diagnosis, preimplantation genetic diagnosis) however neither the finances nor the will to do this appear to be in place at present.
2015 Goss CH; MacNeill SJ; Quinton HB; Marshall BC; Elbert A; Knapp EA; Petren K; Gunn E; Osmond J; Bilton D. Children and young adults with CF in the USA have better lung function compared with the UK. Thorax 2015; 70(3):229-36. [PubMed]
A cross-sectional study using 2010 data from patients in the US Cystic Fibrosis Foundation and the UK Cystic Fibrosis patient registries. The a priori outcome measures of interest were lung function and nutritional status. Descriptive statistics and two sample comparisons were performed. Stratification and multivariable linear regression were used to adjust for confounding.
The study cohort included 13,777 children and 11,058 adults from the USA and 3968 children and 3965 adults from the UK. In children, mean body mass index centiles were similar. Lung function (FEV1 and FVC% predicted) was significantly higher in US patients ages 6-25 years of age. In a regression model adjusted for only age, FEV1% predicted was on average 3.31% of predicted (95% CI 2.65 to 3.96) higher in the USA compared with the UK. When adjusted for age, age at diagnosis, gender, pancreatic insufficiency and genotype, FEV1% predicted was on average 3.03% of predicted (95% CI 2.37 to 3.69)
higher in the USA compared with the UK. These differences persisted despite adjustment for possible confounders. Hypertonic saline and dornase alfa were much more commonly prescribed in US children.
The authors concluded children and young adults with CF have better lung function in the USA compared with the UK despite similar nutritional status.
– This is an important study involving international collaboration made possible using the national CF databases. The observation made by the authors, that certain preparations such a dornase alpha and hypertonic saline were much more frequently prescribed in the USA, is likely to be a major factor in the difference in respiratory function (see abstract of the editorial by Taylor-Robinson et al. below).
2015 Taylor-Robinson D C, Schechter M, Smyth RL. Comparing cystic fibrosis outcomes across the pond. Thorax 2015; 70:203-204 Editorial. [PubMed]
This is a very interesting commentary on the study of Goss et al. (Thorax 2015; 70(3):229-36. [PubMed]). The authors raise some questions concerning the conclusion that lung function of USA children is significantly better than that of UK children – a difference most marked around 6 years.
They ask if the samples are fully representative of the entire CF populations of the respective countries? The UK captures almost the entire CF population whereas the US data is for patients attending US accredited centres (an estimated 75%) containing fewer socially disadvantaged patients. However, even removing such patients from the UK data did not account for most of the difference. Also genetic and ethnic differences were not responsible. The data is cross sectional and may not represent true longitudinal differences and the older patients may represent only those healthier individuals who have survived. But even so, the differences in early lung function seem to be genuine albeit less than stated.
Possible reasons for the great discrepancies are the use of rhDNase and possibly nebulised hypertonic saline between young patients (<18yrs) in the UK and USA are possible reasons. For example at the time of the study use of treatments in USA vs. UK were – hypertonic saline 40.9% vs. 8.4%, any nebulised antibiotic 44 .7% vs. 42.9%, rhDNase 77.2% vs. 35.4% and macrolides 33.6% vs. 24.1% Also all the US patients included attended recognised specialist CF Centres, which is not always the case in the UK, even though health and survival have been shown to be better with the more expert experienced care at specialist centres. Such centre care includes more frequent clinic visits, more frequent respiratory cultures and antibiotic treatments particularly at an earlier stage in milder affected patients – all factors known for generations to improve health and survival of people with CF. In this reviewer’s (JML) opinion, the expert care delivered at specialist centres and the great difference in the use of rhDNase are likely to be the main reasons for the discrepancy in respiratory function of the children. Also the overall coverage in the UK will include more patients not attending specialist centres. It is sad that, even today, some UK paediatricians are not convinced of the benefit of referring their patients to a specialist CF centre and complain of the lack of “controlled studies”. As Sir William Osler observed “ Medicine is to be learned by experience and is not an inheritance; it cannot be revealed. Learn to see, learn to hear, learn to smell, and know that by practice alone can you become expert” With regard to the use of rhDNase, almost every study since the treatment became available in the early Nineties has shown significant improvement in some aspect of the condition of the treated patients even amounting to improving survival. Please see Topics -> Mucolytics -> Pulmozyme (rhDNase) where I have reviewed many of the earlier publications, particularly relevant being those showing improvement even in young and mildly affected patients. These findings encouraged the earlier use of rhDNase in infants and preschool children as soon as they were able to inhale the drug at both the Leeds and Copenhagen CF Centres.
This study highlights the great value of such comparative studies which are possible using reliable national databases such as are now established at the CF Foundation, the UK CF Trust and elsewhere. They certainly justify the many problems we experienced in collecting and processing data the early years when the databases were started by these two national organisations.
2015 Merlo CA; Clark SC; Arnaoutakis GJ; Yonan N; Thomas D; Simon A; Thompson R; Thomas H; Orens J; Shah AS. National Healthcare Delivery Systems Influence Lung Transplant Outcomes for Cystic Fibrosis. Am J Transplant 2015; 15(7):1948-57. [PubMed]
Successful lung transplantation (LTx) depends on multiple components of healthcare delivery and performance. The authors conducted an international registry analysis to compare post-LTx outcomes for cystic fibrosis (CF) patients using the UNOS registry in the United States and the National Health Service (NHS) Transplant Registry in the United Kingdom.
– Both the United States and United Kingdom have similar early survival outcomes, suggesting important dissemination of best practices internationally. However, patients using US Medicare/Medicaid insurance had significantly worse survival after lung transplant.
Burgel PR, Bellis G, Olesen HV, Viviani L, Zolin A, Blasi F, Elborn JS; ERS/ECFS Task Force on The Provision of Care for Adults with Cystic Fibrosis in Europe.Future trends in cystic fibrosis demography in 34 European countries.Eur Respir J. 2015 Mar 18. pii: ERJ-01963-2014. [Epub ahead of print]
The aim of this study was to estimate the number of children and adults with CF in 34 European countries by 2025. Western European countries’ forecasts indicate that an increase in the overall number of CF patients by 2025, by approximately 50%, corresponds to an increase by 20% and by 75% in children and adults, respectively. In Eastern European countries the projections suggest a predominant increase in the CF child population, although the CF adult population would also increase.
It was concluded that a large increase in the adult CF population is expected in the next decade. A significant increase in adult CF services throughout Europe is urgently required.
2015 Peckham D, Whitaker P, White H. Research in progress-electronic patient records: a new era. Thorax 2015 May; 70(5):473-5. doi: 10.1136/thoraxjnl-2014-206573. Epub 2014 Dec 10. [PubMed]
Clinical information systems and electronic records are starting to appear in secondary care and herald new potentials for improving health provision and capturing high quality data. In 2006, the authors set up a program to develop electronic patient records (EPR) for chronic disease using Cystic Fibrosis (CF) as their initial model. Seven years on they are now exploring the real time clinical data to identify risks, trends and outcomes in chronic disease management. The authors are also working to establish new models of integration and to connect information between the client and all areas of health care.
– The author’s Regional CF Centre for adults at St James’s University Hospital in Leeds has pioneered the use of electronic records and the unit now is mostly without paper records.
2016 Chevreul K, Michel M, Brigham KB, López-Bastida J, Linertová R, Oliva-Moreno J, Serrano-Aguilar P, Posada-de-la-Paz M, Taruscio D, Schieppati A, Iskrov G, Péntek M, von der Schulenburg JM, Kanavos P, Persson U, Fattore G; BURQOL-RD Research Network. Social/economic costs and health-related quality of life in patients with cystic fibrosis in Europe. Eur J Health Econ. 2016 Apr 8. [Epub ahead of print.[PubMed] A cross-sectional study was carried out on adults and children with CF in eight European countries. A total of 905 patients with CF was included (399 adults and 506 children). The total average annual cost per patient varied from €21,144 in Bulgaria to €53,256 in Germany. Adults had higher direct healthcare costs than children, but children had much higher informal care costs (P<0.0001). Total costs increased with patients’ level of dependence. There was no difference in caregiver HRQOL regardless of whether they cared for an adult or a child. However, caregivers who looked after a child had a significantly higher burden (P=0.0013)
– The study highlights the burden of CF in terms of costs and decreased health related quality of life for both the people with CF and their caregivers throughout Europe.
Cohen-Cymberknoh M, Shoseyov D, Breuer O, Shamali M, Wilschanski M, Kerem E. Treatment of cystic fibrosis in low-income countries. Lancet Respir Med. 2016 Feb;4(2):91-2. doi: 10.1016/S2213-2600(15)00507-X. [PubMed] The duration and quality of life of patients with cystic fibrosis in developed countries has been substantially improved in the past two decades. By contrast, individuals with cystic fibrosis who live in low-income settings without the resources necessary to optimise cystic fibrosis care tend to have a worse clinical outcome than those from more affluent areas, including later age at diagnosis, worse nutritional status, and worse lung function. Present cystic fibrosis care guidelines, generally designed to be used in developed countries, include treatments not available in resource-poor settings.
Elborn JS; Bell SC; Madge SL; Burgel PR; Castellani C; Conway S; De Rijcke K; Dembski B; Drevinek P; Heijerman HG; Innes JA; Lindblad A; Marshall B; Olesen HV; Reimann AL; Sole A; Viviani L; Wagner TO; Welte T; Blasi F. Report of the European Respiratory Society/European Cystic Fibrosis Society task force on the care of adults with cystic fibrosis. Euro Respir J 2016; 47(2):420-8. Access to full text [PubMed] The improved survival in people with cystic fibrosis has led to an increasing number of patients reaching adulthood. This trend is likely to be maintained over the next decades, suggesting a need to increase the number of centres with expertise in the management of adult patients with cystic fibrosis. These centres should be capable of delivering multidisciplinary care addressing the complexity of the disease, in addition to addressing the psychological burden on patients and their families. Further issues that require attention are organ transplantation and end of life management. Lung disease in adults with cystic fibrosis drives most of the clinical care requirements, and major life-threatening complications, such as respiratory infection, respiratory failure, pneumothorax and haemoptysis, and the management of lung transplantation require expertise from trained respiratory physicians. The taskforce therefore strongly recommends that medical leadership in multidisciplinary adult teams should be attributed to a respiratory physician adequately trained in cystic fibrosis management. The task force suggests the implementation of a core curriculum for trainees in adult respiratory medicine and the selection and accreditation of training centres that deliver postgraduate training to the standards of the HERMES programme.
– An up-to-date review of the requirements for adult care by a multidisciplinary team of acknowledged experts.
2016 Madge S; Bell SC; Burgel PR; De Rijcke K; Blasi F; Elborn JS; ERS/ECFS task force: Limitations to providing adult cystic fibrosis care in Europe: Results of a care centre survey. The provision of care for adults with cystic fibrosis in Europe. J Cyst Fibrosis 2016 Jul 25.[PubMed] There are a growing number of adults in Europe with a projected increase of 75% over the next decade. There is concern that provision of care will not be sufficient to meet needs. We aimed to establish the level of CF service throughout Europe. An online survey designed by clinicians and patient representatives to explore level of service.Training opportunities for clinicians and resources (physical and manpower) to provide care to adults with CF are limited in Europe. Although specific adult CF care has been identified, teams continue to be supported by paediatric colleagues and many adults are still being admitted to paediatric wards. In some centres, service delivery, particularly infection control and access to some CF medication is insufficient and in many places poor personnel resources limits access to comprehensive multidisciplinary teams. This survey shows an urgent need for the development of resources for adult CF care, in both physical space and appropriately trained clinicians.
2016 Peckham D. Electronic patient records, past, present and future. Paed Resp Rev 2016; 20 Suppl:8-11. [PubMed] The health informatics revolution was spear-headed in the 1980s by pioneers in primary care who worked in an opportune environment and were able to successfully implement electronic patient records (EPR) as far back as the 1990s. Although the ambitious and costly National Programme for IT failed to deliver an integrated EPR, the project achieved the creation of the Spine, the N3 Network, choose and book, picture archiving, communication systems and standards, which have allowed integration. Real change is taking place within the NHS with the launch of exciting new projects focusing on true integration and secure data flows across primary, community and secondary care. These changes have been brought about by the realisation that linking “best in class” is more likely to secure a successful cost-effective national integrated electronic patient records.
2016 Weber HC, Robinson PF, Saxby N, Beggs SA, Els I. Do children with cystic fibrosis receiving outreach care have poorer clinical outcomes than those treated at a specialist cystic fibrosis centre? Aust J Rural Health. 2016 Nov 17. doi: 10.1111/ajr.12334. [Epub ahead of print][PubMed]

Heinrich Weber
Although cystic fibrosis (CF) centre care is generally considered ideal, children living in regional Australia receive outreach care supported by the academic CF centres.
This is a retrospective database review of children with CF treated at the Royal Children’s Hospital in Melbourne and its outreach clinics in Albury (Victoria), and Tasmania. The aim was to compare the outcomes of children with CF managed at an academic centre with that of outreach care, using lung function, nutritional status and Pseudomonas aeruginosa colonisation. Three models of care, namely CF centre care, Shared care and predominantly Local care, were compared, based on the level of involvement of CF centre multidisciplinary team. In our analyses, we controlled for potential confounders, such as socio-economic status and the degree of remoteness, to determine its effect on the outcome measures.
There was no difference in lung function, i.e. forced expiratory volume in 1 s (FEV1 ), the prevalence of Pseudomonas aeruginosa colonisation or nutritional status (body mass index (BMI)) between those receiving CF centre care and various modes of outreach care. Neither socio-economic status, measured by the Socio-Economic Index for Area (SEIFA) for disadvantage, nor distance from an urban centre (Australian Standard for Geographical Classification (ASGC)) were associated with lung function and nutritional outcome measures. There was however an association between increased Pseudomonas aeruginosa colonisation and poorer socio-economic status.
Outcomes in children with CF in regional and remote areas receiving outreach care at the local hospital by an academic CF centre were no different from children receiving CF centre care.
– The discussion as to the merits of CF centre care versus care at outreach clinics at smaller local hospitals continues. A relatively recent study from Wales in the UK showed advantages for those children who had full centre care (Doull & Evans, 2012 [PubMed]). However, as so often occurs, the findings were disputed by staff at two of the outreach Welsh clinics concerned. In the UK experience of this reviewer, the parents of more severely affected children with complex problems from more distant areas may prefer to seek all their care at the distant major CF centre. This adversely affects the figures at the CF centre and improves those of the local clinic. It would be important to know if this occurred in the present Australian study. Also the experience of staff at the CF centre dealing with hundreds of patients is essential for a minority of patients. Incidentally it is important to note that all significant advances in the management have occurred at CF centres where the staff see many patients, recognise emerging problems and set about seeking solutions.
The authors do not discuss the interesting striking difference in the use of DNase (28.7% at the CF centre, 42.9% on shared care and 58.6% of those receiving local care). In previous studies that failed to show differences between screened and late diagnosed children it was pointed out that more treatment was required to keep the non-screened children is good condition (Simms EJ et al, Pediaitrics 2007; 119:19-28. 17200267) The more frequent use of DNase in the children in the remote areas may be relevant in the present study.
Heinrich Weber (figure) is Associate Professor of Paediatrics in the University of Tasmania.
2017 Agrawal A, Agarwal A, Mehta D, Sikachi RR, Du D, Wang J. Nationwide trends of hospitalizations for cystic fibrosis in the United States from 2003 to 2013. Intractable Rare Dis Res. 2017 Aug;6(3):191-198. doi: 10.5582/irdr.2017.01043.(Full article available on journal website) [Pubmed]

Abhinav Agrawal
The authors analysed the National Inpatient Sample Database (NIS) in the United States for all patients in which CF was the primary discharge diagnosis (ICD-9: 277.0-277.09) from 2003 to 2013 to evaluate the rate of hospitalizations and determine the cost and mortality associated with CF along with other epidemiological findings. The statistical significance of the difference in the number of hospital discharges, lengths of stays and associated hospital costs over the study period was calculated.
In 2003, there were 8,328 hospital discharges with the principal discharge diagnosis of CF in the United States, which increased to 12,590 discharges in 2013 (p < 0.001). The mean hospital charges increased by 57.64% from US$ 60,051 in 2003 to US$ 94,664 in 2013. The aggregate cost of hospital visits increased by 138.31% from US$ 500,105,727 to US$ 1,191,819,760. In the same time, the mortality decreased by 49.3 %. The number of inpatient discharges related to CF has increased from 2003 to 2013. This is due to increased life expectancy of CF patients, resulting in increased disease prevalence.
There has been a significant increase in the mean and aggregate cost associated with CF admissions. Over the last decade, many advances have been made in the diagnosis and treatment of CF, consequentially leading to a significant transformation in the epidemiology and demographics of this chronic disease. Rising hospital costs associated with the care of CF patients necessitates future studies analysing the diagnostic modalities, algorithms and treatment practices of physician’s treating CF patients.
Dr Abhinav Agrawal (figure) is Fellow, in the Division of Pulmonary, Critical Care and Sleep Medicine at the Hofstra Northwell School of Medicine, New York.
McColley SA, Schechter MS, Morgan WJ, Pasta DJ, Craib ML, Konstan MW. Risk factors for mortality before age 18 years in cystic fibrosis. Pediatr Pulmonol. 2017 Jul;52(7):909-915. doi: 10.1002/ppul.23715. Epub 2017 Apr 24.[Pubmed]
Data from the Epidemiologic Study of Cystic Fibrosis (ESCF) collected 1994-2005 were linked with the Cystic Fibrosis Foundation Patient Registry (CFFPR) demographic and mortality data from 2013. Among 5365 patients enrolled in ESCF who met inclusion criteria, 3880 (72%) were linked to the CFFPR. Among these, 191 (5.7%) died before age 18 years; median age at death was 13.4 ± 3.1 years. Multivariable regression showed clubbing, crackles, female sex, unknown CFTR genotype, minority race or ethnicity, Medicaid insurance (a proxy of low socioeconomic status), Pseudomonas aeruginosa on 2 or more cultures, and weight-for-age <50th percentile were significant risk factors for death regardless of inclusion of FEV1 at age 6-8 years in the model.
The authors identified multiple risk factors for childhood death of patients with CF, all of which remained important after incorporating FEV1 at age 6-8 years. Among the factors identified were the presence of clubbing or crackles at age 3-5 years, signs that are not routinely collected in registries.
– A study showing the increasing value of patient registries in confirming clinical impressions. Most clinicians would already recognise crackles, finger clubbing, low weight for age and poor economic status as very bad prognostic signs in children aged 3-5 yrs. Although most of the factors listed as risk factors for death before 18 years are not unexpected, confirmation using the patient registries is useful and presents opportunities for intervention. The need for very early intervention following diagnosis by neonatal screening to identify and prevent or control pulmonary infection is a major problem which many groups are addressing as a matter of urgency.
Roberts JM; Wilcox PG; Quon BS. Evaluating Adult Cystic Fibrosis Care in BC: Disparities in Access to a Multidisciplinary Treatment Centre. Can Respir J 2016:8901756, 2016.[Pubmed]
Cystic fibrosis care that is delivered through dedicated multidisciplinary CF clinics is believed to be partly responsible for improvements in the length and quality of life of persons with CF. The authors hypothesised patients living farthest from a CF clinic would be seen less frequently than recommended, which would result in reduced access to guideline-recommended care and poorer health outcomes. They performed a retrospective chart review of 168 patients who accessed CF care primarily through the St. Paul’s Hospital Adult CF Clinic. Subjects were stratified into four geographical groups according to the estimated one-way travel time by automobile from their home address to the clinic (<45mins, 45-150mins, 150-360mins, and >360mins).
Results. There were no significant differences in pulmonary function, nutritional status, CF-related complications, or access to guideline-recommended CF pulmonary therapies between the four groups. Compared to the reference (<45mins) group, subjects in the two farthest groups (>150mins) were less likely to be seen in the clinic quarterly as recommended by current CF care guidelines (p = 0.002). Those in the farthest group (>360mins) were at risk for more rapid decline in lung function compared to the reference group (FEV1% predicted annual change: -3.1%/year [95% CI -5.1 to -1.1] versus -0.9%/year [95% CI -1.6 to 0.1], resp., p = 0.04).
The authors concluded access to CF care is a challenge for individuals who live outside Metro Vancouver and has health policy implications. Further initiatives should be undertaken to ensure equitable care for people living with CF. They note that while at present some challenges to accessing routine multidisciplinary CF care exist, they have shown that individuals with CF in British Columbia continue to experience similar health outcomes regardless of their location of residence. The approach of a single clinic with an array of multidisciplinary staff, coupled with frequent outreach initiatives, including satellite clinics, telehealth contact, family physician, and local specialist involvement, may be applicable to other “orphan” diseases for which comprehensive multidisciplinary outpatient care might not otherwise be available.
Dr. James Mark Roberts is Clinical Associate, Professor General Internal Medicine, Programme Director Postgraduate Medical Education, University of British Columbia, Vancouver.
2017 Stephenson AL, Sykes J, Stanojevic S, Quon BS, Marshall BC, Petren K, Ostrenga J, Fink AK, Elbert A, Goss CH. Survival Comparison of Patients With Cystic Fibrosis in Canada and the United States: A Population-Based Cohort Study. Ann Intern Med. 2017 Mar 14. doi: 10.7326/M16-0858. [Epub ahead of print] [Pubmed]

Anne Stephenson
In 2011, the median age of survival of patients with cystic fibrosis reported in the United States was 36.8 years, compared with 48.5 years in Canada. Direct comparison of survival estimates between national registries is challenging because of inherent differences in methodologies used, data processing techniques, and ascertainment bias. The purpose of this study was to use a standardised approach to calculate cystic fibrosis survival estimates and to explore differences between Canada and the United States.
Population-based study involving 42 Canadian cystic fibrosis clinics and 110 U.S. cystic fibrosis care centers. Patients followed in the Canadian Cystic Fibrosis Registry (CCFR) and U.S. Cystic Fibrosis Foundation Patient Registry (CFFPR) between 1990 and 2013. Cox proportional hazards models were used to compare survival between patients followed in the CCFR (n = 5941) and those in the CFFPR (n = 45 448). Multivariable models were used to adjust for factors known to be associated with survival.
The Median age of survival in patients with cystic fibrosis increased in both countries between 1990 and 2013; however, in 1995 and 2005, survival in Canada increased at a faster rate than in the United States (P < 0.001). On the basis of contemporary data from 2009 to 2013, the median age of survival in Canada was 10 years greater than in the United States (50.9 vs. 40.6 years, respectively). The adjusted risk for death was 34% lower in Canada than the United States (hazard ratio, 0.66 [95% CI, 0.54 to 0.81]). A greater proportion of patients in Canada received transplants (10.3% vs. 6.5%, respectively [standardised difference, 13.7]). Differences in survival between U.S. and Canadian patients varied according to U.S. patients’ insurance status.
Ascertainment bias due to missing data or nonrandom loss to follow-up might affect the results.
Dr Anne Stephenson (figure) is Assistant Professor at the Institute of Health Policy, Management and Evaluation, Toronto.
– The authors concluded the differences in cystic fibrosis survival between Canada and the United States persisted after adjustment for risk factors associated with survival, except for private-insurance status among U.S. patients. Differential access to transplantation, increased post-transplant survival, and differences in health care systems may, in part, explain the Canadian survival advantage.
AN INTERESTING COMMENTARY ON THE ST MICHAEL’S HOSPITAL (TORONTO) WEBSITE
People with cystic fibrosis are living longer than ever before, but their lifespan is almost 10 years longer in Canada than in the United States, according to research published March 14 in the Annals of Internal Medicine. The median age of survival for individuals with cystic fibrosis in Canada is 50.9 years compared to 40.6 years in the United States, said Dr. Anne Stephenson, a respirologist and cystic fibrosis researcher at St. Michael’s Hospital in Toronto, which has the largest adult CF clinic in Canada. In addition, after taking into account factors such as age and the severity of the disease, the risk of death among people with cystic fibrosis was 34 per cent lower in Canada than in the United States, according to the research by lead author Dr. Stephenson and colleagues. The study was funded by the U.S. Cystic Fibrosis Foundation using data from 45,456 patients in the U.S. Cystic Fibrosis Foundation Registry and 5,941 patients in the Canadian Cystic Fibrosis Registry from 1990 to 2013. The 10-year difference in lifespan was based on data from the last five years, 2009 to 2013. Although the study was not designed to explain why the lifespan differs in the two countries, Dr. Stephenson said there were several possible reasons: transplants, diet and medical insurance.
“Survival has increased in both countries, but Canada began to see greater improvements than the United States starting in 1995, with an even more dramatic increase in the survival rate in Canada noted in 2005,” said Dr. Stephenson. Canadians with cystic fibrosis were exposed to a high fat diet in the 1970s, which was not implemented in the United States until the 1980s. In people with cystic fibrosis, higher caloric intake results in better nutritional status which and in previous studies has been linked to improved survival. Individuals born in the 1970s and exposed to good nutrition from birth could explain why Canadian survival rates saw improvement in 1995. This would suggest that countries where aggressive nutritional support was instituted in later decades should see the survival benefit in the near future.
Lung transplantation is one of the few treatments for cystic fibrosis that can positively impact survival almost immediately and a higher proportion of CF patients received a transplant in Canada than in the United States during the study period. The survival difference increased dramatically in 2005 which coincided with the year that the United States began using a lung allocation score to prioritise people on the lung transplant waiting list. This score is not used in Canada raising the possibility that this difference may be contributing to the survival gap seen.
The study found there was no difference in survival rates between U.S. patients with private health insurance compared to Canadians, who have universal, publicly funded health-care coverage. However, Canadians had a 44 per cent lower risk for death than U.S. patients receiving continuous Medicaid or Medicare, a 36 per cent lower risk than those receiving intermittent Medicaid or Medicare, and a 77 per cent lower risk than those with unknown or no health insurance.
– This is an interesting study and it is likely both the earlier nutritional treatment of the Canadians started in Toronto by Douglas Crozier in the Seventies and the present insurance differences are important factors.
Sykes J, Stanojevic S, Goss CH, Quon BS, Marshall BC, Petren K, Ostrenga J, Fink A, Elbert A, Stephenson AL. A standardised approach to estimating survival statistics for population-based cystic fibrosis registry cohorts. J Clin Epidemiol. 2016 Feb;70:206-13. doi: 10.1016/j.jclinepi.2015.08.026. Epub 2015 Oct 3. 26434789 Free PMC Article[Pubmed] The authors’ objective was to quantify the effect of different statistical techniques, inclusion/exclusion criteria, and missing data on the predicted median survival age. Using the Canadian cystic fibrosis registry (CCFR), the median age of survival was calculated using both the Cox proportional hazards (PH) and the life-table methods. Through simulations, they examined how the median age of survival would change when: (1) patients were excluded, (2) death dates were inaccurate, (3) patients were lost to follow-up, (4) entire years with no clinic visits were excluded even if the patient had a visit in subsequent years, and (5) censoring patients at their date of transplant. Simulations were run assuming 5-35% of data were affected by each scenario.
Over the period 2009-2013, there were 4,666 individuals in the CCFR with 240 deaths. The observed median age of survival calculated by the Cox PH method was 50.9 [95% confidence interval (CI): 47.4, 54.3] and 50.5 from the life-table method (95% CI: 47.5, 53.5). Censoring patients at their transplant date overestimated the median age of survival by 7.2 years (58.1; 95% CI: 53.3, 64.7). Simulations determined that by missing just 15% of deaths, the median age of survival can be overestimated by 3.5 years (54.4; 95% CI: 54.2, 56.1), and having 25% of patients lost to follow-up can underestimate the median age of survival by 3.3 years (47.6; 95% CI: 46.8, 47.7).
– The authors present several important recommendations to assist national cystic fibrosis registries in calculating and reporting the median age of survival in a standardised fashion. It is imperative to state the statistical method used as well as the proportion lost to follow-up and the treatment of missing data and transplanted patients. Registries must be diligent in their data collection as incomplete data can lead to overestimation and underestimation of survival
Dogru D, Çakır E, Şişmanlar T, Çobanoğlu N, Pekcan S, Cinel G, et al. Cystic fibrosis in Turkey: First data from the national registry.Author information. Pediatr Pulmonol. 2019 Nov 11. doi: 10.1002/ppul.24561. [Epub ahead of print]. [Pubmed]
Cystic fibrosis (CF) care has been implemented in Turkey for a long time; however, there had been no patient registry. For this purpose, the Turkish National CF Registry was established. The authors present the first results of registry using data collected in 2017. The data were collected using a data-entry software system, which was accessed from the internet. Demographic and annually recorded data consisted of 15 and 79 variables, respectively.
There were 1170 patients registered from 23 centers; the estimated coverage rate was 30%. The median age at diagnosis was 1.7 years (median current age: 7.3 years); 51 (4.6%) patients were aged over 18 years. Among 293 patients who were under 3 years of age, 240 patients (81.9%) were diagnosed through newborn screening. Meconium ileus was detected in 65 (5.5%) patients. Genotyping was performed in 978 (87.4%) patients and 246 (25.2%) patients’ mutations were unidentified. The most common mutation was deltaF508 with an allelic frequency of 28%, followed by N1303K (4.9%). The median FEV1% predicted was 86. Chronic colonization with Pseudomonas aeruginosa was seen in 245 patients. The most common complication was pseudo-Bartter syndrome in 120 patients. The median age of death was 13.5 years in a total of 15 patients.
The authors comment on the low coverage rate, lack of genotyping, unidentified mutations, and missing data of lung functions are some of their greatest challenges. Including data of all centers and reducing missing data will provide more accurate data and help to improve the CF care in Turkey in the future.
– It must be said that the results are strikingly different from some of the other European countries for example UK CF Registry 2018 the results of which are bracketed after the Turkish figures. Total number 1170 (10508), median age at diagnosis 1.7 years (2 months), current median age 7.3years (20 years), percentage over 18 years 4.6% (16 years and over 60.4%), median age at death 13.5 years (32 years). There was a surprisingly high incidence of pseudo-Bartter’s syndrome in 120 patients presumably related to the warm climate.
From the Division of Pediatric Pulmonology, Faculty of Medicine, Hacettepe University, Ankara, Turkey and the other CF units in Turkey.
– The development of a nationwide CF patient registry is a long job, as we found in the UK. It is good that a start has been made in Turkey for an accurate patient registry is absolutely essential.
Ruth H Keogh, Rhonda Szczesniak, David Taylor-Robinson, Diana Bilton Up-to-date and projected estimates of survival for people with cystic fibrosis using baseline characteristics: A longitudinal study using UK patient registry data.J Cyst Fibros. 2018 Mar;17(2):218-227.doi: 10.1016/j.jcf.2017.11.019. Epub 2018 Jan 6. Free PMC article [Pubmed]

Ruth Keogh
Flexible parametric survival modelling of UK CF Registry data from 2011 to 2015, capturing 602 deaths in 10,428 individuals. Survival curves were estimated from birth; conditional on reaching older ages; and projected under different assumptions concerning future mortality trends, using baseline characteristics of sex, CFTR genotype (zero, one, two copies of F508del) and age at diagnosis.
Findings: Male sex was associated with better survival, as was older age at diagnosis, but only in F508del non-homozygotes. Survival did not differ by genotype among individuals diagnosed at birth. Median survival ages at birth in F508del homozygotes were 46years (males) and 41years (females), and similar in non-homozygotes diagnosed at birth. F508del heterozygotes diagnosed aged 5 had median survival ages of 57 (males) and 51 (females). Conditional on survival to 30, median survival age rises to 52 (males) and 49 (females) in homozygotes. Mortality rates decreased annually by 2% during 2006-2015. Future improvements at this rate suggest median survival ages for F508del homozygous babies of 65 (males) and 56 (females).
Interpretation: Over half of babies born today, and of individuals aged 30 and above today, can expect to survive into at least their fifth decade.
Research in context: Previous studies on survival are reviewed and figures are presented.
Dr Ruth Keogh is Professor of Biostatistics and Epidemiology at the London School of Hygiene and Tropical Medicine.
– It is good to see the data from the CF Trust analysed so clearly.
Kimberly A McBennett, Pamela B Davis, Michael W Konstan.Increasing life expectancy in cystic fibrosis: Advances and challenges. Pediatr Pulmonol 2021 Oct 21.doi: 10.1002/ppul.25733. Online ahead of print. [Pubmed]
Kimberly A McBennett
Since the first description of cystic fibrosis in 1938, there have been significant advances in both quality of life and longevity for people living with this disease. In this article we describe the milestones of the last 80 years and what we perceive to be the remaining barriers to normalcy for this population.
Dr Kimberly A McBennett is at Case Western Reserve University School of Medicine, Cleveland, Ohio, USA.Rainbow Babies and Children’s Hospital, Cleveland, Ohio, USA.
Emrah Gecili, Siva Sivaganesan, Ozgur Asar, John P Clancy, Assem Ziady, Rhonda D Szczesniak. Bayesian regularization for a nonstationary Gaussian linear mixed effects model Stat Med 2022 Feb 20;41(4):681-697.doi: 10.1002/sim.9279. Epub 2021 Dec 12. 3 [Pubmed]

Emrah Gecili
In omics experiments, estimation and variable selection can involve thousands of proteins/genes observed from a relatively small number of subjects. Many regression regularization procedures have been developed for estimation and variable selection in such high-dimensional problems. However, approaches have predominantly focused on linear regression models that ignore correlation arising from long sequences of repeated measurements on the outcome. Our work is motivated by the need to identify proteomic biomarkers that improve the prediction of rapid lung-function decline for individuals with cystic fibrosis (CF) lung disease. We extend four Bayesian penalized regression approaches for a Gaussian linear mixed effects model with nonstationary covariance structure to account for the complicated structure of longitudinal lung function data while simultaneously estimating unknown parameters and selecting important protein isoforms to improve predictive performance. Different types of shrinkage priors are evaluated to induce variable selection in a fully Bayesian framework. The approaches are studied with simulations. We apply the proposed method to real proteomics and lung-function outcome data from our motivating CF study, identifying a set of relevant clinical/demographic predictors and a proteomic biomarker for rapid decline of lung function. We also illustrate the methods on CD4 yeast cell-cycle genomic data, confirming that the proposed method identifies transcription factors that have been highlighted in the literature for their importance as cell cycle transcription factors.
Dr Emrah Gecili is post-doctoral research fellow at Cincinnati Children’s Hospital Medical Center and Cystic Fibrosis Foundation Fellow.
Kimberly A McBennett, Pamela B Davis, Michael W Konstan. Increasing life expectancy in cystic fibrosis: Advances and challenges. Pediatr Pulmonol 2022 Feb;57 Suppl 1(Suppl 1):S5-S12.doi: 10.1002/ppul.25733.Epub 2021 Nov 11. Free PMC article [Pubmed]
Based on data from 2019, the Cystic Fibrosis Foundation Registry Report from the United States calculated the predicted median survival age of a child born that year with cystic fibrosis to be 48.4 years1, a remarkable achievement. Summarized data from the registries of the United Kingdom, Canada, Belgium, Europe, Australia, France and Ireland show a range of median survival age from 44 to 53 years, and median age at death ranging from 29 to 35.6 years2. The greater longevity for patients with CF is not only a therapeutic triumph, but also a therapeutic challenge, as diseases and complications of aging now must be factored into the care of patients with CF. This article and this volume (in much greater depth than this article can provide) will address how the CF field achieved this greatly improved survival expectation, which factors have promoted it and which have not yet been appropriately addressed, and what the rapidly developing therapeutic strategies hold for the future. Since there is variability around the world in the timing and application of various advances, in this article we will concentrate on milestones in the United States.
Dr Kimberly A McBennett a pulmonologist and Director of the CF Center at Case Western Reserve University School of Medicine, Cleveland, and the Rainbow Babies and Children’s Hospital, Cleveland, Ohio, USA.
– This excellent article by three acknowledged experts from the US does, as they clearly state, deal almost exclusively with progress and developments in the US largely ignoring developments elsewhere; this should be kept in mind by the reader.
Jonathan Guo, Anna Garratt, Andrew Hill. Worldwide rates of diagnosis and effective treatment for cystic fibrosis. J Cyst Fibros 2022 Feb 3;S1569-1993(22)00031-5.doi: 10.1016/j.jcf.2022.01.009.Online ahead of print. [Pubmed]
Jonathan Guo
Background: Time has seen management for Cystic Fibrosis (CF) advance drastically, most recently in the development of the disease-modifying triple combination therapy ivacaftor/tezacaftor/elexacaftor. There is currently limited evidence regarding both the global epidemiology of CF and access to this transformative therapy – and therefore where needs are not being met. Therefore, this study aims to define gaps in access to CF treatment.
Methods: Patient data were extracted from established CF registries. Where these were not available, literature searches were conducted alongside an international survey of 51 CF experts to determine the diagnosed patient population. National CF prevalence estimates were combined with registry data on estimated population coverage, to extrapolate the total estimated number of undiagnosed patients. Estimates of ivacaftor/tezacaftor/elexacaftor treatment coverage were extracted from publicly available sales summaries and pricing data.
Results: 162,428 [144,606-186,620] people are estimated to be living with CF across 94 countries. Of these, an estimated 105,352 (65%) are diagnosed, with 19,516 (12%) receiving triple combination therapy. We estimated 57,076 patients with undiagnosed CF. Owing to a paucity of high-quality data, estimates of undiagnosed CF in low- and middle-income countries are highly uncertain. Patient registries were available in 45 countries, and used to identify 90% of the estimated diagnosed population.
Conclusions: A significant CF patient burden exists in countries where disease-modifying drugs are unavailable, and final figures are likely underestimates. This analysis shows the potential to improve rates of diagnosis and treatment for CF, so a higher percentage of patients receive the most effective triple combination treatment.
Dr Jonathan Guo is in the Faculty of Medicine, Imperial College London, United Kingdom.
Adèle Coriati, Xiayi Ma, Jenna Sykes, Sanja Stanojevic, Rasa Ruseckaite, Lydie Lemonnier, Clémence Dehillotte, Jan Tate, Catherine Ann Byrnes, Scott C Bell, Pierre Regis Burgel, Anne L Stephenson. Beyond borders: cystic fibrosis survival between Australia, Canada, France and New Zealand. Thorax. 2022 Sep 15;thoraxjnl-2022-219086.doi: 10.1136/thorax-2022-219086.Online ahead of print. [Pubmed]

Adele Coriati linkedin.com
Background: Life expectancy for people with cystic fibrosis (CF) varies considerably both within and between countries. The objective of this study was to compare survival among countries with single-payer healthcare systems while accounting for markers of disease severity.
Methods: This cohort study used data from established national CF registries in Australia, Canada, France and New Zealand from 2015 to 2019. Median age of survival for each of the four countries was estimated using the Kaplan-Meier method. A Cox proportional hazards model was used to compare risk of death between Canada, France and Australia after adjusting for prognostic factors. Due to low number of deaths, New Zealand was not included in final adjusted models.
Results: Between 2015 and 2019, a total of 14 842 people (3537 Australia, 4434 Canada, 6411 France and 460 New Zealand) were included. The median age of survival was highest in France 65.9 years (95% CI: 59.8 to 76.0) versus 53.3 years (95% CI: 48.9 to 59.8) for Australia, 55.4 years (95% CI: 51.3 to 59.2) for Canada and 54.8 years (95% CI: 40.7 to not available) for New Zealand. After adjusting for individual-level factors, the risk of death was significantly higher in Canada (HR 1.85, 95% CI: 1.48 to 2.32; p<0.001) and Australia (HR 2.08, 95% CI: 1.64 to 2.64; p<0.001) versus France.
Interpretation: We observed significantly higher survival in France compared with countries with single-payer healthcare systems. The median age of survival in France exceeded 60 years of age despite having the highest proportion of underweight patients which may be due to differences in availability of transplant.
Dr Adèle Coriati is a post doctoral fellow in the Department of Respirology, St Michael’s Hospital, Toronto, Ontario, Canada
.
