VITAMINS MAIN SECTION- General, Vitamins A, B, D, E, K
GENERAL
2011 Morton A. Why bother to take vitamins? J R Soc Med 2011; 104 Suppl 1:S19-529.[PubMed]

Alison Morton
This is an excellent review of vitamin therapy in cystic fibrosis by Alison Morton the Chief Dietitian at the Leeds Adult CF Centre. Alison retired in 2016.
1981 Congdon PJ, Bruce G, Rothburn MM, Clarke PCN, Littlewood JM, Kelleher J, Losowsky MS. Vitamin status in treated patients with cystic fibrosis. Arch Dis Child 1981; 56:708-714.[PubMed]
This was our first nutritional research study from Seacroft and St James University Hospital, Leeds collaborating with the University Department of Medicine at St James’s. The data was presented at the 1980 Toronto CF Conference. It was the first of many studies on the nutritional and gastrointestinal

Congden et al 1981
aspects of CF carried out in collaboration with Dr. Jerry Kelleher and members of Professor Monty Losowsky’s Department of Medicine. This study was coordinated by the late Dr. Peter Congden. Many of our patients, and those of some of our paediatric colleagues who were also included, had unexpectedly low fat-soluble vitamin levels (figure 1) and suboptimal control of intestinal absorption despite what we considered to be adequate enzyme and vitamin supplements; but the water soluble vitamin levels were satisfactory.
These disappointing results, reflecting our suboptimal treatment in the late Seventies, prompted us to start annual Comprehensive CF Assessments in May 1980 along the lines suggested by Crozier in 1974; he stated that “success of treatment will depend on a complete assessment of the patient and then continuing attempts to obtain normal bodily function and maintain it”.
Our so-called “Comprehensive CF Assessments”, which we started in 1980, proved so useful in identifying areas where we could improve treatment of our own patients, that in 1981 I offered the service to paediatric colleagues in the Yorkshire Region for their patients. It was through this offer, to accept patients for assessment and advice that the Leeds Regional CF Service developed.
1989 Sokol RJ. Reardon MC. Accurso FJ. Stall C. Narkewicz M. Abman SH. Hammond KB. Fat-soluble-vitamin status during the first year of life in infants with cystic fibrosis identified by screening of newborns. Am J Clin Nutr 1989; 50:1064-1071. [PubMed]

Ronald Sokell
Another report on infants diagnosed in the Colorado neonatal screening programme. Fat-soluble vitamin status during the first year of life in 36 infants with CF was examined; biochemical evidence of fat-soluble-vitamin deficiency is common before the age 3 months in CF infants.
– A further report on these 36 infants (Sokol RJ, et al. Pediatr Pulmonol 1991; Suppl 7:52-55) after treatment with pancreatic enzymes, a multiple vitamin preparation, and additional vitamin E was associated with normalization of serum albumin, retinol, and 25-hydroxyvitamin D and negative PIVKA testing (for vitamin K) at six and 12 months of age. Several patients remained vitamin E deficient, but this was felt to be due to poor adherence to the treatment.
These studies from Denver of some of the earlier screened CF infants were important as they drew attention to the very early onset of nutritional deficiencies in the infants. Biochemical evidence of fat-soluble vitamin deficiency is common before three months of age and responds to adequate supplementation in the first year of life. Also the initial fall off in weight gain may take many months to recover.
HuiChuan J Lai, Lyanne H Chin, Sangita Murali, Taiya Bach, Danielle Sander, Philip M Farrell, FIRST Study Group. Vitamins A, D, E status as related to supplementation and lung disease markers in young children with cystic fibrosis. Pediatr Pulmonol 2022 Jan 11.doi: 10.1002/ppul.25825. Online ahead of print.[Pubmed]

HuiChuan J Lai
Background: The variable response to fat-soluble vitamin supplementation in young children with CF, and factors contributing to this variability, remain under-investigated.
Objective: To determine if recommended supplement doses normalize serum vitamin A (retinol), D (25-hydroxy-vitamin D, 25OHD) and E (α-tocopherol), and identify factors predictive of achieving sufficiency, in children with CF in the first 3 years of life.
Design: We studied 144 infants born during 2012-2017 and diagnosed with CF through newborn screening. Serum retinol, 25OHD, α-tocopherol and plasma cytokines interleukin(IL)-6, IL-8, IL10 and tumor necrosis factor (TNF)-α were measured in early infancy and yearly thereafter. Vitamin supplement intakes and respiratory microbiology were assessed every 1-2 months in infancy and quarterly thereafter.
Results: The prevalence of vitamin D insufficiency (<30 ng/mL) at all ages combined was significantly higher (22%) compared to vitamin A (<200 ng/mL, 3%) and vitamin E (<5 µg/mL, 5%). All children were vitamin A sufficient by age 2 years. Vitamin E insufficiency was rare. Only 42% were early responders of vitamin D and 17% remain insufficient despite high supplement intakes. IL-6 was positively correlated, while IL-8, IL-10 and TNF-α were negatively correlated, with retinol and 25OHD. Multiple regression analysis revealed that supplement dose, season, α-tocopherol, pancreatic insufficiency, respiratory infections and IL-10 were significant predictors of 25OHD.
Conclusion: Diagnosis through newborn screening coupled with supplementation normalized serum retinol and α -tocopherol in almost all infants with CF by age 3 years. However, response to vitamin D supplements in young children with CF occurred later and variably despite early and sustained supplementation.
HuiChuan J Lai is Professor Nutritional Sciences , Pediatrics and Population Health Sciences in the Departments of Nutritional Sciences and the Department of Pediatrics University of Wisconsin-Madison, Madison, Wisconsin, USA.
VITAMIN A
1933 Blackfan KD, Wolbach SB. Vitamin A deficiency in infants. J Pediatr 1933; 3:679-706.

Kenneth Blackfan
Kenneth Blackfan (1883-1941) (figure) was Associate Professor of Pediatrics at Johns Hopkins, then Professor of Pediatrics at Cincinnati and at Harvard from 1923 to 1941. He apparently ‘mentored’ both Louis Diamond and Sydney Farber. In 1941 he died of lung cancer at the age of 58 – at the height of his career. The Children’s’ Hospital in Boston is on Blackfan Street – named after him.
This is an interesting account primarily of early vitamin A deficiency, in which there was considerable interest at the time. In 13 infants and young children, 11 of whom were eventually autopsied, vitamin A deficiency was reported. Epithelial metaplasia due to vitamin A deficiency was considered an important predisposing factor to infection by causing – “loss of protective powers of the epithelium due to diminished or absent mucus secretion and loss of ciliary motion”. Six of the 11 infants autopsied had extensive pancreatic lesions (later recognised as typical of CF), that the authors correctly attributed to inspissation of secretion in the ducts.
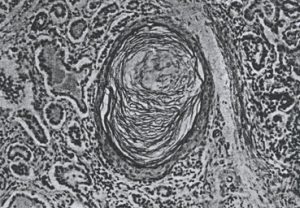
Histology of pancreas Blackfan & Wolbach,1933
The authors noted that “The pancreatic lesions were all identical and presumably representing a disease entity. At first we regarded the pancreatic changes as the result of vitamin A deficiency (as did Dorothy Andersen for some years). As the same condition has been found scores of times without other evidences of vitamin A deficiency and since it is not constant even in vitamin A deficiency, we must consider the two are not necessarily connected”. The photomicrograph of pancreas (figure 3) is typical of the changes seen in CF for which Blackfan & May (1938 below) gave credit to Wolbach for the first clear description.
The authors continue “The pancreatic lesion referred to is characterised by dilatation of acini and ducts, by inspissated secretion, atrophy of the acini, lymphoid and leukocyte infiltration of some degree and fibrosis. Our preliminary studies indicate that the pathogenesis of this striking pancreatic affection resides in the production of an abnormal secretion which inspissates and leads to distension and atrophy of ducts and acini. It is reasonable to assume that this pancreatic lesion, if extensive, may be responsible for failure to utilise fats and hence vitamin A in the presence of an adequate intake”.
The authors concluded that vitamin A deficiency was not infrequent and should be suspected without regard to the characteristic eye signs; histological evidence of vitamin A deficiency may appear in infants who appear to be receiving and adequate intake; they postulate that some factor or factors interfering with storage or utilisation of this vitamin lessens the availability of the supply essential for normal nutrition; certain diagnostic criteria to identify at an early stage are mentioned and vitamin A deficiency should be considered as a general systemic disease rather than as a local disease of the eye.

Simeon Wolbach. From Dept of the History of Science, Havard University websit
Simeon Burt Wolbach was born in 1880 in Grand Island, Nebraska, and grew up on the western plains. He attended Harvard Medical School (M.D., 1903), studying pathology under Councilman and Mallory. After medical school, he worked as director of the Bender Hygienic Laboratory in Albany, NY; pathologist at the Montreal General Hospital and teacher at McGill Medical School. In 1910, he returned to Harvard as an assistant professor of bacteriology. He was promoted to associate professor in 1914. In 1916, he was jointly appointed to the Departments of Bacteriology and Pathology. In 1917, he was pathologist to the Peter Bent Brigham Hospital and the Boston Lying-In Hospital. In 1922, he was appointed the Shattuck professor of pathology at Harvard. He held this position for 25 years. In 1947, he became the director of the Division of Nutritional Research at Children’s Hospital in Boston. He held this position until his death in 1954. Wolbach’s interests ranged from the effects of radiation to tropical medicine and infectious diseases. His work on radiation began with Porter in 1907. Later in life, he served as a consultant to the US Atomic Energy Commission (1951-1953). He did field research in Nigeria in 1911 related to the pathology of general paresis. Best known of his work on infectious diseases are his contributions to the understanding rickettsial illnesses, Rocky Mountain spotted fever (1919), and epidemic typhus in Poland (1920). Wolbach’s most fundamental work was in the field of vitamin research, and the relationships of vitamins to tissue structure and the pathology of scurvy and other diseases.
1946 Palmer HD, Danielson WH, Lubchenco LO, Binkley EL. Absorption of vitamin A following enteral use of prostigmine in cystic fibrosis of pancreas. Am J Clin Path 1946; 16:535-549.
Prostigmine was apparently used by Flack to improve bowel motility, which was presumably the rationale for this study. However, oral or parenteral prostigmine did not improve vitamin A absorption in 3 children with CF but did induce active intestinal peristalsis. So the authors concluded that prostigmine did induce active peristalsis in patients with cystic fibrosis and seemed to promote regularity of bowel movements but the improvement was not greater than in children receiving their current supportive therapy.
1968 Petersen RA, Petersen VS, Robb RM. Vitamin A deficiency with xerophthalmia and night blindness in cystic fibrosis. Am J Dis Child 1968; 116:662-665. [PubMed]
The first report of night blindness in CF due to vitamin A deficiency in 16 year old girl who had been seriously under-treated and who had major social problems. Later reports showed abnormal nocturnal vision due to vitamin A deficiency (Rayner et al,1989 below) but not where vitamin levels had been monitored regularly and maintained in the normal range (Ansari et al, 1999 below).
1970 Keating JP, Feigin RD. Increased intracranial pressure associated with probable vitamin A deficiency in cystic fibrosis. Pediatrics 1970; 46:41-46. [PubMed]
Two infants with CF aged four months had signs of raised intracranial pressure associated with vitamin A deficiency. One infant had xerophthalmia and keratomalacia; one had a cranial nerve injury with facial paralysis (also Abernathy 1976 below). Raised intracranial pressure has been described by a number of authors in young infants with CF and also in non-CF infants with vitamin A deficiency examples of which are reviewed in this paper.
1989 Rayner RJ, Tyrell JC, Hiller EJ, Marenah C, Neugebauer MA, Vernon SA, Brimlow G. Night blindness and conjunctival xerosis due to vitamin A deficiency in cystic fibrosis. Arch Dis Child 1989; 64:1151-1156. [PubMed]
Rosie Rayner, then the CF Research Fellow at Nottingham and now paediatrician in Wolverhampton, studied 43 patients with CF aged 8 to 44 years (median 16 years), for evidence of vitamin A deficiency. Eight had abnormal dark adaptation tests and three had conjunctival xerosis. Serum vitamin A and retinol binding protein concentrations were significantly lower in the affected patients who were also more likely to have abnormal liver function tests. Five patients were treated with 100,000-200,000 IU water miscible vitamin A orally and their daily vitamin supplements were increased to maintain normal concentrations. In four patients dark adaptation tests were repeated. Three were normal, but one patient required three further doses of water miscible vitamin A and a daily supplement of 12,000 IU vitamin A before her dark adaptation threshold returned to normal. Adolescents with cystic fibrosis are liable to develop night blindness and conjunctival xerosis, particularly if they have liver disease or fail to take daily vitamin supplements.
– One of the papers reporting objective evidence of the clinical effects vitamin deficiency rather than merely reduced plasma levels. Obviously very important if adults with CF, of which there were increasing numbers, were driving at night. Histological evidence of vitamin A deficiency was evident in many of the early post-mortem studies – in fact, for some time it was regarded by Dorothy Andersen as a major factor in the pathogenesis of the condition.
1995 Morkeberg JC, Edmund C, Prause JU, Lanng S, Koch C, Michaelsen KF. Ocular findings in cystic fibrosis patients receiving vitamin A supplementation. Graefe’s Arch Clin Exp Ophthalmol 1995; 233:709-713. [PubMed]
Only 26% of 35 patients examined in the Copenhagen clinic had normal vitamin A status as measured by serum retinol and light sensitivity but reduced contrast sensitivity. Conjunctival imprints showed dry eye in 42%; decreased tear stability in 49% and other abnormalities of low tear production (31%) and increased numbers of dying cells (23%). In fact 26% were considered to have the criteria for “keratoconjunctivitis sica”. The authors even suggested that the high incidence of dry eye could be a primary manifestation of CF.
These findings are more likely the result of suboptimal vitamin A status particularly as only 26% had normal vitamin A levels. In studies where vitamin A status is regularly monitored to maintain normal serum levels, only reduced contrast sensitivity is found (Ansari et al. 1999 below) and the cause of this is unexplained.
1999 Ansari EA, Sahni K, Etherington C, Morton A, Conway SP, Moya E, Littlewood JM. Ocular signs and symptoms and vitamin A status in patients with cystic fibrosis treated with daily vitamin A supplements. Br J Ophthalmol 1999; 83:688-691. [PubMed]
Since the first Leeds studies on vitamin levels in 1978 (Congden et al, 1981 above), oral supplementation has been guided by annual monitoring of vitamin levels; also all patients are seen regularly by a CF specialist dietitian and most have a comprehensive annual dietary assessment. None of the 28 patients in this study had vitamin A deficiency, the median value of serum retinol being 48 microg/dl, range 31-80 microg/dl (normal range 30-80 microg/dl). Dark adaptation was normal in all patients compared with the control group where the mean value was 3.4 log units of threshold luminance (95% confidence interval 2.4-4.0). None of the test group had a value of threshold luminance 2 SD above the mean value for the control group. Eight patients had reduced contrast sensitivity. The median value for serum zinc was 14.2 micromol/ l, range 13-81 micromol/l (normal range 8-23 micromol/l) and the median value for retinol binding protein was 36 mg/l, range 13-81 mg/l (normal range 35-58 mg/l). There was no correlation between dark adaptation and serum retinol, zinc, or retinol binding protein. Two patients had clinical evidence of dry eye.
– So regular estimates of plasma vitamin A, together with appropriate supplementation and expert dietetic review, can maintain normal dark adaptation in patients with cystic fibrosis. The occurrence of reduced contrast sensitivity function is well documented in CF and confirmed in this study but remains an unexplained phenomenon (also Morkeberg et al, 1995 above).
2006 Aird FK. Greene SA. Ogston SA. Macdonald TM. Mukhopadhyay S. Vitamin A and lung function in CF. J Cyst Fibros 2006; 5:129-131. [PubMed]
Laboratory evidence suggests that vitamin A could have a protective effect on respiratory status in patients with cystic fibrosis (CF). This study shows a significant correlation between serum vitamin A concentrations and every aspect of lung function tested in 38 patients with stable CF. Serum vitamin D and vitamin E concentrations were also measured but did not show any significant correlations with lung function.
This is interesting as Dorothy Andersen initial likened the changes in the bronchial epithelium to the epithelial metaplasia found in vitamin A deficiency and for some years considered that the pulmonary problems were related to the changes in the bronchial epithelium leading to a infection – i.e. the condition was primarily the result of intestinal malabsorption resulting in vitamin deficiency. The authors of the present paper note this is the first study showing a definite relationship between vitamin A levels and respiratory function tests in CF. Earlier Bines et al 2005 had found no relationship between lung inflammation and vitamin A or vitamin E (Bines JE et al. J Paediatr Child Health 2005; 41:663-668. [PubMed]).
2007 Basu AP. Kumar P. Devlin AM. O’Brien CJ. Cystic fibrosis presenting with bilateral facial palsy. Eur J Paediatr Neurol 2007; 11:240-242. [PubMed]
A 15-week old male infant presented with bilateral lower motor neuron facial palsy of unknown cause. Subsequently his growth deteriorated and he developed progressively worsening cough and wheeze. A diagnosis of cystic fibrosis was confirmed and hypovitaminosis A detected. Improvement of the facial palsy was noted following standard management of cystic fibrosis including vitamin A supplementation.
Presentations due to the manifestations of vitamin deficiency, particularly of vitamin A, are well documented. A similar case in a 10 week old infant was reported with low vitamin A levels and bilateral facial nerve paralysis (Cameron C et al. J Cyst Fibros 2007; 6:241-243. [PubMed]
2010 Cheng MP, Paquette K, Lands LC, Ovetchkine P, Theoret Y, Quach C. Voriconazole inhibition of vitamin A metabolism: are adverse events increased in cystic fibrosis patients? Pediatr Pulmonol 2010; 45:661-666.
Five of six CF patients receiving treatment with voriconazole developed photosensitivity, and all six patients reported visual disturbances. One 7-year-old boy developed striking erythema in the face and upper thorax; a 16-year-old girl who reported unexpected visual disturbances, including scotomas and tunneling vision. So significant adverse effects of voriconazole were noted in all treated CF patients. The authors suggest that this may be due to suppression of activity of hepatic enzymes involved in all transretinonic acid metabolism coupled with vitamin A supplementation in CF. They suggest that consideration should be given to reducing vitamin A supplementation during voriconazole treatment.
Voriconazole is used increasingly frequently to eradicate or control fungal infections such as Aspergillus which are becoming an increasing problem but the drug appears to be associated with significant side effects.
2015 Woestenenk JW; Broos N; Stellato RK; Arets HG; van der Ent CK; Houwen RH. Serum retinol levels and pulmonary function in children and adolescents with cystic fibrosis. J Cyst Fibros 2015; 14(3):392-7.[PubMed]
It has been suggested that higher serum retinol levels could have protective effects on pulmonary function (PF) in patients with cystic fibrosis (CF). However, serum retinol levels will be transiently decreased during pulmonary exacerbation. Therefore, the extent of chronic pulmonary inflammation should be included when describing the association between PF and serum retinol. The authors studied the longitudinal relation between serum retinol, immunoglobulin G (IgG) and PF in paediatric CF patients. They measured the serum retinol, IgG and forced expiratory volumes in one second (FEV1% pred.) of 228 CF patients during a seven-year follow up period. The cross-sectional and longitudinal relations between these variables were assessed.
Serum retinol, with medians levels between 1.2 and 1.4 mumol/l, were relatively stable, while median serum IgG gradually increased during the age years. The FEV1% pred. was longitudinally inversely associated with serum IgG and age, but not with serum retinol. Each g/l increase in serum IgG level was associated with an accelerated yearly decline in FEV1% pred. of 0.5% (95% CI -0.8 to -0.1, p=0.008), and each year increase in age was associated with a 1.7% (95% CI -2.1 to -1.3, p=0.000) decline in FEV1% pred. This effect was not observed with respect to serum retinol levels (95% CI -1.9 to 2.2, p=0.570).
– In this retrospective study the authors found no evidence that higher serum retinol levels had protective effects on pulmonary function. The well-known association between a rising IgG and declining FEV1% pred. was confirmed.
2014 Safi KH, Filbrun AG, Nasr SZ. Hypervitaminosis A causing hypercalcemia in cystic fibrosis. Case report and focused review. Am Thorac Soc 2014; 11(8):1244-7. doi: 10.1513/AnnalsATS.201404-170BC.[PubMed]
Hypercalcemia is a rare complication of hypervitaminosis A. The authors report a 4-year old child with cystic fibrosis (CF) and pancreatic insufficiency who was found to have hypervitaminosis A causing hypercalcemia, complicated by nephrocalcinosis and renal impairment. She was managed by withholding vitamin A supplements, aggressive diuresis, and prednisolone.
The authors emphasise the importance of regular vitamin A monitoring in patients with CF. There is a wide variability for the lowest intake of vitamin A required to cause toxicity.
– It is disappointing to read that there are still children with CF who do not have their fat soluble vitamin
levels monitored on a regular basis – a practice recommended for over 30 years!
VITAMIN B
1973 Rucker RW. Harrison GM. Vitamin B 12 deficiency in cystic fibrosis. N Engl J Med 1973; 289:329. [PubMed]
Some malabsorption of vitamin B12 has been demonstrated in a number of later studies but absorption is much improved when pancreatic extract is added although not in all patients. However, in practice, a deficiency of the vitamin is very rare in CF even though supplements are not usually given (also Deren JJ et al. NEJM 1973; 288:949-950.[PubMed]; Gueant JL et al. Pancreas 1990; 5: 559-567.[PubMed]).
2001 McCabe H. Riboflavin deficiency in cystic fibrosis: three case reports. J Hum Nutr Diet 2001; 14:365-370. [PubMed]

Helen McCabe
Three cases of clinical riboflavin deficiency are reported in children aged 2-10 years attending a regional Cystic Fibrosis clinic. Riboflavin deficiency presented as angular stomatitis in all three patients. Patients were confirmed to be riboflavin deficient by assaying the activity of erythrocyte glutathione reductase. Patients were not on routine supplements of water-soluble vitamins before presentation and were treated with riboflavin supplements as part of a water-soluble vitamin complex. At presentation, one patient had poor nutritional status, but two patients were adequately nourished, receiving overnight gastrostomy feeds. Data on these two patients indicate an adequate dietary intake of riboflavin, suggesting a mechanism for increased requirements, inadequate absorption or utilization. Additional deficiencies of thiamin, pyridoxine and iron were also observed.
This paper reports the occurrence of a riboflavin (vitamin B2) deficiency not previously reported in the cystic fibrosis population.
Helen McCabe is Specialist CF Dietitian at the Great North Children’s Hospital in Newcastle upon Tyne.
2014 Maqbool A. Schall JI. Mascarenhas MR. Dougherty KA. Stallings VA. Vitamin B(12) status in children with cystic fibrosis and pancreatic insufficiency. J Pediatr Gastroenterol Nutr 2014; 58:733-8.[PubMed]
Serum B12 status was assessed in 106 subjects (5-18 years) and categorised as elevated (serum B12 above reference range for age and sex [Hi-B12]) or within reference range (serum B12 within reference range for age and sex) for age and sex. The serum B12 was elevated in the majority of children with CF and PI. However, supplement-based B12 intake was 6 to 10 times the RDA, and strongly predicted elevated serum B12 status.
The authors conclude that health consequences of lifelong high supplement-based B12 intake and high serum B12 are unknown and require further study, as does the inverse correlation between serum B12 and forced expiratory volume at 1 second.
(See also Rucker RW et al, 1973. N Engl J Med 1973; 289:329. Above also Topics -> gastroenterology -> vitamins -> Vitamin B).
VITAMIN D
There are numerous publications on vitamin D status and supplementation usually indicating suboptimal plasma levels and an inadequate degree of supplementation. These are clearly reviewed by Alison Morton in the article mentioned above at the start of this Topic section (Morton A. Why bother to take vitamins? J R Soc med 2011; 104 Suppl 1: S19-s29).
On the subject of vitamin D, a Cochrane Data Base Systematic Review (2012; 4:CD007298) concluded “There is no evidence of benefit or harm in the limited number of small-sized published trials. Adherence to relevant published guidelines on vitamin D should be considered until further evidence is available
2007 Bone mineralisation in cystic fibrosis. Report of the UK Cystic Fibrosis Trust Bone Mineralisation Working group. February 2007.Section 4.4.1. Available on the CF Trust website (www.cftrust.org.uk).
1977 Scott J, Elias E, Moult PJ, Barnes S, Wills MR. Rickets in adult cystic fibrosis with myopathy, pancreatic insufficiency and proximal renal tubular dysfunction. Am J Med. 1977 Sep;63(3):488-92. [PubMed]
Rickets is reported in a 19 year old white man with cystic fibrosis in whom pancreatic and hepatic involvement was advanced. There was evidence of secondary hyperparathyroidism with proximal renal tubular acidosis, aminoaciduria, phosphaturia and hypophosphatemia. Treatment with oral pancreatic and parenteral vitamin D supplements led to full recovery of the rachitic syndrome and the proximal renal tubular dysfunction.
2011 Pincikova T, Nilsson K, Moen IE, Karpati F, Fluge G, Hollsing A, Knudsen PK, Lindblad A, Mared L, Pressler T, Hjelte L. Scandinavian Cystic Fibrosis Study Consortium. Inverse relation between vitamin D and serum total immunoglobulin G in the Scandinavian Cystic Fibrosis Nutritional Study. Eur J Clin Nutr 2011; 65:102-109. [PubMed]
The hallmark of cystic fibrosis (CF) is chronic lung inflammation. The severity of lung disease is closely correlated with immunoglobulin G (IgG) levels. Beyond its contribution to the bone health, the importance of vitamin D has not been fully recognized owing to the lack of human studies providing evidence of its benefit. In the context of the recently described immunomodulatory functions of vitamin D, the authors aimed to assess the relationship between vitamin D and IgG levels. Eight hundred and ninety-six CF patients were included (0.53-65.9 years) from seven centers in Denmark, Norway and Sweden. The authors found that Serum 25OHD was positively associated with FEV1 and concluded that increasing vitamin D intake may positively modulate inflammation in CF. This study supports the proposed role of vitamin D in the immune system during infection and substantiates prospective studies.
This is a relatively recently suggested role for vitamin D and reinforces the importance of adequately supplementing patients with CF to achieve a normal serum vitamin D level.
2014 McCauley LA. Thomas W. Laguna TA. Regelmann WE. Moran A. Polgreen LE. Vitamin D deficiency is associated with pulmonary exacerbations in children with cystic fibrosis. Ann Am Thor Soc 2014; 11(2):198-204.[PubMed]
A study to assess associations between vitamin D and % predicted lung function, pulmonary exacerbations, and first Pseudomonas aeruginosa infection in children with CF. This is a retrospective longitudinal study of 130 children aged 6 to 18 years between 2000 and 2012 examined 25-OHD levels classed in three vitamin D groups: sufficient (>30 mug/L), insufficient (20-29 mug/L), and deficient (<20 mug/L). Longitudinal models followed individuals’ changing vitamin D groups over time to compare numbers of pulmonary exacerbations (defined by hospitalisation), incidence of first P. aeruginosa infection, and % predicted lung function. Cross-sectional comparisons between vitamin D groups were performed at ages 8, 12, and 16 years.
The prevalence of vitamin D deficiency and insufficiency increased slowly through adolescence. The rate of exacerbations for the deficient vitamin D group, aged 15 to 18 years, was 13.1 per 10 patient-years, significantly higher than 4.3 per 10 patient-years for the insufficient and sufficient vitamin D groups (P < 0.05), which were not significantly different There were no differences between vitamin D groups in pulmonary function or incidence of first P. aeruginosa infection, which was about 2 per 10 patient-years.
The authors concluded that higher 25-OHD levels in children with CF were associated with lower rates of pulmonary exacerbations and, in adolescents, higher FEV1.
– Patients with higher vitamin D levels may have received a better general standard of care, with closer attention to nutrition, than those allowed to become vitamin deficient and hence also have had fewer exacerbations. It is surprising the number of patients who are still allowed to become deficient in fat soluble vitamins when the need for regular monitoring of fat soluble vitamin levels in cystic fibrosis has been recognised for over 30 years.
2015 Vanstone MB; Egan ME; Zhang JH; Carpenter TO. Association between serum 25-hydroxyvitamin D level and pulmonary exacerbations in cystic fibrosis. Pulmonology 2015; 50(5):441-6. [PubMed]
The annual number of pulmonary exacerbations in pediatric CF patients was found to be significantly associated with 25-OHD levels and gender, raising the consideration that maintaining vitamin D sufficiency may lead to decreased incidence of pulmonary exacerbations and hospitalisations requiring
antibiotic therapy.
– It is surprising that there are still reports of children with CF who have suboptimal vitamin D levels despite the fact that the tendency to low fat soluble vitamin levels and the need for adequate monitoring and appropriate supplementation has been known for over 30 years! It could be that in the group with increased pulmonary exacerbations and low levels of vitamin D, both were a reflection of the care the patients received?
2014 Simoneau T, Bazzaz O, Sawicki GS, Gordon C. Vitamin D status in children with cystic fibrosis. Associations with inflammation and bacterial colonization. Ann Am Thorac Soc. 2014 Feb;11(2):205-10. doi: 10.1513/AnnalsATS.201306-171BC. [Free full text] [PubMed]
This was a retrospective chart review of patients with CF under the age of 12 years who presented to the Boston Children’s Hospital and had their fat soluble vitamin levels measured. Serum laboratory parameters, growth indices, pancreatic status, CFTR genetics, medications, microbiology, and presence of CF-related co-morbidities were collected for patients who had fat-soluble vitamin levels measured between January 1, 2009 and December 31, 2011. Vitamin D deficiency was defined as a serum 25(OH)D less than 20 ng/ml and insufficiency as serum 25(OH)D 20 to 29.9 ng/ml. Associations between serum vitamin D concentration and clinical/inflammatory markers were assessed using Chi-square and t tests.
Data were collected for 148 children. The mean serum 25(OH)D concentration was 32.4 ng/ml (SD, 8.9). Seven percent (10 of 148) were vitamin D deficient, and 36 (53 of 148) were vitamin D insufficient. Among the pancreatic-sufficient patients, 50% (14 of 28) were vitamin D insufficient/deficient, whereas among pancreatic-insufficient patients, 41% (49 of 120) were vitamin D insufficient/deficient. Pseudomonas aeruginosa was a more common pathogen in the patients who were vitamin D insufficient/deficient (18 of 63 vs. 11 of 85, P = 0.018). There was no difference between vitamin D-sufficient versus -insufficient groups in terms of other bacterial colonisation or inflammatory markers.
The authors concluded vitamin D insufficiency is common among young children with CF presenting at the Boston Children’s Hospital. Vitamin D insufficiency was prevalent even in children who were pancreatic sufficient. In this population, vitamin D insufficiency is associated with a history of Pseudomonas colonization but not with classic markers of systemic inflammation.
– Dose of supplemental vitamin D was available for 131/148 patients, the median daily dose being 800 IU (0 – 3600). Of particular importance was the high frequency of vitamin D deficiency in the “pancreatic sufficient’ children (definition not stated) and the need to monitor their vitamin D status. The study was conducted before the recent CF Foundation vitamin D guidelines (Tangpricha V, et al. J Clin Endocrinol Metab 2012;97:1082–1093).
2014 McCauley LA, Thomas W, Laguna TA, Regelmann WE, Moran A, Polgreen LE. Vitamin D deficiency is associated with pulmonary exacerbations in children with cystic fibrosis. Ann Am Thorac Soc. 2014 Feb;11(2):198-204. doi: 10.1513/AnnalsATS.201208-068OC. Free PMC article [PubMed]
This study assessed associations between vitamin D and % predicted lung function, pulmonary exacerbations, and first Pseudomonas aeruginosa infection in children with CF. The authors hypothesized that children with CF who have 25-hydroxy vitamin D (25-OHD) levels less than 30 μg/L would have worse lung function and more pulmonary exacerbations than those with 25-OHD greater than or equal to 30 μg/L.
This retrospective longitudinal study of 130 children aged 6 to 18 years between 2000 and 2012 examined 25-OHD levels classed in three vitamin D groups: sufficient (≥30 μg/L), insufficient (20-29 μg/L), and deficient (<20 μg/L). Longitudinal models followed individuals’ changing vitamin D groups over time to compare numbers of pulmonary exacerbations (defined by hospitalization), incidence of first P. aeruginosa infection, and % predicted lung function. Cross-sectional comparisons between vitamin D groups were performed at ages 8, 12, and 16 years.
The prevalence of vitamin D deficiency and insufficiency increased slowly through adolescence. The rate of exacerbations for the deficient vitamin D group, aged 15 to 18 years, was 13.1 per 10 patient-years, significantly higher than 4.3 per 10 patient-years for the insufficient and sufficient vitamin D groups (P < 0.05), which were not significantly different There were no differences between vitamin D groups in pulmonary function or incidence of first P. aeruginosa infection, which was about 2 per 10 patient-year.
– This study showed that 25OHD level less than or equal to 20ug/L in children with CF was associated with three times higher rate of pulmonary exacerbations than those sufficient in vitamin D. The cause and effect was a matter of conjecture. The obvious suggestion is that the vitamin D deficiency levels were a reflection of a more general suboptimal standard of care?
Lehoux Dubois C, Labrèche E, Boudreau V, Colomba J, Mailhot M, Lavoie A, Rabasa-Lhoret R, Coriati A.Extra-skeletal impact of vitamin D supplementation protocol in an adult population with cystic fibrosis.Clin Nutr. 2018 Aug 25. pii: S0261-5614(18)32384-7. doi: 10.1016/j.clnu.2018.08.013. [Epub ahead of print] [Pubmed]

Catherine LehouxDubois
The aim was to study the association between serum vitamin D levels and key clinical factors, such as nutritional status, pulmonary function and pulmonary exacerbations (PEx) frequency, in an adult CF population. Prospective analysis of a published vitamin D (VitD3) supplementation protocol (N = 200 adult patients) over a follow-up period of 5 years. Data were collected from the medical files before (baseline) and after (follow-up) the implementation of the VitD3 supplementation protocol, between 2009 and 2014. Serum samples to measure vitamin D were also collected at baseline and follow-up.
A positive relationship between serum vitamin D and lung function was observed at baseline (R = 0.158, P = 0.027), but it disappeared at follow-up (P = 0.454). There was no association between serum vitamin D levels and body mass index. At follow-up, patients with significantly higher serum vitamin D levels were women, older in age, had CF-related diabetes or had a history of recurring PEx.
The authors concluded there was no direct link between heightened serum vitamin D and lung function or BMI in an adult CF population. They suggest that better compliance to treatments and closer follow-up from health professionals could partially explain why such patients reached higher vitamin D serum levels.
Catherine Lehoux Dubois is based at the Institut de recherches clinicque de Mantreal, Canada
Thursfield RM, Naderi K, Leaver N, Rosenthal M, Alton EWFW, Bush A, Davies JC. Children with cystic fibrosis demonstrate no respiratory immunological, infective or physiological, consequences of vitamin D deficiency. J Cyst Fibros. 2018Apr 6. pii: S1569-1993(18)30070-5. doi: 10.1016/j.jcf.2018.02.011. [Epub ahead of print] [Pubmed] Vitamin D has health benefits in many respiratory diseases but the evidence in CF is unclear. Induction of the antimicrobial peptides cathelicidin (LL37) and human-beta-defensin-2 (HBD-2) may be the mechanism of any benefit. The authors hypothesised that antimicrobial peptide levels would be decreased, and airway infection and inflammation greater, in CF children with vitamin D deficiency. The objective of the study was to explore relationships between vitamin D, LL37 and HBD-2, and airway infection, inflammation and physiology in children with CF.
Bronchoalveolar lavage (BALF) and blood were obtained from children undergoing fibreoptic bronchoscopy. 113 patients with CF, 23 with non-CF chronic suppurative lung disease (CSLD) and 6 healthy controls were included. They found no relationship between serum vitamin D and BALF HBD-2 or LL-37. There were no differences in infective or inflammatory markers between vitamin D sufficient and deficient groups. Vitamin D deficient patients (<50 nmol/L) did not have a worse FEV1 (CF: 66 (58-71)% vs. 71.5 (61-76)%, ns; non-CF CSLD: 69 (36-88)% vs. 70 (62-95)%, ns).
So the authors concluded from this, the first bronchoscopy study exploring this question, that vitamin D deficiency is not associated with immunological, infective or clinical markers of disease severity in patients with CF or CSLD.
Abu-Fraiha Y, Elyashar-Earon H, Shoseyov D, Cohen-Cymberknoh M, Armoni S, Kerem E, Wilschanski M.Increasing Vitamin D Serum Levels Is Associated With Reduced Pulmonary Exacerbations in Patients With Cystic Fibrosis.J Pediatr Gastroenterol Nutr. 2019 Jan;68(1):110-115. [PubMed]
-

Yasmeen Abu-Frai
In 2012, The North American Cystic Fibrosis Foundation (NACFF) published new guidelines for the treatment of vitamin D deficiency in individuals with cystic fibrosis (CF). The objectives of our study were to assess the efficacy of these guidelines, and to test the effect of increasing vitamin D dosage on pulmonary function and exacerbations.Pulmonary function tests and serum concentrations of 25-hydroxyvitamin D [25(OH)D] were measured 1 year before increasing vitamin D dosage according to the guidelines and at least 1 year later. In addition, days of hospitalization and pulmonary exacerbations were counted and an average per year (average number of days of hospitalization and average number of pulmonary exacerbations [PEA], respectively) was calculated.
A total of 90 patients from The Cystic Fibrosis Clinic at Hadassah Mount-Scopus Hospital, Jerusalem, Israel. The mean serum concentration of vitamin D increased significantly from 20.97 ng/mL (52.34 nmol/L) at baseline to 25.41 ng/mL (63.42 nmol/L) at the end of follow-up (P < 0.001). The number of PEA decreased significantly from 2.79 ± 3.96 to 2.15 ± 2.91 (P = 0.007). The change in vitamin D levels was correlated with a decrease in PEA (correlation coefficient = -0.318, P = 0.002).
The authors concluded the NACFF guidelines for management of vitamin D deficiency improve vitamin D levels in patients with CF but did not reach the normal values in most patients. The increase in vitamin D serum levels was, however, associated with a decrease in number of pulmonary exacerbations.
A study from the CF Center, Hadassah-University Medcial Center, Jerusalem.
Dr Yasmeen Abu-Fraiha is a young Israeli Arab of Bedouin origincurrently acting as the Executive Director of GENESIS, an NGO she founded that aims to prevent genetic diseases in the Middle East, especially in the Bedouin community, by spearheading premarital genetic testing and matching. She holds a BSc in Medical Science from the Hebrew University of Jerusalem and an MD from the Hebrew University of Jerusalem.
Timmers NKLM, Stellato RK, van der Ent CK, Houwen RHJ, Woestenenk JW.Vitamin D intake, serum 25-hydroxy vitamin D and pulmonary function in paediatric patients with cystic fibrosis: a longitudinal approach. Br J Nutr. 2019 Jan;121(2):195-201. doi: 10.1017/S0007114518003021. Epub 2018 Nov 16. [Pubmed]
The authors aimed to assess whether current vitamin D supplement recommendations are optimal for preventing deficiencies and whether higher serum 25(OH)D levels have long-term beneficial effects on pulmonary function. The authors examined the longitudinal relationship between vitamin D intake, serum 25(OH)D and PF in 190 CF children during a 4-year follow-up period. We found a significant relationship between total vitamin D intake and serum 25(OH)D (β = 0·02; 95 % CI 0·01, 0·03; P = 0·000). However, serum 25(OH)D decreased with increasing body weight (β = -0·79; 95 % CI -1·28, -0·29; P = 0·002). Furthermore, we observed a significant relationship between serum 25(OH)D and forced expiratory volume in 1 s (β = 0·056; 95 % CI 0·01, 0·102; P = 0·018) and forced vital capacity (β = 0·045; 95 % CI 0·008, 0·082; P = 0·017).
The authors conclude that in the present large study sample, vitamin D intake is associated with serum 25(OH)D levels, and adequate serum 25(OH)D levels may contribute to the preservation of PF in children with CF. Furthermore, to maintain adequate levels of serum 25(OH)D, vitamin D supplementation should increase with increasing body weight. Adjustments of the international CF nutritional guidelines, in which vitamin D supplementation increases with increasing weight, should be considered.
Carmen Mangas-Sánchez, María Garriga-García, María Juliana Serrano-Nieto, Ruth García-Romero, Marina Álvarez-Beltrán, Elena Crehuá-Gaudiza, Rosana Muñoz-Codoceo, Lucrecia Suárez-Cortina, Saioa Vicente-Santamaría, Cecilia Martínez-Costa, Juan José Díaz-Martin, Carlos Bousoño-García, David González-Jiménez Vitamin D Status in Pediatric and Young Adult Cystic Fibrosis Patients. Are the New Recommendations Effective? Nutrients 2021 Dec 9;13(12):4413.doi: 10.3390/nu13124413. Free PMC article [Pubmed]

Carmen Mangas-Sanchez
Introduction: In recent years, guidelines for vitamin D supplementation have been updated and prophylactic recommended doses have been increased in patients with cystic fibrosis (CF).
Objective: To evaluate safety and efficacy of these new recommendations.
Results: Two cohorts of pancreatic insufficient CF patients were compared before (cohort 1: 179 patients) and after (cohort 2: 71 patients) American CF Foundation and European CF Society recommendations were published. Cohort 2 patients received higher Vitamin D doses: 1509 (1306-1711 95% CI) vs 1084 (983-1184 95% CI) IU/Day (p < 0.001), had higher 25 OH vitamin D levels: 30.6 (27.9-33.26 95% CI) vs. 27.4 (25.9-28.8 95% CI) ng/mL (p = 0.028), and had a lower prevalence of insufficient vitamin D levels (<30 ng/mL): 48% vs 65% (p = 0.011). Adjusted by confounding factors, patients in cohort 1 had a higher risk of vitamin D insufficiency: OR 2.23 (1.09-4.57 95% CI) (p = 0.028).
Conclusion: After the implementation of new guidelines, CF patients received higher doses of vitamin D and a risk of vitamin D insufficiency decreased. Despite this, almost a third of CF patients still do not reach sufficient serum calcidiol levels.
Carmen Mangas-Sánchez is in the department of Pediatric Gastroenterology and Nutrition Section, Hospital Central de Asturias, 33011 Oviedo, Spain.
VITAMIN E
1956 Nitowsky HM, Gordon HH, Tildon JT. Studies of tocopherol deficiency in infants and children IV. Effects of alpha tocopherol on creatinuria in patients with cystic fibrosis of the pancreas and biliary atresia. Bull Johns Hopkins Hosp 1956; 98:361-71. [PubMed]
There are numerous studies of vitamin E deficiency in CF as the vitamin is always very low in untreated and even in some treated, but inadequately supplemented, patients. Five children with CF and two with biliary atresia had abnormal haemolysis of erythrocytes in hydrogen peroxide decreased by relatively large doses of intravenous or oral vitamin E and decreased haemolysis. Creatinuria was decreased only in the CF children.
1958 Blanc WA, Reid JD, Andersen DH. Avitaminosis E in cystic fibrosis of the pancreas: a morphologic study of gastrointestinal and striated muscle. Pediatrics 1958; 22: 494-506.
Ceroid pigment was present in the smooth muscle fibres of the gastrointestinal tract of patients with cystic fibrosis. It was first seen in those dying during the second year of life and present in all after 5 years of age, the amount increasing with age. The only other condition where this pigment is found is biliary atresia and cirrhosis. It was considered as probably due to prolonged and severe vitamin E deficiency. However, alterations in striated muscle are rare and minimal in CF but common in severe vitamin E deficiency (Martin AJP, Moore T. Some effects of prolonged vitamin E deficiency. J Hyg 1939; 39:643; Human occurrence in one case of CF by Pappenheimer AM, Victor J. Am J Path 1946; 22:395).
1961 Levin S, Gordon MH, Nitowsky HM, Goldman C, di Sant’Agnese P, Gordon HH. Studies of tocopherol deficiency in infants and children. VI. Evaluation of muscle strength and effect of tocopherol administration in children with cystic fibrosis. Pediatr 1961; 27:578-588. [PubMed] This is said to be the first randomized controlled trial in people with cystic fibrosis. A double blind placebo controlled parallel single centre randomised controlled trial in which the effect of tocopherol supplementation on muscle strength was evaluated, by means of a “hand bulb ergograph” which was squeezed to measure grip strength. There was no difference in strength noted with vitamin E supplementation – both the treated and placebo group improved.
Oppenheimer had been the first to report an infant with necrotic changes in muscle resembling those found in tocopherol deficiency (Oppenheimer. EH. Bull Johns Hopkins Hosp 1956; 98:353-358). The authors of the present studies concluded that “although the present study did not demonstrate a clinical functional effect of tocopherol therapy in patients with cystic fibrosis, its administration is recommended because of previously reported biochemical and pathological evidence of vitamin E deficiency in these subjects”.
This reasonable approach would be a lesson for some clinicians who would not use a treatment unless supported by a suitable Cochrane-approved randomised controlled trial – a view I have even heard expressed with regard to vitamin E supplements in CF! Here all the available reasonable information was considered before a policy was recommended that may well do good and was very unlikely to do harm to their patients.
1976 Dolan TF. Hemolytic anemia and edema as the initial signs in infants with cystic fibrosis. Clin Pediatr 1976; 15:597-600.
Much of the interest in vitamin E up to this time had been in premature infants. Three of the 5 infants with CF in this report had low vitamin E levels, all had haemolytic anaemia and marked reticulocytosis. They note that although low levels of vitamin E had been described in CF (Blanc WA et al. Pediatrics 1958; 22:494) no clinical deficiency states had been described. (Review of “The occurrence and effects of human vitamin E deficiency” by Philip Farrell J Clin Invest 1977; 60:233-241).
1977 Farrell PM, Bieri JG, Fratantoni JF, Wood RE, di Sant’Agnese PA. The occurrence and effects of human vitamin E deficiency. J Clin Invest 1977; 60:233-241. [PubMed]
A detailed review of the subject by Phillip Farrell . All 52 CF patients with pancreatic insufficiency were deficient in vitamin E. Hydrogen peroxide induced haemolysis was increased and red cell survival of 15Cr-labelled erythrocytes was significantly decreased but was corrected by vitamin E. The authors concluded that “concomitant effects consistent with mild haemolysis but not anaemia occur and may be reversed with vitamin E therapy”. Daily doses of water soluble vitamin E were recommended for people with cystic fibrosis.
In a subsequent study from Leeds the haemoglobin was significantly increased with vitamin E treatment in the children with CF with long-standing low vitamin E levels from 13.14 g/100ml to 13.47g/100ml (Kelleher J et al. Internat J Vit Nutr Res 1987; 57:253-259). No change was seen in haemoglobin with treatment in this series of Phillip Farrell’s as, although the children had low vitamin E levels, they were not anaemic – Hb14.3g/100ml.
1994 Wilfond BS, Farrell PM, Laxova A, Mischler E. Severe hemolytic anemia associated with vitamin E deficiency in infants with cystic fibrosis. Implications for neonatal screening. Clin Pediatr 1994; 33:2-7. [PubMed]
Three infants with CF and malnutrition leading to severe anemia beginning as early as six weeks of age. They had high reticulocyte counts, negative Coombs’ tests, abnormal peroxide haemolysis test results, and biochemical evidence of vitamin E deficiency. Oral administration of alpha-tocopherol resulted in rapid correction of the laboratory abnormalities.
– Phillip Farrell has published extensively on vitamin E deficiency both in premature infants and those with CF (see Farrell et al, J Clin Invest 1977; 60:233-241 above). This report emphasises the early onset of fat soluble vitamin deficiencies in infants with CF as also found in the Colorado screened infants (Sokol et al, 1991 above).
2005 Koscik RL, Lai HJ, Laxova A, Zaremba KM, Kosorok MR, Douglas JA, Rock MJ, Splaingard ML, Farrell PM. Preventing early, prolonged vitamin E deficiency: an opportunity for better cognitive outcomes via early diagnosis through neonatal screening. J Pediatr 2005; 147:S51-6.[PubMed]
The objective of this study was to evaluate cognitive function in children with CF and the influence of both early diagnosis through neonatal screening and the potential effect of early malnutrition. Significantly lower cognitive scores correlated with indicators of malnutrition and un favourable family factors such as single parents, lower socioeconomic status, and less parental education. Results suggest that prevention of prolonged malnutrition by early diagnosis and nutritional therapy, following neonatal screening, particularly minimizing the duration of vitamin E deficiency, is associated with better cognitive functioning in children with CF.
– Thus important evidence that diagnosis via newborn screening may benefit the cognitive development of children with CF, particularly in those prone to vitamin E deficiency during infancy – which is the majority. Another important positive in favour of newborn screening for CF from the Wisconsin study.
Woestenenk JW, Broos N, Stellato RK, Arets HG, van der Ent CK, Houwen RH. Vitamin E intake, α-tocopherol levels and pulmonary function in children and adolescents with cystic fibrosis. Br J Nutr. 2015 Apr 14;113(7):1096-101. doi: 10.1017/S0007114515000215. Epub 2015 Mar 12.[PubMed]
It has been suggested that higher serum α-tocopherol levels could have protective effects on pulmonary function (PF) in patients with CF. Whether current recommendations are indeed optimal for preventing deficiency and whether vitamin E has therapeutic benefits are subjects of debate. Therefore, the authors studied vitamin E intake as well as the long-term effects of vitamin E intake in the present large sample of children and adolescents with CF.
Vitamin E intake was lower than recommended, but serum α-tocopherol deficiency was rare. They found no evidence that higher serum α-tocopherol levels had protective effects on pulmonary function. Adjustment of the recommendations to the real-life intake of these patients may be considered.
VITAMIN K
1970 Torstenson OL, Humphrey GB, Edson JR, Warwick WJ. Cystic fibrosis presenting with severe hemorrhage due to vitamin K malabsorption: A report of 3 cases. Pediatrics 1970; 45:857-861. [PubMed]
Three infants with CF presented with severe bleeding secondary to vitamin K deficiency at one, three and four months of age . The authors mention that Shwachman had observed CF infants with prothrombin deficiency one of whom developed a subdural bleed (Shwachman et al. Pediatrics 1960; 25:155). Also di Sant’Agnese noted vitamin K deficiency leading to occasional bleeding (di Sant’Agnese & Vidaurreta JAMA 1960; 172:2065) and later four infants aged one to four months were reported by Walters TR & Koch F. (Am J Dis Child 1972; 124:641-642).
1989 Choonara IA, Winn MJ, Park BK, Littlewood JM. Plasma vitamin K1 concentrations in cystic fibrosis. Arch Dis Child 1989; 64:732-734. [PubMed]
One of the first studies on vitamin K from the Leeds CF centre when Prof. Choonara worked there. Plasma concentrations in 37 patients mean age 10.6 years (2-23yrs) median 46ng/l and 16 controls 49ng/l. No relation found between an increase in prothrombin time and vitamin K plasma concentration.
Subsequent studies using more efficient tests showed vitamin K was deficient in many patients and possibly related to later osteoporosis (Conway et al, 2005 below). Supplements were later advised (Dougherty et al, 2010. below).
2005 Conway SP, Wolfe SP, Brownlee KG, White H, Oldroyd B, Truscott JG, Harvey JM, Shearer MJ. Vitamin K status among children with cystic fibrosis and its relationship to bone mineral density and bone turnover. Pediatrics 2005; 115:1325-1331. [PubMed]
The aim of this study was to assess vitamin K status in an unselected population of children with CF and to investigate any vitamin K effect on bone turnover and bone mineral status. One hundred and six children entered the study. Vitamin K1 deficiency was common (70%) and the authors suggested that routine supplements should be considered.
Through its role in the carboxylation of osteocalcin, vitamin K deficiency may be associated with an uncoupling of the balance between bone resorption and bone formation. However, a cause-effect relationship between vitamin K deficiency and low bone mass has not been proved.
2010 Dougherty KA, Schall JI, Stallings VA. Suboptimal vitamin K status despite supplementation in children and young adults with cystic fibrosis. Am J Clin Nutr 2010; 92:660-667. [PubMed]
For children and adolescents with cystic fibrosis and pancreatic insufficiency, the efficacy of routine vitamin K supplementation to normalize vitamin K status remains unclear. This study examined and determined predictors of vitamin K status in subjects aged 8-25 yrs with CF and pancreatic insufficiency taking various vitamin K supplements. In 97 subjects, serum 25-hydroxyvitamin D [25(OH)D], dietary intake, vitamin K supplement intake, and vitamin K status was determined on the basis of the percentage of serum undercarboxylated osteocalcin (%ucOC; sufficient: lt 20%) and plasma proteins induced by vitamin K absence-factor II (PIVKA-II; n = 60; sufficient: le 2 microg/L) were assessed. The vitamin K supplementation groups were as follows: <150 microg/d (low; multivitamins or no supplement), 150-999 microg/d (middle; CF-specific vitamins), and >1000 microg/d (high; mephyton). %ucOC values were compared with 140 healthy subjects aged 6-21 y. RESULTS: In subjects with CF, the median (range) %ucOC was 35% (3%, 76%) and the median (range) for PIVKA-II was 2 (0, 42) micro g/L. Subjects with CF had a higher %ucOC with low [45% (10%, 76%)] and medium [41% (3%, 66%)] supplement intakes but not with a high supplement intake [16% (4%, 72%)] compared with healthy subjects [23% (0%, 43%); both P lt 0. 05]. Supplementation group for males and females and 25(OH)D and age for males were significant predictors of vitamin K status. CONCLUSIONS: Vitamin K status was often suboptimal despite routine supplementation. Only subjects taking high-dose vitamin K achieved a status similar to healthy subjects, and only the vitamin K supplementation dose predicted vitamin K status for males and females. These data suggest that higher doses of vitamin K are required.
It seems clear that vitamin K should be supplemented and this study suggests that high doses are required of > 1000 microg/d to achieve normal levels.
2013 Jagannath VA. Fedorowicz Z. Thaker V. Chang AB. Vitamin K supplementation for cystic fibrosis.[Update of Cochrane Database Syst Rev. 2011;(1):CD008482; PMID: 21249710]
Cochrane Database of Systematic Reviews. 4:CD008482, 2013. [PubMed]
To assess the effects of vitamin K supplementation in people with cystic fibrosis and to determine the optimal dose and route of administration of vitamin K for both routine and therapeutic use. Two trials (total of 32 participants) were included in the review and were assessed as having a moderate risk of bias.
Evidence from randomised controlled trials on the benefits of routine vitamin K supplementation for people with CF is currently weak and limited to two small trials of short duration. However, no harm was found and until further evidence is available, the present recommendations of 1 mg daily should be adhered to.
2015 Krzyżanowska P, Pogorzelski A, Skorupa W, Moczko J, Grebowiec P, Walkowiak J. Exogenous and endogenous determinants of vitamin K status in cystic fibrosis. Sci Rep. 2015 Jul 10;5:12000. doi: 10.1038/srep12000. Free PMC article [PubMed]
Cystic fibrosis (CF) patients are at high risk for vitamin K deficiency. The effects of vitamin K supplementation are very ambiguous. Therefore, the authors aimed to define the determinants of vitamin K deficiency in a large cohort of supplemented – 146 (86.9%) and non-supplemented – 22 (13.1%) CF patients. Vitamin K status was assessed using prothrombin inducted by vitamin K absence (PIVKA-II) and undercarboxylated osteocalcin (u-OC). The pathological PIVKA-II concentration (≥ 2 ng/ml) and abnormal percentage of osteocalcin (≥ 20%) were found in 72 (42.8%) and 60 (35.7%) subjects, respectively. Liver involvement, diabetes, and glucocorticoid therapy were potential risk factors for vitamin K deficiency. Pathological concentrations of PIVKA-II occurred more frequently in patients with pancreatic insufficiency and those who have two severe mutations in both alleles of the CFTR gene. Pathological percentage of u-OC was found more frequently in adult CF patients and those not receiving vitamin K. However, it seems that there are no good predictive factors of vitamin K deficiency in CF patients in everyday clinical care.
Early vitamin K supplementation in CF patients seems to be warranted. It is impossible to clearly determine the supplementation dose. Therefore, constant monitoring of vitamin K status seems to be justified.
– It seems clear that there is a variable need for extra vitamin K in people with CF to avoid depletion and the recommendation of these authors seems to be sound advice.
E Nauwynck, J Vanbesien, J De Schepper, I Gies, A Van Leynseele, E De Wachter, B Hauser, W Staels. Everything in excess is opposed to nature, even vitamin D: a case report. Endocrinol Diabetes Metab Case Rep 2022 Feb 1;2022:21-0181.doi: 10.1530/EDM-21-0181.Online ahead of print. Free PMC article [Pubmed]
Summary: Vitamin D intoxication in children is rare but its incidence is increasing as vitamin D is supplemented more often and in higher doses. Children with cystic fibrosis (CF) are at risk for vitamin D intoxication due to incorrect compounded preparations of liposoluble vitamins. Here, we report a severe vitamin D intoxication in a 4-year-old girl with CF, due to an error in the compounded vitamin A, D, E, and K preparation, presenting clinically with weight loss, constipation, polydipsia, polyuria, and nycturia. The administered compounded preparation contained 10 000-fold the prescribed vititsiamin D dose. The patient was treated with hyperhydration, loop diuretics, and bisphosphonates. Serum calcium levels normalized after 4 days but serum 25-hydroxyvitamin D levels remained elevated even up to 2 months after treatment.
Learning points: Vitamin D intoxication should be ruled out when patients with cystic fibrosis (CF) present with acute polyuria, constipation, and weight loss. Prompt treatment is necessary to avert life-threatening complications. Regularly measuring serum calcium and 25-hydroxyvitamin D concentrations in children with CF receiving vitamin A, D, E, and K supplements is important during their follow-up.
Dr E Nauwynck is in the Division of Pediatric Endocrinolgy, KidZ Health Castle, UZ Brussel Vrije Universitiet, Brussels Belgium
