2016
2016
THE FIRST TWO ABSTRACTS ARE REVIEWS OF VARIOUS ASPECTS OF PROGRESS IN 2016
Adrienne P Savant, Susanna A McColley Cystic fibrosis year in review 2016. Pediatr Pulmonol 2017 Aug;52(8):1092-1102.doi: 10.1002/ppul.23747.Epub 2017 Jun 13. Full text available [PubMed]
In this article, we highlight cystic fibrosis (CF) research and case reports published in Pediatric Pulmonology during 2016. We also include articles from a variety of journals that are thematically related to these articles, or are of special interest to clinicians.
The authors are in the Division of Pulmonary Medicine, Ann & Robert H. Lurie Children’s Hospital of Chicago, Illinois & Department of Pediatrics, Northwestern University Feinberg School of Medicine, Chicago, Illinois.and Susanna McColley also at the Stanley Manne Children’s Resear ch Institute, Chicago, Illinois.
Adelle S Jee , Tamera J Corte, Stephen J Wort, Neil D Eves, Claire E Wainwright, Amanda Piper. Year in review 2016: Interstitial lung disease, pulmonary vascular disease, pulmonary function, paediatric lung disease, cystic fibrosis and sleep. Respirology 2017 Jul;22(5):1022-1034.doi: 10.1111/resp.13080.Epub 2017 May 25. Full text available [PubMed]
There is an interesting section on cystic fibrosis in this review by Prof. Claire Wainwright
Dr Adelle S Jee is at Department of Respiratory and Sleep Medicine, Royal Prince Alfred Hospital, Sydney, New South Wales, Australia. Central Clinical School, University of Sydney, Sydney, New South Wales, Australia.
2016

Fig. 1 Ryan Adam LinkedIn
Adam RJ, Hisert KB, Dodd JD, Grogan B, Launspach JL, Barnes JK, Gallagher CG, Sieren ACI. Acute administration of ivacaftor to people with cystic fibrosis and a G551D-CFTR mutation reveals smooth muscle abnormalities. Insight. 2016 Apr 7;1(4):e86183. [PubMed]
Airflow obstruction is common in cystic fibrosis (CF), yet the underlying pathogenesis remains incompletely understood. People with CF often exhibit airway hyper-responsiveness, CF transmembrane conductance regulator (CFTR) is present in airway smooth muscle (ASM), and ASM from newborn CF pigs has increased contractile tone, suggesting that loss of CFTR causes a primary defect in ASM function. The authors hypothesized that restoring CFTR activity would decrease smooth muscle tone in people with CF. To increase or potentiate CFTR function, they administered ivacaftor to 12 adults with CF with the G551D-CFTR mutation; ivacaftor stimulates G551D-CFTR function. They studied people before and immediately after initiation of ivacaftor (48 hours) to minimize secondary consequences of CFTR restoration. We tested smooth muscle function by investigating spirometry, airway distensibility, and vascular tone. The ivacaftor rapidly restored CFTR function, indicated by reduced sweat chloride concentration. Airflow obstruction and air trapping also improved. Airway distensibility increased in airways less than 4.5 mm but not in larger-sized airways. To assess smooth muscle function in a tissue outside the lung, they measured vascular pulse wave velocity (PWV) and augmentation index, which both decreased following CFTR potentiation. Finally, change in distensibility of <4.5-mm airways correlated with changes in PWV.
Acute CFTR potentiation provided a unique opportunity to investigate CFTR-dependent mechanisms of CF pathogenesis. The rapid effects of ivacaftor on airway distensibility and vascular tone suggest that CFTR dysfunction may directly cause increased smooth muscle tone in people with CF and that ivacaftor may relax smooth muscle.
Ryan J Adam (fig.1) s a post doctoral research fellow at the Department of Biomedical Engineering and Department of Internal Medicine, University of Iowa, Iowa City, Iowa, USA.
Adams C; Icheva V; Deppisch C; Lauer J; Herrmann G; Graepler-Mainka U; Heyder S; Gulbins E; Riethmueller J. Long-Term Pulmonal Therapy of Cystic Fibrosis-Patients with Amitriptyline. Cell Physiol Biochem 2016; 39(2):565-72. [PubMed]

Fig 2. Joachim Riethmueller
Several recent clinical studies revealed an accumulation of ceramide in bronchial epithelial cells of patients with cystic fibrosis (CF). Degradation of ceramide concentrations in lungs of CF patients employing the functional acid sphingomyelinase inhibitor amitriptyline revealed a benefit in lung function, weight and exacerbation rates. To test for a beneficial effect of amitriptyline in vivo, the authors performed two phase II randomised, double-blind, placebo-controlled studies. CF patients were treated with 25 mg amitriptyline twice daily, i.e. a total dose of 50 mg/d. After those two studies part of the patients used amitriptyline in an off-label-use for routine treatment. These patients were observed after one, two and three years after continuous use of amitriptyline and were matched with those patients who were not treated. These patients were used as a control group. After one year of treatment, forced expiratory volume in 1 sec predicted (FEV1) increased significantly by 7.6+/-7.0%, p=<0.001, and weight increased by 2.1+/-2.3kg, p=<0.001 in the amitriptyline population (n=20), whereas FEV1 decreased significantly in the control group by 1.8+/-3.3%, p=0.010, and weight increased by 1.1+/-2.7kg, p=0.010 (n=14). After two years of treatment, FEV1 increased significantly by 5.6+/-10.3%, p=0.009, and weight increased by 3.6+/-2.9kg, p=<0.001 in the amitriptyline population (n=12). In contrast, FEV1 decreased in the control group by 2.1+/-3.7%, p=0.051 and weight increased by only 0.4+/-2.9kg, p=0.31 (n=10). After three years of treatment, FEV1 increased significantly by 7.7+/-8%, p=0.050, and weight increased by 7.3+/-3.8kg, p=0.016, in the amitriptyline population (n=5), whereas FEV1 decreased in the control group by 1.0+/-1.3%, p=0.075 and weight increased by 0.4+/-1.5kg, p=0.29 (n=5). The authors concluded amitriptyline significantly increases FEV1, reduces ceramide in lung cells and increases weight of CF patients. — Further evidence that amitriptyline has a favourable effect in CF. Some of the previous work is reviewed in Topics -> Drug modulation, new drugs ->amitriptyline.
Dr Joachim Riethmueller (fig. 2) is Pediatric Pulmonologist at the University Children’s Hospital, Tubingen
Alton EWFW, Armstrong DK, Ashby D, Bayfield KJ, Bilton D, Bloomfield EV, et al. on behalf of the UK Cystic Fibrosis Gene Therapy Consortium.A randomised, double-blind, placebo-controlled trial of repeated nebulisation of non-viral cystic fibrosis transmembrane conductance regulator (CFTR) gene therapy in patients with cystic fibrosis.Southampton (UK): NIHR Journals Library; 2016 Jul
Fig 3. Eric Alton imperial.ac.uk
To determine clinical efficacy of the formulation delivered to the airways over a period of 1 year in patients with CF. This was a randomised, double-blind, placebo-controlled Phase IIb trial of the CFTRgene–liposome complex pGM169/GL67A. Randomisation was performed via InForm™ version 4.6 (Phase Forward Incorporated, Oracle, CA, USA) and was 1 : 1, except for patients in the mechanistic subgroups (2 : 1). Allocation was blinded by masking nebuliser chambers. Data were collected in the clinical and scientific sites and entered onto a trial-specific InForm, version 4.6 database. Patients with CF aged ≥ 12 years with forced expiratory volume in the first second (FEV1) between 50% and 90% predicted and any combination of CFTR mutations. The per-protocol group (≥ 9 doses) consisted of 54 patients receiving placebo (62 randomised) and 62 patients receiving gene therapy (78 randomised). Subjects received 5 ml of nebulised pGM169/G67A (active) or 0.9% saline (placebo) at 28 (±5)-day intervals over 1 year. The primary end point was the relative change in percentage predicted FEV1 over the 12-month period. A number of secondary clinical outcomes were assessed alongside safety measures: other spirometric values; lung clearance index (LCI) assessed by multibreath washout; structural disease on computed tomography (CT) scan; the Cystic Fibrosis Questionnaire – Revised (CFQ-R), a validated quality-of-life questionnaire; exercise capacity and monitoring; systemic and sputum inflammatory markers; and adverse events (AEs). A mechanistic study was performed in a subgroup in whom transgene deoxyribonucleic acid (DNA) and messenger ribonucleic acid (mRNA) was measured alongside nasal and lower airway potential difference.
RESULTS: There was a significant (p=0.046) treatment effect (TE) of 3.7% [95% confidence interval (CI) 0.1% to 7.3%] in the primary end point at 12 months and in secondary end points, including forced vital capacity (FVC) (p = 0.031) and CT gas trapping (p=0.048). Other outcomes, although not reaching statistical significance, favoured active treatment. Effects were noted by 1 month and were irrespective of sex, age or CFTR mutation class. Subjects with a more severe baseline FEV1 had a FEV1 TE of 6.4% (95% CI 0.8% to 12.1%) and greater changes in many other secondary outcomes. However, the more mildly affected group also demonstrated benefits, particularly in small airway disease markers such as LCI. The active group showed a significantly (p=0.032) greater bronchial chloride secretory response. No difference in treatment-attributable AEs was seen between the placebo and active groups.
CONCLUSIONS: Monthly application of the pGM169/GL67A gene therapy formulation was associated with an improvement in lung function, other clinically relevant parameters and bronchial CFTR function, compared with placebo.
Although encouraging, the improvement in FEV1 was modest and was not accompanied by detectable improvement in patients’ quality of life. Future work will focus on attempts to increase efficacy by increasing dose or frequency, the co-administration of a CFTR potentiator, or the use of modified viral vectors capable of repeated administration.
The further report of the UK Gene Therapy Consortium Trial in Lancet Respiratory Medicine, The, 2015-09-01, Volume 3, Issue 9, Pages 684-691. Eric W F W Alton Prof, David K Armstrong MB ChB, Deborah Ashby Prof, Katie J Bayfield BSc, Diana Bilton Prof, Emily V Bloomfield BSc et al. Repeated nebulisation of non-viral CFTR gene therapy in patients with cystic fibrosis: a randomised, double-blind, placebo-controlled, phase 2b trial. Lancet Respiratory Medicine, The, 2015-09-01, Volume 3, Issue 9, Pages 684-691
Professor Eric Alton (fig.3) is the leader of the UK Gene Therapy Consortium at Imperial College London.
Alton EW, Beekman JM, Boyd AC, Brand J, Carlon MS, Connolly MM, et al. Preparation for a first-in-man lentivirus trial in patients with cystic fibrosis. Thorax. 2016 Nov 16. pii: thoraxjnl-2016-208406. doi: 10.1136/thoraxjnl-2016-208406. [Epub ahead of print] [PubMed]
The authors have recently shown that non-viral gene therapy can stabilise the decline of lung function in patients with cystic fibrosis (CF). However, the effect was modest, and more potent gene transfer agents are still required. Fuson protein (F)/Hemagglutinin/Neuraminidase protein (HN)-pseudotyped lentiviral vectors are more efficient for lung gene transfer than non-viral vectors in preclinical models. In preparation for a first-in-man CF trial using the lentiviral vector, they have undertaken key translational preclinical studies. Regulatory-compliant vectors carrying a range of promoter/enhancer elements were assessed in mice and human air-liquid interface (ALI) cultures to select the lead candidate; cystic fibrosis transmembrane conductance receptor (CFTR) expression and function were assessed in CF models using this lead candidate vector. Toxicity was assessed and ‘benchmarked’ against the leading non-viral formulation recently used in a Phase IIb clinical trial. Integration site profiles were mapped and transduction efficiency determined to inform clinical trial dose-ranging. The impact of pre-existing and acquired immunity against the vector and vector stability in several clinically relevant delivery devices was assessed. A hybrid promoter hybrid cytosine guanine dinucleotide (CpG)- free CMV enhancer/elongation factor 1 alpha promoter (hCEF) consisting of the elongation factor 1α promoter and the cytomegalovirus enhancer was most efficacious in both murine lungs and human ALI cultures (both at least 2-log orders above background).
The efficacy (at least 14% of airway cells transduced), toxicity and integration site profile supports further progression towards clinical trial and pre-existing and acquired immune responses do not interfere with vector efficacy. The lead rSIV.F/HN candidate expresses functional CFTR and the vector retains 90-100% transduction efficiency in clinically relevant delivery devices. The authors consider the data support the progression of the F/HN-pseudotyped lentiviral vector into a first-in-man CF trial in 2017
Alton EW, Boyd AC, Davies JC, Gill DR, Griesenbach U, Harrison PT, Henig N, Higgins T, Hyde SC, Innes JA, Korman MS. Genetic medicines for CF: Hype versus reality. Pediatr Pulmonol. 2016 Oct; 51(S44):S5-S17. doi: 10.1002/ppul.23543. [PubMed]
Since identification of the CFTR gene over 25 years ago, gene therapy for cystic fibrosis (CF) has been actively developed. More recently gene therapy has been joined by other forms of “genetic medicines” including mRNA delivery, as well as genome editing and mRNA repair-based strategies. Proof-of-concept that gene therapy can stabilise the progression of CF lung disease has recently been established in a Phase IIb trial. An early phase study to assess the safety and explore efficacy of CFTR mRNA repair is ongoing, while mRNA delivery and genome editing-based strategies are currently at the pre-clinical phase of development.
This review has been written jointly by some of those involved in the various CF “genetic medicine” fields and will summarise the current state-of-the-art, as well as discuss future developments. Where applicable, it highlights common problems faced by each of the strategies, and also tries to highlight where a specific strategy may have an advantage on the pathway to clinical translation. We hope that this review will contribute to the ongoing discussion about the hype versus reality of genetic medicine-based treatment approaches in CF.
Amin R; Stanojevic S; Kane M; Webster H; Ratjen F. A randomized controlled trial to evaluate the lung clearance index as an outcome measure for early phase studies in patients with cystic fibrosis. Resp Med 2016; 112:59-64. [PubMed]

Fig. 4 Reshma Amin
SickKids.ca
The authors investigated whether the lung clearance index (LCI) measured by multiple breath washout (MBW) can detect a treatment effect of hypertonic saline (HS) inhalation after single dosing within a 24 h period. In this cross over trial CF patients received inhalation of HS and isotonic saline (IS). MBW and spirometry were performed at 5 time points over 24 h. LCI was measured using both a nitrogen washout technique (LCIN2) and sulfur hexafluoride as a tracer gas (LCISF6). The primary endpoint was the change in the LCIN2 between baseline and 24 h. Secondary endpoints included change in LCISF6 and spirometry outcomes.
Twenty-one patients were randomized. Sixteen completed all study visits and all time point measurements. Eighteen patients contributed to the intention to treat analysis. Significant changes were not detected for either LCI or the spirometry outcomes. However, the primary outcome parameter (change in LCI between the baseline visits and 24 h after inhalation) demonstrated a trend towards improved LCI, in the HS treatment arm compared with the IS treatment arm, -0.60 LCIN2 (SE 0.32), p = 0.08); similar trends were not observed for spirometric measures. The overall effect size of HS was smaller than in previous studies of longer duration. The authors concluded these data suggest that LCI may potentially be used as an outcome measure in early phase trials with therapeutic agents that have a larger treatment effects than a single inhalation of HS.
Rashma Amin (fig. 4)is professor in the Division of Respiratory Medicine, Hospital for Sick Children, Toronto, Canada; University of Toronto, Toronto, Canada; Child Health and Evaluative Sciences, Research Institute, Hospital for Sick Children, Toronto, Canada.
Armaghanian N, Brand-Miller JC Markovic TP, Steinbeck KS. Hypoglycaemia in cystic fibrosis in the absence of diabetes: A systematic review. J Cyst Fibros. 2016 Mar 22. pii: S1569-1993(16)30003-0. doi: 10.1016/j.jcf.2016.02.012. [Epub ahead of print] [PubMed]

Fig. 5 Natasha Armaghanian
ResearchGate
A total of 11 studies and five evidence-based guidelines met the inclusion criteria. Prevalence rates of hypoglycaemia unrelated to diabetes varied between studies (7-69%). There was no unifying definition of hypoglycaemia in the absence of diabetes. Only two evidence based guidelines reported possible management strategies.- The systematic review found limited data on this clinical problem and supports the need for high quality methodological studies that are able to describe the experience and the aetiology of hypoglycaemia in CF.
Natasha Armaghanian (fig.5) is in the Discipline of Paediatrics and Child Health, Sydney Medical School, University of Sydney, Australia; Academic Department of Adolescent Medicine, The Children’s Hospital at Westmead, Australia
Ahmed MI; Mukherjee S. Treatment for chronic methicillin sensitive Staphylococcus aureus pulmonary infection in people with cystic firbosis. Cochrane Database of Systematic Reviews. 3:CD011581, 2016. [PubMed]

Fig. 6 Molla Imaduddin Ahmed LinkedIn
Staphylococcus aureus is a major cause of chest infection in people with cystic fibrosis. Early onset, as well as chronic, lung infection with this organism in young children and adults results in worsening lung function, poorer nutrition and increases the airway inflammatory response, thus leading to a poor overall clinical outcome. There are currently no evidence-based guidelines for chronic suppressive therapy for Staphylococcus aureus infection in cystic fibrosis such as those used for Pseudomonas aeruginosa infection. The searches identified 55 trials, but none were eligible for inclusion in the current version of this review. The authors identified no randomised controlled trials which met the inclusion criteria for this review. Although methicillin-sensitive Staphylococcus aureus is an important and common cause of lung infection in people with cystic fibrosis, there is no agreement on how best to treat long-term infection. The review highlights the need to organise well-designed trials that can provide evidence to support the best management strategy for chronic methicillin-sensitive Staphylococcus aureus infection in people with cystic fibrosis.
—- S. aureus is a damaging pathogen which should be prevented in young CF children and eradicated when it appears in older patients. In this reviewer’s opinion it would be wasteful and almost unethical to arrange trials as suggested by these authors. The advice of the UK CF Trust Antibiotic Group seems reasonable i.e. using prophylactic flucloxacillin for the first 3 years then vigorous efforts to eradicate whenever the organism appears.
Useful advice, based on extensive experience, has been published over the years from Copenhagen where the incidence of chronic S. aureus infection is very low (Dalbøge CS et al. A cohort study of the Copenhagen CF Centre eradication strategy against Staphylococcus aureus in patients with CF. J Cyst Fibros. 2013; 12:42-48 [PubMed]). These Danish authors conclude that their anti-S. aureus eradication strategy in CF patients resulted in a low prevalence of chronic infections and high treatment efficacy. Furthermore, anti-staphylococcal treatment may be associated with a short-term improvement in lung function. They further state that “Antibiotic treatment of any relevant micro organisms, ignoring the presence or absence of respiratory symptoms has been our policy since the establishment of our centre in 1968”. They observe that “use of a stepwise two-drug antibiotic combination therapy strategy results in a high level of eradication with a prevalence of chronic S. aureus infection of less than 15% which has been unchanged for decades”. This prevalence is much lower than the 50% reported in many patient registries.
Molla I Ahmed (fig. 6) is a consultant paediatrician and respiratory clinic lead in the Department of Paediatrics, Leicester Royal Infirmary, University Hospitals of Leicester, Infirmary Square, Leicester, UK, LE1 5WW
Alanin MC; Aanaes K; Hoiby N; Pressler T; Skov M; Nielsen KG; Taylor-Robinson D; Waldmann E; Krogh Johansen H; von Buchwald C. Sinus surgery postpones chronic Gram-negative lung infection: cohort study of 106 patients with cystic fibrosis. Rhinology 2016; 54(3):206-13. [PubMed]

Fig 7. Mikkel C Alanin ResearchGate
In patients with cystic fibrosis (CF) the sinuses are a bacterial reservoir for Gram-negative bacteria (GNB). From the sinuses the GNB can repeatedly migrate to the lungs. In a one-year follow-up study, endoscopic sinus surgery (ESS) with adjuvant therapy (2 weeks IV antibiotics and 6 months antibiotic nasal irrigations) reduced the frequency of pulmonary samples positive for GNB (Aanaes K et al, 2013).(See comment below for detail) The authors investigated whether the effect is sustained.They report the effect of ESS and adjuvant therapy three years postoperatively in a CF cohort participating in this prospective clinical follow-up study. The primary endpoint was the lung infection status defined by Leeds criteria.
One hundred and six CF patients underwent ESS; 27 had improved lung infection status after three years. The prevalence of patients free of lung colonization with GNB significantly increased from 16/106 patients (15%) preoperatively to 35/106 patients (33%) after three years. The total cohort had decreasing lung function during follow-up; however, in 27 patients with improved lung infection status lung function was stable. Revision surgery was performed in 31 patients (28%).
The authors concluded ESS with adjuvant therapy significantly improves the lung infection status for at least three years in our cohort of patients with CF and may postpone chronic lung infection with GNB and thus stabilize lung function.
— The procedure is a major undertaking and described in their previous paper (Aaneas K et al, 2013. 23943728). After BAL under general anesthetic, the paranasal sinuses were ventilated and drained to make these accessible for postoperative instrumental cleansing and irrigation with saline and antibiotics. More extensive surgery of the frontal and ethmoid sinuses was undertaken based on the basis of preoperative CT scan and operative findings. As a standard unicinectomy, an anterior ethmoidectomy and medial antrostomy, leaving a relatively large maxillary ostium involving more than half the medial maxillary wall. Any intramucosal abscesses were resected along with other inflamed mucosal tissue when accessible. Following the surgical procedure, the opened and now accessible sinuses were irrigated with saline and colistimethate sodium. After 2 weeks intravenous antibiotics twice daily sinus irrigations with saline and antibiotics were carried out for six months. The authors concluded ESS with adjuvant therapy significantly improves the lung infection status for at least three years in our cohort of patients with CF and may postpone chronic lung infection with GNB and thus stabilise lung function.
Dr Mikkel Alalnin (fig. 7) is head of surgery in the Otorrhinolaryniology Dept of the Rigshospitalet in Copenhagen
Barker DH, Quittner AL. Parental Depression and Pancreatic Enzymes Adherence in Children With Cystic Fibrosis. 2016; 137(2):e20152296. [PubMed]

Fig. 8 David Barker
Parent caregivers often report elevations in depression, and parental depression may adversely affect children’s adherence. This prospective study evaluated adherence to pancreatic enzymes in 83 patients (1-13 years). Adherence to pancreatic enzymes was 49.4% +/- 3.4%. Adherence was higher at school (94.4% +/- 6.1%) than at home (42.3% +/- 3.1%), and higher for toddlers (50.6% +/- 5.2%) than for school-aged children (37.5% +/- 3.7%). Parents reported high rates of depressive symptoms (30% in the clinical range, 18% with moderate symptoms). Children of parents with symptoms of depression versus those without were less adherent (34.8% +/- 4.5% vs 48.5% +/- 4.1%), and adherence to enzymes was significantly related to 3-month weight outcomes. Average gain in weight z scores across 3 months was 0.5 +/- 0.2for children who were >50% adherent and -0.1 +/- 6.1for children who were <33% adherent. Parental depression had a signifcant, indirect effect on weight via adherence (-0.005 +/- 0.003 gain in weight z score per CES-D unit ).
The authors concluded the high rates of parental depressive symptoms, coupled with its negative effects on adherence, suggest that measuring and treating parental depression may improve children’s adherence to therapy.
— The burden and stress of having a child with CF for the parents is well seen in this study (30% in the clinical range of depression and 18% with moderate symptoms) – also the adverse effect of such stress on adherence and ultimately on the physical condition of their child. it is not surprising that the majority of people who have close experience of CF would avoid having an affected child if given the choice through population or antenatal screening.
Dr. David Barker (fig. 8) is a staff psychologist at Rhode Island Hospital in the Department of Child and Adolescent Psychiatry..
Beard CA; Amor DJ; Di Pietro L; Archibald AD. “I’m Healthy, It’s Not Going To Be Me”: Exploring experiences of carriers identified through a population reproductive genetic carrier screening panel in Australia. Am J Med Genet Part A. 2016; 170(8):2052-9. pubmed.ncbi.nlm.nih.gov/27150953/
Advancing genetic testing technologies mean that population-based carrier screening for multiple inherited conditions is now available. As the number of genetic conditions being screened increases, there is a need for research into how people experience these screening programs.
This research aimed to explore how women experience simultaneous carrier screening for three inherited conditions: cystic fibrosis (CF), spinal muscular atrophy (SMA), and fragile X syndrome (FXS). A qualitative approach was adopted using in-depth semi-structured interviews to explore the experiences of ten female participants: five SMA carriers, three CF carriers, and two FXS premutation carriers. Eight participants were pregnant when offered screening by their general practitioner or obstetrician and the decision to have screening was described as straightforward. Participants reported experiencing emotional responses such as anxiety and stress while waiting for either their partner’s carrier screen result (CF or SMA carriers) or the pregnancy’s CVS result (FXS carrier) and sought additional information about the relevant condition during this time
Most participants were in favour of population carrier screening for these conditions, preferably prior to conception. Genetic counsellors played an essential role in supporting couples after they received a carrier result given the variable consent processes undertaken when screening was offered. Further research should focus on the development of reliable online information tailored to people receiving carrier results and strategies for raising awareness of the availability of population carrier screening within the community.
Catherine A Beard is in the Department of Paediatrics, University of Melbourne, and the Murdoch Childrens Research Institute, Melbourne, Victoria, Australia.
Blackman SM; Tangpricha V. Endocrine disorders in cystic fibrosis. Pediatric Clinics of North America. 63(4):699-708, 2016 Aug. [PubMed]

Fig 9. Scott Blackman Johns Hopkins CF Center
Cystic fibrosis is frequently complicated by endocrine disorders. Diabetes can be expected to affect most with CF and pancreatic insufficiency and varies widely in age of onset, but early identification and treatment improve morbidity and mortality. Short stature can be exacerbated by relative delay of puberty and by use of inhaled corticosteroids. Bone disease in CF causes fragility fractures and should be assessed by monitoring bone mineral density and optimizing vitamin D status. Detecting and managing endocrine complications in CF can reduce morbidity and mortality in CF. These complications can be expected to become more common as the CF population ages.
Scott Michael Blackman (fig.9) is Associate Professor of Pediatrics at Johns Hopkins, Baltimore. To improve the clinical care for people with endocrine complications of CF, he started a multidisciplinary clinic for paediatric patients with CF and cystic fibrosis-related diabetes.
Blasi F; Page C; Rossolini GM; Pallecchi L; Matera MG; Rogliani P; Cazzola M. The effect of N-acetylcysteine on biofilms: Implications for the treatment of respiratory tract infections. Resp Med 2016;117:190-7. [PubMed]

Fig. 10 Francesco Blasi www.unimi.it
Difficulty in eradicating biofilms with systemic antibiotics has led clinicians to consider the possible role of non-antibiotic therapy. The aim of this review is to examine current evidence for the use of N-acetylcysteine (NAC) in the treatment of biofilm-related respiratory infections. However, the usefulness of NAC in the treatment of cystic fibrosis and bronchiectasis is still matter of debate. Most of the studies published to date have used oral or intramuscular NAC formulations. Evidence from in vitro studies indicates that NAC has good antibacterial properties and the ability to interfere with biofilm formation and disrupt biofilms. The authors note that results from clinical studies have provided some encouraging findings that need to be confirmed and expanded using other routes of administration of NAC such as inhalation.
— Papers on N-acetyl cysteine continue to appear but, rightly or wrongly, the drug is little used for CF in the UK.
Francesco Blasi (fig.10) is professor in the Department of Pathophysiology and Transplantation, University of Milan, IRCCS Fondazione Cà Granda Ospedale Maggiore Policlinico, Milan, Italy He has been the president of European Respiratory Society during 2012–13. and has served as the president of Italian Respiratory Society during 2015–17.
Bombard Y; Miller FA; Barg CJ; Patton SJ; Carroll JC; C; Milburn J; Ratjen F; Guttmann A; Hayeems RZ. A secondary benefit: the reproductive impact of carrier results from newborn screening for cystic fibrosis. Genet Med 2016 Sep 8. doi:10.1038/gim.2016.125. [PubMed]

Fig. 11 Yvonne Bombard
Unity Health Toronto
The authors examined the reproductive impact of carrier result disclosure of newborn screening for CF in Ontario. They surveyed mothers of carrier infants after NBS (Time 1) and 1 year later (Time 2) to ascertain intended and reported communication of their infants’ carrier results to relatives, carrier testing for themselves/other children, and reproductive decisions. A sub-sample of mothers was also interviewed at Time 1 and Time 2.The response rate was 54%. A little more than half (55%) of mothers underwent carrier testing at Time 1; another 40% of those who intended to undergo testing at Time 1 underwent testing at Time 2. Carrier result communication to relatives was high (92%), but a majority of participants did not expect the results to influence family planning (65%). All interviewed mothers valued learning their infants’ carrier results. Some underwent carrier testing and then shared results with family. Others did not use the results or used them in unintended ways. Mothers valued learning carrier results from NBS, they reported moderate uptake of carrier testing and limited influence on family planning. The study highlights the secondary nature of the benefit of disclosing carrier results of NBS
— The identification of a screened newborn as a carrier of a CF mutation is an incidental opportunity to determine which parent also carries the mutation and undertake cascade screening of his/her blood relatives. It is unfortunate that the take up of such an opportunity is so modest. Failure to divulge such information must now be regarded as unacceptable.
Dr. Yvaonne Bombard (fig 11) is a genomics health services researcher and Scientist at the Li Ka Shing Knowledge Institute of St. Michael’s Hospital. She is an Assistant Professor at the University of Toronto in the Institute of Health Policy Management and Evaluation.
Bosch B; De Boeck K. Searching for a cure for cystic fibrosis. A 25-year quest in a nutshell. Euro J Pediatr 2016; 175(1):1-8. [PubMed]

Fig.12 Barbara Bosch cipp-meeting.org
After 25 years of intensive search, there is not yet a cure for cystic fibrosis (CF). However, the quest has led to major breakthroughs in understanding the basic disease defect and defining strategies to correct it. The first cystic fibrosis transmembrane conductance regulator (CFTR) modulators have been introduced in clinic. Some show an impressive clinical benefit, like the potentiator ivacaftor for the 4% of patients with a class III defect. Others offer at present only a limited benefit, like the combination corrector lumacaftor plus potentiator ivacaftor for subjects homozygous for F508del. These findings prove that the basic defect in CF can be modified and hold the promise that one day CF will no longer be a life-shortening disease. CONCLUSION: This review updates the clinician on recent achievements as well as on the CF research pipeline. WHAT IS KNOWN: Cystic fibrosis (CF) is a common and life-shortening disease that currently cannot be cured. However, for each of the six CF mutation classes, disease-modifying drugs are under way. WHAT IS NEW: This review is a concise update for the clinician on new drugs that reached the CF clinical pipeline. The research strategies in CF have become a paradigm for clinical trials in other inherited diseases.
Barbara Bosch (fig.12) is in the Department of Paediatric Pulmonology, University Hospitals Leuven, Herestraat 49, 3000, Leuven, Belgium. Winner of the International Congress on Paedaitric Pulmonology Award, Prague.
Bratcher PE; Rowe SM; Reeves G; Roberts T; Szul T; Harris WT; Tirouvanziam R; Gaggar A. Alterations in blood leukocytes of G551D-bearing cystic fibrosis patients undergoing treatment with ivacaftor. J Cyst Fibros 2016; 15(1):67-73. [PubMed]

Fig 13. Preston Bratcher
Ivacaftor improves clinical outcome by potentiation of mutant G551D CFTR. Due to the presence of CFTR in monocytes and polymorphonuclear neutrophils (PMNs), we hypothesized that ivacaftor may impact leukocyte activation. METHODS: We examined blood leukocytes from G551D CF subjects prior to and at one and six months after receiving ivacaftor. Blood leukocytes from ivacaftor-naive G551D, F508del, and healthy controls were also treated with ivacaftor ex vivo to assess mutation-specific effects.Compared to healthy controls, G551D CF subjects had significantly higher expression of active CD11b on PMNs and of CD63 on monocytes, which were normalized by in vivo ivacaftor treatment. Ex vivo exposure to ivacaftor of blood cells from G551D, but not F508del and healthy subjects, resulted in changes in CXCR2 and CD16 expression on PMNs.
The authors concluded in vivo and ex vivo exposure of G551D CF leukocytes to ivacaftor resulted in an altered activation profile, suggesting mutation-specific leukocyte modulation.
Dr. Preston Bratcher (fig.13) is a scientist working at National Jewish Health, Denver; his research is focused on pulmonary inflammation and the innate immune sytem of the lung.
Button BM, Wilson C, Dentice R,et al. Physiotherapy for cystic fibrosis in Australia and New Zealand: A clinical practice guideline. Respirology. 2016 May;21(4):656-67. doi: 10.1111/resp.12764. Epub 2016 Apr 18. [PubMed] Free PMC Article

Fig. 14 Brenda Button
Monash University
The aim of this guideline is to optimise the physiotherapy management of people with CF in Australia and New Zealand. A systematic review of the literature in key areas of physiotherapy practice for CF was undertaken. Recommendations were formulated based on National Health and Medical Research Council (Australia) guidelines and considered the quality, quantity and level of the evidence; the consistency of the body of evidence; the likely clinical impact; and applicability to physiotherapy practice in Australia and New Zealand.
A total of 30 recommendations were made for airway clearance therapy, inhalation therapy, exercise assessment and training, musculoskeletal management, management of urinary incontinence, managing the newly diagnosed patient with CF, delivery of non-invasive ventilation, and physiotherapy management before and after lung transplantation. These recommendations can be used to underpin the provision of evidence-based physiotherapy care to people with CF in Australia and New Zealand.
– This is a comprehensive review of physiotherapy for CF in Australia and New Zealand and the free article is a valuable review of present best practice.
Barbara Button (fig.14) is a senior clinical physiotherapist and Adjunct Clinical Associate Professor at the Alfred Hospital. She has published extensively on a wide variety of CF subjects.
Bryant JM, Grogono DM, Rodriguez-Rincon D, Everall I, Brown KP, Moreno P, et al. Emergence and spread of a human-transmissible multidrug-resistant nontuberculous mycobacterium. Science. 2016 Nov 11;354(6313):751-757. [PubMed]

Fig. 15 Josie Bryant
Wellcome Sanger Institute
Lung infections with Mycobacterium abscessus, a species of multidrug-resistant nontuberculous mycobacteria, are emerging as an important global threat to individuals with cystic fibrosis (CF), in whom M. abscessus accelerates inflammatory lung damage, leading to increased morbidity and mortality. Previously, M. abscessus was thought to be independently acquired by susceptible individuals from the environment. However, using whole-genome analysis of a global collection of clinical isolates, we show that the majority of M. abscessus infections are acquired through transmission, potentially via fomites and aerosols, of recently emerged dominant circulating clones that have spread globally. We demonstrate that these clones are associated with worse clinical outcomes, show increased virulence in cell-based and mouse infection models, and thus represent an urgent international infection challenge.
Josephine M Bryant (fig.15) is at the Wellcome Trust Sanger Institute, Hinxton, UK.and the University of Cambridge Department of Medicine, MRC-Laboratory of Molecular Biology, Cambridge, UK.
Burke DG, Harrison MJ, Fleming C, McCarthy M, Shortt C, Sulaiman I, Murphy DM, Eustace JA, Shanahan F, Hill C, Stanton C, Rea MC, Ross RP, Plant BJ. Clostridium difficile carriage in adult cystic fibrosis (CF); implications for patients with CF and the potential for transmission of nosocomial infection. J Cyst Fibros. 2016 Nov 29. pii: S1569-1993(16)30610-5. doi: 10.1016/j.jcf.2016.09.008. [Epub ahead of print] [PubMed]
Despite increasing carriage rates and the presence of C. difficile toxin in stool, patients with CF rarely appear to develop typical manifestations of C. difficile infection (CDI). C. difficile was detected in 50% (30/60) of patients with CF by culturing for the bacteria. C. difficile toxin was detected in 63% (19/30) of C. difficile-positive stool samples. All toxin-positive stool samples contained toxigenic C. difficile strains harbouring toxin genes, tcdA and tcdB. Despite the presence of C. difficile and its toxin in patient stool, no acute gastrointestinal symptoms were reported. Ribotyping of C. difficile strains revealed 16 distinct ribotypes (RT), 11 of which are known to be disease-causing including the hyper-virulent RT078. Additionally, strains RT002, RT014, and RT015, which are common in non-CF nosocomial infection were described. All strains were CF susceptible to vancomycin, metronidazole, fusidic acid and rifampicin.
No correlation was observed between carriage of C. difficile or any characteristics of isolated strains and any recorded clinical parameters or treatment received. The study demonstrates a high prevalence of hypervirulent, toxigenic strains of C. difficile in asymptomatic patients with CF. This highlights the potential role of asymptomatic patients with CF in nosocomial transmission of C. difficile.
– Further confirmation of the common asymptomatic carriage of C. difficile by people with CF. The authors review the situation regarding the potential for cross infection and also the possible gut-lung axis relationship. They suggest that further studies are needed with regard to the need for eradication.
D G Burke is at the APC Microbiome Institute, University College Cork, Ireland.
Burgess JC, Bridges N, Banya W, Gyi KM, Hodson ME, Bilton D, Simmonds NJ. HbA1c as a screening tool for cystic fibrosis related diabetes. J Cyst Fibros. 2016 Mar;15(2):251-7. doi: 10.1016/j.jcf.2015.03.013. Epub 2015 Apr 11. [PubMed]
Early diagnosis of cystic fibrosis (CF) related diabetes (CFRD) is important to improve outcomes. International guidelines recommend an oral glucose tolerance test (OGTT) for all CF patients aged ≥10 years – this approach is controversial. The aim of this study was to develop an effective screening tool and reduce the need for a universal OGTT.Adult CF patients (without CFRD) attending an annual review assessment at the Royal Brompton, London were recruited prospectively (March 2009-July 2012) into two sequential studies – a primary investigative study followed by validation study. All patients underwent an OGTT and were simultaneously screened by predetermined biochemical/clinical criteria to identify their risk of CFRD. A sensitivity/specificity analysis was performed using the World Health Organisation diabetes criteria as gold standard; modifications were made to improve the screening tool’s accuracy and determine the optimal screening thresholds. This was tested in the validation study.429 patients (primary, n=94; validation, n=335: mean age=31.7 ± 10.4(SD), 43% female, 77% on pancreatic supplements). Primary study: in predicting a positive OGTT, the test sensitivity was 66.7% and specificity 60%. HbA1c was carried over to the validation study as it was the most discriminative (optimal threshold ≥5.8% (40 mmol/mol); receiver operating curve, ROC, score 0.60). Validation study: the number of patients with a normal, impaired and diabetic OGTT was 268 (80%), 51(15.2%) and 16(4.8%), respectively. HbA1c provided a test sensitivity, specificity and ROC score of 93.8%, 53.0% and 0.73, respectively.
The authors concluded that the use of HbA1c ≥ 5.8% (40 mmol/mol) is an effective tool for CFRD screening and reduced the need for an OGTT by 50.7%.
Juliana Burgess is at the National Heart and Lung Institute, Imperial College, London, United Kingdom; Adult Cystic Fibrosis Centre, Royal Brompton Hospital, London, United Kingdom.
Boudreau V, Coriati A, Desjardins K, Rabasa-Lhoret R. Glycated hemoglobin cannot yet be proposed as a screening tool for cystic fibrosis related diabetes. J Cyst Fibros. 2016 Mar;15(2):258-60. doi: 10.1016/j.jcf.2016.02.005. [PubMed]

Fig 16. Remi Rabassa-Lhoret
With improved life expectancy of cystic fibrosis (CF) patients, CF-related diabetes (CFRD) has become a major complication. The oral glucose tolerance test (OGTT) is the standard test to detect it. However, the use of OGTT is controversial, in addition to being a burden for patients and the treatment team. Research to find alternative ways of testing is ongoing. While some propose that glycated hemoglobin (HbA1c) may be an effective alternative, our past results suggest otherwise.A new analysis involving the OGTT and HbA1c values of 207 patients, between 2004 and 2015, proposes that the threshold of a lower value of HbA1c of ≥5.8%(39.9 mmol/mol) gives a sensitivity of 68.2% and a specificity of 60.5%. With such sensitivity to identify patients in need of an OGTT, 31.8% of CFRD diagnosis would be missed if the suggested HbA1c value of ≥5.8% was used as a screening tool to identify patients in need of OGTTs.
– Considering their results, the authors believe the HbA1c does not possess the characteristics of a suitable screening test for CFRD as 31.8% would be missed.
Dr. Remi Rabasa-Lhoret, (fig. 16) the corresponding author, is Director of the Metabolic Unit in the Nutrition Department in the endocrine service of the Montreal University Hospital.
Widger J; Hameed S; Ooi CY; Verge C. Using HbA1c as a screening tool for Cystic Fibrosis Related Diabetes. J Cyst Fibros 2006; 15(2):263-4. [PubMed]

Fig 17 John Widger
Using the proposed cut off for HdA1c (5.8%) would fail to detect patients with early glucoseabnormalities. Therefore until it is clarified if insulin treatment should be offered to patients with early insulin deficiency the authors caution against the use od HbA1c as a screening tool in this population.
John Widger (fig. 17) is Staff Specialist and Head of Respiratory Medicine, Sydney Children’s Hospital, Randwick
Schnyder MA; Benden C; Schmid C. bA1c: An effective screening tool for cystic fibrosis related diabetes?. J Cyst Fibros 2016; 15(2):261-2.[PubMed]

Fig 18. Marie-Angela Schnyder
Recently HbA1c has been accepted as a diagnostic criterion fir Type 1 and type 2 diabetes if 6.5% or more. This would have a poor sensitivity to detect CFRD – the same is true for fasting plasma glucose of 7mmol/l or more. By contrast a 2hr glucose value of 11.1mmol/l or more remains an accepted criterion for Type1 and type2 diabetes and CFRD. In the context of severely ill patients referred to this transplant centre, impaired insulin secretion is also important and is more reliably reflected and identified by a high 2hr plasma glucose than by a high FPG or HbA1c. In patients in good condition, a low HbA1c could possibly serve as to reduce the numbers of oral glucose tolerance tests (oGTT) but in patients with advanced CF lung disease in poor condition with a high probability of insulinopenia oGTT is preferred as these patients my benefit from insulin treatment beyond the control of hyperglycaemia ideally improving muscle and lung functions.
Marie-Angela Schnyder (fig.18) works in the Department of Endocrinology, Diabetology and Clinical Nutrition, University Hospital, Zurich.
Onady GM; Stolfi A. Insulin and oral agents for managing cystic fibrosis-related diabetes. [Review][Update of Cochrane Database Syst Rev. 2013;(7):CD004730; PMID: 23893261] Cochrane Database of Systematic Reviews. 4:CD004730, 2016. [PubMed]

Fig. 18a Gary Onady
LinkedIn
The Cystic Fibrosis Foundation recommends both short-term and long-acting insulin therapy when cystic fibrosis-related diabetes has been diagnosed. Diagnosis is based on: an elevated fasting blood glucose level greater than 6.94 mmol/liter (125 mg/deciliter); or oral glucose tolerance tests greater than 11.11 mmol/liter (200 mg/deciliter) at two hours; or symptomatic diabetes for random glucose levels greater than 11.11 mmol/liter (200 mg/deciliter); or glycated hemoglobin levels of at least 6.5.
This is a detailed review and the authors have not found any significant conclusive evidence that long-acting insulins, short-acting insulins or oral hypoglycemic agents have a distinct advantage over one another in controlling hyperglycemia or clinical outcomes associated with cystic fibrosis-related diabetes. While some cystic fibrosis centers use oral medications to help control diabetes, the Cystic Fibrosis Foundation (USA) clinical practice guidelines support the use of insulin therapy and this remains the most widely-used treatment method. Randomized controlled trials specifically related to controlling diabetes with this impact on the course of pulmonary disease process in cystic fibrosis continue to be a high priority.There is no demonstrated advantage yet established for using oral hypoglycemic agents over insulin, and further trials need to be evaluated to establish whether there is clear benefit for using hypoglycemic agents. Agents that potentiate insulin action, especially agents with additional anti-inflammatory potential should be further investigated to see if there may be a clinical advantage to adding these medications to insulin as adjuvant therapy.
Gary M Onady (fig. 18a) is at the Boonshoft School of Medicine, Wright State University, Room 105, Medical Sciences Building, 3640 Colonel Glenn Highway, Dayton, Ohio, USA, OH 45435. Prof. Onady also studied jazz trumpet.
Balfour-Lynn IM, Welch K. Inhaled corticosteroids for cystic fibrosis. Cochrane Database Syst Rev. 2016 Aug 23;8:CD001915. doi: 10.1002/14651858.CD001915.pub5.

Fig. 19 Ian Balfour-Lynn rbht.nhs.uk
To assess the effectiveness of taking regular inhaled corticosteroids, compared to not taking them, in children and adults with cystic fibrosis. Randomised or quasi-randomised trials, published and unpublished, comparing inhaled corticosteroids to placebo or standard treatment in individuals with cystic fibrosis.The searches identified 34 citations, of which 26 (representing 13 trials) were eligible for inclusion. These 13 trials reported the use of inhaled corticosteroids in 506 people with cystic fibrosis aged between six and 55 years. Although the previous publications come in for the customary Cochrane criticism (!), there is little doubt that some children with CF do benefit from inhaled corticosteroids. Although the authors state withdrawal in those already taking them has been shown to be safe, this has not been shown to apply to all children on inhaled steroids as some parents and paediatricians were unwilling to stop the drugs and so were not included in the writer’s trial.
— In this reviewer’s opinion it would be wise to consider the individual patient’s clinical history prior to their starting inhaled steroids before considering withdrawing the treatment. Note that the summary of the article (Balfour-Lynn et al, 2006) does not mention the 24 patients whose steroids the clinicians and/or parents were unwilling to stop; they had more asthma, more were atopic and they had more exacerbations and were in a worse condition. Many of these patients are considerably, even dramatically, improved when they commence inhaled steroids. Trials of N=1 are obviously useful in this clinical situation.
Ian Balfour-Lynn (fig.19) is a consultant in paediatric respiratory medicine based at Royal Brompton Hospital, London and is co-director of children’s services at the Trust.
Borowitz D, Lubarsky B, Wilschanski M, Munck A, Gelfond D, Bodewes F, Schwarzenberg SJ. Nutritional Status Improved in Cystic Fibrosis Patients with the G551D Mutation After Treatment with Ivacaftor. Dig Dis Sci. 2016 Jan;61(1):198-207. doi: 10.1007/s10620-015-3834-2. Epub 2015 Aug 7. [PubMed]

Fig 20. Drucy Borowitz cysticfibrosisnewstoday.com
To further analyze improvements in weight and body mass index (BMI) in two studies of ivacaftor in patients aged ≥6years with CF and the G551D mutation.Patients were randomized 1:1 to ivacaftor 150mg or placebo every 12h for 48weeks. Primary end point (lung function) was reported previously. Other outcomes included weight and height measurements and CF Questionnaire-Revised (CFQ-R).Studies included 213 patients (aged≤20years, n=105; aged>20years, n=108). In patients ≤20years, adjusted mean change from baseline to week 48 in body weight was 4.9 versus 2.2kg (ivacaftor vs. placebo, p=0.0008). At week 48, change from baseline in mean weight-for-age z-score was 0.29 versus -0.06 (p<0.0001); change in mean BMI-for-age z-score was 0.26 versus -0.13 (p<0.0001). In patients >20years, adjusted mean change from baseline to week 48 in body weight was 2.7 versus -0.2kg (p=0.0003). Mean BMI change at week 48 was 0.9 versus -0.1kg/m(2) (p=0.0003). There was no linear correlation evident between changes in body weight and improvements in lung function or sweat chloride. Significant CFQ-R improvements were seen in perception of eating, body image, and sense of ability to gain weight
Drucy Borowitz (fig.20) is the vice president of community partnerships at the CF Foundation. For more than 25 years, Drucy was the CF center director at the Women and Children’s Hospital of Buffalo, and she is a clinical professor of pediatrics at the Jacobs School of Medicine of the University at Buffalo.
Bourke SJ, Booth Z, Doe S, Anderson A, Rice S, Gascoigne A, Quibell R. A service evaluation of an integrated model of palliative care of cystic fibrosis. Palliat Med 2016: 30(7):698-702. [PubMed]

Fig. 21 Stephen J Bourke Newcastle Hospitals.nhs.uk
Patients with advanced cystic fibrosis have severe symptoms with a complex trajectory of exacerbations and recovery. They are often awaiting lung transplantation, and many die without receiving specialist palliative care.We introduced an integrated model whereby palliative specialists joined the cystic fibrosis team to provide palliative care in parallel with standard care. A service evaluation of this model of care was undertaken in a prospective case series documenting symptoms and outcomes, the views of the cystic fibrosis team and the experience of the palliative specialists.Over 3 years, 28 (10%) of 282 patients attending the cystic fibrosis centre had specialist palliative care. They had advanced lung disease (mean forced expiratory volume in 1 s (FEV1) = 0.86 L (25% predicted)), and 17 died: 6 were on a transplant waiting list at death; 10 were unsuitable and 1 died post transplantation. All who died over these 3 years had specialist palliative care. Four patients had successful transplants. Assessment showed a high prevalence of breathlessness, cough, pain, vomiting and fatigue, with a significant impact on daily life.The cystic fibrosis team rated this model of care highly, felt that palliative care should be members of the team, and thought that patients had found it helpful. The palliative specialists gained knowledge of cystic fibrosis, found it beneficial to meet patients earlier in the disease, and identified unmet needs in managing bereavement and the effects of deaths on other patients with cystic fibrosis.This model has been successful in overcoming the difficulties in access to specialist palliative care for patients with cystic fibrosis.
– Unfortunately still an important area of care and management for many people with CF. This is a helpful record of experience from the team at the Adult CF Unit at Newcastle UK.
Stephen J Bourke (fig.21) is consultant respiratory physician in Department of Respiratory Medicine, Royal Victoria Infirmary, Newcastle upon Tyne, UK
Castellani C, Massie J, Sontag M, Southern KW. Newborn screening for cystic fibrosis information. Lancet Respir Med. 2016; 4(8):653-661. [PubMed]
In the past decade, NBS has undergone rapid expansion and an unprecedented number of infants with cystic fibrosis have access to early diagnosis and care. Cystic fibrosis NBS has now moved on from the development phase and is entering an era of consolidation. The authors suggest that in the future, research should focus on the rationalization and optimization of existing programmes, with particular attention to bioethical implications such as unwanted detection of carriers and inconclusive diagnoses.
– The “unwanted carrier detection issue” was considered a problem and discussed at some length in years gone by. However, failing to reveal carrier status now would be regarded as bad practice by most clinicians and relatives who appreciate the full serious implications of having CF. Many welcome the opportunity that carrier detection in the infant offers in terms of subsequent cascade screening for the family and relatives.
Castellani C, Tridello G, Tamanini A, Assael BM. Sweat chloride and immunoreactive trypsinogen in infants carrying two CFTR mutations and not affected by cystic fibrosis. Arch Dis Child. 2016 Jan 11. pii: archdischild-2015-309348. doi: 10.1136/archdischild-2015-309348. [Epub ahead of print. [PubMed]
Newborns with raised immunotrypsinogen levels who have non-pathological sweat chloride values and carry two cystic fibrosis transmembrane regulator (CFTR) mutations of which at least one is not acknowledged to be cystic fibrosis (CF)-causing are at risk of developing clinical manifestations consistent with CFTR-related disorders or even CF. It is not known whether newborns with similar genotypes and normal immunoreactive trypsinogen (IRT) may share the same risk. This study found that newborns with these characteristics and normal IRT have lower sweat chloride values than those with raised IRT (p=0.007)
.- Interesting information but perhaps could have been predicted. Presumably all will require careful follow up.
Castellani C, Picci L, Tridello G, Casati E, Tamanini A, Bartoloni L, Scarpa M, Assael BM. Cystic fibrosis carrier screening effects on birth prevalence and newborn screening. Genet Med. 2016 Feb;18(2):145-51. doi: 10.1038/gim.2015.68. Epub 2015 Jun 18. [PubMed]

Fig. 22 Carlo Castellani
The effects of cystic fibrosis (CF) carrier screening on birth prevalence trends and newborn screening (NBS) efficiency were evaluated by comparing two Italian regions; carrier screening was performed in one region (eastern region (ER)) and not in the other (western region (WR)). Annual births of infants with CF, NBS false-positive results, NBS uncertain diagnoses (borderline sweat chloride (BSC)), carrier tests performed, and carriers detected were monitored during the 1993-2013 period.
A total of 259 newborns with CF were detected. In the eastern region, 150 carrier couples were found. Mean annual percentage of birth prevalence decrease was 9% per 10,000 (P = 0.002) and was greater in the ER (15%, P = 0.0008; WR 1%, P = ns). The WR estimated birth prevalence was 1/3,589 in 1993 and 1/3,870 in 2013; in the ER it was 1/2,730 in 1993 and 1/14,200 in 2013. The ER birth prevalence correlated inversely with the number of carrier couples (P = 0.0032). The ratio between CF cases and NBS-positive results significantly decreased in the ER (1.6%, P = 0.0001) but not in the WR. The ratio between prevalence of BSC and of CF cases increased in the ER (P = 0.008) but not in the WR (P = 0.1).
Carrier screening was connected with a decrease in birth prevalence of CF. Poorer NBS performance was observed in the carrier screening area
— An example of how the introduction of CF carrier screening will significantly reduce the incidence of CF in a region. A similar effect has been reported to follow the introduction of general newborn CF screening.
Chevreul K, Michel M, Brigham KB, López-Bastida J, Linertová R, Oliva-Moreno J, Serrano-Aguilar P, Posada-de-la-Paz M, Taruscio D, Schieppati A, Iskrov G, Péntek M, von der Schulenburg JM, Kanavos P, Persson U, Fattore G; BURQOL-RD Research Network. Social/economic costs and health-related quality of life in patients with cystic fibrosis in Europe. Eur J Health Econ. 2016 Apr 8. [Epub ahead of print. [PubMed]
A cross-sectional study was carried out on adults and children with CF in eight European countries. A total of 905 patients with CF was included (399 adults and 506 children). The total average annual cost per patient varied from €21,144 in Bulgaria to €53,256 in Germany. Adults had higher direct healthcare costs than children, but children had much higher informal care costs (P<0.0001). Total costs increased with patients’ level of dependence. There was no difference in caregiver HRQOL regardless of whether they cared for an adult or a child. However, caregivers who looked after a child had a significantly higher burden (P=0.0013)
– The study highlights the burden of CF in terms of costs and decreased health related quality of life for both the people with CF and their caregivers throughout Europe.( I have not read full article so not sure relation to use of modulators)
Callemeyn J, van Haecke P; Peetermans WE; Blockmans D. Clubbing and hypertrophic osteoarthropathy: insights in diagnosis, pathophysiology, and clinical significance. Acta Clinica Belgica 2016; 71(3):123-30. [PubMed]

Fig. 23 Jasper Callemeyn
ResearchGate
This article reviews clinical criteria and pathophysiology of clubbing and hypertrophic osteoarthropathy (HOA). A diagnostic algorithm is proposed, based on etiology and current insights. The prognostic impact on associated diseases is discussed. The Internet databases Medline and Embase were searched. Articles were selected based on relevance of abstract, article type and impact of the journal.
Diagnostic criteria include Lovibond’s profile sign, distal/interphalangeal depth ratio and Schamroth’s sign. Three pathophysiological causes of clubbing can be distinguished: hypoxia, chronic inflammation and aberrant vascularization. A prominent role for vascular endothelial growth factor is suggested. Associated symptoms and clinical signs should guide the initial diagnostic evaluation. Finally, clubbing is a negative prognostic factor in certain pulmonary disorders, including cystic fibrosis.
Jasper Callemeyen (fig.23) is in the Department of Microbiology and Immunology at the Faculty of Medicine , KU Leuven University, Belgium.
Ceulemans LJ; Strypstein S; Neyrinck A; Verleden S; Ruttens D; Monbaliu D; De Leyn P; Vanhaecke J; Meyns B; Nevens F; Verleden G; Van Raemdonck D; Pirenne J. Combined liver-thoracic transplantation: single-center experience with introduction of the ‘Liver-first’ principle. Transplant Int 2016; 29(6):715-26. [PubMed]

Fig.24 Laurens Ceulemans
kuleuven.be
Combined liver/thoracic transplantation (cLiThTx) is a complex procedure for end-stage/advanced liver and heart(H)/lung(Lu) disease. Fourteen consecutive patients underwent cLiThTx: 3 cLiHTx, 10 cLiLuTx, and 1 cLiHLuTx. Recipient age was 42 years (17-63 years). Most frequent indications were cystic fibrosis (n = 5), hepatopulmonary fibrosis (n = 2), amyloidosis (n = 2), and epithelioid hemangio-endothelioma (n = 2). . Estimated 5-year patient survival is 90%. The authors concluded combined liver thoracic transplantation is safe with excellent short-/long-term surgical and immunological results.
Lauren Ceulemans (fig.24) is at the Department of Microbiology and Immunology, Abdominal Transplant Surgery, and the Department of Clinical and Experimental Medicine, Thoracic Surgery, University Hospitals Leuven, KU Leuven, Belgium.
Cil O; Phuan PW; Lee S; Tan J; Haggie PM; Levin MH; Sun L; Thiagarajah JR; Ma T; Verkman AS. CFTR activator increases intestinal fluid secretion and normalizes stool output in a mouse model of constipation. Cell Mol Gastroenterol Hepatol 2016 May 2(3): 317-327. [PubMed]

Fig. 25 Alan Verkman
The authors hypothesized that direct activation of CFTR would cause fluid secretion and reverse the excessive dehydration of stool found in constipation. A cell-based high-throughput screen was done for 120,000 drug-like, synthetic small molecules. Active compounds were characterized for mechanism of action and one lead compound was tested in a loperamide-induced constipation model in mice. Several classes of novel CFTR activators were identified, one of which, the phenylquinoxalinone CFTRact-J027, fully activated CFTR chloride conductance with EC50 ~ 200 nM, without causing elevation of cytoplasmic cAMP.
Orally administered CFTRact-J027 normalized stool output and water content in a loperamide-induced mouse model of constipation with ED50 ~0.5 mg/kg; CFTRact-J027 was without effect in cystic fibrosis mice lacking functional CFTR. Short-circuit current, fluid secretion and motility measurements in mouse intestine indicated a pro-secretory action of CFTRact-J027 without direct stimulation of intestinal motility. Oral administration of 10 mg/kg CFTRact-J027 showed minimal bioavailability, rapid hepatic metabolism and blood levels <200 nM, and without apparent toxicity after chronic administration.
The authors concluded CFTRact-J027 or alternative small-molecule CFTR-targeted activators may be efficacious for the treatment of constipation.
Alan Verkman (fig. 25) is Professor in the Departments of Medicine and Physiology, University of California, San Franscisco.
Collaco JM; Blackman SM; Raraigh KS; Corvol H; Rommens JM; Pace RG; Boelle PY; McGready J; Sosnay PR; Strug LJ; Knowles MR; Cutting GR. Sources of Variation in Sweat Chloride Measurements in Cystic Fibrosis. A J Resp Crit Care 2016 Jun 3. [PubMed]

Fig 26. Michael Callaco
Expanding the use of CFTR potentiators and correctors for the treatment of cystic fibrosis (CF) requires precise and accurate biomarkers. Sweat chloride concentration provides an in vivo assessment of CFTR function, but it is unknown the degree to which CFTR mutations account for sweat chloride variation.
2639 sweat chloride measurements were obtained in 1761 twins/siblings from the CF Twin-Sibling Study, French CF Modifier Gene Study, and Canadian Consortium for Genetic Studies. Variation in the CFTR gene was found to be the predominant cause of sweat chloride variation; most of the non-CFTR variation is due to testing variability and unique environmental factors. If test precision and accuracy can be improved, sweat chloride measurement could be a valuable biomarker for assessing response to therapies directed at mutant CFTR.
Michael Collaco (fig.26) is Assitant Professor of Pediatric Pulmonology at the Johns Hopkins School of Medicine.
Sarah Collins (Chair), Joanne Barrett, Caroline Elston, Alison Morton, Ruth Watling, Sue Wolfe.(Section Leads). Nutritional Management of Cystic Fibrosis. Second Edition, September 2016. Nutrition Working Group of the Cystic Fibrosis Trust. Full document available on the CF Trust website (www,cystic fibrosis .org.uk)

Fig 27 Sarah Collins
A detailed up to date account of nutritional management published by the UK CF Trust. Written by UK experts of great experience in this field, the document contains almost 400 references. The document updates the CF Trust’s previous 2002 guidelines. It represents what the current Nutrition Consensus Working Group and those who have contributed to the document consider to be the best clinical practice. The document has been reviewed by relevant experts in addition to peer reviews
Sarah Collins (fig.27) is specialist CF Dietitian at Kings College London.
Cohen-Cymberknoh M; Gilead N; Gartner S; Rovira S; Blau H; Mussaffi H; Rivlin J; Gur M; Shteinberg M; Bentur L; Livnat G; Aviram M; Picard E; Tenenbaum A; Armoni S; Breuer O; Shoseyov D; Kerem E. Eradication failure of newly acquired Pseudomonas aeruginosa isolates in cystic fibrosis. J Cyst Fibrosis 2016 Apr 30. [PubMed]

Fig 28. Malena Cohen-Cymberknoh
A study to determine eradication success rate of newly acquired PA and to identify characteristics associated with eradication failure. Data from patients with newly acquired PA infection from 2007 to 2013 were collected. Clinical variables were compared in patients with and without successful eradication for >1year. Of 183 patients out of 740 (25%) from 7 CF Centers that had newly acquired PA, eradication succeeded in 72%. Patients with the highest risk of failure had multi-resistant PA, fewer sputum cultureswere older, and were diagnosed at a later age. The risk of eradication failure increased by 1.3% with each year of delayed CF diagnosis; successful eradication increased by 17% with each additional sputum culture taken.The authors concluded delayed detection of PA infection leading to delayed treatment and growth of multi-resistant organisms is associated with eradication failure.
– This study confirms the now well-established fact that it is virtually impossible to eradicate Pseudomonas aeruginosa infection when it is chronically established. Delayed diagnosis and infrequent cultures will contribute to the percentage of eradication failures.
Dr Malena Cohen-Cymberknoh (fig. 28) is Senior Pediatrician and Specialist in Pediatric Pulmonology at Hadassah Hospital, Israel.
Cohen-Cymberknoh M, Shoseyov D, Breuer O, Shamali M, Wilschanski M, Kerem E. Treatment of cystic fibrosis in low-income countries. Lancet Respir Med. 2016 Feb;4(2):91-2. doi: 10.1016/S2213-2600(15)00507-X. [PubMed]
The duration and quality of life of patients with cystic fibrosis in developed countries has been substantially improved in the past two decades. By contrast, individuals with cystic fibrosis who live in low-income settings without the resources necessary to optimise cystic fibrosis care tend to have a worse clinical outcome than those from more affluent areas, including later age at diagnosis, worse nutritional status, and worse lung function. Present cystic fibrosis care guidelines, generally designed to be used in developed countries, include treatments not available in resource-poor settings.
— This always likely to be the case with conditions requiring sophisticated and very expensive care. The situation regarding CF will be exacerbated by the crippling cost of the new mutation specific treatments.
Colombo C, Crosignani A, Alicandro G, Zhang W, Biffi A, Motta V, Corti F, Setchell KD. Long-Term Ursodeoxycholic Acid Therapy Does Not Alter Lithocholic Acid Levels in Patients with Cystic Fibrosis with Associated Liver Disease. J Pediatr. 2016 Jun 10. pii: S0022-3476(16)30216-5. doi: 10.1016/j.jpeds.2016.05.008. [Epub ahead of print]. [PubMed]

Fig 29. Carla Colombo
To evaluate the fasting and postprandial serum bile acid composition in patients with cystic fibrosis-associated liver disease (CFLD) after chronic administration of ursodeoxycholic acid (UDCA) (20mg/kg/day). The aim was to specifically focus on the extent of biotransformation of UDCA to its hepatotoxic metabolite, lithocholic acid, because of recent concerns regarding the safety of long-term, high-dose UDCA treatment for CFLD.Twenty patients with CFLD (median age 16years, range: 2.4-35.0) prescribed UDCA therapy for at least 2years were studied. Total and individual serum bile acids were measured by stable-isotope dilution mass spectrometry, in fasting and 2-hour postprandial samples taken during chronic UDCA (20mg/kg/day) administration.During chronic UDCA administration (median duration 8years, IQR: 6-16), UDCA became the predominant serum bile acid in all patients (median, IQR: 3.17, 1.25-5.56μmol/L) and chenodeoxycholic acid concentrations were greater than cholic acid (1.86, 1.00-4.70μmol/L vs 0.40, 0.24-2.71μmol/L). The secondary bile acids, deoxycholate and lithocholate, were present in very low concentrations in fasted serum (<0.05μmol/L). After UDCA administration, 2-hour postprandial concentrations of both UDCA and chenodeoxycholic acid significantly increased (P<.01), but no significant changes in serum lithocholic acid concentrations were observed.
— These data do not support recent suggestions that enhanced biotransformation of UDCA to the hepatotoxic secondary bile acid lithocholic occurs when patients with CFLD are treated with relatively high doses of UDCA.
Carla Colombo (fig.29) is Professor of Paediatrics in Milan and has pioneered the use of URSO for people with cystic fibrosis.
Cooney A L, Abou Alaiwa MH, Shah VS, Bouzek DC, Stroik MR, Powers LS, Gansemer ND, Meyerholz DK, Welsh MJ, Stoltz DA, Sinn PL, McCray PB Jr. Lentiviral-mediated phenotypic correction of cystic fibrosis pigs. JCI Iy Al, nsight. 2016 Sep 8;1(14). pii:e88730.1.pubmed.ncbi.nlm.nih.gov/27656681/

Fig.30Ashley Cooney sinn.lab.uiowa.edu
Regardless of the disease-causing CF mutation, gene therapy is a strategy to restore anion transport to airway epithelia. Indeed, viral vector-delivered CFTR can complement the anion channel defect. In this proof-of-principle study, functional in vivo CFTR channel activity was restored in the airways of CF pigs using a feline immunodeficiency virus-based (FIV-based) lentiviral vector pseudotyped with the GP64 envelope.
Three newborn CF pigs received aerosolized FIV-CFTR to the nose and lung. Two weeks after viral vector delivery, epithelial tissues were analysed for functional correction. In freshly excised tracheal and bronchus tissues and cultured ethmoid sinus cells, there was a significant increase in transepithelial cAMP-stimulated current, evidence of functional CFTR. In addition, we observed increases in tracheal airway surface liquid pH and bacterial killing in CFTR vector-treated animals.
— Together, these data provide the first evidence that lentiviral delivery of CFTR can partially correct the anion channel defect in a large-animal CF model and validate a translational strategy to treat or prevent CF lung disease.
Ashley Cooney (fig.30) is a postdoctoral scholar at Pappajohn Biomedical Institute, Roy J. and Lucille A. Carver College of Medicine
Deppisch C; Herrmann G; Graepler-Mainka U; Wirtz H; Heyder S; Engel C; Marschal M; Miller CC; Riethmuller J. Gaseous nitric oxide to treat antibiotic resistant bacterial and fungal lung infections in patients with cystic fibrosis: a phase I clinical study. Infection 2016; 44(4):513-20. [PubMed]
The authors assessed feasibility and safety of inhaled NO in eight CF patients who received 160 ppm NO for 30 min, three times daily for 2 periods of 5 days. The NO treatment was safe and in none of the patients were serious drug-related adverse events observed which caused termination of the study. The intention-to-treat analysis revealed a significant mean reduction of the colony forming units of all bacteria and all fungi, while mean forced expiratory volume 1 s % predicted (FEV1) relative to baseline increased 17.3 +/- 8.9 % (P = 0.012).
The authors concluded NO treatment may improve the therapy of chronic microbial lung infections in CF patients, particularly concerning pathogens with intrinsic or acquired resistance to antibiotics.
Caroline Deppisch is at the Comprehensive Cystic Fibrosis Center, Children’s Clinic, Tübingen, Germany.
Darrah RJ; Mitchell AL; Campanaro CK; Barbato ES; Litman P; Sattar A; Hodges CA; Drumm ML; Jacono FJ. Early pulmonary disease manifestations in cystic fibrosis mice. J Cyst Fibros 2016 May 23. [PubMed]

Fig. 31 Rebecca Darrah
case.edu
The authors investigated young CF mice to determine if they exhibit pulmonary pathophysiology consistent with the early CF lung phenotype. Lung histology and pulmonary mechanics were examined in 12- to 16-week-old congenic C57bl/6 F508del and R117H CF mice using a forced oscillation technique (flexiVent). RESULTS: There were no significant differences in the resistance of the large airways. However, in both CF mouse models, prominent differences in the mechanical properties of the peripheral lung compartment were identified including decreased static lung compliance, increased elastance and increased tissue damping. CF mice also had distal airspace enlargement with significantly increased mean linear intercept distances.An impaired ability to stretch and expand the peripheral lung compartment, as well as increased distances between gas exchange surfaces, were present in young CF mice carrying two independent Cftr mutations. This altered pulmonary histopathophysiology in the peripheral lung compartment, which develops in the absence of infection, is similar to the early lung
– These findings of early structural abnormalities in the absence of infection are in keeping with previously described tracheal and histological abnormalities.
Rebecca J Darrah (fig.31) is at the Frances Payne Bolton School of Nursing, Case Western Reserve University, Cleveland, OH 44106, United States; Department of Genetics and Genome Sciences, Case Western Reserve University, Cleveland, OH 44106, United S
Davis SD, Ratjen F, Brumback LC, Johnson RC, Filbrun AG, Kerby GS, Panitch HB, Donaldson SH, Rosenfeld M; ISIS Study Group. Infant lung function tests as endpoints in the ISIS multicenter clinical trial in cystic fibrosis. J Cyst Fibros 2016; 15(3):386-91. 26547590. [PubMed]

Fig. 32 Stephanie Davis
The Infant Study of Inhaled Saline (ISIS) in CF was the first multicenter clinical trial to utilise infant pulmonary function tests (iPFTs) as an endpoint. Secondary analysis of ISIS data was conducted in order to assess feasibility of iPFT measures and their associations with respiratory symptoms. The authors concluded iPFTs are not appropriate primary endpoints for multicenter clinical trials due to challenges of obtaining acceptable data and near-normal average raised volume measurements. However, raised volume measures have potential to serve as secondary endpoints in future clinical CF trials.
Dr Stephanie Davis (fig. 32) is a Paediatric Pulmonologist and Professor of Pediatrics at Indiana School of Medicine
Davies JC; Cunningham S; Harris WT; Lapey A; Regelmann WE; Sawicki GS; Southern KW; Robertson S; Green Y; Cooke J; Rosenfeld M; KIWI Study Group. Safety, pharmacokinetics, and pharmacodynamics of ivacaftor in patients aged 2-5 years with cystic fibrosis and a CFTR gating mutation (KIWI): an open-label, single-arm study.The Lancet Respir Med 2016; 4(2):107-15.[PubMed]

Fig. 33 Jane Davies Royal Brompton Hospital
Ivacaftor has been shown to be a safe, effective treatment for cystic fibrosis in patients aged 6 years or older with a CFTR gating mutation. The authors aimed to assess the safety, pharmacokinetics, and pharmacodynamics of ivacaftor in children aged 2-5 years.In the two-part KIWI study, we enrolled children aged 2-5 years weighing 8 kg or more with a confirmed diagnosis of cystic fibrosis and a CFTR gating mutation on at least one allele from 15 hospitals in the USA, UK, and Canada. Participants received oral ivacaftor 50 mg (if bodyweight <14 kg) or 75 mg (if bodyweight >14 kg) every 12 h for 4 days in part A (to establish the short-term safety of doses for subsequent assessment in part B), and then for 24 weeks in part B (to assess safety and longer-term pharmacodynamics). Children could participate in both or just one part of the study. Primary outcomes were pharmacokinetics and safety, analysed in all patients who received at least one dose of ivacaftor. Secondary outcomes were absolute change from baseline in sweat chloride concentrations and bodyweight, body-mass index (BMI), and height Z scores, and pharmacokinetic parameter estimation of ivacaftor. This study is registered with ClinicalTrials.gov, number NCT01705145.
Between Jan 8, 2013, and March 1, 2013, nine patients were enrolled onto part A of the study, all of whom completed the 4 day treatment period, and eight of whom took part in part B. Between June 28, 2013, and Sept 26, 2013, 34 patients were enrolled in part B, 33 of whom completed the 24 week treatment period. All patients received at least one dose of ivacaftor. Results of ivacaftor pharmacokinetics suggested that exposure was similar to that reported in adults (median Cmin were 536 ng/mL for the 50 mg dose; 580 ng/mL for the 75 mg dose; median ivacaftor AUC values were 9840 ng x h/mL and 10 200 ng x h/mL, respectively). Common adverse events in part B included cough (in 19 [56%] of 34 patients) and vomiting (in ten [29%]). Five (15%) patients had liver function test (LFT) results that were more than eight times higher than the upper limit of normal, four of whom had study drug interrupted, and one of whom had study drug discontinued. Six (18%) of 34 patients had seven serious adverse events; a raised concentration of transaminases was the only serious adverse event regarded as related to ivacaftor and the only adverse event that resulted in study treatment discontinuation. At week 24, in patients for whom we had data, sweat chloride had changed from baseline by a mean of -46.9 mmol/L (SD 26.2, p<0.0001), weight Z score by 0.2 (0.3; p<0.0001), BMI Z score by 0.4 (0.4, p<0.0001), and height Z score by -0.01 (0.3; p=0.84).
Ivacaftor at doses of 50 mg and 75 mg seems to be safe in children aged 2-5 years with cystic fibrosis with a gating mutation followed up for 24 weeks, although the frequency of elevated LFTs suggests that monitoring should be frequent in young children, particularly those with a history of elevated LFTs. Results of an ongoing extension study assessing durability of these effects and longer-term safety are warranted.
– This study confirmed that ivacaftor was safe and effective for children aged 2-5 years.
Jane Davies (Fig. 33) is Professor at Imperial College London, London, UK; Royal Brompton and Harefield NHS Foundation Trust, London, UK.
Dentice RL; Elkins MR; Middleton PG; Bishop JR; Wark PA; Dorahy DJ; Harmer CJ; Hu H; Bye PT. A randomised trial of hypertonic saline during hospitalisation for exacerbation of cystic fibrosis. Thorax. 71(2):141-7, 2016 Feb. [PubMed]

Fig. 34 Ruth Dentice
eMedEvents
To determine the effects of hypertonic saline inhalation during hospitalisation for exacerbation of CF.
132 adults with an exacerbation of CF were randomised to inhale three nebulised doses a day of either 4 mL 7% saline or a taste-masked control of 0.12% saline, throughout the hospital admission. The primary outcome measure was length of hospital stay.The authors concluded the addition of hypertonic saline to the management of a CF exacerbation did not reduce the length of hospital stay but hypertonic saline speeds the resolution of exacerbation symptoms and allows patients to leave hospital with greater symptom resolution.
– The authors do not state whether they have adopted the use of hypertonic saline as part of their regime for treating pulmonary exacerbations; they suggest that other centres should examine the possibility.
Ruth L Dentice (fig.44) is senior physiotherapist at the Department of Respiratory Medicine, Royal Prince Alfred Hospital, Sydney, New South Wales, Australia Sydney Medical School, University of Sydney, Sydney, New South Wales, Australia.
Doumit M, Belessis Y; Stelzer-Braid S; Mallitt KA; Rawlinson W; Jaffe A. Diagnostic accuracy and distress associated with oropharyngeal suction in cystic fibrosis. J Cyst Fibros 2016; 15(4):473-8. [PubMed]

Fig. 45 Michael Doumit
UNSW Sydney
This study aimed to assess the diagnostic accuracy of oropharyngeal suction (OPS) samples in obtaining airway bacterial cultures in young children with cystic fibrosis (CF), and the level of child distress caused by obtaining OPS samples.Young children with CF undergoing broncho-alveolar lavage (BAL) as part of concurrent research or routine annual surveillance were studied. OPS was performed by stimulating a cough and suctioning the back of the oropharynx in the awake child to replicate clinical practice. BAL of the right upper, middle and lingula lobes was then performed. Samples were sent for standard bacterial culture. The child’s distress during OPS was rated using the Groningen Distress Scale (1=calm, 2=timid/nervous, 3=serious distress but still under control, 4=serious distress with loss of control, 5=panic).
There were 65 paired samples obtained from 39 children (21 boys, mean age on day of first sampling was 34.1 months, SD 19.1 months). For Pseudomonas aeruginosa, specificity, sensitivity, NPV and PPV with 95% CI were 98% (87-99), 75% (20-96), 98% (91-98) and 60% (15-93%) respectively. In all age groups combined, median level of distress was 3 (IQR 2-4), with distress highest in 2 and 3 year olds, with a median of 4 (IQR 3-4).-
The authors concluded OPS has diagnostic utility in determining the absence of organisms in the lower airway, with specificity for P. aeruginosa detection of 98%. However, a positive OPS result is not necessarily a good indicator of lower airway infection. Distress levels were high during OPS, mostly in 2 and 3 year olds. They suggest there is a need for interventions to reduce distress or to find alternative methods which are less distressing.
Michael Doumit (fig. 45) is at Sydney Children’s Hospital, High St, Randwick, NSW2031, Australia; University of NSW, High St, Randwick, NSW2031, Australia.
Demir SO; Atici S; Akkoc G; Yakut N; Ikizoglu NB; Eralp EE; Soysal A; Bakir M. Neurologic Adverse Events Associated with Voriconazole Therapy: Report of Two Pediatric Cases. Case Reports Infectious Diseases. 2016:3989070, 2016. [PubMed]
The current report presents two cases, one a 9-year-old boy and the other a 17-year-old girl, who experienced neurologic side effects associated with voriconazole therapy. The first case was a 9-year-old boy with cystic fibrosis and invasive aspergillosis that developed photophobia, altered colour sensation, and fearful visual hallucination.
The second case was a 17-year-old girl with cystic fibrosis and allergic bronchopulmonary aspergillosis, and she experienced photophobia, fatigue, impaired concentration, and insomnia, when the dose of voriconazole therapy was increased from 12mg/kg/day to 16mg/kg/day. The complaints of the two patients disappeared after discontinuation of voriconazole therapy. In addition, although serum voriconazole concentration was not measured in the present cases, therapeutic drug monitoring for voriconazole seems to be critically important in preventing neurologic side effects in pediatric patients.
Sevilla Ocal Demir is at Marmara University School of Medicine, Department of Pediatrics, Division of Pediatric Infectious Diseases, 34912 Istanbul, Turkey.
Durham SH; Garza KB; Eiland LS. Relationship between vancomycin dosage and serum trough vancomycin concentrations in pediatric patients with cystic fibrosis. American Journal of Health-System Pharmacy. 73(13):969-74, 2016 Jul 1. [PubMed]The

Fig.46 Spencer Durham
ResearchGate
association between vancomycin dosage and serum trough vancomycin concentrations in pediatric patients with cystic fibrosis (CF) was examined. A study of hospital admissions involving pediatric patients with CF revealed no significant correlation, when all admissions were considered, between the initial or final vancomycin dosage regimen and the corresponding serum trough vancomycin concentration. Both correlations were significant for the subgroup of admissions representing patients who were at least 12 years old.
Spencer H Durham (fig.46) is at the Department of Pharmacy Practice, Auburn University Harrison School of Pharmacy, Auburn, AL.
Dryden C; Wilkinson J; Young D; Brooker RJ; Scottish Paediatric Cystic Fibrosis Managed Clinical Network (SPCFMCN). The impact of 12 months treatment with ivacaftor on Scottish paediatric patients with cystic fibrosis with the G551D mutation: a review. Arch Dis Child 2016 Jun 10. [PubMed]

Fig. 47 Carol Dryden
ResearchGate
The authors reviewed the impact of ivacaftor on Scottish paediatric patients with cystic fibrosis >6 years of age after 12 months of treatment. Statistically significant improvements in FEV1 and body mass index and a reduction in sweat chloride, all comparable with previously published data were observed. The findings also suggested reduced use of intravenous antibiotics and oral antibiotics. No significant adverse effects were observed but a possible association with cataract formation could not be excluded.This review suggests that, in the short term at least, ivacaftor is effective and safe in Scottish paediatric patients >6 years of age with G551D.
Carol Dryden (fig.47) is a consultant paediatrician at the Department of Paediatrics, Wishaw General Hospital, Wishaw, UK.
Dugueperoux I; L’Hostis C; Audrezet MP; Rault G; Frachon I; Bernard R; Parent P; Blayau M; Schmitt S; Genin E; Ferec C; Scotet V. Highlighting the impact of cascade carrier testing in cystic fibrosis families. J Cyst Fibros 2016; 15(4):452-9. [PubMed]
Cascade carrier testing within cystic fibrosis (CF) affected families offers relatives of CF patients the opportunity to know their status regarding the mutation that segregates within their family, and thus to make informed reproductive choices.
As an Australian study has recently shown that this test seemed underused, we searched to assess uptake of this test in a European area where CF is common, and to report its public health implications. METHODS: This study relied on 40 CF-affected families from western Brittany, France. Investigations included drawing of family trees and registration of carrier tests performed in those families.
RESULTS: Of the 459 relatives eligible for testing, 185 were tested, leading to an adjusted uptake rate of testing of 40.7% (95% CI: [34.1%; 47.3%]). The main predictors for having testing were being female (p=0.031) and having a high prior risk (p<0.001). Planning a pregnancy or expecting a child (reported in at least 38.4% of tested relatives) also appeared critical in choosing to be tested. Overall, carrier testing allowed to reassure more than 1/4 of the relatives and to detect five new 1-in-4 at-risk couples who then requested prenatal diagnosis.
CONCLUSIONS: This observational study assesses, for first time in Europe, uptake of CF cascade carrier testing within CF families, which is a critical tool to reassure non-carriers and to detect early new at-risk couples.
— The take-up of carrier testing by eligible relatives is usually a disappointing 40-50% as in this French study.
Ingrid Dugueperoux is at Inserm, UMR 1078, Brest, France; Univ. Brest, Brest, France; Etablissement Français du Sang-Bretagne, Brest, France.
Dellon EP, Chen E, Goggin J, Homa K, Marshall BC, Sabadosa KA, Cohen RI. Advance care planning in cystic fibrosis: Current practices, challenges, and opportunities. J Cyst Fibros. 2016 Jan;15(1):96-101. doi: 10.1016/j.jcf.2015.08.004. Epub 2015 Sep 8 .[PubMed]

Fig. 48 Elisabeth P Dellon
UNC School of Medicine
Studies in cystic fibrosis report late attention to advance care planning (ACP). The purpose of this study was to examine ACP with patients receiving care at US adult CF care programs.Chart abstraction was used to examine ACP with adults with CF dying from respiratory failure between 2011 and 2013.The authors reviewed 210 deaths among 67 CF care programs. Median age at death was 29 years (range 18-73). Median FEV1 in the year preceding death was 33% predicted (range 13-100%); 68% had severe lung disease with FEV1<40% predicted. ACP was documented for 129 (61%), often during hospitalisation (61%). Those with ACP had earlier documentation of treatment preferences, before the last month of life (73% v. 35%; p=<0.01). Advance directives were completed by 93% of those with ACP versus 75% without (p<0.01); DNR orders and health care proxy designation occurred more often for those with ACP. Patients awaiting lung transplant had similar rates of ACP as those who were not (67% v. 61%; p=0.55). The frequency of ACP varied significantly among the 29 programs contributing data from four or more deaths.Advanced care planning in CF often occurs late in the disease course. Important decisions default to surrogates when opportunities for ACP are missed. Provision of ACP varies significantly among adult CF care programs.
The authors suggest that careful evaluation of opportunities to enhance ACP and implementation of recommended approaches may lead to better practices in this important aspect of CF care.
Elisabeth P Dellon (Fig 48) is Medical Director Children’s Supportive Care Team at the University of North Carolina School of Medicine, Chapel Hill, NC, United States.
Darrah R, Nelson R, Damato EG, Decker M, Matthews A, Hodges CA. Growth Deficiency in Cystic Fibrosis Is Observable at Birth and Predictive of Early Pulmonary Function. Biol Res Nurs. 2016 Oct;18(5):498-504. doi: 10.1177/1099800416643585. Epub 2016 Apr 13.[PubMed]
Greater body mass at an early age is associated with improved pulmonary function, but it is unknown at what age weight becomes predictive of pulmonary disease severity. The purpose of this study was to investigate the relationship between birth weight and pulmonary function in CF.Birth weight was significantly lower in babies with CF and correlated with pulmonary disease at ages 6 and 10 years but not with age at which Pseudomonas aeruginosa colonisation was observed.
The authors note these data suggest that CF growth deficiency has prenatal origins. Early nutritional intervention for babies with CF and a low birth weight is warranted to maximise pulmonary potential
— It is now well documented that growth deficiency in CF has prenatal origins (Hsia DY. 1- 959. pubmed.ncbi.nlm.nih.gov/14403569/; affected infants were significantly lighter than their unaffected sibs. Not only is the birth weight of CF infants significantly less than control infants but the skull circumference is also reduced (Ghosal S et al, 1995 pubmed.ncbi.nlm.nih.gov/7702380/). The degree of growth deficiency evident at birth may be a measure of the severity e.g. more marked in those with meconium ileus.
Dr Rebecca Darrah (fig 31 above) is an Assistant Professor at the Frances Payne Bolton School of Nursing with particular interest in the genetics of respiratory diseases.
Dee A. Carter, Shona E. Blair, Nural N. Cokcetin, Daniel Bouzo, Peter Brooks, Ralf Schothauer, Elizabeth J. Harry. Therapeutic Manuka Honey: No Longer So Alternative. Front Microbiol. 2016; 7: 569. Published online 2016 Apr 20. doi: 10.3389/fmicb.2016.00569 Free PMC article. [PubMed]

Fig 49. Dee A Carter
Medicinal honey research is undergoing a substantial renaissance. From a folklore remedy largely dismissed by mainstream medicine as “alternative”, we now see increased interest by scientists, clinical practitioners and the general public in the therapeutic uses of honey. There are a number of drivers of this interest: first, the rise in antibiotic resistance by many bacterial pathogens has prompted interest in developing and using novel antibacterials; second, an increasing number of reliable studies and casereports have demonstrated that certain honeys are very effective wound treatments; third, therapeutic honey commands a premium price, and the honey industry is actively promoting studies that will allow it to capitalize on this; and finally, the very complex and rather unpredictable nature of honey provides an attractive challenge for laboratory scientists.
In this paper the authors review manuka honey research, from observational studies on its antimicrobial effects through to current experimental and mechanistic work that aims to take honey into mainstream medicine. They outline current gaps and remaining controversies in our knowledge of how honey acts, and suggest new studies that could make honey a no longer “alternative” alternative.
— The free full text of this article is available and reviews relevant work in detail and should be consulted for further information. See also article by Jenkins R et al in the 2015 section of this History.
Dee Carter (fig. 49) is Associate Professor and Head of Microbiology in the University of Sydney. Her interests are ecology and population genetics of pathogenic fungi and symbiotic algae,
Drzymala-Czyz S, Jończyk-Potoczna K, Lisowska A, Stajgis M, Walkowiak J. Supplementation of ursodeoxycholic acid improves fat digestion and absorption in cystic fibrosis patients with mild liver involvement. Eur J Gastroenterol Hepatol. 2016 Feb 12. [Epub ahead of print][PubMed]

Fig. 50 Slawomira Drzymała-czyz
food-forum.pl
Ursodeoxycholic acid (UDCA) supplementation is recommended for cystic fibrosis (CF) patients with associated liver disease. However, its effect on fat digestion and absorption is not known.
In 23 patients with mild liver involvement, a C-mixed triglyceride breath test was performed on UDCA supplementation (with and without pancreatic enzymes – standard and increased dose) and after 1 month of UDCA withdrawal. Cumulative percentage dose recovery [CPDR; median (interquartile range)] has been considered to reflect lipid digestion and absorption.The enzyme supplementation resulted in a significant CPDR improvement [0% (0-0) vs. 4.6% (0.4-6.0); P<0.00046]. With the increased dose of enzymes in 16 patients with abnormal C-mixed triglyceride breath test results and lipase dose less than 3000 U/g of fat, higher CPDR values [8.6% (5.6-12.7); P<0.000027] were observed. However, a 1-month UDCA withdrawal resulted in a significant reduction in (P<0.000031) fat digestion and absorption [2.9% (0.7-5.8)]
The authors conclude that UDCA supplementation seems to enhance lipid digestion and absorption in pancreatic insufficient CF patients with mild liver involvement. This finding points toward the potential impact of UDCA supplementation on nutritional status in CF patients with liver disease and underscores the often-overlooked role of factors other than pancreatic enzymes on digestion and absorption of fats in CF.
Slowamira Drzymala-Czyz (fig. 50) is in the Departments of Pediatric Gastroenterology and Metabolic Diseases Pediatric Radiology, Poznań University of Medical Sciences, Poznań, Poland.
El Khoury J; Habre S; Nasr M; Hokayem N. Botulinum Neurotoxin A for Parotid Enlargement in Cystic Fibrosis: The First Case Report. J Oral Maxil Surg 2016; 74(9):1771-3. [PubMed]

Fig 52. Appearance after treatment

Fig 51. Swollen parotid glands before treatment
The literature on submaxillary gland involvement has failed to address the parotid gland and any specific treatment of salivary gland manifestations of CF. Treatment is mainly symptomatic, consisting of analgesics, gustatory stimulation, and massage. Salivary secretion has clearly been linked to parasympathetic and sympathetic signals through intracellular calcium release. CF alters salivary composition with increased calcium and phosphorus concentrations and causes histologic changes (duct enlargement, dilation of acini, and abnormal mucous plug
This study investigated whether botulinum toxin injected into the parotid gland during an acute exacerbation of CF-associated salivary gland disease could alleviate pain and control future exacerbations. A 19-year-old woman with CF had severe parotid enlargement 3 times a year for 2 years usually at the times of respiratory exacerbations. The pain and swelling resolved dramatically over a week after injection of abobotulinumtoxin A at three points of the gland. This is the first description of this treatment.
— There are impressive before (fig. 51) and after treatment (Fig. 52) illustrations in the article (both are reproduced with permission). Barbero and Sibinga first reported this complication in 1962 [see Sixties section]. Although the submandibular glands are often easily palpable, symptoms are unusual.
Elborn JS; Bell SC; Madge SL; Burgel PR; Castellani C; Conway S; De Rijcke K; Dembski B; Drevinek P; Heijerman HG; Innes JA; Lindblad A; Marshall B; Olesen HV; Reimann AL; Sole A; Viviani L; Wagner TO; Welte T; Blasi F. Report of the European Respiratory Society/European Cystic Fibrosis Society task force on the care of adults with cystic fibrosis. Euro Respir J 2016; 47(2):420-8. Access to full text [PubMed]
The improved survival in people with cystic fibrosis has led to an increasing number of patients reaching adulthood. This trend is likely to be maintained over the next decades, suggesting a need to increase the number of centres with expertise in the management of adult patients with cystic fibrosis. These centres should be capable of delivering multidisciplinary care addressing the complexity of the disease, in addition to addressing the psychological burden on patients and their families. Further issues that require attention are organ transplantation and end of life management. Lung disease in adults with cystic fibrosis drives most of the clinical care requirements, and major life-threatening complications, such as respiratory infection, respiratory failure, pneumothorax and haemoptysis, and the management of lung transplantation require expertise from trained respiratory physicians. The taskforce therefore strongly recommends that medical leadership in multidisciplinary adult teams should be attributed to a respiratory physician adequately trained in cystic fibrosis management. The task force suggests the implementation of a core curriculum for trainees in adult respiratory medicine and the selection and accreditation of training centres that deliver postgraduate training to the standards of the HERMES programme.
– An up-to-date review of the requirements for adult care by a multidisciplinary team of acknowledged experts.
Ellemunter H; Eder J; Fuchs S; Gappa M; Steinkamp G. Long-term improvement of lung clearance index in patients with mild cystic fibrosis lung disease: Does hypertonic saline play a role?. J Cyst Fibros 2016; 15(1):123-6. [PubMed]

Fig 53. Gratiana Steinkamp
To assess whether long-term inhalation with hypertonic saline is able to halt the progression of mild CF lung disease, we analysed longitudinal data of lung clearance index (LCI) and spirometry.
A total of 34 patients with mild lung disease (FEV1 > 70% of predicted) had at least one LCI result before and >2 LCI measurements after start of hypertonic saline (HS) therapy.
After a mean follow-up of 39.7 (SD 7.4) months after starting HS, LCI improved significantly from 7.89 (SD 1.35) at baseline to 6.96 (SD 1.03), and 19/34 patients had a normal LCI value at the last measurement. No decrease in mean FEV1 was observed. Thus, ventilation inhomogeneity can improve in patients with mild lung disease.
– This record of experience is certainly valuable and encouraging although essentially “real world” rather than a clinical trial.
Dr. med. Gratiana Steinkamp (fig.53) is a self-employed medical writer and free scientist with a focus on lung diseases. She has been working with cystic fibrosis patients since 1983. In 1986 she started a position at Hannover Medical School as the first full-time CF physician in Germany. During the following years, the Hannover CF-Centre became one of the three largest specialized institutions in Germany.
Elborn JS; Ramsey BW; Boyle MP; Konstan MW; Huang X; Marigowda G; Waltz D; Wainwright CE; VX-809 TRAFFIC and TRANSPORT study groups. Efficacy and safety of lumacaftor/ivacaftor (ORKAMBI) combination therapy in patients with cystic fibrosis homozygous for Phe508del CFTR by pulmonary function subgroup: a pooled analysis. The Lancet Respiratory Medicine. 4(8):617-26, 2016 Aug. [PubMed]
Lumacaftor/ivacaftor combination therapy (Orkambi) has shown clinical benefits in patients with cystic fibrosis homozygous for the Phe508del CFTR mutation; however, pretreatment lung function is a confounding factor that potentially affects the efficacy and safety of this therapy. The authors aimed to assess the efficacy and safety of lumacaftor/ivacaftor therapy in these patients, defined by specific categories of lung function. METHODS: Both trials (TRAFFIC and TRANSPORT) included in this pooled analysis were multinational, randomised, double-blind, placebo-controlled, parallel-group, phase 3 studies. Eligible patients from 187 participating centres in North America, Australia, and the European Union (both trials) were aged 12 years or older with a confirmed diagnosis of cystic fibrosis, homozygous for the Phe508del CFTR mutation, and with a percent predicted FEV1 (ppFEV1) of 40-90 at the time of screening. Patients were randomly assigned with an interactive web response system (1:1:1) to receive placebo, lumacaftor (600 mg once daily) plus ivacaftor (250 mg every 12 h), or lumacaftor (400 mg every 12 h) plus ivacaftor (250 mg every 12 h) for 24 weeks. Prespecified subgroup analyses of pooled efficacy and safety data by lung function, as measured by ppFEV1, were done for patients with baseline ppFEV1 (<40 and >40) and screening ppFEV1 (<70 and >70). The primary endpoint was the absolute change from baseline in ppFEV1 at week 24 analysed in all randomised patients who received at least one dose of study drug. Both trials are registered with ClinicalTrials.gov (TRAFFIC: NCT01807923; TRANSPORT: NCT01807949).
FINDINGS: Both trials were done between April, 2013, and April, 2014. Of the 1108 patients included in the efficacy analysis, 81 patients had a ppFEV1 that decreased to lower than 40 between screening and baseline and 1016 had a ppFEV1 of 40 or higher at baseline. At screening, 730 had a ppFEV1 of less than 70, and 342 had a ppFEV1 of 70 or higher. Improvements in the absolute change from baseline at week 24 in ppFEV1 were observed with both lumacaftor/ivacaftor doses in the subgroup with baseline ppFEV1 levels lower than 40 (least-squares mean difference vs placebo was 3.7 percentage points [95% CI 0.5-6.9; p=0.024] in the lumacaftor [600 mg/day]-ivacaftor group and 3.3 percentage points [0.2-6.4; p=0.036] in the lumacaftor [400 mg/12 h]-ivacaftor group). Improvements in ppFEV1 compared with placebo were also reported in the subgroup with baseline ppFEV1 levels of 40 or higher (3.3 percentage points [2.3-4.4; p<0.0001] in the lumacaftor [600 mg per day]-ivacaftor group and 2.8 percentage points [1.7-3.8; p<0.0001] in the lumacaftor [400 mg/12 h]-ivacaftor group). Similar absolute improvements in ppFEV1 compared with placebo were observed in subgroups with screening ppFEV1 levels lower than 70 and ppFEV1 levels of 70 or higher. Increases in body-mass index and reduction in number of pulmonary exacerbation events were observed in both lumacaftor/ivacaftor dose groups compared with placebo across all lung function subgroups. Treatment was generally well tolerated, although the incidence of some respiratory adverse events was higher with lumacaftor/ivacaftor than with placebo in all subgroups. In patients with baseline ppFEV1 levels lower than 40, these adverse events included cough, dyspnoea, and abnormal respiration.The authors consider these analyses confirm that lumacaftor/ivacaftor combination therapy benefits patients with cystic fibrosis homozygous for Phe508del CFTR who have varying degrees of lung function impairment.
Elborn JS, Ramsey B, Wainwright C, Boyle. Response to: ‘Lumacaftor/ivacaftor for patients homozygous for Phe508del-CFTR: should we curb our enthusiasm?’ by Jones and Barry. (Thorax 2015; 70:215-216. ). Thorax. 2016 Feb;71(2):185-6. doi: 10.1136/thoraxjnl-2015-207611. Epub 2015 Oct 27. [PubMed]
The article by Andy Jones and Peter Barry, to which Stuart Elborn and his co-authors are responding, essentially carries a cautionary message. In contrast to the impressive clinical and physiological response to ivacaftor in people with an Gly551Asp mutation, the response of patients with Phe508del mutations to the lumacaftor/ivacaftor combination is significantly less impressive, doubting “whether the results merit heralding the study as a landmark advance”. The potential problems of the two-drug combination, between which interactions have been reported, also the high cost of treatment are mentioned. Finally, with such modest results, the adverse effect of non-adherence, well described with ivacaftor, would be significant in view of the already modest effects. In conclusion the authors agree “the study represents a success for the CF community and should be welcomed as such; however, the recognition of these results should not represent the “holy grail” for Phe508del homozygote patients is equally important”
In the present response Stuart Elborn and his co-authors consider Jones and Barry’s view to be rather pessimistic. They consider the proof of principle of clinical benefit from a corrector/potentiator combination is a very significant development in CF treatment. The addition of the combination to maximal conventional therapy (as was the case) still demonstrated additional spirometric, exacerbation, quality of life and nutritional effects. The emphasise the primary goal of treatment is to restore CFTR function and they consider this combination therapy represents significant progress and should not be underestimated. The cost of treatment should not impact the interpretation of data. Pharmaceutical companies and health care commissioners must find ways to deliver sustainable funding arrangements that recognise the costs of developing new therapies. Although more effective CFTR modulators may become available, lumacaftor/ivacaftor should not be denied to patients who will benefit.
Elsas CR, Schwind EL, Hercher L, Smith MJ, Young KG. Attitudes Toward Discussing Approved and Investigational Treatments for Cystic Fibrosis in Prenatal Genetic Counseling Practice. J Genet Couns. 2016 Jun 9. [Epub ahead of print] [PubMed]
Most of the genetic counsellors had never heard of ivacaftor or Kalydeco™ prior to taking the survey. Therefore, counsellors need to be better educated about the availability of CFTR mutation-based treatments before they will be able to incorporate discussion of new treatment options into their counseling.
— It is no surprise that most counselors had never heard of ivacaftor. However, the impact of the new treatments will undoubtedly influence prenatal counseling practice. (As we have discussed elsewhere. See also Massie et al Lancet. 2014 Mar 8; 383:923-5. Summarised in the 2015 section).
Emiralioglu N, Dogru D Tugcu GD, Yalcin E, Kiper N, Ozcelik U. Omalizumab Treatment for Allergic Bronchopulmonary Aspergillosis in Cystic Fibrosis. Ann Pharmacother. 2016 Mar;50(3):188-93. doi: 10.1177/1060028015624204. Epub 2015 Dec 23 [PubMed]
A review of 6 CF patients with ABPA receiving omalizumab. All patients were treated with oral prednisolone and itraconazole. Omalizumab was started if the patient was not responding to steroid treatment, which was determined according to serum IgE levels and/or clinical findings or depending on if there were side effects caused by steroid treatment. (Details in PubMed)
This study showed steroid-sparing effect, decreasing IgE levels, and improvement in respiratory symptoms in 6 CF patients with omalizumab treatment.
Fidler MC, Beusmans J, Panorchan P, Van Goor F. Correlation of sweat chloride and percent predicted FEV1 in cystic fibrosis patients treated with ivacaftor. J Cyst Fibros. 2016 Oct 20. pii: S1569-1993(16)30614-2. doi: 10.1016/j.jcf.2016.10.002. [Epub ahead of print][PubMed]

Fig. 54 Meredith Fidler
emedevents.com
The goal of the analysis was to help define the potential value of sweat chloride as a pharmacodynamic biomarker for use in CFTR modulator trials. For any given study, reductions in sweat chloride levels and improvements in absolute ppFEV1 were not correlated for individual patients. However, when the data from all studies were combined, a statistically significant correlation between sweat chloride levels and ppFEV1 changes was observed (p<0.0001).
The authors concluded the sweat chloride level changes in response to potentiation of the CFTR protein by ivacaftor appear to be a predictive pharmacodynamic biomarker of lung function changes on a population basis, but are unsuitable for the prediction of treatment benefits for individuals.
Meredith Fidler (Fig. 54) is a scientist at Vertex Pharmaceuticals LLC, 11010 Torreyanna Road, San Diego, CA 92121,USA
Fitzgerald C, B. Linnane, E. Heery, N. Conneally, S. George, P. Fitzpatrick. Newborn bloodspot screening for cystic fibrosis: What do antenatal and postnatal women know about cystic fibrosis? J Cyst Fibros 2016;15(4):436-42. [PubMed]

Fig 55. Barry Linnane
Newborn bloodspot screening (NBS) for CF was added to the NBS programme in Ireland in July 2011. Little is known about antenatal or postnatal women’s knowledge about CF.This was a cross-sectional study of 662 antenatal (≥36weeks gestation) and 480 postnatal women (post NBS). Women were asked to self-complete a questionnaire including 14 CF knowledge questions. Among the respondents significantly more postnatal than antenatal women were aware that CF is included on the NBS (81.8% vs 63.5%; p<0.001). 92.7% believe that there are health consequences to being a carrier and 33.6% believe there is a cure for CF. In the multivariate analysis, lower educational status, being an antenatal mother, having no family history of CF were associated with poor CF knowledge, while increasing age was found to be protective against poor CF knowledge
The authors suggest the results from this study provide a useful insight into women’s preexisting knowledge about CF, which could be used to inform initial discussions with parents about their child’s diagnosis.
Barry Linnane (fig 55) is Professor and Director of the Cystic Fibrosis Programme and Paediatric Respiratory Consultant, University Hospital, Limerick.
Fakhro M; Ingemansson R; Skog I; Algotsson L; Hansson L; Koul B; Gustafsson R; Wierup P; Lindstedt S. 25-year follow-up after lung transplantation at Lund University Hospital in Sweden: superior results obtained for patients with cystic fibrosis. Interactive Cardiovascular & Thoracic Surgery. 23(1):65-73, 2016 Jul. pubmed.ncbi.nlm.nih.gov/27052747/

Fig. 56 Mohammed Fakhro
LinkedIn
In Sweden, two centres perform lung transplantation for a population of about 9 million and the entire population is covered for lung transplantation by government health insurance. Lund University Hospital is one of these centres. This retrospective report reviews the 25-year experience of the Skane University Hospital Lung Transplant Program with particular emphasis on short-term outcome and long-term survival but also between different subgroups of patients and types of transplant [single-lung transplantation (SLTx) versus double-lung transplantation (DLTx)] procedure performed.
Between January 1990 and June 2014, 278 patients underwent lung transplantation at the Skane University Hospital Sweden. DLTx was performed in 172 patients, SLTx was performed in 97 patients and heart-lung transplantation was performed in 9 patients. In addition, 15 patients required retransplantation (7 DLTx and 8 SLTx).Overall 1-, 5-, 10-, 15- and 20-year survival rates were 88, 65, 49, 37 and 19% for the whole cohort. DLTx recipients showed 1-, 5-, 10- and 20-year survival rates of 90, 71, 60 and 30%, compared with SLTx recipients with 1-, 5-, 10- and 20-year survival rates of 83, 57, 34 and 6% (P < 0.05), respectively. Comparing the use of intraoperative extracorporeal membrane oxygenation, extracorporeal circulation (ECC) and no circulatory support in the aspect of survival, a significant difference in favour of intraoperative ECC was seen.Superior long-term survival rates were seen in recipients diagnosed with cystic fibrosis, alpha1-antitrypsin deficiency and pulmonary hypertension. DLTx showed better results compared with SLTx especially at 10 years post-transplant. In the present study, the authors present cumulative incidence rates of bronchiolitis obliterans syndrome of 15% at 5 years, 26% at 10 years and 32% at 20 years post-transplant; these figures are in line with the lowest rates presented internationally.
– Impressive results from the Skane University Hospital in Sweden.
Mohammed Fakhro (fig.56) is in the Department of Cardiothoracic Surgery, Skåne University Hospital, Lund University, Lund, Sweden.
Floto RA; Olivier KN; Saiman L; Daley CL; Herrmann JL; Nick JA; Noone PG; Bilton D; Corris P; Gibson RL; Hempstead SE; Koetz K; Sabadosa KA; Sermet-Gaudelus I; Smyth AR; van Ingen J; Wallace RJ; Winthrop KL; Marshall BC; Haworth CS; US Cystic Fibrosis Foundation and European Cystic Fibrosis Society. US Cystic Fibrosis Foundation and European Cystic Fibrosis Society consensus recommendations for the management of non-tuberculous mycobacteria in individuals with cystic fibrosis. Thorax. 71 Suppl 1:i1-22, 2016 Jan. [PubMed]
Fig 57. Andres Floto
Non-tuberculous mycobacteria (NTM) are ubiquitous environmental organisms that can cause chronic pulmonary infection, particularly in individuals with pre-existing inflammatory lung disease such as cystic fibrosis (CF). Pulmonary disease caused by NTM has emerged as a major threat to the health of individuals with CF but remains difficult to diagnose and problematic to treat. In response to this challenge, the US Cystic Fibrosis Foundation (CFF) and the European Cystic Fibrosis Society (ECFS) convened an expert panel of specialists to develop consensus recommendations for the screening, investigation, diagnosis and management of NTM pulmonary disease in individuals with CF. Nineteen experts were invited to participate in the recommendation development process. Population, Intervention, Comparison, Outcome (PICO) methodology and systematic literature reviews were employed to inform draft recommendations. An anonymous voting process was used by the committee to reach consensus. All committee members were asked to rate each statement on a scale of: 0, completely disagree, to 9, completely agree; with 80% or more of scores between 7 and 9 being considered ‘good’ agreement. Additionally, the committee solicited feedback from the CF communities in the USA and Europe and considered the feedback in the development of the final recommendation statements. Three rounds of voting were conducted to achieve 80% consensus for each recommendation statement. Through this process, they have generated a series of pragmatic, evidence-based recommendations for the screening, investigation, diagnosis and treatment of NTM infection in individuals with CF as an initial step in optimising management for this challenging condition.
Andres Floto (fig.57) is Professor of Respiratory Biology, Cambridge Immunology Network. Research interests include control of antigen processing by Fcgamma receptors and mycobacterial-host reactions.
Flume PA; VanDevanter DR; Morgan EE; Dudley MN; Loutit JS; Bell SC; Kerem E; Fischer R; Smyth AR; Aaron SD; Conrad D; Geller DE; Elborn JS. A phase 3, multi-center, multinational, randomized, double-blind, placebo-controlled study to evaluate the efficacy and safety of levofloxacin inhalation solution (APT-1026) in stable cystic fibrosis patients. J Cyst Fibros 2016; 15(4):495-502. [PubMed]
APT-1026 (levofloxacin inhalation solution, LIS) is a fluoroquinolone in development for management of chronic P. aeruginosa airways infection in patients with CF. This study was to compare the safety and efficacy of a 28-day course of treatment with LIS 240mg or placebo BID in persons >12years old with CF and chronic P. aeruginosa infection.A multinational, randomized (2:1), double-blinded study of LIS and placebo over 28days in CF patients >12years with chronic P. aeruginosa infection. An improvement in FEV1 (% predicted) at 28days was observed and LIS was well tolerated. LIS is safe and has a potential role in the management of CF patients with chronic P. aeruginosa.
Flume PA; Clancy JP; Retsch-Bogart GZ; Tullis DE; Bresnik M; Derchak PA; Lewis SA; Ramsey BW. Continuous alternating inhaled antibiotics for chronic pseudomonal infection in cystic fibrosis. J Cyst Fibros, 2016 May 24. [PubMed]

Fig. 58 Patrick Flume
www.cff.org
The use of continuous inhaled antibiotic regimens of differing combinations is growing. This double-blind trial compared continuous alternating therapy (CAT) to an intermittent treatment regimen. Subjects were treated with 3 cycles of 28-days inhaled aztreonam (AZLI) or placebo 3-times daily alternating with 28-days open-label tobramycin inhalation solution (TIS). 90 subjects were randomized over 18months. Study enrollment was limited, in part because of evolving practices by clinicians of adopting a CAT regimen in clinical practice; consequently the study was underpowered. AZLI/TIS treatment reduced exacerbation rates by 25.7% (p=0.25; primary endpoint) and rates of respiratory hospitalizations by 35.8% compared with placebo/TIS (p=0.14). AZLI/TIS CAT therapy was well tolerated.This trial illustrates challenges with studying treatment regimens in a constantly evolving CF care environment. Nonetheless, the results of this trial indicate that AZLI/TIS CAT is well tolerated and may provide additional clinical benefit in CF patients compared with intermittent use of TIS alone.
– Although the initial approval for Tobi was for use on alternate months, clinicians gradually introduced a second inhaled antibiotic (often colistin) for the off-Tobi months to maintain the improved respiratory function. This study, to look at this practice using aztronam for the alternated months, has a modest finding that it is “well tolerated and possibly providing additional clinical benefit”.
Patrick Flume (fig.58) is professor of medicine and pediatrics at the Medical University of South Carolina.
Fraquelli M; Baccarin A; Corti F; Conti CB; Russo MC; Della Valle S; Pozzi R; Cressoni M; Conte D; Colombo C. Bowel ultrasound imaging in patients with cystic fibrosis: Relationship with clinical symptoms and CFTR genotype. Digest Liver Dis 2016; 48(3):271-6. [PubMed]

Fig. 59 Mirella Fraquelli
ResearchGate
A prospective study from Milan of 70 consecutive patients with cystic fibrosis and 45 controls who underwent abdominal ultrasound; pertinent findings were related to gastrointestinal symptoms and, in cystic fibrosis patients, to pancreatic status, malabsorption degree, lipase intake, CFTR genotype (classified as severe or mild against functional class of CFTR mutations).
RESULTS: 96% patients showed at least one abnormal bowel ultrasound sign. Most frequent signs were lymph node enlargement (64%), bowel loop dilatation (55%), thick corpuscular intraluminal content (49%), bowel wall hypervascularization (26%), thickened bowel wall (22%) and intussusception (17%). Patients with recurrent abdominal pain showed more bowel wall hypervascularization than patients without recurrent pain (47% vs. 19%, respectively; p = 0.02) and intussusception (58% vs. 17%, respectively; p < 0.01). Genotype was not associated to specific bowel ultrasound signs. Patients with bowel loop intussusception showed greater lipase intake than those without intussusception (8.118 +/- 2.083 vs. 5.994 +/- 4.187, respectively; p < 0.01)
The authors confirmed that CF patients present a higher rate of bowel ultrasound abnormalities than controls and these ultrasound abnormalities are associated with abdominal symptoms
Mirella Fraquelli (fig 59) is senior consultant in Medical Gastroenterology and Hepatology, Gastroenterology and Endoscopy Unit, Fondazione IRCCS Cà Granda, Ospedale Maggiore Policlinico, Milan, Italy.
Franasiak JM; Olcha M; Bergh PA; Hong KH; Werner MD; Forman EJ; Zimmerman RS; Scott RT Jr. Expanded carrier screening in an infertile population: how often is clinical decision making affected?. Genet Med 2016 Mar 3. doi: 10.1038/gim.2016.8. [PubMed]
Fig 60. Jason Frasaniak
Options for preconception genetic screening have grown dramatically. Expanded carrier screening (ECS) now allows for determining carrier status for hundreds of genetic mutations by using a single sample, and some recommend ECS prior to in vitro fertilization. This study seeks to evaluate how often ECS alters clinical management when patients present for infertility care. All patients tested with ECS at a single infertility care center from 2011 to 2014 were evaluated. The overall rate of positive ECS results and the number of couples who were carriers of the same genetic disorder were evaluated.A total of 6,643 individuals were tested, representing 3,738 couples; 1,666 (25.1%) of the individuals had a positive test result for at least one disorder. In 8 of the 3,738 couples, both members of the couple were positive for the same genetic disorder or had a test result that placed them at risk of having an affected child. Three of eight cases were cystic fibrosis. In this cohort, ECS affected clinical care eight times after 6,643 tests (0.12%, confidence interval: 0.05-0.24%) in 3,738 couples (0.21%, confidence interval: 0.09-0.42%).The authors note that Expanded Carrier Screening is becoming more widespread. In a large case series, ECS affected clinical decision making for patients presenting for infertility care in 0.21% of cases. The authors suggest this information must be weighed when utilizing these tests and may be a helpful part of patient counseling
— This is data from a selected population of couples attending an infertility clinic but nonetheless interesting and is likely to be the way forward in the future when it will not be acceptable to ignore opportunities to avoid serious inherited disease.
Jason Frasaniak (fig. 60) is attending Physician and Laboratory Supervisor – Reproductive Medicine Associates of New Jersey Marlton Office
Fink AK, Yanik EL, Marshall BC, Wilschanski M, Lynch CF, Austin AA, Copeland G, Safaeian M, Engels EA. Cancer risk among lung transplant recipients with cystic fibrosis. J Cyst Fibros. 2016 Aug 15. pii: S1569-1993(16)30568-9. doi: 10.1016/j.jcf.2016.07.011. [Epub ahead of print] [PubMed]

Fig. 61 Aliza Fink
Cystic Fibrosis Foundation
Previous studies demonstrated increased digestive tract cancers among individuals with cystic fibrosis (CF), particularly among lung transplant recipients. The authors describe cancer incidence among CF and non-CF lung recipients using data from the US transplant registry and 16 cancer registries. Standardized incidence ratios (SIRs) compared cancer incidence to the general population, and competing risk methods were used for the cumulative incidence of colorectal cancer.They evaluated 10,179 lung recipients (1681 with CF). Risk was more strongly increased in CF recipients than non-CF recipients for overall cancer (SIR 9.9 vs. 2.7) and multiple cancers including colorectal cancer (24.2 vs. 1.7), oesophageal cancer (56.3 vs. 1.3), and non-Hodgkin lymphoma (61.8 vs. 9.4). At five years post-transplant, colorectal cancer was diagnosed in 0.3% of CF recipients aged <50 at transplant and 6.4% aged ≥50.
It was concluded CF recipients have increased risk for colorectal cancer, suggesting a need for enhanced screening.
Aliza Fink (fig.61) is an epidemiologist who joined the CF Foundation in 2012 to develop and implement a research program that is based on the data in the CF Foundation Patient Registry.Cystic Fibrosis Foundation, Bethesda, MD, USA. Subsequently Aliza moved to NORD as Director of Research.
Forrester DL, Knox AJ, Smyth AR, Barr HL, Simms R, Pacey SJ, Pavord ID, Honeybourne D, Dewar J, Clayton A, Fogarty AW. Glutamine supplementation in cystic fibrosis: A randomized placebo-controlled trial. Pediatr Pulmonol. 2016 Mar;51(3):253-7. doi: 10.1002/ppul.23370. Epub 2015 Dec 27. [PubMed]
A study to test the hypothesis that oral glutamine supplementation (21 g/day) for 8 weeks in adults with cystic fibrosis would decrease pulmonary inflammation and improve clinical status.
There was no effect of glutamine supplementation on markers of pulmonary inflammation in the intention-to-treat analysis.
Gentzsch M; Ren HY; Houck SA; Quinney NL; Cholon DM; Sopha P; Chaudhry IG; Das J; Dokholyan NV; Randell SH; Cyr DM. Restoration of R117H CFTR folding and function in human airway cells through combination treatment with VX-809 and VX-770. Am J PhysioL – Lung Cell Mol PhysioL 311(3):L550-9, 2016 Sep 1. [PubMed]

Fig. 62 Martina Gentzsch
UNC School of Medicine
The potentiator VX-770 was the first CFTR modulator approved by the FDA for treatment of CF patients with the gating mutation G551D. Orkambi is a drug containing VX-770 and corrector VX809 and is approved for treatment of CF patients homozygous for F508del, which has folding and gating defects. At least 30% of CF patients are heterozygous for the F508del mutation with the other allele encoding for one of many different rare CFTR mutations. Treatment of heterozygous F508del patients with VX-809 and VX-770 has had limited success, so it is important to identify heterozygous patients that respond to CFTR modulator therapy. R117H is a more prevalent rare mutation found in over 2,000 CF patients.In this study the authors investigated the effectiveness of VX-809/VX-770 therapy on restoring CFTR function in human bronchial epithelial (HBE) cells from R117H/F508del CF patients. They found that VX-809 stimulated more CFTR activity in R117H/F508del HBEs than in F508del/F508del HBEs. R117H expressed exclusively in immortalized HBEs exhibited a folding defect, was retained in the ER, and degraded prematurely. VX-809 corrected the R117H folding defect and restored channel function.
The authors conclude that because R117 is involved in ion conductance, VX-770 acted additively with VX-809 to restore CFTR function in chronically treated R117H/F508del cells. Although treatment of R117H patients with VX-770 has been approved, these studies indicate that Orkambi may be more beneficial for rescue of CFTR function in these patients.
Martina Gentzsch (fig. 62) is at the Marsico Lung Institute/Cystic Fibrosis Research Center, University of North Carolina, Chapel Hill, North Carolina; Department of Cell Biology and Physiology. University of North Carolina, Chapel Hill, North Carolina.
C. Guissart, C. Dubucs, C. Raynal, A. Girardet, F. Tran Mau Them, V. Debant, C. Rouzier, A. Boureau-Wirth, E. Haquet, J. Puechberty, E. Bieth, D. Dupin Deguine, P. Khau Van Kien, M.P. Brechard, V. Pritchard, M. Koenig, M. Claustres, M.C. Vincent. Non-invasive prenatal diagnosis (NIPD) of cystic fibrosis: an optimized protocol using MEMO fluorescent PCR to detect the p.Phe508del mutation. J Cyst Fibros. 2016 Dec 28. pii: S1569-1993(16)30680-4. doi: 10.1016/j.jcf.2016.12.011. [Epub ahead of print] [PubMed]
Analysis of cell-free foetal DNA (cff-DNA) in maternal plasma is very promising for early diagnosis of monogenic diseases; in particular, cystic fibrosis (CF). However, NIPD of single-gene disorders has been limited by the availability of suitable technical platforms and the need to set up patient or disease-specific custom-made approaches. To make research applications more readily accessible to the clinic, the authors report a simple assay combining two independent methods to determine the presence or absence of paternally inherited foetal allele p.Phe508del (the most frequent mutation in CF patients worldwide).
The first method detects the presence or absence of a p.Phe508del allele by Mutant Enrichment with 3′-Modified Oligonucleotide PCR coupled to Fragment Length Analysis (MEMO-PCR-FLA). The second method detects the p.Phe508del allele with classical Multiplex Fluorescent PCR including five intragenic and extragenic STR markers of the CFTR locus and a specific SRY sequence.
They collected 24 plasma samples from 23 women carrying foetuses at risk for CF and tested each sample using both methods. Their new procedures were successfully applied to 10 couples where fathers carried the p.Phe508del mutation and mothers were carrying a different mutation in the CFTR gene.
These simple tests provided clear positive or negative results from the maternal plasma of the pregnant women. They confirmed the presence of cff-DNA in the studied samples by the identification of a tri-allelic DNA profile using a miniSTR kit. All results were correlated with chorionic villus sampling or amniocentesis analyses.
The authors concluded this non-invasive prenatal approach, easily set up in any clinical laboratory where prenatal diagnosis is routinely performed, offers many advantages over current methods: it is simple, rapid, and cost-effective. It opens up the possibility for testing a large number of couples with offspring at risk for CF.
From Laboratoire de Génétique Moléculaire, IURC, CHRU de Montpellier, France; Equipe Accueil EA7402, Université Montpellier, Montpellier, France.
Hatziagorou E; Kampouras A; Sidiropoulou M; Markou A; Anastasiou A; Tsanakas J. Pancreatic Cystosis in Two Adolescents with Cystic Fibrosis. Case Reports in Pediatrics. 2016:5321785, 2016. Free article. [PubMed]

Fig. 64 Elpis Hatziagorou
ecorn-cf.eu
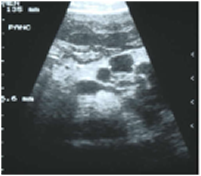
Fig 63. Multiple pancreatic cysts in a boy with CF
Pancreatic cystosis in two dolescents with cystic fibrosis, a 13-year-old girl hand an 18-year-old boy. In pancreatic cystosis, which is a rare manifestation of CF, the pancreatic parenchyma is replaced with multiple cysts of different sizes. Pancreatic cystosis is mainly an imaging based diagnosis and frequent follow-up should be recommended.
Fig. 63 shows abdominal ultrasound of multiple pancreatic cysts in an adolescent boy with cystic fibrosis (not from this paper. See also Topics –>Pancreas -> 2000)
Ellis Hatziagorou (fig.64) is assistant professor in Paediatric Pulmonology and CF Unit, 3rd Paediatric Department, Hippokration Hospital, Aristotle University of Thessaloniki, 49 Konstantinoupoleos street, 54642 Thessaloniki, Greece.
Howlett C, Ronan NJ, NiChroinin M, Mullane D, Plant BJ. Partial restoration of pancreatic function in a child with cystic fibrosis. Lancet Respir Med. 2016 May;4(5):e21-2. doi: 10.1016/S2213-2600(16)30032-7.pubmed.ncbi.nlm.nih.gov/27304562/

Fig 65 Ciara Howlett
3cf.ie
The authors observed changes in fecal elastase (FE-1) in a child (aged 6·5 years) after commencing ivacaftor treatment. A female (genotype F508del/G551D ) diagnosed at 4 years and 9 months old, after hospital admission with increased respiratory effort and cough. FE-1 was measured at diagnosis and was consistent with severe pancreatic insufficiency at less than 15 μg/g. At this time, the patient was started on four 150 mg pancreatin capsules per day. The patient started ivacaftor therapy on her sixth birthday in accordance with local regulatory guidelines.After 6 months of ivacaftor treatment, the patient reported abdominal pain and constipation. As a result, her treatment regimen was reduced by 50% to two 150 mg pancreatin capsules per day. FE-1 was measured and was in the normal range at 259 μg/g. Two subsequent FE-1 measurements were made after 7 months of treatment (118 μg/g and 121 μg/g) and were consistent with moderate pancreatic insufficiency.The authors of the KIWI study have highlighted the potential for a partial restoration of pancreatic function in early life in some CF patients given ivacaftor (Davies JC et al, 2016). Also a significant 60% reduction in pancreatic enzyme requirement occurred in one 16 year old woman after commencing ivacaftor (Harrison MJ et al, N Eng J Med 2013;369:1280-1282. [PubMed])
— It is encouraging that specific therapy with ivacaftor appears to have a favourable effect on both endocrine and exocrine pancreatic function. Not only does the output of pancreatic enzymes improve, and the enzyme replacement requirement fall, but insulin secretion also improves and even resolution of CF related diabetes has been reported (Hayes D et al, 2014. [PubMed])
Ciara Howlett (fig. 65) is dietitian at the Cork Cystic Fibrosis Centre, University College Cork, Cork University Hospital, Wilton, Cork, Ireland.
Jain K, Wainwright C, Smyth AR. Bronchoscopy-guided antimicrobial therapy for cystic fibrosis. Cochrane Database Syst Rev. 2016 Jan 21;1:CD009530.doi:10.1002/14651858.CD009530.pub3. [PubMed]
This review, essentially of Claire Wainwright’s own important study – a well-designed randomized-controlled study, shows no clear evidence to support the routine use of bronchoalveolar lavage for the diagnosis and management of pulmonary infection in pre-school children with cystic fibrosis compared to the standard practice of providing treatment based on results of oropharyngeal culture and clinical symptoms. No evidence was available for adult and adolescent populations.
— A important study answering basic question regarding management of pre-school children with CF. The study clearly failed to show an advantage in regular bronchoalveolar surveillance of such children. This is a relief for to arrange annual bronchoscopy for all young children with CF would have been a major undertaking.
Janssens S, Chokoshvilli D, Binst C, Mahieu I, Henneman L, De Paepe A, Borry P. Attitudes of cystic fibrosis patients and parents toward carrier screening and related reproductive issues. Eur J Hum Genet. 2016 Apr;24(4):506-12. [PubMed]

Fig. 66 Sandra Janssens
UZ Gent
Cystic fibrosis (CF) is a life-limiting autosomal recessive disorder affecting ~1 in 2500-4000 Caucasians. As most CF patients have no family history of the disorder, carrier screening for CF has the potential to prospectively identify couples at risk of conceiving an affected child. At-risk couples may consequently choose to act on the provided information and take steps to avoid the birth of a child with CF. Although carrier screening is widely believed to enhance reproductive autonomy of prospective parents, the practice also raises important ethical questions. A written questionnaire was administered to adult patients and parents of children with CF with the aim to explore participants’ attitudes toward CF carrier screening and related reproductive issues. The study population was recruited from a CF patient registry in Belgium and comprised 111 participants (64 parents, 47 patients aged 16 or older). The authors found that more than 80% of all participants were in favor of preconception carrier screening for CF.However, some were concerned over potential negative consequences of population-wide CF carrier screening. Regarding future reproductive intentions, 43% of the participants indicated a desire to have children. Among these, preimplantation genetic diagnosis was found to be the most preferred reproductive option, closely followed by spontaneous pregnancy and prenatal diagnosis. Although the findings of our study suggest that patients and parents of children with CF support a population-based carrier screening program for CF, they also highlight some issues deserving particular attention when implementing such a program
– It is no surprise that 80% of people familiar with the major problems of CF are in favour of preconception carrier screening. This contrasts with the relative lack of interest in the general population as evidenced by the less than 50% response for cascade carrier screening in most studies.
Sandra Janssens (fig.66) is clinical geneticist, professor and Head of Clinic, Centre for Medical Genetics Ghent, University Hospital Ghent, Ghent, Belgium.
Kaminski R, Nazareth D. A successful uncomplicated CF pregnancy while remaining on Ivacaftor. J Cyst Fibros. 2016 Jan;15(1):133-4. doi: 10.1016/j.jcf.2015.11.013. Epub 2015 Dec 14. [PubMed]

Fig. 67 Rachel Kaminski
Twitter.com
A 25 year old (G551D:3272-26A>G) gravida 1, BMI 20.8kg/m2, infected with Achromobacter xylosoxidose. On Ivacaftor since 2013 following which her FEV1 rose from 85% to 95%. With the patient’s agreement, after discussion, the Ivacaftor was continued through a normal pregnancy with an FEV1 of 95% with two courses of IV antibiotics. A normal 7 lb 8oz baby girl was born at 39 weeks. The mother did not wish to breast feed for reasons unrelated to her treatment.
— This is first report of the use of Ivacaftor throughout pregnancy. Previous animal studies failed to show a risk to the fetus.
Rachel Kaminski (fig.67) is at Bristol Adult Cystic Fibrosis Centre, University Hospitals Bristol NHS Foundation Trust, Upper Maudlin Street, Bristol BS2 8HW, United Kingdom; subsequently a respiratory consultant at Cheltenham and Gloucester NHS Trust, UK
Khanna AR; Coumans JV. Spontaneous Improvement of Chiari I Malformation and Syringomyelia in a Patient With Cystic Fibrosis: Case Report. Neurosurgery. 78(2):E305-8, 2016 Feb. [PubMed]

Fig. 67 Arjun Khanna
loop.frontiersin.org
Syringomyelia is highly associated with Chiari I malformation, but the pathophysiologic mechanism of syrinx formation and its relation to downward cerebellar tonsillar displacement remains elusive. Cough, Valsalva maneuver, and other physiological strains transiently exacerbate the clinical symptoms of these conditions, exert profound effects on the flow dynamics across the craniospinal junction, and are thought to play an important role in the pathogenesis of syringomyelia.
A patient with cystic fibrosis who presented during an exacerbation of bronchiectasis and was found to have a Chiari I malformation with associated syringomyelia. Eight months later, when the patient had returned to baseline pulmonary status, repeat imaging showed interval improvement in both the size of the syrinx and descent of cerebellar tonsils.The authors concluded this rare case of spontaneous improvement of syringomyelia and Chiari I malformation attributable to relief from chronic cough offers interesting insight into the mechanism of these disorders.
— This condition was first reported in CF by Needleman in 2000 and is a serious neurological complication found in 5 of 400 patients with CF. An important complication of which many paediatricians will have heard of in relation to spina bifida and hydrocephalus but not associated with CF. Two infants with CF and the Chiari type 1 malformation were reported in 2003 (Rakheja D et al. Pediatr Develop Path 2003; 6:88-93.[PubMed]) and other described in CNS Topics section.
Arjun R Khanna (fig.67) is a neurosurgeon in the Department of Neurosurgery, Massachusetts General Hospital, Boston, Massachusetts.
Kitt H, Lenney W, Gilchrist FJ. Two case reports of the successful eradication of new isolates of Burkholderia cepacia complex in children with cystic fibrosis. BMC Pharmacol Toxicol. 2016 Mar 28;17(1):14. doi: 10.1186/s40360-016-0054-0. [PubMed]
Burkholderia cepacia was successfully eradicated in a 14 year old boy with CF and Burkholderia gladioli successfully eradicated in a six year old girl with CF. In both children two weeks of intravenous (IV) tobramycin, ceftazidime and temocillin were used followed by three months of inhaled tobramycin. Bronchoalveolar lavage samples taken during flexible bronchoscopy were used prior to treatment to exclude spontaneous clearance as well as after treatment to confirm eradication.New isolates of BCC can be successfully eradicated in children with CF. More research is urgently required in this area to identify the best treatment regimen for BCC eradication.
— It is certainly not general experience that “New isolates of BCC can be successfully eradicated in children with CF” as stated by the authors. Horsley et al, 2011. [PubMed] reported routine use of therapies to attempt eradication of new BCC is commonly used in the UK (12/17 centers responded). This typically involves a combination of intravenous and nebulised antibiotics. Of 19 eligible cases of new BCC infection, the organism was been eradicated in 7 (37%). Three of these did not receive specific eradication therapy. Of 14 patients who have received eradication therapy and completed follow up, BCC were cleared in only 4 (29%). Once established and chronic it is usually impossible to eradicate the organism.
From Royal Stoke University Hospital, Stoke on Trent, ST4 6QG, UK.
Konstan MW, Flume PA, Galeva I, Wan R, Debonnett LM, Maykut RJ, Angyalosi G. One-year safety and efficacy of tobramycin powder for inhalation in patients with cystic fibrosis. Pediatr Pulmonol. 2016 Apr;51(4):372-8. doi: 10.1002/ppul.23358. Epub 2015 Dec 27. [PubMed]
This is an integrated analysis of data from patients with cystic fibrosis (CF) aged 6-21 years who were treated with up to seven cycles of tobramycin powder for inhalation (TIP(TM) ) over a period of at least 1 year. Safety and key efficacy endpoints were analyzed. The improvement in lung function and decrease in sputum P. aeruginosa (Pa) density from baseline were sustained over the 1-year treatment period. The number of adverse events (AEs) was low and did not increase with additional cycles of TIP treatment. Some increase in tobramycin minimum inhibitory concentration (MIC) was observed, but there was no significant increase in emergence of resistant strains based on the parenteral breakpoint for tobramycin.
Efficacy of TIP was maintained for up to seven cycles. Long-term treatment with TIP was generally safe and well tolerated with no increase in AEs.
Konstan MW, McKone EF, Moss RB, Marigowda G, Tian S, Waltz D, Huang X, Lubarsky B, Rubin J, Millar SJ, Pasta DJ, Mayer-Hamblett N, Goss CH, Morgan W, Sawicki GS. Assessment of safety and efficacy of long-term treatment with combination lumacaftor and ivacaftor therapy in patients with cystic fibrosis homozygous for the F508del-CFTR mutation (PROGRESS): a phase 3, extension study. Respir Med. 2016 Dec 20. pii: S2213-2600(16)30427-1. doi: 10.1016/S2213-2600(16)30427-1. [Epub ahead of print] [PubMed]

Fig. 68 Michael W Konstan Cleveland.com
24-week safety and efficacy of lumacaftor/ivacaftor combination therapy was shown in two randomised controlled trials (RCTs)-TRAFFIC and TRANSPORT-in patients with cystic fibrosis who were aged 12 years or older and homozygous for the F508del-CFTR mutation. We aimed to assess the long-term safety and efficacy of extended lumacaftor/ivacaftor therapy in this group of patients in PROGRESS, the long-term extension of TRAFFIC and TRANSPORT.PROGRESS was a phase 3, parallel-group, multicentre, 96-week study of patients who completed TRAFFIC or TRANSPORT in 191 sites in 15 countries. Patients were eligible if they were at least 12 years old with cystic fibrosis and homozygous for the F508del-CFTR mutation. Exclusion criteria included any comorbidity or laboratory abnormality that, in the opinion of the investigator, might confound the results of the study or pose an additional risk in administering the study drug to the participant, history of drug intolerance, and history of poor compliance with the study drug. Patients who previously received active treatment in TRANSPORT or TRAFFIC remained on the same dose in PROGRESS.
Patients who had received placebo in TRANSPORT or TRAFFIC were randomly assigned (1:1) to receive lumacaftor (400 mg every 12 h)/ivacaftor (250 mg every 12 h) or lumacaftor (600 mg once daily)/ivacaftor (250 mg every 12 h). The primary outcome was to assess the long-term safety of combined therapy. The estimated annual rate of decline in percent predicted FEV1 (ppFEV1) in treated patients was compared with that of a matched registry cohort. Efficacy analyses were based on modified intention-to-treat, such that data were included for all patients who were randomly assigned and received at least one dose of study drug.RESULTS. Between Oct 24, 2013, and April 7, 2016, 1030 patients from the TRANSPORT and TRAFFIC studies enrolled in PROGRESS, and 1029 received at least one dose of study drug. 340 patients continued treatment with lumacaftor 400 mg every 12 h/ivacaftor 250 mg every 12 h; 176 patients who had received placebo in the TRANSPORT or TRAFFIC studies initiated treatment with lumacaftor 400 mg every 12 h/ivacaftor 250 mg every 12 h, the commercially available dose, for which data are presented. The most common adverse events were infective pulmonary exacerbations, cough, increased sputum, and haemoptysis. Modest blood pressure increases seen in TRAFFIC and TRANSPORT were also observed in PROGRESS. For patients continuing treatment, the mean change from baseline in ppFEV1 was 0·5 (95% CI -0·4 to 1·5) at extension week 72 and 0·5 (-0·7 to 1·6) at extension week 96; change in BMI was 0·69 (0·56 to 0·81) at extension week 72 and 0·96 (0·81 to 1·11) at extension week 96. The annualised pulmonary exacerbation rate in patients continuing treatment through extension week 96 (0·65, 0·56 to 0·75) remained lower than the placebo rate in TRAFFIC and TRANSPORT. The annualised rate of ppFEV1 decline was reduced in lumacaftor/ivacaftor-treated patients compared with matched controls (-1·33, -1·80 to -0·85 vs -2·29, -2·56 to -2·03). The efficacy and safety profile of the lumacaftor 600 mg once daily/ivacaftor 250 mg every 12 h groups was generally similar to that of the lumacaftor 400 mg every 12 h/ivacaftor 250 mg every 12 h groups.
The authors concluded the long-term safety profile of lumacaftor/ivacaftor combination therapy was consistent with previous RCTs. Benefits continued to be observed with longer-term treatment, and lumacaftor/ivacaftor was associated with a 42% slower rate of FEV1 decline than in matched registry controls.
— An important review reproduced here in some detail. Although not as convincing as the response of people with G551D to ivacaftor, there is a significant fall in frequency of exacerbations which is an increasingly valuable end point.
Michael Konstan (fig.68) is a paediatric pulmonologist at Case Western Reserve University School of Medicine and Rainbow Babies and Children’s Hospital, Cleveland, OH, United States.
Konstan MW, Pasta DJ, Wagener JS, VanDevanter DR, Morgan WJ. BMI fails to identify poor nutritional status in stunted children with CF. J Cyst Fibros. 2016 Dec 1. pii: S1569-1993(16)30663-4. doi: 10.1016/j.jcf.2016.11.005. [PubMed]
Body mass index (BMI) is currently emphasized for evaluating nutritional status in children with cystic fibrosis (CF). Weight for age (WFA) and height for age (HFA) may get less attention. Data from the Epidemiologic Study of Cystic Fibrosis were used to compare patient WFA, HFA, and BMI percentiles for children age 2 to 18years.
For children with BMI between the 25th and 50th percentiles, 16.8% had WFA <10th percentile and 26.6% had HFA <10th percentile.
BMI fails to identify a substantial proportion of children with CF who have stunting or potentially poor nutritional status as measured by WFA and/or HFA.
Labombarda F; Saloux E; Brouard J; Bergot E; Milliez P.Heart involvement in cystic fibrosis: A specific cystic fibrosis-related myocardial changes? [Review] Resp Med 2016; 118:31-8. [PubMed]
Fig. 69 Fabien Labombarda
ResearchGate
Over the last four decades pathological, experimental, and clinical evidence points towards the existence of a specific myocardial involvement in cystic fibrosis. Multi-modality cardiac imaging, especially recent echocardiographic techniques, evidenced diastolic and/or systolic ventricular dysfunction in cystic fibrosis leading to the concept of a cystic fibrosis-related cardiomyopathy. Hypoxaemia and inflammation are among the most important factors for heart involvement in cystic fibrosis. Cystic Fibrosis Transmembrane Regulator was found to be involved in the regulation of cardiomyocyte contraction and may also account for cystic fibrosis-related myocardial dysfunction. This review, mainly focused on echocardiographic studies, seeks to synthesise the existing literature for and against the existence of heart involvement in cystic fibrosis, its mechanisms and prognostic implications. Careful investigation of the heart function may be helpful for risk stratification and therapeutic decisions in patients with cystic fibrosis.
Fabien Labombarda (fig. 69) is a cardiologist at Caen CHU, Department of Cardiology, Caen, F-14000, Franc
Lands LC, Stanojevic S. Oral non-steroidal anti-inflammatory drug therapy for lung disease in cystic fibrosis. Cochrane Database Syst Rev. 2016 Apr 7;4:CD001505. [Epub ahead of print] [PubMed]

Fig. 70 Larry Lands thechildren.com
The searches identified 10 trials; four are included (287 participants aged five to 39 years; maximum follow up of four years). Combined data from the two largest ibuprofen trials showed a significantly lower annual rate of decline for lung function in the ibuprofen group in younger children. In one trial, long-term use of high-dose ibuprofen was associated with reduced intravenous antibiotic usage, improved nutritional and radiological pulmonary status. The authors concluded high-dose ibuprofen can slow the progression of lung disease in people with cystic fibrosis, especially in children, which suggests that strategies to modulate lung inflammation can be beneficial for people with cystic fibrosis.- Despite the logic of using an effective anti-inflammatory drug in a condition where chronic inflammation is destroying lung tissue, enthusiasm for the long-term use of ibuprofen remains low and ibuprofen is taken by less than 5% of the patients in the CFF 2014 registry.
Larry C Lands (fig. 70) is Director, Pediatric Respiratory Medicine, Pediatric Cystic Fibrosis Clinic, and Pediatric Pulmonary Function Laboratory Montreal Children’s Hospital, 2300 Tupper Street, Montreal, QC, Canada, H3H 1PA.
Lahiri T, Hempstead SE, Brady C, Cannon CL, Clark K, Condren ME, Guill MF, Guillerman RP, Leone CG, Maguiness K, Monchil L, Powers SW, Rosenfeld M, Schwarzenberg SJ, Tompkins CL, Zemanick ET, Davis SD. Clinical Practice Guidelines From the Cystic Fibrosis Foundation for Preschoolers With Cystic Fibrosis. Pediatrics. 2016 Mar 23. pii: peds.2015-1784. [Epub ahead of print] [PubMed] (Available to download from CFF website}

Fig. 71 Thomas Lahiri UMV Health Network
Cystic fibrosis (CF) clinical care guidelines exist for the care of infants up to age 2 years and for individuals ≥6 years of age. An important gap exists for preschool children between the ages of 2 and 5 years. This period marks a time of growth and development that is critical to achieve optimal nutritional status and maintain lung health. Given that disease often progresses in a clinically silent manner, objective and sensitive tools that detect and track early disease are important in this age group. Several challenges exist that may impede the delivery of care for these children, including adherence to therapies. A multidisciplinary committee was convened by the CF Foundation to develop comprehensive evi dence-based and consensus recommendations for the care of preschool children, ages 2 to 5 years, with CF. This document includes recommendations in the following areas: routine surveillance for pulmonary disease, therapeutics, and nutritional and gastrointestinal care.
Thomas Lahiri (fig.71) is a Pediatric Pulmonologist, at the University of Vermont Children’s Hospital and Department of Pediatrics, University of Vermont College of Medicine, Burlington, Vermont;
Lazarin GA, Haque IS. Expanded carrier screening: A review of early implementation and literature. Perinatol. 2016 Feb;40(1):29-34. doi: 10.1053/j.semperi.2015.11.005. Epub 2015 Dec 21. [PubMed]

Fig.72 Gabriel A Lazarin
emedevents.com
Carrier screening is the practice of testing individuals to identify those at increased risks of having children affected by genetic diseases. Professional guidelines on carrier screening have been available for more than 15 years, and have historically targeted specific diseases that occur at increased frequencies in defined ethnic populations.
Enabled by rapidly evolving technology, expanded carrier screening aims to identify carriers for a broader array of diseases and may be applied universally (equally across all ethnic groups). This new approach deviates from the well-established criteria for screening models.
– In this review, the authors summarise the rationale for expanded carrier screening using available literature regarding clinical and technical data, as well as provider perspectives. They also discuss important avenues for further research.
Gabriel Lazarin (fig.72) îs a medical geneticist at Counsyl, 180 Kimball Way, South San Francisco, CA 94080.
Lee AL; Rawlings S; Bennett KA; Armstrong D. Pain and its clinical associations in individuals with cystic fibrosis: A systematic review. Chron Resp Dis 2016; 13(2):102-17. [PubMed]

Fig. 73 Ann Marie Lee Research.monash.edu
The pooled prevalence of pain in adults with CF was 77% (95% confidence interval (CI): 57%-92%) and in children was 42% (95% CI: 0%-91%). Common regions of pain included back, abdomen, chest and limbs. In children and adults, pain was associated with a poorer quality of life (QOL) and significant interference with treatments. Pain is a common problem in both children and adults with CF. It has negative clinical associations with QOL and the ability to successfully undertake treatment.
Annemarie Lee is a cardiorespiratory physiotherapist and Associate Professor at West Park Healthcare Centre, Victoria, Australia.
Lee SY; Chesdachai S; Lee MJ; He XM; Tangpricha V; Braverman LE. Thyroid Function in Patients with Cystic Fibrosis: No Longer a Concern?. Thyroid 2016; 26(7):875-9. [PubMed]

Fig. 74 Sun Y Lee
bumc.bu.edu
Development of goiter and hypothyroidism has been reported in patients with cystic fibrosis (CF) since the 1970s, especially when treated with iodine-based expectorants. With iodine-containing expectorants no longer in routine use, the prevalence of thyroid dysfunction in CF patients is unknown.
This cross-sectional study assessed thyroid function status in a large cohort of CF patients. Although 24 (27%) of the patients had abnormal serum thyroid function tests, overt thyroid dysfunction was rare in this cohort of 89 patients with CF. The degree of hypothyroxinemia was marginal, likely due to non-thyroidal illness. There were no significant predictors of thyroid dysfunction.
Sun Y Lee (fig.74) is Assistant Professor in the Section of Endocrinology, Diabetes, and Nutrition, Boston University School of Medicine , Boston, Massachusetts.
Lee TW, Southern KW, Perry LA, Penny-Dimri JC, Aslam AA. Topical cystic fibrosis transmembrane conductance regulator gene replacement for cystic fibrosis-related lung disease. Cochrane Database Syst Rev. 2016 Jun 17;6:CD005599. doi: 10.1002/14651858.CD005599.pub5. [PubMed]

Fig. 75 Tim Lee
author’s photo
To determine whether topical CFTR gene replacement therapy to the lungs in people with cystic fibrosis is associated with improvements in clinical outcomes, and to assess any adverse effects.Four randomised controlled studies met the inclusion criteria for this review, involving a total of 302 participants lasting from 29 days to 13 months; 14 studies were excluded.One study of liposome-based CFTR gene transfer therapy demonstrated some improvements in respiratory function in people with CF, but this limited evidence of efficacy does not support this treatment as a routine therapy at present. There was no evidence of efficacy for viral-mediated gene delivery. Future studies need to investigate clinically important outcome measures.
– A useful source of information on the present state of gene therapy, which is obviously not at a stage that it, can be used as routine treatment,
Tim W R Lee (fig.75) is paediatrician and Director Leeds Regional Paediatric Cystic Fibrosis Centre, A Floor, Clarendon Wing, Leeds General Infirmary, Great George Street, Leeds, West Yorkshire, UK,
Labombarda F, Saloux E, Brouard J, Bergot E, Milliez P. Heart involvement in cystic fibrosis: A specific cystic fibrosis-related myocardial changes? Respir Med. 2016 Sep;118:31-8. doi: 10.1016/j.rmed.2016.07.011. Epub 2016 Jul 15. [PubMed]
Over the last four decades pathological, experimental, and clinical evidence points towards the existence of a specific myocardial involvement in cystic fibrosis. Multi-modality cardiac imaging, especially recent echocardiographic techniques, evidenced diastolic and/or systolic ventricular dysfunction in cystic fibrosis leading to the concept of a cystic fibrosis-related cardiomyopathy. Hypoxaemia and inflammation are among the most important factors for heart involvement in cystic fibrosis. Cystic Fibrosis Transmembrane Regulator was found to be involved in the regulation of cardiomyocyte contraction and may also account for cystic fibrosis-related myocardial dysfunction.
– This review, mainly focused on echocardiographic studies, seeks to synthesise the existing literature for and against the existence of heart involvement in cystic fibrosis, its mechanisms and prognostic implications. Careful investigation of the heart function may be helpful for risk stratification and therapeutic decisions in patients with cystic fibrosis.
Fabien Labombarda (fig. 69 above) is a cardiologist at Caen CHU, Department of Cardiology, Caen, F-14000, Franc
Levine H; Cohen-Cymberknoh M; Klein N; Hoshen M; Mussaffi H; Stafler P; Breuer O; Kerem E; Blau H. Reversible airway obstruction in cystic fibrosis: Common, but not associated with characteristics of asthma. J Cyst Fibros 2016; 15(5):652-9. [PubMed]

Fig 76. Hagit Levine
As asthma-like symptoms are common in CF, the authors evaluated reversible airway obstruction and associated characteristics by a retrospective analysis of charts including spirometry and bronchodilator response.Of 190 CF patients (103 at Schneider’s, 87 at Hadassah clinic), aged 14.4 (4-76) years, median (range), 39% had reversible obstruction (DELTAFEV1% predicted >12%), associated with younger age (p=0.01) and severe genotype (p=0.02). There was no association with family history of asthma, serum IgE, blood eosinophils, pancreatic status, FEV1<40% predicted, Aspergillus or Pseudomonas infection.Of the 39% of patients with reversible obstruction, 74% were on bronchodilator and 68% on inhaled corticosteroid therapy but 54% and 57% respectively receiving these therapies did not have reversible obstruction.
The authors confirmed that reversible airway obstruction is common in CF, more frequent in younger patients and those with severe genotype, with no correlation to markers of atopy or CF clinical severity. Bronchodilator and inhaled corticosteroid therapies are commonly prescribed even for patients without reversible obstruction.
– During the treatment of an exacerbation if twice daily respiratory function is performed (even with a simple peak flow meter) before and after a bronchodilator, the degree of reversibility lessens each day during the course of IV antibiotic treatment as the inflammation is controlled and respiratory function improves. So in this situation the reversibility certainly does appear to be related to the severity of the inflammation. Ian Balfour Lynn has described the frequent, and at times apparently unnecessary, use of inhaled corticosteroids in the UK even in those patients with no reversibility (Balfour-Lynn IM et al. Am J Respir Crit Care Med 2006; 173(12): 1356-62). However, it is important to recognise the minority of CF patients who do respond impressively to inhaled steroids – presumably those in Balfour—Lynn’s study whose parents refused to enter the steroid withdrawal trial.
Dr Hagit Levine (fig. 76) is Paediatric Pulmonologist at Schneiders Children’s Hospital. Israel.
Liew Z, Mallikarjuna S, Hasan A, Gould FK, Bunn S, Thomas MF, Lordan JL, O’Brien C, Brodlie M. Successful outcome following pneumonectomy in a teenage boy with cystic fibrosis: a case report. BMC Pulm Med. 2017 Jan 13;17(1):17. doi: 10.1186/s12890-016-0350-x. Free PMC article [PubMed]

Fig. 77 Zheti Lieu
ResearchGate
Lung resection surgery is seldom indicated in cystic fibrosis and the associated medical literature is relatively sparse.
A 14 year old boy was referred for lung transplantation assessment. He had a chronic history of complete collapse and consolidation of his entire right lung. This was causing severe morbidity in terms of a continuous requirement for intravenous antibiotics over the last year, poor exercise tolerance with forced expiratory volume in 1 s of 35-40% predicted and need for home tuition. He also had significant nutritional problems and gastrointestinal symptoms following a Nissen’s fundoplication operation a year earlier.
His nutritional status was firstly improved by the institution of jejunal feeding, which also greatly improved his distressing symptoms of nausea and wretching. After thorough multidisciplinary assessment the therapeutic option of performing a right pneumonectomy was considered due to relative sparing of the left lung, which demonstrated only mild bronchiectasis on computed tomography scan. This was performed uneventfully with a smooth peri-operative course. Targeted antimicrobials were used to treat the multiresistant organisms colonising his airways. Subsequently his quality of life, nutritional status and lung function all improved significantly and requirement for lung transplantation has been delayed. A successful outcome following pneumonectomy in a teenage boy with cystic fibrosis referred for lung transplantation assessment with chronic unilateral collapse and consolidation of his right lung. Pneumonectomy can be a feasible option in this clinical situation in cystic fibrosis but the associated risks must be considered carefully on a case-by-case basis.
– The first pneumonectomy in a 14 year old boy with CF was reported as far back as 1952 from Staten Island Hospital, New York (Lloyd MS, Robitzek EH Quart Bull Sea View Hospital 1952; 13:114-124.[PubMed] also see Topics -> Surgery for more information)
Zheti Liew ( fig. 77) is in the Department of Paediatric Respiratory Medicine, Great North Children’s Hospital, Newcastle upon Tyne, UK.
Loring HS; ElMallah MK; Flotte TR.Development of rAAV2-CFTR: History of the First rAAV Vector Product to be Used in Humans. Human Gene Therapy. Part B. Methods. 27(2):49-58, 2016 Apr. [PubMed]
The first human gene therapy trials using recombinant adeno-associated virus (rAAV) vectors were performed in cystic fibrosis (CF) patients. Over 100 CF patients were enrolled in 5 separate trials of rAAV2-CFTR administration via nasal, endobronchial, maxillary sinus, and aerosol delivery. Recombinant AAV vectors were designed to deliver the CF transmembrane regulator (CFTR) gene and correct the basic CFTR defect by restoring chloride transport and reverting the upregulation of proinflammatory cytokines.
However, vector DNA expression was limited in duration because of the low incidence of integration and natural airway epithelium turnover. In addition, repeated administration of AAV-CFTR vector resulted in a humoral immune response that prevented effective gene transfer from subsequent doses of vector. AAV serotype 2 was used in human trials before the comparison with other serotypes and determination that serotypes 1 and 5 not only possess higher tropism for the airway epithelium, but also are capable of bypassing the binding and trafficking processes-both were important hindrances to the effectiveness of rAAV2.
Although rAAV-CFTR gene therapy does not appear likely to supplant newer small-molecule CFTR modulators in the near future, early work with rAAV-CFTR provided an important foundation for later use of rAAV in humans
.— A clear summary of the present situation regarding viral vectors for gene therapy in CF.
Heather S Loring is at the Horae Gene Therapy Center, University of Massachusetts Medical School , Worcester, Massachusetts.
Madge S; Bell SC; Burgel PR; De Rijcke K; Blasi F; Elborn JS; ERS/ECFS task force: Limitations to providing adult cystic fibrosis care in Europe: Results of a care centre survey. The provision of care for adults with cystic fibrosis in Europe. J Cyst Fibrosis 2016 Jul 25.[PubMed]

Fig. 78 Sue Madge
There are a growing number of adults in Europe with a projected increase of 75% over the next decade. There is concern that provision of care will not be sufficient to meet needs. We aimed to establish the level of CF service throughout Europe. An online survey designed by clinicians and patient representatives to explore level of service.Training opportunities for clinicians and resources (physical and manpower) to provide care to adults with CF are limited in Europe. Although specific adult CF care has been identified, teams continue to be supported by paediatric colleagues and many adults are still being admitted to paediatric wards. In some centres, service delivery, particularly infection control and access to some CF medication is insufficient and in many places poor personnel resources limits access to comprehensive multidisciplinary teams. This survey shows an urgent need for the development of resources for adult CF care, in both physical space and appropriately trained clinicians.
Dr Sue Madge (fig.78) is a Consultant Nurse at the Royal Brompton and Harefield Hospitals.
Mainz JG, Schumacher U, Schädlich K, Hentschel J, Koitschev C, Koitschev A, Riethmüller J, Prenzel F, Sommerburg O, Wiedemann B, Staab D, Gleiber W, Fischer R, Beck JF, Arnold C. Sino nasal inhalation of isotonic versus hypertonic saline (6.0%) in CF patients with chronic rhinosinusitis – Results of a multicenter, prospective, randomized, double-blind, controlled trial. J Cyst Fibros. 2016 Jun 4. pii: S1569-1993(16)30052-2. doi: 10.1016/j.jcf.2016.05.003. [Epub ahead of print] [PubMed]

Fig. 79 Jochen Mainz
Sixty nine CF patients with chronic rhino-sinusitis in eleven German CF centers were randomized to receive sinonasal vibrating inhalation of either NaCl 6.0% or NaCl 0.9% for 28days. After 28days of washout, patients crossed over to the alternative treatment. The primary outcome parameter was symptom score in the disease-specific quality of life Sino-Nasal Outcome Test-20 (SNOT-20). Additionally, pulmonary function was assessed, as well as rhinomanometry and inflammatory markers in nasal lavage (neutrophil elastase, interleukin (IL)-1β, IL-6, and IL-8) in a subgroup.Both therapeutic arms were well tolerated and showed slight improvements in SNOT-20 total scores (NaCl 6.0%: -3.1±6.5 points, NaCl 0.9%: -5.1±8.3 points, ns). In both treatment groups, changes of inflammatory parameters in nasal lavage from day 1 to day 29 were not significant. We suppose that the irritating properties of NaCl 6.0% reduced the suitability of the SNOT-20 scores as an outcome parameter. Alternative primary outcome parameters such as MR-imaging or the quantity of sinonasal secretions mobilised with both saline concentrations were, however, not feasible.
The authors concluded sinonasal inhalation with NaCl 6.0% did not lead to superior results vs. NaCl 0.9%, but recall in a previous study dornase alfa had been significantly more effective than NaCl 0.9%.
Jochen G Mainz (fig. 79) is professor at Jena University Hospital, CF Centre, Jena, Germany.
Massie J; Robinson PJ; Cooper PJ. The story of cystic fibrosis 1965-2015 J Paediatr Child H 2016 Sep 1. [PubMed]
There have been dramatic changes in the care of children with cystic fibrosis (CF) from 1965 to 2015. The initial improvements were the result of incremental gains in medical knowledge and better use of available therapies. Some CF-specific drugs were developed (recombinant human DNase and purified tobramycin for inhalation), but these simply delayed the progression of the lung damage. The discovery of the CF transmembrane conductance regulator gene in 1989 created an explosion of knowledge of airway biology and CF pathophysiology. Now mutation-specific therapy to potentiate mutated CF transmembrane conductance regulator is available for some patients with CF and is transforming their lives. Further advances are eagerly anticipated to benefit all patients with CF.
Massie J. Newborn screening and population carrier screening for cystic fibrosis: Two ends of the same rope. J Cyst Fibros. 2016 Jul;15(4):407-8. doi: 10.1016/j.jcf.2016.05.006. Epub 2016 May 31.[PubMed]

Fig. 80 John Massie melbournepaediatric specialists
In this timely editorial John Massie discuses four papers on this subject in this issue – a subject on which he has extensive practical experience. He notes as CF is inherited more than the affected infants can benefit from the diagnosis. With access to cascade screening why does anyone have to have their first child with CF to derive these benefits when the same mutation analysis test used for screening is widely available and not all that expensive?The four articles discussed are on maternal knowledge about CF NBS (Fitzgerald et al, 2016), on parental experience of screening (Rueegg et al, 2016), on how families use the information about a family member with CF for cascade carrier testing (Dugueperoux et al, 2016) and the fourth about community based carrier testing and its relevance to NBS (Stafler et al, 2016). These papers are discussed in more detail below.Massie concludes this group of papers on CF NBS and carrier screening demonstrates the value of on going quality improvement, relevant to new programs and existing ones alike. The timeliness of definitive diagnosis by post-NBS including sweat testing and consultation with the CF team is essential to quality care. He suggests further work needs to be done to consider the consent process for NBS. This respects parents’ autonomy and in doing so augments the provision of information that will help a wider knowledge of CF and promote cascade family testing and perhaps population carrier screening. As we move forward we should aim for the best possible CF screening service. Finally CF NBS, cascade carrier testing and population-based screening are a continuum that could well be served by single national programs to offer all people reproductive choices and have those born with CF referred for care sooner. This suggestion is very relevant as many families are not, at present, benefiting from the choices possible with optimal use our existing knowledge
An excellent review of this area by an acknowledged paediatric expert in the field.
Prof. John Massie (fig 80) Respiratory Paediatrician Department of Respiratory Medicine, Royal Children’s Hospital, Australia; Department of Paediatrics, University of Melbourne, Australia.
McColley SA. A safety evaluation of ivacaftor for the treatment of cystic fibrosis. Expert Opin Drug Saf. 2016 Apr 7:1-7. [Epub ahead of print] [PubMed]

Fig. 81 Susanna A McColley Feinberg.northwestern.edu
This article reviews ivacaftor safety. Areas covered: Safety findings in ivacaftor clinical trials, and reported subsequently, were accessed by a PubMed search using key words “VX-770” or “ivacaftor”. Additional information was accessed via Google Search. Transaminitis (“raised transaminase coupled with non-specific hepatitis”) was noted in ivacaftor and combination lumacaftor-ivacaftor trials. Ivacaftor was associated with cataracts in juvenile rat pups in pre-clinical studies; non-congenital cataracts have been found in children taking ivacaftor. Ivacaftor is a CYP3A substrate; CYP3A inhibitors and inducers should be avoided during its administration. Ivacaftor and its M1 metabolite may inhibit CYP3A and P-gp; therefore, ivacaftor may increase systemic exposure to drugs which are substrates of CYP3A and/or P-gp, increasing the potential for adverse events.
Expert opinion: Ivacaftor therapy may be associated with ocular and hepatic side effects; specific recommendations for monitoring are available.The authors advise potential drug interactions should be evaluated in patients taking ivacaftor. High clinical efficacy suggests that the risk benefit ratio of ivacaftor favors therapy.
McElvaney NG. Alpha-1 antitrypsin therapy in Cystic Fibrosis and the Lung Disease Associated with Alpha-1 antitrypsin Deficiency. Ann Am Thor Soc 2016; 13 Suppl 2:S191-6.[PubMed]

Fig. 82 Gerry McElvaney
Cystic fibrosis and alpha-1 antitrypsin (AAT) deficiency are two of the commonest lethal hereditary lung diseases affecting white individuals. Although having quite different phenotypic extrapulmonary presentations, the lung disease associated with these conditions is exemplified by a neutrophil-dominated inflammation in which neutrophil elastase plays a major role. In AAT deficiency the diminution of the anti-neutrophil elastase protection, due to diminished AAT levels in the lung, predisposes the lung to an unopposed neutrophil elastase attack, whereas, in cystic fibrosis, the levels of AAT and other antiproteases are normal, but the neutrophil elastase burden is so large that it overwhelms the normal anti-neutrophil elastase protection. With this as background, it seems logical to augment the anti-neutrophil elastase defences of the lung in both conditions using exogenous AAT. The type of AAT, the route of administration, and the physiologic, radiologic, and clinical readouts for this type of therapy are discussed, along with the similarities and differences between the two conditions and their responses to AAT therapy.
Noel G McElvaney (fig 82) is Professor at Respiratory Research Division, Royal College of Surgeons in Ireland, Beaumont Hospital, Dublin, Ireland.
Mika M, Korten I, Qi W, Regamey N, Frey U, Casaulta C, Latzin P, Hilty M; SCILD study group. The nasal microbiota in infants with cystic fibrosis in the first year of life: a prospective cohort study. Lancet Respir Med. 2016 Aug;4(8):627-35. doi: 10.1016/S2213-2600(16)30081-9. Epub 2016 May 11. [PubMed]

Fig. 83 Moana Mika
sp-ps.ch
Between Feb 1, 2011, and May 31, 2014, the authors enrolled 30 infants with a diagnosis of cystic fibrosis. Microbiota characterisation was done with 16S rRNA gene pyrosequencing and oligotyping of nasal swabs collected every 2 weeks from the infants with cystic fibrosis. They compared these data with data for an age-matched cohort of 47 healthy infants. They additionally investigated the effect of antibiotic treatment on the microbiota of infants with cystic fibrosis.
FINDINGS. The microbiota of infants with cystic fibrosis differed compositionally from that of healthy infants (p=0·001). This difference was also found in exclusively antibiotic-naive samples (p=0·001). The disordering was mainly, but not solely, due to an overall increase in the mean relative abundance of Staphylococcaceae in infants with cystic fibrosis compared with healthy infants. Oligotyping analysis enabled differentiation between Staphylococcus aureus and coagulase-negative Staphylococci. Whereas the analysis showed a decrease in S. aureus at and after antibiotic treatment, coagulase-negative Staphylococci increased.
The authors suggest their findings could be used to inform future studies of the effect of antibiotic treatment on the microbiota in infants with cystic fibrosis, and could assist in the prevention of early disease progression in infants with this disorder.
— This study confirms a reduction in S. aureus with antibiotic treatment being supportive of the (controversial to some!!!) recommendations of the UK CF Trust Antibiotic Group for long term flucloxacillin for the first 3 years.
Moana Mika (fig. 83) is at the Institute for Infectious Diseases, University of Bern, Bern, Switzerland; Graduate School for Cellular and Biomedical Sciences, University of Bern, Bern, Switzerland.
Milla CE, Ratjen F, Marigowda G, Liu F, Waltz D, Rosenfeld M; VX13-809-011 Part B Investigator Group. Lumacaftor/Ivacaftor in Patients Aged 6-11 Years With Cystic Fibrosis Homozygous for F508del-CFTR. Am J Respir Crit Care Med. 2016 Nov 2. [Epub ahead of print] [PubMed]

Fig 84 Carlos Milla profiles,stantford.edu
Combination lumacaftor/ivacaftor has been shown to improve lung function and other endpoints in patients aged ≥12 years with cystic fibrosis homozygous for F508del-CFTR but has not been assessed in younger patients.
This open-label phase 3 trial evaluated the safety, tolerability, pharmacodynamics, and efficacy of lumacaftor/ivacaftor combination therapy in patients aged 6-11 years with cystic fibrosis homozygous for F508del-CFTR. Patients (N = 58) received 200 mg lumacaftor/250 mg ivacaftor orally every 12 hours for 24 weeks in addition to their existing cystic fibrosis medications.
Lumacaftor/ivacaftor was well tolerated; the safety profile was generally similar to that observed in larger lumacaftor/ivacaftor trials in older patients. Four patients discontinued (two due to drug-related adverse events: elevated liver transaminases, n=1; rash, n=1). No safety concerns were associated with spirometry. No significant changes in % predicted FEV1 were observed (change from baseline at Week 24, +2.5 percentage points; 95% CI, -0.2 to 5.2; P = 0.0671). At Week 24, significant improvements from baseline were observed in sweat chloride (-24.8 mmol/L; 95% CI, -29.1 to -20.5; P < 0.0001), BMI z score (+0.15; 95% CI, 0.08 to 0.22; P < 0.0001), Cystic Fibrosis Questionnaire-Revised respiratory domain score (+5.4; 95% CI, 1.4 to 9.4; P = 0.0085), and lung clearance index 2.5 (-0.88; 95% CI, -1.40 to -0.37; P = 0.0018).
— Lumacaftor/ivacaftor was well tolerated in this young population; no new safety concerns were identified. Improvements in lung clearance index, sweat chloride, nutritional status, and health-related quality of life were observed after 24 weeks of treatment.
Carlos E Milla (fig.84) is Professor in the Department of Pediatrics, Stanford University, Palo Alto, California.
Moran Gal, Khen Khermesh, Michal Barak, Min Lin, Hadas Lahat, Haike Reznik Wolf, Michael Lin, Elon Pras, and Erez Y. Levanon![]() Expanding preconception carrier screening for the Jewish population using high throughput microfluidics technology and next generation sequencing BMC Med Genomics 2016 ;9(1):24. Free PMC article. [PubMed]
Expanding preconception carrier screening for the Jewish population using high throughput microfluidics technology and next generation sequencing BMC Med Genomics 2016 ;9(1):24. Free PMC article. [PubMed]
The authors examine the implementation of the combined high-throughput technologies of specific target amplification and next generation sequencing (NGS), for expanding the carrier screening program in the Israeli Jewish population as a test case.They compiled a panel of 370 germline mutations, causing 120 disorders, previously identified in affected Jewish individuals from different ethnicities. This mutation panel was simultaneously captured in 48 samples using a multiplex PCR-based microfluidics approach followed by NGS, thereby performing 17,760 individual assays in a single experiment.The sensitivity (measured with depth of at least 50×) and specificity of the target capture was 98 and 95% respectively, leaving minimal rate of inconclusive tests per sample tested. 97% of the targeted mutations present in the samples were correctly identified and validated.
The authors concluded their methodology was shown to successfully combine multiplexing of target specific primers, samples indexing and NGS technology for population genetic screens. Moreover, it’s relatively ease of use and flexibility of updating the targets screened, makes it highly suitable for clinical implementation.This protocol was demonstrated in pre-conceptional screening for pan-Jewish individuals, but can be applied to any other population or different sets of mutations.
Moran Gal is at The Mina and Everard Goodman Faculty of Life Sciences, Bar-Ilan University, Ramat Gan, 52900, Israel.
Munck A; Alberti C; Colombo C; Kashirskaya N; Ellemunter H; Fotoulaki M; Houwen R; Robberecht E; Boizeau P; Wilschanski M; CF/Pancreas ESPGHAN Working Group and DIOS Study Group. International prospective study of distal intestinal obstruction syndrome in cystic fibrosis: Associated factors and outcome. J Cyst Fibros 2016; 5(4):531-9. [PubMed]

Fig. 85 Anne Munck
European CF Society
Distal intestinal obstruction syndrome (DIOS) is a specific complication of cystic fibrosis. METHODS: A study was performed in 10 countries to prospectively evaluate the incidence, associated factors, and treatment modalities in children and adults. RESULTS: 102 patients presented 112 episodes. The incidence of DIOS was similar in children and adults. Medical treatment failed only in cases of complete DIOS (11%). Children with meconium ileus had a higher rate of surgery for DIOS (15% vs. 2%, p=0.02). Complete DIOS entailed longer hospitalisation (4 [3; 7] days vs. 3 [1; 4], p=0.002). Delayed arrival at hospital and prior weight loss had a significant impact on the time needed for DIOS resolution. Associated CF co-morbidities for DIOS included meconium ileus (40% vs. 18%, p<0.0001), exocrine pancreatic insufficiency (92% vs. 84%, p=0.03), liver disease (22% vs. 12%, p=0.004), diabetes mellitus (49% vs. 25%, p=0.0003), and Pseudomonas aeruginosa (68% vs. 52%, p=0.01); low fibre intake and insufficient hydration were frequently observed. Female gender was associated with recurrent DIOS (75% vs. 52%, p=0.04), constipation with incomplete episodes (39% vs. 11%, p=0.03), and poor patient compliance in taking pancreatic enzyme therapy during complete episodes (25% vs. 3%, p=0.02).
The authors concluded DIOS is a multifactorial condition having a similar incidence in children and adults. They show that delayed arrival at hospital after the initial symptoms causes significant morbidity. Early recognition and treatment would improve the prognosis.
Anne Munck (fig. 85) is at the Hôpital Robert Debré, Paediatric Gastroenterology and Respiratory Department, CF Centre, University Paris 7, 75019 Paris, France.
Nielsen AO; Qayum S; Bouchelouche PN; Laursen LC; Dahl R; Dahl M. Risk of asthma in heterozygous carriers for cystic fibrosis: A meta-analysis. J Cyst Fibros 2016; 15(5):563-7. [PubMed]

Fig. 86 Anne Orholm Nielsen
LinkedIn
The authors screened the medical literature from 1966 to 2015 and performed a meta-analysis to determine the risk of asthma in CF heterozygotes vs. non-carriers. Aggregating data from 15 studies, the odds ratio for asthma in CF heterozygotes compared with non-carriers was significantly elevated at 1.61 (95% CI: 1.18-2.21) showing that heterozygous carriers for CF have a higher risk of asthma than non-carriers.
— There are similar findings by Schultz and Tummler
Anne Orholm Nielsen (fig.86) is at Department of Clinical Biochemistry, Zealand University Hospital, Køge, Denmark.
Schulz A; Tummler B. Non-allergic asthma as a CFTR-related disorder. J Cyst Fibros 2016; 15(5):641-4. pubmed.ncbi.nlm.nih.gov/26526220/
Subjects with cystic fibrosis-like disease, equivocal sweat chloride concentrations and no or one disease-causing CFTR mutation were investigated by intestinal current and/or nasal potential difference measurements. A subgroup of 7 female patients who had been diagnosed to suffer from non-allergic asthma showed intermediary chloride concentrations in sweat test, normal chloride secretory responses in the intestine and an abnormal nasal potential difference with Sermet scores in the cystic fibrosis range.
The authors concluded non-allergic asthma is a clinical entity that may be associated with CFTR dysfunction of the respiratory epithelium. Nasal potential difference is a rapid reliable and cost effective CFTR biomarker to identify subjects with CFTR related disorder among patients with non-allergic asthma or idiopathic bronchiectasis.
Angela Schultz is at the Clinic for Paediatric Pneumology, Allergology and Neonatology, Hannover Medical School, Hannover, Germany; Biomedical Research in Endstage and Obstructive Lung Disease (BREATH), German Center for Lung Research, Hannover, Germany.
Niccum DE, Billings JL, Dunitz JM, Khoruts A. Colonoscopic screening shows increased early incidence and progression of adenomas in cystic fibrosis. J Cyst Fibros. 2016 Feb 2. pii: S1569-1993(16)00009-6. doi: 10.1016/j.jcf.2016.01.002. [Epub ahead of print] [PubMed]

Fig. 87 David Niccum
LinkedIn
Colorectal cancer is an emerging problem in cystic fibrosis (CF). The goal of this study was to evaluate adenoma detection by systematic colonoscopic screening and surveillance. The authors analyzed prospectively collected results of colonoscopies initiated at age 40 years from 88 CF patients at a single Cystic Fibrosis Center. They also reviewed results of diagnostic colonoscopies from 27 patients aged 30-39years performed during the same time period at the Center.The incidence of polyp detection increased markedly after age 40 in CF patients.
Greater than 50% were found to have adenomatous polyps; approximately 25% had advanced adenomas as defined by size and/or histopathology; 3% were found to have colon cancer.
Multivariate analysis demonstrated specific risk factors for adenoma formation and progression.
Authors suggested early screening and more frequent surveillance should be considered in patients with CF due to early incidence and progression of adenomas in this patient population.
— This is obviously potentially a serious problem as the survival improves for people with CF.
David E Neccum (fig. 87) is in the Department of Medicine, Division of Pulmonary, Allergy, Critical Care and Sleep Medicine, University of Minnesota, United States. From 2016 he is with Health Partners Greater Minneapolis-St Paul Area
Nichols DP, Happoldt CL, Bratcher PE, Caceres SM, Chmiel JF, Malcolm KC, Saavedra MT, Saiman L, Taylor-Cousar JL, Nick JA. Impact of azithromycin on the clinical and antimicrobial effectiveness of tobramycin in the treatment of cystic fibrosis. J Cyst Fibros. 2016 Dec 24. pii: S1569-1993(16)30672-5. doi: 10.1016/j.jcf.2016.12.003. [Epub ahead of print][PubMed]

Fig. 88 David Nichols depts.washington.edu
Concomitant use of oral azithromycin and inhaled tobramycin occurs in approximately half of US cystic fibrosis (CF) patients. Recent data suggest that this combination may be antagonistic. Test the hypothesis that azithromycin reduces the clinical benefits of tobramycin by analyses of clinical trial data, in vitro modeling of P. aeruginosa antibiotic killing, and regulation of the MexXY efflux pump. Ongoing administration of azithromycin associates with reduced ability of inhaled tobramycin, as compared with aztreonam, to improve lung function and quality of life in a completed clinical trial. In users of azithromycin FEV1 (L) increased 0.8% during a 4-week period of inhaled tobramycin and an additional 6.4% during a subsequent 4-week period of inhaled aztreonam (P<0.005). CFQ-R respiratory symptom score decreased 1.8 points during inhaled tobramycin and increased 8.3 points during subsequent inhaled aztreonam (P<0.001). A smaller number of trial participants not using azithromycin had similar improvement in lung function and quality of life scores during inhaled tobramycin and inhaled aztreonam. In vitro, azithromycin selectively reduced the bactericidal effects tobramycin in cultures of clinical strains of P. aeruginosa, while up regulating antibiotic resistance through MexXY efflux.
The authors concluded azithromycin appears capable of reducing the antimicrobial benefits of tobramycin by inducing adaptive bacterial stress responses in P. aeruginosa, suggesting that these medications together may not be optimal chronic therapy for at least some patients.
— Further doubts about the value of long term azithromycin.
David P Nichols is Associate Professor of Pediatrics, CF clinician, and Medical Director of the TDN Coordinating Center at the Department of Pediatrics, Seattle Children’s Hospital, University of Washington School of Medicine, Seattle, WA, United States.
O’Connor MG; Seegmiller A. The effects of ivacaftor on CF fatty acid metabolism: An analysis from the GOAL study. J Cyst Fibros 2016 Jul 26. [PubMed]

Fig. 89 Michael G O’Connor
health.usnews.com
Abnormalities in fatty acid metabolism have previously been shown to be a characteristic of CFTR dysfunction. The authors hypothesized that as a reflection of this clinical improvement, ivacaftor would improve plasma fatty acid levels and decrease urine prostaglandin E metabolite levels. They analyzed plasma fatty acid levels and urine prostaglandin E metabolites (PGE-M) in 40 subjects with CF participating in the G551D observational (GOAL) study who demonstrated response to the medication by a significant decrease in sweat Cl levels.
They found ivacaftor reduces inflammatory PGE without fully correcting the plasma fatty acid abnormalities of CF. Age-related differences in fatty acid levels were observed, that may be a result of other clinical factors, such as diet, clinical care, or drug response.
Michael Glenn O’Connor is in the Department of Pediatrics, Division Pediatric Pulmonary, Allergy, and Immunology, Vanderbilt University School of Medicine, Nashville, TN, United States.
Ooi CY; Jeyaruban C; Lau J; Katz T; Matson A; Bell SC; Adams SE; Krishnan U. High ambient temperature and risk of intestinal obstruction in cystic fibrosis. J Paediatr Child Health 2016; 52(4):430-5. [PubMed]

Fig 90. (Keith) Chee Lee Ooi
Distal intestinal obstruction syndrome (DIOS) and constipation in cystic fibrosis (CF) are conditions associated with impaction and/or obstruction by abnormally viscid mucofaecal material within the intestinal lumen. Dehydration has been proposed as a risk factor for DIOS and constipation in CF. A study primarily aimed to determine whether warmer ambient temperature and lower rainfall are risk factors for DIOS and constipation in CF
The authors found that relatively high ambient temperature may play a role in the pathogenesis of DIOS and constipation in CF.
Chee Yee Ooi (fig.90) is Paediatric Gastroenterologist at the Sydney Children’s Hospital and has a particular interest in the field of CF diagnosis, gastrointestinal disease in CF and pancreatitis.
O’Neill K; Tunney MM; Johnston E; Rowan S; Downey DG; Rendall J; Reid A; Bradbury I; Elborn JS; Bradley JM. Lung clearance index in adults and children with cystic fibrosis. Chest. , 2016 Jul 6 [PubMed]

Fig. 91 Katherine O’Neill
LinkedIn
Lung clearance index (LCI) has good clinimetric properties and an acceptable feasibility profile as a surrogate endpoint in Cystic Fibrosis (CF). Although most studies to date have been in children, increasing numbers of adults with CF also have normal spirometry. Further study of LCI as an endpoint in CF adults is required. Therefore, the purpose of this study was to determine the clinimetric properties of LCI over the complete age range of people with CF.Clinically stable adults and children with CF and age matched healthy controls were recruited. LCI and spirometry data for 110 CF subjects and 61 controls were collected at a stable visit. CF Questionnaire-Revised (CFQ-R) was completed by 80/110 CF subjects. Fifty-six CF subjects completed a second stable visit. The LCI CV% was 4.1% in adults and 6.3% in children with CF. The coefficient of repeatability of LCI was 1.2 in adults and 1.3 in children. In both adults and children, LCI (AUC(ROC)=0.93 and 0.84) had greater combined sensitivity and specificity to discriminate between people with CF and controls compared to FEV1 (AUC(ROC)=0.88 and 0.60) and FEF25-75 (AUC(ROC)=0.87 and 0.68). LCI correlated significantly with the CFQ-R treatment burden in adults (r=-0.37; p<0.01) and children (r=-0.50; p<0.01). Washout tests were successful in 90% of CF subjects and were perceived as comfortable and easy to perform in both adults and children.
The authors consider these data support the use of LCI as a surrogate outcome measure in CF clinical trials in adults as well as children.
Katherine O’Neill (fig. 91) is Clinical Research Fellow at the Centre for Experimental Medicine, School of Medicine, Dentistry and Biomedical Sciences, Queen’s University Belfast, Northern Ireland. Subsequently Katherine became Change Project Manager iREACH Health Queen’s University Belfast.
Peckham D; Williams K; Wynne S; Denton M; Pollard K; Barton R. Fungal contamination of nebuliser devices used by people with cystic fibrosis. J Cyst Fibros 2016; 15(1):74-7. [PubMed]

Fig 92. Miles Denton and Daniel Peckham
A total of 170 nebulisers from 149 subjects were screened by wetting a sterile cotton swab with sterile water and swabbing each drug chamber. The swab was then plated out on Sabouraud and on Scel+agar and incubated at 27 degree C for up to 2 weeks.Fungal cultures were positive in 86 (57.7%) patient’s devices. In 28/149 (18.8%), 39/149 (26.2%), 47/149 (31.5%) and 20/149 (13.4%) of subjects Aspergillus species, yeasts, moulds and both yeasts and moulds were isolated respectively. There was no difference in contamination rates between different devices.
The authors concluded nebuliser devices are frequently contaminated by moulds and yeasts and emphasis should be placed on ensuring adequate nebuliser hygiene.
Daniel Peckham (fig. 92) is Professor of Respiratory Medicine and Director of the Leeds Regional Adult CF Centre.
Miles Denton (fig.92) is consultant Microbiologist at Leeds Teaching Hospitals NHS Trust
Peckham D. Electronic patient records, past, present and future. Paed Resp Rev 2016; 20 Suppl:8-11. [PubMed]
The health informatics revolution was spear-headed in the 1980s by pioneers in primary care who worked in an opportune environment and were able to successfully implement electronic patient records (EPR) as far back as the 1990s. Although the ambitious and costly National Programme for IT failed to deliver an integrated EPR, the project achieved the creation of the Spine, the N3 Network, choose and book, picture archiving, communication systems and standards, which have allowed integration.
Real change is taking place within the NHS with the launch of exciting new projects focusing on true integration and secure data flows across primary, community and secondary care. These changes have been brought about by the realisation that linking “best in class” is more likely to secure a successful cost-effective national integrated electronic patient records.
Pisaturo M; Deppen A; Rochat I; Robinson WM; Hafen GM. Death after cessation of treatment by cystic fibrosis patients: An international survey of clinicians. Palliative Med 2016 Mar 15.[PubMed]

Fig 93. Maria Soriano-Pisaturo
An online survey was distributed across three continents. Distribution to the medical directors of the cystic fibrosis centres affiliated with the US Cystic Fibrosis Foundation, Cystic Fibrosis Australia (inclusion of New Zealand) and to every clinician member of the European Cystic Fibrosis Society.The clinicians surveyed reported more than 200 cystic fibrosis patients not considered being terminally ill and, who voluntarily ceased treatment. Detailed data were reported in 102 patients (4 children, 25 adolescents and 73 adults). Only one child, six adolescents and one adult were judged by clinicians not to be competent to make the decision to stop treatment.
Time-consuming and low immediate-impact therapies, such as respiratory physiotherapy, were most frequently discontinued. Resignation was the main reported reason for discontinuing treatment, followed by reactive depression and lack of familial support. A total of 69% of the patients received palliative care and 72% died in the 6 months following cessation of treatment.These details concerning death of cystic fibrosis patients, not considered to be terminally ill, due to voluntary cessation of treatment are reported in Europe, the United States and Australia.
– Despite the understandable enthusiasm for the new mutation specific treatments, life with CF can prove to be quite intolerable for some people with the condition as evidenced by this study.
Maria A. Soriano-Pisaturo MD (fig. 93) practices Hospice & Palliative Medicine in North Providence, RI. She currently practices at Roger Williams Senior Healthcare Associates and is affiliated with Roger Williams Medical Center.
Plantinga M, Birnie E, Abbott KM, Sinke RJ, Lucassen AM, Schuurmans J, Kaplan S, Verkerk MA, Ranchor AV, van Langen IM. Population-based preconception carrier screening: how potential users from the general population view a test for 50 serious diseases. J Hum Genet. 2016 Oct;24(10):1417-23. doi: 10.1038/ejhg.2016.43. Epub 2016 May 11. [PubMed]

Fig. 94 Mirjam Plantinga
rug.nl/staff
To date, preconception carrier screening (PCS) has largely targeted single diseases such as cystic fibrosis, but next generation sequencing (NGS) allows the testing of many genes or diseases simultaneously. The authors have developed an expanded NGS PCS test for couples; simultaneously it covers 50 very serious, early-onset, autosomal recessive diseases that are untreatable.
This is the first, noncommercial, population-based, expanded PCS test to be offered prospectively to couples in a health-care setting in Europe. So far, little is known about how potential users view such a PCS test. They therefore performed an online survey in 2014 among 50 people from the target population in the Netherlands. They enquired about their intention to take an expanded PCS test if one was offered, and through which provider they would like to see it offered.
One-third of the respondents said they would take such a test were it to be offered. The majority (44%) preferred the test to be offered via their general practitioner (GP) and 58% would be willing to pay for the test, with a median cost 75 Euro. They intend to perform an implementation study in which this PCS test will be provided via selected GPs in the Northern Netherlands.
– This is the way forward although for conditions such as cystic fibrosis there seems to be limited enthusiasm for such a policy. Lack of knowledge and some religious beliefs are obstacles to progress.
Mirjam Plantinga (Fig (94 ) is a Senior Researcher in Department of Genetics, University Medical Center Groningen, University of Groningen, Groningen, The Netherlands.
Prayle AP; Jain K; Touw DJ; Koch BC; Knox AJ; Watson A; Smyth AR. The pharmacokinetics and toxicity of morning vs. evening tobramycin dosing for pulmonary exacerbations of cystic fibrosis: A randomised comparison. J Cyst Fibros 2016; 15(4):510-7. 2 Free article[PubMed]

Fig. 95 Andrew Prayle cf.cochrane.org
Circadian variation in renal toxicity of aminoglycosides has been demonstrated in animal and human studies. People with CF are frequently prescribed aminoglycosides. Altered pharmacokinetics of aminoglycosides are predictive of toxicity. The aim was to investigate whether the time of day of aminoglycoside administration modulates renal excretion of tobramycin and toxicity in children with CF. To determine whether circadian rhythms are disrupted in children with CF during hospital admission. The authors’ conclusions were that renal elimination of tobramycin was not affected by the time of day of administration. Urinary KIM-1 raises the possibility of greater nephrotoxicity with evening administration. Four children showed disturbed circadian rhythm and high melatonin levels.
The authors sate the clinical implications of a rise in KIM1 for the individual patient is not yet known
Andrew P Prayle (fig. 95) is in the Division of Child health at The University of Nottingham, Nottingham, United Kingdom.
Prevaes SM; de Winter-de Groot KM; Janssens HM; de Steenhuijsen Piters WA; Tramper-Stranders GA; Wyllie AL; Hasrat R; Tiddens HA; van Westreenen M; van der Ent CK; Sanders EA; Bogaert D. Development of the Nasopharyngeal Microbiota in Infants with Cystic Fibrosis. Am J Resp Crit Care 2016; 193(5):504-15. [PubMed]

Fig. 96 Sabine Prevaes
ResearchGate
A study to investigate the development of nasopharyngeal microbiota profiles in infants with CF compared with those of healthy control subjects during the first 6 months of life. A prospective cohort study, from the time of diagnosis onward, in which the authors collected questionnaires and 324 nasopharynx samples from 20 infants with CF and 45 age-matched healthy control subjects. In infants with CF, early Staphylococcus aureus and, to a lesser extent, Corynebacterium spp. and Moraxella spp. dominance were followed by a switch to Streptococcus mitis predominance after 3 months of age. In control subjects, Moraxella spp. enrichment occurred throughout the first 6 months of life. In a multivariate analysis, S. aureus, S. mitis, Corynebacterium accolens, and bacilli were significantly more abundant in infants with CF, whereas Moraxella spp., Corynebacterium pseudodiphtericum and Corynebacterium propinquum and Haemophilus influenzae were significantly more abundant in control subjects, after correction for age, antibiotic use, and respiratory symptoms. Antibiotic use was independently associated with increased colonization of gram-negative bacteria such as Burkholderia spp. and members of the Enterobacteriaceae bacteria family and reduced colonization of potential beneficial commensals. From diagnosis onward, the authors observed distinct patterns of nasopharyngeal microbiota development in infants with CF under 6 months of age compared with control subjects and a marked effect of antibiotic therapy leading toward a gram-negative microbial composition.
Sabine M P J Prevaes (fig.96) is a Fellow Pediatric Pulmonology and Clinical Researcher in the Department of Pediatrics, Wilhelmina Children’s Hospital, University Medical Center Utrecht, Utrecht, the Netherlands.
Psoter KJ; DE Roos AJ; Wakefield J; Mayer JD; Bryan M; Rosenfeld M. Association of meteorological and geographical factors and risk of initial Pseudomonas aeruginosa acquisition in young children with cystic fibrosis. Epidemiol Infect 2016; 144(5):1075-83.[PubMed]
Meteorological and geographical factors and risk of initial Pa acquisition in young children with CF were examined using the U.S. Cystic Fibrosis Foundation Patient Registry from 2003 to 2009. The results suggest that environmental factors may play a previously unrecognized role in the aetiology of initial Pa acquisition.
— The authors concluded meteorological and geographical factors, particularly increased temperature, dew point and rainfall were found to be associated with time to initial Pa acquisition in young children with CF. They have published on this subject previously and this paper is a useful source of references on the subject.
K J Poster is in the Department of Biostatistics, Johns Hopkins Bloomberg School of Public Health,Baltimore,MD,USA.
Quittner AL; Abbott J; Georgiopoulos AM; Goldbeck L; Smith B; Hempstead SE; Marshall B; Sabadosa KA; Elborn S; International Committee on Mental Health; EPOS Trial Study Group. International Committee on Mental Health in Cystic Fibrosis: Cystic Fibrosis Foundation and European Cystic Fibrosis Society consensus statements for screening and treating depression and anxiety. Thorax 2016; 71(1):26-34.Free full PMC article [PubMed]
Studies measuring psychological distress in individuals with cystic fibrosis (CF) have found high rates of both depression and anxiety. Psychological symptoms in both individuals with CF and parent caregivers have been associated with decreased lung function, lower body mass index, worse adherence, worse health-related quality of life, more frequent hospitalisations and increased healthcare costs. To identify and treat depression and anxiety in CF, the CF Foundation and the European CF Society invited a panel of experts, including physicians, psychologists, psychiatrists, nurses, social workers, a pharmacist, parents and an individual with CF, to develop consensus recommendations for clinical care.
— There is agreement in all similar studies and that depression and anxiety are frequent in both children and adults with CF and their parents. It is unlikely that these will lessen even with the newer mutation specific drugs and talk of a “cure”. It is unfortunate that the now extensive knowledge of carrier detection, population and antenatal screening, which allow known carrier couples to choose to have an unaffected child, receive such low priority.
Alexandra Quittner is at the University of Miami, Coral Gables, Florida, USA.
Ram B; Aggarwal AN; Dhooria S; Sehgal IS; Garg M; Behera D; Chakrabarti A; Agarwal R. A pilot randomized trial of nebulized amphotericin in patients with allergic bronchopulmonary aspergillosis. J Asthma 2016; 53(5):517-24. [PubMed]

Fig. 97 Babu Ram
LinkedIn
Consecutive subjects of ABPA with recurrent exacerbations were randomised to receive nebulised amphotericin plus nebulized budesonide (NEB) or NEB alone. At one year, the numbers of patients experiencing exacerbation was significantly lower in the NAB arm (1/12 [8.3%] vs. 6/9 [66.7%]; p=0.016). The other secondary end points were not different between the two groups. There were no major adverse events leading to discontinuation of any of the study drugs. Three patients experienced bronchospasm after first dose of NAB; however, the subsequent doses were well tolerated. The authors concluded nebulised amphotericin seems to be beneficial in decreasing the frequency of exacerbations in patients with ABPA complicating asthma. The suggest larger trials are required to confirm their study results.
– These patients had asthma, not CF, complicated by ABPA but the findings are helpful and not unexpected.
Babu Ram is a Technical Assistant in the Department of Pulmonary Medicine , Postgraduate Institute of Medical Education and Research (PGIMER) , Chandigarh , India .
Ramsey KA, Rosenow T, Turkovic L, Skoric B, Banton G, Adams AM, Simpson SJ, Murray C, Ranganathan SC, Stick SM, Hall GL; AREST CF. Lung Clearance Index and Structural Lung Disease on Computed Tomography in Early Cystic Fibrosis. Am J Respir Crit Care Med. 2016 Jan 1;193(1):60-7. doi: 10.1164/rccm.201507-1409OC. [PubMed]

Fig 98. Kathryn Ramsay
The lung clearance index is a measure of ventilation distribution derived from the multiple-breath washout technique. It has been suggested as a surrogate for chest computed tomography to detect structural lung abnormalities in individuals with cystic fibrosis; however, the associations between lung clearance index and early structural lung disease are unclear. The authors assessed the ability of the lung clearance index to reflect structural lung disease on the basis of chest computed tomography across the entire pediatric age range.
In infants with CF, lung clearance index is insensitive to structural disease (κ = -0.03 [95% confidence interval, -0.05 to 0.16]). In preschool children with CF, lung clearance index correlates with total disease extent. In school-age children, lung clearance index correlates with extent of total disease, bronchiectasis, and air trapping. In preschool and school-age children, lung clearance index has a good positive predictive value (83-86%) but a poor negative predictive value (50-55%) to detect the presence of bronchiectasis.
The authors observe these data suggest that lung clearance index may be a useful surveillance tool to monitor structural lung disease in preschool and school-age children with CF. However, lung clearance index cannot replace chest computed tomography to screen for bronchiectasis in this population.
Dr Kathryn Ramsey (fig.98) is a researcher at the Telethon Kids Institute Australia and recently Research Fellow at Chapel Hill, University of North Carolina
Comment–Florian Singer, Carmen Casaulta, and Philipp Latzin “How to Monitor Early Cystic Fibrosis Lung Disease. By Multiple-Breath Washout, Chest Computed Tomography, or Both?” American Journal of Respiratory and Critical Care Medicine, Vol. 193, No. 1 (2016), pp. 7-8.
Reicher JJ; Mohabir P; Rad E; Gayer G. Increased prevalence of tracheal diverticula in cystic fibrosis patients. Brit J Radiol 2016; 89(1060). [PubMed]

Fig. 99 Joshua J Reicher
health.usnews.com
This investigation sought to evaluate the prevalence and imaging characteristics of tracheal diverticula (TD) among patients with cystic fibrosis (CF). 113 patients with CF, with a median age of 29 years, had chest CT examinations between 2002 and 2014.Of the 113 cases reviewed, 20 (17.7%) patients were found to have 1 or more TD. The presence of TD was associated with more severe disease by imaging criteria. Pulmonary function tests demonstrated an insignificant trend towards worsening function in patients with
The authors concluded the prevalence was 17.7% – a higher prevalence in patients with CF than in the general population and associated with more severe pulmonary disease.
— Initially estimated as present in 1% of an autopsy series, more recent CT studies estimate the incidence as 2% – 3.7%. Diverticula arise from the posterior tracheal wall where the cartilage rings are incomplete. Usually asymptomatic they may cause haemoptysis, dyspnoea, and dysphagia; they may act as a reservoir for infection
Joshua J Reicher (fig.99) s a radiologist and Resident Physician at Stanford Hospital & Clinics, Department of Radiology, Stanford, CA, USA.
Reznikov LR. Cystic Fibrosis and the Nervous System. Chest. 2016 Nov 19. pii: S0012-3692(16)62356-5. doi: 10.1016/j.chest.2016.11.009. [PubMed]
Many of the features observed in people with CF and organs affected in CF are modulated by the nervous system. CFTR expression has been reported in both the peripheral and central nervous systems, and it is well known that the transport of anions, such as chloride, greatly modulates neuronal excitability. Thus, it is predicted that in CF, lack of CFTR in the nervous system affects neuronal function. Consistent with this prediction, several nervous system abnormalities and nervous system disorders have been described in people with CF and animal models of CF. The goal of this special feature article is to highlight the expression and function of CFTR in the nervous system. Special emphasis is placed on nervous system abnormalities described in people with and animal models of CF. Lastly, features of CF that may be modulated by or attributed to faulty nervous system function are discussed.
Reznikov LR, Abou Alaiwa MH, Dohrn CL, Gansemer ND, Diekema DJ, Stoltz DA, Welsh MJ. Antibacterial properties of the CFTR potentiator ivacaftor. J Cyst Fibros. 2014 Sep;13(5):515-9. Doi 10.1016/j.jcf.2014.02.004. Epub 2014 Mar 5. [PubMe]

Fig 100. Leah Reznikov
Ivacaftor increases CFTR channel activity and improves pulmonary function for individuals bearing a G551D mutation. Because ivacaftor structurally resembles quinolone antibiotics, the authors tested the hypothesis that ivacaftor possesses antibacterial properties.Ivacaftor induced a dose-dependent reduction in bioluminescence of S. aureus and decreased the number of colony forming units. They observed a similar but less robust effect in P. aeruginosa following outer membrane permeabilization. Ivacaftor inhibited the growth of respiratory isolates of S. aureus and Streptococcus pneumoniae and exhibited positive interactions with antibiotics against lab’ and respiratory strains of S. aureus and S. pneumoniae.
– These data indicate that ivacaftor exhibits antibacterial properties and raise the possibility that ivacaftor might have an antibiotic effect in people with CF.
Dr Leah Reznikov (fig 100) is Assistant Professor in the Department of Physiological Sciences, University of Florida.
Rodriguez-Miguelez P, Thomas J, Seigler N, Crandall R, McKie KT, Forseen C, Harris RA. Evidence of microvascular dysfunction in patients with cystic fibrosis. Am J Physiol Heart Circ Physiol. 2016 Jun 1;310(11):H1479-85. doi: 10.1152/ajpheart.00136.2016. Epub 2016 Apr 15. [PubMed]

Fig 102. Ryan Harris

Fig 101. Paula Rodriguez-Miguelez
Recent findings have described impairment in conduit vessel function in patients with CF; however, whether microvascular function is affected in this population has yet to be elucidated. Using laser-Doppler imaging, the authors evaluated microvascular function through post occlusive reactive hyperaemia (PORH), local thermal hyperaemia (LTH), and iontophoresis with acetylcholine (ACh). PORH [518 ± 174% (CF) and 801 ± 125% (control), P = 0.039], LTH [1,338 ± 436% (CF) and 1,574 ± 620% (control), P = 0.045], and iontophoresis with ACh [416 ± 140% (CF) and 617 ± 143% (control), P = 0.032] were significantly lower in patients with CF than control subjects.
In addition, the ratio of PORH to LTH was significantly (P = 0.043) lower in patients with CF (55.3 ± 5.1%) than control subjects (68.8 ± 3.1%). Significant positive correlations between LTH and forced expiratory volume in 1 s (%predicted) (r = 0.441, P = 0.013) and between the PORH-to-LTH ratio and exercise capacity (r = 0.350, P = 0.049) were observed.
— These data provide evidence of microvascular dysfunction in patients with CF compared with control subjects. In addition, the data demonstrate a complex relationship between microvascular function and classical markers of disease severity (i.e., pulmonary function and exercise capacity) in CF.
Dr Paula Rodriguez-Miguelez (fig. 101) is Postdoctoral Fellow, Georgia Prevention Institute, Augusta University
Dr Ryan Harris (fig. 102) is Director, Laboratory of Integrative Vascular and Exercise Physiology and Associate Professor, Pediatrics, Physiology and Graduate Studies
Rowe SM, McColley SA, Rietschel E, Li X, Bell SC, Konstan MW, Marigowda G, Waltz D, Boyle MP; VX09‐809‐102 Study Group.Lumacaftor/Ivacaftor Treatment of Patients with Cystic Fibrosis Heterozygous for F508del-CFTR. Ann Am Thorac Soc. 2016 Nov 29. [Epub ahead of print] [PubMed]
Fig. 103 Steven M. Rowe the.asci.org
Lumacaftor/ivacaftor treatment (≤28 days) in patients with cystic fibrosis (CF) heterozygous for F508del-CFTR did not improve lung function. This study was to evaluate an optimised lumacaftor/ivacaftor dosing regimen with longer duration in a cohort of patients heterozygous for F508del-CFTR.
Patients age ≥18 years with a confirmed CF diagnosis and percent predicted forced expiratory volume in 1 second (ppFEV1) of 40 to 90 were randomised to lumacaftor/ivacaftor (400 mg/250 mg every 12 hours) or placebo daily for 56 days. Primary outcomes were change in ppFEV1 at day 56 and safety. Other disease markers were evaluated.Of 126 patients; 119 (94.4%) completed the study. Lumacaftor/ivacaftor was well tolerated, although chest tightness and dyspnea occurred more frequently with active treatment than with placebo (27.4% vs 14.3% and 14.5% vs 6.3%, respectively). Mean (SD) ppFEV1 at baseline was 62.9 (14.3) [active treatment] and 60.1 (14.0) [placebo]. Absolute change in ppFEV1 (least squares mean [SE]) at day 56 was -0.6 (0.8) [active treatment] and -1.2 (0.8) percentage points [placebo] (P = 0.60). CF respiratory symptom scores improved by a mean of 5.7 points versus a decrease of -0.8 for placebo (P < 0.01). No changes in body mass index (BMI) occurred. Change from baseline in sweat chloride (least squares mean [SE]) at day 56 was -11.8 (1.3) mmol/L [active treatment] and -0.8 (1.2) mmol/L [placebo] (P < 0.0001).
The authors concluded sweat chloride and respiratory symptom scores improved with lumacaftor/ivacaftor, though no meaningful benefit was seen in ppFEV1 and BMI in patients heterozygous for F508del-CFTR.
— This is a modest effect for patients heterozygous for F508del which would be unlikely to result in the treatment being recommended for patients heterozygous for F508del – certainly in the UK where the combination therapy is not even approved by NICE for patients homozygous for F508del.
Steven M Row (fig 103) is a pulmonologist and scientist in the Division of Pulmonary, Allergy & Critical Care Medicine, University of Alabama at Birmingham, Birmingham, Alabama.
Samson C; Tamalet A; Thien HV; Taytard J; Perisson C; Nathan N; Clement A; Boelle PY; Corvol H. Long-term effects of azithromycin in patients with cystic fibrosis. Resp Med 2016;117:1-6. [PubMed]
The aim of this retrospective study was to investigate the effects of low-dose azithromycin treatment on the progression of CF lung disease in patients treated for more than 12 months. All of the CF patients followed in a pediatric center and who had been on low-dose azithromycin for more than 12 sequential months were included. The clinical data were collected for one year before and three years after the initiation of the azithromycin treatment. A total of 68 patients were included (mean age: 9.95 yrs (3.61)).
After 12 months, significant reductions in the numbers of pulmonary exacerbations and antibiotic courses were present. However, this effect was not maintained in the subsequent periods, during which increased rates of both pulmonary exacerbations and antibiotic courses were observed. The lung function decline was not modified during the treatment, and a decreasing time-dependent trend typical of CF was observed for the various parameters. No differences in the airway colonization by pathogens such as Pseudomonas aeruginosa and methicillin-sensitive and/or -resistant Staphylococcus aureus were observed during the treatment. However, isolated Staphylococcus aureus strains became resistant to macrolides after 6 months of azithromycin and remained resistant thereafter.
The authors concluded no clinical benefits of low-doses azithromycin were present after one year of treatment in young CF patients. Selection for macrolide-resistant strains of bacteria occurred, which should lead to a reconsideration of the duration of azithromycin treatment in CF.
— The initial interest in the use of macrolides (erythromycin) in chronic P. aeruginosa infection followed impressive results from Japan in diffuse panbronchiolitis (Kudoh S et al 1998. [PubMed]). The use in CF was approved following a study from USA showing a reduction in exacerbations (Saiman L et al.2003. [PubMed]). Further experience shows the benefits are not sustained and rarely cardiac abnormalities have been described.
The CF Foundation guidelines recommend long term azithromycin for all patients of 6 years and older chronically infected with P. aeruginosa.
In contrast, in the UK the CF Trust Antibiotic Working Group recommends azithromycin only if the patient is “deteriorating on conventional therapy”; the UK group considers there is insufficient evidence to recommend all patients with chronic P. aeruginosa should receive long term azithromycin.[see also Topics->Antibiotics classified-> Macrolides]
Clementine Samson is at Hôpital Trousseau, Pediatric Pulmonology Department, Paris, France; Besançon Hospital, Pediatric Department, Besançon, France.
Safe M; Gifford AJ; Jaffe A; Ooi CY. Resolution of Intestinal Histopathology Changes in Cystic Fibrosis after Treatment with Ivacaftor. Ann Amer Thorac Soc 2016; 13(2): 297-8. [PubMed]

Fig. 105 Mark Safe paediatricgastro.com
A six year old CF patient (Phe508del/p.Gly551Asp) had duodenal biopsies before and after 6 months treatment with ivacaftor (fig. 104) demonstrating resolution of changes consistent with CF. before treatment the duodenal biopsies showed inspissated eosinophilic mucin within the crypts. After 6 months treatment with ivacaftor duodenal biopsies showed an absence of the previous changes of CF
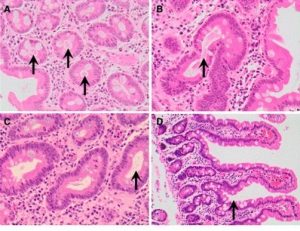
Fig 104. A&B Duodenal biopsies before treatment showing aspirated material in crypts. C Biopsy after treatment cleared material from crypts D Normal duodenal mucosa (from website of the American Thoracic Society)
Mark Safe (fig 105) is a paediatric gastroenterologist and hepatologist at Sydney Children’s Hospital Randwick, Australia.
Sismanlar T; Aslan AT; Kose M; Pekcan S; Ezgu FS; Budakoglu II; Yenicesu I. Early severe anemia as the first sign of cystic fibrosis. Eur J Pediatr 2016; 175(9):1157-63. [PubMed]

Fig. 106 Tugba Şişmanlar avesis.gazi.edu.tr
Severe anaemia as the first sign of CF was noted in 17 of 231 patients. Patient age, prolonged PT/INR and the albumin level differed significantly between the 2 groups of patients (P < 0.001). Feeding pattern, pancreatic insufficiency, vitamin E and A levels, and the types of genetic mutations did not differ between the 2 groups. The mean haemoglobin level was 5.59 +/- 0.21 g/dL and respiratory symptoms began a mean 6.3 months after diagnosis of CF in the anaemia group. In early infancy severe anaemia in the absence of respiratory symptoms can be the first sign of CF. CF should be considered in the differential diagnosis of severe anaemia in infants. Anaemia can occur several months before respiratory symptoms in patients with CF and may be caused due to several reaso
— These anaemic CF infants were not screened in the neonatal period. Extensive investigation showed the anemia was not primarily due to iron deficiency, vitamin E or Vitamin A deficiency. The authors concluded that the most important characteristics of the anemia were hypoalbuminemia suggesting that ineffective erythropoiesis due to general protein energy malnutrition might cause the anemia in these patients. So the complication should not be observed in early-treated screened CF infants.
Tugba Şişmanlar (Fig 106) is associate professor in the Pediatric Pulmonology Department, Gazi University Faculty of Medicine, Besevler, 06500, Ankara, Turkey.
Skolnik K, Levy RD, Wilcox PG, Quon BS. Coronary artery disease in cystic fibrosis: An emerging concern? J Cyst Fibros. 2016 Nov;15(6):e70-e71. doi: 10.1016/j.jcf.2016.09.010. Epub 2016 Oct 14. [PubMed]
Between 1996 and 2016 and 16 patients 40 years and older, 14 (88%) underwent coronary angiography. The coronary angiography reports and “still” diagrams were carefully reviewed for evidence of luminal narrowing or complete obstruction of the coronary vessels consistent with atherosclerosis. Interestingly, no vessels had evidence of narrowing and not a single atherosclerotic plaque was documented in the 14 patients examined. Overall, this data is reassuring as natural history studies have shown that atherosclerotic changes often appear in coronary arteries years and sometimes decades before the onset of clinically significant coronary heart disease.
— Previously it has been suggested the infrequency of coronary artery disease in people with CF is related to the low levels of serum lipids. In an earlier study 20 hearts from people with CF who were receiving heart-lung transplants were used for domino transplants for heart recipients. No coronary artery disease was present in 12 of these recipients who had angiography at 1 year (Jacob M H et al 1990. [PubMed])
Kate Skolnik is in the Department of Medicine, University of Calgary, AB, Canada.
Stonebraker JR, Ooi CY, Pace RG, Corvol H, Knowles MR, Durie PR, Ling SC. Features of Severe Liver Disease With Portal Hypertension in Patients with Cystic Fibrosis. Clin Gastroenterol Hepatol. 2016 Apr 5. pii: S1542-3565(16)30016-7. doi: 10.1016/j.cgh.2016.03.041. [Epub ahead of print] [PubMed]

Fig. 107 Jaclyn Stonebraker med.unc.edu
A retrospective analysis of data from 561 patients with CF (63% male, 99% with pancreatic insufficiency), liver disease. All patients were enrolled in the Genetic Modifier Study of Severe CF Liver Disease at 76 international centers, from January 1999 through July 2013.Male patients were diagnosed with liver disease at a younger age than female patients (10 vs 11 years; P=.01). Splenomegaly was observed in 99% of patients and varices in 71%. Levels of liver enzymes were near normal in most patients. Thrombocytopenia affected 70% of patients and was more severe in patients with varices (88×109/L vs. 145×109/L; P<.0001). Ninety-one patients received liver transplants (16%), at a median age of 13.9 years. Compared to patients who did not receive liver transplants, patients who received liver transplants had lower platelet counts (78×109/L vs 113×100/L; P<.0001), higher international normalized ratios (P<.0001), and lower levels of albumin (P=.0002). The aminotransferase to platelet ratio index (APRI) and fibrosis index based on 4 factor (FIB4) values were above diagnostic thresholds for CF liver disease in 96% and 90% of patients, respectively. Patients who received liver transplants or who had varices had higher APRI and FIB4 values than patients who did not. In patients with CF, severe liver disease develops early in childhood (around 10 years of age) and is more common in boys than girls. Patients with varices and those who receive liver transplants have high platelet counts and APRI and FIB4 scores.
— A large series of patients the findings confirming, in particular, the fact that liver disease tends to develop early in childhood.
Jaclyn Stonebraker (fig.107) is a research associate at the Marsico Lung Institute/Cystic Fibrosis Research Center, School of Medicine, The University of North Carolina at Chapel Hill, Chapel Hill, North Carolina.
Savant AP; McColley SA. Pediatric Pulmonology year in review 2015: Part 4. [Review] Pediatr Pulmonol 2016; 51(7):754-65. [PubMed] In this article, wthe authors highlight cystic fibrosis research published in Pediatric Pulmonology during 2015. Articles from other journals that reflect similar themes, and those of special importance, are also included.
Shen Y; Liu J; Zhong L; Mogayzel PJ Jr; Zeitlin PL; Sosnay PR; Zhao S. Clinical Phenotypes and Genotypic Spectrum of Cystic Fibrosis in Chinese Children. J Pediatr 2016; 171:269-76. [PubMed]
The authors recruited and characterized the phenotypes of 21 Chinese children with CF. All 27 exons and their flanking sequences of the CF transmembrane conductance regulator gene were amplified and sequenced to define the genotypes. RESULTS: Bronchiectasis (95.2%) and sinusitis (76.2%) were the most common clinical presentations among our patients. By contrast, pancreatic insufficiency was rare (14.3%). The predominant organism found in the airways was Pseudomonas aeruginosa (66.7%). There were obvious reductions of forced expiratory volume in the first second (mean +/- SD: 71.8% +/- 17.2% predicted) and forced expiratory flows at 75% of exhaled vital capacity (33.7% +/- 20.4% predicted) in children with CF. Overall, we identified 22 different mutations, including 12 missense, 5 nonsense, 2 frameshift, 1 in-frame insertion, 1 splice site, and 1 3’untranslated region mutation. Of these, 7 were novel observations (W216X[780G->A], 1092insA, Q359X, D567Y, 2623-126T->C, 3439delA and 4575+110C->G), and the most common types were L88X and I556V. One de novo mutation (1092insA) was also revealed. Except for N1303K and R334W, none of them were present in the common Caucasian CF transmembrane conductance regulator mutation-screening panels.There was a 5.7-year delay between the first clinical presentation and the eventual CF diagnosis, suggesting that CF may be under-diagnosed in China. The clinical phenotypes and genotypic spectrum are different from that observed in Caucasians.
– The rarity of CF in China presumably is one factor accounting for the delay in eventual diagnosis.
From Department No. 2 of Respiratory Medicine, Beijing Children’s Hospital Affiliated to Capital Medical University, Beijing, China.
Shoseyov D, Cohen-Cymberknoh M, Wilschanski M. Ataluren for the treatment of cystic fibrosis. Expert Rev Respir Med. 2016 Feb 24:1-5. [Epub ahead of print] [PubMed]

Fig 108. David Shoseyov
Ataluren is orally bioavailable and was shown to be effective in Cystic Fibrosis. Phase I and II studies established the safety and dosing regimens for Ataluren. The results of a short study showed modest improvements in pulmonary function and a reduction in quantitative cough assessment. There was improvement in nasal potential difference and nasal epithelial CFTR protein.
However, in a phase III trial this effect was not observed in patients that were concomitantly treated with tobramycin inhalation. Following these positive findings, a multinational Phase III placebo-controlled efficacy trial is currently underway.
– This paper sums up the present situation regarding the use of ataluren for people with CF and stop mutations.
Dr David Shoseyov (fig.108) is Senior Physician and Advisor on Pediatric Lung Disease, Hadassah Medical Center, Jerusalem and Chair of Israeli Cystic Fibrosis Council’s Medical Advisory Committee
Stafler P, Mei-Zahav M, Wilschanski M, Mussaffi H, Efrati O, Lavie M, Shoseyov D, Cohen-Cymberknoh M, Gur M, Bentur L, Livnat G, Aviram M, Alkrinawi S, Picard E, Prais D, Steuer G, Inbar O, Kerem E, Blau H.The impact of a national population carrier screening program on cystic fibrosis birth rate and age at diagnosis: Implications for newborn screening. J Cyst Fibros. 2016 Jul;15(4):460-6. doi: 10.1016/j.jcf.2015.08.007. Epub 2015 Sep 16. [PubMed]

Fig 109. Patrick Stafler
Population carrier screening (PCS) has been available in Israel since 1999 and universally subsidized since 2008. The authors sought to evaluate its impact using a retrospective review of governmental databanks, the national CF registry and CF centers.CF rate per 100,000 live births has decreased from 14.5 in 1990 to 6 in 2011. From 2004-2011 there were 387 couples carrying two mutations who opted for invasive pre-natal diagnosis. 87 pregnancies annually were terminated. From 2004-2011 there were 95 CF births: 22 utilized PCS; 68 (72%) had 2 known CFTR mutations; 37% were pancreatic sufficient. At diagnosis, age was 6 (0-98) months; 53/95 had respiratory symptoms, 41/95 failure to thrive and 19/95 pseudomonas. Thirty-four (36%) were Arabs and 19 (20%) orthodox Jews, compared to 20% and 8% respectively, in the general population. PCS markedly reduced CF birth rates with a shift towards milder mutations, but was often avoided for cultural reasons. As children with CF regularly have significant disease at diagnosis, the authors suggest a balanced approach, utilizing both PCS and newborn screening.
— So a nationally funded population screening programme, but no neonatal screening programme, resulted in unacceptable late diagnosis for those eventually born with CF (at mean age of 6 months) by which time over half had respiratory disease and 20% were infected with P. aeruginosa.
Patrick Stafler (fig.109) is senior physician in the Pediatric Pulmonology Department of Schneider Children’s Medical Center of Israel.
Stanojevic S, Davis SD, Retsch-Bogart G, Webster H, Davis M, Johnson RC, Jensen R, Pizarro ME, Kane M, Clem CC, Schornick L, Subbarao P, Ratjen FA. Progression of Lung Disease in Preschool Patients with Cystic Fibrosis. Am J Respir Crit Care Med. 2016 Dec 12. [Epub ahead of print] [PubMed]

Fig. 110 Sanja Stanojevic medicine.dal.ca
Implementation of intervention strategies to prevent lung damage in early cystic fibrosis (CF) requires objective outcome measures that capture and track lung disease. A study to define the utility of the Lung Clearance Index (LCI), measured by Multiple Breath Washout (MBW), as a means to track disease progression in preschool children with CF.
CF children between the ages of 2.5 and 6 years with a confirmed diagnosis of CF and age-matched healthy controls were enrolled at three North American CF centres. MBW tests were performed at baseline 1, 3, 6 and 12 months to mimic time points chosen in clinical care and interventional trials; spirometry was also conducted. A generalised linear mixed-effects model was used to distinguish LCI changes associated with normal growth and development (i.e. healthy children) from the progression of CF lung disease.
Data were collected on 156 participants with 800 LCI measurements. While both LCI and spirometry discriminated health from disease, only the LCI identified significant deterioration of lung function in CF over time. The LCI deterioration worsened during cough episodes as well as pulmonary exacerbations, whereas similar symptoms in healthy children were not associated with increased LCI values.
The authors concluded that LCI is a useful marker to track early disease progression and may serve as a tool to guide therapies in young patients with cystic fibrosis.
Sanja Stanojevic (fig. 110) is in the Division of Respiratory Medicine, and Physiology and Experimental Medicine, Research Institute, Hospital for Sick Children, Toronto, Canada.
Stick SM, Kicic A, Ranganathan S. Of Pigs, Mice, and Men: Understanding Early Triggers of Cystic Fibrosis Lung Disease. Am J Respir Crit Care Med. 2016 Oct 1;194(7):784-78. [PubMed]

Fig. 111 Stephen Stick business news.com.au
In this issue of AJRCCM Bartlett and colleagues report that acute inflammatory responses to S, aureus are dysregulated in newborn pigs, suggesting a mechanism for the early neutrophil airway inflammation that leads to progressive structural damage. Although, there were no differences in the markers of inflammation
In CF and non-CF pigs, transcription analysis of tracheal and mixed cellular tissue revealed damped host defence pathways in the CF pig compared with controls – observations that can be replicated in vitro. The authors suggest that these findings support immunoregulatory dysregulation in the epithelium and the possible reasons are discussed.
Stephen M Stick (fig.111) is at the Telethon kids Institute Perth Australia. He is a leading researcher and national leader in various areas of CF research.
Suthoff ED; Bonafede M; Limone B; O’Callaghan L; Sawicki GS; Wagener JS. Healthcare resource utilization associated with ivacaftor use in patients with cystic fibrosis.J Med Econom 2016; 19(9):845-51. [PubMed]
The objective of this analysis was to analyse the impact of ivacaftor on health resource utilisation through analysis of claims data. Ivacaftor therapy was associated with significant reductions in hospitalisations along with high rates of adherence to treatment over 12 months.
From Vertex Pharmaceuticals Incorporated , Boston , MA , USA ;
Tarshish Y, Huang L, Jackson F, Edwards J, Fligor B, Wilkins A, Uluer A, Sawicki G, Kenna M. Risk Factors for Hearing Loss in Patients with Cystic Fibrosis. J Am Acad Audiol. 2016 Jan;27(1):6-12. doi: 10.3766/jaaa.14104. [PubMed]
A retrospective study of audiometric results and medication information in a cohort of patients with CF. Records of 178 CF patients seen at Boston Children’s Hospital for audiometric testing from 2007 to 2010 were reviewed. Mean age of patients was 18 yr (standard deviation = 10 yr), and 98 (55%) of the patients were female. Audiometric results, medications, and hospitalisations were recorded. Multivariable logistic regression was used to evaluate the association between SNHL and the number of hospitalisations and chronic antibiotic use in the year prior to the patients’ audiometry.In this sample, 37/178 (21%) patients had sensori-neuronal hearing loss (SNHL). Twenty-nine (78%) of the 37 patients had bilateral SNHL and 8 (22%) had unilateral SNHL. Across all age groups, the majority of patients had a bilateral hearing loss (HL). A multivariable model showed that older age and more frequent hospitalisations were associated with SNHL. The number of courses of chronic antibiotics in the year prior to audiometric testing was not correlated with rate of HL.The findings suggests that age and frequency of hospitalisations are key predictors of HL development.
The authors suggest that increased awareness and regular screening for SNHL should be included in the routine care of CF patients, particularly those at the highest risk.
Taylor CJ; Thieroff-Ekerdt R; Shiff S; Magnus L; Fleming R; Gommoll C. Comparison of two pancreatic enzyme products for exocrine insufficiency in patients with cystic fibrosis.J Cyst Fibros 2016; 15(5):675-80. [PubMed]

Fig 112. John Dodge and Chris Taylor. Author’s photo
Zenpep (APT-1008) is a pancreatic enzyme product for the treatment of exocrine pancreatic insufficiency (EPI) associated with cystic fibrosis (CF). METHODS: Zenpep and Kreon, both containing 25,000 lipase units, were compared in a randomised, double-blind, crossover, non-inferiority study for CF-associated EPI in patients aged >12years. Patients on a standardised diet and stabilised treatment were randomised to two treatment sequences: Zenpep/Kreon or Kreon/Zenpep. The primary efficacy endpoint was the coefficient of fat absorption over 72h (CFA-72h). 96 patients (mean age 19.2years, 60.4% males) were randomised with 83 completers of both sequences comprising the efficacy population.
Zenpep demonstrated non-inferiority and equivalence to Kreon in fat absorption (LS mean CFA-72h: Zenpep, 84.1% [SE 1.1] vs. Kreon, 85.3% [SE 1.1]; p=0.297). Safety and tolerability were similar.The authors concluded Zenpep is comparable with Kreon in efficacy and safety for the treatment of adolescents and adults with CF-associated EPI
— A formidable study conducted at 34 sites in 7 European countries demonstrating comparability between a new pancreatic enzyme product Zenpep 25000 (APT-1008 to be marketed Enzepi) and the established Kreon 25000. Apparently a distinctive lack of overfill with Zenpep permits more accurate dosing, in particular lessening the likelihood of overdosing.
Professor Chris Taylor (fig. 112) was founder of the Sheffield Paedaitric CF Centre; he and Professor John Dodge (fig.112) are two of the UK’s leading paediatric gastroenterologists and cystic fibrosis experts.
Taylor-Cousar J, Niknian M, Gilmartin G, Pilewski JM; VX11-770-901 investigators. Effect of ivacaftor in patients with advanced cystic fibrosis and a G551D-CFTR mutation: Safety and efficacy in an expanded access program in the United States.J Cyst Fibros. 2016 Jan;15(1):116-22. doi: 10.1016/j.jcf.2015.01.008. Epub 2015 Feb 11 [PubMed]

Fig. 113 Jennifer Taylor-Cousar som.cuanschultz.edu
Patients with severe lung disease were excluded from the randomised Phase 3 trials. This open-label study was designed to provide ivacaftor to patients in critical medical need prior to commercial product availability. CF patients aged ≥6years with a G551D-CFTR mutation and FEV1≤40% predicted or listed for lung transplant received ivacaftor 150mg every 12h. The primary endpoint was safety as determined by adverse events. Secondary endpoints included assessment of lung function and weight. The rate of serious adverse events was consistent with disease severity.
At 24 weeks of treatment with ivacaftor, there was a mean absolute increase in percent predicted FEV1 of 5.5 percentage points and a 3.3kg mean absolute increase in weight from baseline.
– The authors concluded that in patients with severe lung disease, ivacaftor was well tolerated and was associated with improved lung function and weight gain. This appears to be the experience of others.
Jennifer Taylor-Cousar (fig. 113) is Professor of Medicine-Pulmonary Sciences & Critical Care at National Jewish Health, Denver, CO, United States
Taylor-Cousar JL, Janssen JS, Wilson A, Clair CG, Pickard KM, Jones MC, Brayshaw SJ, Chacon CS, Barboa CM, Sontag MK4, Accurso FJ, Nichols DP, Saavedra MT, Nick JA. Glucose >200 mg/dL during Continuous Glucose Monitoring Identifies Adult Patients at Risk for Development of Cystic Fibrosis Related Diabetes J Diabetes Res. 2016;2016:1527932. doi: 10.1155/2016/1527932. Epub 2016 Nov 24. [PubMed]
Guidelines suggest that screening for CFRD be performed annually using the 2-hour 75-gram oral glucose tolerance test (OGTT). Adherence to recommended screening has been poor, with only approximately one-quarter of adults with CF undergoing OGTT in 2014. Use of continuous glucose monitoring (CGM) for diagnosis may become an alternative. The authors objective was to determine whether abnormal CGM predicts subsequent development of CFRD, lung function, and body mass index (BMI) decline and increased rate of CF pulmonary exacerbations in adults with CF.
In a prospective single center pilot trial from September 2009 to September 2010, 21 adult patients due for routine OGTT were recruited to complete simultaneous 3-day CGM and 2-hour 75 gram OGTT. Subsequently, clinical information was reviewed from 2008 to 2015.
There was a moderate correlation between interpreted results of 2-hour OGTT and CGM (p = 0.03); CGM indicated a greater level of glucose impairment than OGTT. Glucose >200 mg/dL by CGM predicted development of CFRD (p = 0.0002).
Jennifer L Taylor-Cousar (fig. 113) is a paediatric and adult pulmonologist at National Jewish Health.
Tepper LA; Caudri D; Rovira AP; Tiddens HA; de Bruijne M. The development of bronchiectasis on chest computed tomography in children with cystic fibrosis: can pre-stages be identified?. Eur Radiol 2016 Apr 23. [PubMed]

Fig 114. Leonie Tepper
Bronchiectasis is an important component of cystic fibrosis (CF) lung disease but little is known about its development. We aimed to study the development of bronchiectasis and identify determinants for rapid progression of bronchiectasis on chest CT. Forty-three patients with CF with at least four consecutive biennial volumetric CTs were included. Areas with bronchiectasis on the most recent CT were marked as regions of interest (ROIs). These ROIs were generated on all preceding CTs using deformable image registration. Observers indicated whether: bronchiectasis, mucus plugging, airway wall thickening, atelectasis/consolidation or normal airways were present in the ROIs.
They identified 362 ROIs on the most recent CT. In 187 (51.7 %) ROIs bronchiectasis was present on all preceding CTs, while 175 ROIs showed development of bronchiectasis. In 139/175 (79.4 %) no pre-stages of bronchiectasis were identified. In 36/175 (20.6 %) bronchiectatic airways the following pre-stages were identified: mucus plugging (17.7 %), airway wall thickening (1.7 %) or atelectasis/consolidation (1.1 %). Pancreatic insufficiency was more prevalent in the rapid progressors compared to the slow progressors (p=0.05).
Most bronchiectatic airways developed within 2 years without visible pre-stages, underlining the treacherous nature of CF lung disease. Mucus plugging was the most frequent pre-stage.In conclusion the authors observed the development of bronchiectasis in cystic fibrosis lung disease on CT. Most bronchiectatic airways developed within 2 years without pre-stages. The most frequently identified pre-stage was mucus plugging. They emphasise their study underlines the treacherous nature of CF lung disease.
– With the widespread introduction of neonatal CF screening increasing attention has been given to the recognition and treatment of early lung infection and damage. This study indicates the difficulty in identifying early damage from infection. Possibly combining clinical symptoms, bacteriological, biochemical and hematological data would perhaps improve recognition. For example the value of a persisting, even if mild, new cough is a valuable sign of unwelcome activity in the lower airways and should be treated aggressively!
Dr. Leonie Tepper (fig.114) is a member of the CF team at Erasmus MC Sophia , Rotterdam.
Thomsen K, Christophersen L, Bjarnsholt T, Jensen PØ, Moser C, Høiby N. Anti-Pseudomonas aeruginosa IgY antibodies augment bacterial clearanc`e in a murine pneumonia model. J Cyst Fibros. 2016 Mar;15(2):171-8. doi: 10.1016/j.jcf.2015.08.002. Epub 2015 Aug 21. [PubMed]
Oral prophylactic therapy by gargling with pathogen-specific egg yolk immunoglobulins (IgY) may reduce the initial airway colonization with Pseudomonas aeruginosa in cystic fibrosis (CF) patients. IgY antibodies impart passive immunisation and the authors investigated the effects of anti-P. aeruginosa IgY antibodies on bacterial eradication in a murine pneumonia model. P. aeruginosa pneumonia was established in Balb/c mice and the effects of prophylactic IgY administration on lung bacteriology, clinical parameters and subsequent inflammation were compared to controls.
Prophylactic administration of IgY antibodies targeting P. aeruginosa significantly reduced the bacterial burden by 2-log 24h post-infection compared to controls and was accompanied by significantly reduced clinical symptom scores and successive inflammatory cytokine profile indicative of diminished lung inflammation.Passive immunization by anti-P. aeruginosa IgY therapy facilitates promptly bacterial clearance and moderates inflammation in P. aeruginosa lung infection and may serve as an adjunct to antibiotics in reducing early colonization
— The results of a European trial of IgY therapy in people with CF which started in 2012 was eventually available and the result was clearly negative showing the IgY treatment to be of no value in preventing Pseudomonas colonisation.=. Very sad after twenty years work.
Tian X; Liu Y; Yang J; Wang H; Liu T; Xu W; Li X; Zhu Y; Xu KF; Zhang X. p.G970D is the most frequent CFTR mutation in Chinese patients with cystic fibrosis. Human Genome Variation. 3:15063, 2016. [PubMed]
The authors previously identified CFTR mutations in 20 Chinese patients with CF. In this study, eight Chinese patients with a clinical diagnosis of suspected CF were newly collected and screened for CFTR mutations using a combination of conventional Sanger sequencing and multiplex ligation-dependent probe amplification (MLPA) analysis. The CFTR mutations observed in Chinese CF patients, both reported previously and identified in the present study, were also summarised. In the newly collected patients, they identified 10 different CFTR mutations, including p.F508del, the most common CF-causing mutation in Caucasians, and three novel mutations (p.V1212Afs*15; p.L666* and p.A969A). Most notably, the previously reported p.G970D mutation was found in six patients, making it the most frequent CFTR mutation identified in Chinese CF patients thus far. They detected p.F508del for the first time, identified additional novel CFTR mutations and recorded the most frequent CF-causing mutation in Chinese CF patients.
Xinlin Tain is at Department of Respiratory Medicine, Peking Union Medical College Hospital , Beijing, China.
Turck D; Braegger CP; Colombo C; Declercq D; Morton A; Pancheva R; Robberecht E; Stern M; Strandvik B; Wolfe S; Schneider SM; Wilschanski M. ESPEN-ESPGHAN-ECFS guidelines on nutrition care for infants, children, and adults with cystic fibrosis. Clin Nutr 2016; 35(3):557-77. [Full text from Clinical Nutrition website] [PubMed]

Fig. 115 Dominique Turck emedevents.com
ESPEN, ESPGHAN and ECFS recommended guidelines to cover nutritional management of patients with CF. The guidelines were developed by an international multidisciplinary working group in accordance with officially accepted standards. The GRADE system was used for determining grades of evidence and strength of recommendation. Statements were discussed, submitted to Delphi rounds, reviewed by ESPGHAN and ECFS and accepted in an online survey among ESPEN members.
The Working Group recommends that initiation of nutritional management should begin as early as possible after diagnosis, with subsequent regular follow up and patient/family education. Exclusive breast feeding is recommended but if not possible a regular formula is to be used. Energy intake should be adapted to achieve normal weight and height for age. When indicated, pancreatic enzyme and fat-soluble vitamin treatment should be introduced early and monitored regularly. Pancreatic sufficient patients should have an annual assessment including fecal pancreatic elastase measurement. Sodium supplementation is recommended and a urinary sodium:creatinine ratio should be measured, corresponding to the fractional excretion of sodium. If iron deficiency is suspected, the underlying inflammation should be addressed. Glucose tolerance testing should be introduced at 10 years of age. Bone mineral density examination should be performed from age 8-10 years. Oral nutritional supplements followed by polymeric enteral tube feeding are recommended when growth or nutritional status is impaired. Zinc supplementation may be considered according to the clinical situation. Further studies are required before essential fatty acids, anti-osteoporotic agents, growth hormone, appetite stimulants and probiotics can be recommended.Nutritional care and support should be an integral part of management of CF. Obtaining a normal growth pattern in children and maintaining an adequate nutritional status in adults are major goals of multidisciplinary CF centers.
– An authoritative 30-page document outlining the present recommended nutritional management for people with cystic fibrosis.
Dominique Turck (fig.115) is Professor at Univ. Lille, Inserm U995, LIRIC – Lille Inflammation Research International Center, Division of Gastroenterology, Hepatology and Nutrition, and Cystic Fibrosis Center, Department of Pediatrics, CHU Lille, F-59000 Lille, France.
Tsabari R; Elyashar HI; Cymberknowh MC; Breuer O; Armoni S; Livnat G; Kerem E; Zangen DH. CFTR potentiator therapy ameliorates impaired insulin secretion in CF patients with a gating mutation. J Cyst Fibros 2016; 15(3):e25-7. [PubMed]
To investigate the effect of treatment with ivacaftor on insulin secretion in patients with cystic fibrosis (CF) (DELTAF508\S549R) having CFRD/impaired insulin secretion. A standard OGTT was performed before and after 16weeks of treatment with ivacaftor in 2 sibling patients with CF carrying the S549R gating mutation. The area under the curve (AUC) for glucose and insulin was calculated using the trapezoidal estimation.Before treatment, the OGTT of case 1 showed indeterminate glycemia; the OGTT of case 2 indicated CFRD. After ivacaftor treatment the OGTT demonstrated improved insulin secretion pattern mainly by increased first phase early insulin secretion, resulting in reduction of the AUC of glucose in both cases.
The authors concluded the treatment with ivacaftor in patients with CF carrying a gating mutation can ameliorate impaired insulin secretion and suggested further studies and larger cohorts are needed to evaluate the impact of ivacaftor.
Reuven Tsabari is at the Division of Pediatric Pulmonology and CF center, Jerusalem 91240, Israel.
Ullrich G; Bobis I; Bewig B. Parenting stress in mothers with cystic fibrosis. Disabil Rehabil 2016; 38(2):174-9. [PubMed]

Fig. 116 Gerald Ullrich
Helios Kliniken Schwerin
In line with the only comparable study, mothers with CF seem to be a remarkably resilient group who mostly cope well with parental stress even in the face of a progressive, chronic disease requiring time-consuming treatment. Today, motherhood is increasingly becoming an option in fertile women with cystic fibrosis. The additional burden of parenting seems to be rewarded by fulfilling essential personal goals. The authors advise CF clinics should routinely address a possible wish for a child and to discuss it, openly.
Gerald Ullrich (fig. 116) is a clinical psychologist at a Private Practice , Schwerin, Germany and the Adult CF Centre, University Hospital Schleswig-Holstein , Kiel , Germany.
Usatin D, Yen EH, McDonald C, Asfour F, Pohl J, Robson J. Differences between WHO AND CDC early growth measurements in the assessment of Cystic Fibrosis clinical outcomes. J Cyst Fibros. 2016 Dec 15. pii: S1569-1993(16)30670-1. doi: 10.1016/j.jcf.2016.12.001. [PubMed]

Fig. 117 Danielle Usatin mydoctor.kaiserpermanente.org
Adulthood CF outcomes based on early weight-for-length (WFL) measurements, using either World Health Organization (WHO) or Centers for Disease Control (CDC) scales, have not been compared. Cystic Fibrosis Foundation registry patients were studied (n=3014). Participants were categorised at age two years as WFL <50th percentile on both WHO and CDC scales, ≥50th percentile on WHO but not CDC, or ≥50th percentile on both. Pulmonary function and overall survival were assessed at age 18years. Results: Stepwise gains in pulmonary function and lung transplant-free survival were noted across the three increasing WFL categories. Children with CF who achieve higher WFL at age two years have improved pulmonary and survival outcomes into adulthood. The authors advise CF providers to continue to utilize current early growth recommendations, with goal WFL ≥50th percentile on CDC growth charts before age two. Data from article -<50th WHO >50th WHO >50th WHO and CDC not CDC and CDCFEV1%86.3 (77.8-89.4) 87(80.9-95.4) 89.7(85-95.4)Transplant-free survival 83.8% 88.7% 92.3%
– An interesting study from the CFF Patient Registry confirming the importance of early progress on later outlook.
Danielle Usatin (fig.117) from the Division of Pediatric Gastroenterology, Hepatology and Nutrition, Department of Pediatrics, Benioff Children’s Hospital, University of California, San Francisco, CA, United States.
van Koningsbruggen-Rietschel S, Heuer HE, Merkel N, Posselt HG, Staab D, Sieder C, Ziegler J, Krippner F, Rietschel E. Pharmacokinetics and safety of an 8 week continuous treatment with once-daily versus twice-daily inhalation of tobramycin in cystic fibrosis patients J Antimicrob Chemother. 2016 Mar;71(3):711-7. doi: 10.1093/jac/dkv399. Epub 2015 Nov 30. [PubMed]

Fig. 118 Silke van Koningsbruggen Researchgate
The authors evaluated the pharmacokinetics, safety and tolerability of two different continuous treatment regimens of tobramycin inhalation solution (TIS) in 29 cystic fibrosis (CF) patients chronically infected with Pseudomonas aeruginosa.In this randomised, multicentre, open-label, two-period crossover study, TIS (300 mg/5 mL) was administered via PARI eFlow(®) rapid once daily and twice daily each for 8 weeks.
For once-daily treatment, tobramycin levels were 10% higher after 8 weeks compared with 4 weeks (AUC0-90min ratio = 1.096, 90% CI = 0.860-1.396, P = 0.5237). For twice-daily treatment, tobramycin levels after 8 weeks showed a 40% decrease compared with 4 weeks (AUC0-90min ratio = 0.608, 90% CI = 0.461-0.802, P = 0.0055). The AUC0-90min ratio at 8 weeks (once daily versus twice daily) did not differ significantly (AUC0-90min ratio = 0.749, 90% CI = 0.514-1.092, P = 0.2009). The mean FEV1 did not differ markedly compared between treatment periods or with baseline. No audiological or nephrotoxic side effects were noted.
The authors concluded continuous treatment with TIS (once daily or twice daily) over 8 weeks appears to be safe and tolerable.
Silke van Koningsbruggen-Rietschel (Fig.118) is at the CF Center, Children’s Hospital, Faculty of Medicine, University of Cologne, Cologne, Germany
Navarro S. Historical compilation of cystic fibrosis].Gastroenterol Hepatol. 2016 Jan;39(1):36-42. doi: 10.1016/j.gastrohep.2015.04.012. Epub 2015 Jun 10.(Spanish) [PubMed]
Cystic fibrosis is the most common life-shortening recessively inherited disorder in the Caucasian population. The genetic mutation that most frequently provokes cystic fibrosis (ΔF508) appeared at least 53,000years ago. For many centuries, the disease was thought to be related to witchcraft and the “evil eye” and it was only in 1938 that Dorothy H. Andersen characterized this disorder and suspected its genetic origin. The present article reviews the pathological discoveries and diagnostic and therapeutic advances made in the last 75 years. The review ends with some considerations for the future.
— A short interesting review of CF history written in Spanish. The author kindly provided me with an English translation. In the published version Figure 4 is Karl Landsteiner not Sydney Farber and the author has arranged an erratum.
Salvador Navarro is Consultor sénior jubilado, Servicio de Gastroenterología, Institut de Malalties Digestives i Metabòliques, Hospital Clínic, Barcelona, España.
VanDevanter DR, Kahle JS, O’Sullivan AK, Sikirica S, Hodgkins PS. Cystic fibrosis in young children: A review of disease manifestation, progression, and response to early treatment. J Cyst Fibros. 2016 Mar;15(2):147-57. Free full text [PubMed]

Fig 119 Donald (Dutch) VanDevanter ResearchGate
The authors observe that studies have described illness associated with cystic fibrosis (CF) early in life, but there is no comprehensive accounting of the prevalence and ages of disease manifestation and progression described in individual studies. They searched for peer-reviewed English-language studies of the health of children ≤6years old with CF (published 1990-2014). Structural abnormalities and dysfunction of the digestive and respiratory systems were summarized across relevant studies by system and age group. Primary studies (125 total) from 22 countries described abnormalities, dysfunction, and disease progression in infancy and early childhood. Improved health was consistently observed in association with diagnosis via newborn screening compared with cohorts diagnosed later by symptomatic presentation.
In conclusion, they found the peer-reviewed literature to be remarkably consistent regarding all three of the three initial research questions they posed.
(1) At what ages have CF-related dysfunction and structural differences been demonstrated in young children with CF (≤ 6 years of age)? CF-associated growth impairment and airway abnormalities are reported at birth and the underlying pathology of CF directly related to reduced CFTR protein function was demonstrated in young children with CF. Abnormalities and dysfunction of the digestive and respiratory systems were reported throughout early childhood in CF.
(2) At what ages has disease progression been reported in young children with CF? Disease progression is reported in infancy and throughout childhood. The youngest age at which disease progression was reported was by the age of 6 months in both digestive (pancreatic sufficiency decline) and respiratory systems (lung function decline). Accumulation of lung damage was reported by 1 year of age, and lung structure and function worsened significantly each year of life in young children, with potentially irreversible lung damage reported by the age of 2 years.
(3) At what ages are there improved outcomes with early versus late treatment initiation in young children with CF? Earlier access to routine CF management improved subsequent health status. Earlier diagnosis (by 4–14 months) and standard-of-care treatment initiation in infancy compared with later diagnosis and subsequent treatment initiation improved long-term outcomes, including survival.
Dr Donald (Dutch) VanDevanter (Fig. 119) is an Adjunct Professor of Pediatrics, Case Western Reserve University School of Medicine, Cleveland.
— This is a valuable extensive review (143 references) of a very important topic which is attracting increasing interest as it is appreciated that damage from abnormal CFTR function occurs very early – even in utero – and is usually irreversible. It is of particular interest as more effective modulators become available for use in young children.
van der Feen C; van der Doef HP; van der Ent CK; Houwen RH. Ursodeoxycholic acid treatment is associated with improvement of liver stiffness in cystic fibrosis patients. J Cyst Fibros 2016 Jul 29. pii: S1569-1993(16)30566-5. doi: 10.1016/j.jcf.2016.07.009. [PubMed]

Fig. 120 Cathelijine van der Freen Jeroen Bosch Ziekenhuis
Ursodeoxycholic acid (UDCA) might prevent progression of cystic fibrosis liver disease, but objective parameters for its effect are lacking. The authors used liver stiffness measurements to evaluate the effect of ursodeoxycholic acid. Paired measurements of liver stiffness were done in 73 patients without UDCA and in 32 patients with UDCA. In the latter group, 6 patients had cirrhosis; in 15 patients, UDCA was started based on Colombo criteria, and in 11 patients for other reasons. In patients without UDCA, liver stiffness increased: 0.19 (-0.03 to 0.59) kPa/year. Liver stiffness also increased in patients with cirrhosis: 4.6 (0.67-12.4)kPa/year. In patients who had UDCA based on Colombo criteria, a decrease of liver stiffness was observed: 0.70 (-1.6 to 0.55)kPa/year (P=0.01). In patients on UDCA for other reasons, liver stiffness increased: 0.23 (-0.20 to 0.51)kPa/year.
The authors concluded UDCA reduced liver stiffness in patients with well-defined, mild liver disease.They noted that these data were the first objective evidence of the beneficial effect if UDCA therapy in this group of patients with mild liver involvement. They suggest that UDCA started before severe liver damage is present, might be able to prevent progression of CF related liver disease and may even induce a reversal of fibrosis
[*Carla Colombo’s criteria for URSO treatment in CF – At least two of the following criteria – hepatomegaly confirmed by ultrasound, other U/S abnormalities of liver parenchyma and persistently increased liver enzymes (ASAT, ALAT, GGT) – being abnormal for at least 12 months].
Dr Catherine van der Feen (fig.120) is a paediatrician at Jeroen Bosch Ziekenhuis in the Netherlands.
van der Haak N; Boase J; Davidson G; Butler R; Miller M; Kaambwa B; Kritas S. Preliminary report of the (13)C-mixed triglyceride breath test to assess timing of pancreatic enzyme replacement therapy in children with cystic fibrosis. J Cyst Fibros 2016; 15(5):669-74. [PubMed]

Fig.121 Natalie van der Haak
Researchgate
Despite guidelines suggesting pancreatic enzyme replacement therapy (PERT) should be taken before or during a meal, it is currently unknown whether this has benefits over administration after a meal in individuals with cystic fibrosis. 18 children with pancreatic insufficient CF were randomised to two (13)C-mixed triglyceride ((13)C-MTG) breath tests to assess lipase activity with PERT administered 10min before and 10min after a meal. Results were expressed as percentage cumulative dose recovered (PCDR) of (13)CO2 and were compared with established values in healthy subjects. Gastric half emptying time (T1/2) was also assessed by a (13)C-octanoate breath test.
There was no difference in mean PCDR of (13)CO2 between taking PERT before versus after the meal (p=0.68). Eleven subjects had a greater PCDR when PERT was taken before and 7 when PERT was taken after the meal. 6/8 subjects (75%) with a lower than normal PCDR at one time point normalised PCDR when PERT timing was changed.
The authors concluded that changing PERT timing can result in normalized lipase activity. Gastric emptying rate may influence optimal timing of PERT.
— This study from Adelaide carries a useful message that consideration should be given to changing the timing of PERT administration in patients with persisting symptoms of fat malabsorption despite a reasonable dose of enzymes. The great inter-patient variability in malabsorption characteristics is shown. Undoubtedly, trial and error is still required for some patients to achieve optimal absorption. In this context it is worth emphasising that symptoms do not always correlate with the coefficient of fat absorption, which, unfortunately, is so rarely checked even by simple methods.
Natalie van der Haak (fig.121) is Senior Dietitian in the Department of Nutrition, Women’s and Children’s Hospital, North Adelaide, South Australia, Australia; Adjunct Associate Lecturer Finders University Adelaide.
Van Iterson EH, Wheatley CM, Baker SE, Morgan WJ, Snyder EM. The relationship between cardiac haemodynamics and exercise tolerance in cystic fibrosis. Heart Lung 2016 (May-Jun);45(3):283-90. doi: 10.1016/j.hrtlng.2016.03.001. Epub 2016 Apr 1.[PubMed]

Fig. 122 Erik Van Iterson my.clevelandclinic.org
Individuals with cystic fibrosis (CF) have reduced pulmonary function and exercise tolerance. Additionally, these individuals may develop abnormal cardiac function. The implications of abnormal cardiac function on exercise tolerance are unclear in CF. Aim was to study relationships between exercise, cardiac haemodynamics and exercise tolerance in CF. 17 CF and 25 controls participated in cardiopulmonary exercise testing to measure exercise duration and peak workload (PW). Cardiac index (QI) was measured using acetylene rebreathe and oxygen uptake (VO2) breath-by-breath. Forced expiratory volume in 1-second (FEV1) was performed at rest. Peak QI was 6.7 ± 0.5 vs. 9.1 ± 0.3 mL/min/m(2), CF vs. controls, respectively (P < 0.05). Linear regressions between QI (R(2) = 0.63 and 0.51) and exercise duration or PW were stronger than VO2 (R(2) = 0.35 and 0.37) or FEV1 (R(2) = 0.34 and 0.36) in CF, respectively (P < 0.05).
These data are clinically relevant suggesting attenuated cardiac function in addition to low airway function relate to exercise tolerance in CF.
— In the Sixties, when more children with CF were surviving childhood with chronic respiratory problems, there was increasing interest in secondary cardiac problems including pulmonary hypertension. Interest seems to be now to be focusing on other areas such as the nervous system and cardiovascular system. It is interesting that in the early days of transplantation in the Eighties, the so-called domino procedure used the heart of the CF recipient of a heart-lung transplant for a heart transplant for a non-CF recipient. The use of domino hearts donated by CF recipients of heart-lung transplants is beneficial and is associated with an excellent early and longer-term outcome (Smith JA et al. Eur J Cardiothorac Surg 1996; 10(8):628-33 [PubMed]).
Erik H Van Iterson (fig.122) is Director, Cardiac Rehabilitation; and Quality Director, Metabolic Exercise Stress TestingDepartment of Cardiovascular Diseases, Mayo Clinic, Rochester and the School of Kinesiology, University of Minnesota, Cooke Hall, 1900 University Ave. SE. Minneapolis, MN 55455, USA.
Vears DF, Delany C, Massie J, Gillam L. Parents’ experiences with requesting carrier testing for their unaffected children. Genet Med. 2016 Mar 24. doi: 10.1038/gim.2016.24. [Epub ahead of print] [PubMed]

Fig. 123 Danya Vears
Loop(Frontiers)
International guidelines generally recommend delaying genetic carrier testing in children until the child reaches the age of majority or is mature enough to be involved in the decision. Several studies have shown that carrier testing of children does occur in some instances, particularly in siblings of a child affected with a genetic condition. However, little research has explored parents’ experiences with the testing process, the impact of knowing a child’s carrier status, and whether parents communicate carrier information to their children.Semi-structured interviews were conducted with 33 parents of children who had one of three genetic conditions (cystic fibrosis, haemophilia, and Duchenne muscular dystrophy). Inductive content analysis was used to analyse the data.Eight distinct pathways to carrier testing were distinguishable. While some parents had requested testing, others had been offered testing and some had received carrier results incidentally following testing to exclude affected status. Some parents were discouraged from testing, which led to frustration.
Overall, 67% of the parents had received carrier results for at least one child, and parents were happy to have results, even if their children were carriers. Despite recommendations against carrier testing, this study provides evidence of varying practices and highlights a need to review the guidelines.
— This reviewer disagrees with the advice against carrier testing in the case of CF. In the case of a newborn identified by neonatal screening, and of course with the parents’ permission, the siblings and blood relatives of child bearing age should be offered a check for mutations as part of cascade screening; the parents and siblings should be informed of the results. Unfortunately, this search for carriers still occurs in less than half the instances when a newborn is identified as having CF by screening; there is a definite lack of enthusiasm on the part of relatives
Danya F Vears (fig.123) is a postdoctoral senior researcher at the Centre for Health Equity, Melbourne School of Population and Global Health, University of Melbourne, Parkville, Australia; Department of Public Health and Primary Care, Center for Biomedical Ethics and Law, KU Leuven, Leuven, Belgium; Murdoch Childrens Research Institute, Parkville, Australia.
Vears DF; Delany C; Massie J; Gillam L Why Do Parents Want to Know their Child’s Carrier Status? A Qualitative Study. J Genet Counsel 2016 May 19. [PubMed]
To address this question, semi-structured interviews were conducted with parents of 32 children with cystic fibrosis, haemophilia, and Duchenne muscular dystrophy who wanted to know the carrier status of their other children. Data was analysed using inductive content analysis. Parents expressed a range of reasons for desiring their child’s carrier status, which fell into two broad categories: 1) benefit for the parents and 2) perceived benefit to the child. Parents discussed the desire for certainty and peace of mind derived from having knowledge of their child’s status.
The most commonly expressed reason for wanting to know their child’s carrier status was in order to communicate the information to their child to provide them with the ability to make informed reproductive decisions.These reasons suggest parents are seeking their children’s carrier information both as a coping strategy and to communicate carrier information as part of their role as a parent. This has important implications for genetic counseling practice, especially as international guidelines generally recommend against carrier testing in children.
— As cascade screening of CF relatives still has only some 50% take up in the most recent reports, it is sensible to identify carriers at an early stage. In conditions such as CF identification of carrier couples can avoid the birth of a CF infant by use of preimplantation genetic diagnosis. The study seems to indicate that parents would not agree with the present “international guidelines”.
Veit G, Avramescu RG, Chiang AN, Houck SA, Cai Z, Peters KW, Hong JS, Pollard HB, Guggino WB, Balch WE, Skach WR, Cutting GR, Frizzell RA, Sheppard DN, Cyr DM, Sorscher EJ, Brodsky JL, Lukacs GL. From CFTR biology toward combinatorial pharmacotherapy: expanded classification of cystic fibrosis mutations. Mol Biol Cell. 2016 Feb 1;27(3):424-33. doi: 10.1091/mbc.E14-04-0935. [PubMed]

Fig 124 Guido Veit
ResearchGate
More than 2000 mutations in the cystic fibrosis transmembrane conductance regulator (CFTR) have been described that confer a range of molecular cell biological and functional phenotypes. Most of these mutations lead to compromised anion conductance at the apical plasma membrane of secretory epithelia and cause cystic fibrosis (CF) with variable disease severity. Based on the molecular phenotypic complexity of CFTR mutants and their susceptibility to pharmacotherapy, it has been recognised that mutations may impose combinatorial defects in CFTR channel biology. This notion led to the conclusion that the combination of pharmacotherapies addressing single defects (e.g., transcription, translation, folding, and/or gating) may show improved clinical benefit over available low-efficacy mono therapies.
Indeed, recent phase 3 clinical trials combining ivacaftor (a gating potentiator) and lumacaftor (a folding corrector) have proven efficacious in CF patients harbouring the most common mutation (deletion of residue F508, ΔF508, or Phe508del).
This drug combination was recently approved by the U.S. Food and Drug Administration for patients homozygous for ΔF508. Emerging studies of the structural, cell biological, and functional defects caused by rare mutations provide a new framework that reveals a mixture of deficiencies in different CFTR alleles. Establishment of a set of combinatorial categories of the previously defined basic defects in CF alleles will aid the design of even more efficacious therapeutic interventions for CF patients.
— This article is distributed by The American Society for Cell Biology under license from the author(s). Two months after publication it is available to the public under an Attribution–Noncommercial–Share Alike 3.0 Unreported Creative Commons License (http://creativecommons.org/licenses/by-nc-sa/3.0).
— The beneficial effects of the drug combination of Ivacaftor and Lumacaftor although approved by the FDA is less striking than that of Ivacaftor alone on people with G551D mutation.
Guido Veit (fig. 124) is in the Department of Physiology, McGill University, Montréal, QC H3G 1Y6, Canada.
Vermeulen F; Le Camus C; Davies JC; Bilton D; Milenkovic D; De Boeck K. Variability of sweat chloride concentration in subjects with cystic fibrosis and G551D mutations. J Cyst Fibros 2016 Mar 17. [PubMed]

Fig. 125 Francois Vermeulen
UZ Leuven
Sweat chloride concentration, a biomarker of CFTR function, is an appropriate outcome parameter in clinical trials aimed at correcting the basic CF defect. Although there is consensus on a cut-off value to diagnose CF, there is only limited information on the within subject variability of sweat chloride over time. Such information would be useful for sample size calculations in clinical trials. Therefore, the authors retrospectively analyzed repeated sweat chloride values obtained in patients with G551D mutation(s) assigned to placebo in an ivacaftor interventional trial. Sample size calculations showed that the minimal treatment effect on sweat chloride concentration that can be demonstrated for a group of 5 patients is around 15mmol/L, using a cross-over design and combinations of 4 tests for each phase of the trial.
The authors concluded that although the sweat test is considered a robust measure, sweat chloride measurements in patients with CF and a G551D mutation had an inherent biological variability that is higher than commonly considered. They considered further analyses of placebo group data are crucial to learn more about the natural variability of this parameter
Francois Vermeulen (fig.125) is at the Cystic Fibrosis Reference Centre, University Hospital of Leuven, Leuven, Belgium.
Vidya P; Smith L; Beaudoin T; Yau YC; Clark S; Coburn B; Guttman DS; Hwang DM; Waters V. Chronic infection phenotypes of Pseudomonas aeruginosa are associated with failure of eradication in children with cystic fibrosis. Eur J Clin Microbiol 2016; 35(1):67-74. [PubMed]

Fig. 126 Valerie Waters SickKids
In 10-40 % of cases, eradication fails and the reasons for this are poorly understood. The purpose of this study was to determine whether specific microbial characteristics could explain eradication treatment failure. This was a cross-sectional study of CF patients (aged 0-18 years) with incident P. aeruginosa infection from 2011 to 2014 at the Hospital for Sick Children, Toronto, Canada. Phenotypic assays were done on all incident P. aeruginosa isolates, and eradicated and persistent isolates were compared using the Mann-Whitney test or the two-sided Chi-square test. A total of 46 children with CF had 51 incident P. aeruginosa infections.
In 72 % (33/46) of the patients, eradication treatment was successful, while 28 % failed eradication therapy. Persistent isolates were less likely to be motile, with significantly less twitch motility (p=0.001), were more likely to be mucoid (p=0.002), and more likely to have a tobramycin minimum inhibitory concentration (MIC)>128 mug/mL (p=0.02) compared to eradicated isolates. Although biofilm production was similar, there was a trend towards more persistent isolates with deletions in quorum-sensing genes compared with eradicated isolates (p=0.06).
The authors concluded that the initial acquisition of P. aeruginosa with characteristics of chronic infection is associated with failure of eradication treatment.
Valerie Waters (fig. 126), the corresponding author, is Professor of Paediatrics and Staff Physician Division of Infectious Diseases Hospital for Sick Children, Toronto.
Webb AK, Fitzjohn J. Poetry, Music, Writing and Painting; Developing the artistic talents of Adults with Cystic Fibrosis. Paediatr Respir Rev. 2016 Jan;17:39-41. doi: 10.1016/j.prrv.2015.08.007. Epub 2015 Oct 30.[PubMed]
Art is an expressive outlet for the physical limitations and emotional frustrations of

Fig. 127 Prof. Kevin Webb receiving the ECFS Award from Prof. Stuart Elborn, the President (2013)
living with a life limiting condition such cystic fibrosis. In the Manchester Adult Cystic Fibrosis Centre we have facilitated the sharing of the inherent artistic talent of our patients with the support of painters, musicians, potters, creative writers, photographers and textile specialists and our own ward staff in our dedicated 22 bed CF inpatient unit. The programme has provided some splendid works that enliven our ward and, more importantly, continue to inspire our patients as they attempt to overcome the socially limiting consequences of hospital admission.
– An interesting article from Prof. Kevin Webb’s unit in Manchester exemplifying the “whole patient” approach for which they are well known.
Weber HC, Robinson PF, Saxby N, Beggs SA, Els I. Do children with cystic fibrosis receiving outreach care have poorer clinical outcomes than those treated at a specialist cystic fibrosis centre? Aust J Rural Health. 2016 Nov 17. doi: 10.1111/ajr.12334. [Epub ahead of print][PubMed]

Fig. 128 Heinrich Weber
LinkedIn
Although cystic fibrosis (CF) centre care is generally considered ideal, children living in regional Australia receive outreach care supported by the academic CF centres.
This is a retrospective database review of children with CF treated at the Royal Children’s Hospital in Melbourne and its outreach clinics in Albury (Victoria), and Tasmania. The aim was to compare the outcomes of children with CF managed at an academic centre with that of outreach care, using lung function, nutritional status and Pseudomonas aeruginosa colonisation. Three models of care, namely CF centre care, Shared care and predominantly Local care, were compared, based on the level of involvement of CF centre multidisciplinary team. In our analyses, we controlled for potential confounders, such as socio-economic status and the degree of remoteness, to determine its effect on the outcome measures.
RESULTS:
There was no difference in lung function, i.e. forced expiratory volume in 1 s (FEV1 ), the prevalence of Pseudomonas aeruginosa colonisation or nutritional status (body mass index (BMI)) between those receiving CF centre care and various modes of outreach care. Neither socio-economic status, measured by the Socio-Economic Index for Area (SEIFA) for disadvantage, nor distance from an urban centre (Australian Standard for Geographical Classification (ASGC)) were associated with lung function and nutritional outcome measures. There was however an association between increased Pseudomonas aeruginosa colonisation and poorer socio-economic status.
CONCLUSION:
Outcomes in children with CF in regional and remote areas receiving outreach care at the local hospital by an academic CF centre were no different from children receiving CF centre care.
— The discussion as to the merits of CF centre care versus care at outreach clinics at smaller local hospitals continues. A relatively recent study from Wales in the UK showed advantages for those children who had full centre care (Doull & Evans, 2012 [PubMed]). However, as so often occurs, the findings were disputed vigorously by staff at two excellent paediatricians of the outreach Welsh clinics concerned.
In the UK experience of this reviewer, the parents of more severely affected children with complex problems from more distant areas may prefer to seek all their care at the distant major CF centre. This adversely affects the figures at the CF centre and improves those of the local clinic. It would be important to know if this occurred in the present Australian study. Also, the experience of staff at the CF centre dealing with hundreds of patients is essential for a minority of patients. Incidentally it is important to note that all significant advances in the management have occurred at CF centres where the staff see many patients, recognise emerging problems and then set about seeking solutions.
Heinrich C Weber (fig.128) is Associate Professor of Paediatrics at University of Tasmania & Clinical Leader – Paediatrics THO Northwest; Faculty of Health, University of Tasmania, Rural Clinical School, Burnie, Tasmania, Australia.
Walkowiak J, Glapa A, Nowak JK, Bober L, Rohovyk N, Wenska-Chyży E, Sobkowiak P, Lisowska A. Pancreatic Elastase-1 Quick Test for rapid assessment of pancreatic status in cystic fibrosis patients. J Cyst Fibros. 2016 Jun 7. pii: S1569-1993(16)30511-2. doi: 10.1016/j.jcf.2016.05.009. [Epub ahead of print] [PubMed]

Fig. 129 Jaroslaw Walkowiak
ResearchGate
This prospective study aims at evaluating the sensitivity and specificity of the instant Elastase-1 Quick™ Test by comparing the results with the standard ELISA test.The study involved three groups: the screening-diagnosed cystic fibrosis (CF) patients (n=28), the screened, but non-CF subjects (n=36) and non-screened CF patients (n=62). Pancreatic status (normal vs abnormal) was evaluated using the Pancreas Elastase-1 Quick™ Test. Fecal elastase-1 concentration was determined with a commercially available ELISA kit, used as reference. The cut-off for abnormal results was set at <200μg/g of stool.
The Pancreatic Elastase-1 Quick Test™ showed the following sensitivities and specificities in the studied groups: 92.8% and 96.6% in all subjects, 90.5% and 100% in screening samples, and 92.8 and 90.5% in CF patients.The authors concluded Pancreatic Elastase-1 Quick Test™ proves to be a rapid and reliable option to qualitatively evaluate pancreatic function for diagnostic purposes in a clinical setting of CF care.
– Pancreatic elastase has proved to be an excellent non-invasive test of pancreatic function, particularly useful, as the result is valid without stopping exogenous pancreatin. This new test now permits the result to be immediately available.
Jaroslaw Walkowiak (fig.129) is Professor in the Department of Pediatric Gastroenterology and Metabolic Diseases, Poznan University of Medical Sciences, Poznan, Poland.
Wielputz MO; Eichinger M; Biederer J; Wege S; Stahl M; Sommerburg O; Mall MA; Kauczor HU; Puderbach M. Imaging of Cystic Fibrosis Lung Disease and Clinical Interpretation.Rofo: Fortschritte auf dem Gebiete der Rontgenstrahlen und der Nuklearmedizin. 188(9):834-45, 2016 Sep. [PubMed]

Fig. 130 Mark O Wielputz loop.frontiersin.org
Chest X-ray (CXR), computed tomography (CT) and magnetic resonance imaging (MRI) are now available as routine modalities, each with individual strengths and drawbacks, which need to be considered when choosing the optimal modality adapted to the clinical situation of the patient. CT stands out with the highest morphological detail and has often been a substitute for CXR for regular severity monitoring at specialized centers. Multidetector CT data can be post-processed with dedicated software for a detailed measurement of airway dimensions and bronchiectasis and potentially a more objective and precise grading of disease severity. However, changing to CT was inseparably accompanied by an increase in radiation exposure of CF patients, a young population with high sensitivity to ionizing radiation and lifetime accumulation of dose. MRI as a cross-sectional imaging modality free of ionizing radiation can depict morphological hallmarks of CF lung disease at lower spatial resolution but excels with comprehensive functional lung imaging, with time-resolved perfusion imaging currently being most valuable.
KEY POINTS:* Hallmarks are bronchiectasis, mucus plugging, air trapping, perfusion abnormalities, and emphysema.* Imaging is more sensitive to disease progression than lung function testing.* CT provides the highest morphological detail but is associated with radiation exposure.* MRI shows comparable sensitivity for morphology but excels with additional functional information.* MRI sensitively depicts reversible abnormalities such as mucus plugging and perfusion abnormalities.
Mark Wielputz (fig.130) is in the Department of Diagnostic and Interventional Radiology, Subdivision of Pulmonary Imaging, University Hospital of Heidelberg, Heidelberg, Germany.
Wong SC; Dobie R; Altowati MA; Werther GA; Farquharson C; Ahmed SF. Growth and the Growth Hormone-Insulin Like Growth Factor 1 Axis in Children With Chronic Inflammation: Current Evidence, Gaps in Knowledge, and Future Directions. [Review] Endocrine Reviews. 37(1):62-110, 2016 Feb. [PubMed]

Fig. 131 S C Wong
ReseaarchGate
Growth failure is frequently encountered in children with chronic inflammatory conditions like juvenile idiopathic arthritis, inflammatory bowel disease, and cystic fibrosis. Delayed puberty and attenuated pubertal growth spurt are often seen during adolescence. The underlying inflammatory state mediated by pro-inflammatory cytokines, prolonged use of glucocorticoid, and suboptimal nutrition contribute to growth failure and pubertal abnormalities. These factors can impair growth by their effects on the GH-IGF axis and also directly at the level of the growth plate via alterations in chondrogenesis and local growth factor signalling. Recent studies on the impact of cytokines and glucocorticoid on the growth plate further advanced our understanding of growth failure in chronic disease and provided a biological rationale of growth promotion. Targeting cytokines using biological therapy may lead to improvement of growth in some of these children, but approximately one-third continue to grow slowly. There is increasing evidence that the use of relatively high-dose recombinant human GH may lead to partial catch-up growth in chronic inflammatory conditions, although long-term follow-up data are currently limited.
In this review, the authors comprehensively review the growth abnormalities in children with juvenile idiopathic arthritis, inflammatory bowel disease, and cystic fibrosis, systemic abnormalities of the GH-IGF axis, and growth plate perturbations. They also systematically reviewed all the current published studies of recombinant human GH in these conditions and discussed the role of recombinant human IGF-1.
— This extensive well-referenced article (477 references!) includes a section on cystic fibrosis with detailed review of the various factors affecting growth. The existing literature of growth in CF suggests that nutritional issues and pulmonary exacerbations are not sufficient to explain the growth abnormalities in these children. There is now sufficient evidence to suggest that poor growth in CF is already seen in the neonatal period and that the CF genotype (ΔF508) plays a contributing role.
Sze Choong Wong (fig. 131) is Senior Clinical Lecturer and is affiliated with the Developmental Endocrinology Research Group (S.C.W., M.A.A., S.F.A.), University of Glasgow, Royal Hospital for Children, Glasgow G51 4TF, United Kingdom.
Woodruff SA; Sontag MK; Accurso FJ; Sokol RJ; Narkewicz MR. Prevalence of elevated liver enzymes in children with cystic fibrosis diagnosed by newborn screen. J Cyst Fibros 2016 Aug 20. [PubMed

Fig 132 Samantha Woodruff childrenscolorado.org
Prevalence and risks for elevated liver enzymes have not been studied systematically in children with CF identified by newborn screening by the team in Denver. 298 CF children had been identified by newborn screen since 1982. AST, ALT and GGT were tested at annual visits. The percent of children with 1 or >2 values of elevated AST, ALT and GGT determined. Relationship of liver enzymes to clinical factors or subsequent liver disease was analyzedAt least one abnormal value for AST (63%), ALT (93%) and ALT >1.5x ULN (52%) occurred by 21years of age. Liver enzyme elevations were not correlated with CFTR mutation, meconium ileus or ethnicity. AST and GGT >1.5x ULN were associated with later advanced liver disease HR (CI) 6.53 (2.02-21.1) and 4.03 (1.15-13.45), respectively.The authors concluded elevated liver enzymes are common during childhood in CF patients identified by newborn screening. Elevated AST and GGT may be markers for risk of advanced liver disease.
— A useful long-term study from Colorado, one of the first areas to introduce newborn CF screening in 1982 where Keith Hammond was the involved biochemist. The opportunity to undertake long-term follow-up, identifying findings that may indicate later significant liver involvement, is helpful. The finding raised AST, GGT would perhaps influence the earlier introduction of treatment with ursodeoxycholic acid?
Samantha A Woodruff (fig 132 ) is in the Department of Pediatrics, Section of Pediatric Gastroenterology, Hepatology and Nutrition and Digestive Health Institute, University of Colorado School of Medicine and Children’s Hospital Colorado, Aurora, CO, United States.
Yadav H; Lim KG. Chronic cough with normal sweat chloride: Phenotypic descriptions of two rare cystic fibrosis genotypes. Resp Med Case Reports 2016; 17:17-9. [PubMed]

Fig. 133 Hemming Yadav
Mayo Clinic
Diagnosis of CF in non-classical mutations remains a clinical challenge. We describe the clinical presentation of two patients with chronic cough found to have normal sweat chlorides. We discuss the subsequent evaluation that lead to the diagnosis of two rare CF mutations. We briefly discuss the use of the expanded 106-panel of CF mutations (homozygous 3849 + 10 kb C > T), and the role of whole CFTR gene sequencing (heterozygous c.2752-26 A > G/5T).
Hemang Yadav is a member of the Pulmonary and Critical Care Medicine Department of the Mayo Clinic
Hemang Yadav (fig.133) is in the Division of Pulmonary and Critical Care Medicine, Mayo Clinic, Rochester, MN, USA.
Yang C; Chilvers M; Montgomery M; Nolan SJ. Dornase alfa for cystic fibrosis. [Review][Update of Cochrane Database Syst Rev. 2010;(3):CD001127; PMID: 20238314]Cochrane Database of Systematic Reviews. 4:CD001127, 2016. [PubMed]

Fig. 134 Connie Yang
its-sct.ca
To determine whether the use of dornase alfa in cystic fibrosis is associated with improved mortality and morbidity compared to placebo or other medications that improve airway clearance, and to identify any adverse events associated with its use.
— Review of the published data on dornase alpha, the first really effective mucolytic for people with CF, confirms it is an excellent drug with a good safety record and undoubtedly one of the major therapeutic advances of the early Nineties (Shak et al, 1990; Fuchs et al, 1994).
Connie Yang (Fig. 134) is a paediatric respirologist in the Department of Pediatrics, Division of Respiratory Medicine, BC Children’s Hospital, 4480 Oak Street, Vancouver, BC, Canada, V6H 3V4.
Yammine S, Singer F, Latzin P. CFTR modulation for young children with cystic fibrosis. Lancet Respir Med. 2016 Feb;4(2):84-5. doi: 10.1016/S2213-2600 (16)00009-6. Epub 2016 Jan 21. No abstract available. [PubMed]

Fig. 135 Sophie Yammine kinderklinik.insel.ch
This is a comment on Davies JC, Cunningham S, Harris WT, et al: Safety, pharmacokinetics, and pharmacodynamics of ivacaftor in patients aged 2–5 years with cystic fibrosis and a . Lancet Respir Med 2016; undefined: In The Lancet Respiratory Medicine ,
Jane C Davies and colleagues reported data on safety and pharmacokinetics from an open-label, single-arm ivacaftor trial in children aged 2–5 years with at least one CFTR gating mutation. They reported a similar safety profile and pharmacokinetics as reported in adults. The most frequently reported adverse events in children were cough in 19 (56%) of 34 patients and vomiting in ten (29%). The drug has a proven efficacy and good plasma concentration, despite the high occurrence of vomiting. This finding raises the question as to whether or not the suggested dose is indeed needed to achieve therapeutic benefit. Particular attention has been paid to the rise in liver enzymes in 15% of the children, which has not been described to such an extent in patients older than 5 years. The role of ursocholic acid remains unclear, but additional monitoring of liver function in preschool children is suggested.
— Comment on the dose and effect on liver function in young children taking Ivacaftor.
Sophie Yammine (fig. 135) is a paediatrician at the University Children’s Hospital Bern, Bern, Switzerland.
Yao R, Goetzinger KR. Genetic Carrier Screening in the Twenty-first Century. Cli Lab Med. 2016 Jun;36(2):277-88. doi: 10.1016/j.cll.2016.01.003. Epub 2016 Mar 5. [PubMed]

Fig. 136 Ruofan Yao Loma Linda University Health
Historically, carrier screening for a small number of autosomal recessive disorders has been offered to targeted populations based on ethnicity and family history. These chosen disorders are associated with severe morbidity or mortality, have a well-established carrier frequency in the targeted population, and have an acceptably high detection rate to make screening efficient. With advancing genetic technology, expanded panels rapidly are being designed and offered to the panethnic general population. This article reviews current recommendations for ethnicity-specific carrier screening for common disorders as well as the limitations and counselling complexities associated with expanded panels.
Selected Key Points in the article relevant to CF — Carrier screening for cystic fibrosis should be offered to all patients in the preconception or prenatal period regardless of ethnicity
Ruofan Yao (fig. 136) is in the Department of Obstetrics, Gynecology and Reproductive Medicine, University of Maryland School of Medicine, 22 S Greene Street, Baltimore, MD 21201, USA.
— American College of Medical Genetics currently supports a carrier screening panel for 9 disorders for persons of Ashkenazi Jewish descent; however, expanded panels are available
Pre and post test genetic counselling, including residual risk estimation should be made available to all couples undergoing carrier screening.
In 1997, the National Institutes of Health (NIH) held a consensus conference to address the complex issues associated with CF carrier screening in a panethnic population. This conference was followed, in 1998, by an additional NIH conference directed at the implementation of this committee’s recommendations. Based on these recommendations, CF carrier screening was to be offered to (1) adults with a positive family history of CF, (2) partners of known CF carriers, (3) couples currently planning a pregnancy, and (4) couples seeking prenatal care (NIH Consensus Development Conference Statement on genetic testing for cystic fibrosis Arch Int Med 1999; 159:1529-39).
In 2001, recommendations were issued from another steering committee composed of representatives from the American College of Medical Genetics (ACMG), the American College of Obstetricians and Gynecologists (ACOG), and the National Human Genome Research Institute. This group recommended narrowing the screening population to non-Jewish white people and Ashkenazi Jews, although testing was still made available to other ethnic groups with informed consent and recognition of limitations of screening (Grody WW et al, Genet Med 2001;3:149-54).
In addition, in 2005, ACOG revised its recommendations to state that it is reasonable to offer CF carrier screening to all patients, with the caveat that screening is most efficacious in the non-Hispanic white and Ashkenazi Jewish populations. This recommendation is based on the fact that it is becoming increasingly difficult to assign an individual to any particular ethnic group. Patients electing carrier screening for CF should undergo both pretest and post test counselling, with particular attention paid to ethnic background, detection rate, and residual risk estimate.- This is a very useful review article of the present position.
The UK seems to be slow to recommend prenatal and antenatal screening. The UK National Screening Committee did not recommend this screening in 2006 and failed to review their decision in 2010 as promised. However, the matter was to be reviewed in 2017.
As far back as 1999 a UK Health Technology Assessment recommended antenatal CF screening should be offered routinely to women and their partners in all maternity units. Also it was observed that pre-conceptional screening would provide more reproductive options and should be made available in the family planning clinic or GP setting for couples without a family history who request the test because a pregnancy is planned. Also screening should be made available in assisted reproduction units for those having ICSI and for sperm donors (Murray J, Cuckle H, Taylor G, Littlewood J, Hewison J. Screening for cystic fibrosis. Health Technol Assess 1999; 3(8))1999. [PubMed] Full article available). This recommendation was rejected on the grounds of expense by the National UK Screening Committee as was the HTA’s recommendation for neonatal CF screening although neonatal screening was eventually approved by the Government in 2001 and eventually implemented countrywide by 2007. Antenatal screening for CF is still not routine in the UK although available for selected high risk couples.
Zampoli M; Pillay K; Carrara H; Zar HJ; Morrow B.Microbiological yield from induced sputum compared to oropharyngeal swab in young children with cystic fibrosis. J Cyst Fibros 2016; 15(5): 605-10. [PubMed]

Fig 138. marco Zampoli

Fig 137. Heather Zar
Standard respiratory sampling in young children with cystic fibrosis (CF) is by oropharyngeal swab (OPS) as they cannot spontaneously expectorate. The authors consider sputum induction (IS) has been poorly investigated in this population. They aimed to compare the bacteriological yield of OPS vs. IS in young children with CF. They confirm sputum induction is feasible, safe and superior to OPS for detecting CF-associated bacteria in young children with CF.
– A little unkind to previous paediatric studies (see paper) but a useful paper from South Africa by people with experience in diagnosing TB and other respiratory infections in young children.
Heather Zar (fig. 137) is Head of Paediatric Pulmonology, Red Cross Children’s Hospital, Capetown.
Marco Zampoli (fig. 138) is a consultant paediatrician in the Red Cross Children’s Hospital, Capetown.
Zeybel GL; Pearson JP; Krishnan A; Bourke SJ; Doe S; Anderson A; Faruqi S; Morice AH; Jones R; McDonnell M; Zeybel M; Dettmar PW; Brodlie M; Ward C. Ivacaftor and symptoms of extra-oesophageal reflux in patients with cystic fibrosis and G551D mutation. J Cyst Fibrosis 2016 Jul 27. [PubMed]

Fig. 139 Gemma Zeybel
LinkedIn
Extra-oesophageal reflux (EOR) may lead to micro aspiration in patients with cystic fibrosis (CF), a probable cause of deteriorating lung function. Successful clinical trials of ivacaftor highlight opportunities to understand EOR in a real world study. METHODS: Data from 12 patients with CF and the G551D mutation prescribed ivacaftor (150mg bd) was collected at baseline, 6, 26 and 52weeks. The changes in symptoms of EOR were assessed by questionnaire (reflux symptom index (RSI) and Hull airway reflux questionnaire (HARQ)).Six patients presented EOR at baseline (RSI >13; median 13; range 2-29) and 5 presented airway reflux (HARQ >13; median 12; range 3 to 33). Treatment with ivacaftor was associated with a significant reduction of EOR symptoms (P<0.04 versus baseline) denoted by the reflux symptom index and Hull airway reflux questionnaire.The authors concluded ivacaftor treatment was beneficial for patients with symptoms of EOR, thought to be a precursor to microaspiration.
Gemma Zeybel (fig. 139) is a specialist dietitian at the Institute for Cell and Molecular Bioscience, Newcastle University, Catherine Cookson Building, Framlington Place, Newcastle Upon Tyne NE2 4HH, United Kingdom.
Zlotogora J, Grotto I, Kaliner E, Gamzu R. The Israeli national population program of genetic carrier screening for reproductive purposes. Genet Med. 2016 Feb;18(2):203-6. doi: 10.1038/gim.2015.55. Epub 2015 Apr 16. pubmed.ncbi.nlm.nih.gov/25880436/
The Israeli population genetic screening program for reproductive purposes, launched in January 2013, includes all known, nationally frequent severe diseases (carrier frequency 1:60 and/or disease frequency 1 in 15,000 live births). The carrier-screening program is free of charge and offers testing for cystic fibrosis, fragile X syndrome, and spinal muscular atrophy for nearly the entire population, according to disease frequency among the different groups within the population.
The authors report the results of the first year of the program.Data on the tests performed over a 12-month period were collected from laboratories nationwide. More than 62,000 individuals were examined. The carrier frequency was within the expected range for most of the diseases. The few exceptions included lower carrier rates for cystic fibrosis among Muslim Arabs (1:236) and Druze (1:1,021) and Niemann-Pick type A among Muslim Arabs in a delineated region of Israel (1:229)
The national population genetic carrier screening is aimed toward providing couples with knowledge of the existing options for the prevention of serious genetic conditions when it is relevant for them. The authors suggest that it is still too early to determine whether this aim has been achieved.
Joel Zlotogora prof. of Human Genetics is affiliated with Department of Community Genetics. Public Health Services. Ministry of Health, Jerusalem, Israel. Hadassah Medical School, Hebrew University, Jerusalem, Israel.
Zhang Z; Lindstrom MJ; Farrell PM; Lai HJ; Wisconsin Cystic Fibrosis Neonatal Screening Group. Pubertal Height Growth and Adult Height in Cystic Fibrosis After Newborn Screening. Pediatrics 2016; 137(5):May. [PubMed]

Fig 140 Zhumin Zhang biostat.wiscwebedu
To examine long-term growth benefit of newborn screening (NBS), adolescent peak height velocity (PHV), and adult height were compared between the screened (diagnosed early via NBS) and the control (identified generally by symptoms) in the Wisconsin Randomized Clinical Trial. Data from 107 children born in 1985-1994 and followed through 2012 were analyzed. PHV was estimated by a semiparametric growth curve model and compared with Tanner reference. RESULTS: Meconium ileus (MI; n = 25) was associated with the worst pubertal growth and adult height, including 1 child who did not experience apparent PHV; children with pancreatic sufficiency (n = 18) achieved the best growth (normal PHV and adult height). In children with pancreatic insufficiency without meconium ileus (n = 64), the subgroup most likely to benefit from NBS, screened children had similar PHV but better adult height compared with controls. Specifically, in boys, the screened group (n = 22) achieved normal PHV (9.5 cm at 13.5 years); the control group (n = 19) had similar onset age (13.6 years) but 0.6-cm lower magnitude (P = .08). In girls, the screened group (n = 10) had somewhat later (12.5 years vs 11.7 years, P = .12) and lower PHV (7.3 cm vs 7.9 cm, P = .33) than the controls (n = 13), coinciding with later menarche (13.6 years vs 12.2 years, P = .10). Adult height was taller in the screened than the control (50th vs 29th percentile, P = .02), even after adjusted for genetic potential (32nd vs15th percentile, P = .006). Differences in adult height were primarily attributable to NBS and better prepubertal growth. CONCLUSIONS: Early linear growth benefits of NBS were sustained through puberty, leading to better adult height in cystic fibrosis.
— The better height achieved in later childhood by the screened CF infants compared to unscreened in an earlier Wisconsin study was one of the main reasons the UK government (Minister of Health –Yvette Cooper) wisely agreed with the UK CF Trust’s intensive campaign for the introduction of national neonatal CF screening in 2001 – against the advice of the National Screening Committee. (Farrell PM et al. Early diagnosis of cystic fibrosis through neonatal screening prevents severe malnutrition and improves long-term growth. Pediatrics 2001; 107:1-13. [PubMed]). See 2001 entry for more details).
Dr Zhumin Zhang,(fig.140) a biostatistician in the Departments of Nutritional Sciences. Biostatistics and Medical Informatics, and Pediatrics, University of Wisconsin-Madison, Madison, Wisconsin Departments of Nutritional Sciences, Biostatistics and Medical Informatics, and Pediatrics, University of Wisconsin-Madison, Madison, Wisconsin the Department of Nutritional Science. Wisconsin Cystic Fibrosis Neonatal Screening Group.
Dr Zhumin Zhang passed away suddenly on November 10th 2022. She was obviously a highly regarded colleague – a valued member of the department.
Zhu B, Padroni M, Colombo G, Phillips G, Crapper J, Young PM, Traini D. The development of a single-use, capsule-free multi-breath tobramycin dry powder inhaler for the treatment of cystic fibrosis. J Pharm. 2016 Apr 5. pii: S0378-5173(16)30284-8. doi: 10.1016/j.ijpharm.2016.04.009. [Epub ahead of print] [PubMed]

Fig.141 Bing Zhu
ResearchGate
The aerosol performance and delivery characteristics of tobramycin for the treatment of respiratory infection were evaluated using the Orbital™, a multi-breath, high dose, dry powder inhaler (DPI). Micronised tobramycin was prepared and tested in the Orbital and in the commercially available TOBI Podhaler (Novartis AG). Furthermore, the TOBI Podhaler formulation containing tobramycin as Pulmospheres was tested in both the commercial Podhaler device (T-326) and Orbital for comparison.The Orbital was shown to be capable of delivering high efficiency, high dose antibiotic therapy for inhalation without the need for the use of multiple capsules as used in current devices.
– This appears to be an improvement on one of the most widely used and effective methods of treatment and is likely to improve adherence, which, understandably, is a major problem.
Bing Zhu (fig. 141) is Assistant Director new project Department, Respiratory Technology, Woolcock Institute of Medical Research, Australia.
Zemanick ET; Ong T; Daines CL; Dellon EP; Muhlebach MS; Esther CR Jr. Highlights from the 2015 North American Cystic Fibrosis Conference. [Review] Pediatr Pulmonol 2016; 51(6):650-7. [PubMed]

Fig. 142 Edith Zemanick childrenscolorado.org
The 29th Annual North American Cystic Fibrosis Conference was held in Phoenix, Arizona on October 8-10, 2015. Abstracts were published in a supplement to Pediatric Pulmonology.(1) In this review, the authors summarise presentations in several of the topic areas addressed at the conference. Their goal was to provide an overview of presentations with relevance to emerging or changing concepts in several areas rather than a comprehensive review. Citations from the conference are by first author and abstract number or symposium number, as designated in the supplement.
Edith Zemmanick (fig. 142) is Associate Director, Pediatric Cystic Fibrosis Center, Children’s Hosptial Colorado; Clinical Research Medical Director, Breathing Institute.