History – 2019 A to J
THE FIRST ABSTRACTS ARE REVIEWS OF VARIOUS ASPECTS OF PROGRESS IN 2019
Adrienne P Savant, Susanna A McColley. Cystic fibrosis year in review 2019: Section 1 CFTR modulators. Pediatr Pulmonol 2020 Dec;55(12):3236-3242.doi: 10.1002/ppul.25039.Epub 2020 Sep 1. Free access. [PubMed]

Fig. 1 Adrienne Savant
During the year 2019, research and case reports/series in the field of cystic fibrosis (CF) were in abundance. To adequately address the large body of CF research published during 2019, the CF year in review will be divided into three sections. This report is the first section, focusing specifically on new research related to cystic fibrosis transmembrane conductance regulator modulator therapy. Additional sections will concentrate on pulmonary and infections research and the multisystem effects of CF. It is an exciting time to be providing care for patients and their families with CF with all the exciting new discoveries that will be shared in these reviews.
Adrienne P Savant (fig. 1) is at the Children’s Hospital of New Orleans, New Orleans, Louisiana and Department of Pediatrics, Division of Pulmonary Medicine, Tulane University School of Medicine, New Orleans, Illinois.
Susanna McColley is in the Department of Pediatrics, Feinberg School of Medicine, Northwestern University Chicago, Illinois. Stanley Manne Children’s Research Institute, Chicago, Illinois and Ann & Robert H. Lurie Children’s Hospital of Chicago, Chicago, Illinois.
Adrienne P Savant, Susanna A McColley. Cystic fibrosis year in review 2019: Section 2 pulmonary disease and infections. Pediatr Pulmonol 2020 Sep 24.doi: 10.1002/ppul.25091. Online ahead of print. [PubMed]
During the year 2019, research and case reports or series in the field of cystic fibrosis (CF) were in abundance. To adequately address the large body of CF research published during 2019, the CF year in review will be divided into three sections. This report is the second section, focusing specifically on new research related to pulmonary disease and infections. Additional sections will concentrate on CF transmembrane conductance regulator modulators and the multisystem effects of CF. It is an exciting time to be providing care for patients and their families with CF with all the exciting new discoveries that will be shared in these reviews.
Adrienne P Savant is at the Children’s Hospital of New Orleans, New Orleans, Louisiana and Department of Pediatrics, Division of Pulmonary Medicine, Tulane University School of Medicine, New Orleans, Illinois.
Susanna McColley is in the Department of Pediatrics, Feinberg School of Medicine, Northwestern University Chicago, Illinois. Stanley Manne Children’s Research Institute, Chicago, Illinois and Ann & Robert H. Lurie Children’s Hospital of Chicago, Chicago, Illinois.
Adrienne P Savant, Susanna A McColley. Cystic fibrosis year in review 2019: Section 3 multisystem-based care and research. Pediatr Pulmonol 2020 Nov 19.doi: 10.1002/ppul.25158. Online ahead of print. [PubMed]

Fig.2 Susanna McColley
During the year 2019, numerous research studies and other reports were published that are interesting and instructive to professionals who care for people with cystic fibrosis (CF) and their families. This report is the third of 3 CF year in review articles and focuses on the multisystem manifestations of CF care. Previous articles have addressed cystic fibrosis transmembrane regulator modulators and reports on CF pulmonary disease and airway infections. It is an exciting time to be involved in care and research that aims to improve care for people with CF and their families.
Adrienne P Savant is at the Children’s Hospital of New Orleans, New Orleans, Louisiana and Department of Pediatrics, Division of Pulmonary Medicine, Tulane University School of Medicine, New Orleans, Illinois.
Susanna McColley (fig.2) is in the Department of Pediatrics, Feinberg School of Medicine, Northwestern University Chicago, Illinois. Stanley Manne Children’s Research Institute, Chicago, Illinois and Ann & Robert H. Lurie Children’s Hospital of Chicago, Chicago, Illinois.
Iolo Doull Cystic fibrosis 2019: Year in review. Paediatr Respir Rev 2020 Sep;35:95-98. doi: 10.1016/j.prrv.2020.04.001.Epub 2020 Apr 9. [PubMed]

Fig. 3 Iolo Doull
The evidence base for modulator therapies in cystic fibrosis (CF) has continued to expand, and it is likely that up to 90% of people with CF could benefit. Worldwide there are however marked inequalities of access to basic CF care and modulator therapies. For infants and young children there is now an evidence base for inhaled hypertonic saline. There is increasing evidence that structural lung disease in CF is not due purely to infection and that mucus retention and inflammation are also key, and further evidence of the value of azithromycin in those chronically infected with Pseudomonas aeruginosa. Finally, exercise is good for you, but airway clearance is better for mucus clearance.
Dr Iolo Doull (fig.3) is in the Department of Paediatric Respiratory Medicine and Paediatric Cystic Fibrosis Centre, Children’s Hospital for Wales, Cardiff CF14 4XN, United Kingdom.
===============================
Abu-Fraiha Y, Elyashar-Earon H, Shoseyov D, Cohen-Cymberknoh M, Armoni S, Kerem E, Wilschanski M.Increasing Vitamin D Serum Levels Is Associated With Reduced Pulmonary Exacerbations in Patients With Cystic Fibrosis.J Pediatr Gastroenterol Nutr. 2019 Jan;68(1):110-115. [PubMed]
-

Fig. 4 Yasmeen Abu-Frai
In 2012, The North American Cystic Fibrosis Foundation (NACFF) published new guidelines for the treatment of vitamin D deficiency in individuals with cystic fibrosis (CF). The objectives of our study were to assess the efficacy of these guidelines, and to test the effect of increasing vitamin D dosage on pulmonary function and exacerbations.Pulmonary function tests and serum concentrations of 25-hydroxyvitamin D [25(OH)D] were measured 1 year before increasing vitamin D dosage according to the guidelines and at least 1 year later. In addition, days of hospitalization and pulmonary exacerbations were counted and an average per year (average number of days of hospitalization and average number of pulmonary exacerbations [PEA], respectively) was calculated.
A total of 90 patients from The Cystic Fibrosis Clinic at Hadassah Mount-Scopus Hospital, Jerusalem, Israel. The mean serum concentration of vitamin D increased significantly from 20.97 ng/mL (52.34 nmol/L) at baseline to 25.41 ng/mL (63.42 nmol/L) at the end of follow-up (P < 0.001). The number of PEA decreased significantly from 2.79 ± 3.96 to 2.15 ± 2.91 (P = 0.007). The change in vitamin D levels was correlated with a decrease in PEA (correlation coefficient = -0.318, P = 0.002).
The authors concluded the NACFF guidelines for management of vitamin D deficiency improve vitamin D levels in patients with CF but did not reach the normal values in most patients. The increase in vitamin D serum levels was, however, associated with a decrease in number of pulmonary exacerbations.
(The CF Foundation recommends that all individuals with CF, age greater than 12 months to 10 yr, with a serum 25-hydroxyvitamin D level of at least 20 ng/ml (50 nmol/liter) but less than 30 ng/ml (75 nmol/liter), and with confirmed adherence to the prescribed regimen, have the dose of vitamin D3 increased to 1,600-3,000)
A study from the CF Center, Hadassah-University Medcial Center, Jerusalem.
– Dr Yasmeen Abu-Fraiha (fig.4) is a young Israeli Arab of Bedouin origincurrently acting as the Executive Director of GENESIS, an NGO she founded that aims to prevent genetic diseases in the Middle East, especially in the Bedouin community, by spearheading premarital genetic testing and matching. She holds a BSc in Medical Science from the Hebrew University of Jerusalem and an MD from the Hebrew University of Jerusalem.
Adler A . To treat or not to treat: dysglycaemia in cystic fibrosis.Diabet Med. 2019 Aug 20. doi: 10.1111/dme.14112. [Epub ahead of print] [Pubmed]

Fig. 5 Amanda Adler Radcliffe department of Medicine
Good evidence for treating hyperglycaemia in cystic fibrosis is lacking. The accompanying commentary [1] questions whether treating cystic fibrosis-related diabetes (CFRD) and, specifically, lesser degrees of dysglycaemia in people with cystic fibrosis leads to better outcomes [1]. Although epidemiological studies have documented that people with cystic fibrosis and diabetes die earlier than people with cystic fibrosis without diabetes [2], and among people with CFRD, those with higher compared to lower measures of glycaemia also die earlier [3], this evidence falls short of proving that treating people for hyperglycaemia will make them live longer. Warren, then, is correct to offer a ‘reality check’, and chooses to focus not on CFRD, but rather on dysglycaemia, that is, values of blood glucose approaching, but not attaining, the diagnostic criteria for diabetes.
Dr Amanda Adler (Fig.5) is consultant physician at Addenbrooke’s Hospital Cambridge with an interest in diabetes. She also has many advisory and administrative roles with in the UK health system.
Ahmed B, Cox MJ, Cuthbertson L, James P, Cookson WOC, Davies JC, Moffatt MF, Bush A. Longitudinal development of the airway microbiota in infants with cystic fibrosis. Sci Rep. 2019 Mar 26;9(1):5143. doi: 10.1038/s41598-019-41597-0 [Pubmed] Free PFMC Article
The pathogenesis of airway infection in cystic fibrosis (CF) is poorly understood. The authors performed a longitudinal study coupling clinical information with frequent sampling of the microbiota to identify changes in the airway microbiota in infancy that could underpin deterioration and potentially be targeted therapeutically.
Thirty infants with CF diagnosed on newborn screening (NBS) were followed for up to two years. Two hundred and forty one throat swabs were collected as a surrogate for lower airway microbiota (median 35 days between study visits) in the largest longitudinal study of the CF oropharyngeal microbiota. Streptococcus spp. and Haemophilus spp. were the most common genera (55% and 12.5% of reads respectively) and were inversely related. Only beta (between sample) diversity changed with age (Bray Curtis r2 = 0.15, P = 0.03). Staphylococcus and Pseudomonas were rarely detected. These results suggest that Streptococcus spp. and Haemophilus spp., may play an important role in early CF. Whether they are protective against infection with more typical CF micro-organisms, or pathogenic and thus meriting treatment needs to be determined.
Dr Bushra Ahmed of National Heart and Lung Institute, Imperial College and the Department of Respiratory Paediatrics, Royal Brompton Hospital, London
– The uncertainty regarding the early bacterial content of the CF airways, and whether to treat it, seems to continue.
Ahmed MI, Kulkarni H, Shajpal S, Patel D, Patel P, Claydon A, Modha DE, Gaillard EA. Early detection of non-tuberculous mycobacteria in children with cystic fibrosis using induced sputum at annual review.Pediatr Pulmonol. 2019 Mar;54(3):257-263. doi: 10.1002/ppul.24220. Epub 2018 Dec 18.[Pubmed]

Fig. 6 Erol Gaillard Leicester Hospitals
The authors aimed to test the hypothesis that performing sputum induction at routine annual review results in earlier identification of NTM in non-sputum producing children with CF. They conducted a 5-year prospective observational cohort study involving children with CF aged 5-17 years who had sputum induction with hypertonic saline for microbiological surveillance including NTM at their annual review.
Forty-two children (19 males, mean age 11.4 years ± 3.6, mean FEV1 % predicted 94.7 ± 20.6) participated in the study. Six samples from six children (14% of the cohort) yielded NTM never previously isolated from the patient. We also detected three isolates of Pseudomonas aeruginosa and one isolate each of Burkholderia cepacia complex and Meticillin resistant Staphylococcus aureus (MRSA), all of which were first time isolates.
The author conclude that annual induced sputum for microbiological surveillance is useful for early detection of NTM and other important respiratory pathogens, particularly in non-expectorating children. This may lead to earlier identification and help inform initiation of eradication treatment in children with NTM. Children can also be cohorted earlier, before they potentially infect other children in the clinic.
Dr Erol A Gaillard (fig.6) is Senior Lecturer and lead Paediatric CF Consultant in Leicester
Akshintala VS, Kamal A, Faghih M, Cutting GR, Cebotaru L, West NE, Jennings MT, Dezube R, Whitcomb DC, Lechtzin N, Merlo CA, Singh VK. Cystic fibrosis transmembrane conductance regulator modulators reduce the risk of recurrent acute pancreatitis among adult patients with pancreas sufficient cystic fibrosis. Pancreatology. 2019 Sep 28. pii: S1424-3903(19)30735-5. doi: 10.1016/j.pan.2019.09.014. [Epub ahead of print] [Pubmed]

Fig. 7 Venkata S Akshintala
ResearchGate
Approximately 1 in 5 patients with pancreas sufficient cystic fibrosis (PS-CF) will develop acute pancreatitis (AP). It is not known whether ivacaftor alone or in combination with other CFTR (cystic transmembrane regulator) modulators (tezacaftor or lumacaftor) can reduce the risk of AP in patients with PS-CF and AP history.
The authors retrospectively queried the CF registry at our institution for adult patients with PS-CF, a documented history of AP and initiation of CFTR modulators for pulmonary indications. Patient characteristics including demographics, CFTR genotype, pancreatitis risk factors, pancreatic exocrine function and other relevant laboratory, imaging parameters were obtained from the time of the sentinel AP episode through the follow-up period.
A total of 15 adult CF patients were identified with mean age of 44.1 years (SD ± 13.8). In the 24 months preceding CFTR modulator initiation, six of these patients had at least 1 episode of AP with median of 2 episodes [1.75, 2.5]. None of the patients had evidence of pancreatic calcifications or exocrine pancreas insufficiency at the time of CFTR modulator initiation. The mean duration of follow-up after CFTR modulator initiation was 36.7 months (SD ± 21.5). None of the patients who remained on CFTR modulators developed an episode of AP or required hospitalisation for AP related abdominal pain during follow-up.
The authors concluded CFTR modulators, alone or in combination, substantially reduce the risk of recurrent AP over a mean follow-up period of 3 years in adult patients with PS-CF and a history of prior AP. These data suggest that any augmentation of CFTR function can reduce the risk of pancreatitis.
Dr Venkata S Akshintala (fig.7) is Assistant professor at the Pancreatitis Center, Division of Gastroenterology, Johns Hopkins Medical Institutions, Baltimore, MD, USA
Al-Aloul M, Nazareth D, Walshaw M. The renoprotective effect of concomitant fosfomycin in the treatment of pulmonary exacerbations in cystic fibrosis Clin Kidney J. 2019 Feb 7;12(5):652-658. doi: 10.1093/ckj/sfz005. eCollection 2019 Oct. [Pubmed] Free PMC Article

Fig. 8 Mohamed Al-Aloul hcahealthcare.co.uk
Fosfomycin, effective in Cystic Fibrosis (CF), competes with aminoglycosides at renal binding sites and may therefore afford a renoprotective effect when used in combination therapy. We explored this by using markers of acute renal tubular damage [N-acetyl-β-d-glucose-aminidase (NAG), alanine amino-peptidase (AAP) and β2-microglobulin]. Using a prospective randomized crossover trial design, at an acute pulmonary exacerbation, 18 adult CF patients received either 14 days of intravenous (IV) tobramycin or IV tobramycin and IV fosfomycin, both in combination with a second IV antibiotic (colomycin).
Urinary NAG (P = 0.003) and AAP (P = 0.03) following treatment with concomitant fosfomycin were lower than those after treatment with tobramycin and colomycin alone. Fosfomycin attenuated the total 24-h urinary protein leak (P = 0.0001). The 14-day improvements in all surrogate markers of exacerbation resolution (FEV1% predicted, FVC, white cell count and C-reactive protein) were similar for both treatment regimens.
The authors concluded the addition of fosfomycin reduces acute renal injury caused by IV aminoglycoside therapy in CF pulmonary exacerbations.
Dr M Al-Aloul (fig. 8) is at Manchester University NHS Foundation Trust, Wythenshawe, UK, and the School of Biological Sciences, University of Manchester
Albu CC, Stancu IG, Grigore LG, Albu DF, Albu ŞD, Pătraşcu A, Gogănău AM. Impact of genetic testing and family health history of cystic fibrosis in the early prenatal diagnosis and prevention of a new case of genetic disorder. Rom J Morphol Embryol. 2019;60(2):667-671. Free full text [Pubmed]

Fig. 9 Cristina-Crenguta Albu kenkeyugroup.org
The authors state the aim of the present case report is to highlight the importance of genetic testing in the early prenatal diagnosis and prevention of a new case of CF. Cystic fibrosis (CF) is a multi-system autosomal recessive disorder, results of mutations in the CF transmembrane conductance regulator (CFTR) gene, located on the long arm of chromosome 7. We present a special family couple with particular medical history of CF, who comes to our Clinic for genetic tests and a prenatal genetic counseling, to prevent the birth of a new affected CF child. Genetic analysis showed that the first affected child, a daughter, is compound heterozygous for two clinically significant recessive mutations: c.1521_1523delCTT; p.Phe508del, inherited from her mother, who carries the same CFTR mutation, and c.1853_1863delTTTTGCATGAA; p.IIe618Argfs 2, inherited from her father, who is heterozygous, healthy carrier, for the same CFTR mutation. In our case report, early prenatal genetic testing, pre- and post-test genetic counseling was crucial in the management of the present pregnancy, to prevent the birth of a new affected CF child.
Dr Cristina Crenguta Albu (fig.9) is an associate Professor in the Department of Genetics, “Carol Davila” University of Medicine and Pharmacy, Bucharest, Romania.
Altman K, McDonald CM, Michel SH, Maguiness K. Nutrition in cystic fibrosis: From the past to the present and into the future. Pediatr Pulmonol. 2019 Nov;54 Suppl 3:S56-S73. doi: 10.1002/ppul.24521. [Pubmed]

Fig. 10 Kimberly Altman LinkedIn
Nutritional management is an integral part of multidisciplinary care for persons with cystic fibrosis. This review will look at how nutrition care has evolved over time. In addition, they will look at how some newer therapies impact nutrition care.early
– This is a long, detailed and very interesting account of nutritional management in CF. In the summary the authors note there has been a shift from focus on the pulmonary components of CF care to an emphasis on diet and nutrition aspects of care. This may be so in recent years and in adult units (where emphasis on the chest was the rule), however in the early years after Dorothy Andersen described CF in 1938, when there were no adults, CF was considered by Andersen to be primarily a nutritional disorder with other organ involvement such as the chest as secondary to the nutritional problems. It is worth remembering that Dr Douglas Crozier of Toronto led the way in abandoning the traditional low fat diet in the Seventies and was ultimately responsible for the superior Canadian results reported by Mary Corey in 1988 (Corey et al, J Clin Epidemiol 1988; 41:588-591).
Kimberly Altman (fig.10) is a Cystic Fibrosis Dietitian at the Gunnar Esiason Adult Cystic Fibrosis and Lung Center, New York Presbyterian/Columbia University Medical Center, New York. Her co-authors are from Salt Lake City, South Carolina and Indiana.
Amico G, Brandas C, Moran O, Baroni D. Unravelling the Regions of Mutant F508del-CFTR More Susceptible to the Action of Four Cystic Fibrosis Correctors. Int J Mol Sci. 2019 Nov 1;20(21). pii: E5463. doi: 10.3390/ijms20215463. Free full text [Pubmed]

Fig. 11 Debora Baroni
dpi.com
Cystic fibrosis (CF) is a genetic disease associated with the defective function of the cystic fibrosis transmembrane conductance regulator (CFTR) protein that causes obstructive disease and chronic bacterial infections in airway epithelia. The most prevalent CF-causing mutation, the deletion of phenylalanine at position 508 (F508del), leads to CFTR misfolding, trafficking defects and premature degradation. A number of correctors that are able to partially rescue F508del-CFTR processing defects have been identified. Clinical trials have demonstrated that, unfortunately, mono-therapy with the best correctors identified to date does not ameliorate lung function or sweat chloride concentration in homozygous F508del patients. Understanding the mechanisms exerted by currently available correctors to increase mutant F508del-CFTR expression is essential for the development of new CF-therapeutics.
The authors investigated the activity of correctors on the mutant F508del and wild type (WT) CFTR to identify the protein domains whose expression is mostly affected by the action of correctors, and we investigated their mechanisms of action.
They found that the four correctors under study, lumacaftor (VX809), the quinazoline derivative VX325, the bithiazole compound corr4a, and the new molecule tezacaftor (VX661), do not influence either the total expression or the maturation of the WT-CFTR transiently expressed in human embryonic kidney 293 (HEK293) cells. Contrarily, they significantly enhance the expression and the maturation of the full length F508del molecule. Three out of four correctors, VX809, VX661 and VX325, seem to specifically improve the expression and the maturation of the mutant CFTR N-half (M1N1, residues 1-633). By contrast, the CFTR C-half (M2N2, residues 837-1480) appears to be the region mainly affected by corr4a. VX809 was shown to stabilize both the WT- and F508del-CFTR N-half isoforms, while VX661 and VX325 demonstrated the ability to enhance the stability only of the mutant F508del polypeptide.
Corresponding author is Dr Debora Baroni (fig.11) of the Istituto di Biofisica, Consiglio Nazionale delle Ricerche, 16149 Genova, Italy.
Armirotti A, Tomati V, Matthes E, Veit G, Cholon DM, Phuan PW, Braccia C, Guidone D, Gentzsch M, Lukacs GL, Verkman AS, Galietta LJV, Hanrahan JW, Pedemonte N. Bioactive Thymosin Alpha-1 Does Not Influence F508del-CFTR Maturation and Activity. Sci Rep. 2019 Jul 16;9(1):10310. doi: 10.1038/s41598-019-46639-1. [Pubmed]

Fig. 12 Andrea Armirotti iit.it
Deletion of phenylalanine 508 (F508del) in the cystic fibrosis transmembrane conductance regulator (CFTR) anion channel is the most frequent mutation causing cystic fibrosis (CF). F508del-CFTR is misfolded and prematurely degraded. Recently thymosin a-1 (Tα-1) was proposed as a single molecule-based therapy for CF, improving both F508del-CFTR maturation and function by restoring defective autophagy. However, three independent laboratories failed to reproduce these results. Lack of reproducibility has been ascribed by the authors of the original paper to the use of DMSO and to improper handling. Here, these authors address these potential issues by demonstrating that Tα-1 changes induced by DMSO are fully reversible and that Tα-1 peptides prepared from different stock solutions have equivalent biological activity.
Considering the negative results here reported, six independent laboratories failed to demonstrate F508del-CFTR correction by Tα-1. This study also calls into question the autophagy modulator cysteamine, since no rescue of mutant CFTR function was detected following treatment with cysteamine, while deleterious effects were observed when bronchial epithelia were exposed to cysteamine plus the antioxidant food supplement EGCG. Although these studies do not exclude the possibility of beneficial immunomodulatory effects of thymosin α-1, they do not support its utility as a corrector of F508del-CFTR.
Dr Andrea Armirotti (fig.12) is Researcher Technologist, Department of Drug Discovery and Development. Analytical Chemistry and In-vivo Pharmacology Facility, Fondazione Istituto Italiano di Tecnologia, Genova, Italy
— So the initial report that thymosin alpha-1 may be a single molecule-based therapy for CF has not been confirmed by a number of scientists.
Aksit MA, Bowling AD, Evans TA, Joynt AT, Osorio D, Patel S, West N, Merlo C, Sosnay PR, Cutting GR, Sharma N. Decreased mRNA and protein stability of W1282X limits response to modulator therapy. J Cyst Fibros. 2019 Feb 22. pii: S1569-1993(19)30027-X. doi: 10.1016/j.jcf.2019.02.009. [Epub ahead of print] [Pubmed]

Fig. 13 Melis Atalar Aksit
Google Scholar
Cell-based studies have shown that W1282X generates a truncated protein that can be functionally augmented by modulators. However, modulator treatment of primary cells from individuals who carry two copies of W1282X generates no functional CFTR.
To understand the lack of response to modulators, we investigated the effect of W1282X on CFTR RNA transcript levels. qRT-PCR and RNA-seq were performed on primary nasal epithelial (NE) cells of a previously studied individual who is homozygous for W1282X, her carrier parents and control individuals without nonsense variants in CFTR.
CFTR RNA bearing W1282X in NE cells shows a steady-state level of 4.2 ± 0.9% of wild-type (WT) CFTR RNA in the mother and 12.4 ± 1.3% in the father. NMDI14, an inhibitor of nonsense-mediated mRNA decay (NMD), restored W1282X mRNA to almost 50% of WT levels in the parental NE cells. RNA-seq of the NE cells homozygous for W1282X showed that CFTR transcript level was reduced to 1.7% of WT (p-value: 4.6e-3). Negligible truncated CFTR protein was generated by Flp-In 293 cells stably expressing the W1282X EMG even though CFTR transcript was well above levels observed in the parents and proband. Finally, we demonstrated that NMD inhibition improved the stability and response to correctors of W1282X-CFTR protein expressed in the Flp-In-293 cells.
The authors concluded their results show that W1282X can cause substantial degradation of CFTR mRNA that has to be addressed before efforts aimed at augmenting CFTR protein function can be effective.
Melis A Aksit (fig 13) is at the McKusick-Nathans Institute of Genetic Medicine, Johns Hopkins University School of Medicine, Baltimore, MD, United States.
Avedissian SN, Rhodes NJ, Ng TMH, Rao AP, Beringer PM.The Potential for QTc Prolongation with Chronic Azithromycin Therapy in Adult Cystic Fibrosis Patients. Pharmacotherapy. 2019 May 2. doi: 10.1002/phar.2270. [Epub ahead of print] [Pubmed]

Fig.14 Sean Avedissian unmc.edu
Oral azithromycn (AZM) has been shown to reduce airway inflammation and disrupt biofilm formation. However, chronic AZM therapy may result in QT interval (QTc) prolongation. The goals of this study were twofold: 1) to characterize the risk of QTc prolongation in adult cystic fibrosis (CF) patients on AZM and other potential QTc prolonging agents, and 2) to describe and capture the number of potential QTc prolonging agents CF patients are prescribed.
A retrospective study was conducted over a 3-year period in an adult CF Center. QTc values were recorded from electrocardiograms. Univariate and multivariate analyses were conducted. Standard QTc prolongation definitions (Males: ≥ 450 msec, Female: ≥ 470 msec) were used.
A total of 89 adult CF patient’s records were reviewed. Sixty-eight patients received chronic AZM therapy. Two male patients had prolonged QTc, but only 1 received chronic AZM therapy. The median QTc interval between patients receiving and not receiving AZM was not significantly different (405 [interquartile range, IQR: 388-425] versus 394 [IQR:384-413] msec, respectively, P=0.14). Also, the QTc interval for patients taking chronic AZM 500mg Monday/Wednesday/Friday or 250mg daily was not significantly different (401 [IQR: 383-419] versus 409 [IQR:394-427] msec, respectively, P=0.48). When stratified by the number of QTc prolonging medications (AZM vs no AZM), there was no significant difference in median QTc values between patients receiving zero to ≥ 5 QTc prolonging medications.
The authors concluded an association between chronic AZM therapy and longer QTc intervals or significant QTc prolongation was not shown in this study.
Sean N Avedissian (fig 14) is in the Department of Pharmacy Practice, Midwestern University, Chicago. Subsequently Assistant Professor, College of Pharmacy University of Nebraska Medical Center.
— The early literature up to 2014 has been reviewed by Albert RK, Schuller JL (AJRCCM 2014; 189(10) PubMed.[Pubmed] ). Their summary describes the electrophysiological effects of macrolides, reviews literature indicating that the large majority of subjects experiencing cardiac arrhythmias from macrolides have coexisting risk factors and that the incidence of arrhythmias in absence of coexisting risk factors is very low, examines recently published studies describing the relative risk of arrhythmias from macrolides, and concludes that this risk has been overestimated and suggests an approach to patient evaluation that should reduce the relative risk and the incidence of arrhythmias to the point that chronic macrolides can be used safely in the majority of subjects for whom they are recommended. Indeed they are still being recommended and prescribed for people with CF.
Ayoub F, Li H, Blay C, Trillo-Alvarez C, Lascano J, Morelli G. Multidisciplinary Care for Cystic Fibrosis Liver Disease: Where Does the Adult Hepatologist Fit In? Clin Liver Dis (Hoboken). 2019 Dec 20;14(5):187-190. doi: 10.1002/cld.845. eCollection 2019 Nov [Pubmed] Free full text
Fig. 15 Fares Ayoub Twitter.com
The authors conclude the improving life expectancy of patients with CF has led to a significant increase in the number of adults presenting with and suffering from complications of CFLD. The adult hepatologist is expected to play an increasingly important role in the care of adults with CF both within and outside the context of multidisciplinary CF centers. The authors institutional experience with a combined pulmonology/hepatology adult CF clinic was positive and well received by our adult patients with CF. Our experience may serve as a positive example for other centers implementing adult hepatologists into multidisciplinary CF clinics.
— The full article is available via PubMed. The use of UDCA is recommended in view of its low toxicity and clinical effect – despite the fact that Cochrane reviewers found insufficient evidence to recommend its use.
Dr Fares Ayoub (fig. 15) is now a gastroenterology fellow at the University of Chicago. This paper reports experience from the Department of Medicine, University of Florida
Bakhshayeshkaram M, Aghahosseini F, Vaezi F, Kahkooei S, Salehi Y, Hassanzad M, Jamaati HR, Velayati AA. CT-measured pulmonary artery diameter as an independent predictor of pulmonary hypertension in cystic fibrosis. Pol J Radiol. 2018 Aug 23;83:e401-e406. doi: 10.5114/pjr.2018.79204. eCollection 2018. [Pubmed]

Fig. 16 Mehrdad Bakhshayeshkaram
sebum-ir.academia.edu
The aim of the present study was to evaluate the diagnostic performance of thoracic vascular parameters on CT to detect pulmonary hypertension (PH). CF patients who contemporaneously underwent CT and echocardiography were retrospectively enrolled. Baseline characteristics in addition to pulmonary artery diameter (PAD) and pulmonary to aortic (PA/A) ratio were compared between cohorts with and without PH, based on the results of echocardiography separately in paediatric patients (< 18) and adults (≥ 18).
Of a total 119 CF patients, 39 (32.8%) had PH (paediatric: 23/78, 29.5%, adult: 16/41, 39%). In paediatric CF patients, mean age, HCo3, PCo2, and pulmonary artery diameter (PAD) were significantly higher in the PH group compared to the non-PH group. Mean pulmo however, only PAD remained as the independent predictor of PH based on multivariate analysis (overall: 22.86 mm [±3.86] vs. 18.43 mm [±4.72], p = 0.005, paediatric patients: 22.63 mm [±4.4] vs. 17.10 mm [±4.64], p = 0.03). Using a cut off of 19.25 mm, the diagnostic performance of PAD to detect PH was found to be as follows: sensitivity = 82%, specificity = 70%, and accuracy = 73.1%. No significant difference was demonstrated in PAD between PH and non-PH groups in adults with CF (23.19 [±3.60] vs. 21.34 [±3.49], p = 0.7).
In CF patients, PAD revealed an age-dependent performance to detect PH. PAD can be applied to predict pulmonary hypertension in paediatric CF patients and may be recommended to be routinely measured on follow-up chest CT scan in childhood CF.
Mehrdad Bakhshayeshkaram (fig.16) is Professor of Radiology at the Respiratory Diseases Research Center, National Research Institute of Tuberculosis and Lung Diseases (NRITLD), Shahid Beheshti University of Medical Sciences, Tehran, Iran.
Bortoluzzi CF, Pontello E, Pintani E, de Winter-de Groot KM, D’Orazio C, Assael BM, Hunink MGM, Tiddens HAWM, Caudri D; CF Clinics Study Group.Collaborators (36).The impact of chest computed tomography and chest radiography on clinical management of cystic fibrosis lung disease. J Cyst Fibros. 2019 Sep 4. pii: S1569-1993(19)30837-9. doi: 10.1016/j.jcf.2019.08.005. [Epub ahead of print] Pubmed]

Fig. 17 Carla F Bortoluzzi
LinkedIn
Recent standards of care mention chest radiography (CR) but not chest computed tomography (CT) in routine annual follow-up of children with cystic fibrosis (CF). To minimise radiation risk, CT or CR should only be performed if they impact clinical decision making. We investigated whether in addition to a wide range of commonly used clinical parameters, chest CT and/or CR in routine follow-up of CF patients influence clinical decisions.
36 web based clinical vignettes (i.e. case simulations) were designed using clinical data from patients aged 8-18 years, randomly selected from two CF centres in The Netherlands. In a randomized cross-over design, clinicians assessed eight vignettes and suggested therapeutic/diagnostic management on two occasions, with a ten-week interval. Radiological information (CT or CR) was included at only one of the two assessments, in random order. Any differences in management could be attributed to information from CT or CR, and were compared by McNemar analysis.
44 European and Australian clinicians completed a total of 143 CT vignette pairs and 167 CR vignette pairs. CT was associated with a significant increase in anti-fungal treatment (Risk Ratio (RR) 2.8 (1.3-6.0, p = .02)), bronchoscopies (RR 1.6 (1.1-2.5, p = .04)), mycobacterial cultures (RR 1.3 (1.0-1.5, p = .02)), and ‘need for hospitalization’ (i.e. intravenous antibiotics and/or bronchoscopy) (RR 1.4 (1.0-1.9, p = .03)). CR led to a significant increase in inhaled antibiotics only (RR 1.3 (1.0-1.6, p = .04)).
The authors concluded CT but not CR, at routine biennial follow-up was associated with several changes in treatment and/or diagnostic testing, including the need for hospitalisation.
Dr Carla-Frederrica Bortoluzzi (Fig. 17) is a paediatrician at at Unità Fibrosi Cistica, Pediatria, ULSS 2 Ospedale Ca’ Foncello, Treviso, Italy.
Beauchamp KA, Johansen Taber KA, Grauman PV Spurka L, Lim-Harashima J, Svenson A, Goldberg JD, Muzzey D. Sequencing as a first-line methodology for cystic fibrosis carrier screening. Genet Med. 2019 Apr 30. doi: 10.1038/s41436-019-0525-y. [Epub ahead of print] [Pubmed]

Fig. 18 Kyle A Beauchamp
mskcc.org
Medical society guidelines recommend offering genotyping-based cystic fibrosis (CF) carrier screening to pregnant women or women considering pregnancy. The authors assessed the performance of sequencing-based CF screening relative to genotyping, in terms of analytical validity, clinical validity, clinical impact, and clinical utility. Analytical validity was assessed using orthogonal confirmation and reference samples. Clinical validity was evaluated using the CFTR2 database. Clinical impact was assessed using ~100,000 screened patients. Three screening strategies were compared: genotyping 23 guideline-recommended variants (“CF23”), sequencing all coding bases in CFTR (“NGS”), and sequencing with large copy-number variant (CNV) identification (“NGS + CNV”). Clinical utility was determined via self-reported actions of at-risk couples (ARCs). They found analytical accuracy of NGS + CNV was 100% for SNVs, indels, and CNVs; interpretive clinical specificity relative to CFTR2 was 99.5%. NGS + CNV detected 58 ARCs, 18 of whom would have gone undetected with CF23 alone. Most ARCs (89% screened preconceptionally, 56% prenatally) altered pregnancy management, and no significant differences were observed between ARCs with or without at least one non-CF23 variant.
The authors’ conclusion was that modern NGS and variant interpretation enable accurate sequencing-based CF screening. Limiting screening to 23 variants does not improve analytical validity, clinical validity, or clinical utility, but does fail to detect approximately 30% (18/58) of ARCs.
Kyle A Beauchamp (fig.18) is a postdoctoral fellow at Myriad Women’s Health (formerly Counsyl), South San Francisco, CA, USA. and Myriad Genetics, Salt Lake City, UT, USA. Recently Senior Director of Data Science Tempus, Inc.
Bell SC, Mainz JG, MacGregor G, Madge S, Macey J, Fridman M, Suthoff ED, Narayanan S, Kinnman N. Patient-reported outcomes in patients with cystic fibrosis with a G551D mutation on ivacaftor treatment: results from a cross-sectional study. BMC Pulm Med. 2019 Aug 13;19(1):146. doi: 10.1186/s12890-019-0887-6.Free article[Pubmed]

Fig. 19 Scott Bell
Clinical studies demonstrate that ivacaftor (IVA) improves health-related quality of life (HRQoL) in patients aged ≥6 years with cystic fibrosis (CF). The real-world impact of IVA and standard of care (SOC) in groups of patients with G551D and F508del mutations, respectively, was assessed using a survey comprising disease-specific and generic HRQoL measures. Patients with CF aged ≥12 years, or aged 6-11 years with caregiver support, with either (1) a G551D mutation and receiving IVA (G551D/IVA) for ≥3 months, or (2) homozygous for F508del and receiving SOC before lumacaftor/IVA availability (F508del/SOC), were eligible to participate in a cross-sectional survey. Demographic and clinical characteristics, and HRQoL measures were compared between patient groups, and multiple regression analyses were conducted. After differences in patient demographic and clinical characteristics were controlled for, significantly better scores were observed in the G551D/IVA group than in the F508del/SOC group on multiple domains of the validated Cystic Fibrosis Questionnaire-Revised and the EuroQol 5-dimensions 5-level questionnaire.
The authors concluded G551D/IVA patients reported better HRQoL than F508del/SOC patients on generic and disease-specific measures in a real-world setting
Scott Bell (Fig.19) is the Chief Executive of the Translational Research Institute and a Senior Physician of the Adult Cystic Fibrosis Centre at The Prince Charles Hospital in Brisbane, Australia.
Bell SC, Mall MA, Gutierrez H, Macek M, Madge S, Davies JC, et al. The future of cystic fibrosis care: a global perspective. Lancet Respir Med. 2019 Sep 27. pii: S2213-2600(19)30337-6. doi: 10.1016/S2213-2600(19)30337-6. [Epub ahead of print] [Pubmed]full article via Pubmed
This is an important review by 39 international experts in cystic fibrosis. The past six decades have seen remarkable improvements in health outcomes for people with cystic fibrosis, which was once a fatal disease of infants and young children. However, although life expectancy for people with cystic fibrosis has increased substantially, the disease continues to limit survival and quality of life, and results in a large burden of care for people with cystic fibrosis and their families. Furthermore, epidemiological studies in the past two decades have shown that cystic fibrosis occurs and is more frequent than was previously thought in populations of non-European descent, and the disease is now recognised in many regions of the world. The Lancet Respiratory Medicine Commission on the future of cystic fibrosis care was established at a time of great change in the clinical care of people with the disease, with a growing population of adult patients, widespread genetic testing supporting the diagnosis of cystic fibrosis, and the development of therapies targeting defects in the cystic fibrosis transmembrane conductance regulator (CFTR), which are likely to affect the natural trajectory of the disease. The aim of the Commission was to bring to the attention of patients, health-care professionals, researchers, funders, service providers, and policy makers the various challenges associated with the changing landscape of cystic fibrosis care and the opportunities available for progress, providing a blueprint for the future of cystic fibrosis care. The discovery of the CFTR gene in the late 1980s triggered a surge of basic research that enhanced understanding of the pathophysiology and the genotype-phenotype relationships of this clinically variable disease. Until recently, available treatments could only control symptoms and restrict the complications of cystic fibrosis, but advances in CFTR modulator therapies to address the basic defect of cystic fibrosis have been remarkable and the field is evolving rapidly. However, CFTR modulators approved for use to date are highly expensive, which has prompted questions about the affordability of new treatments and served to emphasise the considerable gap in health outcomes for patients with cystic fibrosis between high-income countries, and low-income and middle-income countries (LMICs). Advances in clinical care have been multifaceted and include earlier diagnosis through the implementation of newborn screening programmes, formalised airway clearance therapy, and reduced malnutrition through the use of effective pancreatic enzyme replacement and a high-energy, high-protein diet. Centre-based care has become the norm in high-income countries, allowing patients to benefit from the skills of expert members of multidisciplinary teams. Pharmacological interventions to address respiratory manifestations now include drugs that target airway mucus and airway surface liquid hydration, and antimicrobial therapies such as antibiotic eradication treatment in early-stage infections and protocols for maintenance therapy of chronic infections. Despite the recent breakthrough with CFTR modulators for cystic fibrosis, the development of novel mucolytic, anti-inflammatory, and anti-infective therapies is likely to remain important, especially for patients with more advanced stages of lung disease. As the median age of patients with cystic fibrosis increases, with a rapid increase in the population of adults living with the disease, complications of cystic fibrosis are becoming increasingly common. Steps need to be taken to ensure that enough highly qualified professionals are present in cystic fibrosis centres to meet the needs of ageing patients, and new technologies need to be adopted to support communication between patients and health-care providers.
In considering the future of cystic fibrosis care, the Commission focused on five key areas, which are discussed in this report: the changing epidemiology of cystic fibrosis (section 1); future challenges of clinical care and its delivery (section 2); the building of cystic fibrosis care globally (section 3); novel therapeutics (section 4); and patient engagement (section 5). In panel 1, they summarise key messages of the Commission. The challenges faced by all stakeholders in building and developing cystic fibrosis care globally are substantial, but many opportunities exist for improved care and health outcomes for patients in countries with established cystic fibrosis care programmes, and in LMICs where integrated multidisciplinary care is not available and resources are lacking at present. A concerted effort is needed to ensure that all patients with cystic fibrosis have access to high-quality health care in the future.
— This is a quite awesome overview of the present situation and future for people with cystic fibrosis. The paper runs to 60 pages with 521 references. Scott Bell and Felix Ratjen coordinated the Commission and reviewed and edited all sections of the paper; also they coauthored the Executive Summary. They are to be congratulated on the result!!
Bellier J, Lhommet P, Bonnette P, Puyo P, Le Guen M, Roux A, Parquin F, Chapelier A, Sage E; Foch Lung Transplantation Group. Extracorporeal membrane oxygenation for grade 3 primary graft dysfunction after lung transplantation: long-term outcomes. Clin Transplant. 2019 Jan 18:e13480. doi: 10.1111/ctr.13480. [Epub ahead of print] [Pubmed]

Fig. 20 Jocelyn Bellier
Doctolib
Extracorporeal membrane oxygenation (ECMO) is an efficient and innovative therapeutic tool for primary graft dysfunction (PGD). However, its effect on survival and long-term lung function are not well-known. This study evaluated those parameters in patients with PGD requiring ECMO. This single-centre, retrospective study included patients who underwent LTx at our institute between January 2007 and December 2013. Patients and disease characteristics, survival and pulmonary function tests were recorded.
A total of 309 patients underwent LTx during the study period and 211 were included. The patients were predominantly male (53.5%), the median age was 39 years, and the primary pathology was suppurative disease (53.1%). ECMO for PGD was mandatory in 24 (11.7%) cases. Mortality at 3 months in the ECMO group was 50% (N=12). However, long-term survival after PGD did not correlate with ECMO. Forced expiratory volume and vital capacity were significantly reduced in patients with PGD requiring ECMO, especially those with idiopathic pulmonary fibrosis.
It is concluded veno-arterial ECMO appears to be suitable for management of primary graft dysfunction after lung transplant. Patients with PGD requiring ECMO show increased initial mortality; however, long-term survival was comparable with that of other patients in the study. Lung function does not appear to be related to PGD requiring ECMO.
Jocelyn Bellier (Fig. 20) is a thoracic and cardiovascular surgeon in the Thoracic Surgery Dept., Foch Hospital, Suresnes, France
Bener A, Al-Mulla M, Clarke A. Premarital Screening and Genetic Counseling Program: Studies from an Endogamous Population. Int J Appl Basic Med Res. 2019 Jan-Mar;9(1):20-26. doi: 10.4103/ijabmr.IJABMR_42_18. [Pubmed]

Fig. 21 Abdulbari Bener
mejfm.com
Studies in Arab countries have shown a significant lack of knowledge of Premarital Screening and Genetic Counseling (PMSGC) Program. PMSGC can identify and modify, through prevention and management, some behavioral, medical, and other health risk factors known to impact pregnancy outcomes.
The aim of this study was to explore the knowledge, attitudes, and practice of Qatari’s toward the premarital screening program and shedding more light on a complex matter.
The current study revealed that knowledge and attitude regarding PMSGC program were low in population. Motivation, enforcement, and implementation of program at the school and university educational campaigns are vital. Improved counseling and adding new topics for counseling on genetic, chronic, and mental illness; building healthy families; and reproduction and fertility are considered to be top priorities in community
Dr Abdulbari Bener (fig.21) is professor in the Department of Biostatistics and Medical Informatics, Cerrahpasa Faculty of Medicineistanbul, Istanbul University, İstanbul, Turkey. Other authors are from Manchester, Qatar and Cardiff
Gitte Berkers , Peter van Mourik, Annelotte M Vonk, Evelien Kruisselbrink, Johanna F Dekkers, Karin M de Winter-de Groot, Hubertus G M Arets, Rozemarijn E P Marck-van der Wilt, Jasper S Dijkema, Maaike M Vanderschuren, Roderick H J Houwen, Harry G M Heijerman, Eduard A van de Graaf, Sjoerd G Elias, Christof J Majoor, Gerard H Koppelman, Jolt Roukema, Marleen Bakker, Hettie M Janssens, Renske van der Meer, Robert G J Vries, Hans C Clevers, Hugo R de Jonge, Jeffrey M Beekman, Cornelis K van der Ent Rectal Organoids Enable Personalized Treatment of Cystic Fibrosis. Cell Rep 2019 Feb 12;26(7):1701-1708.e3.doi: 10.1016/j.celrep.2019.01.068. Free article [Pubmed]

Fig.22 Gitte Berkers ResearchGate
In vitro drug tests using patient-derived stem cell cultures offer opportunities to individually select efficacious treatments. Here, we provide a study that demonstrates that in vitro drug responses in rectal organoids from individual patients with cystic fibrosis (CF) correlate with changes in two in vivo therapeutic endpoints. We measured individual in vitro efficaciousness using a functional assay in rectum-derived organoids based on forskolin-induced swelling and studied the correlation with in vivo effects. The in vitro organoid responses correlated with both change in pulmonary response and change in sweat chloride concentration. Receiver operating characteristic curves indicated good-to-excellent accuracy of the organoid-based test for defining clinical responses. This study indicates that an in vitro assay using stem cell cultures can prospectively select efficacious treatments for patients and suggests that biobanked stem cell resources can be used to tailor individual treatments in a cost-effective and patient-friendly manner.
Gitte Berkers (fig.22) is a PhD student in the Department of Pediatric Pulmonology, Wilhelmina Children’s Hospital, University Medical Center Utrecht, Utrecht University, 3584 EA Utrecht, the Netherlands.
Bianco B, Horsley A, Brennan A. Implications of fatherhood in cystic fibrosis. Paediatr Respir Rev. 2019 Mar 16. pii: S1526-0542(19)30022-3. doi: 10.1016/j.prrv.2019.02.008. [Epub ahead of print] [Pubmed]
Advances in fertility treatment mean that men with CF are increasingly able to become fathers. This is a report of clinical outcomes in 22 men with CF who have become fathers for the first time. Overall mean (SD) FEV1% predicted declined from 60.1(18.0)% to 57.4(20.2)% from baseline to 1 year (p = 0.15). Weight declined from mean (SD) 70.6 kg (10.4) to 68.3 kg (10.2), p = 0.0001. Six men had an FEV1% predicted ≤40% at the time of birth: 50% died or received lung transplantation within the 12-15 month follow up period. Becoming a parent is a major life event, and as with new mothers, fathers with CF may be at risk of significant decline.
Brooke Bianco is a CF research nurse at the Manchester Adult CF Centre, Manchester University Hospital NHS Foundation Trust, Manchester M23 9LT, United Kingdom.
Bisch AL, Wheatley CM, Baker SE, Peitzman ER, Van Iterson EH, Laguna TA, Morgan WJ, Snyder EM. Cystic Fibrosis Transmembrane Conductance Regulator Genotype, Not Circulating Catecholamines, Influences Cardiovascular Function in Patients with Cystic Fibrosis.Clin Med Insights Circ Respir Pulm Med. 2019 Mar 29;13:1179548419835788. doi: 10.1177/1179548419835788. eCollection 2019.[Pubmed] Free PMC Article
Previous work has shown that a single dose of aβ-agonist increases cardiac output (Q) and stroke volume (SV) and decreases systemic vascular resistance (SVR) in healthy subjects. This effect is attenuated in patients with CF; however, the mechanism is unknown. Potential explanations for this decreased cardiovascular response to a β-agonist in CF include inherent cardiovascular deficits secondary to the CFTR mutation, receptor desensitization from prolonged β-agonist use as part of clinical care, or inhibited drug delivery to the bloodstream due to mucus buildup in the lungs. This study sought to determine the effects of endogenous epinephrine (EPI) and norepinephrine (NE) on cardiovascular function in CF and to evaluate the relationship between cardiovascular function and CFTR F508del mutation.
A total of 19 patients with CF and 31 healthy control subjects completed an assessment of Q (C2H2 rebreathing), SV (calculated from Q and heart rate [HR]), Q and SV indexed to body surface area (BSA, QI, and SVI, respectively), SVR (through assessment of Q and mean arterial blood pressure [MAP]), and HR (from 12-lead electrocardiogram [ECG]) at rest along with plasma measures of EPI and NE. We compared subjects by variables of cardiovascular function relative to EPI and NE, and also based on genetic variants of the F508del mutation (homozygous deletion for F508del, heterozygous deletion for F508del, or no deletion of F508del).

Fig.23 Eric Snyder
Cystic fibrosis patients demonstrated significantly lower BSA (CF = 1.71 ± 0.05 m2 vs healthy = 1.84 ± 0.04 m2, P = .03) and SVI (CF = 30.6 ± 2.5 mL/beat/m2 vs healthy = 39.9 ± 2.5 mL/beat/m2, P = .02) when compared with healthy subjects. Cystic fibrosis patients also demonstrated lower Q (CF = 4.58 ± 0.36 L/min vs healthy = 5.71 ± 0.32 L/min, P = .03) and SV (CF = 54 ± 5.5 mL/beat vs healthy = 73.3 ± 4.5 mL/beat, P = .01), and a higher HR (CF = 93.2 ± 3.9 bpm vs healthy = 80.5 ± 2.7 bpm, P < .01) and SVR (CF = 2082 ± 156 dynes*s/cm-5 vs healthy = 1616 ± 74 dynes*s/cm-5, P = .01) compared with healthy subjects. Furthermore, CF patients demonstrated a lower SV (P < .01) corrected for NE when compared with healthy subjects. No significant differences were seen in HR or Q relative to NE, or SVR relative to EPI. Differences were seen in SV (F(2,14) = 7.982, P < .01) and SV index (F(2,14) = 2.913, P = .08) when patients with CF were stratified according to F508del mutation (number of deletions).
The authors concluded individuals with CF have lower cardiac and peripheral hemodynamic function parameters at rest. Furthermore, these results suggest that impairment in cardiovascular function is likely the result of F508del CFTR genotype, rather than receptor desensitization or inhibited drug delivery.
From a Thesis by Alexander Louis Bisch in the Department of Kinesiology, University of Minnesota, Minneapolis, MN, USA The advisor was Dr Eric M Snyder (fig.23) Assistant Professor and Director, Clinical Exercise Physiology Laboratory
Blanchard AC, Tang L, Tadros M, Muller M, Spilker T, Waters VJ, LiPuma JJ, Tullis E.Burkholderia cenocepacia ET12 transmission in adults with cystic fibrosis. Thorax. 2019 Nov 15. pii: thoraxjnl-2019-214098. doi: 10.1136/thoraxjnl-2019-214098. [Epub ahead of print][Pubmed]
Fig. 24 Ana Blanchard ResearchGate
This report describes transmission of a Burkholderia cenocepacia ET12 strain (ET12-Bc) at the Toronto Adult Cystic Fibrosis (CF) Centre occurring from 2008 to 2017. Epidemiological and genomic data from 11 patients with CF were evaluated. Isolates were analysed using whole genome sequencing (WGS). Epidemiological investigation and WGS analysis suggested nosocomial transmission, despite enhanced infection control precautions. This was associated with subsequent deaths in 10 patients. ET12-Bc positive patients are no longer cared for on the same unit as ET12-Bc negative patients.
Ana C Blanchard (fig.24) is a research fellow in the Dept of Pediatrics, Infectious Diseases, Hospital for Sick Children, Toronto, Ontario, Canada
Boëlle PY, Debray D, Guillot L, Clement A, Corvol H; French CF Modifier Gene Study Investigators. Cystic Fibrosis Liver Disease: Outcomes and Risk Factors in a Large Cohort of French Patients.Hepatology. 2019 Apr;69(4):1648-1656. doi: 10.1002/hep.30148. Epub 2018 Dec 28. [Pubmed]

Fig.25 Pierre-Yves Boelle ResearchGate
Cystic fibrosis (CF)-related liver disease (CFLD) is a common symptom in patients with CF. However, its prevalence, risk factors, and evolution are unclear. We analyzed a large database of patients with CF to investigate the incidence of CFLD, its related risk factors, and the use and effect of ursodeoxycholic acid (UDCA) treatment. We retrospectively analyzed 3,328 CF patients with pancreatic insufficiency born after 1985 and recruited into the French CF Modifier Gene Study since 2004. We determined liver status, age at CFLD and severe CFLD onset, sex, CFTR genotype, history of meconium ileus, treatment with UDCA, and respiratory and nutritional status.
The incidence of CFLD increased by approximately 1% every year, reaching 32.2% by age 25. The incidence of severe CFLD increased only after the age of 5, reaching 10% by age 30. Risk factors for CFLD and severe CFLD were male sex, CFTR F508del homozygosity, and history of meconium ileus. Increasingly precocious initiation of UDCA treatment did not change the incidence of severe CFLD. Finally, patients with severe CFLD had worse lung function and nutritional status than other CF patients.
The authors concluded CFLD occurs not only during childhood but also later in the lifetime of patients with CF; male sex, CFTR F508del homozygosity, and history of meconium ileus are independent risk factors for CFLD development; earlier use of UDCA over the last 20 years has not changed the incidence of severe CFLD, leading to questions about the use of this treatment in young children given its possible adverse effects.
— Another large study in CFLD from France with similar findings to those of Toledano et al 2019 using the UK CF Patient Registry data. In contrast to this French study, the UK data identified a positive association with survival and the use of URSO.
Pierre-Yves Boelle (fig.25) is Professor at the Pierre and Marie Curie University, Paris
Bourke SJ, Anderson A, Briggs J, Doe S, Echevarria C, Choudhary M, McEleny K, Stewart J. Current status of fertility and family formation in men with cystic fibrosis. Hum Fertil (Camb). 2019 Aug 29:1-6. doi: 10.1080/14647273.2019.1656824. [Epub ahead of print] [Pubmed]

Fig.26 Stephen Bourke ResearchGate
Men with cystic fibrosis are nearly always infertile due to congenital bilateral absence of the vas deferens, but can undergo assisted reproduction. Ill health may influence reproductive choices. This paper reports data on fertility and family formation in CF including the use of assisted reproduction in a total cohort of 205 men (mean age 30.9, range 16.6-64.3 years) studied over a 10-year period. Overall 102 (49.5%) were single, 52 (25.7%) were married, 48 (23.3%) were in long-term heterosexual relationships, and 3 (1.5%) were in same-sex relationships. One (0.5%) was fertile naturally. In total, 30 children were born to 23 (11%) men by assisted reproduction: 4 used donor sperm and 19 had sperm retrieval and intracytoplasmic sperm injection (ICSI). Two men each adopted two children; 15 (7.3%) men were acting as step-fathers to 20 children from their partners’ previous relationships. Overall 41 (20%) men had fatherhood roles. ICSI was unsuccessful in 4 men. A further 16 men were referred for fertility treatment but did not proceed. Of the 19 men having children by ICSI, 3 died leaving 4 children. Men with CF face complex decisions when considering their relationships, fertility and fatherhood.
Dr Stephen Bourke (fig.26) is consultant physician and Director of the Newcastle Adult Cystic Fibrosis Centre. Mr Kevin McEleny is consultant urologist Newcastle fertility centre and Freeman Hospital Dr Jane Stewart is consultant in reproductive medicine at Newcastle Fertility Centre and the Royal Victoria Infirmary Newcastle upon Tyne Dr Meenakshi Choudhary is Consultant Gynaecologist Newcastle Fertility Centre
Boyle M, Moore JE, Whitehouse JL, Bilton D, Downey DG. The diagnosis and management of respiratory tract fungal infection in cystic fibrosis: A UK survey of current practice. Med Mycol. 2019 Feb 1;57(2):155-160. doi: 10.1093/mmy/myy014. [Pubmed]
-

Fig. 27 Damion Downey Queens University Belfast
- The aim of this survey was to assess the variability in current practice across the UK in diagnosis and management of fungal lung disease in CF patients. A 21 question anonymous online survey was sent to 94 paediatric and adult CF consultants in the UK. The response rate was 60.6% (32 adult physicians, 25 pediatricians) with 55 full and 2 partially completed surveys.
For a first diagnosis of ABPA 20 (35.1%) treat with prednisolone alone, 38 (66.7%) use prednisolone with itraconazole and 2 (3.5%) choose voriconazole. Only 5 (8.8%) treat with prednisolone alone for a 1st relapse, 33 (58%) used prednisolone with itraconazole. To reduce treatment, 21 (36.8%) decrease steroids to zero over time and maintain azole therapy, 18 (31.6%) stop the azole and steroid after a fixed time, and 5 (8.8%) stop the azole after a fixed time and maintain a small steroid dose. Thirty-eight (66.7%) respondents believe Aspergillus colonization of the airway can cause clinical deterioration, and 37 (66.1%) would treat this. Scedosporium apiospermum infection has been diagnosed and treated by 35 (61.4%) of respondents. Results of this survey highlight the variance in clinical practice and the limited evidence available to guide management of fungal infection in CF.
Damion Downey (fig.27) is a Clinical Professor, School of Medicine, Dentistry and Biomedical Sciences Belfast.
Breuer O, Schultz A, Turkovic L, de Klerk N, Keil AD, Brennan S, Harrison J, Robertson C, Robinson PJ, Sly PD, Ranganathan S, Stick SM, Caudri D; AREST CF.The Changing Prevalence of Lower Airway Infections in Young Children with Cystic Fibrosis.Am J Respir Crit Care Med. 2019 Feb 27. doi:10.1164/rccm.201810-1919OC. [Epub ahead of print] [Pubmed]
-

Fig. 28 Osmed Breuer and daughter
- Historical studies suggest that airway infection in cystic fibrosis (CF) initiates with Staphylococcus aureus and Haemophilus influenzae with later emergence of Pseudomonas aeruginosa. Aspergillus species are regarded as relatively infrequent, late occurring infections. The authors assessed the prevalence and change in prevalence of early lower airway infections in a modern cohort of children with CF.
All infants diagnosed with CF after newborn screening, participating in the AREST-CF cohort study between 2000-2018, were included. Participants prospectively underwent bronchoalveolar lavage (BAL) at 3-6 months,1 year and annually up to 6 years of age. Lower airway infection prevalence was described. Changes in prevalence patterns were assessed longitudinally using generalized estimating equations controlling for age and repeated visits.
A total of 380 infants underwent 1,759 BALs. The overall prevalence and median age of first acquisition of the most common infections were: S. aureus 11%, 2.5yrs, P. aeruginosa 8%, 2.4yrs, Aspergillus species 11%, 3.2yrs, H. influenzae 9%, 3.1yrs. During the study, a significant decrease in prevalence of P. aeruginosa (p<0.001) and S. aureus (p<0.001) was observed with significant change towards more aggressive treatment. Prevalence of Aspergillus infections did not significantly change (p=0.669). T
The study demonstrated Aspergillus species and P. aeruginosa are commonly present in the lower airways from infancy. The decrease in prevalence of P. aeruginosa and S. aureus since 2000, coinciding with more aggressive therapeutic approach, has resulted in Aspergillus becoming the most commonly isolated pathogen in young children. Further research is warranted to understand the implication of these findings.
Dr Oded Breuer (fig.28) of the Pediatric Pulmonology Unit Hadassah –Hebrew University Medical Center Jerusalem currently on two year Ausimed Fellowship at the Telethon Kids Institute and Perth Children’s Hospital, Australia.
Breuer O, Schultz A, Garratt LW, et al. Aspergillus Infections and Progression of Structural Lung Disease in Children with Cystic Fibrosis [published online ahead of print, 2019 Nov 20]. Am J Respir Crit Care Med. 2019;10.1164/rccm.2158501908-OC. doi:10.1164/rccm.201908-1585OC [Pubmed]
The authors aimed to evaluate longitudinal associations between Aspergillus infections and lung disease in young children with CF.Longitudinal data on 330 children participating in the Australian Respiratory Early Surveillance Team for Cystic Fibrosis surveillance program between 2000-2018 who underwent annual chest computed tomography (CT) and bronchoalveolar lavage (BAL) were used to determine the association between Aspergillus infections and the progression of structural lung disease. Results were adjusted for the effects of other common infections, associated variables and repeated visits. Secondary outcomes included inflammatory markers in BAL, respiratory symptoms and admissions for exacerbations.
Results: H. influenzae, S. aureus, P. aeruginosa and Aspergillus infections were all associated with worse CT scores in the same year (p overall<0.05). Only P. aeruginosa and Aspergillus were associated with progression in CT scores in the year following an infection and worse CT scores at the end of the observation period. P. aeruginosa was most significantly associated with development of bronchiectasis (difference 0.9; 95%CI, 0.3-1.6; p=0.003) and Aspergillus with trapped-air (difference 3.2; 95%CI, 1.0-5.4; p=0.004). Aspergillus infections were also associated with markers of neutrophilic inflammation (p<0.001) and respiratory admissions risk (p=0.008).
The authors concluded lower respiratory Aspergillus infections are associated with the progression of structural lung disease in young children with CF. They consider this study highlights the need to further evaluate early Aspergillus species infections and the feasibility, risk and benefit of eradication regimens.
Dr Osmed Breuer (fig.28) is from the Perth Children’s Hospital and the Hadassah University Hospital, Jerusalem
(see also Harun SN et al below on Aspergillus)
Bry C, Hubert D, Reynaud-Gaubert M, Dromer C, Mal H, Roux A, Boussaud V, Claustre J, Le Pavec J, Murris-Espin M, Danner-Boucher I. Pregnancy after lung and heart-lung transplantation: a French multicentre retrospective study of 39 pregnancies. ERJ Open Res. 2019 Oct 30;5(4). pii: 00254-2018. doi: 10.1183/23120541.00254-2018. eCollection 2019 Oct [Pubmed] Free PMC Article
Pregnancy after lung and heart-lung transplantation remains rare. This French study deals with change in lung function after a pregnancy and the maternal and newborn outcomes. We retrospectively included 39 pregnancies in 35 women aged >20 years. Data on patients, course of pregnancies and newborns were collected from nine transplantation centres. Mean age at time of pregnancy was 28 years. Cystic fibrosis affected 71% of patients. Mean±sd time between transplantation and pregnancy was 63±44 months. 26 births occurred (67%) with a mean term of 36 weeks of amenorrhoea and a mean birthweight of 2409 g. Prematurity was observed in 11 cases (43%). Forced expiratory volume in 1 s was 83.9% of predicted before pregnancy and 77.3% of predicted 1 year after the end of pregnancy (p=0.04). 10 patients developed chronic lung allograft dysfunction after delivery. Nine patients died at a mean±sd time after transplantation of 8.2±7 years and a mean±sd time after pregnancy of 4.6±6.5 years.
These data show that pregnancy remains feasible in lung and heart-lung transplant recipients, with more frequent maternal and newborn complications than in the general population. Survival in this cohort appears to be similar to the global survival observed in lung transplant recipients. Planned pregnancy and multidisciplinary follow-up are crucial.
Dr Charlotte Bry is an Assistant-Chef de Clinique Service de Pneumologie, CHU de Nantes, Nantes, France.
Burgel PR, Munck A, Durieu I, Chiron R, Mely L, Prevotat A, Murris-Espin M, Porzio M, Abely M, Reix P, Marguet C, Macey J, Sermet-Gaudelus, Corvol H, Bui S, Lemonnier L, Dehilotte C, Da Silva J, Paillasseur JL, Hubert D; French Cystic Fibrosis Reference Network study group. Real-Life Safety and Effectiveness of Lumacaftor-Ivacaftor in Patients with Cystic Fibrosis. Am J Respir Crit Care Med. 2019 Oct 11. doi: 10.1164/rccm.201906-1227OC. [Epub ahead of print] [Pubmed]

Fig. 29 Pierre Regis Burgel ResearchGate
A study to evaluate the safety and effectiveness of lumacaftor-ivacaftor in adolescents (≥12 years) and adults (≥18 years) in a real-life post-approval setting. Among the 845 patients (292 adolescents, 553 adults) who initiated lumacaftor-ivacaftor, 18.2% (154 patients) discontinued treatment due to respiratory (48.1%, 74 patients) or non-respiratory (27.9%, 43 patients) adverse events. In multivariable logistic regression, factors associated with increased rates of discontinuation included adult age group, percent predicted forced expiratory volume in 1 sec (ppFEV1)<40% and numbers of intravenous antibiotic courses during the year prior to lumacaftor-ivacaftor initiation. Patients with continuous exposure to lumacaftor-ivacaftor showed an absolute increase in ppFEV1 (+3.67%), an increase in body mass index (+0.73 kg/m2), and a decrease in intravenous antibiotic courses by 35%. Patients who discontinued treatment had significant decrease in ppFEV1, without improvement in BMI or decrease in intravenous antibiotic courses.
The authors concluded treatment with Lumacaftor-ivacaftor was associated with improvement in lung disease and nutritional status in patients who tolerated treatment. Adults who discontinued lumacaftor-ivacaftor, often due to adverse events, were found at high risk of clinical deterioration.
Dr Pierre-Régis Burgel (fig.29) currently works at the Faculty of Medicine, Paris Descartes, CPSC. He does research in Pulmonology and Cell Biology.
Calvo-Lerma J, Hulst J Boon M, Colombo C, Masip E, Ruperto M, Fornés-Ferrer V, van der Wiel E, Claes I, Garriga M, Roca M, Crespo-Escobar P, Bulfamante A, Woodcock S, Martínez-Barona S, Andrés A, de Boeck K, Ribes-Koninckx C; MyCyFAPP project.Clinical validation of an evidence-based method to adjust Pancreatic Enzyme Replacement Therapy through a prospective interventional study in paediatric patients with Cystic Fibrosis. PLoS One. 2019 Mar 12;14(3):e0213216. doi: 10.1371/journal.pone.0213216. eCollection 2019. [PubMed]
-

Fig. 30 Joaquim Calvo-Lerma SEDYN
- A method to adjust Pancreatic Enzyme Replacement Therapy in Cystic Fibrosis is not currently available. To assess the in vivo efficacy of a method to adjust the dose of enzymatic supplement in CF extrapolated from previous in vitro digestion studies (theoretical optimal dose, TOD). Secondly, to assess how individual patient characteristics influence the expected coefficient of fat absorption (CFA) and thus to identify an individual correction factor to improve TOD.
A prospective interventional study in 43 paediatric patients with CF from 5 European centres. They followed a 24h fixed diet with the theoretical optimal dose for each meal. Faecal collection was carried out between colorimetric markers in order to include all the faeces corresponding to the fixed diet. Beta regression models were applied to assess the associations of individual patient characteristics with the CFA.
Median CFA was 90% (84, 94% 1st, 3rd Q.) with no significant differences among centres. Intestinal transit time was positively associated with CFA (p = 0.007), but no statistical associations were found with and age, gender, phenotype or BMI. Regression model showed no improvement of the in vitro predicted theoretical optimal dose when taking individual patient characteristics into account.
Strict adherence to the theoretical optimal dose of enzymatic supplement for a prescribed meal, led to median CFA levels at the clinical target of 90% with a low variability between patients. The proposed method can be considered as a first approach for an evidence-based method in PERT dosing based on food characteristics. Results have to be confirmed in free dietary settings.
The investigation led by Joaquim Calvo-Lerma (fig.30) Instituto de Investigacion Sanitaria La Fe de Valencia, Spain.
– This is undoubtedly rather complicated! It seems very complex and the problem of lack of adherence to such a regimen would be a real possibility.
-
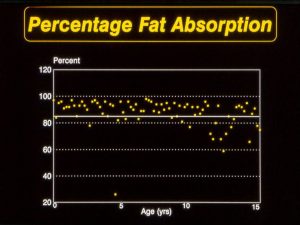
Fig. 31 Fat absorption in children attending the Leeds Regional Paedaitric CF Centre
- The author’s assumption that “patients with CF have to decided the dose of enzymatic supplement to take every single time they eat”. In many centres the CF dietitian is regularly involved to help the patient/parents decide on the their enzyme requirements. Published evidence, from the few centres where intestinal fat absorption is actually measured, suggests that similar CFA are achieved as reported in this publication – for example children at the Leeds Regional CF Centre (Fig.31). Commonly patients are receiving unnecessarily large doses of enzymes, the dose having been increased in response to abdominal or bowel symptoms without any measure of fat absorption to establish if the symptoms are due to malabsorption.
Calvopina DA, Noble C, Weis A, Hartel GF, Ramm LE, Balouch F, Fernandez-Rojo MA, Coleman MA, Lewindon PJ, Ramm GA. Supersonic shear-wave elastography and APRI for the detection and staging of liver disease in pediatric cystic fibrosis. J Cyst Fibros. 2019 Jul 11. pii: S1569-1993(19)30820-3. doi: 10.1016/j.jcf.2019.06.017. [Epub ahead of print][Pubmed]

Fig. 32 Grant Ramm
QIMR Berghofer
Current diagnostic methods for the diagnosis of Cystic fibrosis (CF)-associated liver disease (CFLD) are non-specific and assessment of disease progression is difficult prior to the advent of advanced disease with portal hypertension. This study investigated the potential of(SSWE) to non-invasively detect CFLD and assess hepatic fibrosis severity in children with CF.125 children were enrolled in this study including CFLD (n = 55), CF patients with no evidence of liver disease (CFnoLD = 41) and controls (n = 29). CFLD was diagnosed using clinical, biochemical and imaging best-practice guidelines. Advanced CFLD was established by the presence of portal hypertension and/or macronodular cirrhosis on ultrasound. Liver stiffness measurements (LSM) were acquired using supersonic shear-wave elastography (SSWE) and diagnostic performance for CFLD detection was evaluated alone or combined with aspartate aminotransferase-to-platelet ratio index (APRI).Liver stiffness measurement (LSM) was significantly higher in CFLD (8.1 kPa, IQR = 6.7-11.9) versus CFnoLD (6.2 kPa, IQR = 5.6-7.0; P < 0.0001) and Controls (5.3 kPa, IQR = 4.9-5.8; P < 0.0001). LSM was also increased in CFnoLD versus Controls (P = 0.0192). Receiver Operating Characteristic (ROC) curve analysis demonstrated good diagnostic accuracy for LSM in detecting CFLD using a cut-off = 6.85 kPa with an AUC = 0.79 (Sensitivity = 75%, Specificity = 71%, P < 0.0001). APRI also discriminated CFLD (AUC = 0.74, P = 0.004). Classification and regression tree modelling combining LSM + APRI showed 14.8 times greater odds of accurately predicting CFLD (AUC = 0.84). The diagnostic accuracy of SSWE for discriminating advanced disease was excellent with a cut-off = 9.05 kPa (AUC = 0.95; P < 0.0001).
The authors concluded SSWE-determined LSM shows good diagnostic accuracy in detecting CFLD in children, which was improved when combined with aspartate aminotransferase-to-platelet ratio index (APRI). Supersonic shear-wave elastography alone discriminates advanced CFLD.
From the Hepatic Fibrosis Group, QIMR Berghofer Medical Research Institute,Herston, Australia; Faculty of Medicine, The University of Queensland, Brisbane,
Grant Ramm (fig.32) is Professor and Head of the Hepatic Fibrosis Laboratory and Coordinator of the Cell and Molecular Biology Department and is a Senior Principal Research Fellow at QIMR Berghofer.
Carzino R, Frayman KB, King L, Vidmar S, Ranganathan S; AREST CF. Regional differences in infection and structural lung disease in infants and young children with cystic fibrosis. J Cyst Fibros. 2019 Nov 6. pii: S1569-1993(19)3-6. doi: 10.1016/j.jcf.2019.10.018. [Epub ahead of print][Pubmed]

Fig. 33 Rosemary Carzino rch.org.au
Both infection and inflammation are critical to the progression of cystic fibrosis (CF) lung disease. Potential anatomical differences in lower airway infection, inflammation and bronchiectasis in young children with CF raise questions regarding the pathogenesis of early structural lung disease.
A longitudinal multi-centre birth cohort study of infants newly diagnosed with CF was conducted. Paired bronchoalveolar lavage (BAL) samples were obtained from the right middle lobe (RML) and lingula bronchi. Chest computed tomography (CT) was performed biennially and analysed using the modified CF-CT scoring system.
One hundred and twenty-four children (0.11 – 7.0 years) contributed 527 BAL samples and underwent 388 CT chest scans. Pro-inflammatory microbes were detected in 279 BAL samples (53%), either in both lingula and RML samples (69%), in the lingula alone (24%), or in the RML alone in only 7% of samples. Overall, the prevalence of structural lung disease was greater in the setting of pro-inflammatory microbes. Although infection was less commonly isolated in the right lung, bronchiectasis was more commonly detected in the right lung compared with the left. No anatomical differences in the presence of air trapping were detected.
The authors concluded overall that the detection of pro-inflammatory microbes in the lower airways was associated with increased risk of both air trapping and bronchiectasis. However, the apparent discordance between commonest sites of isolation of pro-inflammatory microbes and the anatomical site of early bronchiectasis warrants further exploration.
Rosemary Carzino (fig 33) Respiratory Diseases Group, Murdoch Children’s Research Institute, Victoria, Australia.
Chandler NJ, Ahlfors H, Drury S, Mellis R, Hill M, McKay FJ, Collinson C, Hayward J, Jenkins L, Chitty LS. Noninvasive Prenatal Diagnosis for Cystic Fibrosis: Implementation, Uptake, Outcome, and Implications.Clin Chem. 2019 Sep 24. pii: clinchem.2019.305011. doi: 10.1373/clinchem.2019.305011. [Epub ahead of print] [Pubmed]

Fig. 34 Natalie Chandler North Thames GMS
Non-invasive prenatal diagnosis (NIPD) for monogenic disorders has a high uptake by families. Since 2013, our accredited public health service laboratory has offered NIPD for monogenic disorders, predominantly for de novo or paternally dominantly inherited mutations.
Here we describe the extension of this service to include definitive NIPD for a recessive condition, cystic fibrosis (CF). Definitive NIPD for CF was developed using next-generation sequencing. Validation was performed on 13 cases from 10 families before implementation. All cases referred for CF NIPD were reviewed to determine turnaround times, genotyping results, and pregnancy outcomes.
Of 38 referrals, 36 received a result with a mean turnaround of 5.75 days (range, 3-11 days). Nine cases were initially inconclusive, with 3 reported unaffected because the low-risk paternal allele was inherited and 4 cases in which the high-risk paternal allele was inherited, receiving conclusive results following repeat testing. One case was inconclusive owing to a paternal recombination around the mutation site, and one case was uninformative because of no heterozygosity. Before 2016, 3 invasive referrals for CF were received annually compared with 38 for NIPD in the 24 months since offering a definitive NIPD service.
The authors concluded timely and accurate NIPD for definitive prenatal diagnosis of CF is possible in a public health service laboratory. The method detects recombinations, and the service is well-received as evidenced by the significant increase in referrals. The bioinformatic approach is gene agnostic and will be used to expand the range of conditions tested for.
Natalie Chandler (fig.34) is the senior Clinical Scientist in the Rare Diseases Laboratory NE Thames Genomic Laboratory Hub. Great Ormond Street, London.
Charbek E, Kamel G, Nayak RP. Ivacaftor for the Treatment of Cystic Fibrosis Coexisting with Trisomy 21: A Case Report. Cureus. 2019 Nov 18;11(11):e6179. doi: 10.7759/cureus.6179.[Pubmed] Free PMC Article

Fig. 35 Edward Charbek ssmhealth.com
The association between cystic fibrosis (CF) and trisomy 21, or Down Syndrome (DS) is rare, and it pertains a poor prognosis with the majority of patients dying in infancy. We report a case of a 28-year-old male with DS and moderate CF (ΔF508/G551D, FEV1 1.92 L, 60% predicted at the age of 18 years) diagnosed in childhood. The patient’s lung function continued to deteriorate over time (FEV1 nadir of 1.29 L), and he was started on ivacaftor in the year 2012 following ivacaftor release and approval. FEV1 and FVC improved significantly along with an increase in the patient’s body mass index. Ivacaftor potentiates the open-channel probability of the G551D-CFTR. It has been shown to improve lung function, symptoms, weight, and sweat chloride concentration and decrease the risk of pulmonary exacerbations in patients with severe pulmonary CF (G551D). Our case argues against the reported literature of poor prognosis when the two chronic diseases coexist as only one case report in the literature described a DS patient with CF surviving into adulthood.
In our patient, treatment with ivacaftor resulted in an increase in FEV1 and weight that exceeded the response observed in the ivacaftor landmark trial. Genetic studies are underway to understand the genetic basis of the large variation in DS phenotypes, which is probably caused by allelic heterogeneity on multiple chromosomes. The latter may explain the enhanced response observed in our patient and suggests that although patients with concomitant DS and CF may have worse lung disease, their response to novel therapies may be intensified. Further studies are needed in this subset of patient population to better characterize CF with trisomy and other genetic disorders.
Dr Edward Charbek (fig.35) is a pulmonologist at Internal Medicine, Saint Louis University School of Medicine, St. Louis, USA
Gang Chen , Ling Sun , Takafumi Kato, Kenichi Okuda, Mary B Martino, Aiman Abzhanova , Jennifer M Lin , Rodney C Gilmore , Bethany D Batson, Yvonne K O’Neal, Allison S Volmer, Hong Dang, Yangmei Deng, Scott H Randell, Brian Button, Alessandra Livraghi-Butrico, Mehmet Kesimer, Carla Mp Ribeiro, Wanda K O’Neal, Richard C Boucher. IL-1β dominates the promucin secretory cytokine profile in cystic fibrosis. J Clin Invest 2019 Oct 1;129(10):4433-4450. doi: 10.1172/JCI125669. Free PMC article [Pubmed]
Fig. 36 Gang Chen chenab.unc.edu
Cystic fibrosis (CF) lung disease is characterized by early and persistent mucus accumulation and neutrophilic inflammation in the distal airways. Identification of the factors in CF mucopurulent secretions that perpetuate CF muco-inflammation may provide strategies for novel CF pharmacotherapies. We show that IL-1β, with IL-1α, dominated the mucin prosecretory activities of supernatants of airway mucopurulent secretions (SAMS). Like SAMS, IL-1β alone induced MUC5B and MUC5AC protein secretion and mucus hyperconcentration in CF human bronchial epithelial (HBE) cells. Mechanistically, IL-1β induced the sterile α motif-pointed domain containing ETS transcription factor (SPDEF) and downstream endoplasmic reticulum to nucleus signaling 2 (ERN2) to upregulate mucin gene expression. Increased mRNA levels of IL1B, SPDEF, and ERN2 were associated with increased MUC5B and MUC5AC expression in the distal airways of excised CF lungs. Administration of an IL-1 receptor antagonist (IL-1Ra) blocked SAMS-induced expression of mucins and proinflammatory mediators in CF HBE cells. In conclusion, IL-1α and IL-1β are upstream components of a signaling pathway, including IL-1R1 and downstream SPDEF and ERN2, that generate a positive feedback cycle capable of producing persistent mucus hyper-concentration and IL-1α and/or IL-1β-mediated neutrophilic inflammation in the absence of infection in CF airways. Targeting this pathway therapeutically may ameliorate mucus obstruction and inflammation-induced structural damage in young CF children.
Dr Gang Chen (fig.36) is research associate at the Marsico Lung Institute and Cystic Fibrosis Research Center, University of North Carolina at Chapel Hill, Chapel Hill, North Carolina, USA.
Dr Ling Sun of Research Center of Regeneration Medicine, West China Hospital, Sichuan University, Chengdu, Sichuan Province, China.
Chevalier B, Hinzpeter A. The influence of CFTR complex alleles on precision therapy of cystic fibrosis. J Cyst Fibros. 2019 Dec 25. pii: S1569-1993(19)30988-9. doi: 10.1016/j.jcf.2019.12.008. [Epub ahead of print] [Pubmed]
CFTR is an extensively studied gene and multiple sequence variants have been identified, many of which still need to be defined as neutral or disease causing. Complex alleles are defined when at least two variants are identified on the same allele. Each pathogenic variant can affect distinct steps of the CFTR biogenesis. As CFTR modulators are being developed to alleviate specific defects, pathogenic variants need to be characterized to propose adequate treatments. Conversely, cis-variants can affect treatment response when defects are additive or if they alter the binding or efficacy of the modulator.
Hence, complex alleles increase the complexity of CFTR variant classification and need to be assigned as neutral, disease causing or modulating treatment efficacy. This review was based on a symposium session presented at the 16th ECFS Basic Science Conference, Dubrovnik, Croatia, 27 to 30 March, 2019.
Dr Benoit Chevalier is at INSERM U1151, Institut Necker Enfants Malades, Paris, France; Université Paris Descartes, Paris, France.
Christian F, Thierman A, Shirley E, Allen K, Cross C, Jones K. Sustained Glycemic Control With Ivacaftor in Cystic Fibrosis-Related Diabetes. Author information. J Investig Med High Impact Case Rep. 2019 Jan-Dec;7:2324709619842898. doi: 10.1177/2324709619842898. Full article available on Journal website [Pubmed]

Fig 37. Francis Christian OU College of Medicine
Recent small studies have shown improvement in endogenous insulin secretion with a short period of ivacaftor therapy in primarily pediatric patients with cystic fibrosis transmembrane conductance regulator mutations amenable to potentiation.
In this article, the authors present the case of a 34 year old adult who had CFRD from the age of 20 years who developed sustained improvement in glycemic control after initiation of ivacaftor; also stabilisation of a declining FEV1.
Dr Francis Christian (fig.37) from the University of Oklahoma Health Sciences Center, Oklahoma City, OK, USA.
Hayward J, Chitty LS. Beyond screening for chromosomal abnormalities: Advances in non-invasive diagnosis of single gene disorders and fetal exome sequencing. Semin Fetal Neonatal Med. 2018 Apr;23(2):94-101. doi: 10.1016/j.siny.2017.12.002. Epub 2018 Jan 2. [Pubmed]

Fig. 38 Lynn Chitty
eMedEvents
Fig. 37 Jane Hayward
LinkedIn
Emerging genomic technologies, largely based around next generation sequencing (NGS), are offering new promise for safer prenatal genetic diagnosis. These innovative approaches will improve screening for fetal aneuploidy, allow definitive non-invasive prenatal diagnosis (NIPD) of single gene disorders at an early gestational stage without the need for invasive testing, and improve our ability to detect monogenic disorders as the aetiology of fetal abnormalities. This presents clinicians and scientists with novel challenges as well as opportunities. In addition, the transformation of prenatal genetic testing arising from the introduction of whole genome, exome and targeted NGS produces unprecedented volumes of data requiring complex analysis and interpretation. Now translating these technologies to the clinic has become the goal of clinical genomics, transforming modern healthcare and personalized medicine. The achievement of this goal requires the most progressive technological tools for rapid high-throughput data generation at an affordable cost. Furthermore, as larger proportions of patients with genetic disease are identified we must be ready to offer appropriate genetic counselling to families and potential parents. In addition, the identification of novel treatment targets will continue to be explored, which is likely to introduce ethical considerations, particularly if genome editing techniques are included in these targeted treatments and transferred into mainstream personalized healthcare.
Here the authors review the impact of NGS technology to analyse cell-free DNA (cfDNA) in maternal plasma to deliver NIPD for monogenic disorders and allow more comprehensive investigation of the abnormal fetus through the use of exome sequencing.
Lynn Chitty (fig.38) (now Dame) is Professor of Genetics & Fetal Medicine. From North East Thames Regional Genetics Laboratory, Great Ormond Street NHS Foundation Trust, London, UK.
Jane Hayward (Fig. 37) is a senior scientist with the North East Thames Regional Genetics Laboratory, Great Ormond Street NHS Foundation Trust, London, UK.
Chouchane I, Stremler-Lebel N, Reix P. Lumacaftor/ivacaftor initiation in two liver transplantation patients under tacrolimus and antifungal azoles. Clin Case Rep. 2019 Feb 17;7(4):616-618. doi: 10.1002/ccr3.2053. eCollection 2019 Apr. [Pubmed]
The authors report the initiation of CFTR modulator lumacaftor/ivacaftor combination (LUM/IVA) in two adolescents with cystic fibrosis who were treated with antifungal azoles (AZO) and tacrolimus (TCS) for liver transplantation. Despite multiple drug-drug interactions, maintaining therapeutic TCS levels was achievable. During the following year, LUM/IVA was well tolerated, providing clinical benefits.
Ikrame Couchane from Service de pédiatrie, Hôpital Mère Enfant Centre Hospitalier Universitaire, Hôpital Dupuytren Limoges France.
Choudhury M, Taylor P, Morgan PH, Duckers J, Lau D, George L, Ketchell RI, Wong FS.Association between HbA1c and the development of cystic fibrosis-related diabetes. Diabet Med. 2019 Jan 30. doi: 10.1111/dme.13912. [Epub ahead of print] [Pubmed]
A study to examine HbA1c as a predictor of risk for future development of cystic fibrosis-related diabetes and to assess the association with the development of retinopathy in people with cystic fibrosis-related diabetes. The authors considered there is a link between HbA1c level and the future development of dysglycaemia in cystic fibrosis based on oral glucose tolerance test, as well as microvascular outcomes. Although current guidance does not advocate the use of HbA1c as a diagnostic tool in cystic fibrosis-related diabetes, it may be of clinical use in determining individuals at risk of future development of cystic fibrosis-related diabetes.
- Fig. 39 Ian Ketchell
- Fig. 40 Dawn Lau
- Fig. 41 Jamie Duckers
- Fig. 42 Susan Wong
From the All Wales Adult Cystic Fibrosis Centre, University Hospital Llandough, Cardiff, UK. and the Diabetes Research Group, Division of Infection and Immunity, Cardiff, UK.
Dr Ian Ketchell (fig. 39) is Director of the Adult CF Centre
Dr Jamie Duckers (fig.41) is consultant in CF and lead for the CF Research Programme
Dr Dawn Lau (fig.40) is consultant in CF and with a special interest in Education
Professor Susan Wong,(fig. 42) School of Medicine, Cardiff has conducted extensive research into type 1 diabetes and immunotherapy to prevent diabetes.
Tan SMJ, Coffey MJ, Ooi CY. Differences in clinical outcomes of paediatric cystic fibrosis patients with and without meconium ileus. J Cyst Fibros. 2019 Oct 28. pii: S1569-1993(19)30892-6. doi: 10.1016/j.jcf.2019.09.008. [Epub ahead of print] [Pubmed]

Fig. 43 Keith Chee Ooi research.unsw.edu.au
Meconium ileus (MI) affects up to 20% of newborns with cystic fibrosis (CF). The authors compared clinical outcomes between Australian paediatric CF patients with and without meconiu ileus (non-MI). There were 162 matched pairs (N=324, 52% female) with mean (SD) age of 15.3 (8.2) and 14.9 (7.9) years for MI and non-MI patients respectively (P=0.6).
MI patients aged 5-23 had poorer FEV1% compared to non-MI patients (estimate -0.070 SE [0.02], P=0.003). There were no significant differences in P. aeruginosa isolation rates; however S. aureus isolation rates were lower in MI patients (72%) compared to non-MI (82%) (OR 0.6 [0.3-1.0], P=0.03). Chronic colonisation rates for P. aeruginosa and S. aureus were not significantly different between groups. MI patients aged 2-20 had significantly lower BMI Z-scores over time (estimate -0.25 SE [0.1], P=0.02). MI patients were more likely to receive oral feed supplements (OR 2.8 [1.4-6.1], P=0.003) and gastrostomy formation (OR 4.4 [1.1-24.6], P=0.02).
The authors concluded CF patients with MI may have worse lung function, growth and nutrition than non-MI patients over time. Meconium ileus may be an early poor prognostic factor for CF.
— There is much previous work supporting the fact that infants with MI seem to have a more severe manifestations of their CF – one being in their growth. Previous work is reviewed clearly in this article. MI seems to “mark the severity of mutations of the Cystic Fibrosis Transmembrane Conductance Regulator (CFTR) gene” (Dupuis et al 2016)
Keith Chee Ooi (fig.43) is associate professor in the the Department of Gastroenterology, Sydney Children’s Hospital, High Street, Randwick NSW 2031, Australia.
Cho DY, Zhang S, Lazrak A, Grayson JW, Peña Garcia JA, Skinner DF, Lim DJ, Mackey C, Banks C, Matalon S, Woodworth BA. Resveratrol and ivacaftor are additive G551D CFTR-channel potentiators: therapeutic implications for cystic fibrosis sinus disease. Int Forum Allergy Rhinol 2019; 9(1):100-105 [Pubmed]

Fig. 44 Do-Yeon Cho
UAB Medicine
Fisher rat thyroid cells (FRT) transfected with G551D CFTR and human sinonasal epithelial cells (HSNE) containing the CFTR G551D mutation were subjected to pharmacologic manipulation of transepithelial ion transport in Ussing chambers. Activity was further evaluated using whole-cell patch clamp methods in G551D FRT cells.
The authors observed additive improvement in G551D CFTR-mediated Cl– secretion suggests that resveratrol could enhance ivacaftor therapy in these patients and improve CF-related rhinosinusitis.
Do-Yeon Cho (fig.44) is in the Department of Otolaryngology, University of Alabama at Birmingham and Gregory Fleming James Cystic Fibrosis Research Center, University of Alabama at Birmingham, Birmingham, AL.
John Paul Clancy, Calvin U Cotton, Scott H Donaldson, George M Solomon, Donald R VanDevanter, et al. CFTR modulator theratyping: Current status, gaps and future directions. J Cyst Fibros 2019 Jan;18(1):22-34.doi: 10.1016/j.jcf.2018.05.004. Epub 2018 Jun 20. Free PMC article [Pubmed]

Fig. 45 John Clancy
Background: New drugs that improve the function of the cystic fibrosis transmembrane conductance regulator (CFTR) protein with discreet disease-causing variants have been successfully developed for cystic fibrosis (CF) patients. Preclinical model systems have played a critical role in this process, and have the potential to inform researchers and CF healthcare providers regarding the nature of defects in rare CFTR variants, and to potentially support use of modulator therapies in new populations.
Methods: The Cystic Fibrosis Foundation (CFF) assembled a workshop of international experts to discuss the use of preclinical model systems to examine the nature of CF-causing variants in CFTR and the role of in vitro CFTR modulator testing to inform in vivo modulator use. The theme of the workshop was centered on CFTR theratyping, a term that encompasses the use of CFTR modulators to define defects in CFTR in vitro, with application to both common and rare CFTR variants.
Results: Several preclinical model systems were identified in various stages of maturity, ranging from the expression of CFTR variant cDNA in stable cell lines to examination of cells derived from CF patients, including the gastrointestinal tract, the respiratory tree, and the blood. Common themes included the ongoing need for standardization, validation, and defining the predictive capacity of data derived from model systems to estimate clinical outcomes from modulator-treated CF patients.
Conclusions: CFTR modulator theratyping is a novel and rapidly evolving field that has the potential to identify rare CFTR variants that are responsive to approved drugs or drugs in development.
Dr John Paul Clancy (fig.45) is the vice president of clinical research for the Cystic Fibrosis Foundation and a professor of pediatric pulmonary medicine at Cincinnati Children’s Hospital Medical Center, Cincinnati, OH, United States.
Cohen RWF, Folescu TW, Boechat MCB, Fonseca VM, Marques EA, Leão RS. High-resolution computed tomography findings in young infants with cystic fibrosis detected by newborn screening. Clinics (Sao Paulo). 2019 Oct 21;74:e1399. doi: 10.6061/clinics/2019/e1399. eCollection 2019.Free full text [Pubmed]

Fig. 46 Renata Wrobel Folescu Cohen Doctoralia
High-resolution computed tomography (HRCT) allows the early detection of pathological changes in the lung structure, and reproducible scoring systems can be used to quantify chest computed tomography (CT) findings in patients with cystic fibrosis (CF). The aim of the study was to describe early HRCT findings according to a validated scoring system in infants with CF diagnosed by newborn screening (NBS).
This cross-sectional study included infants with CF diagnosed by NBS who were born between January 2013 and January 2017 and who underwent HRCT scanning within the first year after diagnosis when they were clinically stable. The CT scans were evaluated using the modified Bhalla score.
Thirty-two subjects underwent HRCT scanning. The mean total-modified Bhalla score was 3.6±2.1, and 93.8% of the scans were abnormal. Pseudomonas aeruginosa airway colonization was associated with increased modified Bhalla score values. Bronchial wall thickening was the most common feature (90.6%), followed by bronchial collapse/consolidation (59.4%), mosaic attenuation/perfusion (50%), bronchiectasis (37.5%) and mucus plugging (15.6%). Bronchial wall thickening was diffuse in most of the patients.
Conclusion: A substantial proportion of infants diagnosed with CF after detection by NBS already showed evidence of lung disease. P. aeruginosa colonization was associated with increased Bhalla scores, highlighting the importance of this CF pathogen in early structural lung disease. The presence of bronchial wall thickening at such a young age may reflect the presence of airway inflammatory processes. The detection and quantification of structural abnormalities with the modified Bhalla score may aid in the identification of lung disease before it is clinically apparent.
Dr Renata Wrobel Folescu Cohen (fig. 46) is in the Faculdade de Ciencias Medicas, Universidade do Estado do Rio de Janeiro, Rio de Janeiro, RJ, BR.
Costabile G, Provenzano R, Azzalin A, Scoffone V, Chiarelli LR, Rondelli V, Grillo I, Zinn T, Lepioshkin A, Savina S, Miro A, Quaglia F, Makarov V, Coenye T, Brocca P, Riccardi G, Buroni S, Ungaro F. PEGylated mucus-penetrating nanocrystals for lung delivery of a new FtsZ inhibitor against Burkholderia cenocepacia infection. Nanomedicine. 2019 Oct 25;23:102113. doi: 10.1016/j.nano.2019.102113. [Epub ahead of print] [Pubmed]

Fig. 47 Gabriella Costabile Faculty of Chemistry
C109 is a potent but poorly soluble FtsZ inhibitor displaying promising activity against Burkholderia cenocepacia, a high-risk pathogen for cystic fibrosis (CF) sufferers. To harness C109 for inhalation, we developed nanocrystal-embedded dry powders for inhalation suspension consisting in C109 nanocrystals stabilized with D-α-tocopheryl polyethylene glycol 1000 succinate (TPGS) embedded in hydroxypropyl-β-cyclodextrin (CD). The powders could be safely re-dispersed in water for in vitro aerosolization. Owing to the presence of a PEG shell, the rod shape and the peculiar aspect ratio, C109 nanocrystals were able to diffuse through artificial CF mucus. The promising technological features were completed by encouraging in vitro/in vivo effects. The formulations displayed no toxicity towards human bronchial epithelial cells and were active against planktonic and sessile B. cenocepacia strains. The efficacy of C109 nanosuspensions in combination with piperacillin was confirmed in a Galleria mellonella infection model, strengthening their potential for combined therapy of B. cenocepacia lung infections.
Gabriella Costabile (fig.47) is in the Department of Pharmacy, University of Napoli “Federico II”, Napoli, Italy.
Cortes-Santiago N, Leung DH, Castro E, Finegold M, Wu H, Patel KR.Hepatic Steatosis Is Prevalent Following Orthotopic Liver Transplantation in Children With Cystic Fibrosis.J Pediatr Gastroenterol Nutr. 2019 Jan;68(1):96-103. doi: 10.1097/MPG.0000000000002154. [Pubmed]
-

Fig. 48 Nahir Cortes-Santiago
- A systematic study of allograft liver histology in children undergoing orthotopic liver transplantation (LT) for cystic fibrosis-related liver disease (CFLD). Retrospective clinic-pathologic review of explants and allograft liver biopsies from 13 children and adolescents with CFLD.In this study, the median age at LT for CFLD was 15.7 years. Notably, 10 of 13 (77%) CF explants had >5% steatosis and 8 of 13 (61.5%) demonstrated variable fibrosis. The median age, sex, type of transplant (liver vs liver-lung), pancreatic insufficiency status, body mass index (BMI) percentile, genotype, and prevalence of diabetes were comparable in those with and without explant steatosis. More than half of allograft biopsies showed significant steatosis (17/31, 54.8%) and lobular inflammation (16/31, 51.6%).Hepatocyte ballooning was less frequent (5/31, 16.1%). Overall, 6 patients (46.2%) had allograft steatosis that worsened over time in 2 patients (33%). None had advanced fibrosis (≥stage 3). Patients with allograft steatosis had significantly more biopsies, were more likely to be “liver only” recipients, had a shorter interval since transplant and higher body mass index percentile (although <85). Patients without explant steatosis never demonstrated allograft steatosis, whereas 60% of patients with explant steatosis (n = 6) developed varying degrees of allograft steatosis. The degree of explant steatosis did not predict its severity in allografts (P = 0.3).
The authors concluded this is the first study highlighting the development of allograft steatosis in CF patients. Their findings suggest that allograft steatosis in patients with CF may be related to pre-existing steatosis in native livers, regardless of other risk factors and may have implications on patient management and long-term graft/patient survival.
Dr Nahir Cortes-Santiago (fig.48) is Medical Resident pathology at Baylor College of Medicine
Couroux P, Farias P, Rizvi L, Griffin K, Hudson C, Crowder T, Tarran R, Tullis E. First clinical trials of novel ENaC targeting therapy, SPX-101, in healthy volunteers and adults with cystic fibrosis. Pulm Pharmacol Ther. 2019 Jul 11:101819. doi: 10.1016/j.pupt.2019.101819. [Epub ahead of print] [Pubmed]

Fig. 50 Peter Couroux
ResearchGate

Fig. 49 Elizabeth Tullis Facebook
ENaC inhibition has been investigated as a CF treatment; however, small molecule inhibitors of ENaC lack efficacy and/or have shown dose-limiting hyperkalemia. SPX-101 is a novel, investigational small peptide (SPLUNC1 mimetic) that regulates ENaC density with the potential for efficacy without systemic effects.
Two trials are presented: The first was a Phase 1, 2-part, randomized, double-blind, placebo-controlled, ascending-dose study of nebulized SPX-101 in healthy adults. Part 1 evaluated 4 single doses of SPX-101 ranging from 20 to 240 mg. Part 2 evaluated a 14-day regimen of SPX-101 at 4 doses of SPX-101 ranging from 10 to 120 mg BID. Pharmacokinetics, adverse events, spirometry, vital signs, electrocardiograms, pulse oximetry, and clinical laboratory values were assessed. The second trial was a tolerability-confirming, Phase 1b, open-label study conducted in 5 adult subjects with CF. Ascending doses of SPX-101 inhalation solution (10 mg-120 mg BID) were administered for 7 days. Safety was assessed as described above.
All 64 healthy volunteers (32 in each Part) completed the single and multiple dose study. SPX-101 was well tolerated with little/no systemic exposure and with no hyperkalemia. Adverse events were generally mild with reported respiratory events associated with the purported pharmacological activity of SPX-101. Tolerability of SPX-101 was similarly observed in adults with CF; all 5 subjects treated with SPX-101 completed the study.
SPX-101 was well-tolerated across a range of doses and had little/no systemic exposure in healthy adults and adults with CF, thus supporting further study in patients with CF.
Dr Peter Couroux (fig.50) is Global Senior Research Director at Inflamax Research Inc, Mississauga, Ontario, Canada.
Dr Elizabeth Tullis (fig. 49) is Director of the Adult Cystic Fibrosis Clinic at St Michael’s Hospital Foundation Toronto. In 2015 she was appointed to the first Cystic Fibrosis Canada Chair in Adult Cystic Fibrosis Research. Dr. Tullis is a Professor of Medicine at the University of Toronto, the Respirology Division Head at St. Michael’s Hospital, and an Associate Scientist in the Li Ka Shing Knowledge Institute. She is the Cystic Fibrosis Canada Chair in Adult CF Research.
Course CW, Hanks R. Newborn screening for cystic fibrosis: Is there benefit for everyone? Paediatr Respir Rev. 2019 Aug;31:3-5. doi: 10.1016/j.prrv.2019.02.003. Epub 2019 Feb 28. [Pubmed]
Fig. 50 Christopher Course profiles.cardiff.ac.uk
Newborn screening for cystic fibrosis (CF) has become a widely accepted and endorsed public health strategy in economically developed countries, although there is little consensus on optimal screening methods and gene panels. Increasing understanding of CFTR genetics and consequent unpredictability of phenotypic and clinical outcomes lead to diagnostic uncertainty, and emergence of Cystic Fibrosis Screen Positive Inconclusive Diagnosis (CF-SPID). Many of these children are clinically well or have a mild phenotype yet may still experience the psychosocial impact of a CF diagnosis. This questions the role of newborn screening and how best to manage those it identifies with CF-SPID.
Christopher Course (fig.50) is a research fellow in the Department of Paediatric Respiratory Medicine and Cystic Fibrosis, Children’s Hospital for Wales, Cardiff, United Kingdom.
— It is difficult to see how the occurrence of CF-SPID “questions the role of newborn screening” the introduction of which has been one of the major advances in CF care over the past 40 years!!!
Dankert-Roelse JE., Bouva MJ., Jakobs BS., Janssens HM., de Winter-de Groot KM., Schonbeck Y., Gille JJP., Gulmans VAM., Verschoof-Puite RK., Schielen PCJI., Verkerk PH.Newborn blood spot screening for cystic fibrosis with a four-step screening strategy in the Netherlands J Cyst Fibros 2019; 18: 54 – 63 [Pubmed]

Fig.51 Jeanette Dankert-Roelse
Newborn screening for cystic fibrosis (NBSCF) was introduced in the Dutch NBS program in 2011 with a novel strategy. Dutch NBSCF consisted of four steps: immuno-reactive trypsin (IRT), Pancreatitis-associated Protein (PAP), DNA analysis by Inno-LiPa (35 mutations), extended gene analysis (EGA) as fourth step and as safety net. Only samples with two CFTR-variants were considered screen-positive, but samples with one disease-causing variant were considered also screen-positive from April 2013. The first 5 years of NBSCF were evaluated during a follow-up ranging from 2 to 6.8 years for sensitivity, specificity, positive predictive value (PPV), ratio of CF/Cystic Fibrosis Screen Positive infants with an Inconclusive Diagnosis (CFSPID) and median age at diagnosis, and were compared to other novel strategies for NBSCF and European Cystic Fibrosis Society (ECFS) Best Practice Standards of Care.
NBSCF achieved a sensitivity of 90% (95% CI 82%-94%), specificity of 99.991% (95% CI 99.989%-99.993%), PPV of 63% (95% CI 55%-69%), CF/CFSPID ratio of 4/1, and median age at diagnosis of 22 days, if samples with two variants as well as samples with one disease-causing variant were considered screen-positive.
The authors concluded the program achieved the goal to minimize the number of false positives and showed a favourable performance but sensitivity and CF/CFSPID ratio did not meet criteria of EFCS Best Standards of Care. Changed cut-off values for PAP and IRT and classification of R117H-7T/9T to non-pathogenic may improve sensitivity to ≥95% and CF/CFSPID ratio to 10/1. PPV is estimated to be around 60%
Dr Jeanette Dankert-Roelse (fig.51) wrote her first paper on neonatal CF screening in early Eighties and made many contributions to the CF literature since then.
From the School for Public Health and Primary Care, Dept Pediatrics, Maastricht University Medical Centre, Debyelaan 25, 6229 HX Maastricht, the Netherlands. Electronic address: jeannettedankert@gmail.com.
David J, Chrastina P, Pešková K, Kožich V, Friedecký D, Adam T, Hlídková E, Vinohradská H, Novotná D, Hedelová M, Al Taji E, Holubová A, Skalická V, Macek M, Gaillyová R, Votava 1. Epidemiology of rare diseases detected by newborn screening in the Czech Republic. Cent Eur J Public Health. 2019 Jun;27(2):153-159. doi: 10.21101/cejph.a5441. [Pubmed] Presymptomatic detection of patients with rare diseases (RD), defined by a population frequency less than 1 : 2,000, is the task of newborn screening (NBS). In the Czech Republic (CZ), currently eighteen RD are screened: phenylketonuria/hyperphenylalaninemia (PKU/HPA), congenital hypothyroidism (CH), congenital adrenal hyperplasia (CAH), cystic fibrosis (CF), medium chain acyl-CoA dehydrogenase deficiency (MCADD), long chain 3-hydroxyacyl-CoA dehydrogenase deficiency (LCHADD), very long chain acyl-CoA dehydrogenase deficiency (VLCADD), carnitine palmitoyl transferase I and II deficiency (CPTID, CPTIID), carnitine-acylcarnitine translocase deficiency (CACTD), maple syrup urine disease (MSUD), glutaric aciduria type I (GA I), isovaleryl-CoA dehydrogenase deficiency (IVA), argininemia (ARG), citrullinemia (CIT), biotinidase deficiency (BTD), cystathionine beta-synthase-deficient homocystinuria (CBSD HCU), and methylenetetrahydrofolate reductase deficiency homocystinuria (MTHFRD HCU). The aim was to analyze the prevalence of RD screened by NBS in CZ.
The authors examined the NBS programme in CZ from 1 January 2010 to 31 December 2017, which covered 888,891 neonates. Dried blood spots were primarily analysed using fluorescence immunoassay, tandem mass spectrometry and fluorimetry. The overall prevalence of RD among the neonate cohort was 1 : 1,043. Individually, 1 : 2,877 for CH, 1 : 5,521 for PKU/HPA, 1 : 6,536 for CF (1 : 5,887 including false negative patients), 1 : 12,520 for CAH, 1 : 22,222 for MCADD, 1 : 80,808 for LCHADD, 1 : 177,778 for GA I, 1 : 177,778 for IVA, 1 : 222,223 for VLCADD, 1 : 296,297 for MSUD, 1 : 8,638 for BTD, and 1 : 181,396 for CBSD HCU.
They observed prevalence of rare diseases, based on NBS, corresponds to that expected, more precisely it was higher for BTD and lower for MSUD, IVA, CBSD HCU, MCADD and VLCADD. Early detection of rare diseases by means of NBS is an effective secondary prevention tool.
From the Department of Children and Adolescents, Third Faculty of Medicine, Charles University and University Hospital Kralovske Vinohrady, Prague, Czech Republic. Department of Paediatrics, Second Faculty of Medicine, Charles University and University Hospital Motol, Prague, Czech Republic.
de Poel, E; Lefferts, JW; Beekman, JM. Intestinal organoids for Cystic Fibrosis research. J Cyst Fibros. 2019 Nov 28. pii: S1569-1993(19)30964-6. doi: 10.1016/j.jcf.2019.11.002. [Epub ahead of print] Review. [Pubmed] Free Article

Fig.52 Dr Jeffrey Beekman receiving the ECFS award in 2017
Significant progress has been made in the development of CFTR modulator therapy; however, current CFTR modulator therapies are only available for a minority of the CF-patient population. Additionally, heterogeneity in in vivo modulator response has been reported among individuals carrying homozygous F508del-CFTR, adding to the desire for an optimal prediction of response-to-therapy on an individual level. In the last decade, a lot of progress has been made in the development of primary cell cultures into 3D patient-derived disease models. The advantage of these models is that the endogenous CFTR function is affected by the patient’s mutation as well as other genetic or environmental factors.
– In this review the authors focus on intestinal organoids as in vitro model for CF, enabling for CF disease classification, drug development and treatment optimization in a personalized manner, taking into account rare CFTR mutations and clinical heterogeneity among individuals with CF.
Corresponding author Prof. J M Beekman (fig 52) at the Department of Pediatric Respiratory Medicine, Wilhelmina Children’s Hospital, University Medical Center, Utrecht University.
Dedrick RM, Guerrero-Bustamante CA, Garlena RA, Russell DA, Ford K, Harris K, Gilmour KC, Soothill J, Jacobs-Sera D, Schooley RT, Hatfull GF, Spencer H. Engineered bacteriophages for treatment of a patient with a disseminated drug-resistant Mycobacterium abscessus. Nat Med. 2019 May;25(5):730-733. doi: 10.1038/s41591-019-0437-z. Epub 2019 May 8.[Pubmed]

Fig. 53 Robert Dedrick usf.edu
A 15-year-old patient with cystic fibrosis with a disseminated Mycobacterium abscessus infection was treated with a three-

Fig.54 Helen Spencer Great Ormond Street Hospital
phage cocktail following bilateral lung transplantation. Effective lytic phage derivatives that efficiently kill the infectious M. abscessus strain were developed by genome engineering and forward genetics. Intravenous phage treatment was well tolerated and associated with objective clinical improvement, including sternal wound closure, improved liver function, and substantial resolution of infected skin nodules
Dr Robert Dedrick (fig. 53) is Professor and Programme Coordinator, College of Education University of South Florida
Dr Helen Spencer (Fig. 54) is a Respiratory Paediatrician and has been clinical lead for the Lung Transplantation service at Great Ormond Street since 2007 where this patient was treated.
Denis A, Touzet S, Diabaté L, Durieu I, Lemonnier L, Poupon-Bourdy S, Iwaz J, Reynaud Q, Rabilloud M.Quantifying Long-term Changes in Lung Function and Exacerbations after Initiation of Azithromycin in Cystic Fibrosis. Ann Am Thorac Soc. 2019 Oct 11. doi: 10.1513/AnnalsATS.201812-882OC. [Epub ahead of print] [Pubmed]

Fig. 55 Angelique Denis
LinkedIn
The study sought to quantify the changes in lung function and the number of intravenous antibiotic courses after initiation of azithromycin in patients included in the French Cystic Fibrosis Registry. The study followed-up 1,065 children and 990 adults from 2 years before to 5 years after long-term azithromycin treatment initiated between 2001 and 2011. Mixed change-point models were used to quantify the changes in the forced expiratory volume in one second and the yearly number of intravenous antibiotic courses.
In the year of treatment initiation, the mean forced expiratory volume was significantly higher than expected (+1.6%, p=0.007 in children and +1.3%, p=0.02 in adults). The decline of the forced expiratory volume over time was less marked after than before treatment initiation (slope difference: +0.7% per year, p=0.03 in children and +0.6% per year, p=0.06 in adults). The mean increase in the yearly number of intravenous antibiotic courses was lower after than before treatment initiation. The rate ratio quantifying the effect on the mean increase was 0.93 (95% CI: [0.88; 0.99]; p=0.02) in children and 0.95 (95% CI: [0.90; 1.01]; p=0.08) in adults.
The authors concluded that in children, long-term azithromycin treatment was associated with immediate and sustained beneficial changes in lung function and sustained beneficial changes in the frequency of pulmonary exacerbations. In adults, it was associated with immediate beneficial changes in lung function.
Dr Angelique Denise (fig.55) is at the Centre Hospitalier Universitaire de Lyon, 26900, Pôle de Santé Publique, Lyon, Rhône-Alpes , France
Delatycki MB, Alkuraya F, Archibald A, Castellani C, Cornel M, Grody WW, Henneman L, Ioannides AS, Kirk E, Laing N, Lucassen A, Massie J, Schuurmans J, Thong MK, van Langen I, Zlotogora J. International perspectives on the implementation of reproductive carrier screening. Prenat Diagn. 2019 Nov 27. doi: 10.1002/pd.5611. [Epub ahead of print] [Pubmed]

Fig. 56 Martin Delatycki
Reproductive carrier screening started in some countries in the 1970s for hemoglobinopathies and Tay-Sachs disease. Cystic fibrosis carrier screening became possible in the late 1980s and with technical advances, screening of an ever increasing number of genes has become possible. The goal of carrier screening is to inform people about their risk of having children with autosomal recessive and X-linked recessive disorders, to allow for informed decision making about reproductive options. The consequence may be a decrease in the birth prevalence of these conditions, which has occurred in several countries for some conditions. Different programs target different groups (high school, premarital, couples before conception, couples attending fertility clinics, and pregnant women) as does the governance structure (public health initiative and user pays). Ancestry-based offers of screening are being replaced by expanded carrier screening panels with multiple genes that is independent of ancestry.
— This review describes screening in Australia, Cyprus, Israel, Italy, Malaysia, the Netherlands, Saudi Arabia, the United Kingdom, and the United States. It provides an insight into the enormous variability in how reproductive carrier screening is offered across the globe. This largely relates to geographical variation in carrier frequencies of genetic conditions and local health care, financial, cultural, and religious factors.
Professor Martin B Delatycki (fig.56) is Group Leader Genetics, Victorian Clinical Genetics Services, Parkville, Victoria, Australia.
Dentice R, Elkins MR, Verschuer J, Eberl S, Dwyer G, Bye PTP. Side lying during nebulisation can significantly improve apical deposition in healthy adults and adults with mild cystic fibrosis lung disease: a randomised crossover trial. BMC Pulm Med. 2019 Jul 16;19(1):128. doi: 10.1186/s12890-019-0886-7. [Pubmed]

Fig. 57 Ruth Dentice
eMedEvents
In people with and without Cystic Fibrosis (CF), does side lying during nebulisation change: the proportion of the dose loaded in the nebuliser that is deposited in the lungs; the uniformity of deposition throughout the lungs; or the apical drug density as a percentage of the drug density in the remaining lung? Do these effects differ depending on the degree of lung disease present?
A randomised crossover trial with concealed allocation, intention-to-treat analysis and blinded assessors, involving 39 adults: 13 healthy, 13 with mild CF lung disease (FEV1 > 80%pred), and 13 with more advanced CF lung disease (FEV1 < 80%pred). In random order, 4 mL of nebulised radioaerosol was inhaled in upright sitting and in alternate right and left side lying at 2-min intervals, for 20 min. Compared to sitting upright, lung deposition and the uniformity of deposition were not significantly altered by side lying in any of the three groups. In sitting, the density of the deposition was significantly less in the apical regions than in the rest of the lung in all participants. Side lying significantly improved apical deposition in healthy adults (MD, 13%; 95% CI, 7 to 19), and in minimal CF lung disease (MD, 4%; 95% CI, 1 to 7) but not in advanced disease (MD, 4%; 95% CI, - 2 to 9).
The authors concluded alternating between right and left side lying during nebulisation significantly improves apical deposition in healthy adults and in adults with mild CF lung disease, without substantial detriment to overall deposition.
Dr Ruth Dentice (fig. 57) is senior physiotherapist at the Royal Prince Alfred Hospital, Sydney, Australia.
Ditchfield N, Carroll WD, Gilchrist FJ. Unwarranted use of intravenous aminoglycosides at UK paediatric cystic fibrosis centres. J Cyst Fibros. 2019 Sep 12. pii: S1569-1993(19)30888-4. doi: 10.1016/j.jcf.2019.09.004. [Epub ahead of print] Corresponding author is F J Gilchrist [Pubmed]

Fig.58 Francis Gilchrist UHNM NHS Trust
All 27 UK CF Centres responded to the authors’ questionnaire to clarify under what circumstances IV aminoglycosides are prescribed for children in the UK. IV aminoglycosides are frequently used to treat infective exacerbations in CF due to efficacy against Pseudomonas (PA). The side effects of aminoglycosides include nephrotoxicity, ototoxicity and vestibulo-toxicity.
The authors found more than one third of UK CF centres use tobramycin to treat pulmonary exacerbations in children who have never isolated PA; also more than one half of UK CF centres use tobramycin to treat pulmonary exacerbations in children who have been free of PA for >12 months.
These authors suggest that IV aminoglycosides should be reserved for infective exacerbations in which PA is confirmed or strongly suspected. These drugs given additional benefit if in the absence of PA infection. They suggest than clinicians may lack confidence in the current diagnostic options to identify pulmonary PA infection. Given the proven sensitivity and feasibility of induced sputum and flexible bronchoscopy they advocate considering one of these investigations with an infective exacerbation unwell enough to warrant IV antibiotics with no identifiable organism. The authors suggest induced sputum or bronchoscopy prior to starting IV treatment
From Institute of Applied Science Keele University and the Academic Department of Child Health, University Hospitals of North Midlands NHS Trust, Stoke on Trent
Dr Francis Gilchrist (fig.58) is Senior Lecturer and Consultant in Paediatric Respiratory Medicine, University Hospitals of North Midlands.
— This is quite an alarming finding that IV tobramycin is being used to treat respiratory exacerbations not due to P. aeruginosa in people with cystic fibrosis as virtually all will eventually need aminoglycosides. However, the authors’ suggestion that tobramycin is one of the two antibiotics used, in patients where Pseudomonas in not identified, just in case there is also Pseudomonas present but not cultured is the most likely explanation. This report involves an important details of treatment of immediate and long term relevance to patient care – in contrast to the many scientific publications which now dominate the CF literature.
The published guidelines seem rather vague on the subject –
Guidelines – CF Trust Standards for the clinical care of children and adults with CF in the UK. 2nd Ed. Dec 2011
“Dual therapy is recommended for intravenous antibiotic courses (ß-lactam-based antibiotic with an aminoglycoside)”.
Guidelines – Antibiotic treatment for cystic fibrosis. Third ed. May 2009
“For organisms other than P.aeruginosa a single agent may be appropriate. For P.aeruginosa, a combination of 2 antibiotics with a different mechanism of action should be used for intravenous treatment in CF patients. Ceftazidime and tobramycin are commonly used but meropenem and colistin is a suitable alternative combination”.
ECFS best practice guidelines: the 2018 revision
“For P. aeruginosa, a combination of two or more antibiotics is recommended and, although evidence for choice of antibiotics and optimal treatment duration is lacking”
Dogru D, Çakır E, Şişmanlar T, Çobanoğlu N, Pekcan S, Cinel G, et al. Cystic fibrosis in Turkey: First data from the national registry.Author information. Pediatr Pulmonol. 2019 Nov 11. doi: 10.1002/ppul.24561. [Epub ahead of print]. [Pubmed]

Fig 59 Deniz Dogru
averse.hacettepe.edu.tr
Cystic fibrosis (CF) care has been implemented in Turkey for a long time; however, there had been no patient registry. For this purpose, the Turkish National CF Registry was established. The authors present the first results of registry using data collected in 2017. The data were collected using a data-entry software system, which was accessed from the internet. Demographic and annually recorded data consisted of 15 and 79 variables, respectively.
There were 1170 patients registered from 23 centers; the estimated coverage rate was 30%. The median age at diagnosis was 1.7 years (median current age: 7.3 years); 51 (4.6%) patients were aged over 18 years. Among 293 patients who were under 3 years of age, 240 patients (81.9%) were diagnosed through newborn screening. Meconium ileus was detected in 65 (5.5%) patients. Genotyping was performed in 978 (87.4%) patients and 246 (25.2%) patients’ mutations were unidentified. The most common mutation was deltaF508 with an allelic frequency of 28%, followed by N1303K (4.9%). The median FEV1% predicted was 86. Chronic colonization with Pseudomonas aeruginosa was seen in 245 patients. The most common complication was pseudo-Bartter syndrome in 120 patients. The median age of death was 13.5 years in a total of 15 patients.
The authors comment on the low coverage rate, lack of genotyping, unidentified mutations, and missing data of lung functions are some of their greatest challenges. Including data of all centers and reducing missing data will provide more accurate data and help to improve the CF care in Turkey in the future.
— It must be said that the results are strikingly different from some of the other European countries for example UK CF Registry 2018 the results of which are bracketed after the Turkish figures. Total number 1170 (10508), median age at diagnosis 1.7 years (2 months), current median age 7.3years (20 years), percentage over 18 years 4.6% (16 years and over 60.4%), median age at death 13.5 years (32 years). There was a surprisingly high incidence of pseudo-Bartter’s syndrome in 120 patients presumably related to the warm climate.
Deniz Dogru (fig 59) is professor in the Division of Pediatric Pulmonology, Faculty of Medicine, Hacettepe University, Ankara, Turkey and the other CF units in Turkey.
— The development of a nationwide CF patient registry is a long job, as we found in the UK. It is good that a start has been made in Turkey for an accurate patient registry is absolutely essential.
Carzino R, Frayman KB, King L, Vidmar S, Ranganathan S; AREST CF. Regional differences in infection and structural lung disease in infants and young children with cystic fibrosis. J Cyst Fibros. 2019 Nov 6. pii: S1569-1993(19)30933-6. doi: 10.1016/j.jcf.2019.10.018. [Epub ahead of print]. [Pubmed]

Fig. 60 Rosemary Carzino.Wal-yan Respiratory Research
Both infection and inflammation are critical to the progression of cystic fibrosis (CF) lung disease. Potential anatomical differences in lower airway infection, inflammation and bronchiectasis in young children with CF raise questions regarding the pathogenesis of early structural lung disease.
A longitudinal multi-centre birth cohort study of infants newly diagnosed with CF was conducted. Paired bronchoalveolar lavage (BAL) samples were obtained from the right middle lobe (RML) and lingula bronchi. Chest computed tomography (CT) was performed biennially and analysed using the modified CF-CT scoring system.
One hundred and twenty-four children (0.11 – 7.0 years) contributed 527 BAL samples and underwent 388 CT chest scans.
Pro-inflammatory microbes were detected in 279 BAL samples (53%), either in both lingula and RML samples (69%), in the lingula alone (24%), or in the RML alone in only 7% of samples. Overall, the prevalence of structural lung disease was greater in the setting of pro-inflammatory microbes. Although infection was less commonly isolated in the right lung, bronchiectasis was more commonly detected in the right lung compared with the left. No anatomical differences in the presence of air trapping were detected.
The authors concluded overall, the detection of pro-inflammatory microbes in the lower airways was associated with increased risk of both air trapping and bronchiectasis. However, the apparent discordance between commonest sites of isolation of pro-inflammatory microbes and the anatomical site of early bronchiectasis warrants further exploration.
Dr Rosemary Carzino (fig.60) is a Senior Research Assistant in the Respiratory Diseases Group, Murdoch Children’s Research Institute, Victoria, Australia.
Doyle RM, Rubio M, Dixon G, Hartley J, Klein N, Coll P, Harris KA. Cross- infection is not the source of new Mycobacterium abscessus infections in a multi-centre cohort of cystic fibrosis patients. Clin Infect Dis. 2019 Jun 19. pii: ciz526. doi: 10.1093/cid/ciz526. [Epub ahead of print] [Pubmed]

Fig 61 Ronan Doyle lshtm.ac.uk
Mycobacterium abscessus is an extensively drug resistant pathogen that causes pulmonary disease particularly in cystic fibrosis (CF) patients. Identifying direct patient-to-patient transmission of M. abscessus is critically important in directing infection control policy for the management of risk in CF patients. A variety of clinical labs have used molecular epidemiology to investigate transmission. However there is still conflicting evidence as to how M. abscessus is acquired and whether cross-transmission occurs. Recently labs have applied whole-genome sequencing (WGS) to investigate this further and in this study we investigate whether WGS can reliably identify cross-transmission in M. abscessus. These authors retrospectively sequenced the whole genomes of 145 M. abscessus isolates from 62 patients seen at four hospitals in two countries over 16 years. They showed that a comparison of a fixed number of core single nucleotide variants (SNVs) alone cannot be used to infer cross-transmission in M. abscessus but does provide enough information to replace multiple existing molecular assays. They detected one episode of possible direct patient-to-patient transmission in a sibling pair. We found that patients acquired unique M. abscessus strains even after spending considerable time on the same wards with other M. abscessus positive patients.They concluded this novel analysis has demonstrated that the majority of patients in this study have not acquired M. abscessus through direct patient-patient transmission or a common reservoir. Tracking transmission using WGS will only realise its full potential with proper environmental screening as well as patient sampling.
Dr Ronan Doyle (fig 61) is Assistant Professor in the Department of Clinical Research, the London School of Hygiene and Tropical Medicine.
Ehre C, Rushton ZL, Wang B, Hothem LN, Morrison CB, Fontana NC, Markovetz MR, Delion MF, Kato T, Villalon D, Thelin WR, Esther CR Jr, Hill DB, Grubb BR, Livraghi-Butrico A, Donaldson SH, Boucher RC. An Improved Inhaled Mucolytic to Treat Airway Muco-obstructive Diseases. Am J Respir Crit Care Med. 2019 Jan 15;199(2):171-180. doi: 10.1164/rccm.201802-0245OC
-

Fig. 62 Camille Ehre UNC School of Medicine
Mucins, the dominant biopolymer in mucus, organize into complex polymeric networks via the formation of covalent disulfide bonds, which govern the viscoelastic properties of the mucus gel. For decades, inhaled N-acetylcysteine (NAC) has been used as a mucolytic to reduce mucin disulfide bonds with little, if any, therapeutic effects. Improvement of mucolytic therapy requires the identification of NAC deficiencies and the development of compounds that overcome them.
The objectives of this study to elucidate the pharmacological limitations of NAC and test a novel mucin-reducing agent, P3001, in preclinical settings.
The study used biochemical (e.g., Western blotting, mass spectrometry) and biophysical assays (e.g., microrheology/macrorheology, spinnability, mucus velocity measurements) to test compound efficacy and toxicity in in vitro and in vivo models and patient sputa.
Dithiothreitol and P3001 were directly compared with NAC in vitro and both exhibited superior reducing activities. In vivo, P3001 significantly decreased lung mucus burden in βENaC-overexpressing mice, whereas NAC did not (n = 6-24 mice per group). In NAC-treated CF subjects (n = 5), aerosolized NAC was rapidly cleared from the lungs and did not alter sputum biophysical properties. In contrast, P3001 acted faster and at lower concentrations than did NAC, and it was more effective than DNase in CF sputum ex vivo.
The authors consider these results suggest that reducing the viscoelasticity of airway mucus is an achievable therapeutic goal with P3001 class mucolytic agents.
Dr Camille Ehre (fig 62) is assistant Professor at the Marsico Lung Institute.
Eickmeier O, Zissler UM, Wittschorek J, Unger F, Schmitt-Grohé S, Schubert R, Herrmann E, Zielen S. Clinical relevance of Aspergillus fumigatus sensitization in cystic fibrosis. Clin Exp Allergy. 2019 Dec 30. doi: 10.1111/cea.13557. [Epub ahead of print] [Pubmed]

Fig. 63 Olaf Eickmeier
The clinical relevance of sensitization to Aspergillus (A) fumigatus in cystic fibrosis (CF) is unclear. Some researchers propose that specific A. fumigatus IgE is an innocent bystander, whereas others describe it as the major cause of TH-2-driven asthma-like disease. The authors aimed to ascertain whether allergen exposure to A. fumigatus by bronchial allergen provocation (BAP) induces TH-2 inflammation comparable to an asthma-like disease.
A total of 35 patients, aged 14.8±8.5 years, and 20 healthy controls were investigated prospectively. The patients were divided into two groups: group 1 (n=18): specific (s)IgE negative, and group 2 (n=17): sIgE positive (≥ 0.7 KU/L) for A. fumigatus. Lung function, exhaled NO, and induced sputum were analysed. All sensitized patients with an FEV1 > 75% (n=13) underwent BAP with A. fumigatus, and cell counts, and the expression of IL-5, IL-13, INF-γ, and IL-8 as well as transcription factors T-bet, GATA-3, and FoxP3, were measured. Results: Lung function parameters decreased significantly compared to controls, but not within the CF patient group. After bronchial allergen provocation, 8 of 13 patients (61%) had a significant asthmatic response and increased eNO 24 hours later. In addition, marked TH-2-mediated inflammation involving eosinophils, IL-5, IL-13, and FoxP3 became apparent in induced sputum cells.
The authors conclude their study demonstrated the clinical relevance of A. fumigatus for the majority of sensitized CF patients. A distinct IgE/TH-2-dominated inflammation was found in induced sputum after A. fumigatus exposure.
Dr Olaf Eickmeier (fig.63) is in the Department for Children and Adolescents, Division of Allergology, Pulmonology and Cystic fibrosis, Goethe University, Frankfurt.
Ellemunter H, Steinkamp G. Lung clearance index to detect the efficacy of Aztreonam lysine inhalation in patients with cystic fibrosis and near normal spirometry – A single-centre feasibility study.PLoS One. 2019 Sep 9;14(9):e0221673. doi: 10.1371/journal.pone.0221673. eCollection 2019. Free full text [Pubmed]

Fig. 64 Helmut Ellemunter seltenekrankheit.info
Comparing the efficacy of inhaled antibiotics can be difficult in small groups of patients with cystic fibrosis and mild lung disease. In a feasibility study we compared Aztreonam lysine for inhalation solution (AZLI; Cayston®) to standard inhaled antibiotic therapy in patients with cystic fibrosis and near normal spirometry. To detect treatment responses we used both lung clearance index (LCI) and forced expiratory volume in one second (FEV1). At baseline, median FEV1 was 87% pred. and median LCI was 8.6 (upper limit of normal: 7.0). After 4 weeks, LCI improved by -0.36 after AZLI and deteriorated by +0.12 after tobramycin treatment (p= 0.039). No significant differences between treatments (p = 0.195) were observed using FEV1
These results suggest that lung clearance index can be used to detect treatment induced changes in subjects with mild lung disease.
Dr Helmut Ellemunter (fig.64) is at the Cystic Fibrosis (CF) Centre at the Medical University of Innsbruck, Innsbruck, Austria.
Engel TGP, Erren E, Vanden Driessche KSJ, Melchers WJG, Reijers MH, Merkus P, Verweij PE. Aerosol Transmission of Aspergillus fumigatus in Cystic Fibrosis Patients in the Netherlands. Emerg Infect Dis. 2019 Apr;25(4):797-799. doi: 10.3201/eid2504.181110. [Pubmed] Free PMC Article

Fig 65 Tobias Engel
The authors collected sputum samples and cough plates from 15 cystic fibrosis patients in the Netherlands who were colonized with Aspergillus fumigatus; we recovered A. fumigatus of the same genotype in cough aerosols and sputum samples from 2 patients. The belief that transmission of A. fumigatus from cystic fibrosis patients does not occur should be reconsidered.
Tobias G.P. Engel (fig.65) is currently in a residency with a PhD programme at Radboud University Medical Center, Department of Medical Microbiology, Route 777, Geert Grooteplein Zuid 10, 6500 HB Nijmegen, the Netherlands;
Esther CR Jr, Muhlebach MS, Ehre C, Hill DB, Wolfgang MC, Kesimer M, Ramsey KA, Markovetz MR, Garbarine IC, Forest MG, Seim I, Zorn B, Morrison CB, Delion MF, Thelin WR, Villalon D, Sabater JR, Turkovic L, Ranganathan S, Stick SM, Boucher RC. Mucus accumulation in the lungs precedes structural changes and infection in children with cystic fibrosis. Sci Transl Med. 2019 Apr 3;11(486). pii: eaav3488. doi: 10.1126/scitranslmed.aav3488. [Pubmed]

Fig. 66 Charles Esther med.unc.edu
Although destructive airway disease is evident in young children with cystic fibrosis (CF), little is known about the nature of the early CF lung environment triggering the disease.
To elucidate early CF pulmonary pathophysiology, the authors performed mucus, inflammation, metabolomic, and microbiome analyses on bronchoalveolar lavage fluid (BALF) from 46 preschool children with CF enrolled in the Australian Respiratory Early Surveillance Team for Cystic Fibrosis (AREST CF) program and 16 non-CF disease controls.
Total airway mucins were elevated in CF compared to non-CF BALF irrespective of infection, and higher densities of mucus flakes containing mucin 5B and mucin 5AC were observed in samples from CF patients. Total mucins and mucus flakes correlated with inflammation, hypoxia, and oxidative stress. Many CF BALFs appeared sterile by culture and molecular analyses, whereas other samples exhibiting bacterial taxa associated with the oral cavity. Children without computed tomography-defined structural lung disease exhibited elevated BALF mucus flakes and neutrophils, but little/no bacterial infection. Although CF mucus flakes appeared “permanent” because they did not dissolve in dilute BALF matrix, they could be solubilised by a previously unidentified reducing agent (P2062), but not by N-acetylcysteine or deoxyribonuclease.
— There is a long discussion on the significance of these findings in the full article available via the PubMed link
Charles Esther (fig.66) is professor in the Division of Pediatric Pulmonology, University of North Carolina at Chapel Hill, Chapel Hill, NC 27599, USA. and at the Marsico Lung Institute, University of North Carolina at Chapel Hill, Chapel Hill, NC 27599, USA.
Ferrera L, Baroni D, Moran O. Lumacaftor-rescued F508del-CFTR has a modified bicarbonate permeability. J Cyst Fibros. 2019 Feb 6. pii: S1569-1993(18)30927-5. doi: 10.1016/j.jcf.2019.01.012. [Epub ahead of print] [Pubmed]

Fig. 67 Loretta Ferrera
ffc
Deletion of phenylalanine at position 508, F508del, the most frequent mutation among Cystic fibrosis (CF) patients, destabilizes the protein, thus causing both a folding and a trafficking defect, resulting in a dramatic reduction in expression of CFTR. In vitro treatment with lumacaftor produces an enhancement of anion transport in cells. We studied the permeability properties of the CFTR mutant F508del treated with the corrector lumacaftor, showing that the rescued protein has selectivity properties different than the wild type CFTR, showing an augmented bicarbonate permeability. This difference would indicate a diverse conformation of the rescued F508del-CFTR, that is plausibly reflected on an improper regulation of the airway surface liquid, lessening the efficacy of the corrector. Our findings rather support the idea that a combination of correctors would be required to address the CFTR-dependent bicarbonate permeability.
Loretta Ferrera (fig.67) is a researcher at the Istituto Giannina Gaslini, U.O.C. Genetica Medica, Genova, Italy.
The authors suggest these findings indicate that early CF lung disease is characterized by an increased mucus burden and inflammatory markers without infection or structural lung disease and suggest that mucolytic and anti-inflammatory agents should be explored as preventive therapy.
– An interesting combined contribution to the increasing work to understand early lung changes in CF
Fink AK, Graff G, Byington CL, Loeffler DR, Rosenfeld M, Saiman L. Palivizumab and Long-term Outcomes in Cystic Fibrosis. Pediatrics. 2019 Jun 25. pii: e20183495. doi: 10.1542/peds.2018-3495. [Epub ahead of print] [Pubmed]

Fig. 68 Aliza Fink cff.org
The American Academy of Pediatrics does not recommend routine use of palivizumab prophylaxis for infants with cystic fibrosis (CF) but recommends consideration in infants with clinical evidence of chronic lung disease or nutritional compromise. However, the beneficial impact of palivizumab on longer-term outcomes is uncertain.
The authors used Cystic Fibrosis Foundation Patient Registry data to assess the association of receiving palivizumab during the first 2 years of life with longer-term outcomes, including lung function at 7 years old, time to first positive Pseudomonas respiratory culture, and pulmonary-related hospitalisations during the first 7 years of life. Eligible infants were born from 2008 to 2015 and diagnosed with CF during the first 6 months of life. Demographic and clinical confounders of association between palivizumab receipt and outcomes were explored. We created propensity scores to adjust for potential confounding by indication (ie, sicker infants were more likely to receive palivizumab). For each outcome, we performed regression analyses adjusted by propensity scores.
The sample included 4267 infants; 1588 (37%) received palivizumab. Mean percent forced expiratory volume in 1 second predicted at 7 years old was similar among those who did (98.2; 95% confidence interval: 96.9-99.5) and did not (97.3; 95% confidence interval: 96.1-98.5) received palivizumab, adjusting for propensity scores. Time to first positive Pseudomonas aeruginosa culture and annual risk of hospitalisation were similar among those who did and did not receive palivizumab.
The authors concluded at the population level, palivizumab receipt was not associated with improved longer-term outcomes in children with CF.
Dr Aliza K Fink (Fig 68) is an epidemiologist with the CF Foundation involved with Patient Registry research.
Freeman AJ, Sellers ZM, Mazariegos G, Kelly A, Saiman L, Mallory G, Ling SC, Narkewicz MR, Leung DH. A multi-disciplinary approach to pre and post-transplant management of cystic fibrosis associated liver disease. Liver Transpl. 2019 Jan 29. doi: 10.1002/lt.25421. [Epub ahead of print][Pubmed]

Fig. 69 Alvin J Freeman
US News Health
Approximately 5 to 10% of patients with cystic fibrosis (CF) will develop advanced liver disease with portal hypertension, representing the 3rd leading cause of death among patients with CF. CF liver disease (CFLD) represents the most significant risk to patient mortality second only to pulmonary or lung transplant complications in patients with CF. Currently there is no medical therapy to treat or reverse CFLD.
Liver transplantation in patients with CFLD with portal hypertension confers a significant survival advantage over those who do not receive LT, although the timing in which to optimize this benefit is unclear. Despite the value and efficacy of LT in selected patients with CFLD, established clinical criteria outlining indications and timing for LT, as well as disease specific transplant considerations are notably absent.
The goal of this comprehensive and multi-disciplinary report is to present recommendations on the unique CF-specific pre- and post-LT management issues clinicians should consider and will face.
Alvin Jay Freeman (fig.69) is Pediatric Hepatologist at Department of Pediatrics, Emory University School of Medicine, Atlanta, GA.and the Division of Pediatric Gastroenterology, Hepatology and Nutrition, Children’s Healthcare of Atlanta, Atlanta, GA.
Corresponding author is Daniel H Leung Acting Director, Pediatric Hepatology and Liver Transplant Medicine Texas Chidren’s Hospital and Associate Professor of Pediatrics, Baylor College of Medicine
Frost FJ, Nazareth DS, Charman SC, Winstanley C, Walshaw MJ. Ivacaftor Is Associated with Reduced Lung Infection by Key Cystic Fibrosis Pathogens: A Cohort Study Using National Registry Data. Ann Am Thorac Soc. 2019 Jul 19. doi: 10.1513/AnnalsATS.201902-122OC. [Epub ahead of print] [Pubmed] Retrospective cohort study utilising data from the United Kingdom CF Registry 2011-2016. Primary outcome was the annual prevalence ratios for key CF pathogens between ivacaftor users and their contemporaneous comparators. Multivariate log-binomial regression models were designed to adjust for confounders. Changes in Pseudomonas aeruginosa status were compared between groups using non-parametric maximum likelihood estimate for the purposes of Kaplan-Meier approximation.
Ivacaftor use was associated with early and sustained reduction in P. aeruginosa rates (2016 Adjusted Prevalence Ratio [95% CI] 0.68 [0.58, 0.79], p<0.001) via a combination of increased clearance in those with infection (Ivacaftor: 33/87 [37.9%] vs. Non ivacaftor: 432/1872 [22.8%], p<0.001) and reduced acquisition in those without infection (33/134 [24.6%] vs. 1157/2382 [48.6%], p=0.01). The improved prevalence of P. aeruginosa infection was independent of reduced sampling in the ivacaftor cohort. Ivacaftor was also associated with reduced prevalence of Staphylococcus aureus and Aspergillus spp. but not Burkholderia cepacia complex.
The authors concluded that in this study, long-term ivacaftor use was associated with reduced infection with important CF pathogens including P. aeruginosa. These findings have implications for antibiotic stewardship and the need for on-going chronic antimicrobial therapy in this cohort.
– Expected results confirmed with UK CF Registry data.
- Fig. 70 Martin Walshaw
- Fig. 71 Craig Winstaley
- Fig.72 Susan Charman
- Fig.73 Dilip Nazareth
- Fig. 74 Freddy frost
Dr Freddy Frost (fig.74) is an MD student at the Institute of Infection and Global Health, Liverpool.
Dr Dilip Nazareth Fig. 73 is Consultant Pulmonologist, Liverpool.
Dr Susan Charman (fig 72)is Senior Statistician at the UK Cystic Fibrosis Trust Registry. Professor Graig Winstanley(fig.71) is Professor of Clinical Infection, Microbiology and Immunology, Liverpool. Professor Martin Walshaw (fig.70) is pulmonologist and Director (and founder) of the Regional Liverpool Adult CF Centre
Garbuzenko OB, Bah N, Kuzmov A, Pogrebnyak N, Pozharov V, Minko T.Inhalation treatment of cystic fibrosis with lumacaftor and ivacaftor co-delivered by nanostructured lipid carriers. J Control Release. 2019 Jan 21;296:225-231. doi: 10.1016/j.jconrel.2019.01.025. [Epub ahead of print] [Pubmed]
-

Fig. 75 Olga Garbuzenko
- Based on their extensive experience in inhalation delivering of drugs by different nanocarriers, the authors selected nanostructured lipid carriers (NLC) for the delivery both drugs directly to the lungs by inhalation and tested NLC loaded with drugs in vitro (normal and CF human bronchial epithelial cells) and in vivo (homozygote/homozygote bi-transgenic mice with CF). The results show that the designed NLCs demonstrated a high drug loading efficiency and were internalized in the cytoplasm of CF cells. It was found that NLC-loaded drugs were able to restore the expression and function of CFTR protein. As a result, the combination of lumacaftor and ivacaftor delivered by lipid nanoparticles directly into the lungs was highly effective in treating lung manifestations of cystic fibrosis
Dr Olga Garbuzenko (fig 75) is Assistant Research Professor, Ernest Mario School of Pharmacy, Piscataway NJ
Garah J, Rosen I, Shaoul R.Transient Exocrine Pancreatic Insufficiency in Children: An Existing Entity? J Pediatr Gastroenterol Nutr. 2019 Jan 8. doi: 10.1097/MPG.0000000000002267. [Epub ahead of print] [Pubmed]

Fig. 76 Ron Shaoul
LinkedIn
Pancreatic insufficiency in children is usually associated with diseases such as cystic fibrosis, Shwachman-Diamond syndrome, or chronic pancreatitis. Fecal elastase-1 is a reliable laboratory test for the diagnosis of exocrine pancreatic insufficiency (EPI). Transient pancreatic insufficiency has been rarely described and data on this entity are lacking in the medical literature. In this retrospective study we report 17 cases of transient pancreatic insufficiency presented mainly with failure to thrive and/or diarrhoea.
The authors followed 43 children (age range 1 month-18 years) with low fecal elastase-1 between the years 2009 and 2017. We followed growth and laboratory results (particularly, complete blood count, albumin, transaminases, celiac serology, sweat test, and fat-soluble vitamins). Elastase levels <200 mg/g were considered as pancreatic insufficiency.
Twenty-six were excluded due to missing data, a comorbidity or being syndromatic. Enrolled children (17) were all otherwise healthy. The median age at diagnosis was 3 years (range 0.2-15 years), 11 girls and 6 boys. Their main presenting symptoms were failure to thrive and/or diarrhea. Median fecal elastase-1 levels were 71 mg/g (range 18-160). Median time for normalization was 6 months (range 1-48 months). Abdominal sonography, celiac serology, and sweat test were normal for all patients. Most patients were treated with pancreatic enzymes until resolution.
The authors concluded transient EPI without clear aetiology should be in the differential diagnosis of EPI after ruling out known aetiologies. The resolving course pattern may be attributed to an unidentified infectious agent. Further studies to assess the aetiology are mandated.
— Unfortunately I was unable to obtain the full text of this article but one wonders if the transient pancreatic insufficiency was caused by the “failure to thrive and diarrhoea “ rather than it causing the symptoms. Transient pancreatic insufficiency has been described in children with coeliac disease where the pancreatic insufficiency is caused by the malnutrition and it is reversed when the coeliac disease is treated.
Corresponding author: Dr Ron Shaoul (Fig. 76) Director Pediatric Gastroenterology and Nutrition Institute, Ruth Children’s Hospital Haifa, Rambam Medical Center, Israel.
Gardner AI, McClenaghan E, Saint G, McNamara PS, Brodlie M, Thomas MF. Epidemiology of Nontuberculous Mycobacteria Infection in Children and Young People With Cystic Fibrosis: Analysis of UK Cystic Fibrosis Registry. Clin Infect Dis. 2019 Feb 15;68(5):731-737. doi: 10.1093/cid/ciy531. [PubMed]

Fig. 77 Aaron Gardner Gene Food
Data from 2010-2015 for individuals aged <16 years (23200 observations from 5333 unique individuals) were obtained. Univariate analysis of unique individuals comparing all key clinical factors and health outcomes to NTM status was performed. The significant factors that were identified were used to generate a multivariate logistic regression model that, following step-wise removal, generated a final parsimonious model.The prevalence of individuals with a NTM-positive respiratory culture increased every year from 2010 (45 [1.3%]) to 2015 (156 [3.8%]). Allergic bronchopulmonary aspergillosis (odds ratio [OR], 2.66; P = 5.0 × 10-8), age (OR, 1.08; P = 3.4 × 10-10), and intermittent Pseudomonas aeruginosa infection (OR, 1.51; P = .004) were significantly associated with NTM infection.
Dr Aaron Gardner (fig 77) is a PostDoc Research Associate at the Institute of Cellular Medicine, Newcastle University Medcial School Newcastle upon Tyne.
Garg V, Shen J, Li C, Agarwal S, Gebre A, Robertson S, Huang J, Han L, Jiang L, Stephan K, Wang LT, Lekstrom-Himes J. Pharmacokinetic and Drug-Drug Interaction Profiles of the Combination of Tezacaftor/Ivacaftor.Clin Transl Sci. 2019 May;12(3):267-275. doi: 10.1111/cts.12610. Epub 2019 Jan 29.[PubMed] Free PMC Article
Drug-drug interaction (DDI) studies are described for tezacaftor/ivacaftor, a new cystic fibrosis transmembrane conductance regulator modulator therapy for the treatment of cystic fibrosis. Three phase I DDI studies were conducted in healthy subjects to characterize the DDI profile of tezacaftor/ivacaftor with cytochrome P450 (CYP)3A substrates, CYP3A inhibitors, and a permeability glycoprotein (P-gp) substrate. The effects of steady-state tezacaftor/ivacaftor on the pharmacokinetics (PKs) of digoxin (a P-gp substrate), midazolam, and ethinyl estradiol/norethindrone (CYP3A substrates) were evaluated. Effects of strong (itraconazole) and moderate (ciprofloxacin) CYP3A inhibitors on tezacaftor/ivacaftor PKs were also determined. Tezacaftor/ivacaftor increased digoxin area under the curve (AUC) by 30% but did not affect midazolam, ethinyl estradiol, or norethindrone exposures. Itraconazole increased the AUC of tezacaftor 4-fold and ivacaftor 15.6-fold. Ciprofloxacin had no significant effect on tezacaftor or ivacaftor exposure. Coadministration of tezacaftor/ivacaftor may increase exposure of sensitive P-gp substrates. Tezacaftor/ivacaftor is unlikely to impact exposure of drugs metabolized by CYP3A, including hormonal contraceptives. Strong CYP3A inhibitors significantly increase the exposures of tezacaftor and ivacaftor.
Varun Garg is a Vice President at Vertex Pharmaceuticals Incorporated, Boston, Massachusetts, USA.
Gifford AH, Mayer-Hamblett N, Pearson K, Nichols DP. Answering the call to address cystic fibrosis treatment burden in the era of highly effective CFTR modulator therapy. J Cyst Fibros. 2019 Nov 21. pii: S1569-1993(19)30971-3. doi: 10.1016/j.jcf.2019.11.007. [Epub ahead of print] [PubMed]

Fig. 78 Alex H Gifford US News Health
The authors recognise an unprecedented opportunity to study the effects of withdrawing one or more chronic treatments in people with CF (PwCF) who benefit greatly from CFTR modulator therapy, but feasibility and acceptance of such a study within the community is unknown. They surveyed PwCF, their families, and their acquaintances between November 16, 2018, and December 2, 2018, and CF clinicians between December 19, 2018, and January 2, 2019, about treatment withdrawal research. They sought feedback from these groups about their level of interest in this research, the consistency with which they were taking modulator and non-modulator treatments, the ways in which they conceptualized health changes, and what chronic non-modulator treatments they were most interested in stopping. We also asked for stakeholder perspectives on the design of a treatment withdrawal trial, but we intend to report these perspectives elsewhere.
Eighty percent (541/675) of CF community respondents and 95% (206/218) of CF clinicians said that a trial of treatment simplification should be performed in the context of highly effective modulator therapy. Most current CFTR modulator users (292/359, 81%) have not stopped another chronic treatment. Worsening lung function by spirometry or increased daily symptoms were important health indicators. PwCF, their families, and/or their acquaintances ranked airway clearance techniques and inhaled antibiotics as the most burdensome treatments.
There is considerable support among the CF community and CF clinicians in the U.S. for controlled trials to assess the safety and impact of treatment simplification in patients taking highly effective modulator therapy.
Alex H Gifford (fig. 78) is Associate Professor of `Medicine and Director of the Adult Cystic Fibrosis program at Dartmouth-Hitchcock Medical Center, NH, Lebanon, USA; The Dartmouth Institute for Health Policy and Clinical Practice, NH, Lebanon, USA.
— This is an interesting time and it is timely to discuss treatment withdrawal which will require considerable thought and individual variation. PwCF who have already passed the “point of no return” and whose lungs have now entered a slow but relentless deterioration due chronic infection and established damaging inflammation irrespective of CFTR activity, will be less likely to be appropriate for stopping some conventional treatments. Further experience is awaited with interest.
Giordani B, Amato A, Majo F, Ferrari G, Quattrucci S, Minicucci L, Padoan R, Floridia G, Salvatore D, Carnovale V, Puppo Fornaro G, Taruscio D, Salvatore M; Gruppo di lavoro RIFC.[Italian Cystic Fibrosis Registry (ICFR). Report 2015-2016].Collaborators (63) (Italian). Epidemiol Prev. 2019 Jul-Aug;43(4S1):1-36. doi: 10.19191/EP19.4.S1.067.Free Full Text [PubMed]
On the 27th of October 2017 the National Center for Rare Diseases of the Italian National Health Institute (NHI), clinicians of the Italian National Referral and Support Centres for Cystic Fibrosis, Paediatric Hospital “Bambino Gesù”, Italian Cystic Fibrosis Society, and the Italian League for Cystic Fibrosis renewed the agreement about FC data flow for a 3 years period. The possibility to access data by third parties is among the most important new introduced within the agreement.
The present Report shows that Italian CF population is growing (median age) and paediatric mortality is decreasing. A very low percentage of paediatric population is characterized by complication of pulmonary function; adult patients are characterized by an increase of age at death (more than 36 years of age in 2016).
— Although the full text is in Italian, the PubMed abstract is very detailed and makes interesting reading.
Barbara Giordani is with Lega italiana fibrosi cistica ONLUS Roma
Goetz D, Kopp BT Salvator A, Moore-Clingenpeel M, McCoy K, Leung DH, Kloster M, Ramsey BR, Heltshe SH, Borowitz D.Pulmonary findings in infants with cystic fibrosis during the first year of life: Results from the Baby Observational and Nutrition Study (BONUS) cohort study. Pediatr Pulmonol. 2019 Jan 22. doi: 10.1002/ppul.24261. [Epub ahead of print] [Pubmed]
-

Fig. 79 Danielle Goetz ResearchGate
- To report observations about pulmonary correlates of growth and other clinical features in infants with CF. The authors analysed data from the prospective Baby Observational and Nutrition Study conducted in 28 centers across the US, including clinical features, medications, guardian diaries of respiratory symptoms, oropharyngeal swab cultures and chest radiographs (CXR) collected over the first year of life.
Cough was reported in 84% of infants in the first year. Up to 30% had clinically important cough but only 6.3% had crackles; 16.5% had wheeze. Wisconsin CXR score was above 5 in 23% (normal = 0; maximum score = 100). Pseudomonas was recovered from at least one respiratory culture in 24% of infants and was associated with crackles/wheezes and use of proton pump inhibitors (PPI) (OR = 5.47; 95%CI = 1.36, 21.92; P = 0.02) or PPI plus histamine-2 (H2) blocker (OR = 8.2; 95%CI = 2.41, 27.93; P = 0.001), but not H2 blocker alone. Hospitalization for respiratory indications occurred in 18% of infants and was associated with crackles/wheeze and abnormal CXR but not low weight, Pseudomonas or use of acid blockade.
Conclusions were that cough is common in infants with CF, but few present with crackles/wheeze or CXR changes. Pseudomonas is associated with use of PPI or PPI plus H2 blocker, but not with respiratory hospitalization. These observations cannot prove cause and effect but add to our understanding of pulmonary manifestations of CF in infants
Dr Danielle Goetz (Fig. 79) is paediatric Pulmonologist in the Dept. of Pediatrics, Jacobs School of Medicine, University of Buffalo.
Gomez CCS, Parazzi PLF, Clinckspoor KJ, Mauch RM, Pessine FBT, Levy CE, Peixoto AO, Ribeiro MÂGO, Ribeiro AF, Conrad D, Quinton PM, Marson FAL, Ribeiro JD. Safety, Tolerability, and Effects of Sodium Bicarbonate Inhalation in Cystic Fibrosis. Clin Drug Investig. 2019 Nov 13. doi: 10.1007/s40261-019-00861-x. [Epub ahead of print] [Pubmed]

Fig.80 Carla C S Gomez ResearchGate
Among the many consequences of loss of CFTR protein function, a significant reduction of the secretion of bicarbonate (HCO3-) in cystic fibrosis (CF) is a major pathogenic feature. Loss of HCO3- leads to abnormally low pH and impaired mucus clearance in airways and other exocrine organs, which suggests that NaHCO3 inhalation may be a low-cost, easily accessible therapy for CF.
To evaluate the safety, tolerability, and effects of inhaled aerosols of NaHCO3 solutions (4.2% and 8.4%) an experimental, prospective, open-label, pilot, clinical study was conducted with 12 CF volunteer participants over 18 years of age with bronchiectasis and pulmonary functions classified as mildly to severely depressed. Sputum rheology, pH, and microbiology were examined as well as spirometry, exercise performance, quality-of-life assessments, dyspnea, blood count, and venous blood gas levels.
The sputum pH increased immediately after inhalation of NaHCO3 at each clinical visit and was inversely correlated with rheology when all parameters were evaluated: [G’ (elasticity of the mucus) = - 0.241; G″ (viscosity of the mucus) = - 0.287; G* (viscoelasticity of the mucus) = - 0.275]. G* and G’ were slightly correlated with peak flow, forced expiratory volume in 1 s (FEV1), and quality of life; G″ was correlated with quality of life; sputum pH was correlated with oxygen consumption (VO2) and vitality score in quality of life. No changes were observed in blood count, venous blood gas, respiratory rate, heart rate, peripheral oxygen saturation of haemoglobin (SpO2), body temperature, or incidence of dyspnea. No adverse events associated with the study were observed.
The authors concluded nebulized NaHCO3 inhalation appears to be a safe and well tolerated potential therapeutic agent in the management of CF. Nebulized NaHCO3 inhalation temporarily elevates airway liquid pH and reduces sputum viscosity and viscoelasticity. They did however note that even though most measured parameters did not achieve statistical significance, the means of the measurements of effects almost always remained constant or changed in the direction of presumed improvement, giving confidence that the treatment did not depress or impede normal function. The favourable changes observed in several parameters in this study may support inhalation of nebulized NaHCO3 as a safe and well-tolerated therapeutic agent in the management of CF and possibly other obstructive lung diseases.
— Carla Cristina Souza Gomez (Fig 80) is a PhD student. The authors are from Center for Investigation in Pediatrics, Department of Pediatrics, Faculdade de Ciências Médicas, Universidade Estadual de Campinas, 126, Tessália Vieira de Camargo, Campinas, São Paulo, Brazil. Except for Paul Quinton and Douglas Conrad who are from the University of California San Diego School of Medicine; they provided the project concept and edited the manuscript. Paul Quinton has for many years emphasised the role of bicarbonate.
Guimbellot J, Solomon GM, Baines A, Heltshe SL, VanDalfsen J, Joseloff E, Sagel SD, Rowe SM; GOALe(2) Investigators. Effectiveness of ivacaftor in cystic fibrosis patients with non-G551D gating mutations. J Cyst Fibros. 2019 Jan;18(1):102-109. doi: 10.1016/j.jcf.2018.04.004. Epub 2018 Apr 21. [Pubmed]
-

Fig.81 Jennifer Guimbellot
- Patients with non-G551D gating mutations were recruited to an open-label study evaluating ivacaftor. Primary outcomes included: lung function, sweat chloride, weight gain, and quality of life scores. Twenty-one subjects were enrolled and completed 6 months follow-up on ivacaftor; mean age was 25.6 years with 52% <18. Baseline ppFEV1 was 68% and mean sweat chloride 89.6 mEq/L. Participants experienced significant improvements in ppFEV1 (mean absolute increase of 10.9% 95% CI = [2.6,19.3], p = 0.0134), sweat chloride (-48.6 95% CI = [-67.4,-29.9], p < 0.0001), and weight (5.1 kg, 95% CI = [2.8, 7.3], p = 0.0002).
The authors concluded patients with non-G551D gating mutations experienced improved lung function, nutritional status, and quality of life. This study supports ongoing use of ivacaftor for patients with these mutations.
Dr Jennifer Guimbellot (fig.81) is a paediatric pulmonologist at the Gregory Fleming James Cystic Fibrosis Research Center, University of Alabama at Birmingham (UAB), Birmingham, AL, USA; Department of Pediatrics, Division of Pulmonary and Sleep Medicine, UAB, Birmingham, AL, USA
Lamoreux C, Guilloux CA, Beauruelle C, Jolivet-Gougeon A, Héry-Arnaud G. Anaerobes in cystic fibrosis patients’ airways. Crit Rev Microbiol. 2019 Jan 21:1-15. doi: 10.1080/1040841X.2018.1549019. [Epub ahead of print] [Pubmed]

Fig. 82 Claudie Lamoureux
nouveau.univ-brest.fr
Anaerobes are known to constitute an important part of the airway microbiota in both healthy subjects and cystic fibrosis (CF) patients. Studies on the potential role of anaerobic bacteria in CF and thus their involvement in CF pathophysiology have reported contradictory results, and the question is still not elucidated. The aim of this study was to summarise anaerobe diversity in the airway microbiota and its potential role in CF, to provide an overview of the state of knowledge on anaerobe antibiotic resistances (resistome), and to investigate the detectable metabolites produced by anaerobes in CF airways (metabolome). This review emphasises key metabolites produced by strict anaerobic bacteria (sphingolipids, fermentation-induced metabolites and metabolites involved in quorum-sensing), which may be essential for the better understanding of lung disease pathophysiology in CF.
Claudie Lamoureux (fig.82) is at the Centre Hospitalier Regional et Universitaire de Brest, France
For more on anaerobes see also Muhlebach MS et al, 2018 [Pubmed] and Tunney MM et al 2008 [Pubmed]
Hamilton JL, Zobell JT, Robson J. Pancreatic insufficiency converted to pancreatic sufficiency with ivacaftor. Pediatr Pulmonol. 2019 Jul 21. doi: 10.1002/ppul.24454. [Epub ahead of print] [Pubmed]

Fig. 83 Jennifer Hamilton
A six‐year‐old female with cystic fibrosis (CF), genotype Phe508del/G551D, who we follow at our pediatric CF Center. Shortly after her CF diagnosis (through newborn screening), her fecal elastase was noted to be 83 µg/g (normal range >201 µg/g), and she was started on pancreatic enzyme replacement therapy (PERT). This child was started on ivacaftor at 2 years of age, as soon as it was approved by the United States Food and Drug Administration and commercially available for her age and mutations.
She had recurrent bouts of periumbilical abdominal pain extensively investigated with essentially negative findings. Since the serum lipase was mildly elevated and abdominal pain was continuing, a decision was made to investigate exocrine pancreatic function with fecal elastase‐1 testing. The patient’s fecal elastase was shown to have normalized (465 µg/g) at that check and 2 months later it was more than 500 µg/g. On the basis of these results, PERT was discontinued. Since discontinuing PERT, she has had no signs or symptoms of malabsorption. Her abdominal pain eventually improved, with clear precipitating source never identified, and we are monitoring her for recurrence of pancreatitis.
Jennifer Hamilton (fig.83) is at the College of Nursing, University of Utah Health Sciences, and the Paediatric Pulmonary and Sleep Medicine Division of the University of Utah.
Hardaker KM, Panda H, Hulme K, Wong A, Coward E, Cooper P, Fitzgerald DA, Pandit C, Towns S, Selvadurai H, Robinson PD.Abnormal preschool Lung Clearance Index (LCI) reflects clinical status and predicts lower spirometry later in childhood in cystic fibrosis.J Cyst Fibros 2019 Feb 28. pii: S1569-1993(19)30025-6. doi: 10.1016/j.jcf.2019.02.007. [Epub ahead of print] [Pubmed]

Fig. 85 Paul Robinson
-

Fig. 84 Kate Hardaker
- Clinical and prognostic value of preschool Multiple Breath Washout (MBW) remains unclear. Initial MBW results (Exhalyzer® D, EcoMedics AG) in preschool Cystic Fibrosis (CF) subjects (age 2-6 years) at a time of clinical stability were compared to (1) concurrent clinical status measures and (2) later spirometry outcomes. Abnormal Lung Clearance Index (LCI) was defined using published reference data (Upper limit of normal for LCI 8.0).
LCI was abnormal in 56% (28/50), with mean (SD) LCI 8.61(1.85) at age 4.71(1.3) years. Abnormal LCI was associated with higher dornase alfa use, previous positive bacterial cultures and pF508.del homozygous genotype. Later spirometry (n = 44; mean (SD) 2.3(0.5) years after MBW) demonstrated that abnormal initial preschool LCI was a strong predictor of lower later spirometry outcomes.
The authors concluded abnormal preschool LCI was associated with concurrent measures of clinical status and later spirometry deficits, suggesting early prognostic utility of MBW testing in this age range.
Dr. Kate Hardaker (fig.84) is a Respiratory Scientist at the Dept. Respiratory Medicine The Children’s Hospital at Westmead, Sydney.
Dr Paul Robinson (Fig 85) is a Staff Specialist in the Department of Respiratory Medicine, The Children’s Hospital at Westmead, Sydney and Clinical Associate P rofessor in the Discipline of Paediatrics and Child Health, Sydney Medical School, University of Sydney.
— Further work emphasising the importance of very early intervention in infants with CF. Also supporting the practical value of the LCI in young children.
Harindhanavudhi T, Wang Q, Dunitz J, Moran A, Moheet A. revalence and factors associated with overweight and obesity in adults with cystic fibrosis: A single-center analysis. J Cyst Fibros. 2019 Nov 11. pii: S1569-1993(19)30922-1. doi: 10.1016/j.jcf.2019.10.004. [Epub ahead of print] [Pubmed]

Fig. 86 Tasma Harindhanaudhi
The relation between malnutrition and pulmonary death in patients with cystic fibrosis (CF) has resulted in intensive nutritional intervention over the last few decades, leading to a significant decline in underweight and the emergence of overweight/obesity as a potential new problem. The authors performed a cross-sectional database analysis of 484 adults with CF seen at the University of Minnesota CF Center between January 2015-January 2017, to determine the prevalence and pulmonary/cardiovascular risk factors associated with overweight and obesity in this population.
Mean age was 35.2 ± 11.6 years. 5.2% were underweight (BMI<18.5 kg/m2), 62.6% normal weight (BMI ≥ 18.5-24.9 kg/m2), 25.6% overweight (BMI ≥ 25-29.9 kg/m2) and 6.6% obese (BMI ≥ 30 kg/m2). In the subgroup with severe genotypes, 25% had BMI ≥ 25 kg/m2. In the entire cohort, overweight/obese were likely to be older (OR = 1.04, p < 0.0001) and to have a mild CFTR genotype (OR = 3.33, p = 0.0003) and modestly elevated triglyceride levels (OR = 1.008, p < 0.0001). The prevalence of hypertension was higher in overweight (25%) and obese (31%) than normal (17%) or underweight (16%), p = 0.01. Total cholesterol levels were higher in overweight/obese versus normal/underweight (144-147 vs 123-131 mg/dL, p = 0.04) as were LDL levels (70-71 vs 53-60 mg/dL, p = 0.02), but all were within the normal range. Percent predicted FEV1 was higher in overweight/obese (78-81%) versus underweight (59%) and normal (70%), p < 0.0001, and overweight/obese experienced significantly fewer acute pulmonary exacerbations.
The authors concluded that overweight/obesity is common in adults with CF including those with severe genotypes. Lung function is better in the overweight/obese and lipid levels are within the normal range, albeit higher than in normal/underweight.
Dr Tasma Harindhanavudhi (fig 86) is an endocrinologist in the Division of Diabetes and Endocrinology, Department of Medicine, University of Minnesota, Minneapolis,
Harris JK, Wagner BD, Zemanick ET, Robertson CE, Stevens MJ, Heltshe SL, Rowe SM, Sagel SD4; GOAL Investigators of the Cystic Fibrosis Foundation Therapeutics Development Network.Changes in Airway Microbiome and Inflammation with Ivacaftor Treatment in Patients with Cystic Fibrosis and the G551D Mutation. Ann Am Thorac Soc. 2019 Oct 11. doi: 10.1513/AnnalsATS.201907-493OC. [Epub ahead of print] [Pubmed]

Fig. 87 J Kirk Harris
cuanschutz.edu
Modulation of the cystic fibrosis transmembrane conductance regulator (CFTR) protein improves clinical outcomes in patients with cystic fibrosis (CF) and specific CFTR genetic mutations. It remains unclear how improving CFTR function modifies existing airway infection and inflammation. A study to compare sputum microbiome and markers of inflammation before and after 6 months of ivacaftor treatment The cohort that spontaneously expectorated sputum had a lower FEV1, higher proportion with Pseudomonas aeruginosa infection,
In this multicenter cohort, six months of ivacaftor treatment were not associated with significant changes in airway microbial communities or measures of inflammation.
These data suggest that concomitant antimicrobial and anti-inflammatory treatments will still be needed to manage airway disease in CF patients treated with highly effective CFTR modulator therapy, especially in older patients with more advanced disease.
Dr J K Harris (fig.87) is Associate Professor in the University of Colorado, Pediatrics, Aurora, Colorado, United States.
Harun SN, Wainwright CE, Grimwood K, Hennig S; Australasian Cystic Fibrosis Bronchoalveolar Lavage (ACFBAL) study group. Aspergillus and progression of lung disease in children with cystic fibrosis. Thorax. 2019;74(2):125–131. doi:10.1136/thoraxjnl-2018-211550 [Pubmed]

Fig. 88 Sabariah Noor Harun ResearchGate
The impact of Aspergillus on lung disease in young children with cystic fibrosis is uncertain. This study was to determine if positive respiratory cultures of Aspergillus species are associated with: (1) increased structural lung injury at age 5 years; (2) lung function decline between ages 5 years and 14 years and (3) to identify explanatory variables. A cross-sectional analysis of the association between Aspergillus positive bronchoalveolar lavage (BAL) cultures and chest high-resolution CT (HRCT) scan findings at age 5 years in subjects from the Australasian Cystic Fibrosis Bronchoalveolar Lavage (ACFBAL) study was performed. A non-linear mixed-effects disease progression model was developed using FEV1% predicted measurements at age 5 years from the ACFBAL study and at ages 6-14 years for these subjects from the Australian Cystic Fibrosis Data Registry.Positive Aspergillus BAL cultures at age 5 years were significantly associated with increased HRCT scores for air trapping (OR 5.53, 95% CI 2.35 to 10.82). However, positive Aspergillus cultures were not associated with either FEV1% predicted at age 5 years or FEV1% predicted by age following adjustment for body mass index z-score and hospitalisation secondary to pulmonary exacerbations. Lung function demonstrated a non-linear decline in this population.
The authors concluded that In children with cystic fibrosis, positive Aspergillus BAL cultures at age 5 years were associated contemporaneously with air trapping but not bronchiectasis. However, no association was observed between positive Aspergillus BAL cultures on FEV1% predicted at age 5 years or with lung function decline between ages 5 years and 14 years.
Dr Sabariah Noor Harun (fig.88) is a lecturer in the School of Pharmaceutical Sciences, Universiti Sains Malaysia, Penang, Malaysia and School of Pharmacy, University of Queensland, Brisbane, Queensland, Australia.
Hatziagorou E, Orenti A, Drevinek P, Kashirskaya N, Mei-Zahav M, De Boeck K; ECFSPR. Electronic address: ECFS-Patient.Registry@uz.kuleuven.ac.be. Changing epidemiology of the respiratory bacteriology of patients with cystic fibrosis-data from the European cystic fibrosis society patient registry. J Cyst Fibros. 2019 Sep 3. pii: S1569-1993(19)30838-0. doi: 10.1016/j.jcf.2019.08.006. [Epub ahead of print] [Pubmed]

Fig. 89 Elpis Hatziagorou ResearchGate
Monitoring changes in the epidemiology of cystic fibrosis (CF) pathogens is essential for clinical research, quality improvement, and clinical management. We analysed data reported to the European Cystic Fibrosis Society Patient Registry (ECFSPR) from 2011 to 2016 to determine the overall and the age-specific annual prevalence and incidence of selected CF pathogens and their trends during these years. The ECFSPR collects data on three chronic infections: Pseudomonas aeruginosa (PsA), Burkholderia cepacia complex Species (BCC) and Staphylococcus aureus (SA), as well as on the occurrence of non-tuberculous mycobacteria (NTM) and Stenotrophomonas maltophilia (SM). The same analyses were performed for different country groups, according to their gross national income (GNI).
The pathogens with the highest prevalence were SA and PsA, with prevalence, in 2016, equal to 38.3% and 29.8% respectively, followed by SM (8.1%). The pathogens with the lowest prevalence were NTM (3.3%) and BCC (3.1%). The overall prevalence and incidence significantly decreased for PsA; they also decreased for BCC, while they increased significantly for SA. The overall prevalence of NTM and SM increased significantly. The most considerable prevalence changes were observed for PsA, which decreased across all income country groups and all age strata (with the exception of 0-1 years) The prevalence and incidence of pathogens differed significantly according to GNI.
The authors concluded the epidemiology of CF pathogens in Europe has changed; epidemiologic data differ significantly among countries with different socio-economic status. The causes of these observations are multifactorial and include improvements in clinical care and infection control.
Dr Elpis Hatziagorou (fig 89) is Associate Professor of Paediatrics at the Cystic Fibrosis Unit, Hippokration General Hospital of Thessaloniki, Aristotle University of Thessaloniki, Thessaloniki, Greece.
Hayee B, Watson KL, Campbell S, Simpson A, Farrell E, Hutchings P, Macedo P, Perrin F, Whelan K, Elston C. A high prevalence of chronic gastrointestinal symptoms in adults with cystic fibrosis is detected using tools already validated in other GI disorders. European Gastroenterol J. 2019 Aug;7(7):881-888. doi: 10.1177/2050640619841545.[Pubmed]

Fig 90 Bu Hayee Kings College Hospital
People with cystic fibrosis (CF) report a variety of gastrointestinal (GI) symptoms, independent of pancreatic enzyme insufficiency (PEI), reminiscent of other chronic GI disorders. There are currently no accepted or validated assessment tools and neither the range, frequency nor severity of GI symptoms has been systematically described in CF. We present results of a cross-sectional study using established tools and compare them to current measures of quality of life (QOL).
Consecutive patients attending specialist CF appointments were asked to complete questionnaires including the GI Symptom Rating Scale (GSRS); Irritable Bowel Syndrome Symptom Severity Score (IBS-SSS) and Cystic Fibrosis Questionnaire (CFQ-R). Questionnaire terminology was altered to replace references to ‘IBS’ with ‘GI symptoms’
In total, 107 patients were recruited (mean age, 27.8 ± 9.6 years; 60 female), and 94 (88%) had PEI. Body mass index was 22.1 ± 3.6 kg/m2, forced expiratory volume in one second was 59 + 27.7% predicted. Fifty-three (49.5%) were p.Phe508del homozygous. Overall 69/107 (65%) reported significant GI symptoms independent of PEI or adherence to pancreatic enzyme replacement therapy (PERT), with the four most frequent being attributable to the lower GI tract: bloating/distension, flatulence, abdominal pain and borborygmi (gurgling). There was no numerical correlation between any CFQ-R domain (particularly Digestion domain) and GSRS or SSS.
This is the first systematic study measuring GI symptoms in CF using validated GI tools. Symptoms are not related to PERT or genotype and appear to be captured well by the GI symptom rating scale. Further research will study longitudinal changes with treatment, and therapeutic trials in CF may use these tools to demonstrate a positive impact on ‘non-respiratory’ symptoms and QOL.
Dr Bu Hayee (Fig. 90) is a consultant Department of Gastroenterology, King’s College Hospital NHS Foundation Trust, London, UK.
Hayes D Jr, Kopp BT, Hill CL, Lallier SW, Schwartz CM, Tadesse M, Alsudayri A, Reynolds SD. Cell Therapy for Cystic Fibrosis Lung Disease: Regenerative Basal Cell Amplification. Stem Cells Transl Med. 2019 Mar;8(3):225-235. doi: 10.1002/sctm.18-0098. Epub 2018 Dec 1. [Pubmed]

Fig. 91 Don Hayes Jr
Cincinnati Children’s
The human airway epithelium is regenerated by basal cells. Thus, basal cell therapy has the potential to cure cystic fibrosis (CF) lung disease. We previously reported that the human basal cells repopulated the mouse airway epithelium after transplantation, and we estimated that 60 million cells would be needed to treat a human patient. To further develop cell therapy, we compared the proliferation potential of non-CF and CF tissue-derived bronchial basal cells. Three methods were used: regenerative cell frequency, burst size, and cell division frequency. Second, we used a serial passage strategy to determine if CF basal cells could be amplified to the estimated therapeutic dose. These studies evaluated that tissue-derived bronchial basal cells and the basal cells that were recovered by brushing bronchial airways or the nasal respiratory epithelium. Finally, we used the limiting dilution method to isolate non-CF and CF basal cell clones. The proliferation assays and the air-liquid-interface differentiation method were used to determine if cell amplification altered the proliferation and/or differentiation potential of clonal isolates.
The authors demonstrate that: (a) non-CF and CF basal cell proliferation is similar, (b) CF basal cells can be amplified to a therapeutic cell dose, and (c) amplified non-CF and CF basal cell clones differentiate normally. Despite these encouraging findings, we also find that the cell amplification process depletes the regenerative basal cell pool. Analysis of basal cell clones indicates that serial passage selects for long-lived basal cells and raise the possibility that prospective isolation of these stem-like cells will improve the efficacy of cell replacement therapy.
Don Hayes Jr (Fig.91) is professor and medical Director Cincinnati Children’s Hospital Medical Center and University of Cincinnati College of Medicine.
Heijerman HGM, McKone EF, Downey DG, Van Braeckel E, Rowe SM, Tullis E Mall MA, Welter JJ, Ramsey BW, McKee CM, Marigowda G, Moskowitz SM, Waltz D, Sosnay PR, Simard C, Ahluwalia N, Xuan F, Zhang Y, Taylor-Cousar JL, McCoy KS; VX17-445-103 Trial Group. Efficacy and safety of the elexacaftor plus tezacaftor plus ivacaftor combination regimen in people with cystic fibrosis homozygous for the F508del mutation: a double-blind, randomised, phase 3 trial. Collaborators (45). Lancet. 2019 Oct 30. pii: S0140-6736(19)32597-8. doi: 10.1016/S0140-6736(19)32597-8. [Epub ahead of print] Full copy available [Pubmed]

Fig. 92 Harry Heijerman
Cystic fibrosis transmembrane conductance regulator (CFTR) modulators correct the basic defect caused by CFTR mutations. Improvements in health outcomes have been achieved with the combination of a CFTR corrector and potentiator in people with cystic fibrosis homozygous for the F508del mutation. The addition of elexacaftor (VX-445), a next-generation CFTR corrector, to tezacaftor plus ivacaftor further improved F508del-CFTR function and clinical outcomes in a phase 2 study in people with cystic fibrosis homozygous for the F508del mutation.
This phase 3, multicentre, randomised, double-blind, active-controlled trial of elexacaftor in combination with tezacaftor plus ivacaftor was done at 44 sites in four countries. Eligible participants were those with cystic fibrosis homozygous for the F508del mutation, aged 12 years or older with stable disease, and with a percentage predicted forced expiratory volume in 1 s (ppFEV1) of 40-90%, inclusive. After a 4-week tezacaftor plus ivacaftor run-in period, participants were randomly assigned (1:1) to 4 weeks of elexacaftor 200 mg orally once daily plus tezacaftor 100 mg orally once daily plus ivacaftor 150 mg orally every 12 h versus tezacaftor 100 mg orally once daily plus ivacaftor 150 mg orally every 12 h alone. The primary outcome was the absolute change from baseline (measured at the end of the tezacaftor plus ivacaftor run-in) in ppFEV1 at week 4. Key secondary outcomes were absolute change in sweat chloride and Cystic Fibrosis Questionnaire-Revised respiratory domain (CFQ-R RD) score. This study is registered with ClinicalTrials.gov, NCT03525548.
Between Aug 3 and Dec 28, 2018, 113 participants were enrolled. Following the run-in, 107 participants were randomly assigned (55 in the elexacaftor plus tezacaftor plus ivacaftor group and 52 in the tezacaftor plus ivacaftor group) and completed the 4-week treatment period. The elexacaftor plus tezacaftor plus ivacaftor group had improvements in the primary outcome of ppFEV1 (least squares mean [LSM] treatment difference of 10·0 percentage points [95% CI 7·4 to 12·6], p<0·0001) and the key secondary outcomes of sweat chloride concentration (LSM treatment difference -45·1 mmol/L [95% CI -50·1 to -40·1], p<0·0001), and CFQ-R RD score (LSM treatment difference 17·4 points [95% CI 11·8 to 23·0], p<0·0001) compared with the tezacaftor plus ivacaftor group. The triple combination regimen was well tolerated, with no discontinuations. Most adverse events were mild or moderate; serious adverse events occurred in two (4%) participants receiving elexacaftor plus tezacaftor plus ivacaftor and in one (2%) receiving tezacaftor plus ivacaftor.
The authors concluded Elexacaftor plus tezacaftor plus ivacaftor provided clinically robust benefit compared with tezacaftor plus ivacaftor alone, with a favourable safety profile, and shows the potential to lead to transformative improvements in the lives of people with cystic fibrosis who are homozygous for the F508del mutation.
Dr Harry Heijerman (Fig. 92) is professor and head of the Department of Pulmonology, University Medical Center Utrecht, Utrecht, Netherlands.
Hoo ZH, Bramley NR, Curley R, Edenborough FP, Walters SJ, Campbell MJ, Wildman MJ. Intravenous antibiotic use and exacerbation events in an adult cystic fibrosis centre: A prospective observational study. Respir Med. 2019 Jun 18;154:109-115. doi: 10.1016/j.rmed.2019.06.017. [Epub ahead of print] [Pubmed]

Fig. 93 Martin Wildman
In CF, people with higher FEV1 are less aggressively treated with intravenous (IV) antibiotics, with resultant negative impact on their health outcomes. This could be entirely clinician-driven, but patient choice may also influence IV use. In this prospective observational study, we explored IV recommendations by clinicians and IV acceptance by adults with CF to understand how clinical presentations consistent with exacerbations resulted in IV use. Clinical presentations consistent with exacerbations, IV recommendation by clinicians and IV acceptance by patients were prospectively identified for every adult with CF in Sheffield throughout 2016, excluding those who had lung transplantation (n = 7) or on ivacaftor (n = 13). Relevant demographic data, e.g. %FEV1, were extracted from medical records. Multi-level mixed-effects logistic regression models were used to compare IV recommendations vs non-recommendations for all clinical encounters, and IV acceptance vs non-acceptance for all IV recommendations.
Among 186 adults (median age 27 years, median FEV1 78.5%), there were 434 exacerbation events and 318 IV use episodes following 1010 clinical encounters. Only 254 (58.5%) of exacerbations were IV treated. A diagnosis of exacerbation, higher number of symptoms and lower %FEV1 were independent predictors for IV recommendation by clinicians. Higher number of symptoms and lower %FEV1 were also independent predictors for IV acceptance by adults with CF.
The authors concluded lower IV use among adults with higher %FEV1 was influenced by both clinicians’ and patients’ decisions. Therefore using IV antibiotics as an exacerbation surrogate could under-estimate exacerbation rates and conceal differential treatment decisions according to varying clinical characteristics.
Dr Martin Wildman (fig.93) is consultant in Respiratory Medicine and one of the consultants at the Adult CF Centre in Sheffield. He is particularly interested in the various aspects of adherence to treatment in cystic fibrosis.
Hort A, Hameed A, Middleton PG, Pleass HC. Distal intestinal obstruction syndrome: an important differential diagnosis for abdominal pain in patients with cystic fibrosis. ANZ J Surg. 2019 Jul 30. doi: 10.1111/ans.15357. [Epub ahead of print] [Pubmed]
Fig. 94 Amy Hort
LinkedIn
As life expectancy for those with cystic fibrosis (CF) now exceeds 40 years of age, adult hospitals away from specialized CF services are being exposed more frequently to people with acute complications of CF. Well-known manifestations of CF include pulmonary disease and pancreatic insufficiency with malabsorption. However, a less well-known entity is distal intestinal obstruction syndrome (DIOS), which is an important cause of obstructive symptoms in people with CF that must be differentiated from other causes of bowel obstruction. However, one confounding factor is that adults with CF may have elements of both DIOS and mechanical bowel obstruction due to adhesions from previous operations. A recent tragic outcome in a young adult with CF highlights the need for all doctors, both junior and senior, especially those who are not directly involved in day-to-day CF care, to understand the features of DIOS and the appropriate management, which differs from that of a mechanical bowel obstruction. This review aims to highlight the clinical and pathophysiological features of DIOS, differentiate it from other causes of bowel obstruction and contrast management strategies. Improved knowledge of DIOS will help to facilitate appropriate recognition and permit optimal, multidisciplinary management of this CF complication.
Dr Amy Hort (Fig. 94) is from the Department of Surgery, Westmead Hospital, Sydney
— This is an important paper as there are potential dangers for the person with CF being admitted and treated in a surgical unit unfamiliar with the complex problems of the condition. I recall many years ago there was a person with CF admitted and operated on in a non-CF ward. The pancreatic enzymes were not started after the operations, intestinal obstruction recurred, parental nutrition was needed and the patient eventually died from systemic candida infection.
Hoy SM. Elexacaftor/Ivacaftor/Tezacaftor: First Approval. Drugs. 2019 Nov 29. doi: 10.1007/s40265-019-01233-7. [Epub ahead of print]Author information.[Pubmed]

Fig 95 Sheridan Hoy
LinkedIn
A fixed-dose combination tablet of the cystic fibrosis transmembrane conductance regulator (CFTR) corrector tezacaftor and the CFTR potentiator ivacaftor with the next-generation CFTR corrector elexacaftor (hereafter referred to as elexacaftor/ivacaftor/tezacaftor) [Trikafta™] has been developed by Vertex Pharmaceuticals Inc. to treat patients with the most common cystic fibrosis mutation (F508del). Its use has been associated with statistically significant and/or clinically meaningful improvements in lung function and respiratory-related quality of life compared with comparator regimens (placebo or ivacaftor/tezacaftor) in multinational phase II and III studies, and in October 2019 elexacaftor/ivacaftor/tezacaftor was approved by the US FDA for the treatment of cystic fibrosis in patients aged ≥ 12 years who have ≥ 1 F508del mutation in the CFTR gene. A regulatory assessment for elexacaftor/ivacaftor/tezacaftor as a treatment for cystic fibrosis is underway in the EU. This article summarises the milestones in the development of elexacaftor/ivacaftor/tezacaftor leading to this first approval for the treatment of cystic fibrosis in patients aged ≥ 12 years who have ≥ 1 F508del mutation in the CFTR gene.
Dr Sheridan M Hoy (fig.95) is Senior Medical Writer at Springer Nature, Private Bag 65901, Mairangi Bay, Auckland
De la Hoz D, Villamil Osorio M, Restrepo-Gualteros SM. Cystic fibrosis transmembrane conductance regulator modulators: Present and future in cystic fibrosis treatment. A review. Arch Argent Pediatr. 2019 Apr 1;117(2):e131-e136. doi: 10.5546/aap.2019.eng.e131. Free full text [Pubmed]
Cystic fibrosis transmembrane conductance regulator (CFTR) modulators are the present and future of drug management for patients with cystic fibrosis. The objective of this article is to review this therapeutic option. Scientific articles were reviewed by searching the MedLine database, which is available through the Cystic Fibrosis Foundation’s official website, from 2009 to 2018, in English. Twelve articles about the current status of research in CFTR modulators were selected without restrictions regarding the type of study. To date, the United States Food and Drug Administration has approved three modulators: ivacaftor, lumacaftor + ivacaftor, and tezacaftor + ivacaftor, while other 11 drugs are being studied in different investigation phases. CFTR modulator therapy is a developing reality aimed at the highest goal of personalized medicine and promises to improve the quality of life of cystic fibrosis patients.
David De la Hoz From Universidad Nacional de Colombia, Departamento de Pediatría, Bogotá DC, Colombia. dcdeg@unal.edu.co.
— The full text is a very readable summary of the major facts and leading references regarding CFTR modulators. The first author’s previous publications appear to have concerned various aspects of acetylcholinesterase.
Irons JY, Petocz P, Kenny DT, Chang AB. Singing as an adjunct therapy for children and adults with cystic fibrosis. Cochrane Database Syst Rev. 2019 Jul 12;7:CD008036. doi: 10.1002/14651858.CD008036.pub5. [Epub ahead of print][Pubmed]

Fig. 96 J Yoon Irons
Anecdotal reports suggest that singing may provide both appropriate exercise for the whole respiratory system and a means of emotional expression which may enhance quality of life. This is an update of a previously published review.
To evaluate the effects of singing as an adjunct therapy to standard treatment on the quality of life, morbidity, respiratory muscle strength and pulmonary function of children and adults with cystic fibrosis.
Only one small study (n = 40) was included, so no meta-analysis could be performed. The included randomised controlled study was of parallel design and undertaken at two paediatric hospitals in Australia. The study evaluated the effects of a singing program on the quality of life and respiratory muscle strength of hospitalised children with cystic fibrosis (mean age 11.6 years, 35% male). While the singing group received eight individual singing sessions, the control group participated in preferred recreational activities, such as playing computer games or watching movies. This study was limited by a small sample size (51 participants) and a high drop-out rate (21%). There were no differences between the groups at either post-intervention or follow-up; although by the end of treatment there were some improvements in some of the domains of the quality of life questionnaire Cystic Fibrosis Questionnaire-Revised (e.g. emotional, social and vitality domains) for both singing and control groups.
The conclusion was there is insufficient evidence to determine the effects of singing on quality of life or on the respiratory parameters in people with cystic fibrosis. However, there is growing interest in non-medical treatments for cystic fibrosis and researchers may wish to investigate the impact of this inexpensive therapy on respiratory function and psychosocial well-being further in the future.
Dr J Yoon Irons (fig.96) qualified PhD at University of Sydney and is now a Research Fellow at the Department of Health and Social Care Research Centre, University of Derby, Derby, UK. She is interested in exploring health and wellbeing benefits from participating in arts such as singing, music, dance and visual arts.
See also Goldenberg RB. Singing lessons for respiratory health; a literature review. J Voice 2018; 32(1):85-94. In 2017 section and also Physiotherapy Topic section
Isaiah A, Daher A, Sharma PB, Naqvi K, Mitchell RB.Predictors of sleep hypoxemia in children with cystic fibrosis.Pediatr Pulmonol. 2019 Jan 4. doi: 10.1002/ppul.24233. [Epub ahead of print] [Pubmed]
-

Fig. 97 Amal Isaiah University of Maryland
Sleep hypoxemia in children with CF is predicted by both apnea hypopnea index (AHI) and percent predicted forced expiratory volume in one second (pFEV1). This is a study to identify the determinants of nocturnal hypoxemia in children with CF using clinical parameters, polysomnography (PSG), and lung function.
A pFEV1 cut-off of 53% indicated a sensitivity of 0.80 and a specificity of 0.87 in predicting sleep hypoxemia. So pFEV1 is the best predictor of sleep hypoxemia in children with CF and referred for PSG. No demographic or clinical predictors of hypoxemia were identified in this population.
Dr Amal Isaiah (fig.97) is Assistant Professor in the Division of Pediatric Otolaryngology-Head and Neck Surgery, Dallas Texas.
Jones LA, Doucette L, Dellon EP, Esther CR, McKinzie CJ.Use of inhaled imipenem/cilastatin in pediatric patients with cystic fibrosis: A case series. J Cyst Fibros. 2019 May 3. pii: S1569-1993(19)30076-1. doi: 10.1016/j.jcf.2019.04.017. [Epub ahead of print] pubmed.ncbi.nlm.nih.gov/31060800/

Fig 98 Lee Ann Jones
UNC Medical Center
M. abscessus complex pulmonary infections are notoriously difficult to treat, and while many antibiotics are approved for children, drug allergies or intolerances can prohibit their use. In this case series, the authors describe two pediatric patients with cystic fibrosis and previous intolerance or lack of response to standard therapies who received inhaled imipenem/cilastatin for the treatment of chronic M. abscessus infection.
Lee Ann Jones (fig.98) is from the Dept. of Pharmacy University of North Carolina Medical Center.
Jorth P, Ehsan Z, Rezayat A, Caldwell E, Pope C, Brewington JJ, Goss CH, Benscoter D, Clancy JP, Singh PK. Direct Lung Sampling Indicates That Established Pathogens Dominate Early Infections in Children with Cystic Fibrosis. Cell Rep. 2019 Apr 23;27(4):1190-1204.e3. doi: 10.1016/j.celrep.2019.03.086. 31018133 Free full text [Pubmed]

Fig.99 Peter Jorth The Jorth Lab
Culture and sequencing have produced divergent hypotheses about cystic fibrosis (CF) lung infections. Culturing suggests that CF lungs are uninfected before colonization by a limited group of CF pathogens. Sequencing suggests diverse communities of mostly oral bacteria inhabit lungs early on and diversity decreases as disease progresses. The authors studied the lung microbiota of CF children using bronchoscopy and sequencing, with measures to reduce contamination. They found no evidence for oral bacterial communities in lung lavages that lacked CF pathogens. Lavage microbial diversity varied widely, but decreases in diversity appeared to be driven by increased CF pathogen abundance, which reduced the signal from contaminants. Streptococcus, Prevotella, and Veillonella DNA was detected in some lavages containing CF pathogens, but DNA from these organisms was vastly exceeded by CF pathogen DNA and was not associated with inflammation. These findings support the hypothesis that established CF pathogens are primarily responsible for CF lung infections
– This is a very detailed complex scientific article with nevertheless a straight forward conclusion that BALs from children with mild disease primarily contain established pathogens; microbiota from BALs lacking pathogens were indistinguishable from controls; rare oral organisms were found in some BALs containing abundant CF pathogens; CF pathogens strongly correlated with inflammation but oral organisms did not.
Dr Peter A Jorth (Fig 99) is Assistant Professor, Departments of Pathology and Laboratory Medicine, Medicine and Biomedical Sciences, Cedars-Sinai Medical Center, Los Angeles.











