
Seventies – clinical
Seventies
More aggressive comprehensive early treatment in some clinics – “a not so fatal disease” for some
During the Seventies there was a definite change in attitude in a few clinics where the doctors were gaining experience in treating more patients who were surviving for longer. The details and impressive results of LeRoy Matthew’s and Carl Doershuk’s comprehensive treatment programme from 1957 were published in 1964 (Matthews et al, 1964; Doershuk et al, 1964 above) and the methods of management and treatment they used eventually formed the basis of the CF Foundation’s network of CF Centres in the USA from 1961.
Drs Margaret Mearns and Winifred Young (1909-1969) at the Queen Elizabeth Hospital for Children in London published encouraging results

Fig. 2 Winifred Young RCP Museum

Fig. 1. Margaret Mearns. Author’s photo
They’re meticulous clinical and follow-up and treatment reflecting their exceptional care in the Sixties (Mearns, 1972 below). Unfortunately, their expertise did not diffuse into the majority of the general paediatric clinics in the UK where most of the children with CF were still treated. Their results provided further evidence that vigorous, meticulous treatment of the secondary effects of the basic defect at an early stage could significantly improve prognosis. From the 1950s their young patients at the Queen Elizabeth Hospital for Children in Hackney had received prophylactic erythromycin and nebulised neomycin and intensive physiotherapy – before 1957 they had 50 infants who, at a year, were considered to have no significant trouble and who, at 5 years, were still considered to be free of bronchitis (Mearns, 1969 above). These were quite unusual results for the Sixties. Shwachman had also noted that erythromycin was a useful drug – interesting in view of the later work confirming the proven value of macrolides, particularly azithromycin, in chronically infected patients (Saiman et al, 2003 below).
David Lawson recommended early and continuous anti-Staphylococcal antibiotic treatment (Lawson, 1969; Lawson, 1972 below)
Fig.3 David Lawson. CFtrust photo
This seemed logical and was a policy I started in Leeds in 1975 for our screened infants (Evans RT et al, 1981 below) and a treatment we have continued for all patients to the present day. The frequent assertion that treating S. aureus would result in more Pseudomonas aeruginosa may of course occur if early treatment of P. aeruginosa is not routine as was the case in the USA until recently. Where early eradication therapy was routine the prevalence of both S. aureus (Southern et al, 1993 below) and chronic P. aeruginosa infection (Lee et al, 2004 below) both fell to very low levels. However, as was predictable, the number of isolations of other organisms such as Stenotrophomonas maltophilia and Aspergillus fumigatus both increased. It seems that when one organism is eradicated from the CF respiratory tract another will enter – this has been noted from the early years of antibiotic usage e.g. Staphylococcus aureus, then Pseudomonas aeruginosa, then Stenotrophomonas maltophilia or Aspergillus fumigatus or some other gram-negative organism.
Fig. 4 Douglas Crozier Toronto Public Library
Further development of the Specialist CF Centres occurred in some countries but there were few in the UK. However, it was encouraging that in many countries the tide really seemed to be turning. Dr Douglas Crozier, (1924-2015) (Fig. 4) who, in 1958, had started the CF clinic at the Hospital for Sick Children, Toronto, exemplified this new approach (Crozier, 1974 below). In his 1974 article – “Cystic fibrosis – a not so fatal disease”- he gave advice, based on his considerable experience in Toronto, which clearly described the modern aggressive approach to management now adopted in many CF Centres including our own in Leeds – “Success of treatment will depend on a complete assessment of the patient and then continuing attempts to obtain normal bodily function and maintain it” (Crozier, 1974 below).
From the early Seventies, Crozier abandoned the traditional low fat diet believing that “to deprive the child with cystic fibrosis, who usually has very little subcutaneous fat, of this important nutrient seems ridiculous”. So as early as 1972, he changed his patients to a high saturated fat diet of whole milk, butter, eggs, and animal fats which did require the patients to take 60-100 Cotazym pancreatic enzyme capsules each day (Crozier, 1974 below). Later, the significantly superior nutritional state and longer survival of Toronto patients than those in the rest of Canada and also in Boston, was attributed to their better nutritional state (Corey et al, 1988 below).
This lack of acceptance of the status quo approach was also evident in the Danish CF Centre in Copenhagen,
Fig. 5 Erhard Flensborg cystickfibrose.dk
The CF Centre was established in 1968 by Erhard Flensborg (1912-2009) (Fig. 5) (Szaff et al, 1983) where, since 1963, 80% of the country’s 225 patients were treated. In 1976 they realised that chronic Pseudomonas aeruginosa infection and its severity, as judged by the number of precipitins in the patient’s serum, was closely related to the prognosis (Høiby, 1977 below)
Professor Niels Hoiby’s work on precipitins influenced our subsequent interest in Pseudomonas antibodies in the Leeds patients and, with funding from the CF Trust, we appointed an immunologist, Dr Moira Brett, who studied Pseudomonas antibodies in detail and they have been in routine use since the mid-Eighties in Leeds (Brett et al, 1986; Brett et al, 1988; Brett et al, 1992 below) and are still used in the Leeds CF clinics (Pond et al, 1994; Lee et al, 2004a below).
Fig. 6. Niels Hoiby. Author’s photo
In 1976 Hoiby’s work resulted in the adoption of the Danish policy of regular 3-monthly courses of intravenous antibiotics for those patients chronically infected with Pseudomonas (Schiotz et al, 1981; Szaff et al, 1983; Jensen et al, 1989 all below) and cohort isolation which separated patients with Pseudomonas aeruginosa from those without the infection (Høiby & Pedersen, 1989 below); their improving results were later reflected in an impressive increase in survival (Frederiksen et al, 1996 below).
Fig. 7. Christian Koch. Author’s photo
The late Dr Christian Koch (1936-2004) (Fig. 7) and Professor Niels Høiby and their colleagues in Copenhagen have had a major influence on the care of people with CF and their aggressive approach to treatment, general caring attitude, and practically useful and practical contributions to the CF literature have been a major influence on many of us in Europe involved with developing CF care.
As survival improved through the Seventies there was an increasing interest in the chronic nutritional problems. As children survived through childhood to adolescence their nutritional state and growth deteriorated progressively due to inadequate energy intake, poorly controlled intestinal malabsorption and the major catabolic effect of their increasingly severe chest infection (Berry et al, 1975 below).
In an attempt to improve absorption by dietary manipulation, Dr Jimmy Allan, a general paediatrician from Macclesfield in the North of England, popularised a nutritional supplement consisting of beef serum protein hydrolysate, a glucose polymer and medium chain triglycerides – the so called “Allan Diet” on which some children had a definite improvement in weight gain (Allan et al, 1973 below). A subsequent study from Cincinnati, provided further support to the beneficial effect of the “Allan Diet” (Berry et al, 1975 below). Although another trial from Wales by Jeanette Lassa (Fig. 8) reported some improvement in 10 of 28 patients treated with the diet for 12 months, the authors’ conclusions were that “such an unpleasant and expensive diet should be restricted to a few selected cases, rather than given as routine treatment” (Yassa et al, 1978 below).
Fig. 8 Jeanette Yassa measuring subcutaneous fat
However, the new, acid resistant pancreatic enzymes (Pancrease and later Creon) were soon to become available in the early Eighties and they had a dramatic effect on the control of the intestinal malabsorption permitting most patients a normal or near normal fat intake – a more acceptable way of increasing their energy intake.

Fug. 9 Birgitta Strandvik. Researchgate
Abnormalities of fatty acids had been noted by many authors from the Sixties (Kuo et al, 1962 above) to the present. Birgitta Strandvik (Fig 9) (Strandvik et al, 2001 below) and had even been suggested as a primary metabolic abnormality.

Fig. 10. Sir Robert Elliot
Professor Bob Elliott (1934-2020) (Fig. 10) in New Zealand reported an unusual clinical course in a child with CF treated with intravenous infusions of soya oil emulsion, which contains mainly linoleic acid (Elliott & Robinson, 1975 below) and favourable effects in further treated children (Elliott, 1976 below). These reports caused considerable interest at the time. An abnormality of prostaglandin metabolism was suggested (Chase et al, 1978 below). In a subsequent controlled trial (Chase et al, 1979a), “cumulative analysis” showed a greater improvement in the test group although the numbers seemed hardly adequate. This is said to be the first double blind trial of nutritional intervention in cystic fibrosis. Interestingly, the precise role of essential fatty acids is yet to be determined but correcting the essential fatty acid imbalance between docosahexanoic and linoleic acid has been reported to modify the pancreatic histological abnormalities in CF mice (Freedman et al, 1999); also the imbalance is also present in the tissues of people with cystic fibrosis (Freedman et al, 2004); however, the only eventual conclusion was this treatment led to modification of the inflammatory markers (Beharry S et al. 2007 below).
Sir Robert Elliott was knighted in 2020 for his outstanding contributions to cystic fibrosis – in particular for his part in the IRT neonatal screening test. There is an interesting account of his very eventful career on the internet. (https://www.stuff.co.nz/national/health/300091944/sir-bob-elliott–paediatrician-medical-researcher-boatrocker)
A number of important studies in the late Seventies and early Eighties measured the actual energy intake of people with cystic fibrosis. Contrary to the traditional impression, that people with CF had voracious appetites, when their intakes were actually measured professionally by nutritionists or dietitians, it was evident that many consumed less energy even than that recommended for healthy children of their age (Chase et al, 1979b below). It is disappointing that many subsequent studies showed many people with CF in the UK and elsewhere continued to have a suboptimal energy intakes (Littlewood et al, 1984; Littlewood et al, 1988; Littlewood, 1993).
Towards the end of the Seventies, there was an important paper supporting the suggestion that a good nutritional state was associated with a better prognosis (Kraemer et al, 1978). The main lesson from all this work appeared to be that the dietitian or nutritionist was now an essential member of the CF team as most clinicians were not skilled at either accurately measuring dietary intakes or advising on the fine details of nutritional management.
Fig.10a. David Lawson.
At the start of the Seventies Dr David Lawson, (1917-2004) (Fig. 10a) Chairman of the CF Trust’s Research and Medical Advisory Committee, was asked to look into the future for the CF Trust’s magazine the CF News. In an article entitled “Into the 70’s” he reluctantly predicted developments that may occur during the decade.
David Lawson made ten predictions as follows – the diagnosis would be made earlier and the number of adults would increase (yes, it occurred); sudden improvements in outlook would occur where neonatal screening had been introduced (no -but gradual improvements over time); success of prophylactic anti-Staphylococcal therapy would be such as to call in doubt the importance of prophylactic physiotherapy (no – as other organisms caused increasing problems); by 1980 mist tent therapy would be abandoned (yes); whole populations would be screened for carrier status (no – still not introduced generally in UK by 2023 for financial reasons); carriers will be advised not to marry each other (yes – this would be ignored by 75% of young adults); antenatal diagnosis would be available from examination of amniotic fluid (yes); success of these methods would reduce the incidence of CF (no – not in this decade but eventually there was a gradual reduction in incidence), with the success of early treatment it will be difficult for parents to remember they are dealing with a potentially fatal disorder and could be a serious problem in securing the continuity of treatment (yes). Finally, the exact biochemical pathway by which the CF gene exerts its effect upon endocrine glands would be discovered (yes -eventually) and research would be directed towards counteracting these effects throughout life and thus rendering all other forms of treatment unnecessary.
Clinical papers published in the Seventies
1970 Allan JD, Milner J, Moss D. Therapeutic use of an artificial diet. Lancet 1970; i: 785-786.[PubMed]
The first report from Jimmy Allan, a general paediatrician from Macclesfield in the North of England, on the use of an artificial diet to improve nutrition in children with cystic fibrosis – a nutritional supplement consisting of beef serum protein hydrolysate, a glucose polymer and medium chain triglycerides. At this time more children with CF were reaching adolescence with adverse nutritional effects of their poorly controlled malabsorption and increasingly severe chest infection which made normal weight gain and growth impossible in many. So understandably, there was great interest from both parents and professionals in this publication (Allan et al, 1973 below).
1970 Wagget J, Johnson DG, Borns P, Bishop HC. The non-operative treatment of meconium ileus by gastrografin enema J Paediatr 1970; 77:407-411. [PubMed]

Fig. 11 John Wagget British Association Paediatric Surgeons website
This report confirmed the successful use of gastrografin enemas in four infants with meconium ileus. Gastrografin enemas were carefully injected into the colon with a fine tube and syringe under fluoroscopic control over about 45 minutes. While there were dangers (a previous infant’s colon had perforated with use of a Foley catheter), the lack of surgical success and the very poor outlook with the current treatments were considered good reasons for trying this medical procedure (Also Wagget J, Bishop HC, Koop CE. Experience with gastrografin enema in the treatment of meconium ileus. J Pediatr Surg 1970; 5:649-654). [PubMed]
Mr John Wagget (1938-2010) (Fig. 11) was appointed Consultant Paediatric Surgeon in 1971, initially at the Fleming Memorial Hospital for Sick Children and the Babies’ Hospital and later at the Royal Victoria Infirmary (RVI) Newcastle after both those institutions closed.
1970 Holsclaw DS, Grand RJ, Shwachman H. Massive haemoptysis in cystic fibrosis. Pediatrics 1970; 75:829-838. [PubMed]
The first report dealing primarily with 29 episodes of haemoptysis – a serious complication as 13 of the 19 patients died within six months. Treatment was with transfusions and supportive care and surgical resection in one patient (also reported by Lenvitsky S, et al, JAMA 1970; 213:125-127). [PubMed]
Arterial embolisation had not been described at this time and the technique certainly improved the prognosis – for example Stern RC et al, (Am Rev Resp Dis 1978; 117:825. [PubMed]) had no deaths in 38 patients although 48% had recurrent episodes. Also a series of 13 patients treated by bronchial artery embolisation was reported from Shwachman’s unit (Fellows KE et al, J Pediatr 1979; 95:959-963 below [PubMed] ).
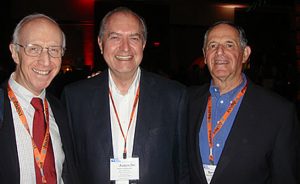
Fig.12. Richard Grand with Jim Littlewood and Beryl Rosenstein Author’s photo
Dr Richard J Grand (Fig. 12) is a distinguished North American paediatric gastroenterologist from Boston. He has 348 publications listed on Pubmed since 1962; he reported Pregnancy in Cystic Fibrosis in 1966. I was privileged to meet him at a North American CF Conference with Dr Beryl Rosenstein.
1970 Keating JP, Feigin RD. Increased intracranial pressure associated with probable vitamin A deficiency in cystic fibrosis. Pediatrics 1970; 46:41-46. [PubMed]
Two infants with CF aged four months had signs of raised intracranial pressure associated with vitamin A deficiency. One infant had xerophthalmia and keratomalacia; one had a cranial nerve injury with facial paralysis (also Abernathy 1976 below). Raised intracranial pressure has been described by a number of authors in young infants with CF and also in non-CF infants with vitamin A deficiency examples of which are reviewed in this paper.
1970 Mearns MB. Aerosol therapy in cystic fibrosis. Arch Dis Child 1970; 45:605-607.[PubMed]

Fig 13. Margaret Mearns. Author’s photo
Margaret Mearns from the UK reviewed the situation regarding the somewhat controversial nocturnal mist tent therapy which was at this stage recommended by the US CF Foundation with strong support from Leroy Matthews and his colleagues at the Cleveland clinic.
Mearns notes that Doershuk et al, 1964 and Matthews et al, 1967 from Cleveland showed improvements in respiratory function after nocturnal mist therapy which regressed when the treatment was withdrawn. Doershuk et al, (Pediatrics 1968; 41: 723-732. [PubMed]) reported good results in more severely affected children using ultrasonic nebulisers however, Matthews et al, (J Asthma Res 1968; 5:267-276. [PubMed]) reported subsequent deterioration of the earlier reported patients at 24 months although they had been improved at 12 months. Mearns mentions that Norman et al, 1969 in London showed no benefit from 2 years of nocturnal mist therapy. Finally Matthews et al, in 1969 (5th International CF Conference Cambridge, 1969:155) found a trend towards normal in early cases considering only 10% showed evidence of progressive lung damage over an average of seven years.
Margaret Mearns noted the need for a well-controlled trial and that “at this stage sitting on the fence is rarely a commendable or comfortable posture and it is one adopted only with reluctant necessity by the present writer after appraisal of the available facts about mist therapy”.
Subsequently a number of studies confirmed the doubts many clinicians had regarding nocturnal mist therapy (Bau et al, 1971 below; Chang et al, 1973 below) and their use diminished during the Seventies. The mist tent story would have raised an “I told you so” from enthusiasts of Cochrane Systematic Reviews in that a demanding, time-consuming, involved treatment had been introduced and officially recommended – even supported by such experts as Shwachman, di Sant’Agnese and the CF Foundation – before any controlled trial. Yet when it was put to the test of a controlled trial (admittedly involving few patients) failed to showed significant benefit.
However, nothing is entirely straightforward, as the highly experienced paediatrician Robert Wood in a detailed review of the treatment in 1976 did not condemn mist tent therapy out of hand (Wood 1976 below). One even wonders if another look at mist therapy would be in order in view of the current support for the low salt theory of pathogenesis and the improved nebulisation techniques available?
1970 Shmerling DH, Forrer JCW, Prader A. Fecal fat and nitrogen in healthy children and in children with malabsorption or maldigestion. Pediatrics 1970; 46:690-695. [PubMed]

Fig. 14. Andrea Prader
This classic paper, from Professor Prader’s (1919-2001) (fig. 14) unit in Zurich, has for many years provided paediatricians with the reference values for intestinal fat and nitrogen absorption in infants and children. Fat and nitrogen per day in normal infants were not more than 4.3 g (mean+/- 2SD) and 1 g respectively and for older children 3.1 g fat and 1.2 g nitrogen. The degree of malabsorption resulting from exocrine pancreatic insufficiency was considerably more severe than in untreated coeliac disease where between 3 to 13 g were excreted daily.
1970 Shwachman H, Redmond A, Kon-Taik Khaw. Report of 130 patients diagnosed under 3 months of age over a 20-year period. Pediatrics 1970; 46:355-343. [PubMed]
This was a classic paper from Harry Shwachman’s unit involving Aileen Redmond, a paediatrician from Belfast who was working in Boston at the time and who later became director of the Northern Ireland Paediatric CF unit at the Belfast Children’s Hospital.

Fig.15.Aileen Remond
In this study patients who had been diagnosed aged less than 3 months between 1949 to 1969. Group A – 63 before symptoms, Group B-13 with mild symptoms, and Group C – 54 diagnosed with more severe symptoms requiring hospitalisation. There were 29 deaths – 11 (15%) in groups A and B and 18 (33%) in group C. Of the 101 survivors 14 were in excellent condition, 71 mildly affected and 12 moderately or severely ill. The calculated survival to 20 years was 77%.The authors mention that the first major treatment advance was chlortetracycline in 1948, pancreatin since 1951, mist tents from 1954 and physiotherapy since 1955. The authors concluded that -”Better health and prolonged life result from early diagnosis and vigorous therapy”.
Dr Aileen Redmond (Fig. 15) from Belfast N. Ireland was working in the Boston with Harry Shwachman at the time of this paper. She subsequently returned to Belfast where she developed an excellent CF service.
1970 Harley RD, Huang NN, Macri CH, Green WR. Optic neuritis and optic atrophy following chloramphenicol in cystic fibrosis patients. Trans Am Acad Ophthalmol Otolaryngol 1070; 74:1011-1031. [PubMed]
This is a review of the literature on chloramphenicol toxicity and experience with eye complications in cystic fibrosis. The authors considered that the peripheral numbness, tingling and cramps frequently preceded the ocular signs which were often sudden. Variable ocular signs were seen including both papilloedema and normal disks. Optic neuritis and visual loss were related both to dosage and duration of treatment. 25 mg/kg/day for not more than 3 months appeared to be safe. Fortunately, most patients’ visual acuity returned soon after stopping the drug.
In 2011 an isolated case of optic neuritis due to chloramphenicol toxicity was reported in a man with CF who was taking large doses of chloramphenicol for chronic prostatitis over several years. The visual symptoms subsided when the drug was stopped. The authors note this is the first case for 20 years (Fung AT et al. BMJ Case Reports 2011.[PubMed]).
1970 Wright GLT, Harper J. Fusidic acid and lincomycin therapy in Staphylococcal infections in cystic fibrosis. Lancet 1979; i:9-14. [PubMed]
This report from Brisbane showed the superiority of lincomycin and fusidic acid combination in eradicating Staphylococcus aureus in 16 patients with cystic fibrosis.Later John Brown from Sydney describing 718 courses of anti-Staphylococcal treatment mentions Wright and Harper’s paper and demonstrated the superiority of clindamycin with or without fusidic acid over all other regimens (Brown J. Aust Paediatr J 1980; 16:207-209.).
1970 Torstenson OL, Humphrey GB, Edson JR, Warwick WJ. Cystic fibrosis presenting with severe hemorrhage due to vitamin K malabsorption: A report of 3 cases. Pediatrics 1970; 45:857-861. [PubMed]
Three infants with CF presented with severe bleeding secondary to vitamin K deficiency at one, three and four months of age . The authors mention that Shwachman had observed CF infants with prothrombin deficiency one of whom developed a subdural bleed (Shwachman H et al. Pediatrics 1960; 25:155). Also di Sant’Agnese noted vitamin K deficiency leading to occasional bleeding (di Sant’Agnese & Vidaurreta JAMA 1960; 172:2065) and later four infants aged one to four months were reported by Walters TR & Koch F. (Am J Dis Child 1972; 124:641-642).
1971 Huang NN, Hiller EJ, Macri CM, Capitanio M, Cundy KR. Carbenicillin in patients with cystic fibrosis: clinical pharmacology and therapeutic evaluation. J Pediatr 1971; 78:338-345. [PubMed]
Further work on carbenicillin, the relatively new intravenous anti-Pseudomonal antibiotic introduced in 1968. (also Bauxerbaum et al, 1968 above).
1971 Bau SK, Aspin N, Wood DE, Levison H. The measurement of fluid deposition in humans following mist tent therapy. Pediatrics 1971; 48:605 – 612. [PubMed]
Mist from an ultrasonic nebuliser labelled with technetium 99m was inhaled in mist tents for an hour by six control patients and eight patients with cystic fibrosis. No attempt was made to control the rate or depth of breathing nor to encourage mouth or nasal breathing. Less than 5% of the radioactivity nebulised and distributed in the tent entered the body – of this 90% lodged in the nasopharynx, was swallowed and rapidly appeared in the stomach. Very little activity was detected over the lungs. The authors concluded – “If mist tents are of value in the treatment of cystic fibrosis the benefit must accrue from reasons other than the deposition of significant quantities of fluid in the lung”.
This was one of a number of studies which cast increasing doubts on the value of nocturnal mist therapy. Henry Levison’s group in Toronto went on to do a small clinical trial which failed to show benefit from nocturnal mist therapy (Chang et al, 1973 below). As mentioned above, Robert Wood questioned the accuracy of the labelled technetium studies as apparently the isotope is removed very rapidly from the airways – also he had observed considerable fluid deposition in the airways when performing bronchoscopies soon after mist tent therapy (Wood et al. 1976, below).
1971 Holsclaw DS, Permutter AD, Jockin H, Shwachman H. Congenital abnormalities in male patients with cystic fibrosis. J Urol 1971; 106:568-574. [PubMed]
Fig. 16 Douglas Holscaw – author’s photo
The genetic link between men with CF and those with congenital absence of the vas deferens (CBAVD) was first postulated by Douglas Holsclaw (Fig. 16) and colleagues and subsequently confirmed following the availability of genetic analysis after the identification of the CF gene in 1989 (Dumur V et al, Lancet 1990; 336:512 [PubMed]; Rigot JM et al. N Eng J Med 1991; 325:64-65 [PubMed]; Anguiano A et al. JAMA 1992; 267:1794-1797. [PubMed]).
1971 Norman AP, Hall M. Nocturnal mist therapy in cystic fibrosis. Practitioner 1971; 206:786 -790. [PubMed]
Archie Norman was unable to show any difference in any objective findings of respiratory or nutritional state between 10 treated in mist tents at night and 10 control children with CF over two years. He commented on the many practical difficulties of delivering the treatment and maintaining the equipment. Only one of nine treated families opted to continue with the tent after the trial ended – this is probably significant indicating the parents had not observed any benefit.
1971 Dolan TF, Gibson LE. Complications of iodide therapy in patients with cystic fibrosis. J Pediatr 1971; 79:684-687. [PubMed]
Iodides had been used for asthma from the 19th century and were reported to have the effect in asthmatics that the “morning cough was of much shorter duration, say 5 minutes instead of 60 minutes, and that the phlegm was now loose” (Bernecker C Acta Allergologica 1969; XXIV:216-225).
In the present study from Yale 47 of 55 patients with CF who were on long term iodides to aid expectoration developed goitres usually within two to three years; also 14 had laboratory evidence of hypothyroidism. Two patients with CF had goitres but were not taking iodides. The rather limited evidence for the efficacy of iodides was reviewed – there were no studies showing improvement in respiratory function.
The authors indicated their intention to discontinue iodide therapy and they planned to evaluate the effect of iodides in a future study (also Ruben et al, 1960 above; Vagenakis et al, 1975 below).
1971 Gottlieb RP. Metabolic alkalosis in cystic fibrosis. J Pediatr 1971; 79:930-936. [PubMed]
An early example of metabolic alkalosis in an infant with cystic fibrosis. This came to be recognised as a mode of presentation eventually known as Pseudo-Bartter’s syndrome. There were subsequently isolated case reports in children with CF and an estimate of incidence in infants with CF by Beckerman & Taussig (1979 below).
1971 George L, Norman AP. Life tables for cystic fibrosis. Arch Dis Child 1971; 46:139-143.[PubMed]
Archie Norman and colleagues produced a number of life tables for people with CF in the UK. Here 128 infants without meconium ileus (MI) and 43 with MI from 1964 for five years are compared with tables for previous 20 years showing obvious improvement in survival – suggested as being due to early diagnosis and treatment. The one year survival was 34% compared with 93%, and at five years 19% vs. 89% between the two periods.
1971 Godfrey S, Mearns M. Pulmonary function and response to exercise in cystic fibrosis. Arch Dis Child 1971; 46:144-151. [PubMed]
In 41 patients with CF, aged between five and 21 years, there was a linear relationship between FEV1 and maximum voluntary ventilation and the general clinical grading. The authors suggested that “the pattern of physiological disturbance is so characteristic that it could well serve as an aid todiagnosis in doubtful cases and can be revealed by steady state exercise without the use of cardiac or arterial catheterisation”. This may have been so in the authors’ experience but these physiological studies have never been made generally available to most people with CF in the UK nor have they made a significant contribution to clinical management or the understanding of the basic CF defect.

Fug. 17. Simon Godfrey. Author’s photo
Professor Simon Godfrey (fig. 17), is a respiratory paediatrician who at the time of this study was working at the Hammersmith Hospital, London; later he moved to Israel. He combined with Margaret Mearns at the Queen Elizabeth Hospital, Hackney on a number of interesting studies relating to CF.
1971 Holsclaw DS, Rocmans C, Shwachman H. Intussusception in patients with cystic fibrosis. Pediatrics 1971; 48:51-58. [PubMed]
Douglas Holsclaw estimated that intussusception occurred in 1% of children with CF with an average age of onset was between nine and 12 years – older than the age of presentation in non-CF children. (also Brown PM et al, NEJM 1960; 263:544; Flux M. South Med J 1976; 60:1184-1186). Compared with non-CF intussusception the onset was less acute and blood was passed rectally in less than a quarter of patients.Even with present day treatment an appreciable number of people with CF have intermittent colicky abdominal pain and distal intestinal obstruction syndrome (DIOS). In attacks the concern is always that they have developed either appendicitis or intussusception. Although in later publications ultrasound was recommended as reliably identifying intussusception, at the time I suggested that a contrast enema should be an early investigation and would usually suggest the diagnosis (Littlewood JM. J R Soc Med 1992; 85 Suppl 18:13-19.[PubMed]).
1971 Harboushe C, Iacocca V, Braddock L, Barbero G. Pseudomonas agglutinins in patients with cystic fibrosis. Pediatrics 1971; 48:973-974. [PubMed]
An early study of 32 patients with CF of whom 24 harboured Pseudomonas aeruginosa. Not surprisingly, these 24 patients had the highest anti-Pseudomonal serum agglutinin antibody response when compared with eight CF patients without Pseudomonas and 32 controls. Although this may appear an obvious finding, at the time of this publication the significance of Pseudomonas in the sputum of people with CF was still not established and some clinicians still doubted its importance i.e. does Pseudomonas invade already damaged lungs or is it a primary cause of the damage? Also this publication was “pre-Hoiby” whose first publications in this area were from 1973. So the presence of an antibody response, suggesting tissue involvement, gave further confirmation as to the importance of P. aeruginosa. Previous studies of immune response had been reported (Diaz F et al. J Inf Dis 1970; 121:269.[PubMed]; Huang N et al CF Club Abstracts 1970:19; Doggett RG, Harrison GM. 5th CF Conference Cambridge 1969:175).
The whole subject of antibody response was later considerably expanded by the many studies of Niels Hoiby from 1973 onwards (below); he correlated the immune response, as judged by antibodies detected by crossed immunoelectrophoresis, with the patient’s clinical course (Hoiby & Axelsen, 1973; Hoiby, 1977 below); certainly his publications stimulated us in Leeds to develop and use Pseudomonas antibodies from 1986 until the present time, using an ELISA test developed by Dr Moira Brett (Brett et al 1986 see below) and more recently using a commercial kit.
1971 Valman HB, France NE, Wallis PG. Prolonged jaundice in cystic fibrosis. Arch Dis Child 1971; 46: 805-809. [PubMed]
Fig. 18. Bernard Valman
Bernard Valman (Fig 18) reviewed previous reports of early hepatic changes (Bodian, 1952; di Sant’Agnese & Blanc, 1956 both above) and of neonatal obstructive jaundice in CF (Gatzimos CD & Jowitt RH, 1955; Bernstein J et al, 1960; Shier KJ & Horn RC, 1963; Kulczycki LL, 1967; Talamo RC & Hendren WH,, 1968). Four new infants with CF and jaundice were reported – resolving in two survivors and one that died of other causes. Histology in the paper already showed established cirrhosis in the infant who died at 22 weeks.
This was an important paper showing a reasonably good prognosis for early prolonged obstructive jaundice in some CF infants. It is also important that this presentation of CF is recognised as infants with CF have been mistakenly thought to have biliary atresia only to be diagnosed as having CF after they had major surgery using a Kasai operation. In some of these CF infants the jaundice settles spontaneously over a few months; others have been reported to respond to treatment with ursodeoxycholic acid – the treatment introduced for older patients with liver disease in the early Nineties (Colombo et al, 1990 below).
(See”Liver” in the “Topics” section of this website)
1971 Davidson AG, Anderson CM. Diagnosis of cystic fibrosis. Br Med J 1971; 4:362 (letter). [PubMed]
Fig. 19.Mary Goodchild, George Davidson & Margaret Mearns. Author’s photo
A short letter from Birmingham UK warning that the meconium test for CF may be negative in pancreatic sufficient infants and tested by the Green and Shwachman technique. An infant with CF was missed in this manner and subsequently proved to have CF but be pancreatic sufficient.
Professor George Davidson (1937-2020) (Fig 19) was born in the Canada and at this time was working in Birmingham with Prof. Charlotte Anderson. He subsequently moved to Vancouver where he built up a major CF centre and also held medical advisory appointments with ICFMA and CF Worldwide.
1972 Cain ARR, Deall AM, Noble TC. Screening for cystic fibrosis by testing meconium for albumin. Arch Dis Child 1972; 47:131-132. [PubMed]
One of the earliest reports from the paediatricians in Newcastle and Ashington in the North of England of meconium screening using the Labstix (Ames) urine test strip for albumin as suggested by Werner Schutt et al 1968 (above). A small smear of meconium was mixed with few drops of water on a glass slide and the Labstix placed on the edge of the drop of thee mixture. In this study one infant with CF was detected in 6200 newborns among whom there were also 2 with meconium ileus – the expected incidence of around 1 in 2000 births.
1972 Mearns MB. Treatment and prevention of pulmonary complications of cystic fibrosis in infancy and early childhood. Arch Dis Child 1972; 47:5-11. [PubMed]
Margaret Mearns, (figure 3 & 19) at the Queen Elizabeth Hospital for Children, Hackney Rd, London was one of the few UK paediatricians with considerable experience in treating children with CF. She wrote “Most patients admitted in early infancy and treated since 1957 remain free of detectable lung damage up to the age of five years. Vigorous treatment and attempts to control and eradicate infection in infancy can prevent most of these patients from becoming chronic respiratory invalids in early childhood”.
Of 76 patients between 1950 and 1964 – 30 were pre-1957 and 46 after 1957 and they had more vigorous treatment including continuous anti-Staphylococcal antibiotics for the first year and they were in better condition at five years. None of Margaret Mearns’s children were treated with mist tents which were very popular throughout the Sixties in the USA (see Lawson D, 1972 below for comment).
Carl Doershuk and others from Cleveland commented and emphasised that, although they believed mist tents to be beneficial, they had NEVER implied they were the main reason for the improved survival but emphasised their overall approach of early diagnosis, prompt and comprehensive care and wherever possible prophylactic (maintenance of normal hygiene) care. Their results were comparable with Mearns’s – continuous antibiotics and no mist tents (London) vs. mist tents and discontinuous antibiotics (Cleveland).
The final paragraph of these two Cleveland paediatricians deserves a full quote exemplifying the attitude adopted by successful CF physicians –“The central issue seems to us to be not how little one can do in treating a progressive life-threatening disease; but rather how effective a programme one can develop and maintain for long term home management of these patients. In our opinion each measure recommended for long term management works best in conjunction with the other measures. However, the continued presence of a concerned and interested physician, routine regular outpatient visits and respiratory cultures cannot be replaced in any way and must be repeatedly emphasised”. This central theme comes through from all the really successful CF centres and clinicians.
1972 Lawson D. Cystic fibrosis – Assessing the effects of treatment. Arch Dis Child 1972; 47:1-4. [PubMed]
Commenting on the preceding paper on CF treatment by Margaret Mearns (1972 above), David Lawson observes “The results are a remarkable tribute to the work of the clinical service led and inspired by the late Dr. Winifred Young and I do not think they can be matched in the literature of the period”.David Lawson posed the interesting and really fundamental question – “How much is the course of the disease, as shown in its natural history untreated (i.e. rare survival beyond the second year), an inevitable peripheral result of the genetic defect? And how much is this due to the interaction of controllable environmental factors with these biochemical and structural remote effects of the gene?”
David Lawson’s question has been, in part, answered for over the years we have seen that the increasingly effective control of environmental factors and the secondary effects results in an impressive increase in survival even though the genetic defect was not yet amenable to treatment.
This editorial is a lengthy review of the situation at the time and of the 1971 meeting of the European Working Group for Cystic Fibrosis, by one of the leading UK CF paediatricians who already saw the need for neonatal screening and treatment before symptoms become established. “Cases must be diagnosed before they come, into trouble, to a clinician: and sophisticated co-operative recording and analysis of prospective studies are necessary if future treatment is to be based upon emerging fact, rather than upon disparate opinion”
1972 May JR, Herrick NC, Thompson D. Bacterial infection in cystic fibrosis. Arch Dis Child 1972; 47:908-913. [PubMed]
Another more extensive study of precipitins against the common respiratory pathogens in 195 patients with CF and cultures obtained from ninety six. The most common precipitins were against P. aeruginosa – more than any other organism being the most frequent organism isolated from children aged six to ten years. S. aureus was not always the first infection and people with CF seemed susceptible to bronchial infection with any pathogen. The fall in prevalence in older patients suggested failure of many patients with P. aeruginosa to survive into adult life in contrast to those with S. aureus.This was an early indication that infection with P. aeruginosa may adversely affect the long term prognosis – a fact confirmed in subsequent studies. These authors noted “as Doggett and Harrison (1969 above) suggested, infection with mucoid P. aeruginosa is currently one of the commonest causes of death of patients with cystic fibrosis, and the need to keep them out of hospital away from sources of cross-infection cannot be too strongly emphasised”. It was some decades during and after the Nineties before all paediatricians and physicians accepted this sensible advice!! (also Harboushe et al, 1971 above).
1972 Mearns MB, Hodson CJ, Jackson ADM, Haworth EM, Sellors TH, Surridge M, France NE, Reid L. Pulmonary resection in cystic fibrosis: results in 23 cases. 1957-1970. Arch Dis Child 1972; 47:499-508. [PubMed]
Another early report showing good results from surgery at a time when many were suggesting surgery should be avoided in non-CF children with bronchiectasis. Twenty three lobectomies or segmental resections were performed. Nine patients were referred from other centres. Twenty one of the 22 survivors had definite benefit and a rather remarkable 16 of the 22 became pathogen free although it is not stated for how long they remained clear. It was advised that surgery should not be done until after six months of conservative treatment. Authors mention that the late Dr Winifred Young found segmental or lobar collapse could take up to six months to resolve with medical treatment.
The fact that 16 of 22 patients became pathogen free is interesting, surprising and important, perhaps suggesting that the impossibility of eradicating chronic infection could be related to local areas of tissue damage rather than general abnormality of all the respiratory mucosa. The first major lung resection in CF was by Lloyd et al, 1952 (above) then by Schuster et al, (1964 above).
1972 Mearns MB, Hunt GH, Rushworth R. Bacterial flora of the respiratory tract in patients with cystic fibrosis 1950-1971. Arch Dis Child 1972; 47:902-907.[PubMed]
Experience from the Queen Elizabeth Hospital for Children, London. Bacterial flora of patients observed from 1950 onwards also bacterial precipitins from 102 patients. The frequency of isolation of S. aureusfell and there was a steady increase in P. aeruginosa in the most severely affected patients – the fall in S. aureus was one of the most striking features. Commenting on the view of David Lawson that prophylactic anti-Staphylococcal therapy is indicated, Margaret Mearns cautioned that this could lead to more P. aeruginosa infection – still a point of discussion today but much feared then as early eradication of the organism had not been described. Certainly there is evidence that this is the case if a wide spectrum antibiotic is used unless a regimen of early eradication of P. aeruginosa is routine – as it was not in 1972. However, May et al believe, almost certainly correctly, that any respiratory pathogen may cause the initial infection including P. aeruginosa.
1972 Taussig LM, Lobeck C, di Sant’Agnese PA, Ackerman DR, Kattwinkel J. Fertility in males with cystic fibrosis. N Eng J Med 1972; 287:586.[PubMed]

Fig.20. Lynn Taussig
Some 2% of 117 men with CF appeared to be fertile and the authors emphasised they should be given genetic counselling. They documented relatively normal semen analysis in only two men with CF and note a further report of male fertility by Feigelson et al, (1969 above) (on male infertility also Denning et al, 1968 above; Kaplan et al, 1968 above).
1972 Stern RC, Doershuk CF, Matthews LW. Use of a heparin lock to administer intermittent intravenous drugs. Clin Ped 1972; 11:521-523. [PubMed]
The first report of the use of heparin locks for giving repeated doses of intravenous antibiotics to children with CF. Robert Stern (Fig 21) was the
Fig. 21.Robert Stern
first to use colistin intravenously in CF and was closely involved in the development of intravenous (IV) antibiotic therapy. The first of his patients were treated at home from 1973 when a 15 year old girl worked as a waitress while receiving IV antibiotics via a heparin lock. Stern writes – “an early, if not the first, pioneer who self administered IV medications while continuing to work and pursue other normal out-of-hospital activities”. Other centres followed (Rucker & Harrison, 1974 below). Crozier in Toronto reported using IV gentamicin and carbenicillin in 1974 for Pseudomonas infections (Crozier, 1974 below).
Dr Robert Stern (Fig 21) gives an interesting account of his early use of the intravenous route, instead of the painful intramuscular route, for colomycin in the mid-Sixties. Colomycin, was the only parenteral antibiotic in the early Sixties, later to be replaced by intravenous gentamicin and soon after carbenicillin and piperacillin became available. He describes the early developments including the heparin lock in the early Seventies, the gradual involvement of the patients with CF in managing their own IV therapy first in hospital and eventually at home (Stern RC. Intravenous treatment: where we are and how we got there. In: Doershuk CF, editor. Cystic Fibrosis in the Twentieth Century. Cleveland: AM Publishing, Ltd, 2001:93-111).

Fig. 22. Ella H Oppenheimer
1972 Oppenheimer EH. Glomerular lesions in cystic fibrosis: possible relation to diabetes mellitus, acquired cyanotic heart disease and cirrhosis of the liver. Hopkins Med J 1972; 131:351-366. [PubMed]
Ella Oppenheimer (Fig. 22) noted glomerular changes at autopsy in four of the five children with CF who also had diabetes mellitus. Other factors were involved but “since cyanotic heart disease, diabetes mellitus and biliary cirrhosis are important complications of cystic fibrosis, it is apparent that greater numbers of cystic fibrosis children with renal complications will be found and that with longer survival renal insufficiency may become an important part of the cystic fibrosis syndrome”.
A prophetic statement as indeed this proved to be the case and diabetes mellitus proved a serious and increasing problem as survival increased. Also a variety of nephrotoxic drugs such as aminoglycosides and colomycin were used repeatedly over many years (Bertenshaw C. Watson AR. Lewis S. Smyth A. Survey of acute renal failure in patients with cystic fibrosis in the UK. Thorax 2007; 62:541-545 below).
1972 Elliott RB. The effect of essential fatty acid on sweat sodium concentrations in cystic fibrosis. Aust Paediatr J 1972; 8:217

Fig 23.Robert (Bob) Elliot
Prof. Bob Elliott (Fig. 23) and colleagues from Auckland, New Zealand published several papers showing improvement in the clinical state when children with CF were supplemented with medium chain triglycerides even to the extent of returning the sweat electrolytes to nearer normal values (also Elliott RB, Robinson PG. Arch Dis Child 1975; 50:75-78 below; Elliott RB. Pediatrics 1976; 57:474-479 below).
There was considerable discussion as to whether a disturbance of fatty acids resulted in an abnormality of prostaglandins. Rivers JA & Hassam AG suggested an abnormality of fatty acid metabolism such that there was a need for increased linoleic acid (Lancet 1975; ii: 642-643). Subsequent studies failed to substantiate their findings (Davidson GP et al. Aust Paediatr J 1978; 14:80-82; Chase et al. Pediatrics 1979; 59:428-432).
1972 Motoyama EK, Gibson LE, Zigas CJ. Evaluation of mist tent therapy in cystic fibrosis using maximum expiratory flow volume curves. Pediatrics 1972; 50:299 – 306. [PubMed]
Sixteen patients with CF were studied every two weeks over four to five months. Half had an initial eight to 12 weeks off mist therapy; the other half had conditions reversed. No improvement occurred with mist tent therapy – in fact, a small decline occurred. Bacterial contamination was present in two thirds of the tents.
So here was further evidence against the use of mist tents (also Norman et al, 1971; Bau et al, 1971; Chang et al, 1973; Bureau et al, 1978).
1973 Taussig LM, Kattwinkel J, Friedewald WT, di Sant’Agnese PA. A new prognostic score and clinical evaluation system for cystic fibrosis. J Pediatr 1973; 82:380-390. [PubMed]
Often referred to as the NIH Score, this system by Lynn Taussig (fig. 20) and colleagues stood up to evaluation well and apparently Shwachman and Kulczycki realised that a “more accurate method of assessment might become available” than their score. Respiratory function tests were included also complications that affected prognosis such as haemoptysis, cor pumonale and pneumothorax. Some considered that the nutritional state was under represented.
We have discussed elsewhere this and a number of subsequent scoring systems (Cystic Fibrosis Clinical Scoring Systems. Conway SP, Littlewood JM. In Cystic Fibrosis – Current Topics. Volume 3. Dodge JA. Brock DJH, Widdicombe JH, editors Chichester: John Wiley & Sons Ltd, 1996:339-358.
Dr Lynn Taussig (fig.20) worked with Paul di Sant’Agnese at the NIH, then as Professor at the Arizona College of Medicine for 20 years and then at the National Jewish Research Center in Denver. He was particularly active in CF care and research during the Seventies and Eighties.
In 1984 Lynn Taussig edited one of the major textbooks on CF (Cystic Fibrosis. Lynn Taussig. New York Theime-Stratton Inc. 1984). In the introduction to the book Charles Lobeck describes Lynn Taussig, Thomas Boat and Robert Schwartz as the professional descendants of Paul di Sant’Agnese who had in turn influenced their colleagues from Cleveland, Tuscon, Rochester and other academic locations. The book contains notable chapters on the gastrointestinal system, the pancreas and the hepatobiliary system written by Paul di Sant’Agnese. There are many other distinguished contributors who have made significant additions to our knowledge of CF.
1973 Weber A, Roy CC, Morin CL, Lasalle R. Malabsorption of bile acids in children with cystic fibrosis. New Engl J Med 1973; 289:1001. [PubMed]
Total faecal bile acid excretion had been reported to be increased (Leyland C. Arch Dis Child 1970; 45:714). This study of 26 children with CF aged two months to nine years from Prof. Roy’s unit in Montreal confirmed that faecal bile acid levels may reach seven times the normal level.
1973 Allan JD, Mason A, Moss AD. Nutritional supplementation in treatment of cystic fibrosis of the pancreas. Am J Dis Child 1973; 126:2-26. [PubMed]
This is the definitive publication of the “Allan Diet” of beef serum protein hydrolysate, glucose polymer and medium chain triglyceride. There had been great interest following the first report of this diet improving and maintaining the nutritional state of children with CF (Allan et al, Lancet 1970; i: 785-786) .More children were surviving for longer but with increasingly severe chest involvement, which drastically increased their energy requirements. As the chest involvement worsened their energy requirement increased, so attempting to maintain a reasonable nutritional state became an increasingly common, difficult and often insoluble problem in the days before more effective pancreatic enzyme preparations became available in the early Eighties.
It is not surprising therefore that the Allan diet received considerable attention from CF families (Berry et al, 1975 below; Yassa et al, 1979 below). Had not the new acid resistant pancreatic enzyme preparations (Pancrease and Creon) become available in the late Seventies/early Eighties the diet may have been used more widely.
1973 Goodchild MC, Nelson R, Anderson CM. Cystic fibrosis and coeliac disease: coexistence in two children. Arch Dis Child 1973; 48:684-691. [PubMed]
Fig .25. Bob Nelson
Fig. 24. Mary Goodchild
Beautifully documented cases from Mary Goodchild (Fig 24.) and Charlotte Anderson from Birmingham, one of the few major CF and paediatric gastroenterological centres in the UK at the time. There are impressive photographs and weight charts showing dramatic response to withdrawal of dietary gluten. The association of the two conditions was first reported by Hide & Burman, 1969 (above). Jejunal biopsy is a useful investigation in the occasional child with CF who presents with unusual features and who fails to thrive as well as expected. The authors’ advice to avoid attributing every problem to the CF is very sound and particularly apt in these days of sub-specialisation. For example, in a later study of CF infants poor weight progress with treatment for the CF was shown to be due to small bowel mucosal damage from cow’s milk protein intolerance (Hill et al, 1989 below).
Dr Mary Goodchild (fig 24) eventually became Director of the Cardiff Paediatric CF Centre and Bob Nelson (fig. 25) subsequently developed the Paediatric CF Centre in Newcastle, UK.
1973 Rucker RW. Harrison GM. Vitamin B 12 deficiency in cystic fibrosis. N Engl J Med 1973; 289:329. [PubMed]
Some malabsorption of vitamin B12 has been demonstrated in a number of later studies but absorption is much improved when pancreatic extract is added although not in all patients. However, in practice, a deficiency of the vitamin is very rare in CF even though supplements are not usually given (also Deren JJ et al. NEJM 1973; 288:949-950. [PubMed]; Gueant JL et al. Pancreas 1990; 5: 559-567.[PubMed]). More recently vitamin B12 status has been reported as elevated in many children with CF related in part to the content of dietary supplements (Maqbool A et al. J Pediatr Gastroenterol Nutr 2014. [PubMed]).
1973 Chang N, Levison H, Cunningham K, Crozier DN, Grosett O. An evaluation of nightly mist tent therapy for patients with cystic fibrosis. Am Rev Resp Dis 1973; 107:672-675. [PubMed]
One of the main studies that led to the abandonment of nocturnal mist therapy. The study was from Henry Levison’s department in the Toronto clinic on 26 patients with CF into the effects of mist tent therapy by assessing changes in clinical condition, pulmonary function and blood gas tensions with and without mist tent therapy for a total period of 6 months. The authors concluded that “The nightly mist tent therapy had no beneficial effect in patients with cystic fibrosis. The severity of the pulmonary disease and the type of nebuliser had no apparent effect on the results”. However, a subjective analysis by patients and parents had eight feeling “better”, four “worse” and 14 noticed “no difference”.
At this time nightly mist tents were the recommended treatment in the National Cystic Fibrosis Research Foundation’s Guide to Diagnosis and Management of Cystic Fibrosis. 1971. This study by Chang et al. was rather short term and entirely concerned with respiratory function tests, in fact, subjectively no less than 30% of the patients felt better in the tent! Also the use of nightly mist tents was supported by many leading CF clinicians in the USA including Paul di Sant’Agnese, Harry Shwachman, Carl Doershuk and Leroy Matthews. (See also Bureau MA et al, Pediatrics 1978; 61:842-846.[PubMed] for more prolonged study of mist tent use which was also negative. Also discussion after Wood 1976 below).Mist tents were still recommended by the Stockholm cystic fibrosis centre for small children in 2000 (Jakobsson B et al. J Hosp Infect 2000; 44:37-41[PubMed])
1973 DiMagno EP, Go VLW, Summerskill WHJ. Relations between pancreatic enzyme outputs and malabsorption in severe pancreatic insufficiency. N Engl J Med 1973; 288:813-815. [PubMed]

Fig. 26. Eugene di Magno
This classic study of DiMagno examined the relationship between steatorrhoea and creatorrhoea and pancreatic lipase and trypsin outputs in 17 non-CF patients with chronic pancreatitis and controls. Steatorrhoea was not observed until lipase output was 10 percent or less of normal and creatorrhoea only when trypsin output had fallen to 10% of normal. These findings provided an explanation for the large reserve of enzyme output and the late appearance of steatorrhoea in chronic pancreatitis.
Professor Eugene DiMagno (Fig. 26) at the Mayo Clinic was a leading expert on pancreatic disorders. These “10%” figures, so convincingly demonstrated in this beautifully clear, concise paper (less than 3 pages), were subsequently repeatedly quoted. The fact that the majority of CF infants have intestinal malabsorption from early life attests to the early onset and great severity of the pancreatic damage in many, but not all, of them.
1973 Hoiby N, Axelsen NH. Identification and quantitation of precipitins against Pseudomonas aeruginosa in patients with cystic fibrosis by means of crossed immunoelectrophoresis with intermediate gel. Acta Path Microbiol Scand 1973; 81:298-308. [PubMed]
Fig. 27. Niels Hoiby
The fourth of over 500 papers by Niels Hoiby listed on Medline! A classic study correlating clinical severity, presence of mucoid Pseudomonas aeruginosa and increased precipitins using a new more sensitive technique of crossed immuno-electrophoresis with intermediate gel to identify precipitins against P. aeruginosa from 33 patients with CF. He suggested there was selection of mucoid strains in CF by means of the immune response; also that the persistent infection and multiple precipitins produced against the bacteria could cause a local immune reaction which could enhance the destructive lesions of the respiratory tract. Very much in line with the modern views on inflammatory damage and the use of anti-inflammatory therapy.
Niels Hoiby (Fig 27) eventually worked with and became a key member of the Danish CF clinic for over 30 years during which time he became one, if not the, world’s leading authority on Pseudomonas aeruginosa and many other aspects of infection and immunity in CF (also Hoiby, 1977).

Fig. 28. Prof. Niels Hoiby receiving the ECFS Award in 2012
The 2012 ECFS Award (Fig. 28) was presented to Professor Niels Høiby in “recognition of his outstanding contribution to the understanding of Pseudomonas lung infection and translating this knowledge into better outcomes for people with cystic fibrosis. He was also recognised for his contribution as the founding President of the European Cystic Fibrosis Society and his lifelong commitment to the CF center in Copenhagen”.
1973 McCrae WM, Cull AM, Burton L, Dodge J. Cystic fibrosis. Parent’s response to the genetic basis of the disease. Lancet 1973; I: 141-143. [PubMed]

Fig. 29. Morris McCrae
One of the early psychosocial studies by paediatricians responsible for children with CF in Edinburgh (Morrice McCrae) and in Cardiff (John Dodge). Parents at the time had a poor understanding of the genetics of CF – and particularly poor instruction from the diagnosing paediatrician was common. There was no means of antenatal diagnosis at the time and 70% of families wanted no further children.
No paediatrician is exempt from occasional lapses in communication skills – the first question to Morrice McCrae after a lecture he gave to parents of CF children in Leeds was “What is a sibling?” – a term he had used frequently during the lecture! Morrice McCrae was one of the few paediatricians with a significant involvement with CF at this time and was responsible for developing the Edinburgh Paediatric CF clinic.
1973 MacLean WC, Tripp RW. Cystic fibrosis with oedema and falsely negative sweat test. J Pediatr 1973; 83:86-88. [PubMed]
An infant with CF, fed soya milk from age of 3 weeks, had oedema from 4 weeks. The sweat Cl values were 15 and 18 meq/l; later these had risen to 73 and 88 meq/l respectively. Subsequent reports of screened CF infants on normal milk feeds showed that, even in healthy CF infants, sweat tests may be relatively low and certainly less than 60 meq/l. (Massie J et al. Pediatr Pulmonol 2000; 29:452-456 below). So values over 30 meq/l would eventually be regarded as abnormal or requiring further investigation for a young infant.Also Lee PA, Roloff DW, Howatt WF. Hypoproteinemia and anaemia in infants with cystic fibrosis: Presenting symptom complex often misdiagnosed. JAMA 1974; 228: 585-588.[PubMed]. Fifty one such infants are already described in literature. One third died and 14 had received soya milk feeds.
1973 Oppenheimer EH, Esterly JR. Cystic fibrosis of the pancreas. Morphologic findings in infants with and without diagnostic pancreatic lesions. Arch Pathol Lab Med 1973; 96:149 – 154. [PubMed]It was suggested that some infants with CF may have normal pancreatic morphology and also it had been reported that some infants with clinical meconium ileus did not have cystic fibrosis (Rickham PP. Intraluminal intestinal obstruction. Prog Pediatr Surg 1971; 2:73-82). In this series ten of 37 infants with meconium ileus did not have typical changes of CF in the pancreas but did have other antatomical lesions compatible with a diagnosis of CF in 34 of the 37 cases and the changes in the other 3 were suggestive. The authors suggest that meconium ileus is always a manifestation of cystic fibrosis although there is variation in organ involvement.Since the Thirties histological changes in the pancreas were the means of identifying CF as a distinct entity from coeliac disease but these studies show the changes were very variable. However, subsequent studies from Toronto showed that pancreatic abnormalities were always present when detailed quantitative microscopy techniques were used (Imrie JR et al, Am J Path 1979; 95: 697-707; Sturgess JM. 1984 below).
1973 Day G, Mearns MB. Bronchial lability in cystic fibrosis. Arch Dis Child 1973; 48:355-359.[PubMed]
The authors comment that Heimlich et al, (J Allerg 1966; 37:103) surprisingly had failed to show a difference in bronchial lability between normal children and those with cystic fibrosis. In the present study only 14 (27%) of the 52 children with CF had normal results; 50% had abnormal bronchodilatation on exercise and 46% had abnormal bronchoconstriction after exercise.
Bronchial lability is commonly present in people with CF and can be seen to gradually lessen as the bronchial infection is treated during an exacerbation.
1973 Landau LI, Phelan PD. The variable effect of a bronchodilating agent on pulmonary function in cystic fibrosis. J Pediatr 1973; 82:863-868. [PubMed] 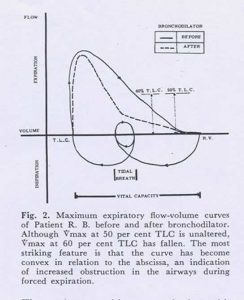
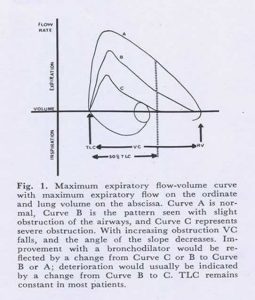
Figures 30 and 31 Maximum expiratory flow curves

Fig. 32. Louis Landau

Fig. 33.Peter Phelan
An important paper from the Royal Children’s Hospital, Melbourne. Nine (18%) of 50 patients with CF had measurable response to bronchodilators as judged by the maximum expiratory flow-volume curve which demonstrates the maximum expiratory flow rate throughout the forced vital capacity manoeuvre (figures 30 and 31).The changes were complex. In 5 (10%) the changes were typical of asthma. Four had a fall in Vmax thought to be due to airway compression during forced expiration as had been reported previously. The authors note that previous reports indicate no effect or minimal improvement with bronchodilators (Cook CD et al. Pediatrics 1959; 24;181; Gandevia B & Anderson C. Arch Dis Child 1959; 34:511; Polgar G & Barbero GJ. Am J Dis Child 1960; 100:733; Zaptetal A et al. Pediatrics 1971; 48:64).
Most people with CF have no changes, a few will show typical asthmatic response and will benefit from bronchodilators, BUT some develop reduced maximum expiratory flow rates possibly from compression of the larger airways – this could impair coughing and sputum clearance.
This is a paper from two experts Louis Landau (Fig. 32) and Peter Phelan (Fig. 33) with a clear message that bronchodilators can sometimes make the situation worse. The authors suggest that MEFV curve should be performed before bronchodilators are prescribed. Despite this and other studies, bronchodilators are prescribed for many people with CF and usually their effect on the MEFV is not checked – usually just the effect on FEV1 and FVC by simple spirometry – and also how the patient feels after the bronchodilator should be noted!! This approach seems to work well for most people with cystic fibrosis.
1974 Kulczycki LL, Schauf V. Cystic fibrosis in blacks in Washington DC. Am J Dis Child 1974; 127:64-67. [PubMed]

Fig. 34 Lucas Kulczycki
An intensive search for black people CF between 1962 to 1971 revealed 16 with cystic fibrosis. The clinical course was similar to the condition in whites. The calculated incidence was estimated as at least one in 17,033 black newborns. Later these findings were confirmed by others. More recently African mutations have been described by Michelle Ramsay and colleagues in South Africa (Carles et al, 1996 below)
1974 Prosser R, Owen H, Bull F, Parry B, Smerkinich J, Goodwin HA, Dathan J. Screening for cystic fibrosis by examination of meconium. Arch Dis Child 1974; 49:597-601. [PubMed]
Dr Prosser, a paediatrician from Newport in Wales, considered the BM Meconium screening test gave too many false negative results. In Wales 34,228 samples were examined over 4 years; 12 infants with CF were detected – only a 60% detection rate. The paper was generally quoted and accepted as showing BM meconium test was unsuitable for neonatal CF screening due to the unacceptable false negative rate. Also, at that time, the standard of treatment of most children with CF in the UK in general paediatric clinics was such that early diagnosis was of little advantage to most infants with CF in terms of long term survival.
Despite these discouraging observations, in one of the Leeds maternity units (St Mary’s in Leeds) we started BM screening 3000 infants each year for CF in 1975. We used the method continuously at St Marys and then at St James’s, when the maternity services moved there, until a change to IRT was made in 1995. When the BM test was done in the laboratory (rather than by the overworked midwives on the wards!!) we achieved an acceptable false negative rate of only some 12% (Evans et al, 1981 below). However, the IRT test described by Crossley and Elliott in 1979 was far superior and a major advance in neonatal CF screening. (also Stephan et al, 1975 below for extensive European experience with the BM Meconium test)
1974 Elliott RB. Wrinkling of skin in cystic fibrosis. Lancet 1974; ii: 108. [PubMed]

Fig. 35 Robert Elliot
The first report of excessive wrinkling of the skin in people with CF when soaked in tap water for three minutes (Fig 36). Prof. Bob Elliott (Fig.35) was a much respected paediatrician with a major “inventor/researcher tendency”! When I visited him in New Zealand in 1990, in relationship to CF, he was keen to describe how he was developing inhaled insulin for children with diabetes mellitus!
This report of finger wrinkling caused considerable interest as the basic defect was still totally obscure (see also Norman et al, 1974 below).
1974 Norman AP, Mall ML, Johns MK. Skin wrinkling in cystic fibrosis. Lancet 1974; ii: 358-359. [PubMed]

Fig 36. Finger wrinkling
Archie Norman at Great Ormond Street confirmed marked skin wrinkling in people with CF in water (figure 14) and commented that it could be an important observation. Johns M K (J Med Biol Illus 1975; 25:205-10) suggested it was due to the excessive salt concentration which increased the water binding capacity of keratin. Later it was suggested as a test of autonomic function (Bull C, Henry JA BMJ 1977; 551-552.[PubMed]).

Fig. 37 Jeanette Firth
In the Leeds CF unit at St James’s, Jeanette Firth, (Fig. 37) the CF centre day unit clinic nurse, performed the test on many children with CF who were attending the unit for Comprehensive Assessments of their CF and confirmed the phenomenon, but disappointingly we found it quite unrelated to the sweat electrolyte levels or any other clinical or laboratory feature of the patient’s condition (unpublished data). Subsequently there was considerable discussion as to autonomic abnormalities in CF of which skin wrinkling is a feature (see Davies et al, 1980).
1974 Chrispin AR, Norman AP. The systematic evaluation of the chest radiograph in cystic fibrosis. Pediatr Radiol 1974; 2:101-106. [PubMed]
An important paper and one of the first methods for the objective assessment of the chest X-ray changes in cystic fibrosis. The score was widely used by clinicians for publications and research. However, in recent years in the UK the “Northern” x-ray score (developed by the clinicians of the Northern CF Club in the UK – Conway et al, 1994 below) is now preferred by many as it correlates well with other X-ray scores and does not require a lateral X-ray – this considerably reduces the radiation the patient receives over the years.
1974 Crozier DN. Cystic fibrosis: a not so fatal disease. Pediatr Clin North Am 1974; 21:935-948.[PubMed]

Fig. 38 Hospital for Sick Children Toronto in the Eighties. Author’s photo.
This paper gives an idea of treatment at the Toronto CF clinic (fig. 38) in the early Seventies. Dr Douglas Crozier (fig. 39), who started the Toronto CF clinic in 1958, stated that “success of treatment will depend on a complete assessment of the patient and then continuing attempts to obtain normal bodily function and maintain it”. He described how he advised his patients to abandon the traditional low fat diet and used of very high doses of pancreatic enzymes (up to 100 Cotazym capsules per day). Crozier believed that “to deprive a child with cystic fibrosis, who usually has very little subcutaneous fat, of this important nutrient seems ridiculous”. The superior nutritional state of the Toronto patients is believed to be the main reason for their better survival. In 1973, 428 people with CF were attending the Toronto clinic of whom 92 (21.4%) were 16 years or older – this was quite remarkable for that time.

Fig 39. Douglas Crozier giving the “Breath of Life Award” to Maureen McChesney (Lavergne). 1970. With permission
Although I was never fortunate enough to meet Crozier I was profoundly influenced by this landmark paper from Toronto regarding the approach to management of people with CF – also by a later visit to Crozier’s successor, Henry Levison, at the Toronto clinic and attendance at the 8th International Cystic Fibrosis Congress there in 1980.
On the basis of Crozier’s recommendation to “perform a complete assessment of the patient” and then “continuing attempts to obtain normal bodily function and maintain it”, in 1980 on returning to Leeds from the Toronto meeting, with the help of a few colleagues at St James’s in Leeds, we started regular Comprehensive CF Assessments on all our children with cystic fibrosis.
1974 Burnell RH, Robertson EF. Cystic fibrosis in a patient with Kartagener’s Syndrome. Am J Dis Child 1974; 127:746-747. [PubMed]
Fig 40. Kartagener’s syndrome
A report from Adelaide Children’s Hospital, Australia. Said to be the third report of this combination with Kartagener’s syndrome of situs inversus totalis, bronchiectasis, and recurrent sinusitis with or without nasal polyps (fig 40). A white boy aged six months had “bronchopneumonia and neglect”. The lowest sweat electrolyte values were sodium 96 and chloride 80 meq/l. The duodenal biopsy showed partial villous atrophy which was rather puzzling and not discussed by the authors. The similarity of the symptoms of the two conditions, CF and Kartagener’s, is discussed. The two previous cases were doubtful. The authors advise excluding CF in all people with Kartagener’s syndrome. (Also Brown & Smith, 1959 above).
1974 Rucker RW, Harrison GM. Outpatient intravenous medications in the management of cystic fibrosis. Pediatrics 1974; 54:358-360. [PubMed]
One of the first reports of home intravenous antibiotic treatment from Texas – the first author was supported by a Clinical Fellowship Grant from the CF Research Foundation. They report a scalp vein needle and tube were used as a heparin lock and this usually required replacing once during the 10 to 12 day course. Mainly gentamicin but also colistin was used in 127 courses in 62 patients with a 68% success rate and no major complications. Seven of the failures subsequently died.
I regret we failed to mention this first really impressive early report from Texas in our 1988 paper on home intravenous antibiotic treatment (Gilbert et al, 1988 below). Robert Stern, who had already described the use of the “Heparin lock” (Stern RC et al. Clin Pediat 1972; 11:521) recalls starting home IV antibiotics in the early Seventies in Cleveland when a 15 year old girl asked if her heparin lock could be covered with a bandage so she “could leave hospital for a few hours to work at the Pronto Room as a waitress that afternoon”!! (Stern R. In Cystic Fibrosis in the 20th Century. Doershuk CF (ed.) 2001 below).
These reports from N. America were considerably in advance of any from the UK, the first being that of Winter RJD et al. in adults (Lancet 1984; i:1388-1339 below) and Gilbert J et al. in children with CF (Arch Dis Child 1988; 63:512-517 below). So in some large CF centres in N. America, treatment in this respect was undoubtedly more advanced than in the UK.
1974 Mearns MB. Cystic fibrosis. Brit J Hosp Med 1974; Oct: 497-506.
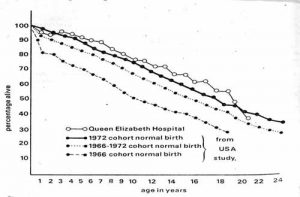
Fig 41. Survival curves from Mearns 1974.
This is a detailed overview of the situation in the UK by Margaret Mearns one of the leading authorities on CF working at one of the few UK paediatric CF units at the Queen Elizabeth Hospital for Children in London. Warwick and Pogue constructed life tables on these children attending the QE Hospital for Margaret Mearns. There was an estimated survival rate of 72% at 12 years and 45% at 20 years (fig. 41).
These survival figures were a tribute to the excellent care the children received at the QE Children’s Hospital from Margaret Mearns and Winifred Young – results in sharp contrast to the outlook for children with CF in most of the UK most of whom did not attend a specialised CF clinic – regrettably subspeciaisation in paediatrics came late to the UK.
1974 Fluge G, Aarskog D. Silver-Russell dwarfism and cystic fibrosis. Am J Dis Child 1974; 127:760-761. [PubMed]
A Norwegian girl aged seven years with CF had the typical features of Silver-Russell dwarfism. Intestinal malabsorption was documented at two years and no effect noted from a gluten free diet. Full investigation at six years showed positive sweat tests (Cl 77-114 & Na 82-137 meq/l) diagnostic of CF and confirmed the features of S-R dwarfism. A previous example of this association had been published by Taussig (Am J Dis Child 1973; 125:495-503).
1975 Shwachman H, Lebenthal E, Khaw P-T. Recurrent acute pancreatitis in patients with cystic fibrosis with normal pancreatic enzymes. Pediatrics 1975; 55:86-94. [PubMed]
Ten adolescents and young adults, who were all pancreatic sufficient, from over 2000 patients with CF, developed recurrent pancreatitis – two before the diagnosis of CF was made. There were typical abdominal symptoms of acute pancreatitis and elevated serum and urinary amylase and serum lipase. Three patients eventually died and the autopsies showed characteristic lesions of cystic fibrosis. The authors mention only one previously recorded patient with pancreatitis (di Sant’Agnese PA, Lepore MJ. Involvement of abdominal organs in cystic fibrosis of the pancreas. Gastroenterology 1961; 40:64).Pancreatitis came to be recognised as a complication in people with CF who were “pancreatic sufficient” i.e. had at least 10% residual pancreatic function and did not require pancreatic enzyme treatment to prevent intestinal malabsorption. Subsequently, after the gene had been identified, a higher than expected number of non-CF people with pancreatitis were found to have one CF mutation (Sharer et al, 1998 below; Cohn et al, 1998 below).
1975 Elliott RB, Robinson PG. Unusual course in a child with cystic fibrosis treated with fat emulsion. Arch Dis Child 1975; 50:76-78.[PubMed]
A child with CF received regular intravenous infusions of soya oil emulsion from the first weeks. The authors state that “Sweat tests improved, pancreatic achylia was relieved and the child at present remains entirely well. Correction of the fatty acid abnormality found in cystic fibrosis may prevent some of the manifestations of the disease”.Elliott and colleagues from Auckland, New Zealand published several papers on this subject the first showing improvement in the clinical state with supplements of medium chain triglycerides even to the extent of returning the sweat electrolytes to nearer normal values (Elliott RB. Aust Paediatr J 1972; 8:217; Elliot RB. 1976; 57:474-479). Unfortunately, subsequent studies failed to substantiate their earlier findings (Davidson GP et al. Aust Paediatr J 1978; 14:80-82. ; Chase et al. Pediatrics 1979; 59:428-432 below).
1975 Feigelson J, Sauvegrain J. Gastro-esophageal reflux in mucoviscidosis. Nouvelle Presse Medicale 1975; 4: 2729-2730. [PubMed]

Fig. 42 Jean Feigelson Author’s photo
This is the possibly first description of significant gastroesophageal reflux in people with CF detected on radiological examination in 56 patients aged four months to 27 years and showed that 26 (46%) had significant gastro-oesophageal reflux. Attention was drawn to this complication and its effects both on the oesophagus and the respiratory system.Subsequently gastro oesophageal reflux was recognised as a frequent and important complication in people with CF of all ages. There was to be continuing interest in GO reflux both in infants (Malfroot & Dabb, 1991 below) and in relation to physiotherapy practices in CF infants (Button et al, 1997 below); also in adults where GO reflux was shown to be frequent and important in exacerbating respiratory symptoms (Scott RB et al, 1985 below; Ledson MJ et al, 1998 below) and particularly in relation to patients after lung transplantation (Button BM et al. J Heart Lung Transplant 2005; 24:1522-1529. [PubMed]). Newer techniques of oesophageal pH monitoring and also fibreoptic endoscopy during the Eighties allowed more frequent recognition and more accurate diagnosis.
1975 Berry HK, Kellog FW, Hunt MM, Ingberg RL, Richter L, Gutjahr C. Dietary supplement and nutrition in children with cystic fibrosis. Am J Dis Child 1975; 129:165-171. [PubMed]
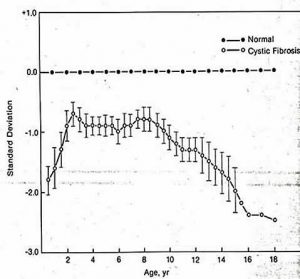
Fig 43. Weight progress of children with cystic fibrosis
Fifteen patients improved over 1 year with the Allan Diet (beef serum hydrolysate, glucose polymer and MCT) with >0.5 SD gain in weight, increase in clinical scores and serum albumin and drop in white blood count. The authors commented that “Changes that occurred following the use of the nutritional supplement are in sharp contrast to our earlier attempts to induce weight gain in patients with CF”. (also Allan et al, 1973 above; Yassa et al, 1979 below).Nonetheless this depressing weight chart (fig.43) shows the typical weight progress of children with CF at the time showing the inexorable decline from the age of 10 years as the chest infection worsened.
1975 Wood RE, Wanner A, Hirsch J, Farrell PM. Tracheal mucociliary transport in patients with cystic fibrosis and its stimulation by terbutaline. Am Rev Respir Dis 1975; 111:733-8.[PubMed]
Robert Wood observed the movement of Teflon discs passing up the trachea through a bronchoscope in 14 adults with cystic fibrosis. The discs moved at 2.6 mm/min in CF and 20.1 mm/min in controls; terbutaline increased the speed of movement in CF to 5.5mm/min. The authors speculated, correctly as it has now become apparent, that this “may play a role in the pathogenesis of pulmonary disease”.Robert Wood pioneered fibreoptic bronchoscopy in children with CF. The 3.5mm paediatric version of the bronchoscope he used in 1975 had no suction port which he circumvented by attaching a fine Teflon tube to the side allowing its use in children down to the age of 18 months; the instrument was developed by the Olympus Corporation into the first flexible pediatric bronchoscope in 1978 at Dr Wood’s request.
1975 Feigelson J, Pecau Y, Cathelineau L, Navarro J. Additional data on hepatic function tests in cystic fibrosis. Acta Paediatr Scand 1975; 64:337-344. [PubMed]
Fig. 44 Jean Navarro
An early contribution (of many over the years) from Jean Feigelson of Paris who must have attended every CF meeting since they started! Since the early Sixties Jean Feigelson has published on a wide range of CF topics, usually based on long personal experience, but unfortunately often for the non-linguists in French journals! In this paper he describes 9 of 50 patients with CF reported who had multilobular cirrhosis observed for 3 years.
The last author on this paper, Professor Jean Navarro (fig. 44), subsequently published many papers on CF, often in French, from Paris and became a leading researcher and clinician in both CF and paediatric gastroenterology and also in various leading roles in the French national CF organisation – Association Vaincre la Mucoviscidose.
1975 Antonowicz I, Ishida S, Shwachman H. Studies in meconium: Disaccharidase activities in meconium from cystic fibrosis patients and controls. Pediatrics 1975; 56:782-787. [PubMed]
The enzymatic activities of disaccharidases in meconium from infants with CF and controls were found to be significantly increased in the infants with CF. The test was suggested as an alternative method for screening for CF or a method of interpreting borderline BM tests but the test did not become widely used and interest soon waned.
1975 Stephan U, Busch E-W, Kollberg H, Hellsing K. Cystic fibrosis detection by means of a test strip. Pediatrics 1975; 55:35-38. [PubMed]
The main review of the results of neonatal CF screening at various European centres by detecting raised levels of albumin in the meconium. The test was later abandoned on the grounds of an unacceptable number of false positives and negatives. This paper reports the results of the BM-Test Meconium applied to (approximately) 69,000 meconium specimens and the detection of 60 infants with CF – but some were known high risk infants; also three of 14 neonates with subsequently proven CF had negative albumin tests.This is really an anecdotal study and as described in this paper is quite difficult to follow. BM screening was evaluated in Wales and abandoned on the grounds of an unacceptable false negative rate (Prosser et al. 1974 above; Bray et al, 1979 below). However, it is likely that their poor results in Wales were related to the tests being carried out (or perhaps not being carried out!) by the midwives on the wards. The practicalities of busy midwives being responsible for carrying out these tests on meconium in the maternity unit were a major problem.
However, at St Mary’s Maternity Hospital in Leeds, where we had 3000 births per year in the Seventies, we used the BM test with success from 1975 for many years. However we found the test useful only because our laboratory kindly agreed to do the tests on small specimens of meconium sent to them rather than asking the overworked midwives to perform the tests on the wards (Evans et al, 1983 below). Neonatal screening for CF was delayed until 1995 in the other major maternity unit in Leeds as the two paediatricians responsible for neonatal care were opposed to it.
1975 Oppenheimer EH, Esterly JR. Pathology of cystic fibrosis. Review of the literature and comparison with 146 autopsied cases. Perspect Pediatr Pathol 1975; 2:241-278. [PubMed]
A classic detailed review of current knowledge of the pathology of cystic fibrosis and a major source of references on the pathology of the condition up to that time and since, for present day autopsy data in children with CF is now rare as it is unusual for children with CF to die.Ella Oppenheimer and John Esterly made major contributions to the pathology of CF with numerous publications on the subject. While attributing the term “mucoviscidosis” to Farber (1944 above), they preferred the term “cystic fibrosis of the pancreas” as the condition is not restricted to the mucus-secreting glands. Three basic observations on the pancreatic changes are there is a spectrum of changes, diagnostic lesions may be absent irrespective of age and there is usually a direct correlation with age and severity of the lesions. Focal biliary cirrhosis was found in 19% of this series. In newborns there is hyperplasia and obstruction of the submucosal glands of the trachea and major bronchi before any infection has occurred.
A quite magnificent paper – apart from the rather surprising incorrect spelling of Dorothy Andersen’s name throughout (as Anderson!). But they are not alone – one distinguished editor of a leading paediatric journal is also guilty!
1975 Sarsfield JK, Davies JM. Negative sweat tests and cystic fibrosis. Arch Dis Child 1975; 50:463-466. [PubMed]

Fig.46 John Davies

Fig. 45 Jim Sarsfield Author’s photo
This paper is included as it was the first publication on CF from our general paediatric unit at Seacroft Hospital, Leeds where I had enlisted the out patient clinic sister (senior nurse), dietitian and physiotherapist to join me in a small monthly CF clinic in 1975; following this there was an increasing interest in CF at the hospital. Dr John Davies, (fig. 46) our senior paediatric registrar at the time, had developed stimulated pancreatic function tests on the lines recommended by Hadorn et al (1968 above), and reliable sweat tests had been available since the mid-Sixties performed by Mr. Alan Steele the biochemist; the latter service was used by many of the paediatricians in the Yorkshire Region from the mid-Sixties. Undoubtedly the small clinic, neonatal CF screening, the reliable sweat tests and the pancreatic function tests were significant factors in the development of the Leeds Regional CF Service. Dr Jim Sarsfield (Fig. 45) was working in the Leeds University Department of Paediatrics and Child Health at this time and later became consultant Paediatrican in Harrogate, Yorkshire. Dr John Davies became a consultant paediatrician in Grimsby.
This report is of two brothers with chronic suppurative pulmonary disease; one had classical CF with complete pancreatic involvement and abnormal sweat tests. The other had incomplete pancreatic disease and repeatedly normal sweat tests. With these findings it was concluded that ”undue reliance on the sweat tests, especially when used for exclusion of cystic fibrosis, may be misplaced”.Subsequently there have been many reports of patients with CF who had normal sweat tests some of whom have had unusual so-called “mild” mutations. Also, a more recent review of sweat tests in infants with CF diagnosed by neonatal screening, has shown that some CF infants do indeed have a sweat test within the normal range for some time (Massie J et al. Pediatr Pulmonol 2000; 29:452-456.[PubMed]).
1975 Vagenakis AG, Braverman LE. Adverse effects of iodides on thyroid function. Med Clin N Am 1975; 59:1075-1088. [PubMed]
The administration of pharmacologic quantities of iodine as iodides for the treatment of pulmonary disease may result in goitre, hypothyroidism, or hyperthyroidism, especially in patients with underlying thyroid disease. The aetiology of iodide-induced goiter and hypothyroidism in patients with cystic fibrosis treated with iodides was unclear.The use of iodides to reduce sputum viscosity was common practice and is mentioned by a number of authors including Shwachman who mentioned their use as helpful in a number of his review articles. In a subsequent report from Shwachman and colleagues (Segall-Blank, M et al, Thyroid gland function and pituitary TSH reserve in patients with cystic fibrosis. J Pediatr 1981; 98:218-222) they state that, in view of the reported enhanced sensitivity to iodide-induced hypothyroidism in patients with cystic fibrosis, studies were carried out to determine the possible mechanism of this abnormality. But their findings did not delineate the mechanism whereby patients with CF develop iodide-induced hypothyroidism (also Ruben et al, 1960 above; Dolan & Gibson, 1971 above). (see Endocrine Topic).
1975 Goodchild MC, Murphy GM, Howell AM, Nutter SA, Anderson CM. Aspects of bile acid metabolism in cystic fibrosis. Arch Dis Child 1975; 50:769-777. [PubMed]
A detailed study by Mary Goodchild (who later moved to head the Cardiff Paediatric CF Unit) from Charlotte Anderson’s unit in Birmingham. Most children with CF had raised faecal bile acid levels which did not correlate with fat excretion but there was an inverse relationship with age.The authors suggested that chronic bile acid loss may eventually deplete the bile acid pool – which was in fact the case. Studies from Prof. Roy’s unit in Montreal also showed a much increased faecal loss of bile acids in children with cystic fibrosis (Weber et al, 1973 above; Roy et al, 1977 below).
1975 Baran D, Dachy A, Klastersky J. Concentration of gentamicin in bronchial secretions of children with cystic fibrosis and tracheostomy. (Comparison between the intramuscular route, the endotracheal instillation and aerosolization). Int J Clin Pharmacol 1975; 12:336-341. [PubMed]

Fig 47. Professor and Mrs. Baran at the 2009 ECFS meeting. Author’s photo
Gentamicin levels in blood and bronchial secretions were measured after 40 mg were directly instilled or given by aerosol. High levels (> 20 mug/ml) were achieved, much greater than after intramuscular injection (< 2 mug/ml); low plasma levels were found by both direct methods. It was concluded that administration of an antibiotic such as gentamicin directly into the trachea by endotracheal injection or by aerolization might prove to be helpful when infection is confined mainly to the tracheobronchial tree. Gentamicin had become available in 1968.
Professor Baran (fig. 47) of Brussels has been involved in CF care and research from the Seventies. This was an important early paper providing evidence of the impressive effect of inhaled aminoglycosides which presumably influenced the use of inhaled aminioglycosides including Margaret Hodson’s important report on the use of inhaled gentamicin and carbenicillin in stabilising patients with chronic P. aeruginosa infection (Hodson et al. 1981 below).
1976 McCrae WM, Raeburn JA, Hanson EJ. Tobramycin therapy of infections due to Pseudomonas aeruginosa in patients with cystic fibrosis: effect and dosage and concentration of antibiotic in sputum. J Inf Dis 1976; 134 Suppl: S191-193. [PubMed]
Fig 48. Morris McCrae
An early report of Pseudomonas aeruginosa infection treated in 17 patients with conventional and larger than conventional doses

Fig 49. Sandy Raeburn
of intravenous tobramycin. Infection was eradicated in four and it appeared that treatment was most successful in those on the highest doses (12mg/kg/day) who achieved the highest peak serum values than in those on conventional doses (5mg/kg/day). Most paediatricians were not using IV tobramycin for P. aeruginosa at this time although there had been one previous report using conventional doses (Hawley HB et al. Curr Ther Res 1974; 16:414-415) and a subsequent one using conventional doses plus carbenicillin – the latter both IV and inhaled (Crozier DN, Khan SR. J Inf Dis 1976; 134:187-190.[PubMed])
This paper from Morrice McCrae (fig. 48) and Sandy Raeburn (Fig. 49) the physician looking after adults with CF in Edinburgh at the time, was the first to suggest that higher doses of IV tobramycin were required for people with CF. Apparently intravenous gentamicin (available since the late Sixties) with carbenicillin had proved disappointing (Marks MI et al. J Pediatr 1971; 79:822-828; Huang NN et al. J Pediatr 1971; 78:338-345).
1976 Warner JO, Taylor BW, Norman AP, Soothill JF. Association of cystic fibrosis and allergy. Arch Dis Child 1976; 51:507-11.[PubMed]

Fig 49a. John Warner. imperial.ac.uk
A number of previous studies had shown an increased prevalence of atopy in people with cystic fibrosis. In this study John Warner (Fig 49a) and colleagues from London confirmed this association. Immediate skin hypersensitivity was present in 59% of 123 children with CF – a much higher incidence than normal. Also atopy was more frequent in the obligate heterozygotes. Allergic children with CF tended to have a worse respiratory state. The authors suggested that the increase in allergypossibly was related to impairedhandling of antigen at mucosal surfaces.
One of many studies on allergy and cystic fibrosis which, other than the major problem of adverse reactions to antibiotics, never seemed to have a great influence on clinical management other than the reactions to Aspergillus fumigatus.
1976 Stapleton FB, Kennedy J, Nousia-Arvanitakis S, Linshaw MA. Hyperuricosuria due to high-dose pancreatic extract therapy in cystic fibrosis. N Eng J Med 1976; 295:246-248. [PubMed]
A child with CF developed dysuria with a normal serum uric acid level. Hyperuricosuria in this and two people with CF was related to ingestion of large doses of pancreatin (Cotazym powder). Symptoms settled with reduction of the pancreatin intake. Later this group suggested reducing fat intake to lessen the need for high doses of pancreatic enzymes (Nousia-Arvanitakis S et al, J Pediatr 1977; 90:302-305).Subsequent studies discussed the relationship to renal stones.Although with modern pancreatic enzymes the problems with hyperuricosuria seem to have regressed there was a recent report from Manchester Adult CF Centre showing nine patients (2.5%) had gout and approximately 35% of patients had serum uric acid levels above the normal limits (Horsley A et al. J R Soc Med 2011; 104 Suppl 1:S36-39.[PubMed]) – the first report of gout in people with CF. However, renal stones still appear to be relatively common in people with cystic fibrosis – in one report they were present in 21% of patients (Terribile M, et al. Nephro Dial Trans 2006; 21:1870-1875). There is some evidence that kidney stones may be more common in CF patients because of increased levels of oxalate chemicals absorbed through the bowel wall into the blood and subsequently excreted through the kidney. These oxalates can be concentrated in the urine and precipitate out to form small stones.
1976 Stern R, Boat TF, Doershuk CF, Tucker AS, Primiano FP Jr, Matthews LW. Course of cystic fibrosis in 95 patients. J Pediatr 1976; 89:406-411. [PubMed]

Fig 50. The team at the Rainbow Babies and Children’s Hospital Pulmonary Faculty in 1980. (L.to R.) Robert Wood, David Orenstein, Leroy Matthews, Carl Doershuk, Dave Dearborn, Thomas Boat, Robert Stern.
The team from The Rainbow Babies and Children’s Hospital PulmonaryFaculty 1980 reporting the results of their comprehensive system of management (Matthews et al. J Pediatr 1964; 65:558-575. above).
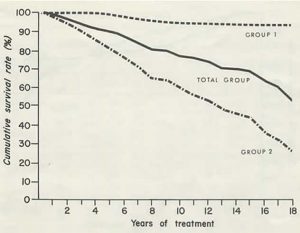
Fig 51. Survival curves Group 1. before extensive lung damage. Group 2 diagnosed only after substantial lung damage
These were the 95 patients they reported in 1964 now after a mean follow up period of 14 years (minimum 13 years). Of the 45 diagnosed before extensive lung damage (figure 25. Group1) only one had died and none were disabled. Of the other 50 diagnosed after substantial lung damage (figure 25. Group 2) 26 had died – mortality being greater in females.Factors contributing to better prognosis were considered to be early diagnosis, aggressive management and comprehensive care, easy access to specialised care and improved antibiotic therapy. The further observations of this group on achieving successful treatment include – early inpatient treatment before significant lung damage in optimal facilities, as and when needed with flexible arrangements for daily absences, outpatient appointments throughout the week including Saturdays. Follow-up exclusively by a centre physician – usually the same physician each visit. All decisions are made by a CF centre physician.
1976 Abernathy RS. Bulging fontanelle as a presenting sign in cystic fibrosis. Am J Dis Child 1976; 130:1360-1362. [PubMed]
A five month old infant whose sole problem was a bulging fontanelle was confirmed as having CF and low vitamin A levels. (Bulging anterior fontanelle also reported in CF by Keating & Feigin, 1970 above; also after tetracycline administration Krewsky S. Michigan Med 1968; 67:597-598; also with nalidixic acid Drigo P et al. Pediatr Medic Chirurg 1983; 5:583-585). Benign intracranial hypertension in infants may be unexplained and resolve spontaneously.
1976 Lawson D, Porter J. Serum precipitins against respiratory pathogens in 522 normal children and 48 cases of cystic fibrosis treated with cloxacillin. Arch Dis Child 1976; 51:890-891. [PubMed]
Since 1964 David Lawson had treated all children with CF with a long term anti-Staphyloccocal antibiotic – cloxacillin. He had monitored their serum precipitins since 1968 and compared the results to those of a normal population of 522 children none of whom had S. aureus precipitins in the first 4 years. (Also similar work was reported by Strandvik et al, 1990 below). The findings indicated that the development of precipitins could be prevented by continuous cloxacillin.So here David Lawson provides further supportive evidence for long term anti-Staphylococcal therapy; he was definitely “the father” of long term prophylactic anti-staphylococcal therapy although Nancy Huang also reported the use of long term oxacillin (Huang NN et al, 1963 above). Long term term flucloxacillin is now recommended in the UK by the CF Trust’s Antibiotic Group (2002 & 2009) – at least for the first 3 years. This recommendation is supported by the trial reported by Weaver et al, 1995 (below) and clinical experience of a low incidence of chronic S. aureus infection in patients on long term flucloxacillin (Southern et al, 1993 below).
It has been our practice in the Leeds clinic to give lifelong cloxacillin and later flucloxacillin since soon after this paper of David Lawson’s was published in 1976. Certainly the frequency of isolation of S. aureus falls when taking continuous flucloxacillin – in the Leeds clinic overall prevalence of chronic S. aureus infection was 14% and in children under 10 years only 8.3% (Southern KW et al. In Clinical Ecology of Cystic Fibrosis Escobar C et al. (eds.).Elsevier Scientific Publishers, 1993). In contrast, in the 2010 CF Foundation Registry no less than 67% of patients cultured positive for S. aureus.
1976 Mitchell-Heggs P, Mearns M, Batten JC. Cystic fibrosis in adolescents and adults. Q J Med 1976; 45:479-504. [PubMed]
The first report from Europe of 45 patients over 12 years from Sir John Batten’s adult CF unit at the Brompton Hospital, London. The mean age at first visit to the adult clinic was 17 years and the patients were followed for an average of 4 years. Most had been cared for previously at paediatric units in London by Drs Winifred Young, Margaret Mearns, Richard Dobbs, Archie Norman and David Lawson. Thirty two (71%) already had severe lung disease. All had cough and sputum, 23 had haemoptysis and 8 pneumothorax. Forty three (96%) were considered to be pancreatic insufficient although 5 had stopped enzyme supplements apparently without problems. Only three had diabetes mellitus.This is a detailed paper of experience at the Brompton Hospital of the management and physical state of CF adults in the mid-Seventies and a review of previous reports of adults with CF from the first of McIntosh (1954 above) from New York. The survival of some of these patients suggest that they may have had “mild” mutations – hence the ability to stop pancreatic extracts without problems may indicate some of these patients were pancreatic sufficient. In some of the earlier reports of adults with CF, the late age of presentation and diagnosis certainly suggests that some may have had milder mutations.
1976 Wood RE, Boat TF, Doershuk CF. State of the Art. Cystic Fibrosis. Am Rev Respir Dis 1976; 113:833-878. [PubMed]

Fig 53. Thomas Boat

Fig 52. Robert Wood
Dr Robert Woods (fig. 52) provides an excellent very detailed review (with 500 references) of the situation in 1976 in the USA when the 50% median survival there was 15 years. The discussion of mist tent therapy, which was falling out of favour at the time, was particularly interesting. Woods mentions that early studies were encouraging (Doershuk et al, 1968 above; Matthews et al, 1967 above) but later studies had not shown a beneficial response (Motoyama et al, 1972 above; Chang et al, 1973 above). However, although studies of radioactive aerosols showed little radioactivity in the lungs (Wolsdorf J et al. Pediatrics 1969; 43:799; Bau SK, et al. Pediatrics 1971; 48:605), Woods suggests that significant deposition may have been masked by the rapid absorption of the radioactive aerosol which was known to occur. He questioned the techniques used in some of the aerosol studies and noted that, at bronchoscopy, he had observed large amounts of mist particles reaching at least the subsegmental bronchi even during nasal breathing. In fact he considers it possible that the radioactivity at any particular site may bare little relation to the amount of fluid deposited.The implication of these observations was that the final word had not been said on mist tent therapy. This is all particularly relevant now in view of the present belief that the low salt theory and drying of the epithelial surfaces accounts for the increased viscosity and easy tendency to infection within the airways. It is worth recalling that highly experienced clinicians such as Shwachman, di Sant’Agnese and particularly Leroy Matthews were impressed by the benefits of mist tent therapy as were some patients who took part in the Toronto studies (Chang et al. 1973). More recently inhaled hypertonic saline has shown significant benefit although administered via a conventional nebuliser rather than in a tent (Elkins et al. 2006 below).
Dr Robert E Wood (fig.52), is a pediatric pulmonary specialist at Cincinnati Children’s Hospital, with particular interest in bronchoscopy having played a major role in the development of flexible bronchoscopy in pediatric patients. He is recognized as a teacher of endoscopic techniques. Also he has extensive experience with clinical problems in pediatric pulmonary medicine, especially children with complex airway problems and cystic fibrosis. Before coming to Cincinnati Children’s Hospital Medical Center, Dr. Wood was on the faculty of Case Western Reserve University in Cleveland, Ohio (1976 to 1983), and the University of North Carolina at Chapel Hill (1983 to 1999).
Dr Thomas Boat (fig. 53) is now dean of the University of Cincinnati College of Medicine and vice president for health affairs. From 1993 to 2007, he served as director of the Cincinnati Children’s Research Foundation and chairman of the UC College of Medicine’s Department of Pediatrics. He also has served as physician-in-chief of Cincinnati Children’s Hospital Medical Center having previously worked at North Carolina and Cleveland. He has had extensive involvement in national medcial affaires and committees.
1976 Robinson PG, Elliott RB. Cystic fibrosis screening in the newborn. Arch Dis Child 1976; 51:301-304. [PubMed]
Using a method of measuring the stool enzyme activity (chymotrypsin) in dry faecal specimens from newborn infants, three infants with CF were detected. The test was proposed as suitable for neonatal CF screening and the specimens could be sent to the laboratory by post. However, the test was soon to be replaced by the blood immunoreactive trypsin test developed in the same Auckland laboratory (Crossley et al, 1977 below; Crossley et al, 1979 below).
1976 Hodson ME, Mearns MB, Batten JC. Meconium ileus equivalent in adults with cystic fibrosis of pancreas: a report of six cases. BMJ 1976; 2:790-791. [PubMed]
Eleven episodes of meconium ileus equivalent (MIE) are described in six adult patients, four of whom were diabetic. Three were surgically treated with one fatality and there were two serious postoperative complications. Treatment with intravenous fluids, nasogastric suction, enemas and oral acetylcysteine was recommended followed by maintenance treatment with oral acetylcysteine.A repeated complaint of CF physicians was of people with CF being admitted with acute gastrointestinal symptoms to a general surgical unit and undergoing unnecessary operations as the staff were unfamiliar with this condition.
The report of the use of gastrografin for the treatment of MIE from the Liverpool CF unit had not yet been published when this report was written (O’Halloran SM et al. 1986 below). It is perhaps relevant that four of the six patients were diabetic and possibly could have been subclinically slightly dehydrated. Later work suggested that a positive effort to increase hydration by drinking more water significantly reduced the incidence of meconium ileus equivalent in people with cystic fibrosis (Obideen et al, 2006 below). Meconium ileus equivalent (MIE) later became referred to as the distal intestinal obstruction syndrome (DIOS).
1976 Dolan TF. Hemolytic anemia and edema as the initial signs in infants with cystic fibrosis. Clin Pediatr 1976; 15:597-600. [PubMed]
Much of the interest in vitamin E up to this time had been in premature infants. Three of the 5 infants with CF in this report had low vitamin E levels, all had haemolytic anaemia and marked reticulocytosis. The author notes that although low levels of vitamin E had been described in CF (Blanc WA et al. Pediatrics 1958; 22:494) no clinical deficiency states had been described. (Review of “The occurrence and effects of human vitamin E deficiency” by Philip Farrell J Clin Invest 1977; 60:233-241. below).
1977 Lararya-Cuasay LR, Lipstein M, Huang NN. Pseudomonas cepacia in the respiratory flora of patients with cystic fibrosis. Pediatr Res 1977; 11:502.
One of the earliest reports of Pseudomonas cepacia (later called first Burkholderia cepacia and then Burkholderia cepacia complex) isolated between 1973 and 1976 from 54 patients with cystic fibrosis; many were severely affected and 14 died. The presence of the organism made treatment more difficult.This was a very early report of P. cepacia which, surprisingly, did not appear to cause concern at the time – in fact, even in John Lloyd-Still’s 1983 Textbook of Cystic Fibrosis there is very brief mention of P. cepacia as one of the “other gram-negative rods that may infect people with cystic fibrosis”. Later Rosenstein & Hall reported pneumonia and septicemia due to Pseudomonas cepacia in a patient with CF (Johns Hopkins Med J 1980; 147:188-189) before the first report from Toronto describing major problems in treating the infection (Gold R et al. J Antimicrob Chemother 1983; 12 Suppl A: 331-336) and before the other major publication from Toronto (Isles A, et al. Pseudomonas cepacia infection in cystic fibrosis: an emerging problem. J Pediatr 1984; 104:206-210 below).
The first report from the UK was from our Leeds centre and did not appear until 1990 when we had identified 11 affected patients since 1984 (Simmonds EJ et al. Arch Dis Child 1990; 65:874-877 below).
The tendency for B. cepacia to spread between patients was not generally accepted in the UK until 1993 when John Govan from Edinburgh published definite evidence of patient to patient spread (Govan et al, 1993 below).
1977 Gayton WF, Friedman SB, Tavormina JF, Tucker F. Children with cystic fibrosis: I. Psychological test findings of patients, siblings, and parents. Pediatrics 1977; 59:888-894.[PubMed]
One of the early papers on the psychological aspects of cystic fibrosis. Not surprisingly, in 43 families both fathers (32%) and mothers (22%) had scores in the range suggestive of emotional disturbance – in terms of decreased family satisfaction and family adjustment. The results did not support previous estimates of an increased incidence of emotional disturbance in children with cystic fibrosis nor in siblings of affected children.
1977 Geller A, Gilles F, Shwachman H. Degeneration of the fasciculus gracilis in cystic fibrosis. Neurology 1977; 27:185-187. [PubMed]
Nineteen percent of 106 of the spinal cords of patients dying with CF after the age of five showed posterior column degeneration. None of the patients had been anaemic or had spinocerebellar degeneration. Nutritional, toxic or hereditary factors were considered as possibly responsible. This possibility seems to have received little attention in recent years.Later Cavalier SJ & Gambetti P.(Neurology 1981; 31:714-718. [PubMed]) reviewed 43 autopsy cases of CF and found 66% had developed dystrophic axons; neuroaxonal dystrophy correlated with the duration of the disease. Demyelination of the fasciculus gracilis occurred in 11%. They said the neuropathology of CF resembled that of vitamin E deficiency in animals but vitamin E replacement had failed to prevent the neuropathology changes in these patients.
1977 Roy CC, Weber AM, Morin CL, Combes JC, Nussle D, Megevand A, Lasalle R. Abnormal biliary lipid composition and cystic fibrosis. N Eng J Med 1977; 297:1301-1305. [PubMed]
Fig. 54 Claude Roy
Early description of the abnormal bile composition in CF from Prof. Roy’s unit in Montreal (fig.54) where there was a particular interest in paediatric liver disease. Cholesterol was similar to that of patients with cholelithiasis; also there were abnormal glycine/taurine ratios that improved with pancreatic enzymes (also Weber et al, 1973 above; Goodchild et al, 1975 above).
1977 Farrell PM, Bieri JG, Fratantoni JF, Wood RE, di Sant’Agnese PA. The occurrence and effects of human vitamin E deficiency. J Clin Invest 1977; 60:233-241.[PubMed]
A detailed review of the subject by Phillip Farrell . All 52 CF patients with pancreatic insufficiency were deficient in vitamin E. Hydrogen peroxide induced haemolysis was increased and red cell survival of 15Cr-labelled erythrocytes was significantly decreased but was corrected by vitamin E. The authors concluded that “concomitant effects consistent with mild haemolysis but not anaemia occur and may be reversed with vitamin E therapy”. Daily doses of water soluble vitamin E were recommended for people with cystic fibrosis.
In a subsequent study from Leeds the mean haemoglobin was significantly increased with vitamin E treatment in the children with CF with long-standing low vitamin E levels from 13.14 g/100ml to 13.47g/100ml. 21 of 30 patients showed some increase; in eight from 0.1-0.5 g/100ml, in 9 from 0.51-1.0 while 4 showed increases of 1.2, 1.8, 1.9 and 2.3 g/100ml. These increases correlated with the increases in vitamin E levels (Kelleher J et al. Internat J Vit Nutr Res 1987; 57:253-259.[PubMed]). No change was seen in haemoglobin with treatment in this series of Phillip Farrell’s as, although the children had low vitamin E levels, they were not anaemic – Hb14.3g/100ml
1977 Khaw KT, Adeniyi-Jones S, Gordon D, Polombo J, Suskind R. Efficacy of pancreatin preparations on fat and nitrogen absorptions in cystic fibrosis. Pediatr Res 1978; 12:437.
An early report of the marked superiority of Pancrease over currently used enzymes at the time. Pancrease consisted of acid resistant micro spheres which only released their enzymes when they reached the more alkaline environment of the upper intestine, thus protecting their active enzyme contents from destruction by the gastric acid. Viokase and Cotazym were the standard enzyme preparations in use at the time both of which were affected by gastric acid. Twelve children with CF aged eight to 14 years took Viokase four, eight or 12 tablets, Cotazym two, four or six capsules and Pancrease one, two or three capsules per meal. All three preparations improved absorption compared with placebo but Pancrease did so at the much smaller dose. Viokase 12 capsules per meal and Pancrease 3 capsules per meal achieved 94% and 94,.8 % fat absorptiion respectively. Similarly six Cotazym and three Pancrease capsules achieved 84.2% and 89.7% fat absorption respectively (also Weber et al, 1979 below).The acid resistant microspheres were undoubtedly one of the major nutritional advances, when gradually introduced during the early Eighties allowing most patients to take a normal fat intake and hence significantly improve their energy intake. The markedly better absorption of fat and protein was shown in all subsequent trials and the reduction in the patients’ unpleasant bowel symptoms and fat intolerance in many was quite dramatic.
1977 Scott J, Elias E, Moult PJA, Barnes S, Wills MR. Rickets in adult cystic fibrosis with myopathy, pancreatic insufficiency and proximal renal tubular dysfunction. Am J Med 1977; 63:488-492.[PubMed]
One of the very few reports of rickets in a white man aged 19 years with CF in whom pancreatic and hepatic involvement was advanced. It was suggested that vitamin D malabsorption occurred due to gross bile salt deficiency due to the known increased bile acid loss in association with pancreatic steatorrhoea. There was evidence of secondary hyperparathyroidism with proximal renal tubular acidosis, aminoaciduria, phosphaturia and hypophosphatemia which may have accelerated the rachitic syndrome. Treatment with oral pancreatic and parenteral vitamin D supplements led to full recovery of the rachitic syndrome and the proximal renal tubular dysfunction.
1977 Hoiby N. Pseudomonas aeruginosa infection in cystic fibrosis. Diagnostic and prognostic significance of Pseudomonas aeruginosa precipitins determined by means of crossed immunoelectrophoresis. Acta Pathol Microbiol Immunol Scand 1977; Supplement (262): 1-96. [PubMed
One of a number of important papers from Niels Hoiby expanding his 1973 results (Hoiby 1973 above). Correlating the clinical condition and microbiological status with the antibodies undoubtedly confirmed the importance of P. aeruginosa.
This early study was important as, surprisingly, some clinicians (usually paediatricians as there were still few adults with CF) still doubted the importance of, and therefore the need to treat, P. aeruginosa infection. A typical comment at the time was “it is not obvious whether Pseudomonas aeruginosa causes increased degenerative lung disease or whether increased degenerative lung disease provides a milieu in which P. aeruginosa may prosper”.
This and other publications from Copenhagen stimulated me to organise Pseudomonas antibody studies in Leeds for which, thanks to funding from the UK CF Trust, we appointed an immunologist, Dr Moira Brett to develop the service. From the mid-Eighties, these Pseudomonas ELISA tests, which Moira Brett developed, have been used, in addition to cultures, to follow Pseudomonas infection. They have been used in the Leeds CF clinics continuously since 1986 (Brett MM et al, 1986 below) until recently when they were replaced by a commercial test. It is surprising that this very valuable test is not more widely used in the UK as persistent absence of an immunological response almost certainly means that the lower respiratory tract is not infected with Pseudomonas; also a rising antibody titre suggests deterioration of the chest due to worsening of the Pseudomonas infection in those patients already chronically infected and indicates the need for more aggressive anti-Pseudomonal therapy even if symptoms and signs are few.
1977 Crossley JR, Berryman CC, Elliott RB. Cystic fibrosis screening in the newborn. Lancet 1977; ii: 1093-1095.[PubMed]
Screening the stools of newborn infants for low trypsin content indicated the possibility of their having cystic fibrosis. Trypsin releases a yellow colour with benzyl-arginine-p-nitroanilide. The same group in Auckland later described the immunoreactive trypsin test (IRT) performed on Guthrie blood spots – this latter proved to be a major advance in neonatal CF screening (see Crossley et al, 1979 below; also Robinson & Elliott, 1976 above) and the test was subsequently adopted around the world for neonatal CF screening.
1978 Bray PT, Clark GC, Moody GL, Thomas G, Thomas JD. Sweat testing for cystic fibrosis. Diagnostic screening with a combination chloride ion-selective electrode. Arch Dis Child 1978; 53: 483-486. [PubMed]
Fig 55. Percy Bray testing a newborn for CF with a chloride electrode
Screening of newborns using an Orion Skin Chloride Measuring System incorporating some innovations. There were a number of potential possibilities for errors with this test (Bray PT et al. Clin Chem Acta 1977; 80:333-338) and it was never introduced into routine care. There was more interest in Meconium screening at the time in Wales.
Dr Percy Bray (fig. 55) was a leading figure in Welsh paediatrics and involved with CF care in Cardiff up to the late Seventies when John Dodge took over the CF clinic in Cardiff. Apparently Percy Bray’s interest in CF started at the end of the second world war when he and Archie Norman worked with Dr Donald Patterson at Great Ormond Street Hospital, London. On his retirement in 1977 he was appointed as Professor of Paediatrics in Kuala Lumpur.
John Dodge has described the early development of CF services in Wales and Percy Bray’s and his own role (Dodge JA. Cystic fibrosis in Wales. Welsh Paed J 1989; 1:4-6.).
1978 Bureau MA, McDougall DM, Beaudry PH, Belmonte MM. Late effects of nocturnal mist tent therapy related to the severity of airway obstruction in children with cystic fibrosis. Pediatrics 1978; 61:842-846. [PubMed]
A study from Montreal to evaluate the long-term effect of nocturnal mist tent therapy on the progression of airway obstruction in children with CF of varying severity. Two matched groups each consisting of 24 children with CF were studied during 18 months on mist tent therapy and 18 months off therapy. The mist therapy failed to benefit any of the groups of children with CF who had early, moderate, or advanced airway obstruction as judged from their respiratory function tests (MMEF values).
The authors concluded that nocturnal mist tent therapy neither decreases airway obstruction nor prevents its progression in children with cystic fibrosis. The authors mention these are similar findings to those of Jehanne M et al, (Ann Pediatr 1974; 21:595) extending for up to 2 years. Other studies failed to confirm benefit from nocturnal mist tent therapy (Bay et al. 1971; Norman & Hall. 1971; Moyatama et al, 1972; Chang et al 1973 – all above).
1978 Erkkila JC, Warwick WJ, Bradford DS. Spine deformities and cystic fibrosis. Clin Orthop Relat Res 1978; 131:146-150. [PubMed]
Of 203 patients with CF 21.5% had more than 35 degrees of kyphosis – the prevalence increasing with age. The prevalence of significant scoliosis with curves greater than 10 degrees was similar to the general population. (Kumar N, et al. 2004 below found an increased prevalence of 15.6% of scoliosis in Leeds patients – some 20 times expected in people of similar age).
1978 Kraemer R, Rudeberg A, Hadorn B, Rossi E. Relative underweight in cystic fibrosis and its prognostic value. Acta Paediatr Scand 1978; 67:33-37. [PubMed]

Fig 56. Richard Kraemer
This paper from from Professor Rossi’s department in Berne is often quoted as confirming the importance of the nutritional state as an indicator of prognosis. Observations on 117 children with CF from Jan 1956 to June 1976 showed that relative under weight (weight loss corrected for height) is most pronounced when chest is bad and correlates closely with survival.Professor Richard Kraemer (fig. 56) is Director of the Paedaitric Department at the University of Berne and for many years has been involved with research and clinical care of children with cystic fibrosis and other respiratory conditions.
1978 Schwarz HP, Kraemer R, Thurnheer U, Rossi E. Liver involvement in cystic fibrosis. A report of 9 cases. Helv Paediat Acta 1978; 33:351-364. [PubMed]
A report of 9 patients amongst the 204 seen at Professor Rossi’s clinic in Berne over the previous 20 years. Focal biliary cirrhosis was the main finding in three with non-specific nodular cirrhosis, an infant with prolonged obstructive neonatal jaundice and two others had steatosis. The authors review the previous literature.
1978 Smalley CA, Addy DP, Anderson CM. Does that child really have cystic fibrosis? Lancet 1978; ii: 415-417.[PubMed]
The first report from a major paediatric centre of children mistakenly diagnosed and treated as having cystic fibrosis. In this report, from Prof. Charlotte Anderson’s Birmingham CF unit, 14 referred children had an incorrect diagnosis of CF – 13 had previous sweat tests in other laboratories “where test not done very often”. Detailed pancreatic function testing was normal in the 5 in which it was performed. None had chest disease and only 2 had any gastrointestinal symptoms. The authors advised that “in the absence of typical clinical features of the disease, a diagnosis of cystic fibrosis should be made with extreme caution”.
This was a very important paper as it prompted a number of reports on mistaken diagnosis (David TJ, Phillips BM. Over diagnosis of cystic fibrosis. Lancet 1982; 2:1204-1206. [PubMed]). Of the first 179 children, already diagnosed and treated as CF in general paediatric departments, who were referred to our Leeds CF Centre for Comprehensive Assessment during the Eighties, no less than 7 (4%) were found not to have CF – a sweat test to check the diagnosis was part of our assessment for which they were referred (Shaw NJ, Littlewood JM. Arch Dis Child 1987; 62:1271-1273 below). The over-diagnosis was usually the result of an uncritical acceptance of a positive sweat test result performed in a laboratory where the test was only performed occasionally.
1978 Chase HP, Dupont J. Abnormal levels of prostaglandins and fatty acids in the blood of children with Cystic Fibrosis. Lancet 1978; ii: 236-238. [PubMed]
Low levels of linoleic acid in 12 children with CF and higher production of prostaglandin F2 than controls, were corrected by linoleic acid supplements (see Chase et al, 1979 below).
1979 Weber AM, de Gheldere B, Roy CC, Fontaine A, Dufour OL, Morin CL, Lasalle R. Cystic Fibrosis Club Abstracts. May 1, 1979.
Second report of the new enzyme preparation Pancrease from Prof. Roy’s unit in Montreal. This enzyme preparation had a major effect on the treatment of the intestinal malabsorption in CF. The table (fig. 57) shows Pancrease compared with Cotazym, the usual widely used preparation at the time, and also shows that crushing the microspheres and removing the protective effect of their pH sensitive coating markedly reduced their effect. Six children aged between 2.2 and 3.8 years were studied.
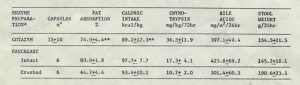
Fig 57. Table comparing fat absorption on Cotazyme or Pancrease
1979 Beckerman RC, Taussig LM. Hypoelectrolytemia and metabolic alkalosis in infants with cystic fibrosis. Pediatrics 1979; 63:580-583. [PubMed]
In Tucson Arizona five of 11 infants with CF diagnosed in the first year between 1972 to 1977 were seen with hypokalemia, hypochloremia and metabolic alkalosis unassociated with marked dehydration, hyperpyrexia or major pulmonary or gastrointestinal symptoms. Chronic loss of sweat electrolytes together with mild gastrointestinal or respiratory disturbance may predispose. The lack of shock and hyperpyrexia differentiates the clinical state from the heat prostration syndrome described by Kessler & Andersen in 1951 (above).This complication came to be known as Pseudo-Bartter’s syndrome. Of course occasionally infants with this clinical picture may not have CF but actually do have true Bartter’s syndrome as did an affected infant we reported in the previous year (Littlewood J M, Lee M R, Meadow S R. Treatment of Bartter’s syndrome in early childhood with prostaglandin synthetase inhibitors. Arch Dis Child 1978; 53:43-48. [PubMed]). Both these situations will be diagnosed if the precaution is taken to always estimate serum electrolytes of any infant, CF or non-CF, who has a significant degree of “failure to thrive”.
1979 Chase HP, Cotton EK, Elliot RB. Intravenous linoleic acid supplementation in children with cystic fibrosis. Pediatrics 1979; 64:207-213. [PubMed]
This study was performed to investigate the previous observation of Prof. Bob Elliott of clinical improvement after IV Intralipid (Elliott & Robinson, 1975, above). On alternate weeks for a year 10 children received either intravenous Intralipid or a similar number of calories as 10% glucose. The Intralipid-treated group were marginally better re. height but the numbers were small and the differences were not significant. The authors thought the differences may have been obscured by the response of all patients to the increased attention they received during the trial. The authors suggested multicentre studies from an early age and also that all should be screened annually for low linoleic acid levels and supplementing those with levels below 2SD of normal.
This was perhaps the first double blind study of a nutritional intervention in cystic fibrosis. Unfortunately the present findings did not confirm Elliot & Robinson’s 1975 observation and did not seem to have a significant impact on CF management at the time. The questions surrounding the importance of fatty acid deficiency in CF would persist for many decades.
1979 Fellows KE, Kon Taik Khaw, Schuster S, Shwachman H. Bronchial artery embolisation in cystic fibrosis; technique and long term results. J Pediatr 1979; 93:959-963. [PubMed]
This technique was first reported in other diseases (Wholey MH et al, JAMA 1976; 236: 2501-2504. [PubMed]) and in two patients with CF in a series of 104 with various conditions (Remy J et al, Radiology 1977; 122:33-37. [PubMed]). In this present series major bleeding ceased in 12 of the 13 patients with CF although five had minor recurrences. The authors advised the procedure should be limited to life-threatening episodes (also Holsclaw DS et al, 1970; Stern et al, 1977 both above).
1979 Newman AJ, Ansell BM. Episodic arthritis in children with cystic fibrosis. J Pediatr 1979; 594-595.[PubMed]

Fig. 58 Barbara Ansell.
Dr Barbara Ansell (1923-2001) (fig. 58) was the leading UK authority on joint disease in children for many years. Referred to her were five children aged two to 10 years with CF who developed transient episodic arthritis. Although polyarticular in distribution, only one joint may be involved during each attack. There was no radiological or laboratory evidence of juvenile chronic arthritis and no permanent joint limitation occurred.
Further reports followed of arthritis in people with CF (Vaze D. J Pediatr 1980; 96:346) including one with rheumatoid arthritis (Sagransky DM, et al, Am J Dis Child 1980; 134:319-320).
We later reported a clear relationship between the joint problems and the activity of the chest infection in children with CF – the problem obviously worsening during exacerbations of respiratory infection and improving during a course of intravenous antibiotic treatment for the exacerbation (Bowler & Littlewood. Lancet 1992; 340:244).
1979 di Sant’Agnese PA, Davies PA. Cystic fibrosis in adults. 75 cases and a review of 232 cases in the literature. Am J Med 1979; 66:121-132. [PubMed]
This is a detailed review of CF as seen in adults at the time. The 75 patients were aged 18 to 47 years. Chronic obstructive pulmonary disease was present in 97% and the major cause of mortality and morbidity and all were infected with Pseudomonas aeruginosa and Staphylococcus aureus. 60% had minor and 7% major haemoptysis, pneumothorax occurred in 16%. Sinusitis in all and 48% had nasal polyposis, pancreatic insufficiency in 95%, and meconium ileus equivalent in 21%. Some had glycosuria, biliary cirrhosis, cholelithiasis or aspermia. Height and weight were usually in the lower limits of normal but some older patients with CF may look quite well.An interesting paper describing adults in the Seventies by one of the leading US experts of the time and one of the future experts. As with other series of people with CF who had reached adulthood, many (22% in this series and 17% in a series of Shwachman, 1977) had been diagnosed after the age of 15 years. A significant number of such patients would almost certainly have at least one so-called “mild” mutation. The presence of these late diagnosed but longer surviving patients has always confounded studies designed to show the importance of early diagnosis; but they are, of course, a minority of patients.
1979 Pryor JA, Webber BA, Hodson ME, Batten JC. Evaluation of the use of forced expiration technique as an adjunct to postural drainage in treatment of cystic fibrosis. BMJ 1979; 2:417-418.[PubMed]
The classic paper from the Brompton team on forced expiratory technique (FET) from the Brompton Hospital, London comparing conventional physiotherapy with FET without the involvement of an assistant. The latter was both more efficient (producing 45.6 g vs. 63.1 g sputum per day) and quicker (358.5 vs. 652.1 mg sputum per minute) than conventional physiotherapy and was not improved by involving an assistant. The authors concluded – “Patients with cystic fibrosis who had to rely on the help of others for their home treatment may now perform more effective treatment without help”.
The value of chest physiotherapy in clearing bronchial secretions in conjunction with postural drainage in patients producing more than 30ml of sputum per day was established first by Cochrane GM et al, (BMJ 1977; 2:1181-1183.[PubMed]) who studied the specific airways conductance (SGAW) of 23 patients with copious sputum production and airflow obstruction before and after physiotherapy to determine the effect of bronchial secretions on pulmonary function. Chest physiotherapy to remove these secretions had the effect of reducing airflow obstruction, as measured by SGAW. These findings were taken to suggest that sputum has a detrimental effect on pulmonary function and that physiotherapy can reduce airways obstruction. Physiotherapy for children with CF had been introduced into Shwachman’s clinic in 1957 by Barbara Doyle (Doyle et al, 1959 above).This forced expiratory technique described in the present paper represented a significant advance allowing the patient more independence and less reliance on others.
Jennifer Pryor has produced a very intersting oral history (http://www.100yearsofphysio.co.nz/oral-histories/jennifer-pryor). Jennifer talks about her training, her early work in Christchurch, her collaboration with Heath and Bunny Thompson, and moving to the Brompton Hospital in London. Also she reviews some of her work in respiratory physiotherapy over the last 50 years.
1979 Ryley HC, Neale LM, Brogan TD, Bray PT. Screening for cystic fibrosis in the newborn by analysis of meconium. Arch Dis Child 1979; 54:92-97. [PubMed]
Fig. 59 Henry Ryley at the 1994 ECFS meeting in Paris
Percy Bray (figure 27) of Cardiff, was one of the few paediatricians in the UK with a special interest in CF at the time. This final report of BM Meconium screening in Wales between 1973-1977 showed the test failed to identify 25% of infants with CF when performed in Wales by midwives in maternity units.
Dr Henry Ryley (Fig 59) of Cardiff was involved in CF Scientific and Clinical Research for many years and even in 2023 provides a summary of the current publications for the ECFS – a very helpful but formidable task.
In East Leeds we started neonatal CF screening with this test in 1975 in the maternity unit where I was responsible for the neonatal care (St Mary’s, Bramley – 3000 deliveries per year) . However, after repeatedly finding small pots of meconium on ward window sills, I soon realized that the overworked midwives were not the people to do this test!!
The laboratory at St James’s kindly offered to do the tests with proper laboratory standard control; so meconium specimens were sent to the laboratory in small bottles where the test was done more professionally. We later reported better results when the test was performed by our laboratory colleagues (Evans et al, 1983).
However, Crossley and Elliott (1979 below) were about to describe their IRT blood test for neonatal CF screening which was a far better test and was soon taken up and used with success by neonatal CF screening enthusiasts making the BM tests redundant. Yet, for financial and administrative reasons (and because with the BM test performed in the laboratory, rather than on the ward, we seemed to be identifying the infants with CF!) we continued to use the BM test with reliable results until well into the Nineties until it was replaced by the IRT method (Littlewood JM et al. 20 years continuous neonatal screening in one hospital: progress of the 37 patients and their families. Pediatr Pulmonol 1995; Suppl 12: Abstr 372 p.284).
1979 Flower KA, Eden RI, Lomax L, Mann NM, Burgess J. New mechanical aid to physiotherapy in cystic fibrosis. BMJ 1979; 2:630-631. [PubMed]

Fig 60. Patient using a mechanical percussor
The authors analysed the effects of the percussion provided by professional physiotherapists for the first time and reproduced in the small portable “Salford Percussor” (fig. 60). Although initially popular with a few parents there was no subsequent work on the device and it was not accepted by UK physiotherapists who, as a group generally, have not been enthusiastic about mechanical aids to physiotherapy – as evidenced by their more recent lack of enthusiasm for the mechanical vest!!! (also Denton, 1962 above; Maxwell & Redmond, 1979 below).
1979 Maxwell M, Redmond A. Comparative trial of manual and mechanical percussion technique with gravity-assisted bronchial drainage in patients with cystic fibrosis. Arch Dis Child 1979; 54:542-544. [PubMed]
Here 14 patients with CF were studied by measuring sputum volumes and respiratory function. The results with the mechanical percussor (figure 30) were comparable with those with manual percussion. All the patients and parents preferred the mechanical percussor.
However, there is no further mention of the mechanical percussor by either the Manchester group (Flower et al, 1979 above) or Belfast group (Maxwell

Fig 61. Aileen Redmond
& Redmond) and they did not gain the support of he majority of UK physiotherapists who seem, as a group, to be unimpressed by mechanical aids for physiotherapy.Mechanical methods had been reported previously in an excellent trial by Robert Denton (Am Rev Respir Dis 1962; 86:41-46 above).
Aileen Redmond (fig. 61) was paediatrician and Director at the Belfast Paediatric CF unit and had worked with Harry Shwachman in Boston – one of the first centres to use physiotherapy. She published on a wide variety of subjects including CF and was one of the few UK experts in CF at the time and one of the first to introduce neonatal IRT CF screening in Northern Ireland in the early Eighties. Her CF unit at the Belfast Children’s Hospital was highly regarded and she eventually achieved a purpose built CF unit – Cherry Tree House in Belfast.
1979 Yassa JG, Prosser R, Dodge JA. Effects of an artificial diet on growth of patients with cystic fibrosis. ArchDis Child 1978; 53:777-783. [PubMed]
Fig 62. Jeanette Yassa measuring subcutaneous fat
A controlled trial to test the Allan Diet by Dr Jeanette Yassa (fig. 62) working with John Dodge in Cardiff at the time and later to became a consultant paediatrician in Sheffield.
Twenty eight children were treated but the diet significantly improved the nutritional state of only ten. The authors concluded that “such an unpleasant and expensive diet should be restricted to a few selected cases, rather than given as routine treatment”.Shortly after this paper was published the new acid resistant microsphere pancreatic enzymes (Pancrease and later Creon) were introduced and they totally revolutionised the treatment of malabsorption so much more efficient were they than the older preparations, so most patients no longer needed this type of artificial diet.
1979 Chase HP, Long MA, Lavin MH. Cystic fibrosis and malnutrition. J Pediatr 1979; 95:337-347. [PubMed]
One of a number of important detailed nutritional studies of patients with CF around this time showing many patients had an inadequate energy intake even for non-CF individuals. As more children survived to adolescence the maintenance of a reasonable nutritional state and growth rate became increasingly difficult both from the inadequately controlled malabsorption and the progressive chest involvement . In this study the authors comment that the importance of the malnutrition in the disease process remains unknown, as does much information about specific nutritional deficiencies in cystic fibrosis. They advised that supplements for children with CF should include extra energy as fat or carbohydrate, a form of linoleic acid that can be absorbed, hydrolyzed protein, fat-soluble vitamins with vitamins A and E in a water emulsion, vitamin B12, probably B vitamins and vitamin C, and trace minerals. Routine measurements of nutritional status, particularly in children with growth failure, should be made at regular intervals and should include a three-day diet record and a simultaneous 72-hour stool fat determination. If fat malabsorption is not controlled even with pancreatic enzymes, the use of antacids or cimetidine should be considered. (also Hubbard & Magnum, 1982; Parsons et al, 1983).
1979 Crossley JR, Elliott RB, Smith PA. Dried blood spot screening for cystic fibrosis in the newborn. Lancet 1979; i: 472-474. [PubMed]

Fig 61. Jeanette Crossley
This study was from Auckland, New Zealand. Serum-immunoreactive-trypsin (IRT) was measured in children with CF and a variety of controls. In the first few months of life all the children with CF had a raised serum- IRT.A dried blood-spot assay for IRT was established using double antibody radioimmunoassay kit (Hoechst Research Laboratories) and presented as having potential as a screening test for CF in the newborn (fig.63). There were none of the disadvantages of stool trypsin screening as infants with residual pancreatic function (“pancreatic sufficient” infants) also has a raised IRT.
In New Zealand Crossley and colleagues further evaluated the test (Crossley JR et al. Clin Chim Acta 1981; 113:111-121; Lyon IC et al. NZ Med J 1983; 96:673-675). Neonatal IRT screening was soon adopted in New Zealand and some states in Australia where Bridget Wilcken of Sydney has been a champion of neonatal screening since the early Eighties. The IRT test now forms the basis of most neonatal CF screening programmes throughout the world – now usually combined with DNA examination for CF-causing mutations when the IRT is positive.
This was a really important landmark paper for neonatal CF screening. Neonatal IRT screening had the great practical advantage of using the same neonatal blood spots already collected by the heel prick in the first week of life for phenylketonuria and later hypothyroidism.

Fig 62. Anthony Heeley
In the UK, Dr Anthony Heeley (figure 37), the biochemist in Peterborough, UK started IRT neonatal screening in East Anglia in 1981 (Heeley et al, 1982 below). In 2009 he kindly commented as follows – “Your summaries of our early papers are excellent. A point to emphasise was that Crossley & Elliott’s seminal work in 1979 required 2 x 12 mm blood spots for the assay. We realised that was unrealistic for routine screening and in our paper in the Lancet the same year (King DN. Heeley AF. Walsh MP. Kuzemko JA. Sensitive trypsin assay for dried-blood specimens as a screening procedure for early detection of cystic fibrosis. Lancet 1979; 2(8154):1217-1219) we showed that their results could be confirmed using 4 mm blood spots which was a much more practical size for routine prospective screening trials. These trials were quickly underway in the Antipodes, here and elsewhere, but we have ascertained that the first case of CF to be detected in a prospective screening trial with IRT was in East Anglia in 1980, a girl born one month before the first case detected prospectively by the New Zealanders. Even better, although homozygous Delta F 508, to my knowledge she led a robust and active life up to late teenage when I lost contact. Her paediatrician could not recall any exacerbation of her condition requiring hospital admission. I still treasure a slide of her as a healthy teenager and I was proudly able to show it at a National Neonatal Screening Seminar in Newcastle a couple of years ago (dragged out of retirement for the historical story!)”.
In 2009 Jeanette Crossley (fig. 61) kindly commented for me as follows –

Fig 63. Serum IRT in children with CF (above) and with out CF (below)
“We were fortunate that our 1979 Lancet paper robustly established the potential of blood spot IRT for CF newborn screening, using the Hoechst-Behring Riagnost Trypsin Kit. The kitset as supplied required a relatively large sample size [we used 2 x 12mm discs from a 5-day Guthrie card], so our next step was modifying that method. We achieved 10-fold greater sensitivity, enabling one 3mm disc as sample, left in the tube throughout the stages of the assay. In a retrospective study of 23 known CFs using this optimized assay [unpublished], each CF was clearly distinguishable from two controls from the same batch of Guthrie cards, despite the Guthrie cards having been stored at room temperature for up to seven years.For several reasons, economics being a main one, we did not conduct an extensive prospective trial using the Hoechst-Behring reagents. Rather, we developed our own Auckland radioimmunoassay ‘from scratch’ [reported in detail in the Clin Chim Acta paper1981]. Its validation included repeating the retrospective study, again clearly distinguishing all the known CFs from controls. We established that the molecular species assayed in blood is trypsinogen. Our ‘Auckland assay’ was more sensitive, and had better linearity for serially diluted samples, than our optimization of the Hoechst-Behring kitset assay. Also, knowing what was in all our reagents gave us confidence – we had been unable to obtain from Hoechst the exact make-up of their assay.
Our team effort launched dried bloodspot CF screening in NZ, first as a pilot, and then nationally – and also enabled Bridget Wilcken to get started in NSW, Australia. I’ve been told that our original purified trypsin and antisera were used in the National CF Screening Programme until about 1990, when changing health and safety policies required a move away from radio-labelled methods. It had been a delight to be invited to present our experience with our ‘Auckland IRT assay’ and with our optimisation of the Hoechst-Behring Riagnost kitset, at an international meeting ‘Immunoreactive Trypsine’ sponsored by Hoechst France in Caen, 25 October 1980. We were very pleased to see the quick and thorough progress being made in several countries with validation of IRT as a CF newborn screening method. The first UK symposium on neonatal screening for cystic fibrosis, for example, sponsored by CIS (UK) Ltd and Sorin Biomedica SpA, was held in London 10 days after the Caen meeting”.
1979 Jenner BM, Landau LI, Phelan PD. Pulmonary candidiasis in cystic fibrosis. Arch Dis Child 1979; 54:555-6. [PubMed]
Despite the frequent and prolonged use of antibiotics, this is the first reported case of pulmonary candidiasis confirmed by lung puncture and treated successfully with 5-flourocytosine. Antibiotics, steroids and intravenous catherisation predisposed to the Candida infection.There are very few reports of Candida in CF as a primary pathogen although it can be isolated from the airways of many patients and is found frequently in dental studies of people with CF. More recently vaginal Candida has been described as a common, significant and under-diagnosed problem in women with CF, considered to be related to the frequent use of antibiotics (Sawyer et al, 1994 below). Also with the more widespread use of intravenous therapy, serious systemic infections have occurred with totally implantable venous access devices (reviewed by Webb AK & Woolnough E. J Roy Soc Med 2006; 99 (Suppl 46):13-16)
1979 Brasfield D, Hicks G, Soong S-j, Tiller RE. The chest radiograph in cystic fibrosis: a new scoring system. Pediatrics 1979; 63:24-29. [PubMed]
A system of X-ray scoring that was quite widely used in the USA. Authors comment that the Chrispin-Norman system (1974 above) was not checked for reproducibility nor correlated with the clinical condition of the patients. The score was further evaluated in a multicentre study (Brasfield D et al. Am J Roentgenol 1970;134:1195-1198. [PubMed]) and was found to have “a moderately high level of reproducibility by and among observers”.There is a detailed comparison and review of the various scoring systems by Conway SP & Littlewood JM. Cystic fibrosis clinical scoring systems. In: Dodge JA, Brock DJH, Widdicombe JH (Eds.). Cystic Fibrosis – Current Topics. Volume 3. John Wiley & Sons, Chichester.1996:339-358.
1979 Loening-Baucke VA, Mischler E, Myers MG. A placebo-controlled trial of cephalexin therapy in the ambulatory management of patients with cystic fibrosis. J Pediatr 1979; 95:630-637. [PubMed]
This trial is often quoted as supporting the view that prophylactic anti-Staphylococcal therapy predisposes to Pseudomonas infection – although most patients included in this trial were already chronically infected with P. aeruginosa at the start of the trial!!
Patients received alternate four months of oral cephalexin or placebo over two years. Initially no less than 15 of 17 patients had P. aeruginosa (4 mucoid and 11 non-mucoid) and 10 of 17 had Staphylococcus aureus. Mucoid strains increased (six patients) as one would expect and disease severity increased in those initially colonised with P. aeruginosa but cephalexin did reduce the frequency of respiratory illnesses and colonisation in patients initially colonised with S. aureus and H. influenzae. Authors concluded that “The long term administration….may be associated with an accelerated rate of colonisation with mucoid strains of P. aeruginosa and the potential for deterioration…”
This small study of 17 patients (of whom 15/17 were already infected with P.aeruginosa) subsequently has been quoted repeatedly, and in my view quite inappropriately, as showing that long term anti-Staphylococcal therapy causes an increase in P. aeruginosa. Certainly some of the patients with non-mucoid P. aeruginosa converted to the mucoid form during the study, but this would be expected as these were the days before early eradication was thought possible or attempted; but essentially this was a small series of children already chronically infected with P. aeruginosa and certainly no conclusions can be drawn regarding long term anti-Staphylococcal therapy – certainly not about long term narrower spectrum therapy with flucloxacillin.
1979 Bradley JA, Axon AT, Hill GL. Nocturnal elemental diet for retarded growth in a patient with cystic fibrosis. Brit Med J 1979; Jan 20th: 167. [PubMed]
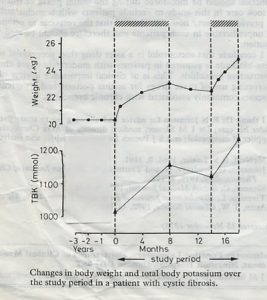
Fig 64. Weight chart of patient Bradley et al, 1979
The first report of continuous nocturnal nasogastric feeding in a child with CF – interestingly not from a CF

Fig 65. Tony Axon
centre as this child was referred by her general paediatrician to Professor Tony Axon (fig. 65) a distinguished gastroenterologist in Leeds. A girl of 13 years with CF used a 8F nasogastric tube for overnight feeding with an elemental diet (Vivonex) infused over 10 hours each night to provide 600 kcal using an infusion pump for eight months then 6 months off then a further 2 months of treatment. There was a 12% increase in body weight in the first six months and overall 20% increase from pre-treatment values (figure 64).The authors mention Andrassy RJ et al. (Surgery 1977; 82:205. [PubMed]) as having given continuous elemental diet by catheter to children with a large variety of illnesses and found the method easy to institute and free from side effects.
Intermittent tube feeding was routine practice in premature baby units at that time but not by continuous feeds – suitable infusion pumps were not yet available. The overnight nasogastric feeding methods and then gastrostomy feeding gradually became widely used in the nutritional treatment of people with CF and a number of studies appeared over the next few years (Shepherd et al, 1980 below; Levy et al, 1985 below; Shepherd et al, 1986 below).
1979 Phelan PD, Allan JL, Landau LI, Barnes GL. Improved survival of patients with cystic fibrosis. Med J Australia 1979; 1:261-263. [PubMed]
Three hundred and twenty patients with CF born after 1958 who were treated at Royal Children’s Hospital, Melbourne had an 80% survival to 11 yrs and a 64% survival to 18 yrs. Those managed between 1973-77, 91% survival to 12 yrs and 80% to 17 yrs.
These were really excellent results for the time and were attributed, almost certainly correctly, to all patients having received Specialist CF Centre care as was later discussed in a very influential subsequent paper from Melbourne the contents of which prompted the formation of the UK Working Party on Cystic Fibrosis in 1982 (Phelan and Hey, 1984 below).
1979 Soter NA, Mihm MC, Colten HR. Cutaneous necrotising venulitis in patients with cystic fibrosis. J Pediatr 1979; 95:197-201. [PubMed]
Two patients developed palpable purpura late in the course of their disease. Biopsies showed necrotising venulitis with perivenular infiltrate composed of neutrophils, fibrin hypogranulated mast cells and endothelial cell necrosis. Circulating immune complexes were detected. A variety of immunological abnormalities have been described in such patients. (Also Finnegan MJ et al, Quart J Med1989; 72:609-621; Hodson ME. J R Soc Med 1992; 85 (Suppl 19):38-40). (figure 39)
1979 Mischler EH, Chesney PJ, Chesney RW, Mazess RB. Demineralization in cystic fibrosis detected by direct photon absorptiometry. Am J Dis Child 1979; 133:632-635. [PubMed]
Bone mineral content, bone width, and their ratio were measured in patients with CF using monoenergetic photon absorptiometry. Serial measurements of the radius and ulna were made in 27 patients with CF and were compared with 968 age-matched controls. Demineralization was found in 37% of the boys and 63% of the girls. Patients under age 10 years had normal bone mineral content and nine of 15 patients aged 13 or older were demineralised (P<0.01). Demineralization correlated with the extent of weight reduction in patients (P<0.001). Patients most likely to be demineralised were adolescent girls. This appears to be the first study of bone mineral status of children with CF indicating that a sizable proportion of people with CF may be demineralised without having overt rickets. In 1979 most people with CF were children or adolescents.
1979 Sinniah D. Omar A. Quantitation of digital clubbing by shadowgram technique. Arch Dis Child 1979; 54:145-146. [PubMed]
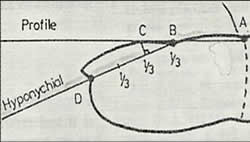
Fig 66. Shadowgram and measurements of finger clubbing
Finger clubbing was quantified from the magnified silhouette of the right index finger in controls and patients using a simple shadowgram technique obtained using an overhead projector and screen. There was good correlation between clinical assessment and measurement of both the profile angle and the hyponychial angle (fig. 66). The hyponychial angle appeared to be a more accurate indicator of clubbing than the profile angle. We used this technique in Leeds to examine the fingers of a series of children with CF (Pitts-Tucker et al. 1986 below).
Measurement in figure 40 is as follows – A = distal digital crease. B = datum point (cuticle). C = point at which a perpendicular from one third of the distances BD meets the nail. D = hyponychium (thickened stratum corner of epidermis lying under the free edge of the nail. ABC = profile angle ABD = hyponychial angle
1979 Vawter GF, Shwachman H. Cystic fibrosis in adults: an autopsy study. Pathol Ann 1979; 14 Pt 2:357-382.[PubMed]
In this population, the most characteristic abnormalities recognized by the pathologist were focal biliary cirrhosis, distinctive obstructive lesions of the male genital tract, prolonged Staphylococcal or Pseudomonas colonization of respiratory secretions, and obstructive bronchopulmonary disease. one form of pancreatic atrophy was usually present.
1979 Price JF, Weller PH, Harper SA, Matthews DJ. Response to bronchial provocation and exercise in children with cystic fibrosis. Clin Allerg 1979; 9:563-570. [PubMed]

Fig 67. John Price
Ten of 15 children with CF who had positive skin prick tests to allergens had an immediate reaction to the allergen inhaled; five had late reactions also but only one had a history of asthma. The most common positive skin reaction was to Aspergillus fumigatus – inhalation of the allergen was negative in two, immediate in one and dual in three. None showed the typical reaction to exercise of asthmatic children. Although the bronchial allergy did not totally explain the tendency for children with CF to have asthma and anti-allergy treatment may have a place.
Professor John Price (fig. 67) founded the Paediatric Respiratory Unit at Kings College Hospital, London. He developed the CF service there and also a shared care programme for children with CF at other general hospitals in the South East of England. More recently he was closely involved in the supervision and organisation of the successful introduction of neonatal screening into the UK in 2007.

