2010
2010
THE FOLLOWING THREE ABSTRACTS ARE REVIEWS OF VARIOUS ASPECTS OF PROGRESS IN 2010
David Honeybourne. Cystic fibrosis papers of the year 2010-2011. J R Soc Med 2012 Jun;105 Suppl 2(Suppl 2):S30-5.doi: 10.1258/jrsm.2012.12s006 Free PMC article [PubMed]

Fig. 1 David Honeybourne
This review is based upon a Medline search of the literature on cystic fibrosis for the latter half of 2010 onwards. The Medline search was carried out in September 2011 and also includes some references published after September 2011. This search revealed articles relating to approximately 482 paediatric studies and 419 adult studies with much overlap between the two groups. Taking into account the multidisciplinary nature of the audience for this symposium and also taking into account the topics in the rest of the programme for the day, a shortlist of 65 papers was then derived. A diversity of topics was clearly necessary and also a mixture of paediatric and adult publications, hence the following papers were chosen.
Dr David Honeybourne (fig. 1) is consultant at the West Midlands Adult Cystic Fibrosis Centre, Heartlands Hospital, Birmingham B9 5SS, UK.
Helen K Reddel, T K Lim, Michiaki Mishima, Claire E Wainwright, Darryl A Knight. Year-in-review 2010: asthma, COPD, cystic fibrosis and airway biology. Respirology 2011 Apr;16(3):540-52. doi: 10.1111/j.1440-1843.2011.01949.x. [PubMed]

Fig. 2 Helen Reddel woolcock.orgs.au
Respiratory diseases are estimated to affect a billion people around the world, and account for 12 million deaths a year. In order to raise awareness of respiratory conditions, the Forum of International Respiratory Societies (FIRS), which includes the Asia Pacific Society of Respirology, declared 2010 the Year of the Lung.1 One of the highlight events of the year was World Spirometry Day on October 14, when over 100 000 free spirometry tests were performed at 412 events worldwide. The Year of the Lung also involved intense lobbying of legislative bodies to promote issues such as air quality and anti-tobacco initiatives, and to encourage direction of research funding towards respiratory conditions.
One of the important goals of the Year of the Lung was to focus awareness on respiratory research. In this review, we describe important global advances in 2010 in asthma, COPD, cystic fibrosis and airway biology, and highlight the contribution of research in these areas from Respirology.
The cystic fibrosis section is reviewed by Prof. Claire Wainwright
Prof. Helen K Reddel (fig.2) is a physician and researcher at the Woolcock Institute of Medical Research, Sydney, New South Wales, Australia. hkr@med.usyd.edu.au
Michael P Boyle. Cystic fibrosis: year in review. Curr Opin Pulm Med 2010 Nov;16(6):583. doi: 10.1097/MCP.0b013e32833f3f0d. A full editorial available via Pubmed link [PubMed]
Fig 3. Michael Boyle
The last year has been an exciting one for cystic fibrosis patients and caregivers. New approaches to care have been evident throughout the CF age spectrum from prenatal and newborn screening becoming an increasingly accepted standard of care, to new guidelines for CF related diabetes (CFRD) which highlight the approximately 50% prevalence of CFRD in adults over the age of 30. Pivotal clinical trials have commenced which do not just see to address symptoms or complications of CF but utilise genotype-specific therapies to address underlying CF transmembrane conductance regulator dysfunction. Around the globe CF care centres have focused on optimising treatment practices and care delivery to assure the best outcomes for their patients.
This year CF review in Current Opinions in Pulmonary Medicine reflects a wide range of advances. It starts with a review of emerging issues in newborn screening by Carlo Castellani and John Massie which highlights recent successes with NBS but also its future challenges. Peter Sloan and Stephen Rowe then provide an update on the new therapies in CF focusing on CFTR protein repair as a therapeutic strategy. We then move into clinical management with Richard Moss presenting both the underlying pathophysiology and current best treatment practices for allergic bronchopulmonary aspergillosis in CF, Andrew Prayle and Alan Smyth discuss therapeutic strategies to maximise efficacy and minimise toxicity of aminoglycosides. We finish with two topics with greatest impact in the adult population; Arlene Stecenko and Antoinette Moran provide an overview of CF relat6ed diabetes (CFRD) with particular attention to its impact on lung health. Charles Howard discusses the impact of CF and bone health.
The theme for all the updates in that increasing understanding of the underlying pathophysiology of CF and its complications has resulted in more effective treatment strategies. These treatment strategies are resulting in a brighter outlook for our for all our patients from the youngest to the oldest
Dr Michael Boyle (fig. 3) is at the Johns Hopkins School of Medicine. From 2019 he is president and chief executive officer of the Cystic Fibrosis Foundation. Prior to his appointment as president and CEO, Dr. Boyle served as the Foundation’s senior vice president, therapeutics development from 2015-2019.
2010
Accurso FJ, Rowe SM, Clancy JP, Boyle MP, Dunitz JM, Durie PR, Sagel SD, Hornick DB, Konstan MW, Donaldson SH, Moss RB, Pilewski JM, Rubenstein RC, Uluer AZ, Aitken ML, Freedman SD, Rose LM, Mayer-Hamblett N, Dong Q, Zha J, Stone AJ, Olson ER, Ordonez CL, Campbell PW, Ashlock MA, Ramsey BW. Effect of VX-770 in persons with cystic fibrosis and the G551D-CFTR mutation. New Engl J Med. 2010; 363:1991-2003. [PubMed] Free PMC article
VX-770, a CFTR potentiator, has been shown to increase the activity of wild-type and defective cell-surface CFTR in vitro. 39 adults with cystic fibrosis and at least one G551D-CFTR allele received oral VX-770 every 12 hours at a dose of 25, 75, or 150 mg or placebo for 14 days (in part 1 of the study) or VX-770 every 12 hours at a dose of 150 or 250 mg or placebo for 28 days (in part 2 of the study).
At day 28, in the group of subjects who received 150 mg of VX-770, there were significant changes towards normal of the sweat chloride, nasal potential difference and respiratory function. The authors concluded that this study to evaluate the safety and adverse-event profile of VX-770 showed that VX-770 was associated with within-subject improvements in CFTR and lung function.
The results of this phase II trial of VX-770, confirm it to be one of the most significant advances up to the present time in increasing CFTR function and with obvious beneficial changes in respiratory function and even normalisation of the abnormal sweat electrolyte levels.
Subsequent Phase III trials fully confirmed that this was indeed a major advance for those people with CF who had at least one G551D mutation – in the UK 5.8% of people with CF.
The drug named Kalydeco (generic name ivacaftor, previously known as VX-770) was approved for clinical use in January 2012 in the USA although it is likely that the cost will prove a problem. The suggested annual cost could be as much as $294,000 per year per patient – a really massive problem for funders be they insurance companies or government.
Aaron SD, Vandemheen KL, Ramotar K, Giesbrecht-Lewis T, Tullis E, Freitag A, Paterson N, Jackson M, Lougheed MD, Dowson C, Kumar V, Ferris W, Chan F, Doucette S, Fergusson D. Infection with transmissible strains of Pseudomonas aeruginosa and clinical outcomes in adults with cystic fibrosis. JAMA 2010; 304:2145-2153. [PubMed]

Fig. 4 Shawn Aaron ohri.ca
Of 446 patients with CF, 102 were infected with 1 of 2 common transmissible strains of P. aeruginosa. Sixty-seven patients were infected with strain A (15%), 32 were infected with strain B (7%), and 3 were simultaneously infected with both strains (0. 6%).
Strain A was found to be genetically identical to the Liverpool epidemic strain but strain B has not been previously described as an epidemic strain. Compared with patients infected with unique strains of P. aeruginosa, these patients had similar declines in lung function but the 3-year rate of death or lung transplantation was significantly greater in those infected with the Liverpool epidemic strain (18. 6%) compared with those infected with unique strains (8. 7%) .
The authors concluded that a common strain of P. aeruginosa (Liverpool epidemic strain/strain A) infects patients with cystic fibrosis in Canada and the United Kingdom. Infection with this strain in adult Canadian patients with cystic fibrosis was associated with a greater risk of death or lung transplantation.
– This study from Canada confirms the increased morbidity of those patients who are infected by a transmissible strain of P. aeruginosa (Liverpool epidemic strain/strain A). This was the experience from the UK reported initially by Andy Jones and colleagues from Manchester (Jones AM et al. Lancet 2001; 358:557-558. [PubMed]). The Liverpool strain was initially reported in children attending the Alder Hey Children’s Hospital CF clinic in Liverpool (Cheng K et al. Lancet 1996; 348:639-642). [PubMed] where it remians a significant problem in the Liverpool adult CF unit.
Dr. Shawn Aaron (fig.4) is a Professor at The University of Ottawa and a Senior Scientist at the Ottawa Hospital Research Institute.
Amin R, Subbarao P, Jabar A, Balkovec S, Jensen R, Kerrigan S, Gustafsson P, Ratjen F. Hypertonic saline improves the LCI (lung clearance index) in paediatric patients with CF with normal lung function. Thorax 2010; 65:379-383. [PubMed]
The authors objective was to study the ability of the lung clearance index (LCI), a measure of ventilation inhomogeneity, to detect a treatment response to hypertonic saline inhalation in paediatric patients with CF with normal spirometry. In a crossover trial, 20 patients with CF received 4 weeks of hypertonic saline (HS) and isotonic saline (IS) in a randomised sequence separated by a 4 week washout period. The primary end point was the change in the LCI due to HS versus IS.Four weeks of twice-daily HS inhalation significantly improved the LCI compared with IS (1. 16, 95% CI 0. 26 to 2. 05; p=0. 016), whereas other outcome measures such as spirometry and quality of life failed to reach statistical significance. Randomisation order had no significant impact on the treatment effect.
The LCI, but not spirometry was able to detect a treatment effect from HS inhalation in patients with CF with mild disease and may be a suitable tool to assess early intervention strategies in this patient population. The early administration of hypertonic saline has a definite effect on improving lung function as measured by the lung clearance index – an impressive sensitive test that is steadily gaining in popularity particularly as more children with CF have normal spirometry.
Amin R, Dupuis A, Aaron SD, Ratjen F. The effect of chronic infection with Aspergillus fumigatus on lung function and hospitalization in patients with cystic fibrosis. Chest 2010; 137:171-176. [PubMed]

Fig.5 Rashma Amin sickkids.ca
The relevance of Aspergillus fumigatus in patients with cystic fibrosis (CF) not affected by allergic bronchopulmonary aspergillosis is unclear. The study was to determine the effect of persistent infection with A. fumigatus on pulmonary exacerbations and lung function in children with CF. This was a retrospective cohort study of patients with CF followed at The Hospital for Sick Children, Toronto from 1999 to 2006. Persistent A. fumigatus infection was defined as the presence of two or more positive sputum or bronchoalveolar cultures for A. fumigatus in a given year. The primary outcome measure was the annual number of hospitalizations for pulmonary exacerbations. Two hundred thirty patients with CF were included in the analysis.
The FEV(1) of patients persistently infected with A. fumigatus was 3.61% (P< or =. 0001) lower during the study period compared with uninfected patients. There was a significant interaction between A. fumigatus and Pseudomonas aeruginosa on lung function (P=. 0006). Patients not infected with either organism had the highest pulmonary function. Persistent A. fumigatus infection (relative risk [RR]=1. 94, P=. 0002) and CF-related diabetes (RR=1. 64, P=. 028) were associated with an increased risk of pulmonary exacerbations requiring hospitalization, whereas there was no increased risk of pulmonary exacerbations among patients with allergic bronchopulmonary aspergillosis (RR=1. 02, P=. 94). When adjusted for baseline pulmonary function, none of these variables were associated with a significantly increased risk of pulmonary exacerbations, with only chronic A. fumigatus infection trending toward significance (RR=1. 40, P=. 065).
The authors concluded that persistent A. fumigatus infection is an independent risk factor for hospital admissions in patients with CF.
Dr Rasma Amin (fig.5) is in the Department of Respiratory Medicine, The Hospital for Sick Children, University of Toronto, 555 University Avenue, Toronto,
Andrieux A, Harambat J, Bui S, Nacka F, Iron A, Llanas B, Fayon M. Renal impairment in children with cystic fibrosis. J Cyst Fibros 2010; 9:263-268. [PubMed]

Fig. 6 Annick Andrieux LinkedIn
A single-center retrospective study analyzing the genetic, clinical and therapeutic characteristics of 112 children. The estimated glomerular filtration rate (GFR), microalbuminuria and lithiasis risk factors were assessed. The median calculated GFR (Schwartz) was 123, 161 and 155ml/min/1. 73m(2) in children aged 1, 6 and 15years, respectively. The cumulative dose of aminoglycosides was not correlated to GFR. Microalbuminuria was present in 22/38 patients. Hyperoxaluria was observed in 58/83 patients and was associated with a severe genotype, pancreatic insufficiency and liver disease. Hypercalciuria, hyperuricuria and hypocitraturia were identified in 16/87, 15/83 and 57/76 patients, respectively.
The authors concluded that renal impairment in CF has various presentations. There appears to be low levels of renal impairment in children with CF. However, the risk of oxalocalcic urolithiasis is enhanced, and GFR may be underestimated by the Schwartz formula.
This is yet another study showing the potential for renal problems in children – presumably leading to the increasingly frequent renal problems reported in CF adults.
Dr Annick Andrieux (fig. 6) is at CHU de Bordeaux, Centre de Ressources et de Compétences de la Mucoviscidose pédiatrique, Hôpital Pellegrin Enfants, Bordeaux, France.
Brodlie M, McKean MC, Johnson GE, Gray J, Fisher AJ, Corris PA, Lordan JL, Ward C. Ceramide is increased in the lower airway epithelium of people with advanced cystic fibrosis lung disease. Am J Resp Crit Care 2010; 182:369-375. [PubMed]

Fig. 7 Malcolm Brodlie paediatric respiratory.com
Ceramide accumulates in the airway epithelium of mice deficient in cystic fibrosis transmembrane conductance regulator, resulting in susceptibility to Pseudomonas aeruginosa infection and inflammation.
Objectives: To investigate quantitatively ceramide levels in the lower airway of people with cystic fibrosis compared with pulmonary hypertension, emphysema, and lung donors using explanted lungs at the Freeman Hospital.
Staining for ceramide was significantly increased in the lower airway epithelium of people with cystic fibrosis (median, 14. 11%) compared with pulmonary hypertension (3. 03%; P = 0. 0009); unused lung donors (3. 44%; P = 0. 0009); and emphysema (5. 06%; P = 0. 01). Significantly raised levels of ceramides C16:0, C18:0, and C20:0 were detected by mass spectrometry in lungs with cystic fibrosis compared with pulmonary hypertension. Immunoreactive ceramide is increased in the lower airway epithelium of people with advanced cystic fibrosis.
– Further evidence of an increase in ceramide in infected CF airways as judged by end stage lungs removed at the time of transplantation.
Dr Malcolm Brodlie (fig. 7) is a clinical scientist and paediatrician at the Sir William Leech Centre For Lung Research, Freeman Hospital, Newcastle upon Tyne, UK.
Becker KA, Tummler B, Gulbins E, Grassme H. Accumulation of ceramide in the trachea and intestine of cystic fibrosis mice causes inflammation and cell death. Biochem Bioph Res Co 2010; 403:368-374. [PubMed]

Fig. 8 Katrin Anne Becker
Recent studies have demonstrated an accumulation of ceramide in the lungs of cystic fibrosis patients and in several mouse models. These findings showed that pulmonary ceramide concentrations play an important role in pulmonary inflammation and infection.
In this study the authors investigated whether ceramide concentrations are also altered in the trachea and the intestine of cystic fibrosis mice and whether an accumulation of ceramide in these organs has functional consequences that are typical of cystic fibrosis.
They found a marked accumulation of ceramide in tracheal and intestinal epithelial cells of cystic fibrosis mice. When acid sphingomyelinase activity is inhibited by treating cystic fibrosis mice with amitriptyline or by genetic heterozygosity of acid sphingomyelinase in cystic fibrosis mice, ceramide concentrations in the trachea and the intestine are normalized. Moreover, increased rates of cell death and increased cytokine concentrations in the trachea, the intestine, or both were normalized by the inhibition of acid sphingomyelinase activity and the concomitant normalization of ceramide concentrations.
– These findings suggest that ceramide plays a crucial role in inflammation and increased rates of cell death in several organs of cystic fibrosis mice. There is considerable interest in ceramide in recent years and the ill effects of its accumulation and inflammation in the CF cells e.g. Teichgraber et al 2008. [PubMed]. Also, the beneficial effect of amitriptyline has been reported which this study confirms (Riethmuller J. Therapeutic efficacy and safety of amitriptyline in patients with cystic fibrosis. Celle Physiol Biochem 2009; 24:65-72. above). [PubMed]
Dr Katrin Anne Becker (fig. 8) is Professor in the Dept. of Molecular Biology, University of Duisburg-Essen, Hufelandstrasse 55, D-45122 Essen, Germany.
[and next two related abstracts]
Becker KA, Riethmuller J, Luth A, Doring G, Kleuser B, Gulbins E. Acid sphingomyelinase inhibitors normalize pulmonary ceramide and inflammation in cystic fibrosis. Am J Resp Cell Mol 2010;. 42:716-724.[PubMed]
Employing genetic mouse models the authors have recently shown that ceramide accumulation is critically involved in the pathogenesis of cystic fibrosis lung disease. Genetic or systemic inhibition of the acid sphingomyelinase (Asm) is not feasible for treatment of patients or might cause adverse effects. Thus, a manipulation of ceramide specifically in lungs of CF mice must be developed. They tested whether inhalation of different acid sphingomyelinase inhibitors does reduce Asm activity and ceramide accumulation in lungs of CF mice. The efficacy and specificity of the drugs was determined. Ceramide was determined by mass spectrometry, DAG-kinase assays, and fluorescence microscopy. They determined pulmonary and systemic Asm activity, neutral sphingomyelinase (Nsm), ceramide, cytokines, and infection susceptibility. Mass spectroscopy, DAG-kinase assays, and semiquantitative immune fluorescence microscopy revealed that a standard diet did not influence ceramide in bronchial respiratory epithelial cells, while a diet with Peptamen severely affected the concentration of sphingolipids in CF lungs.
Inhalation of the Asm inhibitors amitriptyline, trimipramine, desipramine, chlorprothixene, fluoxetine, amlodipine, or sertraline restored normal ceramide concentrations in murine bronchial epithelial cells, reduced inflammation in the lung of CF mice and prevented infection with Pseudomonas aeruginosa.All drugs showed very similar efficacy. Inhalation of the drugs was without systemic effects and did not inhibit Nsm. These findings employing several structurally different Asm inhibitors identify acid sphyngomyelinase as primary target in the lung to reduce ceramide concentrations. Inhaling an Asm inhibitor may be a beneficial treatment for CF, with minimal adverse systemic effects.
Katrin Anne Becker (fig. 8) is Professor and Chair, Department of Molecular Biology, University of Duisburg-Essen, Hufelandstrasse 55, D-45122 Essen, Germany.
Becker KA, Grassme H, Zhang Y, Gulbins E. Ceramide in Pseudomonas aeruginosa infections and cystic fibrosis. [Review] Cell Physiol Biochem 2010; 26:57-66. [PubMed]
The authors discuss recent findings related to the role of sphingolipids, in particular ceramide, in cystic fibrosis and the bacterial infections associated with that disease. Ceramide accumulates in the lungs of cystic fibrosis mice and causes pulmonary inflammation, infection, and cell death, events that are corrected by the genetic deletion or pharmacological inhibition of acid sphingomyelinase; this inhibition normalizes ceramide concentrations in murine models of cystic fibrosis. Initial clinical studies suggest that pharmacological inhibition of acid sphingomyelinase may be a novel strategy for treating patients with cystic fibrosis.
Katrin Anne Becker (fig. 8) is Professor and Chair, Department of Molecular Biology, University of Duisburg-Essen, Hufelandstrasse 55, D-45122 Essen, Germany.
Bronckers A, Kalogeraki L, Jorna HJ, Wilke M, Bervoets TJ, Lyaruu DM, Zandieh-Doulabi B, Denbesten P, de Jonge H. The cystic fibrosis transmembrane conductance regulator (CFTR) is expressed in maturation stage ameloblasts, odontoblasts and bone cells. Bone 2010;46:1188-96. [PubMed]

Fig. 9 Hugo de Jonge author’s photo
Patients with cystic fibrosis (CF) have mild defects in dental enamel. The authors tested the hypothesis that Cftr channels are present and operating in the plasma membranes of mouse ameloblasts.
The authors concluded that Cftr protein locates in the apical plasma membranes of mouse maturation ameloblasts. In mouse incisors Cftr is critical for completion of enamel mineralization and conceivably functions as a regulator of pH during rapid crystal growth. They speculate that the osteopenia found in CF patients as well as in Cftr-deficient mice is likely associated with defective Cftr operating in bone cells.
Professor Hugo de Jonge (fig. 9) ( – 2022) Professor of Biochemistry Department Erasmus University Medical Centre. He describes his main area of research is the transport of anions (chloride, bicarbonate) across cellular membranes, crucial for a broad range of functions, including transport of salt and water across epithelia, the regulation of cell volume, exocytosis, pH regulation, and the control of electrical excitability of muscle and nerves. Their program focuses on CFTR.
Dr Antonius Bronckers is in the Department of Oral Cell Biology, Academic Centre for Dentistry Amsterdam (ACTA), Research Institute MOVE , University of Amsterdam and VU University Amsterdam, The Netherlands.
Carlon M, Toelen J, Van der Perren A, Vandenberghe LH, Reumers V, Sbragia L, Gijsbers R, Baekelandt V, Himmelreich U, Wilson JM, Deprest J, Debyser Z. Efficient gene transfer into the mouse lung by fetal intratracheal injection of rAAV2/6. 2. Molecular Therapy: J Amer Soc Gene Ther 2010; 18:2130-2138.[PubMed]

Fig. 10 Marianne Carlon ResearchGate
Fetal gene therapy is one of the possible new therapeutic strategies for congenital or perinatal diseases with high mortality or morbidity. The authors developed a novel delivery strategy to inject viral vectors directly into the fetal mouse trachea. Histological analysis for beta-galactosidase (beta-gal) revealed 17. 5% of epithelial cells transduced in the conducting airways and 1. 5% in the alveolar cells. Stable gene expression was observed up to 1 month after injection. The authors observe that direct injection of rAAV2/6. 2 in the fetal mouse trachea is superior for transducing the lung and this approach may be useful to evaluate fetal gene therapy for pulmonary diseases such as cystic fibrosis, requiring both substantial numbers of transduced cells as well as prolonged gene expression to obtain a stable phenotypic effect.
– There have been previous suggestions that fetal gene therapy would be necessary for people with CF (Larson et al, 1997; Cohen & Larson, 2006) although the work on which these suggestions were based was not repeatable in a careful UK study (Buckley et al, 2008). In another study (Yu ZY et al, 2007) the authors investigated vesicular stomatitis virus glycoprotein (VSVg)-pseudotyped HIV-1-derived lentivirus vector-mediated gene transfer to the airway epithelium of mid-gestation fetal lambs, both in vitro and in vivo. Even during the early pseudoglandular and canalicular phases of lung development, occurring through mid-gestation, the proximal bronchial airway epithelium was relatively mature and highly resistant to lentivirus-mediated transduction. In contrast, the more distal bronchiolar airway epithelium was relatively permissive for transduction although the absolute levels achieved remained low.
However, it is very unlikely that fetal gene therapy would ever be advisable or indeed approved for CF by the regulatory authorities at the present time.
Dr Marianne Carlon (fig.10) is in the Department of Molecular and Cellular Medicine, Katholieke Universiteit Leuven, Flanders, Belgium.
Castellani C, Macek M Jr, Cassiman JJ, Duff A, Massie J, Kate LP,, Barton D, Cutting G, Dallapiccola B, Dequeker E, Girodon E, Grody W, Highsmith EW, Kääriäinen H, Kruip S, Morris M, Pignatti PF, Pypops U, Schwarz M, Soller M, Stuhrman M, Cuppens H. Benchmarks for cystic fibrosis carrier screening: a European consensus document. J Cyst Fibros. 2010 May;9(3):165-78. doi: 10.1016/j.jcf.2010.02.005. Epub 2010 Apr 2.[PubMed] Free full text

Fig. 11 Carlo Castellani receiving the ECFS Award in 2016 from Kris de Boeck
This paper presents an overview of the conclusions from an international conference convened to address current issues related to the provision of Cystic Fibrosis carrier screening within Europe. Consensus was not aimed at stating whether such a programme should be implemented. Instead the focus was to provide a framework for countries and agencies who are considering or planning its establishment. The general principles and target population of Cystic Fibrosis carrier screening, advantages and disadvantages, health economics, monitoring and future evaluative and research directions were covered. A range of screening strategies have been assessed and compared: pre-conceptional and prenatal screening; individual and couple screening; sequential and simultaneous sampling or testing. Furthermore, technical issues were examined with respect to the choice of the panel of mutations, its detection rate, sensitivity, management of intermediate ‘at-risk’ couples, screening approach to different populations and ethnic minorities, and assurance of laboratory quality control. The consensus statement also aims to establish the benchmarks for communicating with health care providers, the general public and potential and actual participants before and after the genetic test.
– A very detailed and informative article
Dr Carlo Castellani (fig. 11) is an Italian Paediatrician and Geneticist who is involved with many aspects of research and international cooperation with the ECFS. In 2016 he received the ECFS Award.
Cheng MP, Paquette K, Lands LC, Ovetchkine P, Theoret Y, Quach C. Voriconazole inhibition of vitamin A metabolism: are adverse events increased in cystic fibrosis patients? Pediatr Pulmonol 2010; 45:661-666. [PubMed]

Fig. 12 Matthew Pellan Cheng
Twitter
Five of six CF patients receiving treatment with voriconazole developed photosensitivity, and all six patients reported visual disturbances. One 7-year-old boy developed striking erythema in the face and upper thorax; a 16-year-old girl who reported unexpected visual disturbances, including scotomas and tunneling vision. So significant adverse effects of voriconazole were noted in all treated CF patients. The authors suggest that this may be due to suppression of activity of hepatic enzymes involved in all transretinonic acid metabolism coupled with vitamin A supplementation in CF. They suggest that consideration should be given to reducing vitamin A supplementation during voriconazole treatment.
Voriconazole is used increasingly frequently to eradicate or control fungal infections such as Aspergillus which are becoming an increasing problem but the drug appears to be associated with significant side effects.
Dr Matthew Pellan Cheng (fig.12) is an ID physician & microbiologist at The Montreal Children’s Hospital, McGill University, Montreal, Canada.
Chen JH, Stoltz DA, Karp PH, Ernst SE, Pezzulo AA, Moninger TO, Rector MV, Reznikov LR, Launspach JL, Chaloner K, Zabner J, Welsh MJ. Loss of anion transport without increased sodium absorption characterizes newborn porcine cystic fibrosis airway epithelia. Cell; 143:911-923. [PubMed]

Fig. 13 Jeng-Haur Chen
HKU
Defective transepithelial electrolyte transport is thought to initiate cystic fibrosis lung disease. Yet, how loss of CFTR affects electrolyte transport remains uncertain. CFTR-(/)- pigs spontaneously develop lung disease resembling human CF. At birth, their airways exhibit a bacterial host defense defect, but are not inflamed. Therefore, the authors studied ion transport in newborn nasal and tracheal/bronchial epithelia in tissues, cultures, and in vivo.
CFTR-(/)- epithelia showed markedly reduced Cl- and HCO3- transport. However, in contrast to a widely held view, lack of CFTR did not increase transepithelial Na(+) or liquid absorption or reduce periciliary liquid depth. Like human CF, CFTR-(/)- pigs showed increased amiloride-sensitive voltage and current, but lack of apical Cl- conductance caused the change, not increased Na(+) transport. These results indicate that CFTR provides the predominant transcellular pathway for Cl- and HCO3- in porcine airway epithelia, and reduced anion permeability may initiate CF airway disease.
— The increase in sodium absorption is considered to contribute to the reduced periciliary liquid in CF but, as judged by these present results, this appears not to be the case in the CF pig.
Dr Jeng-Haur Chen (fig. 13) is in the Department of Internal Medicine, University of Iowa, Iowa City, 52242, USA.
Chen EY, Yang N, Quinton PM, Chin WC. A new role for bicarbonate in mucus formation. Am J Physiol – Lung C 2010; 299:L542-9. [PubMed]

Fig. 14 Wei-Chun Chin
ucmerced.edu
The impact of small anions on the physical properties of gel-forming mucin has been almost overlooked relative to that of cations. Recently, based on the coincident abnormalities in HCO(3)(-) secretion and abnormal mucus formed in the hereditary disease cystic fibrosis (CF), HCO(3)(-) was hypothesized to be critical in the formation of normal mucus by virtue of its ability to sequester Ca(2+) from condensed mucins being discharged from cells. However, direct evidence of the impact of HCO(3)(-) on mucus properties is lacking. Herein, the authors demonstrate for the first time that mucin diffusivity (~1/viscosity) increases as a function of [HCO(3)(-)]. This study indicates that poor HCO(3)(-) availability in CF may explain why secreted mucus remains aggregated and more viscous in affected organs. These insights bear on not only the fundamental pathogenesis in CF, but also on the process of gel mucus formation and release in general.
For some years Paul Quinton has stressed the important role of bicarbonate in the pathogenesis of CF. This paper gives a clear explanation, for us non-scientists, of the mechanism and role of the bicarbonate, or lack of it, on the mucin kinetics.
Dr Eric E Y Chen is in Bioengineering, Univ. of California at Merced, 95343, USA.
Prof. Paul Quinton is at the Division of Respiratory Medicine, Department of Pediatrics, University of California at San Diego School of Medicine, Rady Children’s Hospital, La Jolla; and the Division of Biomedical Sciences, University of California at Riverside, Riverside, California
Corresponding author is Professor Wei-Chun Chin (fig14)is professor of Bioengineering at of UC Merced
Clifton IJ, Peckham DG. Defining routes of airborne transmission of Pseudomonas aeruginosa in people with cystic fibrosis. [Review]. Exp Rev Respir Med 2010; 4:519-529. [PubMed]

Fig 15. Ian Clifton LinkedIn
The route of cross-infection between people with CF is not clear, but there is increasing evidence that an airborne route may be important. Laboratory studies have shown that P. aeruginosa can survive within droplet nuclei and can potentially remain suspended within aerosols for prolonged periods. Depending upon the air flows, this may result in the bacteria travelling significant distances. A number of clinical studies have demonstrated that people with CF can produce aerosols containing P. aeruginosa and Burkholderia cepacia complex. Infection control guidelines need to consider the possibility of droplet, including small-droplet nuclei, transmission of P. aeruginosa and other pathogens between people with CF. Further studies are needed to more accurately quantify the risk of cross-infection between people with CF and to evaluate interventions to minimize the risk.
— A number of recent studies raise the possibility of droplet airborne spread is a factor to be considered when organising cross infection measures in a CF unit.
Dr Ian Clifton (fig. 15) is Consultant Respiratory Physician, St James’s University Hospital, Leeds.
Clifton IJ, Fletcher LA, Eggs CB, Denton M, Conway SP, Peckham DG. An aerobiological model of aerosol survival of different strains of Pseudomonas aeruginosa isolated from people with cystic fibrosis. J Cyst Fibros 2010; 9:64-68. [PubMed]
Pseudomonas aeruginosa is a common and important pathogen in people with cystic fibrosis (CF). Recently epidemic strains of P. aeruginosa associated with increased morbidity, have been identified. The method of transmission is not clear, but there is evidence of a potential airborne route. The aim of this study was to determine whether different strains of P. aeruginosa isolated from people with CF were able to survive within artificially generated aerosols in an aerobiological chamber. Viable P. aeruginosa could still be detected up to 45min after halting generation of the aerosols. All of the strains of P. aeruginosa expressing a non-mucoid phenotype isolated from people with CF had a reduced ability to survive within aerosols compared to an environmental strain. Expression of a mucoid phenotype by the strains of P. aeruginosa isolated from people with CF promoted survival in the aerosol model compared to strains expressing a non-mucoid phenotype.
— Increasing evidence of airbourne transmission of P. aeruginosa between people with CF.
De Soyza A, Meachery G, Hester KL, Nicholson A, Parry G, Tocewicz K, Pillay T, Clark S, Lordan JL, Schueler S, Fisher AJ, Dark JH, Gould FK, Corris PA. Lung transplantation for patients with cystic fibrosis and Burkholderia cepacia complex infection: a single-center experience. J Heart Lung Transplant 2010; 29:1395-1404. [PubMed]

Fig. 16 Anthony De Souza nihr.ac.uk
The authors from the Freeman Hospital in Newcastle UK report the early and long-term results of a cohort of lung transplant recipients with CF and pre-operative BCC infection. Two hundred sixteen patients with CF underwent lung transplantation and 22 had confirmed pre-operative BCC infection, with 12 of these being B. cenocepacia.Nine of the 12 B. cenocepacia-infected recipients died within the first year, and in 8 BCC sepsis was considered to be the cause of death. In contrast, recipients infected with other BCC species had significantly better outcomes, with post-transplantation survival comparable to other recipients with CF.The authors conclude that the mortality in patients with B. cenocepacia infection was unacceptably high and has led to their no longer accepting patients with this condition onto the lung transplant waiting list. Long-term survival in the non-B. cenocepacia BCC group was excellent, without high rates of acute rejection or bronchiolitis obliterans syndrome (BOS) longer term, and these patients continue to be considered for lung transplantation
— This report from the UK’s leading transplant centre for people with CF (The Freeman Hospital, Newcastle) confirms the poor outlook for transplanted patients who are infected with B. cenocepacia to the extent that they are no longer transplanted.
Anthony De Soyza (fig. 16) is Professor of Pulmonary Medicine Newcastle.upon Tyne. From the Transplantation and Immunobiology Group, Institute of Cellular Medicine, Newcastle University, Newcastle-upon-Tyne, UK
Denyer J, Prince I, Dixon E, Agent P, Pryor J, Hodson M. Evaluation of the Target Inhalation Mode (TIM) breathing maneuver in simulated nebulizer therapy in patients with cystic fibrosis. J Aero Med Pulmon Drug Deliver 2010; 23 Suppl 1:S29-36. [PubMed]
Adaptive Aerosol Delivery (AAD) systems provide efficient drug delivery and improved lung deposition over conventional nebulizers by combining real-time analyses of patient breathing patterns and precisely timed aerosol delivery. Delivery and deposition are further enhanced by breathing techniques involving slow, deep inhalations. This exploratory study assessed the acceptability of slow, deep inhalations in 20 patients with cystic fibrosis (CF) during up to eight simulated nebulizer treatments with the I-neb AAD System. The breathing maneuver, Target Inhalation Mode (TIM) breathing, involved the lengthening of the patient’s inhalation time over successive breaths with guidance from auditory and tactile (vibratory) feedback from the device. At the end of the first treatment, most patients felt that the instructions were easy to understand (90%) and that the vibratory feedback was pleasant (65%). Half of the patients found the procedure to be comfortable. At the end of the final treatment, most patients felt that the breathing maneuver was easy to understand (90%) and use (80%), but that the duration of the breath was too long (100%). Logged data revealed that 90% of patients were able to comply with the breathing maneuver. The two patients unable to comply had a forced vital capacity of <1. 75 L. The average treatment time decreased from 288. 4 to 141. 6 seconds n during the first and final treatments, respectively.
The authors conclude that their study provides preliminary evidence of the acceptability of the TIM breathing maneuver in patients with CF and their ability to perform repeated TIM breathing during simulated nebulizer therapy with the I-neb AAD System
The Adaptive Aerosol is another advance in making routine inhalation therapy more acceptable to patients by increasing efficiency and reducing time spent.
John Denyer is with Philips Respironics, Respiratory Drug Delivery Ltd, Chichester, United Kingdom.
Doe SJ, McSherry A, Iceless B, Earns AM, Bright-Thomas R, Brennan AL, Webb AK, Jones AM. Patient segregation and aggressive antibiotic eradication therapy can control methicillin-resistant Staphylococcus aureus at large cystic fibrosis centres. J Cyst Fibros 2010; 9:104-109. pubmed.ncbi.nlm.nih.gov/20051329/
The prevalence of MRSA in patients with CF has risen in recent years. The authors adhere to a policy of segregation and barrier nursing to manage patients with MRSA, and actively pursue eradication of MRSA. They have evaluated their experiences of MRSA infection in their large adult CF centre. A retrospective review of all MRSA-positive patients from 1998 to 2008 was undertaken. Isolates were subjected to molecular identification to elucidate possible patient-to-patient transmission events. Eradication attempts were scrutinised. They have maintained a low incidence and prevalence (below 3%) of MRSA within this large cohort. A total of 15 pulsotypes of MRSA were identified among the 24 isolates examined, epidemiological data suggested no patient-patient transmission. Based on 6 month follow-up data, successful eradication was achieved in 81% patients. This includes those who had harboured infection for some time. Twenty-one (80. 8%) required only one course of treatment, 3 (11. 6%) patients required two different regimes and 2 (7. 5%) required three courses to fully eradicate the organism.The authors concluded that strict infection control procedures can control MRSA infection and keep the prevalence low in CF clinics. Eradication is achievable in the majority of patients even when significant time has lapsed from initial isolation. In some instances, up to 3 courses of antibiotics were required to achieve eradication.
— Encouraging experience from the Manchester Adult CF Centre showing the prevalence of MRSA can be maintained at a low level with careful monitoring, infection control procedures and aggressive treatment.
Dougherty KA, Schall JI, Stallings VA. Suboptimal vitamin K status despite supplementation in children and young adults with cystic fibrosis. Am J Clin Nutr 2010; 92:660-667. [PubMed]

Fig 17. Virginia Stallings
For children and adolescents with cystic fibrosis and pancreatic insufficiency, the efficacy of routine vitamin K supplementation to normalize vitamin K status remains unclear. This study examined and determined predictors of vitamin K status in subjects aged 8-25 yrs with CF and pancreatic insufficiency taking various vitamin K supplements. In 97 subjects, serum 25-hydroxyvitamin D [25(OH)D], dietary intake, vitamin K supplement intake, and vitamin K status was determined on the basis of the percentage of serum undercarboxylated osteocalcin (%ucOC; sufficient: lt 20%) and plasma proteins induced by vitamin K absence-factor II (PIVKA-II; n = 60; sufficient: le 2 microg/L) were assessed. The vitamin K supplementation groups were as follows: <150 microg/d (low; multivitamins or no supplement), 150-999 microg/d (middle; CF-specific vitamins), and >1000 microg/d (high; mephyton). %ucOC values were compared with 140 healthy subjects aged 6-21 y.RESULTS: In subjects with CF, the median (range) %ucOC was 35% (3%, 76%) and the median (range) for PIVKA-II was 2 (0, 42) micro g/L. Subjects with CF had a higher %ucOC with low [45% (10%, 76%)] and medium [41% (3%, 66%)] supplement intakes but not with a high supplement intake [16% (4%, 72%)] compared with healthy subjects [23% (0%, 43%); both P lt 0. 05]. Supplementation group for males and females and 25(OH)D and age for males were significant predictors of vitamin K status.
CONCLUSIONS: Vitamin K status was often suboptimal despite routine supplementation. Only subjects taking high-dose vitamin K achieved a status similar to healthy subjects, and only the vitamin K supplementation dose predicted vitamin K status for males and females. These data suggest that higher doses of vitamin K are required.It seems clear that vitamin K should be supplemented and this study suggests that high doses of > 1000 microg/d are required to achieve normal levels.
Professor Virginia Stallings (fig.17) is Professor of Pediatrics at the University of Pennsylvania School of Medicine, Director of the Nutrition Centre at the Children’s Hospital of Philadelphia. She has been involved in many national committees and advisory groups on nutrition. She is a paedaitric gastroenterologist and a specialist in nutrition and growth in children with chronic illness. She has published a great deal on the nutritional aspects of CF.
Douglas TA, Brennan S, Berry L, Winfield K, Wainwright CE, Grimwood K, Stick SM, Sly PD. Members of AREST CF and ACFBAL Trial. Value of serology in predicting Pseudomonas aeruginosa infection in young children with cystic fibrosis. Thorax 2010; 65:985-990.
A commercial P. aeruginosa multiple antigen (MAg) ELISA and an in-house exotoxin A (ExoA) ELISA were compared in two populations: a discovery population of 76 children (0. 1-7. 1 years) undergoing annual bronchoalveolar lavage (BAL)-based microbiological surveillance and a test population of 55 children (0. 1-5. 6 years) participating in the Australasian CF Bronchoalveolar Lavage Trial. In the discovery population, P. aeruginosa was cultured from BAL fluid (>=10(5) colony-forming units (cfu)/ml) in 15/76 (19. 7%) children (median age 1. 88 years). Positive MAg and ExoA serological results were found in 38 (50. 0%) and 30 (39. 5%) children, respectively. Positive (PPV) and negative (NPV) predictive values for serology at diagnosing P. aeruginosa infection (>=10(5) cfu/ml) were 0. 14 and 0. 99 respectively (MAg assay) and 0. 11 and 0. 98 (ExoA assay). In the test population, P aeruginosa was cultured from BAL fluid (>=10(5) cfu/ml) in 16/55 (29. 1%) children (median age 1. 86 years) and from oropharyngeal swabs in 32/36 (88. 9%). Positive MAg and ExoA serology was detected in 19 (34. 5%) and 33 (60. 0%) children, respectively. The PPV and NPV of serology were 0. 26 and 0. 94 respectively (MAg assay) and 0. 19 and 0. 98 (ExoA assay) and were marginally higher for oropharyngeal cultures.
The authors concluded that measuring serum antibody responses against P. aeruginosa is of limited value for detecting early P. aeruginosa infection in young children with CF.This is one of many publications over the past 30 years investigating the association of positive serology and the presence of P. aeruginosa in the airways of children with CF. The first publications were to demonstrate that P. aeruginosa was indeed a significant pathogen (Hoiby et al. Acta Paediatr Scand 1974; 63:843-848) [PubMed]) a fact that was questioned by some in the early days. This present Australian study was part of two important Australian research studies on early P. aeruginosa infection.
In the experience of these authors the tests were of limited value in detecting early P. aeruginosa and most would agree, and it is to be expected that there can be early colonisation (which by definition does not significantly involve the tissues in contrast to infection which does) of the airways before there is a significant antibody response from the tissues.
— The Leeds CF centre has been using Pseudomonas antibody results since 1986, when they were developed there by Dr Moira Brett. They find the presence of positive antibody tests an added indication for vigorous antibiotic treatment; also a persisting negative result is reassurance that chronic PA infection is not present. Sometimes an unexpected positive antibody tests leads to a more intensive search for P. aeruginosa, including a bronchoscopy, which would not otherwise have been carried out. Rising serial values in patients with chronic PA infection are an indication for more intensive antibiotic therapy. So more experience suggests that single comparison studies of cultures and antibodies, such as the present one, are less valuable than longer term studies with serial estimations.
Ellemunter H, Fuchs SI, Unsinn KM, Freund MC, Waltner-Romen M, Steinkamp G, Gappa M. Sensitivity of Lung Clearance Index and chest computed tomography in early CF lung disease. Resp Med 2010; 104:1834-1842. [PubMed].

Fig. 18 Helmut Ellementer seltenekrankheit.info
The aim of this study was to prospectively investigate the diagnostic accuracy of the lung clearance index (LCI) measured by multiple Breath Washout (MBW) in comparison to chest computed tomography (CT) in CF patients with early lung disease and normal FEV(1) (>80% pred. ). The diagnostic accuracy of the LCI for detecting CF lung disease in patients with normal FEV(1) was good when compared to CT. Results indicate that structural changes are unlikely if a normal LCI is measured.The authors suggest that serial measurements of the LCI for assessing ventilation inhomogeneity may help to identify early structural lung disease and help to reduce the individual cumulative radiation dose.
— There is increasing evidence that LCI is a sensitive measure of even mild lung involvement in CF. It has the advantage of reducing the radiation to which people with CF are exposed over a lifetime. The technique appears to be a significant advance particularly as chest involvement is less gross in children but even so the early detection of abnormalities is crucial to avoid permanent progressive damage. LCI does seem to represent a significant advance. Paul Aurora from Great Ormond Street, London has published extensively in support of the technique
Prof. Helmut Ellemunter (fig.18) is at the Department of Paediatrics, Medical University Innsbruck, CF Centre Innsbruck, Innsbruck, Austria.
Festini F, Tacetti G, Galici V, Neri S, Bisogni S, Coifi D, Braggion MP. A 1-m distance is not safe for children with cystic fibrosis at risk for cross-infection with Pseudomonas aeruginosa. Am J Infect Control 2010; 38:244-245. [PubMed]

Fig. 19 Filippo Festini scholar.google.it
Although maintaining a distance of 1 meter between persons with cystic fibrosis is a universal recommendation to prevent respiratory cross-infections such as Pseudomonas aeruginosa, evidence supporting this preventive measure is scarce. Examining 336 samples from 42 patients with CF collected experimentally from sterile surfaces after speaking and coughing, the auhtors found that transmission of P. aeruginosa beyond 1 meter is possible during both talking and coughing, although the probability is low (1.7%).
This is valuable information and similar to that from Leeds and elsewhere indicating that P. aeruginosa may travel greater distances than 1 meter with obvious implications for cross infection measures (Clifton IJ. Peckham DG. Exp Rev Respir Med 2010; 4:519-529. [PubMed]).
Gild R, Clay CD, Morey S. Aquagenic wrinkling of the palms in cystic fibrosis and the cystic fibrosis carrier state: a case-control study. Brit J Dermatol 2010; 163:1082- 1084.

Fig. 20. Rochelle Gild HealthShare
Aquagenic wrinkling of the palms (AWP) is hyperwrinkling occurring within 3 min of exposure to water. It is associated with cystic fibrosis (CF) and has been reported in a CF carrier. Twenty-one patients, 13 carriers and 15 controls were studied. Mean time to wrinkling was 11 min in controls, 7 min in carriers and 2 min in patients with CF. AWP was not seen in controls, but occurred in 80% of patients with CF and 25% of carriers. There was a significant difference between groups (P < 0. 001). The study demonstrated that AWP is a sign of both CF and the carrier state. It suggests that time to wrinkling decreases with decreased CFTR protein function. Patients presenting with AWP should be offered screening for both CF and the carrier state.
— Apologies for including yet another paper on finger wrinkling in CF which was first described by Professor Bob Elliott in New Zealand in 1974 (Lancet 1974; ii: 108. above). This present study is the first to show that finger wrinkling was increased in some 25% of CF carriers.
In an unpublished study from Leeds by Jeanette Firth there was no relation between the wrinkling time and the sweat electrolyte values. However, it would seem wise advise to exclude CF in people with significant aquagenic finger wrinkling. Also recently Garcon-Michel N et al,(Brit J Dermatol 2010; 163:162-166.[PubMed]) found the sign in 41% of people with CF.
Dr Rochelle Gild (fig.20) is a dermatologist at the Department of Dermatology, Princess Alexandra Hospital, Woolloongabba, Brisbane, Qld 4102, Australia
Gao Z, Wood-Baker R, Harle R, Muller K, Hauser J, Reid DW. “Bong lung” in cystic fibrosis: a case report. J Med Case Rep 2010; 4:371. [PubMed]
(See free PMC article via PubMed for images)
Marijuana or “bong” lung has been described recently. Subjects typically develop large peripheral paraseptal lung bullae and are predisposed to spontaneous pneumothoraces.A 23 year old man with CF developed large peripheral paraseptal lung bullae and was predisposed to spontaneous pneumothoraces related to using marijuana.A “Bong” is a water pipe, bubbler or moof filtration device used for smoking cannabis or other inhaled substances. The condition would be worth considering in patients who had problems with recurrent pneumothoraces
Dr Zoe Ga0 is in the Departments of Respiratory Medicine, Royal Hobart Hospital, Liverpool Street, Hobart, Tasmania, 7000, Australia
Ghdifan S, Couderc L, Michelet I, Leguillon C, Masseline B, Marguet C. Bolus methylprednisolone efficacy for uncontrolled exacerbation of cystic fibrosis in children. Pediatrics 2010; 125:e1259-64. [PubMed].
Four children with cystic fibrosis, deltaF508/deltaF508, who were admitted with severe respiratory distress and in whom no improvement was obtained by intensive antibiotic therapy and systemic corticosteroids. Chest computed-tomography scans showed hyperinflation and atelectasis. The severity of these exacerbations was explained neither by visible mucus plugging nor by allergic bronchopulmonary aspergillosis. The authors hypothesized that these clinical features were related to a severe inflammatory process in small airways. Therefore, a high-dose short course of methylprednisolone (1 g/1. 73 m(2) per day for 3 days) was given; all the patients’ conditions were dramatically improved, and the therapy was safe. To their knowledge, this is the first reported use of bolus methylprednisolone in the treatment of uncontrolled pulmonary exacerbation in children with cystic fibrosis.
— This is a useful paper describing a treatment possibility when there is difficulty controlling severe respiratory distress as sometimes happens in young CF infants and older patients with severe pulmonary involvement.
Dr Sufian Ghidifan is at the CF Reference Centre, Charles Nicolle University Hospital, Rouen, France.
Guy EL, Peckham DG, Brownlee KG, Conway SP, Lee TW. Cystic fibrosis coexisting with trisomy 21. J Cyst Fibros 2010; 9:330-331. [PubMed]
Previous reports of children with coexistence of cystic fibrosis and full trisomy 21 died in infancy and the oldest reported survivor being 6 years of age. This report describes a young man with genetically confirmed trisomy 21 and homozygous for the F508del cystic fibrosis mutation. Despite the diagnosis of cystic fibrosis being delayed until the age of 2 years he has reached the age of 25 years. However he has poor lung function and a continuous ambulatory oxygen requirement.
The first report of CF in a patient with Down’s syndrome was that of Milunsky A. Pediatrics 1968; 42:501-4.
Guy EL, Bosomworth M, Denton M, Conway SP, Brownlee KG, Lee TW. Serum tobramycin levels following delivery of tobramycin (TOBI) via eFlow advanced nebuliser in children with cystic fibrosis. J Cyst Fibros 2010; 9:292-295. [PubMed]
Safety and toxicity data for nebulised tobramycin are mainly derived from use of the Pari LC Plus nebuliser, yet many centres are now using advanced nebulisers, such as the eFlow. Ten children (ages 2-16 years) receiving 300mg TOBI via eFlow for clinical reasons participated. Serum tobramycin levels were obtained 1hour post nebulisation. Nine children provided samples for urinary NAG, and 10 underwent audiology.Tobramycin levels were >1mg/L in 3 children (maximum 3. 8, 2 children aged 2 years). Urine NAG/creatinine levels were raised (>0. 94micromol/min/mmol) in 5 children, 1 of these had a tobramycin level of >1mg/L. One patient had high frequency hearing loss.
The authors concluded that serum tobramycin levels over 1mg/L can occur 1h post 300mg TOBI delivered by eFlow. Raised urinary NAG levels suggest that some children may have some associated early renal toxicity.
– These results are worrying in view of the fact that the inhaled aminoglycosides are given for prolonged periods of time. Whether the “month on month off” regimen allows complete recovery of the renal tissue is unclear. Also it has been known for decades that the renal effects are to some extent cumulative. To this reviewer 300 mg bd of inhaled tobramycin has always seemed a very high dose when other studies have shown that 80 mg bd of tobramycin will prevent and eradicate early P. aeruginosa infection (Wiesemann HG et al. Pediatr Pulmonol 1998; 25:88-92. [PubMed]).
Pulmonary outcome differences in U. S. and French cystic fibrosis cohorts diagnosed through newborn screening. J Cyst Fibros 2010; 9:44-50. [PubMed]
A comparison of the longitudinal progression of lung disease in cystic fibrosis patients identified through newborn screening (NBS) in cohorts located in two different countries is a “first”.The study included 56 patients in Brittany diagnosed through NBS between 1989 and 1994 and 69 similar patients in Wisconsin between 1985 and 1994. The onset and progression of lung disease was radiographically quantified using the Wisconsin Chest X-ray (WCXR) scoring system. A single pediatric pulmonologist blinded to all identifiers scored the films. RESULTS: Generalized estimating equation analyses adjusted for age, genotype, sex, pancreatic insufficiency, and meconium ileus showed worse WCXR scores in Brittany patients compared to Wisconsin patients (average score difference=4. 48; p<0. 001). Percent predicted FEV1 was also worse among Brittany patients (p<0. 001). The finding of milder radiographically-quantified lung disease using the WCXR scoring system, as well as better FEV1 values, may be explained by variations in nutrition, environmental exposures, or health care delivery.
– This is the first long term comparison of children diagnosed by neonatal screening in two different countries. The clearly worse condition of the Brittany children compared to those born in Wisconsin is not explained. Although the suggestion was made that the French children had less rigorous infection avoidance and more hospitalizations, the bacteriological data was said to be not suitable for comparison which is unfortunate for it is likely to be relevant.
Dr Aimee C Walsh is an internist at the School of Medicine and Public Health University of Wisconsin, Madison, Wisconsin USA.
Li H, Ganta S, Fong P. Altered ion transport by thyroid epithelia from CFTR(-/-) pigs suggests mechanisms for hypothyroidism in cystic fibrosis. Exper Physiol 2010; 95:1132-1144 [PubMed]

Fig. 21 Peying Fong vet.k-state.edu
Subclinical hypothyroidism has been linked to cystic fibrosis, and the cystic fibrosis transmembrane conductance regulator (CFTR) shown to be expressed in the thyroid. The thyroid epithelium secretes Cl- and absorbs Na(+) in response to cAMP. These studies definitively demonstrate that CFTR mediates cAMP-stimulated Cl- secretion in a well-differentiated thyroid culture model and that knockout of CFTR promotes increased Na(+) absorption by a mechanism other than increased ENaC expression. These findings suggest several models for the mechanism of cystic fibrosis-associated hypothyroidism.
– Suggest reader sees the full abstract for details.
There have been a number of publications on the relationship between CF and hypothyroidism in the older literature. (Vagenakis, A G et al, Med Clin N Am 1975; 59:1075-1088.). The use of iodides to reduce sputum viscosity was common practice in the past and is mentioned by a number of authors including Harry Shwachman who mentioned their use as helpful in a number of his review articles. In a subsequent report from Shwachman and colleagues (Segall-Blank, M et al, Thyroid gland function and pituitary TSH reserve in patients with cystic fibrosis. J Pediatr 1981; 98:218-222).[PubMed] they state that, in view of the reported enhanced sensitivity to iodide-induced hypothyroidism in patients with cystic fibrosis, studies were carried out to determine the possible mechanism of this abnormality. But their findings did not delineate the mechanism whereby patients with CF develop iodide-induced hypothyroidism (also see Ruben et al, 1960 above; Dolan & Gibson, 1971 above). The present studies reported here seem to throw some light on the subject.
Dr Peying Fong (fig.21) is Associate Professor of Physiology the Department of Anatomy and Physiology, Kansas State University College of Veterinary Medicine, 1600 Denison Avenue, Manhattan, KS 66506, USA.
Handyside AH. Preimplantation genetic diagnosis after 20 years. Reproductive Biomedicine Online. 21(3):280-2, 2010 Sep. [PubMed]

Fig.22 Alan Handyside ResearchGate
Alan Handyside observes that preimplantation genetic diagnosis (PGD) should not be an option only for the few couples at risk of serious genetic conditions who can afford it. We appear to have lost sight of the original driving force behind the development of PGD, which is that most couples who carry a serious genetic disorder find it more acceptable to choose to conceive with healthy embryos tested in-vitro at preimplantation stages of development within the first week following fertilization, even if that means discarding those diagnosed as affected.
It has been shown using cystic fibrosis as an example, that the cost savings to the US health care system of providing free IVF-PGD to all carrier couples compared to the lifetime costs of medical treatment for patients affected by this disease, run to dozens of billions of dollars. With the increasing emphasis in medicine on early diagnosis and prevention of disease together with the availability of new molecular genetic diagnostic tools, a national IVF-PGD programme seems to be the next step in modern health care.
Professor Alan Handyside (fig.22) , one of the pioneers of PGD, here suggesting the need for a national IVF-PGD programme.
1989 Handyside AH, Pattinson JK, Penketh RJ, Delhanty JD, Winston RM, Tuddenham EG. Biopsy of human preimplantation embryos and sexing by DNA amplification. Lancet 1989; 1 (8634):347-349). The point is well made that “most couples who carry a serious genetic disorder find it more acceptable to choose to conceive with healthy embryos tested in-vitro at preimplantation stages of development within the first week following fertilization even if that means discarding those diagnosed as affected. ” It is likely that his logical suggestion will be taken up eventually – finances and religion permitting”.
Healy F. Mulloy E. Peirce TH. Mahony MJ. Co-morbidity in a cystic fibrosis population attending a regional clinic. Irish Med J 2010; 103:313-314.[PubMed]

Fig 23. Michael J Mahony
Pulmonary disease remains the major cause of morbidity in patients with cystic fibrosis (CF). However, of 115 patients attending a regional CF clinic the authors noted 16 cases (14%) with co-morbid conditions. Of this group, 4 of 115 patients (3.5%) had renal problems including both structural and functional defects and 4 (3.5%) had neurological disorders, 3 of which were types of epilepsy. Notably, 3 of 115 patients (2.6%) had different forms of neoplasia, all of which required significant surgical and/or chemotherapeutic intervention.
There is now increasing evidence of the association between digestive tract malignancy and CF, which further complicates management of these already complex cases.
Dr Michael Mahony (fig. 23) worked with us in Leeds at St James University Hospital for some years before moving to Limerick in Ireland in 1992 as consultant where he built up a large regional CF clinic. This was eventually housed in a purpose built CF unit in the new Paediatric Unit which opened in 2000. It was intended that an Adult CF Unit will be completed by the end of 2013 – an impressive unit for adults and teenagers with CF was opened in 2016; this would cater for 120 adults and teenagers with CF. The development of the multi-diciplinary CF service that Mike Mahony started for the mid-west of Ireland over 20 years is impressive.
Houwen RH, van der Doef HP, Sermet I, Munck A, Hauser B, Walkowiak J, Robberecht E, Colombo C, Sinaasappel M, Wilschanski M. ESPGHAN Cystic Fibrosis Working Group. Defining DIOS and constipation in cystic fibrosis with a multicentre study on the incidence, characteristics, and treatment of DIOS. J Pediatr Gastroenterol Nutr 2010; 50:38-42. [PubMed]

Fig. 24 R H J Houwen umcutrecht.nl
The aims of this study were, therefore, to seek consensus on the definitions for DIOS and constipation in patients with CF and to determine the incidence, characteristics, and treatment of DIOS in a cohort of paediatric patients with CF. During the 2005 European Society for Paediatric Gastroenterology, Hepatology, and Nutrition meeting in Porto a group of paediatric gastroenterologists discussed the definition of DIOS and constipation in CF. Subsequently, all patients younger than or equal to 18 years with complete DIOS according to the definition agreed upon and diagnosed during the years 2001 to 2005 in 8 CF centres were studied.
Distal intestinal obstruction syndrome was defined as an acute complete or incomplete faecal obstruction in the ileo-caecum, whereas constipation was defined as gradual faecal impaction of the total colon. Fifty-one episodes of DIOS in 39 patients were recorded, giving an overall incidence of 6. 2 (95% confidence interval, 4. 4-7. 9) episodes per 1000 patient-years. Of the 39 patients with DIOS, 20% experienced a relapse, 92% were pancreatic insufficient, 44% had a history of meconium ileus at birth, and 82% had a severe genotype. Conservative treatment was effective in 49 of 51 DIOS episodes (96%).
Prof. R H J Houwen (fig.24) is at the Wilhelmina Children’s Hospital, University Medical Center, Utrecht, the Netherlands.
Jones AM, Dodd ME, Morris J, Doherty C, Govan JR, Webb AK. Clinical outcome for cystic fibrosis patients infected with transmissible Pseudomonas aeruginosa: an 8-year prospective study. Chest 2010; 137:1405-9. [PubMed]
Although there is now compelling evidence for cross-infection by strains of Pseudomonas aeruginosa at some specialist cystic fibrosis centres, the clinical impact of infection by transmissible strains is unclear.
In an 8-year prospective study, the authors compared the clinical outcome of two groups of patients with CF infected by transmissible (n = 28) and sporadic strains (n = 52) of P. aeruginosa. There were no differences between the two groups in survival, annual changes in spirometry, or BMI. ; but there were differences in requirements for IV antibiotic treatment (mean [SD]: 29. 3 [21. 9] days vs 53. 1 [32. 5] days) and hospitalization (median [range]: 11. 6 [1. 1, 49. 3] days vs 23. 3 [5. 5, 103. 6] days) between patients infected with sporadic and transmissible strains of P aeruginosa, respectively.
The authors concluded that infection by transmissible P. aeruginosa does not increase mortality but is associated with increased health-care and antibiotic use for patients with CF.
— Highly transmissible strains of P. aeruginosa were described from the Liverpool paediatric CF clinic in 1996 (Cheng et al. 1996) [PubMed] and from the Manchester unit by Andy Jones and colleagues and this paper is a follow-up prospective study from Manchester comparing the outlook for patients infected with transmissible strains and sporadic strains. The results confirm that the patients with the transmissible strains have more problems, need more care and IV antibiotics but do not have an increased mortality during the 8 years of the study.
From the Manchester Adult Cystic Fibrosis Centre, University Hospitals South Manchester NHS Foundation Trust, Southmoor Rd, Manchester, M23 9LT, England.
Kessler L, Bakopoulou S, Kessler R, Massard G, Santelmo N, Greget M, Moreau F, Helms O, Bosco D, Gasche-Soccal P, Morel P, Wolf P, Berney T. GRAGIL group. Combined pancreatic islet-lung transplantation: a novel approach to the treatment of end-stage cystic fibrosis. Am J Transplant 2010; 10:1707-1712. [PubMed]

Fig. 25. Laurence Kessler remed.fr
Patients with end-stage cystic fibrosis (CF) and severe CF-related diabetes (CFRD) may benefit from combined lung-pancreatic islet transplantation.
In the present study, the authors report the long-term follow-up of four end-stage CF patients treated with combined bilateral lung and pancreatic islet transplantation from the same donor. Compared with the pre transplant period, there was a 50% reduction in mean daily insulin needs. Pulmonary function remained satisfactory in all patients.
In conclusion, their patients show that combined bilateral lung and pancreatic islet transplantation may be a viable therapeutic option for patients with end-stage CF and CFRD in cystic fibrosis.
The fact that CF Diabetes is likely to affect most adults eventually suggests that measures to prevent, alleviate or lessen the impact of the diabetes on the health and life style of the CF adult will be a welcome. Little attention has been given to the prevention of CF Diabetes even though for a number of years the islets of Langerhans produce sufficient insulin and there is a potential opportunity to arrest their destruction by an appropriate intervention.
Dr Laurence Kessler (fig.25) is at the Department of Diabetology, University Hospital, University of Strasbourg, France.
Lilley M, Christian S, Hume S, Scott P, Montgomery M, Semple L, Zuberbuhler P, Tabak J, Bamforth F, Somerville MJ. Newborn screening for cystic fibrosis in Alberta: Two years of experience. Paediatr Child Health. 2010; 15:590-594. [PubMed] Free PMC article
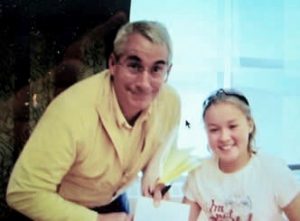
Fig 26. Mark Montgomery “accepting a certificate of appreciation from one of his “kids” from the CF clinic 11 year old Savannah Watson”
On April 1, 2007, Alberta became the first province in Canada to introduce cystic fibrosis (CF) to its newborn screening program. Of the 99,408 newborns screened in Alberta during the first two years of the program, 221 had a positive CF newborn screen. The program subsequently identified and initiated treatment in 31 newborns with CF. A relatively high frequency of the R117H mutation and the M1101K mutation was noted. The M1101K mutation is common in the Hutterite population. The presence of the R117H mutation has created both counselling and management dilemmas. The ability to offer CF transmembrane regulator full sequencing may help resolve diagnostic dilemmas. Counselling and management challenges are created when mutations are mild or of unknown clinical significance.Experience of CF neonatal screening from Alberta.
Although the lead authors are from the Molecular Diagnostic Laboratory, Alberta Health Services Edmonton, Dr Mark Montgomery (fig. 26) a leading (and obviously much appreciated) Canadian paediatrician at the Alberta Children’s Hospital, with members of the CF team in Calgary and Edmonton and the provincial laboratory services, was responsible for initiating the first province-wide newborn screening programme for CF in Canada in 2007. Following Alberta’s lead, Ontario, British Columbia, Saskatchewan, Manitoba, Nova Scotia and New Brunswick have all introduced neonatal CF screening. Surprisingly, Quebec even by 2013 had not introduced screening and called for more studies to be done. Eventually newborn CF screening was introduced into Quebec in 2018.
Lisowska A, Madry E, Pogorzelski A, Szydlowski J, Radzikowski A, Walkowiak J. Small intestine bacterial overgrowth does not correspond to intestinal inflammation in cystic fibrosis. Scand J Clin Lab Invest 2010; 70:322-326. [PubMed]

Fig. 27 Aleksandra Lisowska Centrum
The authors aimed to assess whether small bowel bacterial overgrowth (SIBO) correlates with the intestinal inflammation in CF patients described by a number of previous authors. Fecal calprotectin was measured, as an indication of inflammation, in 25 non-sputum producing CF patients and 30 healthy subjects (HS). All CF subjects were tested for the presence of SIBO using the hydrogen-methane breath test (BT). Fecal calprotectin concentrations in CF patients (range: 1. 8-302. 5; median 80. 0 mg/L) were significantly higher (p < 0. 00001) than in healthy subjects (not detectable-15. 5; 2. 5 mg/L). Calprotectin levels were abnormal in 21 (84%) studied CF subjects and none of HS. Abnormal BT results were found in 10 (40. 0%) of CF patients. Calprotectin concentrations in SIBO positive and negative patients did not differ.Gastrointestinal inflammation is a frequent finding in cystic fibrosis patients. However, small intestine bacterial overgrowth does not seem to be the major or at least is not the only determinant of intestinal inflammation. Indirect measures of intestinal inflammation in CF patients may give false positive results.
– This is another useful addition to the information available on the intestinal pathology in people with CF – a subject that has received more attention in recent years including studies using direct visualisation and biopsy techniques. The present study confirms that there is more to the inflammation, so frequently reported in CF, than the presence of bacteria in the small bowel.
Dr Aleksandra Lisowska (fig. 27) is in the Departments of Gastroenterology & Metabolism, Poznanń University of Medical Sciences, Poznań, Poland.
Mall MA, Button B, Johannesson B, Zhou Z, Levirate A, Caldwell RA, Sherbet SC, Schultz C, O’Neal WK, Preordained S, Homelier E, Rosier BC, Grubb BR, Boucher RC. Airway surface liquid volume regulation determines different airway phenotypes in Liddle compared with betaENaC-overexpressing mice. J Biolog Chem 2010; 285:26945-55. [PubMed]

Fig. 28 Marcus A Mall
Berlin Institute of Health
Studies in CF patients and mice overexpressing the epithelial Na(+) channel beta-subunit (betaENaC-Tg) suggest that raised airway Na(+) transport and airway surface liquid (ASL) depletion are central to the pathogenesis of cystic fibrosis lung disease. However, patients or mice with Liddle gain-of-function betaENaC mutations exhibit hypertension but no lung disease. To investigate this apparent paradox, the authors compared the airway phenotype (nasal versus tracheal) of Liddle with CFTR-null, betaENaC-Tg, and double mutant mice. In mouse nasal epithelium, the region that functionally mimics human airways, high levels of CFTR expression inhibited Liddle epithelial Nat channel (ENaC) hyperfunction. Conversely, in mouse trachea, low levels of CFTR failed to suppress Liddle ENaC hyperfunction. Indeed, Na(+) transport measured in Ussing chambers (“flooded” conditions) was raised in both Liddle and betaENaC-Tg mice. Because enhanced Na(+) transport did not correlate with lung disease in these mutant mice, measurements in tracheal cultures under physiologic “thin film” conditions and in vivo were performed. Regulation of ASL volume and ENaC-mediated Na(+) absorption were intact in Liddle but defective in betaENaC-Tg mice.The authors conclude that the capacity to regulate Na(+) transport and ASL volume, not absolute Na(+) transport rates in Ussing chambers, is the key physiologic function protecting airways from dehydration-induced lung disease.
Dr Marcus S Mall (fig.28) of the Division of Pediatric Pulmonology and Cystic Fibrosis Center, Department of Pediatrics III, University of Heidelberg, Im Neuenheimer Feld 430, 69120 Heidelberg, Germany; Molecular Medicine Partnership Unit, University of Heidelberg and European Molecular Biology Laboratory, Im Neuenheimer Feld 350, 69120 Heidelberg, Germany.
Massie J, Curnow L, Gaffney L, Carlin J, Francis I. Declining prevalence of cystic fibrosis since the introduction of newborn screening. Arch Dis Child 2010; 95:531-533. [PubMed]

Fig. 29 John Massie
news.com.au
Newborn screening for cystic fibrosis (CF) facilitates early diagnosis and genetic counselling for parents of affected infants. Many parents elect to use prenatal testing for subsequent pregnancies, and this may affect the prevalence of CF. The authors reviewed the records of the Victorian newborn screening programme and the clinical records of the three centres caring for patients with CF in Victoria, Australia, in order to determine the live-birth prevalence of patients with CF; before (1979-1988) and after (1989-2006) the introduction of newborn screening. Between 1979 and 1988, the live-birth prevalence of CF was 3. 96 (95% CI 3. 48 to 4. 49) per 10 000 live births. Following the introduction of newborn screening (1989-2006) the live-birth prevalence of CF was 3. 28 (95% CI 2. 97 to 3. 63) per 10 000 live births, representing a reduction of 17% (95% CI 2% to 29%, p=0. 025). In the pre screening period, there were 10 prenatal tests, which identified three affected pregnancies, all of which were terminated. In the later period, there were 304 prenatal tests (mean 17/year), of which 76 were affected, and 70 of these pregnancies were terminated.The authors observed a modest reduction in the live-birth prevalence of CF since the introduction of newborn screening. This is principally due to at-risk couples detected by newborn screening electing to use prenatal testing on subsequent pregnancies.The introduction of CF newborn screening has resulted in a reduction of the number of infants with CF being born.
– This was also the experience in East Anglia in the UK where neonatal screening was started in the early Eighties (Green MR, Weaver LT. J R Soc Med 1994; 87(Suppl 21):5-10) [PubMed]); also it has been the experience in Leeds over the last thirty years and elsewhere that the incidence of CF has fallen following the introduction of neonatal CF screening which is not surprising and to be expected.
Dr John Massie (fig.29) of the Department of Respiratory Medicine, Royal Children’s Hospital, Melbourne, Victoria 3052, Australia.
McPherson H, Rosenthal M, Bush A. Can mucoid Pseudomonas aeruginosa be eradicated in children with cystic fibrosis? Pediatr Pulmonol 2010; 45:566-568. [PubMed]
Whilst the non-mucoid strain can be eradicated in the early stages, it is believed that mucoid PsA is difficult, if not impossible, to eradicate. Children aged under 16 with a confirmed diagnosis of CF and mucoid PsA on respiratory tract culture during a defined 9-year period were eligible for inclusion. One hundred sixteen children had the minimum dataset, and of these patients 67 (58%) cleared mucoid PsA for more than 1 year. Of the 67 patients who cleared mucoid PsA for more than 1 year, 38 (57%) patients remained clear of mucoid PsA at the last available culture (median 30, range 2-106 clear cultures, and median 55, 12-103 months clear). The authors concluded that isolation of mucoid PsA does not necessarily equate to lifelong infection and suggest that trials of eradication of mucoid PsA at first isolation are required.
— Yes is the reassuring answer – mucoid strains of P. aeruginosa can be eradicated and this conforms to experience of smaller numbers of patients.
Dr Helen McPherson is at the University of Aberdeen, Aberdeen, Scotland, UK. The study appears to be from the Royal Brompton Hospital, London.
MacDuff A, Tweedie J, McIntosh L, Innes JA. Pneumothorax in cystic fibrosis: prevalence and outcomes in Scotland. J Cyst Fibros 2010; 9:246-249. [PubMed]

Fig 30. Alistair Innes
A total of 22 episodes of pneumothorax occurred in 20 patients in 3 Scottish CF centres over a 12 year period. 2 patients died as a result of the pneumothorax. 16 pneumothoraces were treated by insertion of an intercostal drain and 8 by observation. 8 patients suffered a prolonged air leak. 5 patients were treated with pleurodesis. Pneumothorax was associated with a small decline in lung function which persisted for at least 1year. Pneumothorax can present a challenge to treat in adult CF. However successful outcomes can be achieved even in cases of prolonged air leaks. Current national guidelines help in selecting optimal pleural interventions.A recent account of experience with pneumothoraces is welcome and as the adult population increases in relation to children, it is likely that the increase in this complication will continue. Pneumothorax is now very rare in the children with CF as evidenced by virtually no instances in children recorded in the recent UK Annual Patient Registry reports.
Dr Alistair Innes (fig. 30) is Consultant in Respiratory Medicine in Edinburgh. He has special interests in lung physiology and cystic fibrosis, and is involved in the UK Cystic Fibrosis Gene Therapy Consortium research program. Alistair is also editor of Davidson’s Essentials of Medicine.
Mandrusiak A, Giraud D, MacDonald J, Wilson C, Watter P. Muscle length and joint range of motion in children with cystic fibrosis compared to children developing typically. Physiotherapy Canada 2010; 62:141-146. [PubMed]

Fug. 31 Allison Mandrusiak shrs.uq.edu.au
Thirty eight children with CF had significantly shorter pectoralis minor, pectoralis major, and gastrocnemius-soleus muscles and significantly greater range of shoulder horizontal abduction than matched controls.
The altered range of movement identified in these children with CF, strengthened the rationale to support proactive physiotherapy management of the musculoskeletal system, aiming to optimize function across the increasing lifespan.
This is another area where consideration is being given to an abnormality which may cause problems in the distant future in view of the steadily increasing length of survival of the majority of patients.
Associate Professor Allison Mandrusiak (fig.31) is in the Division of Physiotherapy, The University of Queensland, Brisbane, Queensland, Australia.
Maeda Y, Stanley T, Stirling J, Griffiths M, Calvert A, Stuart Elborn J, Cherie Millar B, Goldsmith CE, Rendall J, Loughrey A, Rooney PJ, Moore JE. No evidence of transmission of bacteria between reptiles and a CF patient – a case report of a young adult CF patient and reptiles. Zoonoses & Public Hlth 2010; 57:e47-53. [PubMed]
A microbiological study was undertaken to assess the risk of infection to a CF patient from a collection of pet reptiles, particularly atypical mycobacteria. This study helped to verify that the reptiles under the care of the CF patient did not harbour bacterial organisms that would normally be pathogenic to CF patients. However, the chronic carriage of Pseudomonas aeruginosa and other pathogens in the CF patient may constitute a greater risk of infection to the animals being handled.
Therefore, stringent infection control precautions by CF patients and their pets are indicated, particularly adherence to hand washing and disinfection, when handling the animals, their litter or when working with their immediate environment, to potentially minimize the spread of bacterial and other pathogens from animal to human and vice versa. Detailed risk assessments therefore need to be undertaken by clinicians and veterinarians to detail working models that protect both animals and patients from pathogens originating from the other.This single case report draws attention to the potential risks from reptiles and similar pets which have been reported a potential source of infection for people with CF. (www. PetEducation. com Common bacterial infections in Turtles and Tortoises).
From Northern Ireland Public Health Laboratory, Department of Bacteriology, Belfast City Hospital, Belfast, UK.
Meyerholz DK, Stoltz DA, Namati E, Ramachandran S, Pezzulo AA, Smith AR, Rector MV, Suter MJ, Kao S, McLennan G, Tearney GJ, Zabner J, McCray PB Jr, Welsh MJ. Loss of cystic fibrosis transmembrane conductance regulator function produces abnormalities in tracheal development in neonatal pigs and young children. Am J Resp Crit Care 2010; 182:1251-1261.[PubMed]

Fig. 32 David Myerholz Carver College of Medicine
etailed studies of the trachea of CF pigs and young children with CF revealed three abnormalities in the pigs. The trachea and main bronchi were narrow, the trachea was less circular than controls, the tracheal smooth muscle was abnormal and submucosal glands were hypoplastic. A less circular trachea was also present in scans from children with CF less than 2 years old and there was a reduced tracheal lumen in neonates with CF.
– So these changes appear to begin in fetal life. This finding would explain the occasional infant with CF who seems to have a difficult chronic tight wheezy cough as occurs in infants with tracheomalacia and whose symptoms are not amenable to treatment with bronchodilators, antibiotics or steroids but gradually improve with time as the infant grows and the airways increase in size.
Dr David Myerholz (fig 32) is in the Department of Pathology, University of Iowa, Iowa City, 52242, USA
Meyerholz DK, Stoltz DA, Pezzulo AA, Welsh MJ. Pathology of gastrointestinal organs in a porcine model of cystic fibrosis. Am J Pathol 2010; 176:1377-89. [PubMed]
To better understand the initial stages of CF, the authors studied the gastrointestinal pathology of CFTR-/- pigs. By studying newborns, they avoided secondary changes attributable to environmental interactions, infection, or disease progression. Lesions resembling those in humans with CF were detected in intestine, pancreas, liver, gallbladder, and cystic duct. These organs had four common features. First, disease was accelerated compared with that in humans, which could provide a strategy to discover modifying factors. Second, affected organs showed variable hyperplastic, metaplastic, and connective tissue changes, indicating that remodeling was a dynamic component of fetal life. Third, cellular inflammation was often mild to moderate and not always present, which raises new questions as to the role of cellular inflammation in early disease pathogenesis. Fourth, epithelial mucus-producing cells were often increased, producing a striking accumulation of mucus with a layered appearance and resilient structure. Thus, mucus cell hyperplasia and mucus accumulation play prominent roles in early disease. These findings also have implications for CF lung disease, and they lay the foundation for a better understanding of CF pathogenesis.
— This is a very interesting report of the early changes in the gastrointestinal organs of CF pigs. Just as the CF mice were a major advance in 1992/3 so the porcine CF model is proving of immense value.
Middleton PG, House HH. Measurement of airway ion transport assists the diagnosis of cystic fibrosis. Pediatr Pulmonol. 2010 Aug;45(8):789-95. [PubMed]

Fig 33. Peter Middleton author’s photo
Nasal PD was tested using the standard protocol of baseline, amiloride, low chloride, and isoproterenol solutions in 40 healthy non-CF volunteers, 46 CF subjects, and 78 subjects referred for investigation of possible CF. In the diagnostic cohort 58 were given a non-CF diagnosis, 16 had CF confirmed, but 4 remained indeterminate. The subject is reviewed in detail.
Peter Middleton (fig. 33) is Associate Professor at the CF Unit, Westmead Millenium Institute, Sydney. He has published widely on various aspects of diagnosis, management, gene therapy and also contributed to various national and international working parties and consensus groups.
Minasian C, Wallis C, Metcalfe C, Bush A. Comparison of inhaled mannitol, daily rhDNase and a combination of both in children with cystic fibrosis: a randomised trial. Thorax 2010; 65:51-56. [PubMed]
This is the first therapeutic trial of inhaled mannitol in children with CF; it was compared with recombinant human deoxyribonuclease (rhDNase), the current best established mucolytic treatment. 38 children were recruited to an open crossover study. Subjects underwent an initial bronchial provocation challenge with dry powder mannitol. Those children with a negative challenge were randomly allocated to one of three consecutive 12-week treatment blocks (inhaled mannitol alone, nebulised rhDNase alone and mannitol + rhDNase)
.The authors concluded that inhaled mannitol was at least as effective as rhDNase after 3 months treatment. There was a marked individual variation in tolerance to mannitol and in response to treatment. Children who do not respond to rhDNase many benefit from a trial of inhaled mannitol. The combination of mannitol and rhDNase was not useful.
— Although small numbers and a high drop out rate, this is a useful study for clinicians treating children with CF. However, inhaled mannitol never proved popular with children or adults. It is not mentioned in the CFFoundation patient Registry for 2021 and only used by 3% of UK patients- mostly adults.
From the Royal Brompton Hospital & Imperial College, London, UK.
McIlwaine MM, Wong LT, Chillers M, Davidson GF. Long-term comparative trial of two different physiotherapy techniques; postural drainage with percussion and autogenic drainage, in the treatment of cystic fibrosis. Pediatr Pulmonol 2010; 45:1064-1069. [PubMed]

Fig 34 Maggie McIlwaine author’s photo
In N. America, over the past decade, various airway clearance techniques (ACT) have been introduced for the treatment of cystic fibrosis (CF). These Canadian authors hypothesized that autogenic drainage (AD), an ACT developed in Belgium, would be as effective as postural drainage with percussion (PD) in treating patients with CF. They were similar but the patients preferred the autogenic drainage as 10 of 17 receiving autogenic drainage refused to change to postural drainage after a year.
Maggie McIlwaine (fig. 34) is senior physiotherapist at the Cystic Fibrosis Clinic, BC’s Children’s Hospital, Vancouver, BC, Canada.
Mitomo K, Griesenbach U, Inoue M, Somerton L, Meng C, Akiba E, Tabata T, Ueda Y, Frankel GM, Farley R, Singh C, Chan M, Munkonge F, Brum A, Xenariou S, Escudero-Garcia S, Hasegawa M, Alton EW. Toward gene therapy for cystic fibrosis using a lentivirus pseudotyped with Sendai virus envelopes. Mol Ther 2010; 18:1173-1182. Free PMC article. pubmed.ncbi.nlm.nih.gov/20332767/
Gene therapy for cystic fibrosis (CF) is making encouraging progress into clinical trials. However, further improvements in transduction efficiency are desired.
To develop a novel gene transfer vector that is improved and truly effective for CF gene therapy, a simian immunodeficiency virus (SIV) was pseudotyped with envelope proteins from Sendai virus (SeV), which is known to efficiently transduce unconditioned airway epithelial cells from the apical side. This novel vector was evaluated in mice in vivo and in vitro directed toward CF gene therapy.
Katsuyuki Motimo is based at the DNAVEC Corporation, Tsukuba, Japan.
Mohan K, Lakshman V, Fothergill JL, Ledson MJ, Winstanley C, Walshaw MJ. Empyema due to a highly transmissible Pseudomonas aeruginosa strain in an adult cystic fibrosis patient. J Med Microbiol 2010; 59:614-616. [PubMed]

Fig. 35 Kamlesh Mohan ResearchGate
Despite the predilection of P. aeruginosa for the lungs of CF people, infection of the pleura is much less common and is not well described in the CF population. These authors describe what is believed to be the first case of pleural empyema due to a particularly pathogenic transmissible strain of P. aeruginosa (the Liverpool epidemic strain) in an adult CF patient. Yet another complication related to the Liverpool epidemic strain of P. aeruginosa
Dr Kamlesh Mohan (fig.35) is a Consultant Respiratory Physician at the Adult Cystic Fibrosis Unit, Liverpool Heart and Chest Hospital, Thomas Drive, Liverpool L14 3PE, UK.
Molyneux ID, Moon T, Webb AK, Morice AH. Treatment of cystic fibrosis associated cutaneous vasculitis with chloroquine. J Cyst Fibros 2010; 9:439-441. [PubMed]
Vasculitis is a well recognised complication of cystic fibrosis. Corticosteroids are the mainstay of treatment but some cases can be resistant and may require additional disease modifying agents. The authors describe a case of steroid resistant cutaneous vasculitis which was successfully treated with chloroquine in addition to corticosteroids and a subsequent relapse successfully treated with chloroquine alone
Ian D Molyneux is in the Department of Respiratory Medicine, Castle Hill Hospital, Castle Road, Cottingham, HU16 5JQ, UK.
Moss RB. Allergic bronchopulmonary aspergillosis and Aspergillus infection in cystic fibrosis. [Review] Current Opinion in Pulmonary Medicine 2010; 16:598-603. [PubMed]

Fig 36. Richard Moss author’s photo
Recent literature on Aspergillus fumigatus infection and allergy in cystic fibrosis have expanded our understanding of many aspects of allergic bronchopulmonary aspergillosis, and bring new attention to A. fumigatus airways infection and A. fumigatus allergy without allergic bronchopulmonary aspergillosis (ABPA) RECENT FINDINGS: ABPA, A. fumigatus infection and A. fumigatus allergy without ABPA all likely worsen cystic fibrosis (CF) lung disease. Studies examining utility of new serologic assays for diagnosing ABPA include evaluations of standardized measurement of A. fumigatus-specific IgG, serum chemokine TARC levels, and recombinant A. fumigatus allergens; as yet, none appear ideal. Although oral glucocorticoids remain primary therapy, toxicity and incomplete control have led to an ongoing search for further safe and effective agents including itraconazole and voriconazole, intravenous pulse methylprednisolone, nebulized amphotericin B and omalizumab. Little controlled treatment data is available. SUMMARY: Diagnosis of CF-ABPA remains difficult, but improvements in serologic assays are occurring. Treatment remains in many cases unsatisfactory, and new agents offer promise but await proper controlled trials of safety and efficacy. A. fumigatus airway infection and A. fumigatus allergy without ABPA are emerging as further complications of A. fumigatus respiratory colonization in patients with CF, but prospective studies are needed to corroborate largely retrospective findings,
Dr Richard Moss (fig. 36) of Stanford University is one of N. America’s leading CF clinicians and researchers. He has a major interest in the pathogenesis of chronic airways diseases of childhood particularly immunoregulation of inflammation in cystic fibrosis. In the arena of clinical research, as a member of the CFF Therapeutics Development Network his research group conducts many trials. His wide interests include aerosol therapy, gene vectors and corrrection of CFTR-dependent cell biology defects and new treatments for CF complications such as diabetes and osteoporosis, internet-based disease management, and trials of asthma drugs.
Muchekehu RW, Quinton PM. A new role for bicarbonate secretion in cervico-uterine mucus release. J Physiol 2010; 588:2329-42. [PubMed]

Fig. 37 Ruth Muchekehu
www.physoc.or
Cervical mucus thinning and release during the female reproductive cycle is thought to rely mainly on fluid secretion. However, we now find that mucus released from the murine reproductive tract critically depends upon concurrent bicarbonate (HCO(3)(-)) secretion. Prostaglandin E(2) (PGE(2))- and carbachol-stimulated mucus release was severely inhibited in the absence of serosal HCO(3)(-), HCO(3)(-) transport, or functional cystic fibrosis transmembrane conductance regulator (CFTR). In contrast to mucus release, PGE(2)- and carbachol-stimulated fluid secretion was not dependent on bicarbonate or on CFTR, but was completely blocked by niflumic acid. The authors found stimulated mucus release was severely impaired in the cystic fibrosis F508 reproductive tract, even though stimulated fluid secretion was preserved.
Thus, CFTR mutations and/or poor bicarbonate secretion may be associated with reduced female fertility associated with abnormal mucus and specifically, may account for the increased viscosity and lack of cyclical changes in cervical mucus long noted in women with cystic fibrosis.
Further evidence on the role of bicarbonate in mucus formation from Paul Quinton.
Ruth W Muchekehu (fig.37) is in the Department of Pediatrics-0830, School of Medicine, University of California–San Dieg

Fig. 38 Leyla Osman LinkedIn
Osman LP, Roughton M, Hodson ME, Pryor JA. Short-term comparative study of high frequency chest wall oscillation and European airway clearance techniques in patients with cystic fibrosis. Thorax 2010; 65:196-200. [PubMed]
High frequency chest wall oscillation (HFCWO) is standard treatment for airway clearance in the USA and has recently been introduced in the UK and Europe. There is little published research comparing HFCWO with airway clearance techniques (ACTs) frequently used in the UK and Europe. The aim of this study was to compare the short-term effects of HFCWO with usual ACTs in patients with cystic fibrosis hospitalised with an infective pulmonary exacerbation.A 4-day randomised crossover design was used. Significantly more sputum was expectorated during a single treatment session and over a 24 h period (mean difference 4. 4 g and 6. 9 g, respectively) with usual ACTs than with HFCWO (p<0. 001). No statistically significant change in FEV(1)% or oxygen saturation was observed after either HFCWO or usual ACTs compared with baseline. 17 patients (55%) expressed a preference for their usual ACT.
The authors concluded during both a finite treatment period and over 24 h, less sputum was cleared using HFCWO than usual ACT. HFCWO does not appear to cause any adverse physiological effects and may influence adherence.
— This study from the Royal Brompton, London exemplifies the lack of enthusiasm for the HFCWO method shown by UK physiotherapists!!! The fact that the majority of US patients use HFCWO and virtually no UK patients do is interesting. Undoubtedly, the cost of the apparatus (c. £10,000 in the UK) is a major deterrent in the UK – although the cost is shouldered by the medical insurance in the USA; but the lack of enthusiasm of the UK physiotherapists is another significant factor . Certainly, individual UK patients who have used “the vest” at home have been quite enthusiastic.
Leyla Osman (fig.38) is Senior Consultant Physiotherapist at Guy’s and Thomas’ NHS Foundation Trust. Population Genetics and Gene Therapy, National Heart and Lung Institute, Imperial College, London, UK
Proesmans M, Vermeulen F, Vreys M, De Boeck K. Use of nebulized amphotericin B in the treatment of allergic bronchopulmonary aspergillosis in cystic fibrosis. Int J Pediatr 2010; 37:62-87. [PubMed]

Fig. 39 Marijke Proesmans UZ Leuven
Allergic bronchopulmonary aspergillosis (ABPA) often recurs when the corticosteroid treatment is reduced. These authors report successful steroid withdrawal without relapse over 12 months in 6 of 7 patients with difficult ABPA treated with nebulised amphotericin B.Just as corticosteroids, antibiotics, rhDNase are effective via the nebulised route it is not surprising that so is nebulised amphotericin. We found this treatment to be useful in a child with a mixed fungal infection of the airways and its use seems logical in troublesome Aspergillus infection to eradicate or reduce the quantity of the antigen from the airways. Also Aspergillus causing bronchitis, as distinct from allergic bronchopulmonary aspergillosis, is now well described (Shoseyov D et al. Chest 2006; 130:222-226.[PubMed]).
Marijke Proesmans (fig.39) is in the Department of Pediatrics, Cystic Fibrosis Reference Center, University Hospitals Leuven, 3000 Leuven, Belgium.
Quinton PM. Role of epithelial HCO3- transport in mucin secretion: lessons from cystic fibrosis. [Review] Am J Physiol – Cell Physiology 2010; . 299:C1222-33. [PubMed]

Fig.41 Hans Henriksen Ussing Journals

Fig. 40 Paul Quinton ResearchGate
Paul Quinton observed that the invitation to present the 2010 Hans Ussing lecture for the Epithelial Transport Group of the American Physiological Society offered him a unique, special, and very surprising opportunity to join in saluting a man whom he met only once, but whose work was the basis, not only for his career, but also for finding the molecular defect in the inherited disease cystic fibrosis (CF). In this context,he would venture to make the tribute with a new explanation of why a mutation in a single gene that codes for an anion channel can cause devastation of multiple epithelial systems with pathogenic mucus. In so doing, he hoped to raise awareness of a new role for that peculiar anion around which so much physiology revolves, HCO(3)(-).
Quinton begins by introducing CF pathology as he questioned the name of the disease as well as the prevalent view of the basis of its pathology by considering: 1) mucus, 2) salt, and 3) HCO(3)(-). He then presents recent data showing that HCO(3)(-) is required for normal mucus discharge, and will close with conjecture as to how HCO(3)(-) may support mucus discharge and why the failure to transport this electrolyte is pathogenic in CF.
Paul Quinton has published a great deal on the importance of the bicarbonate transport in cystic fibrosis. Here he reviews the subject in a lecture to the American Physiological Society the full text of which is available without cost on the website of their journal (Am J Physiol – Cell Physiol 2010; 299:C1222-33).
Rickert S, Banuchi VE, Germana JD, Stewart MG, April MM. Cystic fibrosis and endoscopic sinus surgery: Relationship between nasal polyposis and likelihood of revision endoscopic sinus surgery in patients with cystic fibrosis. Arch Otolaryngol 2010; 136:988- 992. [PubMed]

Fig. 42 Scott Rickert NYU Langone Health
The authors graded the extent of nasal polyposis endoscopically in a cystic fibrosis population before the first surgical intervention, they observed the patients prospectively and recorded the need for revision endoscopic sinus surgery, and compared this among the individual polyp grading groupings.
There were significant differences depending on the polyp grading – more polyps more recurrent surgery required.
Although the findings were to be expected they are included as there is relatively little published on sinus and polyp problems although they are a major chronic problem for many people with CF.
Scott Rickert (fig.42) is an ENT-otolaryngologist in the Department of Otorhinolaryngology-Head and Neck Surgery, Weill Cornell Medical College, New York-Presbyterian Hospital, New York, NY 10021, USA.
Rogan MP, Reznikov LR, Pezzulo AA, Gansemer ND, Samuel M, Prather RS, Zabner J, Fredericks DC, McCray PB Jr, Welsh MJ, Stoltz DA. Pigs and humans with cystic fibrosis have reduced insulin-like growth factor 1 (IGF1) levels at birth. Proc Nat Acad Sci 2010; 107:20571-5. [PubMed]

Fig. 43 Mark P Rogan medicalindependent.ie
People with cystic fibrosis (CF) exhibit growth defects. That observation has been attributed, in part, to decreased insulin-like growth factor 1 (IGF1) levels, and the reduction has been attributed to malnutrition and pulmonary inflammation. However, patients with CF already have a reduced weight at birth, a manifestation not likely to be secondary to poor intrauterine nutrition or inflammation. Also CF pigs were smaller than their non-CF littermates and had lower IGF1 levels.To better understand the basis of IGF1 reduction, the authors studied newborn CF pigs and found low IGF1 levels within 12 hours of birth. Moreover, humerus length and bone mineral content were decreased, consistent with less IGF1 activity in utero. These findings led them to test newborn humans with CF, and they found that they also had reduced IGF1 levels.
Discovering lower IGF1 levels in newborn pigs and humans indicates that the decrease is not solely a consequence of malnutrition or pulmonary inflammation and that loss of cystic fibrosis transmembrane conductance regulator function has a more direct effect. Consistent with this hypothesis, they discovered reduced growth hormone release in organotypic pituitary slice cultures of newborn CF pigs.These findings may explain the long-standing observation that CF newborns are smaller than non-CF babies and why some patients with good clinical status fail to reach their growth potential. The results also suggest that measuring IGF1 levels might be of value as a biomarker to predict disease severity or the response to therapeutics. Finally, they raise the possibility that IGF1 supplementation beginning in infancy might be beneficial in CF.
– These very interesting findings do explain the suboptimal growth of some CF infants despite optimal treatment and a good clinical condition. Also they provide a very plausible explanation for the well documented reduced birth weight of CF infants as a group. Various studies have shown that growth hormone has some value in improving growth of CF children (see TOPICS – ENDOCRINOLOGY) but as yet IGF-1 supplementation has not been reported although the relationship of growth and IGF-1 has been described in CF (2009 Switzer M. Rice J. Rice M. Hardin DS. Insulin-like growth factor-I levels predict weight, height and protein catabolism in children and adolescents with cystic fibrosis. J Pediatr Endocrinol 2009; 22:417-424).
Dr Mark P Rogan (fig.43) is at Waterford Regional Hospital, Waterford Ireland. At this time he was in the Department of Internal Medicine Roy J and Lucille A Carver College of Medicine, University of Iowa, Iowa City.
Ratjen F, Munck A, Kho P. Angyalosi G. ELITE Study Group. Treatment of early Pseudomonas aeruginosa infection in patients with cystic fibrosis: the ELITE trial. Thorax 2010; 65:286-291. [PubMed].

Fig. 44 Felix Ratjen
Sick Kids Research Institute
The optimal therapeutic regimen and duration for early treatment of P. aeruginosa remains unclear. The Early Inhaled Tobramycin for Eradication (ELITE) study was designed to assess the efficacy and safety of two regimens (28 and 56 days) of tobramycin inhalation solution (TIS) 300 mg/5 ml twice daily for the treatment of early onset P. aeruginosa infection in patients with CF.
In this open-label randomised multicentre study, patients with CF (aged > or = 6 months) with early P. aeruginosa infection were treated for 28 days with TIS twice daily administered by the PARI LC PLUS (PARI GmbH, Starnberg, Germany) jet nebuliser.
After 28 days, patients were randomised 1:1 to either stop TIS (n=45) or to receive a further 28 days of TIS (n=43). The primary endpoint was the median time to recurrence of P. aeruginosa (any strain). Secondary endpoints included the proportion of patients free of P. aeruginosa infection 1 month after cessation of therapy and safety assessments. The median time to recurrence of P aeruginosa (any strain) was similar between the two groups.
In total, 93% and 92% of the patients were free of P aeruginosa infection 1 month after the end of treatment and 66% and 69% remained free at the final visit in the 28-day and 56-day groups, respectively. TIS was well tolerated.
The authors concluded that treatment with TIS for 28 days is an effective and well tolerated therapy for early P aeruginosa infection in patients with CF.
— This is useful information but two points deserve comment. First, this is a large dose of inhaled tobramycin for small children and infants aged 6 months – 80mg would have probably been just as effective as judged by previous European experience (Weismann HG, et al. Pediatr Pulmonol 1998; 25:88-92; Ratjen F, et al. Lancet 2000; 358:983-984; Munck A et al. Pediatr Pulmonol 2001; 32:288-292.[PubMed]).
Second, there is now increasing evidence that inhaled aminoglycosides are absorbed in sufficient amounts to affect renal function (Guy EL et al. Serum tobramycin levels following delivery of tobramycin (Tobi) via eFlow advanced nebuliser in children with cystic fibrosis. J Cyst Fibros 2010; 9:292-295. [PubMed]). Considerations of cost of the dose of tobramycin used will be relevant in countries where funding of treatment is a problem.
Rhodes B, Nash EF, Tullis E, Pencharz PB, Brotherwood M, Dupuis A, Stephenson A. Prevalence of dyslipidemia in adults with cystic fibrosis. J Cyst Fibros 2010; 9:24-28. [PubMed]
A high fat high calorie diet is advocated for patients with cystic fibrosis (CF) however the lipid profiles of individuals with CF, including those with CF-related diabetes (CFRD), are not well studied. The authors conducted a retrospective review of adult CF patients attending St Michael’s Hospital between January 2005 and December 2007. 334 patients (77% pancreatic insufficient (PI)) were included in the study. Mean HDL cholesterol was significantly lower in males (p<0. 0001) with 44% of males having HDL cholesterol <38. 7mg/dL(1mmol/L). Pancreatic sufficient patients were more likely than PI subjects to have total cholesterol >201mg/dL(5. 2mmol/L) (p<0. 01). 5% of subjects had triglyceride concentrations >195mg/dL(2. 2mmol/L). Diabetes was diagnosed in 23% of subjects. Lipid profiles were similar between diabetics and non-diabetics. Total cholesterol and triglycerides both increased with increasing age and increasing BMI (p<0. 01).
The authors concluded that dyslipidemia occurs in CF patients however no differences in lipid profiles were seen between those with diabetes and those without. They suggested that fasting lipids should be monitored in CF patients, particularly those with PS, older age, and high BMI. As survival in CF increases, the prevalence of dyslipidemia may increase resulting in clinically important complications.
Bronwen Jane Rhodes at this time was on a Fellowship at the Toronto Adult Cystic Fibrosis Program, St. Michael’s Hospital, 30 Bond Street, 6th Floor, Toronto, ON, Canada. Subsequently she is a senior doctor in the respiratory services at Waitaha, Canterbury, New Zealand.
Smyth AR, Safely PM, Ortori CA, Righet ti K, Lewis S, Erskine P, Holland ED, Gibson M, Williams P, Camarnba M, Barrett DA, Knox A. Garlic as an inhibitor of Pseudomonas aeruginosa quorum sensing in cystic fibrosis pilot randomized controlled trial. Pediatr Pulmonol 2010; 45:356-362. [PubMed]

Fig. 45 Alan Smyth Cystic Fibrosis Trust
The first clinical trial in man of a QS inhibitor. The authors randomized 34 patients to garlic or olive oil capsules (both 656 mg daily). Clinical outcomes and safety bloods were measured at baseline and after 8 weeks treatment. In this exploratory study, analysis was per protocol. Eight patients withdrew, leaving 26 for analysis (13 garlic). Garlic capsules were well tolerated. Although there was no significant effect of garlic compared to placebo in this pilot study, there was a suggestion of improvement with garlic which the authors suggested should be investigated in a larger trial.
— This is a disappointing result. Although there is a vast literature on the medicinal properties of garlic it is likely there would be few clinicians who would recommend their patients be included in a larger trial particularly as subjects for clinical trials are in short supply.
Alan Smyth (fig.45) is Professor of Paediatrics in Nottingham University UK.
Schechter MS, Gutierrez HH. Improving the quality of care for patients with cystic fibrosis. Curr Opin Pediatrics 2010; 22:296-301. [PubMed]

Fig 46. Michael Schechter
Initiatives considered to improve CF care over the past decade include the refinement of a sophisticated patient registry that allows a comparison of center processes and outcomes; development of evidence-based and consensus-based guidelines regarding standards of care; cultural transformation, including the training of care center teams in a systems-oriented approach to quality improvement; data transparency; and encouragement of a patient-centered and family-centered orientation. Cystic Fibrosis Foundation initiatives have promoted an increase in the consistent provision of evidence-based care and the promulgation of innovative, proactive therapeutic approaches. Unfortunately, so far most of these accomplishments have not been documented in peer-reviewed research articles, but rather in platform presentations at national meetings, meeting abstracts, data reports to center directors, and published reports from individual centers. While several new medications for CF lung disease have been introduced in the last decade, improvements in outcomes have been largely due to refinements in the delivery of care. At this point, the most efficient and reliably effective technique for promoting further improvement still needs to be identified. Recent discussions have centered on attempts at new innovative approaches that utilize more selective teaching of relevant systems-based quality improvement methods in the specific CF environment.
Dr Michael Schechter (fig.46) is at the Department of Pediatrics, Division of Pulmonary, Allergy/Immunology, Cystic Fibrosis and Sleep, Emory University School of Medicine, Children’s Healthcare of Atlanta, Atlanta, Georgia 30322, USA. He has made major contributions to improving care of people with CF. Here he summarises some of the main areas where changes have resulted in a better outlook for people with CF – at this stage changes in these areas far exceeding any specific new drug therapy. I suppose one should add “in recent years” as the introduction of penicillin and broad spectrum antibiotics in the Forties and Fifties were certainly drugs that revolutionised the outlook for people with CF. The advantages of CF centre care have been appreciated by most people for over 25 years – here some of the features are detailed and are underlined in the abstract.
Saiman L, Anstead M, Mayer-Hamblett N, Lands LC, Kloster M, Hocevar-Trnka J, Goss CH, Rose LM, Burns JL, Marshall BC, Ratjen F. Effect of azithromycin on pulmonary function in patients with cystic fibrosis uninfected with Pseudomonas aeruginosa: a randomized controlled trial. JAMA 2010; 303:1707-15. [PubMed]

Fig. 47 Lisa Saiman Find a Doctor
In children and adolescents with CF not chronically infected with P. aeruginosa, treatment with azithromycin for 24 weeks did not result in improved pulmonary function but there fewer respiratory exacerbations – in 21% of the azithromycin group and 39% of the control group. The author concluded that 24 weeks treatment with azithromycin in this group of children did not improve pulmonary function.
— This was a large multi centre trial and answered an important question as to the use of azithromycin in patients uninfected with P. aeruginosa. However, the significant reduction in exacerbations presumably may have a favourable long term effect on lung function as not all patients regain their previuos pulmonary status after an exacerbation.
Lisa Saiman (fig. 47) is Professor of Pediatrics, Columbia University Medical Center. She is an expert on infections and infectious diseases.
Strandvik B. Fatty acid metabolism in cystic fibrosis. [Review] Prostag Leukotr Ess 2010; 83:121-129. [PubMed]

Fig. 48 Birgitta Strandvik Reseachgate.net
The author notes that 20 years ago the gene responsible for cystic fibrosis transmembrane conductance regulator (CFTR), the protein defective in cystic fibrosis (CF), was identified but research of this monogenetic disease has not provided an explanation for the divergent symptoms, and a treatment breakthrough is still awaited
This review discusses different aspects of disturbances in lipid metabolism seen in CF. These include increased release of arachidonic acid (AA) from cell membrane phospholipids and a low status of linoleic and docosahexaenoic acids. Recent research has explored more complicated lipid associations. Disturbances in annexins and ceramides might act in concert to explain the impact on inflammation and AA release. The connections to CFTR and between the disturbances in essential fatty acid metabolism are reviewed. The metabolic interactions, some of which might be compensating, possibly explain the difficulties in understanding the fatty acid disturbances in relation to different symptoms and their relation to the defective CFTR.
Birgitta Strandvik (fig. 48) is one of Europe’s leading paediatricians involved in CF care and research. Birgitta has had a particular interest in fatty acid metabolism in CF for many years and this article by an expert in the subject, brings together some of the existing knowledge; also there does seem to be some interesting and possibly significant associations such as that with ceramides.
Sermet-Gaudelius I, Boeck KD, Casimir GJ, Vermeulen F, leal T, Mogegnet A, Roussel D, Fritch J, hanssens L, Hirawat S, Miller NL, Constantine S, Reha A, Ajayi T, Elfring GL, Miller LL. Ataluren (PTC124) induces cystic fibrosis transmembrane conductance regulator protein expression and activity in children with nonsense mutation cystic fibrosis. Am J Respir Crit Care 2010; 182:1262-1272.[PubMed]

Fig 49. Isabelle Sermet-Gaudelius
A study to evaluate ataluren activity, safety, and pharmacokinetics in children with nonsense mutation CF. Patients were assessed in two 28-day cycles, comprising 14 days on and 14 days off ataluren. Patients took ataluren three times per day (morning, midday, and evening) with randomization to the order of receiving a lower dose (4, 4, and 8 mg/kg) and a higher dose (10, 10, and 20 mg/kg) in the two cycles. The study enrolled 30 patients (16 male and 14 female, ages 6 through 18 yr) with a nonsense mutation in at least one allele of the CFTR gene, a classical CF phenotype, and abnormal baseline nasal epithelial chloride transport.Ataluren induced a nasal chloride transport response (at least a -5-mV improvement) or hyperpolarization (value more electrically negative than -5 mV) in 50% and 47% of patients, respectively, with more hyperpolarizations at the higher dose. Improvements were seen in seven of nine nonsense mutation genotypes represented. Ataluren significantly increased the proportion of nasal epithelial cells expressing apical full-length CFTR protein. Adverse events and laboratory abnormalities were infrequent and usually mild. Ataluren pharmacokinetics were similar to those in adults.
The authors concluded that in children with nonsense mutations CF, Ataluren can induce functional CFTR production and is well tolerated.
Dr Isabelle Sermet-Gaudelus (fig. 49) is a paediatrician at the Hopital Necker-Enfants Malades in Paris. She is actively involved in many areas of CF care and research including bone disease and neonatal screening.
Sermet-Gaudelus I, Mayell SJ, Southern KW. European Cystic Fibrosis Society (ECFS), Neonatal Screening Working Group. Guidelines on the early management of infants diagnosed with cystic fibrosis following newborn screening. J Cyst Fibros 2010; 9:323-329. [PubMed].
In response to current varied practice, the ECFS Neonatal Screening Working Group developed a consensus on the early management of these infants using the Delphi methodology. Following detailed literature review, statements were generated by a core group of experts and then assessed by a larger group using modified Delphi methodology. Forty-one statements were written by the core group. Eighty-six CF specialists contributed to the modified Delphi process. During three rounds, extra statements were added and consensus achieved on 44 (one statement did not achieve consensus). These statements will provide a framework for the management of screened infants in the first year of life. This process highlights the paucity of published and trialed evidence on which to base management of these infants.The authors suggest that to improve this situation, it is important that each infant with CF identified through NBS has opportunity to be included in a randomised controlled trial.
This is a useful practical guide to management of infants detected by neonatal screening. In view of the widely diverse approaches of some paediatricians regarding early treatment (or not!) the guidance was welcome and based on wide opinion of clinicians interested in the subject via the Delphi method.
— This a good method as both published evidence and clinical experience are combined with “common sense”. Paediatricians who have experience of neonatal screening are increasingly impressed by the need to start treatment at a very early stage as both infection and poor weight gain occur extremely early. In Leeds I recommended we start pancreatic enzymes and vitamins, regular flucloxacillin and physiotherapy at the time of diagnosis.
Simmonds NJ, Macneill SJ, Cullinan P, Hodson ME. Cystic fibrosis and survival to 40 years: a case-control study. Eur Respir J 2010; 36:1277-1283. [PubMed]

Fig 50. Margaret Hodson
A case-control study of adult CF patients from the Royal Brompton, London was used to compare long-term survivors (aged >= 40 yrs) with patients who died before reaching 30 yrs of age. Factors resulting in increased probabilities of survival included high body mass index, respiratory function tests on transfer from the paediatric clinics and the exclusive use of oral antibiotics. Factors resulting in decreased probabilities of survival were Pseudomonas aeruginosa acquisition or pneumothorax before transfer to the adult clinic and referral from a paediatric clinic in a deprived area. Long-term survival is associated with the clinical features present by the time of referral to an adult clinic.
This study, from the world’s largest adult CF clinic, confirms the expected factors which are associated with longer survival. They are predictable and include better nourishment and respiratory function tests without need for courses of intravenous antibiotics. The relationship to Pseudomonas was be expected and the influence of social deprivation so obvious for so long to clinicians dealing with patients is confirmed.
— So nothing new but nice to have the facts confirmed.These authors later showed that longer survival was not associated with increased residual CFTR function (Simmonds NJ et al. Eur Respir J 2011; 37:1076-1082). [PubMed]
Margaret Hodson (fig. 50) (1943 – 2023) is Professor of Respiratory Medicine, Senior Research Investigator at the National Heart and Lung Institute, Imperial College London with a research interest in the field of adult cystic fibrosis (CF). For many years Margaret has been a world leader in this area. She is honorary Consultant Physician and Director of Medical Education for the Royal Brompton Hospital.
Scotet V, Dugueperoux I, Audrezet MP, Audebert-Bellanger S, Muller M, Blayau M, Ferec C. Focus on cystic fibrosis and other disorders evidenced in fetuses with sonographic finding of echogenic bowel: 16-year report from Brittany, France. Am J Obstet Gynecol 2010; 203:592. e1-6.pubmed.ncbi.nlm.nih.gov/20932506/

Fig. 51 Virginie Scotet Le Telegramme
Based on the long experience of a region where CF is frequent (Brittany, France), the authors describe disorders diagnosed in fetal echogenic bowel fetuses and assess ultrasonography ability in detecting cystic fibrosis in utero. They reviewed the cases of fetal echogenic bowel diagnosed in pregnant women living in Brittany and referred for CFTR gene analysis over the 1992-2007 period (n = 289). A disorder was diagnosed in 32. 2% of the fetuses, cystic fibrosis being the most commonly identified (7. 6%). They also found digestive malformations (7. 0%), chromosomal abnormalities (3. 7%), and materno-fetal infections (3. 7%). Combining these data with their ongoing newborn screening program since 1989 showed that ultrasonography enabled diagnosis of 10. 7% of the cystic fibrosis cases.
This study highlights the importance of pregnancy ultrasound examinations and their efficiency in detecting cystic fibrosisThis paper reports valuable extensive experience from France indicating the clinical significance of the finding of an echogenic bowel at antenatal ultrasound
Virginie Scotet (Fig. 51) is at Inserm U613, Faculté de Médecine et des Sciences de Santé, Université Brest, Etablissement Français du Sang Bretagne, Brest, France.
Spadafora D, Hawkins EC, Murphy KE, Clark LA, Ballard ST. Naturally occurring mutations in the canine CFTR gene. Physiol Genom 2010; 42:480-485. [PubMed]
Naturally occurring cystic fibrosis (CF)-causing mutations in the CFTR gene have not been identified in any non-human animal species. Since domestic dogs are known to develop medical conditions associated with atypical CF in humans (e. g. , bronchiectasis and pancreatitis), the authors hypothesized that dogs with these disorders are likely have a higher expression rate of CFTR mutations than the at-large population.
Temporal temperature-gradient gel electrophoresis (TTGE) was used to screen canine CFTR in 400 animals: 203 dogs diagnosed with pancreatitis, 23 dogs diagnosed with bronchiectasis, and 174 dogs admitted to clinics for any illness (“at-large” dogs).
Twenty-eight dogs were identified with one of four CFTR missense mutations. P1281T and P1464H mutations occur in relatively unconserved residues. R1456W is analogous to the human R1453W mutation, which has approximately 20% of normal CFTR function and is associated with pancreatitis and panbronchiolitis. R812W disrupts a highly conserved protein kinase A recognition site within the regulatory domain.
The authors conclude that naturally occurring CFTR mutations are relatively common in domestic dogs and can be detected with TTGE. No substantive differences in mutation frequency were observed between the at-large, pancreatitis, and bronchiectasis dogs.This is of interest and CFTR problems in dogs is a new finding. Impressive to collect so many “patients”. with these various disorders!
Domenico Spadafora is in the Department of Physiology, College of Medicine, University of South Alabama, Mobile, Alabama 36688, USA.
Stoltz DA, Meyerholz DK, Pezzulo AA, Ramachandran S, Rogan MP, Davis GJ, Hanfland RA, Wohlford-Lenane C, Dohrn CL, Nelson GA 4th, Chang EH, Taft PJ, Ludwig PS, Estin M, Hornick EE, Launspach JL, Samuel M, Rokhlina T, Karp PH, Ostedgaard LS, Uc A, Starner TD, Horswill AR, Brogden KA, Prather RS, Richter SS, Shilyansky J, McCray PB Jr, Zabner J, Welsh MJ. Cystic fibrosis pigs develop lung disease and exhibit defective bacterial eradication at birth. Science Translational Medicine 2010; 2:29ra31. [PubMed]

Fig. 52 David Stoltz medicine.uiowa.edu
Within months of birth, CF pigs spontaneously developed hallmark features of CF lung disease, including airway inflammation, remodeling, mucus accumulation, and infection. Their lungs contained multiple bacterial species, suggesting that the lungs of CF pigs have a host defense defect against a wide spectrum of bacteria. In humans, the temporal and causal relations between inflammation and infection have remained uncertain. To investigate these processes, the authors studied newborn pigs. Their lungs showed no inflammation but were less often sterile than controls. Moreover, after introduction of bacteria into their lungs, pigs with CF failed to eradicate bacteria as effectively as wild-type pigs. These results suggest that impaired bacterial elimination is the pathogenic event that initiates a cascade of inflammation and pathology in CF lungs. The finding that pigs with CF have a host defense defect against bacteria within hours of birth provides an opportunity to further investigate CF pathogenesis and to test therapeutic and preventive strategies that could be deployed before secondary consequences develop.
A description of some of the features of the CF pig – a major advance in the study of CF already increasing understanding of human disease. Initial findings suggest that defective bacterial elimination precedes inflammation – although it does seem as if there are reasons for excessive inflammation when it does occur.
David A Stoltz (fig.52) is a pulmonologist in the Department of Internal Medicine, Roy J. and Lucille A. Carver College of Medicine, University of Iowa, Iowa City, IA 52242, USA.
Sanders DB, Bittner RC, Rosenfeld M, Hoffman LR, Redding GJ, Goss CH. Failure to recover to baseline pulmonary function after cystic fibrosis pulmonary exacerbation. Am J Respir Crit Care 2010; 182:627-632.[PubMed]

Fig. 53 Don B Sanders Indiana School of medicine
Previous studies have noted that some patients’ lung function (FEV1) does recover to pre-exacerbation levels with antibiotic treatment. This cohort study using the Cystic Fibrosis Foundation Patient Registry from 2003-2006 confirms this finding – that of 8,479 pulmonary exacerbations, 25% failed to recover to baseline FEV(1). The authors identified factors associated with the failure to recover to baseline, allowing clinicians to identify patients who may benefit from closer monitoring and more aggressive treatment.A number of recent studies confirm this finding which is not surprising as some additional permanent pulmonary damage is likely to be sustained with each exacerbation. The finding emphasized the need for optimal treatment of exacerbations and also the value of prevention or reducing the frequency of exacerbations particularly by the use of long term inhaled antibiotics, rhDNase and azithromycin all of which have been shown in trials to reduce the frequency of exacerbations.
Don B Sanders (Fig. 53) is at the Department of Pediatrics, American Family Children’s Hospital, 600 Highland Avenue, Madison, WI 53792-9988, USA.
Sun X, Sui H, Fisher JT, Yan Z, Liu X, Cho HJ, Joo NS, Zhang Y, Zhou W, Yi Y, Kinyon JM, Lei-Butters DC, Griffin MA, Naumann P, Luo M, Ascher J, Wang K, Frana T, Wine JJ, Meyerholz DK, Engelhardt JF. Disease phenotype of a ferret CFTR-knockout model of cystic fibrosis. J Clin Invest 2010; 120:3149-60. [PubMed]

Fig. 54 Xingshen Sun medicine.uiowa.edu
Here, the authors report the phenotype of a CFTR-knockout ferret model of CF. Neonatal CFTR-knockout ferrets demonstrated many of the characteristics of human CF disease, including defective airway chloride transport and submucosal gland fluid secretion; variably penetrant meconium ileus (MI); pancreatic, liver, and vas deferens disease; and a predisposition to lung infection in the early postnatal period. Severe malabsorption by the gastrointestinal (GI) tract was the primary cause of death in CFTR-knockout kits that escaped MI. Elevated liver function tests in CFTR-knockout kits were corrected by oral administration of ursodeoxycholic acid, and the addition of an oral proton-pump inhibitor improved weight gain and survival. To overcome the limitations imposed by the severe intestinal phenotype, the authors cloned 4 gut-corrected transgenic CFTR-knockout kits that expressed ferret CFTR specifically in the intestine. One clone passed feces normally and demonstrated no detectable ferret CFTR expression in the lung or liver. The authors suggest the animals described in this study are likely to be useful tools for dissecting CF disease pathogenesis and developing treatments.
Some details of the recently available CF ferret. The ability to clone gut-corrected transgenic CFTR-knockout kits that expressed the species appropriate CFTR in the intestine was very interesting.
Professor Xingshen Sun (fig. 54) is in the Department of Anatomy and Cell Biology, Carver College of Medicine, University of Iowa, Iowa City, Iowa 52242, USA.
Tramper-Stranders GA, Wolfs TF, van Haren Noman S, van Aalderen WM, Nagelkerke AF, Nuijsink M, Kimpen JL, van der Ent CK. Controlled trial of cycled antibiotic prophylaxis to prevent initial Pseudomonas aeruginosa infection in children with cystic fibrosis. Thorax 2010; 65:915-920. [PubMed]

Fig. 55 Gerdien Tramper-Stranders ResearchGate
This 3-year triple-blind randomised controlled trial included 65 children with CF without P. aeruginosa infection. Intervention existed of 3-monthly 3-week treatments with oral ciprofloxacin and inhaled colistin or both placebo controls. There was no difference in acquisition of P. aeruginosa infection between the control and treatment groups (annual incidence 14% vs 11%; HR 0. 738, 95% CI 0. 299 to 1. 822). Anti-Pseudomonas antibodies emerged earlier in the control group, but this difference had disappeared after 3 years. Chronic infection was observed in 19% of controls and 12% of treated patients. Decline in pulmonary function and other clinical outcomes did not differ between the two groups. The authors concluded that this regimen of three-monthly cycled anti-P. aeruginosa prophylaxis does not reduce the risk of initial and chronic infection in P. aeruginosa-negative children with CF of all ages.
– One would not expect that 3 weeks treatment every 3 months would be effective prophylaxis against new P. aeruginosa infection as antibiotic cover would be present only 25% of the time. However, previous work from Austria with continuous inhaled gentamicin did show a significant reduction in the incidence of new P. aeruginosa isolations (Heinzl B et al. Pediatr Pulmonol 2002; 33:32-37).[PubMed]However, there was concern over the possibility of renal damage as judged by raised urinary NAG levels in the treated children and the gentamicin treatment was discontinued in some (Ring E et al. Arch Dis Child 1998; 78:540-543). [PubMed] Also 80mg bd of tobramycin was adequate to prevent Pseudomonas infection in another study (Wiesemann HG et al. Pediatr Pulmonol 1998; 25:88-92). [PubMed]
Gerdien A Tramper-Stranders (fig.55) is in the Department of Paediatric Respiratory Medicine, Cystic Fibrosis Center, WilhelminaChildren’s Hospital, University Medical Center Utrecht, The Netherlands.
Tolland JP, Boyle J, Hall V, McKenna KE, Elborn JS. Aquagenic wrinkling of the palms in an adult cystic fibrosis population. Dermatology 2010; 221:326-330. [PubMed]

Fig. 56 Julia Tolland Hillsborough Private Clinic
A study to determine the incidence and characteristics of aquagenic wrinkling of the palms (AWP) in the adult CF population in Northern Ireland. 105 patients were asked whether they noticed excess wrinkling of the hands when exposed to water. If they answered ‘yes’, further questions were asked regarding clinical characteristics. The atopic status, CF genotype and drug history were recorded for each patient. Formal testing of 7 patients was carried out. 43 of 105 (41%) described AWP; 20 were male and 23 were female. There was no association with genotype, atopy or concomitant drug intake. The authors suggest that condition is under-reported in cystic fibrosis.
– The first descriptions of finger wrinkling caused great excitement as there was a suggestion the sign may be related to the basic defect which was quite unknown at the time (Elliott RB, 1974 [PubMed]; Norman AP et al, 1974). [PubMed] Johns M K (J Med Biol Illus 1975; 25:205-210).[PubMed] suggested the wrinkling was due to the excessive salt concentration which increased the water binding capacity of keratin. Later it was suggested as a test of autonomic function (Bull C, Henry JA BMJ 1977; 551-2).[PubMed]

Fig. 57 Jeanette Firth. Cystic Fibrosis Medicine
In the Leeds CF unit Jeanette Firth (fig.57), the CF centre clinic nurse, performed the test under controlledconditions on many children with CF who were attending the unit for Comprehensive Assessments of their CF and confirmed the phenomenon, but disappointingly we found it quite unrelated to the sweat electrolyte levels or any other of the numerous clinical or laboratory features of the patient’s condition (unpublished data). Subsequently, there was considerable discussion as to autonomic abnormalities in CF of which skin wrinkling is a feature (see Davies et al, 1980).
van der Doef HP, Kook FT, Seek FJ, Wontedness JW, Ferruling SP, Houwen RH. Constipation in pediatric cystic fibrosis patients: an underestimated medical condition. J Cyst Fibros 2010; 9:59-63. [PubMed]

Fig. 58 Hubert van der Doef LinkedIn
he aims of this study were to determine prevalence, risk factors and treatment of constipation in patients with cystic fibrosis, as well as the diagnostic value of abdominal radiography. A cohort of 214 pediatric CF patients was investigated. Furthermore, 106 abdominal radiographs of CF patients with or without constipation were independently assessed by three observers on two separate occasions using the Barr and Leech scores. The prevalence of constipation was 47%. Low total fat absorption and meconium ileus were independent risk factors for constipation in CF, while fiber and fluid intake were not associated. In CF patients the inter and intra observer variabilities of the Barr and Leech scores were poor to moderate.The authors concluded constipation is a significant medical issue in CF and was associated with low total fat absorption and a history of meconium ileus. Finally, abdominal radiography seems of little value in the regular follow-up of CF patients.
Hubert P van der Doer (fig.58) at this time was a resident at the Wilhelmina Children’s Hospital, University Medical Center Utrecht, Lundlaan 6, 3584 EA, Utrecht, The Netherlands.
– This reviewer would maintain that abdominal radiography is of value in the follow up of those CF patients who are complaining of abdominal symptoms – particularly abdominal pain which may affect over 20% of patients in some CF clinics. By definition, constipation implies the infrequent passage of hard stools and this is not synonymous with colonic overloading which is common in people with CF. In my experience much of the pain experienced by people with CF is related to colonic overloading but the patient may not complain of “constipation” or any disturbance of bowel habit (Littlewood et al, Pediatr Pulmonol 2006; 41:34-49). [PubMed] The European Society for Paediatric Gastroenterology, Hepatology, and Nutrition CF Working Group definitions of DIOS and constipation in CF are specific and make a clear distinction between these 2 entities. The incidence of DIOS in the present study was considerably higher than reported previously.
Varelogianni G, Oolitic I, Roomans GM, Johannesson M. The effect of N-acetylcysteine on chloride efflux from airway epithelial cells. Cell Biology International 2010; 34:245-252.[PubMed]

Fig. 59 Georgia Varelogianni Facebook
NAC (N-acetylcysteine) is a well known mucolytic and antioxidant drug, and an indirect precursor of glutathione. Since GSNO (S-nitrosoglutathione) previously has been shown to be able to promote Cl- efflux from CF airway epithelial cells, it was investigated whether NAC also could stimulate Cl- efflux from CF and non-CF epithelial cells and through which mechanisms. CFBE (CF bronchial epithelial cells) and normal bronchial epithelial cells (16HBE) were treated with 1 mM, 5 mM, 10 mM or 15 mM NAC for 4 h at 37 degrees C. The effect of NAC on Cl- transport was measured by Cl- efflux measurements and by X-ray microanalysis. Cl- efflux from CFBE cells was stimulated by NAC in a dose-dependent manner, with 10 mM NAC causing a significant increase in Cl- efflux with nearly 80% in CFBE cells.The intracellular Cl- concentration in CFBE cells was significantly decreased up to 60% after 4 h treatment with 10 mM NAC. Moreover immunocytochemistry and Western blot experiments revealed expression of CFTR channel on CFBE cells after treatment with 10 mM NAC. The stimulation of Cl- efflux by NAC in CF airway epithelial cells may improve hydration of the mucus and thereby be beneficial for CF patients.
– Another paper on NAC which although used as a mucolytic in Europe since the first reports (1962 Webb WR. Clinical evaluation of a new mucolytic agent acetyl-cysteine. J Thorac Cardiovasc Surg 1962; 44:330-343. [PubMed] ) has not found favour in the UK nor has performed well in CF in recent trials.The more recent relationship as a precursor to glutathione adds further interest to the NAC story. Apparently N-acetylcysteine and other sulphydryl compounds act by depolymerising mucus in vitro by breaking disulphide bonds of the glycoproteins thereby lowering the viscosity (Sheffner AL. Ann N Y Acad Sci 1963; 106:298-310).
Dr Georgia Varelogianni (fig. 59) is in the Department of Medical Cell Biology, Uppsala University, Box 571, SE-75123 Uppsala, Sweden.
Vincenzi F, Bizzarri B, Ghiselli A, de’ Angelis N, Fornaroli F, de’ Angelis GL. Cystic fibrosis and Crohn’s disease: successful treatment and long term remission with infliximab. World J Gastroenterol 2010; 16:1924-7. [PubMed]

Fig. 60 Francesca Vincenzi LinkedIn
he association of cystic fibrosis and Crohn’s disease (CD) is well known, but to date, there are very few reports in the literature of patients suffering from mucoviscidosis who have required treatment with infliximab. The authors report the case of a 23-year-old patient suffering from cystic fibrosis and severe CD treated successfully with infliximab without any infective complications or worsening of the pulmonary disease and with a long term (2 years) complete remission.
Infliximab is a monoclonal antibody against tumour necrosis factor alpha used to treat autoimmune disease.
Dr Francesca Vincenzi (fig. 60) is at the Gastroenterology and Endoscopy Unit, University of Parma, via Gramsci 14, 43100 Parma, Italy.
Webb AK, Dudley-Southern R, Jones AM. Development of a modern adult cystic fibrosis centre in Manchester. J R Soc Med 2010; 103 Suppl 1:S15-19. [PubMed]

Fig 61. Kevin Webb

Fig 62. Andy Jones

Fig 63. Rowland Bright-Jones

Fig 64 Rachel Rowe

Fig 65 Amanda Bennan

Fig 66. Mary Dodd CBE
An interesting account of the development of the Manchester Adult CF Centre in the North of England from its beginning in 1982 to care for the 30 or so adults still attending paediatric clinics in the city at that time to the present large purpose built centre opened in September 2009.The stormy early course is described by Professor Kevin Webb (fig.61) who, with Mary Dodd CBE (fig.66) the physiotherapist, has been responsible for driving the development forward and building up an internationally recognised Adult CF Service at the UHSM Manchester Adult Cystic Fibrosis Centre. In recent years the consultant team has been joined by Dr Andy Jones (fig. 62) and Dr Rowland Bright-Thomas (fig.63) and Amanda Brennan (fig.65). Dr Rachel E Rowe (fig. 64), an endocrinologist, has provided expertise on the management of CF related diabetes for over 12 years both in Manchester and for the CF Trust guidelines.
Weiss B, Bujanover Y, Yahav Y, Vilozni D, Fireman E, Efrati O. Probiotic supplementation affects pulmonary exacerbations in patients with cystic fibrosis: a pilot study. Pediatr Pulmonol 2010; 45:536-540. [PubMe]

Fig. 65 Batya Weiss Shebaonline.org
Probiotics reduce intestinal inflammation, and Lactobacillus GG (LGG) reduces pulmonary exacerbation rate cystic fibrosis (CF) patients. the authors intended to determine the effect of a mixed probiotic preparation on pulmonary exacerbations and inflammatory characteristics of the sputum in CF patients. A prospective pilot study of 10 CF patients with mild-moderate lung disease and Pseudomonas aeruginosa colonization, were treated with probiotics for 6 months. Pulmonary function tests (PFT’s), sputum cultures with semi-quantitative bacterial analysis, and sputum neutrophil count and interleukin-8 (IL-8) levels were compared to pre-treatment and post-treatment values. The rate of pulmonary exacerbations was compared to 2 years prior to the study. The exacerbation rate was significantly reduced in comparison to the previous 2 years and to 6 months post-treatment (P = 0. 002). PFT’s have not changed at the end of treatment and during 6 months post-treatment. No change in sputum bacteria, neutrophil count, and IL-8 levels was observed.
The authors concluded that probiotics reduce pulmonary exacerbations rate in patients with CF and may have a preventive potential for pulmonary deterioration in CF patients. Although this study involved few patients and there were historical controls, there is increasing evidence that probiotics may have a favourable effect in people with CF and also other conditions such as rosacea.
Dr Batya Weiss (fig. 65) is Director of the Division of Pediatric Gastroenterology and Nutrition, Safra Children’s Hospital, Tel-Hashomer, Israel.
Werlin SL, Benuri-Silbiger I, Kerem E, Adler SN, Goldin E, Zimmerman J, Malka N, Cohen L, Armoni S, Yatzkan-Israelit Y, Bergwerk A, Aviram M, Bentur L, Mussaffi H, Bjarnasson I. Wilschanski M. Evidence of intestinal inflammation in patients with cystic fibrosis. J Pediatr Gastroenterol Nutr 2010; 51:304-308. [PubMed]

Fig. 66 Steven L Werlin
findatopdoc.com
Treatment with pancreatic enzymes fails to completely correct malabsorption and gastrointestinal symptoms in patients with cystic fibrosis (CF). The aim of the present study was to examine the small intestine of patients with CF without overt evidence of gastrointestinal disease using capsule endoscopy (CE).
Patients with CF received the agile patency capsule and, depending on the result of that procedure, then underwent standard CE using the PillCam SB capsule (Given Imaging, Yokneam, Israel). A stool specimen was taken on the same day as the CE for determination of the calprotectin level. Forty-two patients with CF ages 10 to 36 years were included; 29 had pancreatic insufficiency. One patient failed to excrete the patency capsule after 36 hours and was withdrawn from the study. Pulmonary function was mild to moderate with FEV1 68. 5% +/- 16% predicted.
Review of the CE videos showed that most of the patients had varying degrees of diffuse areas of inflammatory findings in the small bowel including oedema, erythema, mucosal breaks, and frank ulcerations. There were no adverse events. Fecal calprotectin levels were markedly high in patients with pancreatic insufficiency, 258 microg/g (normal <50).
The authors conclude that small bowel mucosal pathology may be detected using capsule endoscopy in most of the patients with CF. The high fecal calprotectin levels found are suggestive of mucosal inflammation, which may correlate with the capsule endoscopy findings. Additional study is required to examine the possible relation of these mucosal lesions, which may be part of a newly identified enteropathy associated with CF, with persistent intestinal malabsorption in many of these patients.
– This is an impressive study with some striking pictures of the inflamed small intestinal mucosa in the full paper. Evidence of inflammation had been reported previously but these findings are the first visual support for the lesions which would seem to be one factor in failing to achieve normal intestinal absorption in some people with CF despite the use of pancreatic enzymes.
Dr Steven L Werlin (fig. 66) is at Department of Pediatrics, Medical College of Wisconsin, Milwaukee, WI, USA.
Wine JJ. The development of lung disease in cystic fibrosis pigs. Science Translational Medicine 2010; 2:29ps20. [PubMed]

Fig. 67 Jeffrey Wine profiles.stanford.edu
The leading cause of death in cystic fibrosis (CF) patients is lung disease; yet despite enormous research efforts, its pathogenesis is not well understood. Because CF mice do not develop human-like airway disease, CF pigs were produced on the premise that they would offer insights into the pathogenesis of CF lung disease. Unfortunately CF pigs develop severe intestinal blockage and often die shortly after birth.Now, a team of scientists report results from five CF pigs that lived for 2 to 6 months; during this time, they developed some of the key features of human CF lung disease and revealed that infection precedes inflammation.The discussion as to whether infection precedes inflammation or whether the inflammation is the first abnormality has been a source of discussion for many years. It seems that infection precedes inflammation as suggested here but that when inflammation occurs it may be excessive and prolonged.
Jeffrey J Wine (fig. 67) is a scientist at Cystic Fibrosis Research Laboratory, Stanford University, Stanford, CA 94305-2130, USA.

Fig. 68 Munir Zaman
Zaman MM, Martin CR, Andersson C, Bhutta AQ, Cluette-Brown JE, Laposata M, Freedman SD. Linoleic acid supplementation results in increased arachidonic acid and eicosanoid production in CF airway cells and in cftr-/- transgenic mice. Am J Physiol – Lung C 2010; 299:L599-606. [PubMed]
Cystic fibrosis (CF) patients display a fatty acid imbalance characterized by low linoleic acid levels and variable changes in arachidonic acid. This led to the recommendation that CF patients consume a high-fat diet containing >6% linoleic acid. The authors hypothesized that increased conversion of linoleic acid to arachidonic acid in CF leads to increased levels of arachidonate-derived pro inflammatory metabolites and that this process is exacerbated by increasing linoleic acid levels in the diet.To test this hypothesis, they determined the effect of linoleic acid supplementation on downstream pro inflammatory biomarkers in two CF models: 1) in vitro cell culture model using 16HBE14o(-) sense [wild-type (WT)] and antisense (CF) human airway epithelial cells; and 2) in an in vivo model using cftr(-/-) transgenic mice.
Mice supplemented with 100 mg of linoleic acid had increased arachidonic acid levels in lung tissue associated with increased neutrophil infiltration into the airway compared with control mice.
These findings support the hypothesis that increasing linoleic acid levels in the setting of loss of cystic fibrosis transmembrane conductance regulator (CFTR) function leads to increased arachidonic acid levels and pro inflammatory mediators. The findings are important as there was considerable interest in linoleic acid supplementation in people with CF – even a trial of intravenous linoleic acid in the Seventies (see “TOPICS” section – gastroenterology – fatty acids where some of the previous work on fatty acids is reviewed). The situation regarding essential fatty acids remains unclear to this reviewer!
Dr Munir M Zaman (fig. 68) is at the Beth Isreal Deaconess Medical Center, Boston.


