2001
Aitken ML, Moss RB, Waltz DA, Dovey ME, Tonelli MR. McNamara SC, Gibson RL, Ramsey BW, Carter BJ, Reynolds TC. A phase I study of aerosolized administration of tgAAVCF to cystic fibrosis subjects with mild lung disease. Human Gene Therapy 2001; 12:1907-1916. [PubMed]

Fig. 1 Moira L Aitken Md.com
A Phase I, single administration, dose escalation trial was designed and executed to assess safety and delivery of tgAAVCF, an adeno-associated virus vector encoding the human CFTR cDNA, by nebulisation to the lungs of CF subjects. Sequential bronchoscopies were performed to gather analytical samples throughout the study. All 12 subjects completed the study. A clear dose-response relationship was observed in vector gene transfer.
This study confirmed aerosolized tgAAVCF is safe and widely delivered to the proximal airways of CF subjects by nebulisation.
Later a large trial (Moss et al, 2007 below) confirmed safety and delivery but had no significant clinical effect.
Dr Moira L Aitken (fig.1) is a pulmonologist in the Department of Medicine and Pediatrics, University of Washington, Seattle,
Burns JL, Gibson RL, McNamara S, Yim D, Emerson J, Rosenfeld M, Hiatt P, McCoy K, Castile R, Smith AL, Ramsey BW. Longitudinal assessment of Pseudomonas aeruginosa in young children with cystic fibrosis. J Infect Dis 2001; 183:444-452. [PubMed]

Fig 1a. Jane Burns
This study investigated genotypic and phenotypic changes in P. aeruginosa from oropharynx (OP) and bronchoalveolar lavage fluid (BALF) in a cohort of 40 children with CF during their first 3 years. A high degree of genotypic variability was identified, and each patient had unique genotypes. Early isolates had a phenotype distinct from those of usual CF isolates: generally they were non-mucoid and antibiotic susceptible. Genotype and phenotype correlated between OP and BALF isolates. As determined by culture, 72.5% of patients demonstrated P. aeruginosa during their first 3 years. On the basis of combined culture and serologic results, 97.5% of patients had evidence of infection by age 3 years, which suggests that P. aeruginosa infection occurs early in CF and may be intermittent or undetectable by culture.
– This very high incidence of P. aeruginosa is quite atypical of UK experience. We do not believe that so many young children are chronically infected (Lee et al, 2004 below; Lebecque P et al. below [PubMed]) this is based on numerous serial throat cultures, cough swabs and Pseudomonas antibody levels estimated over years which correlate closely with the degree of respiratory infection (Brett et al, 1986 above). It seems that the longitudinal careful observation of a group of patients often yields important additional information not apparent in even the most sophisticated controlled trials or cross sectional studies.
Dr Jane Burns (fig. 1a) is one of N. America’s leading CF microbiologists. Her basic research focuses on the natural history of CF airway infections including the pathogenesis of chronic infection and bacterial antibiotic resistance. Dr. Burns is closely involved with the CF Foundation-funded Therapeutics Development Network (TDN) of clinical trials in CF. She serves as the director of the TDN Core Microbiology Laboratory that performs thousands of cultures of CF specimens from clinical trials in the US each year.
Cohen RG, Starnes VA. Living donor lung transplantation. World J Surg 2001; 25: 244-250.[PubMed]
Fig 2. Vaughn Starnes. Health News Today
Since 1993 a total of 101 living-donor bilateral lung transplants had been performed with acceptable results. Though most recipients were patients with CF who were rapidly deteriorating, the indications for live-donor lung transplantation had been expanded to include some CF patients in a more elective setting, as well as select patients with other end-stage pulmonary diseases. One-year Kaplan-Meier recipient survival is 72%. Seventy-six percent of deaths occur within the first 2 months after transplantation. There has been no donor mortality and 83% had no problems.
This is a remarkable series which does not appear to have been replicated anywhere else, although there are further publications on the subject from Starnes group reporting further experience (Backhus LM. et al. J Heart Lung Transpl 2005; 24:2086-90. [PubMed]). Eighty-seven transplants were performed on 84 adult recipients from 1993 through 2003 – 76 had cystic fibrosis.
Vaughn Starnes (fig. 2) had been publishing on the subject of living donor lung transplants since 1996. The technique has not become popular in the UK. He is chair of the Department of Surgery, Surgeon-in-Chief at USC Norris Cancer and Keck Hospital of USC, and the H. Russell Smith Foundation Chair for Cardiovascular Thoracic Research at the Keck School of Medicine of USC. He is also founding executive director of USC’s Cardiac and Vascular Institute and chief of cardiothoracic surgery at Children’s Hospital Los Angeles
Cornacchia M, Zenorini A, Perobelli S, Zanolla L, Mastella G, Braggion C. Prevalence of urinary incontinence in women with cystic fibrosis. BJU Internat 2001; 88: 44-48. [PubMed]
Of 176 women with CF, 41% were never incontinent, 35% were occasionally incontinent of urine but 24% of women were regularly incontinent. As urine loss is likely to be an under-reported problem, particularly in a CF clinic devoted to mainly chest problems, the authors suggest that women with CF should be asked directly about urinary incontinence as part of their routine follow-up. Pelvic floor muscle exercises were said to help.Also there was a similar report from Manchester Adult CF clinic (Orr A et al. BMJ 2001; 322:1521.[PubMed]).
– These are really useful reports which would improve the recognition of a distressing and relatively common symptom in women with CF which may go unreported and cause considerable distress for many years.
Duszyk M, MacVinish L, Cuthbert AW. Phenanthrolines – a new class of CFTR chloride channel openers. Brit J Pharmacol 2001; 134:853-864. [PubMed]

Fig 3. Alan Cuthbert
Professor Alan Cuthbert (fig. 3) and his colleagues in Cambridge UK examined a number of phenanthrolines and benzoquinolines for their ability to activate epithelial chloride secretion in mouse colon epithelium. Their experiments showed that the phenanthrolines and benzoquinolines they described, with dual actions affecting CFTR and basolateral K(+) channels, may constitute useful lead compounds for adjunct therapy in CF.
Subsequent related publications from this group:-
Murthy M, Pedemonte N, MacVinish L, Galietta L, Cuthbert A, 4-Chlorobenzo[F]isoquinoline (CBIQ), a novel activator of CFTR and DeltaF508 CFTR. Eur J Pharmacol 2005; 516:118-124. [PubMed]
4-Chlorobenzo[F]isoquinoline (CBIQ) is a novel compound, in this study shown to activate both CFTR Cl- ion channels and KCNN4, intermediate conductance, calcium-sensitive K+-channels, present in transporting epithelia by the use of heterologous expression systems. However, this study also shows that CBIQ can activate DeltaF508 CFTR. This property is not shared with the other benzoquinolines. As activation of CFTR and KCNN4 work in unison to promote epithelial chloride secretion, CBIQ is a new chemical scaffold for developing agents that may be useful in cystic fibrosis.
Professor Alan Cuthbert FRS (1932-2016) (fig.3) was the Emeritus Shield Professor of Pharmacology, University of Cambridge. He had a long-standing interest in ion channels and receptors, particularly those found in epithelia, especially the epithelial sodium channel, ENaC and a variety of epithelial chloride channels. For many years he has made major contributions to CF research and when he retired he fortunately continued his research in this area of CF treatment (see also Williamson 1991 above). Alan was an important member of our UK CF Trust’s Research and Medcial Advisory Committee during my (Jim Littlewood) years as chairman of that committee. He was a very pleasant person and a source of great wisdom, advice and good humour.
Also publications in the same area –
Stratford FL, Pereira MM, Becq F, McPherson MA, Dormer RL. Benzo(c) quinolizinium drugs inhibit degradation of Delta F508-CFTR cytoplasmic domain. Biochemical & Biophysical Research Communications 2003; 300(2):524-530). : [PubMed]
Clancy JP, Bebök Z, Ruiz F, King C, Jones J, Walker L, Greer H, Hong J, Wing L, Macaluso M, Lyrene R, Sorscher EJ, Bedwell DM. Evidence that systemic gentamicin suppresses premature stop mutations in patients with cystic fibrosis. Am J Resp Crit Care 2001; 163:1683-1692.[PubMed]

Fig 4. John Clancy
Five patients with CF with stop mutations and five CF control subjects were treated with parenteral gentamicin for 1 wk, and underwent repeated in vivo measures of CFTR function (nasal potential difference [PD] measurements and sweat chloride [Cl(-)] testing).
Results suggest that gentamicin treatment can suppress premature stop mutations in airway cells from patients with CF, and produce small increases in CFTR Cl(-) conductance (as measured by the nasal PD) in vivo.
Dr John Clancy (fig. 4) has served in a variety of leadership roles at University of Alabama Cincinnati Children’s and within the international CF community including CF Foundation and NIH and European CF Society. He has published on a wide variety of scientific and clinical topics relating to cystic fibrosis – his main areas of interest being cystic fibrosis, airway cell biology and CFTR regulation.
Cunningham S, Prasad A, Collyer L, Carr S, Lynn IB, Wallis C. Bronchoconstriction following nebulised colistin in cystic fibrosis. Arch Dis Child 2001; 84:432-433. [PubMed]

Fig. 4a Colin Wallis author’s photo
Nebulised colistin significantly reduced FEV(1), MEF(25%), and SaO(2) for 15 minutes. In 20 children the reduction was greater than 10% from baseline FEV(1), and was still at that level in five at 30 minutes.
– By this time colistin was the most widely used inhaled antibiotic in the UK both for early eradication of P. aeruginosa and for chronic suppressive therapy. Pre-treatment assessment was recommended and was the usual practise in most CF centres.
Dr Colin Wallis (fig 4a), was originally from S.Africa where I first met him,. He became one of the leading UK paediatricians at Great Ormond Street, London caring for children with CF and respiratory disorders.
Doull IJ, Ryley HC, Weller P, Goodchild MC. Cystic fibrosis-related deaths in infancy and the effect of newborn screening. Pediatr Pulmonol 2001; 31:363-366, 2001 [PubMed]

Fig. 4b Iolo Doull Author’s photo
Between 1985-1989 infants, born in Wales and the West Midlands were randomized to newborn CF screening by heel-prick immunoreactive trypsin (IRT) measurement or diagnosis by clinical presentation. Eligible children with CF who died in the first 5 years of life were identified from the local pediatricians and from the National UK CF Survey. In all, 230,076 infants were randomized to be screened, while 234,510 were unscreened. One hundred seventy-six CF children were identified, of whom 7 died in the first 5 years of life, 3 having presented with meconium ileus. Median age of diagnosis in the screened group was 8 weeks. On an intention to treat analysis, all 4 non meconium ileus-related deaths occurred in the unscreened group (Fisher’s exact test, P < 0.05). However, the clinical presentation of 2 of these infants led to them being diagnosed prior to 8 weeks, i.e., earlier than would have been likely by screening. In conclusion, newborn screening has the potential to decrease infant CF deaths, but if it is to be successful, identification and treatment must occur as soon as possible after birth.
This is the last report of data from the Wales West Midlands neonatal CF screening study funded by the CF Trust during the Eighties. The lessons from this study were that neonatal screening is of no advantage if the diagnosis of the infants is delayed and also if they do not also receive CF centre care once diagnosed.
Dr Iolo Doull (Fig 4b) was the senior Consultant Respiratory paediatrician in Cardiff responsible for the CF Centre service there and developing a regional service. Iolo is the Medical Director at Welsh Health Specialised Services Committee. He was the first specialist respiratory paediatrician appointed in Wales and he established a specialist paediatric respiratory service for South and Mid Wales at the Children’s Hospital for Wales, including a paediatric cystic fibrosis centre, a specialist severe asthma service, a flexible bronchoscopy service and a sleep and long-term ventilation service. He was with me in Leeds as an SHO early in his career.
Dormer RL, McNeilly CM, Morris MR, Pereira MM, Doull IJ, Becq F, Mettey Y, Vierfond JM, McPherson MA. Localisation of wild-type and DeltaF508-CFTR in nasal epithelial cells. Euro J Physiol 2001; 443 (Suppl 1):S117-120. [PubMed]
Fig 5. Bob Dormer and Maggie MacPherson
Work from experienced CF husband and wife researchers in Cardiff, Bob Dormer and Maggie McPherson (fig. 5).
Surface nasal epithelial cells from three control and three CF individuals were obtained from nasal brushings. Wild-type CFTR was localised predominantly apically, whereas DeltaF508-CFTR was located mainly inside the cell in a region close to the nucleus. Incubation of cells with MPB-07 (250 microM) at 37 degrees C for two hours resulted in pronounced movement of DeltaF508-CFTR to the cell periphery, but did not change the localisation of wild-type CFTR (Becq et al, 1999).
These results confirmed that DeltaF508-CFTR is mislocalised in native nasal epithelial cells and that its distribution is altered in response to the new CFTR activator, MPB-07. It was suggested that the findings should lead to development of a rational drug treatment for CF patients carrying the DF508 mutation. They did later provide evidence that benzo(c)quinolizinium compounds protect a proteolytic cleavage site by direct binding to the first cytoplasmic domain of Delta F508-CFTR and this is a likely mechanism for increasing Delta F508-CFTR trafficking in intact cells (Stratford FL et al. Biophys Res Commun 2003; 300:524-530 below).
Equi AC, Pike SE, Davies J, Bush A. Use of cough swabs in a cystic fibrosis clinic. Arch Dis Child 2001; 85:438-439. [PubMed]

Fig 6. Amanda Equi
The authors audited prospectively 322 cough swabs taken from children with CF and compared cough swabs with concomitant sputum samples in 30 expectorating patients. They found that a positive cough swab is a strong predictor of sputum culture. However, a negative cough swab does not rule out infection. Persistent symptoms should be further investigated.
A practically useful study as cough swabs are widely used to monitor respiratory pathogens in children with CF in the UK. One could add that repeatedly negative throat swabs, particularly if associated with negative antibody studies, make infection in the lower respiratory tract increasingly unlikely but not impossible.
Dr Amanda Equi (fig. 6) at the time of this study was at the Royal Brompton in London. She subsequently became lead consultant for Paediatric Respiratory Medicine for the West Herefordshire Hospitals with links to the Brompton Hospital, London and Great Ormond Street.
Farrell PM, Kosorok MR, Rock MJ, Laxova A, Zeng L, Lai HC, Hoffman G, Laessig RH, Splaingard ML. Early diagnosis of cystic fibrosis through neonatal screening prevents severe malnutrition and improves long-term growth. Pediatrics 2001; 107:1-13. [PubMed]
Follow-up of the Wisconsin screened infants showing significantly better long term growth and nutritional state in the screened group.
This particular paper was influential in the eventual recommendation for nationwide neonatal CF screening by the UK Government in May 2001 when Yvette Cooper was the Health Minister.
Background; There had been a major campaign to introduce national neonatal CF screening led by the UK CF Trust since 1996. Previously the Child Health Subgroup of the UK National Screening Committee (NSC) had considered the evidence of long term benefit was insufficient to recommend national neonatal CF screening. A previous paper from Wisconsin (Farrell et al, N Eng J Med 1997; 337:963-969 [PubMed]) was considered, by Professor NJ Wald, to provide no evidence of any benefits from screening.
Even after the UK Government’s decision, following this 2001 paper, the the Child Health Group of the National Screening Committee remained unconvinced! As recently as 2002, after the Government had agreed to neonatal CF screening in 2001, Dr David Elliman, Chair of the Child Health Subgroup of the UK National Screening Committee, wrote that the National Screening Committee (NSC) concluded that there was currently insufficient evidence of longer term benefit, specifically in relation to pulmonary function, to support implementation of newborn screening and he then adds, without any comment, “subsequently a ministerial decision was made in July 2001 to formally introduce screening in England followed shortly by a similar decision in Scotland” (Elliman DAC, et al. Arch Dis Child 2002; 87:6-9. [PubMed]). This view was still held by the NSC in 2005.

Fig 7. Health Minister Yvette Cooper, new baby and father Ed Balls Daily Mail
Fortunately this crucial 2001 report from Wisconsin resulted in the agreement of the then Health Minister Yvette Cooper (fig 7 with husband Ed Balls and her new baby) and the UK Government and was the culmination of a 7 year, vigorous and at times heated, campaign by Mrs Rosie Barnes (Director of the CF Trust) and Dr Jim Littlewood (Chair of the Research and Medical Advisory Committee the UK CF Trust).
The introduction of national neonatal CF screening was undoubtedly one of the major clinical advances, if not the major advance, of the decade in the UK. The support of Yvette Cooper MP, who had a baby herself later that year, in overruling the unreasonable opposition of the National Screening Committee was central to our success.
Fig. 8 Philip Farrell pediatrics.wisc.edu
Phillip Farrell (fig. 8) is the Professor of Pediatrics and Population Health Sciences at the University of Wisconsin School of Medicine and Public Health and responsible for the Wisconsin neonatal screening programme from 1985. He trained with Paul di Sant’Agnese at the NIH until he moved to Wisconsin in 1977. His work with CF was one influential factor in the introduction of neonatal screening in the UK between 2001 and 2007 and also throughout the United States by 2009. Among many awards over the years, in 2005, he was awarded the Paul di Sant’Agnese Distinguished Scientific Achievement Award of the US Cystic Fibrosis Foundation.
Goldman A, Labrum R, Claustres M, Desgeorges M, Guittard C, Wallace A, Ramsay M. The molecular basis of cystic fibrosis in South Africa. Clin Genet 2001; 59:37-41. [PubMed].

Fig 9. Michelle Ramsay. h3africa.org
The spectrum of CFTR mutations in three South African populations is presented. To date a total of 192 white patients (384 chromosomes) with confirmed CF have been tested. deltaF508 accounts for 76% of the CF chromosomes in this group, with 3272-26A–>G, 394delTT and G542X occurring at the following frequencies: 4, 3.6 and 1.3%, respectively. A further 11 mutations account for 6% of CF chromosomes. A total of 91% of the CF-causing mutations can now be detected in the South African white population. Haplotype analysis suggests a founder effect in South Africans of European origin for the two common CFTR mutations, 3272-26A–>G and 394delTT.
The diagnosis of CF has been confirmed in 14 coloured and 12 black CF patients. In the coloured population, both the deltaF508 and 3120 + 1G–>A mutations occur at appreciable frequencies of 43 and 29%, respectively. In the black population, the most common CF-causing mutation, the 3120 + 1G–>A mutation, occurs at an estimated frequency of 46%. Four other mutations have been detected, resulting in the identification of a total of 62.5% of mutations in this population.
Michelle Ramsay (fig. 9) is a professor in the Division of Human Genetics at the National Health Laboratory Service and University of the Witwatersrand (Wits) in Johannesburg.

Fig. 9a Charlie Howarth author’s photo
Haworth CS, Selby PL, Adams JE, Mawer EB, Horrocks AW, Webb AK. Effect of intravenous pamidronate on bone mineral density in adults with cystic fibrosis. Thorax 2001; 56:314-316. [PubMed]
The aim of this study was to assess the effect of intravenous pamidronate on BMD in these subjects. Intravenous pamidronate increases axial BMD in adults with cystic fibrosis, but the high incidence of bone pain associated with this treatment might limit its use.
Dr Charlie Howarth (Fig.9a) This study was carried out when Charlie Haworth was working with Kevin Webb at the CF Centre in Manchester. Charlie later became consultant and CF Clinic Director at the Royal Papworth Hospital in Cambridge.
Hardin DS, Ellis KJ, Dyson M, Rice J, McConnell R, Seilheimer DK. Growth hormone improves clinical status in prepubertal children with cystic fibrosis: results of a randomized controlled trial. J Pediatr 2001; 139:636-642.[PubMed]

Fig. 9a Dana Hardin. healthliine.com
Nine children with CF treated with growth hormone had significantly greater height, height velocity, weight, weight velocity and change in lean tissue mass. Also the treated group had significant improvement in forced vital capacity compared with the year before the study, and respiratory muscle strength improved. The number of hospitalizations and outpatient intravenous antibiotic courses significantly decreased in the treated group but did not change in the control group. Results of this before and after study of GH treatment in cystic fibrosis suggested that GH improves growth and clinical status.
Subsequently there was a controlled trial published by Hardin DS et al. 2006 (below). Also Schnabel D et al. 2007 (below) from Germany.
Most recently a large multi centre controlled trial was reported from the USA (Stalvey MS et al. Pediatr Pulmonol 2012; 47:252-263.[PubMed]).The authors concluded treatment with human growth hormone in prepubertal children with CF was effective in promoting growth, weight, lean body mass, lung volume and lung flows and had an acceptable safety profile. However, most centres do not use and perhaps would be unlikely to use daily injections of growth hormone to treat children with CF. In 2013 its role is still not entirely clear particularly as the nutritional state of children with CF improves with better treatment.
The most recent Cochrane Database Syst Re 2018 Dec 17;12(12):CD008901e (https://pubmed.ncbi.nlm.nih.gov/30557452/-) concluded “When compared with no treatment, rhGH therapy is effective in improving the intermediate outcomes in height, weight and lean body mass. Some measures of pulmonary function showed moderate improvement, but no consistent benefit was seen across all trials. The significant change in blood glucose levels, although not causing diabetes, emphasizes the need for careful monitoring of this adverse effect with therapy in a population predisposed to CF-related diabetes. No significant changes in quality of life, clinical status or side-effects were observed in this review due to the small number of participants. Long-term, well-designed randomised controlled trials of rhGH in individuals with CF are required prior to routine clinical use of rhGH in CF”.
Iwasa S, Fujiwara M, Nagata M, Watanabe T. Three autopsied cases of cystic fibrosis in Japan. Pathol Internat 2001; 51:467-472. [PubMed]
The incidence of CF is very low in the Japanese. All three patients initially developed meconium ileus, and hepatobiliary and pancreatic changes became more severe as age increased. None had the DeltaF508 mutation. The authors reviewed 22 Japanese autopsied cases of CF in the literature. They suggested that the high incidence of meconium ileus in Japanese CF patients may relate to a clinically severe phenotype and reflect a different genetic background between Caucasians and Japanese.
The incidence of CF in Japanese had been estimated previously at 1:350,000 considering 104 reported cases in 1997 (Yamashiro Y et al, 1997; 24:544-547. [PubMed]); also Nishimori I, Onishi S. Hereditary pancreatitis in Japan: a review of pancreatitis-associated gene mutations. Pancreatology 2001; 1:444-447. [PubMed]).
Jones AM, Govan JR, Doherty CJ, Dodd ME, Isalska BJ, Stanbridge TN, Webb AK. Spread of a multiresistant strain of Pseudomonas aeruginosa in an adult cystic fibrosis clinic. Lancet 2001; 358:557-558. [PubMed]

Fig 10. Andy Jones
A prospective surveillance study in the Manchester Adult CF centre showed 22 (14%) of 154 patients with chronic P. aeruginosa had isolates with similar and new pyocin and pulsed-field gel electrophoresis types. Cross-infection by a new multiresistant P. aeruginosa strain had therefore occurred. The authors recommended CF centres should undertake microbiological surveillance of their patients.
A subsequent report from Manchester showed that patients infected with this strain of Pseudomonas required more intensive treatment (Jones AM et al. Thorax 2002; 57:924-925. below [PubMed]).

Fig. 10a John Govan. ResearchGate.net
A landmark paper by Dr (now Professor) Andy Jones (fig. 10), consultant physician at the Manchester Adult CF Centre working with Prof. John Govan (fig.10a) of Edinburgh, that was influential in the eventual introduction of widespread microbiological surveillance of CF centres in the UK. This led to the discovery that cross infection was a common occurrence in many of the large CF centres (Scott & Pitt 2004. below). A similar clinical situation with a transmissible P. aeruginosa had been reported from the Liverpool Paediatric CF clinic in 1996 (Cheng K et al, 1996 above). These papers were influential in the introduction of a more rigorous policy of segregation according to microbiological status in most CF centres.
In May 2001 the CF Trust published the report of its Control of Infection Group “Pseudomonas aeruginosa infection in people with cystic fibrosis. Suggestions for prevention and infection control”. However, and somewhat surprisingly, some clinicians only accepted the report with some degree of reluctance for example one senior physician wrote in the Lancet- “There is a real risk of stigmatisation by sputum bacteriology, enhanced anxiety about what may be a relatively benign organism (many adults with CF remain well despite positive cultures of Pseudomonas aeruginosa for decades) and fear of attending a CF centre or any school or social event where another person with CF may be met. There are risks in doing too little but it may be worse to do too much”. (Geddes DM. Lancet 2001; 358:522-523).
Also another London paediatrician wrote – “This (segregation) means there will be loss of continuity of care as well as flexibility for the families choosing which days they come to see us”.
Another of his more outspoken and irascible paediatric colleagues from the Royal Brompton described those of us at the UK CF Trust responsible for recommending the policy of patient segregation as “an unruly bunch of zealots”!! Fortunately, only a minority of clinicians held these views!!
Kanagasundaram SA, Lane LJ, Cavalletto BP, Keneally JP, Cooper MG. Efficacy and safety of nitrous oxide in alleviating pain and anxiety during painful procedures. Arch Dis Child 2001; 84:492-495. [PubMed]
The repeated need for venous access is a major problem for a significant proportion of children with CF, in some resulting in severe needle phobia. Another simple method of improving their quality of life was to use inhaled nitrous oxide before venepuncture. The technique was already used successfully in Belfast (Mills et al. 2001 below) and subsequently elsewhere for children with CF undergoing painful procedures (Williams V et al. Paediatr Nurse; 2006:18:31-33. [PubMed]).
– This seemed an excellent form of treatment for children having distressing procedures as very occaisionally a child would become quite uncontrollable at the prospect of a yet another venepuncture. It is obviously used successfully in a number of CF centres by experienced clinicians (Mills & Redmond, 2001 below) and the method is now used in many CF Centres in the UK.
Mahenthiralingam E, Vandamme P, Campbell ME, Henry DA, Gravelle AM, Wong LT, Davidson AG, Wilcox PG, Nakielna B, Speert DP. Infection with Burkholderia cepacia complex genomovars in patients with cystic fibrosis: virulent transmissible strains of genomovar III can replace Burkholderia multivorans. Clin Infect Dis 2001; 33:1469-1475.[PubMed]

Fig 11. “Esch” Mahenthiralingam
Infection with Burkholderia cepacia complex in patients with cystic fibrosis (CF) results in highly variable clinical outcomes. The purpose of this study was to determine if there are genomovar-specific disparities in transmission and disease severity. B. cepacia complex was recovered from 62 patients with CF on > or =1 occasions (genomovar III, 46 patients; genomovar II [B. multivorans], 19 patients; genomovar IV [B. stabilis], 1 patient; genomovar V [B. vietnamiensis], 1 patient; and an unclassified B. cepacia complex strain, 1 patient). Patient-to-patient spread was observed with B. cepacia genomovar III, but not with B. multivorans. Genomovar III strains replaced B. multivorans in 6 patients. Genomovar III strains were also associated with a poor clinical course and high mortality. Infection control practices should be designed with knowledge about B. cepacia complex genomovar status; patients infected with transmissible genomovar III strains should not be cohorted with patients infected with B. multivorans and other B. cepacia genomovars.
An important paper regarding the management of people with CF who are infected with organisms in the B. cepacia complex from experts in this area.
Prof. Mahenthiralingam (fig. 11) is a leading CF microbiologist and now at Cardiff University in the UK.
Kosorok MR, Zeng L, West SE, Rock MJ, Splaingard ML, Laxova A, Green CG, Collins J, Farrell PM. Acceleration of lung disease in children with cystic fibrosis after Pseudomonas aeruginosa acquisition. Pediatr Pulmonol 2001; 32:277-287. [PubMed]

Fig. 11a Michael R Kosorok mkosarok.web.unc.edu
Pseudomonas acquisition is associated with declining pulmonary status in children with CF, and that this effect is probably gradual rather than precipitous. Because these patients were diagnosed and treated aggressively, the estimates of the effects of Pa acquisition may be conservative. The authors conclude that the Wisconsin CXR appears to be more sensitive than FEV(1)/FVC in detecting early changes in lung disease associated with CF. Further details in the abstract.
Michael R Kosorok (fig.11a) At the time of this paper he was working in Wisconsin and combined with the paediatricians. He was eventually a distinguished Professor of Biostatistics and Professor of Statistics and Operations Research at UNC Chapel Hill. His CV is very varied and impressive.
McCabe H. Riboflavin deficiency in cystic fibrosis: three case reports. J Hum Nutr Diet 2001; 14:365-370. [PubMed]
Three cases of clinical riboflavin deficiency are reported in children aged 2-10 years attending a regional Cystic Fibrosis clinic.

Fig 12. Helen McCabe
Riboflavin deficiency presented as angular stomatitis in all three patients. Patients were confirmed to be riboflavin deficient by assaying the activity of erythrocyte glutathione reductase. Patients were not on routine supplements of water-soluble vitamins before presentation and were treated with riboflavin supplements as part of a water-soluble vitamin complex. At presentation, one patient had poor nutritional status, but two patients were adequately nourished, receiving overnight gastrostomy feeds. Data on these two patients indicate an adequate dietary intake of riboflavin, suggesting a mechanism for increased requirements, inadequate absorption or utilization. Additional deficiencies of thiamin, pyridoxine and iron were also observed.
This paper reports the occurrence of a vitamin deficiency not previously reported in the cystic fibrosis population.
Helen McCabe (fig. 12) is Specialist CF Dietitian at the Great North Children’s Hospital in Newcastle upon Tyne. UK. Helen McCabe currently works as Principal Paediatric Dietitian in the department of Newcastle Nutrition at The Newcastle upon Tyne Hospitals NHS Foundation Trust. Helen does research in nutrition and dietetic related clinical issues largely within her specialist paediatric areas of Cystic Fibrosis and Respiratory , and including practice education , evidence based practice, quality and standards related issues
Mastella G, Zanolla L, Castellani C, Altieri S, Furnari M, Giglio L, Lombardo M, Miano A, Sciuto C, Pardo F, Magazzu G. Neonatal screening for cystic fibrosis: long-term clinical balance. Pancreatology 2001; 1:531-537. [PubMed]

Fig.13 Gianni Mastella
Very few studies have been performed on the long-term clinical advantages of neonatal CF screening programs and many of these have been inconclusive. This is a preliminary report of two observational cohort studies on this subject from Italy where neonatal CF screening has been pioneered in Europe since the mid-Seventies.
In the first study, CF patients born between 1973 and 1981 in North Eastern Italy were split into 4 groups according to the method of diagnosis: screening by meconium test (58 patients); meconium ileus (45 patients); symptoms and pancreatic insufficiency (PI; 75 patients), or symptoms and pancreatic sufficiency (PS; 19 patients). The patients were followed for up to 26 years by three CF centres sharing common treatment protocols. In this first study, the patients detected by newborn screening (PI) showed better survival and nutritional status compared to patients diagnosed through meconium ileus or symptomatic presentation with PI. The PS patients diagnosed by symptoms showed the best outcome as would be expected as most of them had a mild genotype.
In the second study, two cohorts of CF patients born between 1983 and 1992 were compared. Patients from one cohort (126 patients) were born in the Veneto region, where a neonatal screening program had been established based on immunoreactive trypsinogen. Patients from the other cohort (152 patients) were born in Sicily, where an intensive program of early diagnosis by symptoms was implemented. The cohorts were comparable for CF incidence, CFTR genotypes, gender proportion and common treatment protocols. In this second study, the Veneto neonatal screened cohort showed better outcome with regard to survival and nutritional status over 16 years of follow-up.
Observational cohort studies cannot give definitive evidence of the clinical benefit of neonatal CF screening; however, data have been accumulated which strongly suggest a better clinical outcome for CF patients born in an area where a screening program is performed always provided they receive good care after diagnosis. The Italians, in particular astute clinicians such as Gianni Mastella.
Prof. Gianni Mastella (fig. 13) ( – 2021) deserves the credit for having pioneered neonatal CF screening in Europe since 1973; he was awarded the Rossi Medal of the European CF Society for his work with cystic fibrosis.
Mills HL, Redmond AOB. Cystic fibrosis patients’ view of self administered nitrous oxide (Entonox) during insertion of epicutaneo-cava catheters (long lines). 24th ECFS Conference Vienna 2001. Poster 291.
The distress of some children at even the thought of an intravenous injection or insertion of a venous catheter, when they have had many such insertions before, has to be seen to be believed. It is distressing not only for the unfortunate patient and the parents but also for the unfortunate doctor and nurse inserting the needle! The use of nitrous oxide is a great idea and appears very acceptable to most people. (The method was first published by Kanagasundaram et al, 2001 above.[PubMed]) above.
McCallum SJ, Corkill J, Gallagher M, Ledson MJ, Hart CA, Walshaw MJ. Superinfection with a transmissible strain of Pseudomonas aeruginosa in adults with cystic fibrosis chronically colonised by P. aeruginosa. Lancet 2001; 358:558-560.[PubMed]
Two further examples, from the Liverpool Adult CF Centre, of a transmissible Liverpool strain of P. aeruginosa shown to be identical by genotyping, infecting patients in the same clinic. Here it was shown to have infected patients already chronically infected with another strain of Pseudomonas. The Liverpool strain (LES strain), was first recognised in the Liverpool paediatric clinic, (Cheng et al. 1996. above [PubMed]) was identified in a number of other UK CF centres in a subsequent survey carried out by Scott and Pitt (J Med Microbiol 2004; 53:609-615. below.[PubMed]).
Mulheran M, Degg C, Burr S, Morgan DW, Stableforth DE. Occurrence and risk of cochleotoxicity in cystic fibrosis patients receiving repeated high-dose aminoglycoside therapy. Antimicrob Agents Chemother 2001; 45:2502-9. [PubMed]
The primary aim of this retrospective study was to establish the incidence and severity of auditory deficit in 70 people with CF. Twelve (17%) displayed hearing loss considered to be caused by repeated exposure to aminoglycosides. There was a nonlinear relationship between the courses of aminoglycoside therapy received and the incidence of hearing loss. The severity of the loss did not appear to be related to the number of courses received. Assuming the risk of loss to be independent for each course, preliminary estimates of per course risk of hearing loss were less than 2%.
Upon comparison with previous clinical studies and experimental work, these findings suggest that the incidence of cochleotoxicity in CF patients is considerably lower than would be expected, even suggesting that the CF condition may confer some protection against aminoglycoside cochleotoxicity.
Subsequently increased susceptibility to aminoglycoside toxicity has been related to the possession of a particular gene the mitochondrial 12S rRNA A1555G mutation is one of the important causes of aminoglycoside-induced and nonsyndromic hearing loss (Qian Y, Guan MX. Antimicrobial Agents & Chemotherapy 2009; 53:4612-4618. [PubMed]; Bitner-Glindzicz Met al. Prevalence of mitochondrial 1555A->G mutation in European children. N Engl J Med 2009; 360:640-642. [PubMed]).
Dr Mike Mulheran at the time was a scientist in MRC Toxicology Unit, University of Leicester. He subsequently was in the Department of Cell Physiology and Pharmacology at the University.
Munck A, Bonacorsi S, Mariani-Kurkdjian P, Lebourgeois M, Gerardin M, Brahimi N, Navarro J, Bingen E. Genotypic characterization of Pseudomonas aeruginosa strains recovered from patients with cystic fibrosis after initial and subsequent colonization. Pediatr Pulmonol 2001; 32:288-292. [PubMed]

Fig 14. Anne Munck
After early eradication treatment of Pseudomonas aeruginosa subsequent serial isolates were characterized by means of molecular methods to determine whether they were genetically related to the initial strain. Initial colonization was eradicated in all 19 patients and 14 patients subsequently acquired a new PA strain with a distinct genotypic profile, suggesting a new source of contamination. Five patients had two PA isolates with identical genotypes, suggesting either previous undetected respiratory tract colonization or a persistent environmental source of contamination.
This was a very important, practically very useful and now oft-quoted, paper which settled the question as to whether Pseudomonas was eradicated or merely suppressed with initial eradication antibiotic therapy. It showed quite clearly that, in the majority of patients, the Pseudomonas had been eradicated rather than merely being suppressed as recurrences were of a different genotypic profile.
Dr Anne Munck (fig. 14) is a paediatrician specializing in gastroenterology, nutrition and cystic fibrosis at the University Hospital Robert Debre, Paris. She is heavily involved in cystic fibrosis care and research on a national and international basis.
Moore JE, McIlhatton B, Shaw A, Murphy PG, Elborn JS. Occurrence of Burkholderia cepacia in foods and waters: clinical implications for patients with cystic fibrosis. J Food Protect 2001; 64:1076-1078.[PubMed].

Fig. 15 John Moore LinkedIn
Two hundred forty-eight retail “ready-to-eat” foodstuffs in eight food categories and 134 waters categorized into nine types were analyzed for the presence of the Burkholderia cepacia complex of organisms. Of these, 14 of 26 (53.8%) samples of raw unpasteurized bovine milk were positive for this organism. Consumption of raw unpasteurized milk may therefore act as a potential source of infection with this organism, which is of particular concern for patients with cystic fibrosis, where colonization and infection with this organism can lead to a fatal necrotizing pneumonia and premature death. In addition to the associated risk of infection from fecal pathogens, patients with cystic fibrosis should therefore avoid the consumption of raw unpasteurized milk to minimize the risk of becoming infected with this organism.
Of considerable practical importance as unpasteurised milk is still available in some countries. Distribution of raw milk is illegal in Scotland. While it is legal in England, Wales, and Northern Ireland, the only registered producers are in England. About 200 producers sell raw, or “green top” milk direct to consumers, either at the farm, at a farmers’ market, or through a delivery service. The bottle must display the warning “this product has not been heat-treated and may contain organisms harmful to health”, and the dairy must conform to higher hygiene standards than dairies producing only pasteurised milk. As it is only legal to supply unpasteurised milk direct to consumers, it is illegal to be sold on the High Street, via shops or supermarkets. Raw milk is available in the USA but illegal in Canada.
Dr John Moore (fig. 15) is Clinical Microbiologist at the Belfast City Hospital.
Nixon GM, Armstrong DS, Carzino R, Carlin JB, Olinsky A, Robertson CF, Grimwood K. Clinical outcome after early Pseudomonas aeruginosa infection in cystic fibrosis. J Pediatr 2001; 138:699-704.[PubMed]).

Fog. 15a Gillian Nixon Monash University
A prospective, observational cohort study of 56 children from Melbourne. All were identified as having CF by newborn screening during 1990-92 and the study involved each child having an annual bronchial lavage during the first 2 to 3 years of life. Clinical outcome was determined at 7 years of age. P. aeruginosa infection was diagnosed in 24 (43%) children. Four children died before 7 years of age, all of whom had been infected with a multi-resistant, mucoid strain of P. aeruginosa (Armstrong et al, 2002 below). In the survivors, P. aeruginosa infection was associated with significantly increased morbidity as measured by lower National Institutes of Health scores, greater variability in lung function, increased time in the hospital, and higher rates of rhDNase (Pulmozyme) therapy (P <.01)
Despite neonatal CF screening, the acquisition of P. aeruginosa was common by 7 years of age in this CF birth cohort and was associated with increased morbidity and mortality. The high incidence of P. aeruginosa infection here is presumably a reflection of the fact the children were born between 1990 and 1992 when early eradication therapy was not routine practice outside certain European CF centres. The high prevalence (43%) of chronic Pseudomonas infection at 7 years contrasts with the much lower prevalence (of around 4%) at some European centres where early eradication has been the policy for some years.
This paper should be read in conjunction with the following paper (Armstrong et al, 2002 below) where the unusual situation at the time is described of a particularly virulent strain of Pseudomonas in the clinic that caused the death of the 4 children.
Dr Gillian Nixon (Fig 15a) is a is a paediatric respiratory and sleep physician with a 50% research appointment (Adjunct Associate Professor Research) and 50% clinical practice.
Quan JM, Tiddens HAWM, Sy JP, McKenzie SG, Montgomee ry MD, Robinson PJ, Wohl ME, Konstan MW. Pulmozyme Early Intervention Trial Study Group. A two-year randomised placebo controlled trial of dornase alfa in young patients with cystic fibrosis with mild lung function abnormalities. J Pediatr 2001; 139:813-820. [PubMed]

Fig 16. Mary Ellen Wohl. PubMed central
This was a 96-week, randomized, double-blind, placebo-controlled trial involving 49 CF centers and 474 children aged 6 to 10 years with good respiratory function (FVC 85% predicted). At 96 weeks the treated group had maintained their respiratory function levels with slight treatment benefit for dornase alfa compared with placebo with a 34% reduction in the risk of respiratory tract exacerbations.
The results of this trial influenced some clinicians to try young CF patients on Pulmozyme before they developed chronic infection; this became routine practice in at least one large UK Paediatric CF Centre and also in Copenhagen where the treatment was found to reduce the incidence of new positive respiratory cultures (Frederiksen B et al. Acta Paediatr 2006; 95:1070-1074. below [PubMed]).
One of the senior members of this study group, whom I was fortunate to meet, was Dr Mary Ellen Wohl (1932-2009) (figure 16) who had made major contributions to paediatric respiratory physiology and care since 1968. Many of her colleagues pay tribute to her in an obituary in The Boston Globe of Nov. 9th 2009 – “Dr. Wohl was the grand dame of pediatric pulmonary diseases,’’ Dr. James Mandell, Children’s chief executive officer, said in a statement. Her work “helped validate a number of regimens now the standard of care. As a doctor in the trenches,’’ he said, “she worked tirelessly to optimize care and outcomes for children with cystic fibrosis and, more recently, those with HIV infections, and developed several multicenter clinical trials of new treatment for those diseases.’’
Ranganathan SC, Dezateux C, Bush A, Carr SB, Castle RA, Madge S, Price J, Stroobant J, Wade A, Wallis C, Stocks J. Airway function in infants newly diagnosed with cystic fibrosis. Lancet 2001; 358:1964-5. [PubMed]

Fig 17. Sarah Ranganathan
The airway function of 33 infants with CF was significantly reduced compared with 87 healthy controls, even in those without clinically recognised previous lower respiratory illness.
Some degree of airway obstruction, increased residual volume and hyperinflation from an early age has been recognised for many years (Keats TE. Generalized pulmonary emphysema as an isolated manifestation of early cystic fibrosis of the pancreas. Radiology 1955; 65:223-226. [PubMed] above and subsequent studies). This present study confirms this fact. A follow up study was performed by Ranganathan et al. (Am J Resp Crit Care Med 2004; 169:928-933. [PubMed]) FEV 0.5 was measured soon after diagnosis (median age of 28 weeks) and 6 months later in subjects with CF and in healthy infants on two occasions 6 months apart using the raised-volume technique. The mean FEV 0.5 was significantly lower in infants with CF both shortly after diagnosis and at the second test with 72% of infants having a value less than the fifth percentile.
So the airway function is already diminished soon after diagnosis in infants with CF and does not catch up during infancy and early childhood. These findings have important implications for early interventions in CF.
Dr Sarath Ranganathan (fig. 17) from Royal Melbourne Children’s Hospital carried out this work at Great Ormond Street Hospital in London in Professor Stocks’s department. He subsequently moved to Royal Melbourne Children’s Hospital as Respiratory Paediatrician, then returned to Brighton and Sussex Medical School in the UK before eventually returning to RMCH Melbourne as Director of Respiratory Medicine.
Ratjen F, Döring G, Nikolaizik WH. Effect of inhaled tobramycin on early Pseudomonas aeruginosa colonisation in patients with cystic fibrosis. Lancet 2001; 358:983-984. [PubMed]

Fig 18. Felix Ratjen
One of the early studies (the first using tobramycin) confirming that early nebulised antibiotic treatment of airway colonisation with Pseudomonas aeruginosa could delay onset of chronic lung infection in patients with cystic fibrosis. There was successful eradication of the organism in 14 of 15 patients with cystic fibrosis who had been colonised by P. aeruginosa. Patients inhaled 80 mg tobramycin twice daily for 12 months. Eradication was confirmed by sequential respiratory cultures and serum antibody titres that were negative for P. aeruginosa. The antibiotic therapy regimen maintained pulmonary function at high levels (Further support for Littlewood et al, 1985 [PubMed] above and Valerius et al, 1991. above [PubMed]).
It is of interest, with respect to the dose of tobramycin required, that a subsequent trial showed that 80 mg of nebulised injectable tobramycin twice daily on a regular basis showed similar benefit to alternate monthly cycles of 300 mg twice daily of tobramycin for inhalation (Nikolaizik WH et al. Can Respir J 2008; 15:259-262 [PubMed]). However, this trial involved patients with chronic Pseudomonas infection.
The authors concluded “the present trial fails to provide convincing evidence for superiority of either of the two treatment regimens of inhaled tobramycin in CF patients”
Professor Felix Ratjen (fig. 18) was head of the CF Centre in Essen Germany until 2005 when he moved to the Hospital for Sick Children in Toronto as Head of Respiratory Medicine to hold the Sellers Chair for Cystic Fibrosis. He is involved in many areas of pediatric respiratory medicine but particularly in cystic fibrosis. Although a scientific researcher into areas of inflammation and respiratory function, he is heavily involved in patient care and the introduction of new treatments.
Rosenfeld M, Gibson R, McNamara S, Emerson J, McCoyd KS, Shell R, Borowitz D, Konstan MW, Retsch-Bogart G, Wilmott RW, Burns JL, Vicini P, Montgomery AB, Ramsey B. Serum and lower respiratory tract drug concentrations after tobramycin inhalation in young children with cystic fibrosis. J Pediatr 2001; 139:572-577. [PubMed]
First of two important papers from Rosenfield et al. to assess the serum and lower respiratory tract tobramycin concentrations produced by a single dose of tobramycin for inhalation (TOBI) in patients with CF aged 6 months to 6 years. A 180-mg dose of inhaled tobramycin produced a mean peak serum level of 0.5 microg/ml; a 300-mg dose produced a mean peak serum level of 0.6 microg/ml both well below the accepted maximum trough concentration with parenteral dosing (2 microg/ml). The target epithelial lining fluid level in the lung was 20 microg/ml – 10-fold greater than the minimal inhibitory concentration for most Pseudomonas isolates. The mean epithelial fluid level was 90 microg/ml.
So in patients with CF, aged 6 months to 6 years, even a single 300-mg dose of inhaled tobramycin (TOBI) was considered to produce safe serum concentrations and high drug concentrations in the bactericidal range in the lower respiratory tract. Although it is not known if these serum levels, sustained over many years, are without side effects. Also, this reviewer does not understand why such a large dose of tobramycin was used?
Rosenfeld M, Gibson RL, McNamara S, Emerson J, Burns JL, Castile R, Hiatt P, McCoy K, Wilson CB, Inglis A, Smith A, Martin TR, Ramsey BW. Early pulmonary infection, inflammation, and clinical outcomes in infants with cystic fibrosis. Pediatr Pulmonol 2001; 32:356-366. [PubMed]

Fig 19. Margaret Rosenfeld
Forty infants from 3 participating sites over a 2-year period had annual bronchoalveolar lavage (BAL) for culture and measurements of pro- and anti-inflammatory cytokines, semi-annual infant pulmonary function testing, and quarterly clinical evaluations. Both the prevalence of CF pathogens and their density in BAL fluid increased with age. Infants had neutrophilic lower airway inflammation and elevated IL-8 concentrations independent of whether CF pathogens were recovered. Total leukocyte and neutrophil densities and IL-8 concentrations increased with density of CF pathogens in BAL fluid, whether the isolated organism was P. aeruginosa or another pathogen. IL-10 concentrations were similar in CF subjects and non-CF historical controls. Infants generally had suboptimal growth (low weight and height percentiles) and obstructive lung disease (decreased expiratory flows and air trapping). Subjects from whom CF pathogens were isolated at > 105 cfu/ml had the worst air trapping and lowest Brasfield chest X-ray scores. The authors considered that their findings would provide a foundation for future studies of early intervention in CF lung disease, including antimicrobial and anti-inflammatory therapy.
It must be observed that in these infants, who were recruited from the CF care centres at each of 3 participating sites, there was an alarming frequency of isolation of pathogens from the lower airways. Unfortunately, antibiotic prescribing practices were not specified although the values were said merely not to correlate with antibiotic use. Obviously the presence of S. aureus in cultures would be related to whether prophylactic anti-staphyloccocal antibiotics were used and whether a policy of early eradication of Pseudomonas was practised.
With regard to these patients, by the age of 3 years, no less than 21% of the children had >105 cfu/ml of P. aeruginosa, and 39% of any pathogen. The authors considered that carefully conducted randomized controlled trials in very young patients with CF would help to establish the risk-benefit ratio of therapeutic interventions in this important and vulnerable population.
This ultra cautious attitude shows a radically different approach to that recommended in the UK and many European centres where neonatal screening had been routine for many years and early interventions are the rule e.g. long term flucloxacillin from diagnosis, amoxycillin with all “colds” even if no positive culture and also for any positive airway cultures, and early eradication therapy for positive P. aeruginosa cultures whether there are symptoms or not etc, etc. (These policies are detailed in the CF Trust consensus documents e,g, Antibiotic Treatment for Cystic Fibrosis. UK CF Trust, 2009). This difference in approach is reflected in the much higher chronic infection rates in young children in the US than in some UK and many European CF centres.
Dr Rosenfeld (fig. 19) is Medical Director of the Clinical Pediatric Research Center and also Medical Director of the Pulmonary Function Laboratory at the Seattle Children’s Hospital where she is attending physician.
Strandvik B, Gronowitz E, Enlund F, Martinsson T, Wahlstrom J. Essential fatty acid deficiency in relation to genotype in patients with cystic fibrosis. J Pediatr 2001; 139:650-655.[PubMed]

Fig 20. Birgitta Strandvik
Serum concentrations of linoleic acid and docosahexaenoic acid were significantly lower in patients with severe cystic fibrosis transmembrane conductance regulator mutations, such as DF508, suggesting an association between the basic defect and abnormal essential fatty acid metabolism in CF patients. A relationship between these fatty acids and the basic defect had been suggested previously – most recently by Freeman et al, (1999 above).
Professor Birgitta Strandvik, MD, PhD, (figure 20) is Professor Emeritus of Pediatrics at Goteborg University, Sweden. She has published more than 250 scientific papers and book chapters and made major contributions to the scientific and clinical aspects of both cystic fibrosis and paediatric gastroenterology. She has a particular interest in essential fatty acids but has always been obviously greatly concerned in the practical care of patients with cystic fibrosis. Birgitta was still involved in a study output of scientific articles on nutrition and essential fatty acids in 2023.
In 2014 Birgitta received a special Award from the European CF Sociaty for her work with cystic fibrosis.
Suri R, Metcalfe C, Lees B, Grieve R, Flather M, Normand C, Thompson S, Bush A, Wallis C. Comparison of hypertonic saline and alternate day or daily recombinant human deoxyribonuclease in children with cystic fibrosis: a randomised trial. Lancet 2001; 358:1316-1321. [PubMed]

Fig 20a Ranjan Suri NetDoctor
In an open cross-over trial, 48 children were allocated in random order to 12 weeks of once-daily rhDNase (2.5 mg), alternate-day rhDNase (2.5 mg), and twice-daily 5 ml 7% hypertonic saline. The primary outcome was FEV1.
The mean FEV1 increased by 16% (SD 25%) with daily rhDNase, by 14% (22%) with alternate-day rhDNase, and by 3% (21%) with hypertonic saline. There was no significant difference between daily and alternate-day rhDNase. However, daily rhDNase showed a significantly greater increase in FEV1 than hypertonic saline (8% {2 to 14}, p=0.01).
It is no surprise that hypertonic saline, delivered by jet nebuliser, was not as effective as daily rhDNase, although there was variation in individual response. Interestingly there was no evidence of a difference between daily and alternate-day rhDNase. Although inhaled hypertonic saline was less effective as a mucolytic than rhDNase, it was considerably cheaper. It must be stressed that these are group responses and there is considerable individual variation between patients and it is important that clinicians assess the individual response of each patient when prescribing these treatments. Also, it was later shown that failure to respond to rhDNase may be related to the magnesium status of the patient (Sanders NN et al, Thorax 2006; 61:962-968. [PubMed]).
Dr Ranjan Suri (Fig 20a) is a Paediatric Respiratory Consultant at Great Ormond Street Hospital, London.
Sood N, Paradowski LJ, Yankaskas JR. Outcomes of intensive care unit care in adults with cystic fibrosis. Am J Resp Crit Care 2001; 163:335-338. [PubMed]

Fig 21. James Yankaskas
Mechanical ventilation had been discouraged in CF because of poor outcomes, but improved survival and the availability of lung transplantation have increased the indications for care of CF patients in the intensive care unit (ICU).
The authors studied the outcomes of all CF patients admitted to the University of North Carolina Hospitals Medical ICU from January 1990 through December 1998. Seventy-six patients, ranging in ages from 17 to 45 yr (mean: 27 yr), and of whom 53% were female, had 136 admissions for exacerbations of CF with respiratory failure (RF, n = 65), haemoptysis (n = 33), antibiotic desensitization (n = 30), pneumothorax (n = 3), or other reasons (n = 5). Eighty-six percent of the patients with haemoptysis and all of those with desensitization and pneumothorax were alive 1 yr after ICU discharge. Of the 42 patients with RF, 37 (88%) required assisted ventilation. Twenty-three (55%) of the patients with RF survived to ICU discharge and 19 (45%) died. Seventeen (40%) of the patients with RF received lung transplants and 14 were alive 1 yr later. Without transplantation, three (7%) of the patients with RF were alive and three (7%) were dead 1 yr later. Sex, body mass index, and respiratory bacteria did not correlate with survival. We conclude that ICU care for adults with CF who have reversible complications is appropriate and effective. Ventilatory support is appropriate for some transplant candidates.
This is an indication of the fate of people with CF admitted to an ICU in a major CF Centre at the present time. Undoubtedly the policy of not admitting to an ICU or ventilating people with CF is no longer valid.
Dr James Yankaskas (fig. 21) is Professor of Medicine in the Department of Pulmonary Diseases and Critical Care Medicine, Department of Medicine, University of North Carolina. His research interests include the physiology of human airway epithelia, cystic fibrosis in adults and the use of systems based quality improvement methods to improve care delivery and outcomes in adult CF, pulmonary clinic and medical ICUs.
Saiman L, Chen Y, Tabibi S, San Gabriel P, Zhou J, Liu Z, Lai L, Whittier S. Identification and antimicrobial susceptibility of Alcaligenes xylosoxidans isolated from patients with cystic fibrosis. J Clin Microbiol 2001; 39:3942-5. [PubMed]

Fig. 21a Lisa Saiman paediatrics.columbia.edu
A total of 106 strains from 78 patients from 49 CF centers in 22 states were studied. Most (89%) were correctly identified by the referring laboratories as Alcaligenes xylosoxidans. However, 12 (11%) strains were misidentified; these were found to be P. aeruginosa (n = 10), Stenotrophomonas maltophilia (n = 1), and Burkholderia cepacia (n = 1). Minocycline, imipenem, meropenem, piperacillin, and piperacillin-tazobactam were the most active since 51, 59, 51, 50, and 55% of strains, respectively, were inhibited. High concentrations of colistin (100 and 200 microg/ml) inhibited 92% of strains. Chloramphenicol paired with minocycline and ciprofloxacin paired with either imipenem or meropenem were the most active combinations and inhibited 40 and 32%, respectively, of strains. Selective media and biochemical identification proved to be useful strategies for distinguishing A. xylosoxidans from other CF pathogens. Standards for processing CF specimens should be developed, and the optimal method for antimicrobial susceptibility testing of A. xylosoxidans should be determined
One of an increasing number of relatively new pathogens isolated from people with CF.
Lisa Saiman (fig.21a) is Professor of Pediatrics at Columbia University Medical Centre. Her primary research and clinical interests are hospital epidemiology and healthcare-associated infections across the spectrum of healthcare, ranging from the neonatal ICU to cystic fibrosis to pediatric long-term care with a particular focus on respiratory viruses.
Saglani S, Bush A. Cystic fibrosis and Down’s syndrome: not always a poor prognosis. Pediatr Pulmonol 2001; 31:321-322. [PubMed]

Fig 21b Segal Saglani Imperial College News
A child developed a bronchiolitis-like illness and was found to have mosaic Down’s syndrome (diagnosed on karyotype) and also cystic fibrosis, diagnosed on the basis of a high sweat osmolality (247 mosmoles/kg sweat; normal, 62-137) and a homozygous delta F508 genotype. Despite two potentially life-threatening conditions, the child is doing well at the age of 7 years, despite being pancreatic insufficient.
Dr Sejal Saglani was at the time at the Royal Brompton Hospital. Eventually she was a Professor at the National Heart and Lung Institute, London. In 2023 she was appointed Director of the Centre for Paediatrics Imperial College London,
Standards for the Clinical Care of Children and Adults with Cystic Fibrosis in the UK. The CF Trust Clinical Standards and Accreditation Group. London. Cystic Fibrosis Trust, May 2001.
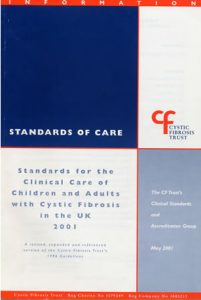
Fig 22. CF Trust’s Standards of Care
This document (figure 22) was influential in improving care both in the UK and Europe. The principles were similar to those subsequently incorporated in to the ECFS standards of care document in 2005 (Kerem et al. J Cyst Fibros 2005; 4:7-26. below). As a basis for this 2001 Standards we used the report of a Working Group of the CF Trust, the British Paediaitric Association and the British Thoracic Societychaired by Dr Tony Jackson, the then Chair of the CF Trust’s Research and Medical Advisory Committee (J Roy Coll Phys Lond 1996; 30:305-308). The report of the 2001 Working Group, chaired by Jim Littlewood, was still widely used until it was replaced by an extensively revised 2nd edition in 2011 chaired by Dr Ian Balfour-Lynn and Dr. Sue Madge.
The full text of 2nd edition 2011 is available on the CF Trust website (www.cystic fibrosis.org.uk).
It is hard to believe that now (in 2023) it is over 20 years since we first wrote and published the 2001 CF Trust Standards of Care document. The many meetings to agree the various recommendations in the first document were frequent, long, hard work and often heated but the advice has stood the test of time over the decade until the second extensively revised and excellent 2nd edition was published in 2011.
Visca P, Cazzola G, Petrucca A, Braggion C. Travel-associated Burkholderia pseudomallei infection (Melioidosis) in a patient with cystic fibrosis: a case report. Clin Infect Dis 2001; 32:E15-6.[PubMed]
In September 1997, a 25-year-old Italian lady with CF spent 3 weeks in Thailand. In August 1998, her pulmonary function rapidly declined, with productive cough and intermittent fever. The chest x-ray films revealed diffuse, small, patchy opacities in the upper lobes. Burkholderia pseudomallei (BP) were isolated from specimens of the patient’s sputum and were identified by means of 16S rDNA sequencing. The diagnosis of melioidosis was serologically confirmed. Continuous therapy with ceftazidime and co-trimoxazole and maintenance with co-trimoxazole, doxycycline, and chloramphenicol resulted in eradication of Burkholderia pseudomallei.
This infection appears to be a particular risk for the increasing number of adults with CF travelling aboard to places such as Thailand as they seem to be prone to melioidosis. Subsequently further cases were reported. Burkholderia pseudomallei is an important cause of pneumonia and septicaemia in Thailand particularly in the rainy season when it may contaminate the water supply. There are now almost 70 cases of the infection causing serious illness reported in people with cystic fibrosis. So going on holiday to Thailand represents a definite risk for a person with CF particularly in the rainy season. B. pseudomallei infection has also been reported affecting a person with CF in Brazil (Barth AL et al, 2007. [PubMed] below).
Wojtczak HA, Kerby GS, Wagener JS, Copenhaver SC, Gotlin RW, Riches DW, Accurso FJ. Beclomethasone diproprionate reduced airway inflammation without adrenal suppression in young children with cystic fibrosis: a pilot study. Pediatr Pulmonol 2001; 32:293-302.[PubMed]

Fig 22a Henry Wojtczak
LinkedIn
There are few studies evaluating the safety of inhaled steroids in young children. The authors prospectively administered beclomethasone diproprionate (BDP) 420 mcg daily for 2 months to 12 clinically stable young children with CF without affect on urine and blood cortisol levels, adrenal reserve, or increase in airway infection. Also there was a fall in bronchoalveolar lavage fluid inflammatory markers following the inhaled steroid treatment.
This was one of a number of small short term studies of inhaled corticosteroids in people with cystic fibrosis. Clinical experience shows that a few patients quite obviously do benefit significantly from inhaled steroids particularly young patients with troublesome wheezing and bronchial lability. However, a subsequent UK study of withdrawal of inhaled steroids from people with CF showed many patients were deriving no apparent benefit and their inhaled steroids could be withdrawn without ill effects (Balfour-Lynn et al. 2006 [PubMed]below). Presumably some of these patients would have derived some benefit at the time the steroids were started. However, there are a few children with CF who definitely appear to derive great benefit from inhaled steroids (That is also this reviewer’s experience). However, it important to note that these patients were not included in Balfour-Lynn’s steroid withdrawal study as, understandably, their doctors (and almost certainly their parents!) were unwilling to stop their steroid treatment.
Also, although some paediatricians who published short term studies on inhaled steroids found it difficult to accept, undoubtedly in some children the rate of growth is affected by taking inhaled steroids in the doses used in this present study and this will be detected provided the children are followed up for longer and measured carefully (by no means always the case in busy general paediatric clinics!). Obviously two months is an inadequate time to identify adverse effects on growth (see Littlewood et al, 1988 [PubMed] above for full discussion of the adverse effect of inhaled steroids on growth).
Henry Wojtczak (Fig. 22a) is at the Division of Pulmonary Medicine, Department of Pediatrics, Naval Medical Center, San Diego, California, USA.
Ziebach R, Pietsch-Breitfeld B, Bichler M, Busch A, Riethmuller J, Stern M. Bronchodilatory effects of salbutamol, ipratropium bromide, and their combination: double-blind, placebo-controlled crossover study in cystic fibrosis. Pediatr Pulmonol 2001; 31: 431-435. [PubMed]

Fig. 23 Rita Ziebach Kinderarztpraxis-Ziebach-
Salbutamol alone or in combination with ipratropium bromide was superior to ipratropium alone. The authors concluded that bronchodilator therapy with a sympathomimetic agent alone is usually sufficient and only where there was proven additional benefit from inhalation by anticholinergic drugs should combination therapy be recommended.
A useful practical study which confirms the experience of most clinicians that most patients don’t need ipratropium bromide adding to their salbutamol, but also that salbutamol is often helpful. A later Leeds study showed 15 of 83 patients (18%) showed significant Reversibility with nebulised salbutamol at their annual assessment (Hughes T et al, J Cyst Fibros 2006; 5 (Suppl1):S44).
Dr Rita Ziebach (Fig. 23) is the University Children’s. Hospital Tübingen, Department 1, Tübingen, Germany.


