The Fifties
Fifties
The abnormal sweat electrolytes are described – the first major step towards understanding the basic defect and a major aid in diagnosis
Fig. 1 Paul di Sant’Agnese
Undoubtedly the major advance during the Fifties was the recognition of the increased salt content of the sweat in people with CF by Paul di Sant’Agnese in 1953 (below). This followed the report of Kessler and Andersen in 1951 (below) of heat prostration in children with CF that occurred during a New York heat wave in August 1948. Subsequently the availability of the sweat test permitted an accurate diagnosis when CF was suspected and gradually replaced the more invasive duodenal intubation to obtain duodenal juice for tryptic activity. Towards the end of the decade diagnosis by sweat analysis became more practicable, accurate, safe and more generally available when localised sweating was stimulated by the pilocarpine iontophoresis, as described by Gibson & Cooke, in 1959, (below) rather than by the various potentially dangerous methods of heating the whole child to stimulate sweating. The availability of the sweat test permitted the recognition of people with CF who had sufficient remaining pancreatic function to achieve normal fat absorption – so-called “pancreatic sufficient” individuals. Finally, it became apparent that if the test was carried out by inexperienced laboratory or medical staff erroneous results were not infrequent; eventually much attention was paid to ensuring that adequate standards of sweat testing were in place.
Fig. 3 Lucas Kulczycki
Fig. 2 Harry Shwachman
In 1958 Shwachman and Kulczycki published their classic review of experience with 105 patients in which they described an improving outlook for children with CF and noted that, in their Boston clinic, survival into adult life was occurring with increasing frequency (Shwachman & Kulczycki, 1958 below). Courses of antibiotics such as chlortetracycline (Aureomycin) or oxytetracycline (Terramycin) were recommended for infections but used continuously only for those who were chronically infected; large doses combined with chloramphenicol or erythromycin were recommended for those with more severe infections but, in contrast to present day practice, antibiotics were seldom given intravenously or even intramuscularly. Intravenous access for prolonged periods, as needed for a two week course of intravenous antibiotics, was a major problem at that time. Antibiotic resistant Staphylococcus aureus and the appearance of Pseudomonas aeruginosa were, even then, emerging problems. Aerosol antibiotics, penicillin and streptomycin or neomycin and polymyxin (both of which were later recognised as toxic), were added for more severe infections (Shwachman, 1960 below).

Fig. 4 Archie Norman
Objective evidence of the beneficial effect of pancreatic enzyme therapy in children with CF was reported from Dr Archie Norman’s unit at Great Ormond Street in London (Harris et al 1955 below). However, not all paediatricians were impressed with the effect of enzymes, maintaining that their unpleasant taste adversely affected the childrens’ appetites. However, many patients were unable to tolerate a normal fat intake even when taking the available enzyme supplements and this compromised their energy intake, contributing to the almost inevitable progressive malnutrition which eventually affected virtually all children who survived beyond early childhood.
Fig 5 Winifred Young
RCP Museum
Physiotherapy, in the form of postural drainage and percussion, had been introduced into the treatment of children with CF from the time of diagnosis in Dr Winifred Young’s clinic at the Queen Elizabeth Hospital, London in 1950 – this was one of the few specialist paediatric CF clinics in the UK at that time (Mearns, 1993 below) – there was no call for adult CF clinics for, as yet, there were so few adults. The so-called “English” methods of physiotherapy (Doyle, 1959 below) were used and commended by Shwachman on a number of occasions (Shwachman, 1960 below). However, not even all experienced paediatricians were convinced of the value of physiotherapy – “The ritual of carefully positioning the patient to drain every segment separately is usually an exercise in futility” (Jack Docter of Seattle. In 1000 years of Cystic Fibrosis. Warren Warwick (ed). Minnesota. 1981).
Towards the end of the decade the introduction of LeRoy Matthews’s “comprehensive and prophylactic (preventive) treatment programme” was undoubtedly a major milestone in CF care. Dr William Wallace, Chairman of Pediatrics at the Babies and Children’s Hospital, Cleveland had been approached in 1957 by a CF parents’ organisation – the “Cousins Club” – one of whom had already lost a child and had another deteriorating from cystic fibrosis. The parents asked Dr Wallace to start a “research orientated treatment programme for CF” for which they would provide funding. To develop the programme Dr Wallace appointed a young pediatrician, Dr LeRoy Matthews, to plan and initiate the “comprehensive and prophylactic (preventive) treatment programme” for cystic fibrosis (Carl Doershuk, 2001 below).
Fig. 7 Carl Doershuk
Fig. 6 Leroy Matthews
The comprehensive and prophylactic treatment programme subsequently developed by Leroy Matthews incorporated many of the components now regarded as essential for modern CF centre care e.g. early correct diagnosis, a comprehensive programme to deal with all the aspects of the disease and data collection to validate the impact of the treatment on morbidity and survival (Matthews et al, 1964; Doershuk et al, 1964; Doershuk et al, 1965 – all below). Other important components of the treatment programme included regular physiotherapy, regular monthly respiratory cultures to guide antibiotic therapy, special microbiology techniques for CF sputum, regular nebulised treatment using phenylephrine as decongestant and propylene glycol as a mucolytic. The use of mist tents was the only major component which is not used today.
Nocturnal mist tent therapy was a popular form of treatment in the USA during the Sixties but was never popular in the UK. Although objective evidence of the positive value of mist tent therapy was published in 1967 by respected paediatricians in the USA (Matthews et al, 1967 below), subsequent studies failed to confirm significant fluid deposition below the larynx or beneficial clinical effect and the treatment was finally discontinued after further, albeit rather limited, studies showed little or no lung deposition of fluid (Chang et al, 1973 below). Interestingly, this was not the view pediatricians such as di Sant’Agnese and Shwachman with vast personal experience of CF and the use of mist tents; they seemed to favour this form of treatment at the time even though it is true their enthusiasm diminished over the years.
More specialist CF centres developed during the Fifties; in Canada by Dr Alan Ross (figure 1) at Montreal Children’s Hospital by Dr Alan Ross by Dr Douglas Crozier at the Hospital for Sick Children, Toronto in 1958 and by Dr William Cochrane (fig.3) at the Halifax Children’s Hospital, Nova Scotia – later succeeded by Dr Terence Gillespie in 1966.
Fig. 8 Terence Gillespie
Dr Gillespie (fig.8) remained as the CF Centre Director in until 1992; he was awarded the Order of Canada in 2008 for his work there. He describes, in a fascinating account, the detailed development of CF services in Nova Scotia for which first Dr Cochrane and then he was responsible in a chapter in Dr Doershuk’s book “Cystic Fibrosis in the 20th Century” (see Future section for more detail). With Dr Cochrane’s firm encouragement Dr Gillespie took up a fellowship in Cleveland with Dr Leroy Matthews. Dr Cochrane had remarked that ” We’re doing everything he’s doing but we’re not getting those results. I want you to find out why’. The reason was soon clear to the young Dr Gillespie who noted “the fundamental difference was a matter of degree rather than kind”. Full treatment from the day of diagnosis for every patient was the rule rather than waiting until the respiratory disease was quite evident.
I was fortunate to meet Dr Gillespie on a number of occaisions at CF meetings. He was a great enthusiast and rightly proud of his achievedments in developing the CF servicies in Nova Scotia

Fig.9 William Cochrane.
Fig.10 Alan Ross
Dr Alan Ross (fig. 10) was a distinguished and recognized leader in Montreal paediatrics for over 40 years. As Physician-in-Chief for 15 years at the Montreal Children’s Hospital and Chair of the Department of Paediatrics at McGill University, Dr. Ross earned an international reputation for his work in child health.
Dr William Cochrane (fig.9) was a quite remarkable man whose career spanned the fields of medicine, biomedical research, education and business. His considerable facility in, and dedication to, each of these fields produced lasting contributions to the health and well being of people across Canada.
In the UK there were few paediatric CF Centres until the Eighties and only one large adult CF centre at the Royal Brompton in London which started in the mid-Sixties by Sir John Batten. The National Health Service in the UK had started in 1948. General consultant paediatricians, working at District General Hospitals, cared for most children with CF but very few of their patients survived childhood. Even in teaching centres most consultant paediatricians each looked after a few children with CF until they died – as most did.

Fig. 11 Margaret Mearns
Fig. 10 Winifred Young
However, in London, Winifred Young (Fig. 10), later joined by Margaret Mearns (Fig.11), established a CF clinic at the Queen Elizabeth Hospital, Hackney. Also Archie Norman’s clinic at Great Ormond Street in London and Dr David Lawson, at Carshalton Hospital in Surrey UK, were also treating increasing numbers of children with CF and making a major contribution to clinical care, research and to the development of the UK CF Research Trust from 1964.
In 1953, in Australia, Dr Howard Williams, the distinguished Director of Clinical Research at the Royal Children’s Hospital, Melbourne had appointed Dr Charlotte Anderson to start a CF clinic ; in 1968 she moved to Birmingham in the UK as Professor of Paediatrics. Although Sir John Batten’s adult CF clinic started in the mid-Sixties at the Royal Brompton Hospital in London, in most parts of the UK there was no demand for adult CF care as there were virtually no children who survived to adulthood.
Fig. 12 Erhard Flensborg
In Denmark, most patients were treated at the main Danish CF Centre in Copenhagen from 1968 where it was shown subsequently that the outlook could be improved in chronically infected patients by more aggressive treatment with regular courses of intravenous antibiotics (Schiotz et al, 1981 below; Jensen et al, 1989 below). The Danish CF centre in Copenhagen was started by F W Flensborg (Fig. 12) and provides one of the most advanced CF services in the world.
I was privileged to be involved in making a video at the Copenhagen CF centre in 1997 to record the details of their clinic routines which confirmed my admiration for the work of the late Christian Koch, Niels Hoiby and their colleagues and predecessors
(Littlewood JM. A Visit to the Copenhagen CF Centre. A video sponsored by Forest Laboratories UK. 1997 – previously Pharmax).

Fig. 13 Minimeter peak flow meter.

Fig. 14 Early Vitalograph from 1966

Fig. 16 Wright’s Peak Flow Meter – first model introduced in 1959.
There were early reports of the use of pulmonary function testing (West et al, 1954 below; Mearns, 1968 below), which allowed more accurate documentation of the patients’ declining lung function.
The Wright’s Peak Flow Meter (Wright & McKerrow, 1959 below) in the late Fifties and later the Minimeter, which was used by patients at home, made a major contribution to routine patient care.
Fig. 17 Martin Wright
The first simple bellows Vitalograph, available from the mid-Sixties, was eventually replaced by portable electronic spirometers in the Eighties. However, more complex respiratory function studies, although of major interest to academic paediatric respirologists, have made only a modest contribution to the practical management of children with CF; such complex respiratory function tests were rarely used, or indeed required, for routine management. In recent years more sophisticated tests such as lung clearance index are increasingly used and provide a non-invasive, accurate method of measuring and following respiratory function in patients of all ages – particularly in young children
Basil Martin Wright (1912 – 2001) Fig. 17 was a British bioengineer who invented several notable medical instruments, including the peak flow meter and syringe driver. The “alcolmeter” he developed won a Queen’s Award for Industry and is the breathalyser most often used at the road-side in the United Kingdom. (more details at the end of the Fifties section)
Papers published in the Fifties
1950 Gibbs GE, Bostick WL, Smith PM. Incomplete pancreatic deficiency in cystic fibrosis of the pancreas. J Pediatr 1950; 37:320-325. [PubMed]
A series of 38 patients with CF included two, proved at autopsy to have CF by having typical pancreatic histological changes, who had sufficient residual pancreatic exocrine function to achieve normal fat absorption in life. Investigation showed the reduction in pancreatic enzymes was not complete. Possibly another four patients were in this category (13% of the series).
Subsequently it was shown that pancreatic enzyme output could fall to only about 10% of normal before intestinal malabsorption occurred (DiMagno et al. 1973 below). The present authors mention the previous case report of incomplete pancreatic involvement by Sinclair W Jr, 1948 (above). Also there were soon reports of similar patients who were described as “pancreatic sufficient” i.e. they had sufficient residual pancreatic function to achieve normal fat absorption (Shwachman et al 1952 & 1956 below; di Sant’Agnese al, 1956 below).
1950 Glanzmann E, Berger H. Meconium ileus; clinical and anatomopathologic observations, and chemical analysis of the intestinal content in a case of fatal meconium ileus in a six-day old child. Ann Paediatr – Internat Rev Pediatr 1950; 175:33-48. [PubMed]
An early report describing abnormal composition of meconium in CF infant that is “so altered physically and chemically that ileus inevitably occurs”. The meconium contained a protein which in contact with fatty material forms a gelatinous substance. The protein is present in only small amounts or absent in normal meconium.
The increased meconium protein subsequently provided the basis for a neonatal CF screening test.
1950 Rapoport S, Buchanan DJ. Composition of meconium: Isolation of blood group specific polysaccharides. Abnormal composition of meconium. I. Meconium ileus. Science 1950; 112:150.[PubMed]
Meconium was shown to consist largely of a mucopolysaccharide which demonstrated a very high amount of blood-group-specific activity (also Buchanan & Rapoport, 1952 below).
1950 Koyama Y, Kurosawa A, Tsuchiya A, Takakuta K. A new antibiotic, colistin, produced by spore-forming soil bacteria. J Antibiot Tokyo. 1950; 3:457.
The antibiotic colistin was discovered by Koyama et al in 1949, as a fermentation product of the bacteria Bacillus colistinus and the discovery had a direct bearing on the treatment of CF. At first the drug was given intramuscularly (and apparently it was very painful) and in 1959 an intravenous formulation (colistimethate sodium) was released commercially; but this was temporarily abandoned in the Seventies due to reports of a high incidence of nephrotoxicity (Price et al, 1970; Koch-Weser et al, 1970) and also there was increasing use of intravenous gentamicin from 1968. Later, the early clinical reports of toxicity with colistin were considered as likely to have occurred as a result of inappropriate patient selection and higher dosing than was recommended and inappropriate monitoring (Li et al, 2005).
– However, interest in colistin was rekindled following a rise in the prevalence of multiresistant Gram-negative strains most of which were sensitive to colomycin and particularly following the report of its use in the successful early eradication of P. aeruginosa in children with cystic fibrosis (Littlewood et al, 1985 below). Nebulised colistin is now widely used for the treatment of both chronic infections and the early eradication of P. aeruginosa in people with cystic fibrosis (Littlewood et al, A ten year review of colomycin. Resp Med 2000; 94:632-640.2000 below).
1950 Meeting of the Royal Society of Medicine, Section of Paediatrics at the Queen Elizabeth Hospital for Children, Banstead, Surrey. Proceedings of the Royal Society of Medicine. May 12th 1950.
One of the early reports from the UK of the case histories of five children with CF presented by junior doctors “on behalf of” consultants – one of the juniors presenting was Winifred Young who in this year started the CF clinic at the Queen Elizabeth Hospital for Children in Hackney, London.
The four infants described were aged less than a year and the rather unlikely statement made that “none of these children has chronic pulmonary disease”, although two had repeated attacks of respiratory infection and one had had meconium ileus. All infants had an absence of tryptic activity in the duodenal fluid or in the stools. Treatment consisted of “a diet (high calorie, high protein, and low fat), vitamin supplements in large doses, and pancreatin 0.5-1.0 gramme with feeds”. Antibiotics were mentioned in two infants – oral penicillin in one and penicillin, sulphonamides, streptomycin and chloromycetin in another.
1951 Johnstone DE, Neter E. Studies on laboratory diagnosis of cystic fibrosis of the pancreas: Positive gelatine film tests due to gelatine-liquefying bacteria in feces and duodenal juice. Pediatrics 1951; 7:483-490. [PubMed]
A report suggesting that gelatine-liquefying bacteria would interfere with the reliability of the gelatine film test for faecal trypsin which had been described recently by Shwachman (Shwachman et al, 1949 above) and had seemed such a welcome alternative to duodenal aspiration. The authors suggested this complication was related to the increasing frequency of organisms, particularly Pseudomonas aeruginosa, in the stools which they suggested was related to the more prolonged use of antibiotics.
Fortunately Johnstone later showed that if a dilution of faeces of 1 in 120 was used the results were reliable (Johnstone, 1952 below).
Although no longer used, this test was very important at the time as the sweat abnormality was not described until 1953 and sweat tests were not widely available until the Sixties. So at this time the diagnosis of CF relied heavily on the clinical picture and the absence of tryptic activity either ideally in the duodenal aspirate or in the stools to identify the pancreatic abnormality.
1951 Poncher HG. Year Book of Pediatrics. Chicago: Year Book Publishers, 1951: 128-129.
An interesting comment from Dr Henry Poncher, the Editor of the 1951 Year Book of Pediatrics, on the increasing survival of people with CF and the more frequent isolation of Pseudomonas aeruginosa, possibly as a result of prolonged antibiotic therapy. He makes prophetic comments on the likely causes – “For future progress, control of Pseudomonas infections is necessary” – an astute and relevant observation as it turned out! The interruption of therapy when immediate effects have been achieved and the use of two antibiotics having different mechanisms of action are mentioned as reasonable practices.
– So already the obvious benefits of repeated and prolonged use of antibiotics were apparent but also their adverse effects were reported, particularly as they related to their repeated and prolonged use, with suggestions as to how these could be reduced.
The tendency to use repeated and prolonged courses of antibiotics brought new problems of bacterial resistance, toxicity, and drug allergies. The change in predominant bacterial flora from Staphylococcus aureus to P. aeruginosa appeared to be related to the frequent and prolonged use of antibiotics.
1951 Kessler WR, Andersen DH. Heat prostration in fibrocystic disease of the pancreas and other conditions. Pediatrics 1951; 8:648. [PubMed]
One of the most important papers up to that time from New York. Walter Kessler, the senior resident at the time, and Dorothy Andersen reported 12 children with heat prostration. Ten were admitted during a New York heat wave in 1948 and two in following years; no less than seven were known to have cystic fibrosis. The authors state that – “Unfortunately most of the patients included in this report were admitted during a weekend when it was not feasible to obtain many laboratory data. (Only two patients had electrolytes estimated at the time of admission – in Case 12, Na 130, K 2.7, Cl 59 mEq/l). Moreover, many of the children were too ill at the time of admission to warrant any but the most essential procedures. Several cases of heat prostration were observed among patients in the Babies Hospital during this period. One of these was a six year old child with fibrocystic disease who was in hospital at the time for further study and treatment of chronic and recurrent asthma. However, the relative frequency of cases of heat prostration with antecedent cystic fibrosis of the pancreas was unexpected and seemed of sufficient interest to be placed on record”.
These were the days before air conditioning was generally available in New York and 1948 was a particularly hot summer. Paul di Sant’Agnese was working with Dorothy Andersen at the time and looking after her patients, and later said that he treated these particular infants as Andersen was away vacationing in Europe when they were admitted. The authors of this present report queried whether the sweat glands, as well as the glands of the pancreas and other organs, were inadequate in function or alternatively whether a low grade infection lowered the margin of tolerance to increased temperatures.
At the time of this report there was no explanation as to why infants with CF were particularly susceptible to heat prostration and salt depletion – fortunately Paul di Sant’Agnese decided to find out! This was the first report that children with CF were particularly susceptible to heat. It was this original incident that eventually led Paul di Sant’Agnese to search for the reason for salt depletion in many of these CF infants and eventually to his recognising the abnormally high sweat sodium and chloride, and to a lesser extent potassium. This was undoubtedly the first and most important step towards understanding of the causation of CF up to that time (see di Sant’Agnese et al, 1953 below).
Dr Walter Kessler (1913-1978) was a resident at the time, eventually became a successful expert on paediatric allergy developing “areas of allergy medicine and diagnostic tests for cystic fibrosis”
1951 Levy E. A case of fibrocystic disease of the pancreas with intestinal obstruction. Arch Dis Child 1951; 26:335-339. Full text available. [PubMed]
The first of many reports of late intestinal obstruction which has proved to be an important and frequent complication as the age of survival has increased (also Fisher 1954 below). A seven month old infant known to have CF underwent laparotomy for a presumed intussusception. The plum-coloured distended small bowel was obstructed by putty like material with haemorrhages at the root of the mesentery. The colon was empty and contracted. No surgery was done and the infant died the next day.
1951 Ayers WB, Stowens D, Ochsner A, Platou RV. Splanchnicectomy for pancreatic fibrosis: analysis of results in 24 patients. Pediatrics 1951; 8:657-663. [PubMed]
It was known that stimulation of various abdominal viscera could cause bronchospasm. So it was suggested that the changes of CF in the pancreas may cause a state of “autonomic dyskinesia” causing more or less persistent bronchospasm and bronchorrhoea. It was argued that interruption of the splanchnic nerves may break the afferent limb of such a reflex; so this rather alarming operation was performed to interrupt these nerves. The procedure in 15 children with CF showed only temporary improvement in 3 and no change in the others.
– Mercifully the operation was abandoned although it was understandable that the new and novel treatment caused considerable interest at the time mainly as there was little else to offer many patients (also Am J Dis Child 1951; 82:238-239.[PubMed]). Despite the negative results, the authors still believed the operation “may have a place” in controlling distressing respiratory symptoms. Dorothy Andersen said she had not advised the operation and welcomed this frank report from which “we may expect relief from the pressure on the part of referring physicians and referred patients to persuade us to do splanchnicectomies”. She queried the situations, if any, when the operation would be useful – the possibility of the relief of progressive respiratory distress when all else had failed was mentioned. Subsequently little was heard of this treatment.
1951 Royce SW. Cor pulmonale in infancy and early childhood; report on 34 patients with special reference to the occurrence of pulmonary heart disease in cystic fibrosis of the pancreas. Pediatrics 1951; 8:255-274. [PubMed]
This paper by Stephen Royce of California and the subsequent publication of the paediatric cardiologist Alexander Nadas (Nadas et al, 1952 below) are early reports of cor pulmonale in children with CF who now were surviving for sufficient time for the cardiovascular problems secondary to severe lung disease to become evident. Seventy percent of children who died of chronic lung disease showed evidence of cor pulmonale at autopsy. Over half died in severe right sided heart failure and not surprisingly, therapy of the secondary heart problems was usually unsuccessful although understandably the complication received considerable attention as more children survived for longer periods.
1951 Chung AW, Morales S, Snyderman SE, Lewis JM, Holt LE Jr. Studies in steatorrhoea. Effect of the level of dietary fat upon absorption of fat and other foodstuffs in idiopathic celiac disease and cystic fibrosis of the pancreas. Pediatrics 1951; 7:491-502. [PubMed]
This was a very important paper as it showed that fat absorption remained proportional to the dietary intake. Thus increasing fat intake, as was done so successfully in Toronto by Douglas Crozier (Crozier 1974 below), would be likely to improve total fat absorption and thus energy absorption. However, many clinicians and patients noted that higher fat intakes increased the already unpleasant abdominal symptoms, the volume of the stools and faecal calcium loss; therefore they continued to recommend a low fat diet. In fact, many patients could not tolerate a normal fat intake due to distressing abdominal symptoms even with large doses of the relatively inefficient pancreatic enzymes which were available at the time – this was before the acid resistant microspheres became available. These acid resistant microspheres (Pancrease and Creon) were not generally available until the early Eighties and when patients were changed onto them from the older preparations their superiority over standard preparation was immediately quite obvious to both patients and clinicians.
It is no exaggeration to say that these new acid resistant enzymes revolutionised the management of the intestinal malabsorption in people with CF during the Eighties permitting many to take a normal amount of fat in their diet and so improve their energy intake and nutritional state.
1951 Garrard SD, Richmond JB, Hirsch MM. Pseudomonas aeruginosa infection as a complication of therapy in pancreatic fibrosis (Mucoviscidosis). Pediatrics 1951; 8:482-8.[PubMed]
The authors discuss the potential problems of antibiotic prophylaxis – the potential for altering the tracheobronchial flora and the importance of Pseudomonas aeruginosa as an emerging opportunistic infection challenge. They asked the paediatric community to critically examine the clinical recommendation for prolonged antibiotic prophylaxis. They suggested – “Effective antibiotics should be employed judiciously and changed when specifically indicated, based upon cultures of the tracheobronchial secretions. To minimize the appearance of resistant strains, combinations of two antibiotics having different mechanisms of action are desirable”.
– This practice is still recommended but still not always heeded by paediatricians. In fact, a recent Cochrane Systematic Review failed to find published evidence supporting the use of two intravenous antibiotics rather than monotherapy – however, serious consequences may have been related to the habitual use of intravenous ceftazidime monotherapy in one large UK CF centre (Cheng et al, 1996 below) where a multiresistant P. aeruginosa eventually affected a majority of the patients. So virtually all experienced clinicians would now use two anti-Pseudomonal antibiotics for intravenous antibiotic treatment.
This present paper from Chicago, is said to be the first report of Pseudomonas aeruginosa as a significant pathogen in people with CF. However, Dorothy Andersen had already noted in 1949 – “those with most severe changes sometimes develop bronchitis due to Ps. pyocyaneus (the old term for Pseudomonas aeruginosa) or other gram negative bacilli, a complication rarely seen before the days of penicillin” (Andersen, 1949 above).
1951 Denton R, Smith RM. Portable humidifying unit. II. Large capacity metal nebulizer. Am J Dis Child 1951; 82:433- 438. [PubMed]
Robert Denton of Philadelphia was a scientist whose wife, Wynne Sharples, was a paediatrician – they had two children with cystic fibrosis. This is one of Robert Denton’s early papers which was said to set the scene for mist tent therapy. Soon Denton produced a clinical paper describing mist tent therapy (Denton R. Dis Chest 1955; 28:123-140 below) a treatment which was eventually widely used in the USA.
Early encouraging reports of mist tent therapy (Matthews LW et al. Pediatrics 1967; 39:176 below; Doershuk CF et al. Pediatrics 1968; 41:723-732. [PubMed]; Parks CR. J Pediatr 1970; 76: 305-313. [PubMed]) were eventually followed by others failing to demonstrate benefit from the treatment (Motoyama EK et al. Pediatrics 1972; 50:299 below; Chang N et al. Am Rev Respir Dis 1973; 107:672 below) and the mist tent treatment was eventually abandoned by most, but not all clinics, in the early Seventies.
1952 Nadas AS, Cogan G, Landing BH, Shwachman H. Studies in pancreatic fibrosis: cor pulmonale; clinical and pathologic observations. Pediatrics 1952; 10:319-327. [PubMed]
Alexander Nadas (1913 – 2000) (fig.18) of Harvard was described as the father of paediatric cardiology. This is another early report of cardiac complications in eight of 45 children aged six months to 17 years (17% of the patients); one died
Fig. 18 Alexander Nadas.
in right heart failure, the rest showed electrocardiographic changes of right ventricular hypertrophy. The authors suggested that cardiac complications may be an increasing problem with the efficiency of antibiotic treatment and increasing survival and this proved to be the case (also Royce, 1951 above).
1952 Shwachman H, Silverman BK, Patterson PR, Zheutlin LJ. Antibiotics in treatment of pancreatic fibrosis with emphasis on terramycin. JAMA 1952; 149:1101-1108. [PubMed]
Terramycin, aureomycin and mixed varied antibiotic treatments were compared. All those on terramycin, most of those on aureomycin and the mixed group responded well. Terramycin was introduced in early 1950 and well tolerated. Shwachman mentions the importance of early diagnosis and prolonged treatment also the value of nebulised penicillin and streptomycin (the value of which later he seemed to doubt). As with aureomycin, withdrawal of terramycin led to relapse and it was decided to use the drugs continuously – the subject of a subsequent report of patients so treated (Shwachman et al, 1954 below).
1952 Buchanan DJ, Rapoport S. Chemical comparison of normal meconium and meconium from a patient with meconium ileus. Pediatrics 1952; 9:304-310.[PubMed]
This is the first report of increased protein content in the meconium of an infant with meconium ileus when compared with meconium from three non-CF infants. Normal meconium contained less nitrogen than the meconium from the CF infant with meconium ileus. This observation would eventually form the basis of the BM Meconium screening test for cystic fibrosis (also Green et al, 1958 below; Green & Shwachman, 1968 below; Schutt & Isles, 1968 below)
1952 Lavik PS, Matthews LW, Buckaloo GW, Lemm FJ, Spector S, Friedell HL. Use of I 131 labelled protein in the study of protein digestion and absorption in children with and without cystic fibrosis of the pancreas. Pediatrics 1952; 10:667-676. [PubMed]
Nine controls and 5 children with CF were studied using a test meal with I131 labelled protein. Less than 6% of the ingested isotope was excreted in the faeces in non-CF children but 10-40% was excreted by children with cystic fibrosis; there was a 50% decrease in faecal loss when the CF children were on pancreatin, so failure of protein absorption due to failure of digestion was confirmed.
Shwachman commented that this study further showed that pancreatin was working as there was, even then, still some dispute as to its value in improving absorption.

Fig.19. Martin Bodian

Fig. 20 Archie Norman

Fig.21 Cedric Carter
1952 O’Brien D, Powell BW. Tryptic activity of stools in newborn. Great Ormond Street J, 1952; 33-35.
One of a number of papers discussing the estimation of faecal tryptic activity as an indication of pancreatic function, suggesting that absence of tryptic activity in the first few days suggested cystic fibrosis.
It is not surprising that there were a number of papers published on this subject as the demonstration of tryptic activity in the stools was the most important test, other than duodenal intubation, in differentiating CF from coeliac disease in the days before the sweat test became more widely available during the late Fifties and Sixties
1952 Bodian ML. Fibrocystic Disease of the Pancreas. A Congenital Disorder of Mucus Production (Mucosis). London, W Heinemann, 1952.
The first substantial work on CF from the UK by Martin Bodian (Fig.19) and his colleagues at the Hospital for Sick Children, Great Ormond Street, London (GOS). Dr. Martin Bodian (1910-1963),(fig.19) had been appointed morbid anatomist at GOS in 1946. Dr Archie Norman (1912-2016) (fig. 20) was the paediatrician in charge of the CF clinic at GOS and a leading figure in CF care in the UK for many years. Dr. Cedric Carter (1917-1984), (fig. 21) was a clinical geneticist who started the first genetic counselling clinic at GOS in 1957.
In the preface of this book Martin Bodian notes the contents encompass almost a decade of work since Donald Patterson diagnosed the first child with CF at Great Ormond Street in 1943 (above). The authors reviewed their own and previously published families and concluded there was a recessive mode of inheritance and suggested parents of a child with CF should be given a 1 in 4 risk of further children being affected; this confirmed the findings of Andersen & Hodges (1946 above) and the earlier suggestion of Howard (1944 above).
1952 Johnstone DE. Studies on cystic fibrosis of pancreas: role of various diluents and the dilution factor in interpretation of X-ray film test for fecal trypsin. Am J Dis Child 1952; 84:191-198. [PubMed]
An astonishing 9,600 tests on 963 stool specimens from 216 children! Johnstone had already published on false negativity with the stool gelatine test due to bacterial digestion of the gelatine (Johnstone & Neter, 1951 above). However, in this study he showed importantly that false results did not occur if a 1/120 dilution of the stool was used.
This test was still very important for diagnosis in 1952, as the sweat test was not yet available and duodenal intubation and aspiration was invasive, unpleasant for the infant, and difficult for the nursing and medical staff.
1952 Shwachman H, Leubner H, Patterson P, Weill CC. Mucoviscidosis with partial pancreatic insufficiency. Am J Dis Child 1952; 84:763-765.[PubMed]
Previously some people with CF had escaped diagnosis as the duodenal trypsin test gave normal results. Progressive loss of pancreatic activity could be shown. Partial pancreatic insufficiency could be demonstrated by various techniques – examining duodenal fluid for various enzymes, viscosity and pH. In the discussion the need to differentiate the various causes of coeliac syndrome was stressed as some coeliac children were being falsely labelled as CF as a result of “the present interest in the cystic fibrosis”. For many years a frequent examination question for medical students was to list the differences between coeliac disease and cystic fibrosis; just as they must know the differences between children with hypothyroidism and Down’s syndrome.
– By 1952 Shwachman had obviously become cautious about using secretin intravenously for pancreatic function tests as he warns that secretin “may occasionally produce disastrous effects…..usually not a purified substance….some children are allergic to it”. So, although 10 years previously Shwachman had presented a study of secretin pancreatic stimulation tests in children (Maddock et al, 1943 above), he now preferred olive oil as a stimulant and believed “The most reliable diagnostic procedure is study of the duodenal fluid” (also Gibbs et al, 1950 above).
1952 Lloyd MS, Robitzek EH. Pneumonectomy for suppurative disease in cystic fibrosis of the pancreas and lung: case report. Q Bull Sea View Hosp 1952; 13:114-124. [PubMed]
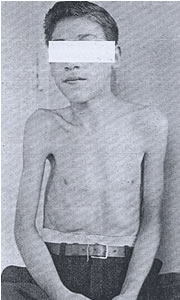
Fig 22. Boy who had a pneumonectomy
This quite remarkable report, from Staten Island Hospital, New York, is possibly the first of such radical lung surgery in a person with CF for extensive lung damage.
The report concerns a boy with CF born in 1935 who had a right pneumonectomy aged 14 years when severely ill and in virtual respiratory failure. After the operation he was said to be considerably improved with an “excellent” physical condition much helped by regular terramycin. Although he had a morning cough there were no added sounds in the remaining left lung (fig.22).
There have been many subsequent reports of benefit from resection of severely affected parts of the lung in children with CF mostly with good results. At this time, in 1952, surgery was not recommended for non-CF bronchiectasis but the results in this and many subsequent reports are surprisingly good if the patient had cystic fibrosis. In this paper Milton Lloyd observed “the improved outlook achieved by better medical care demands our attitude to surgical therapy be re-examined”.
Sea View Hospital, in the centre of Staten Island, was at one time the largest TB hospital when fresh air, away from the polluted air of the cities (a major factor in chest disease at the time), was considered to be the most effective treatment. The buildings have long since fallen into disrepair.
1952 Wallenstein L, Snyder J. Neurotoxic reactions to Chloromycetin. Ann Int Med 1952; 36:1526-1528. [PubMed]
The first report of some of the serious side effects of chloramphenicol (the antibiotic first became available in 1951) in a 24 year-old patient with ulcerative colitis after 4 months continuous treatment with the antibiotic. The lady developed loss of vision, optic and peripheral neuritis but fortunately this settled when the drug was stopped.
This is the first of a number of reports of chloramphenicol toxicity following prolonged use (Keith CG. Arch Dis Child 1966; 41:262-266. [PubMed]; Harley RD et al. Trans Am Acad Ophthalmol Otolaryngol 1970; 74:1011-1031.[PubMed]). Lasky MA et al. (JAMA 1953; 151:1403-1404. [PubMed]) reported a boy aged 14 with Staphylococcal endocarditis who had 6 g of chloramphenicol daily for 6 weeks and developed optic neuritis; later there was no recovery of vision.
The first reports of side effects in people with CF, who also required prolonged courses of antibiotics, was some 10 years later (Denning et al, 1963 below; Huang NN. J Pediatr 1966; 68:32-44 below).

Fig.23 Robert Darling. From www.cumc.columbia.edu
1953 Darling RC, di Sant’Agnese PA, Perera GA, Andersen DH. Electrolyte abnormalities of the sweat in fibrocystic disease of pancreas. Am J M Sc 1953; 225:67-70.[PubMed]
The first report of elevated sweat electrolytes in cystic fibrosis. di Sant’Agnese (1914-2005) (fig. 24) collaborated with Robert (Bob) Darling (1908-1998)(fig.23) who was the head of the Rehabilitation Department of the Columbia Presbyterian Hospital, New York. In this department there was a constant temperature room and a method of collecting sweat. Initially two teenagers with CF and two controls were selected and although the sweating rate was similar the level of electrolytes was much higher in the patients with cystic fibrosis. Subsequently sweat from nine CF children and eight controls showed chloride more than three times higher in the people with CF than in the controls. This was an unexpected finding quite unrelated to any previously recognised abnormalities in the condition (di Sant’Agnese et al, 1953 below) but it was the most important observation since the clear identification of CF as a specific entity by Dorothy Andersen in 1938.
1953 di Sant’Agnese PA, Darling RC, Perera GA, Shea E. Sweat electrolyte disturbances associated with childhood pancreatic disease. Am J Med 1953; 15:777-784. [PubMed]
In this study there were 50 patients with CF, 9 with other pancreatic diseases and 50 controls. All the CF patients had similar elevations in the sweat electrolytes. Their adrenal and renal function was normal. The authors considered the findings to justify abandoning the term “mucoviscidosis” and returning to the unsatisfactory term “cystic fibrosis of the pancreas” until a better one was proposed.
1953 di Sant’ Agnese PA, Darling RC, Perera GA, Shea E. Abnormal electrolyte composition of the sweat in cystic fibrosis: Clinical significance and relationship to the disease. Pediatrics 1953; 12: 549-563. [PubMed]
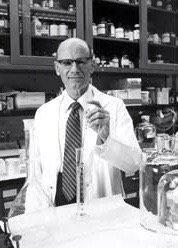
Fig. 24 Paul di Sant’Agnese
This is the main paper that di Sant’Agnese (fig.24) himself quotes as describing the sweat electrolyte abnormality expanding on the paper of Darling et al, 1953 (above). Di Sant’Agnese mentions the original report of Kessler and Andersen 1951 (above) and also that the susceptibility of patients with CF to heat in the summers was noted also during subsequent summers after 1948. Paul Quinton more recently recalled that di Sant’Agnese told him that the development of heat tolerance among troops sent to North Africa was attributed to adaptations to sweating, so di Sant’Agnese pursued excessive salt loss in the sweat as the most likely origin of volume depletion during the high heat stress (Quinton, 1999 below).
Bob Darling (Fig.23) was head of Rehabilitation at Columbia Presbyterian Hospital and had a constant temperature room. Di Sant’Agnese decided “as a shot in the dark to see if sweating function was impaired in CF patients that would lead to a smaller than normal volume of sweat, or whether there was something wrong with the sweat electrolyte concentration”. di Sant’Agnese continued – “In April 1952 two teenage children with CF and two controls were put in the constant temperature room and their sweat then analysed for electrolytes. To my surprise and excitement the answer was right there. There was a tremendous difference in the sweat electrolyte concentration between the two groups”. “In contrast the sweating rate was similar in the two groups”. (Described in detail by Paul di Sant’Agnese. Experiences of a Pioneer Researcher. In: Doershuk CF (ed.) Cystic Fibrosis in the 20th Century 2001; Fanos JH. 2008; 17-35.). Sant’Agnese and colleagues showed the sweat abnormality was unrelated to renal or adrenal disease and was definitely related to sweat losses.
For this present paper they examined 43 people with CF, nine patients with other pancreatic diseases and 50 controls in a room at 32.2 C for one to two hours. Sweat was collected onto dry gauze under adhesive waterproof plaster. Sweat chloride in the CF patients was 106 (60-160) meq/l, in controls and other pancreatic diseases only 32 meq/l (4-80) and in CF the Na 133 (80-190), and in controls 59 (10-120).
This was undoubtedly the most important advance in the understanding of CF up to that time. However, astonishingly, di Sant’Agnese recalls the paper received a very cool reception at the 1953 meeting of the American Pediatric Society with not a single question!! Also when presented before Jas Kuno, apparently a distinguished sweat physiologist, Kuno uttered one word -“impossible”- and walked out of the room! It is also said that even di Sant’ Agnes’s close colleague Dorothy Andersen was at first reluctant to accept the findings. However, and perhaps predictably, Harry Shwachman soon visited di Sant’Agnese in New York; he was impressed and with his usual alacrity and energy was able to present a large supportive series by October 1954 much to di Sant’Agnese’s delight!
1953 Dicke WK, Weijers HA, van de Kamer JH. Coeliac disease. The presence in wheat of a factor having a deleterious effect in cases of coeliac disease. Acta Paediatr Scand 1953; 42:34-42. [PubMed]
Although not strictly related to CF, this was undoubtedly a major discovery and an advance in further separating coeliac disease (the aetiology of which was unknown up to this time) from CF and other causes of intestinal malabsorption. The characteristic intestinal mucosal changes of subtotal villous atrophy were not described until the late Fifties (for details see the entry of Gee, 1888 above in this History section).

Fig. 24 Willem Dicke. From Wikipedia.
Dr Willem Dicke,(1905-1962) (fig.24) was a Dutch paediatrician who described the central role of a “wheat factor”, which was not starch but eventually identified as gluten, in the aetiology of coeliac disease in his MD Thesis in 1952. Apparently he had believed that wheat was the injurious factor since the Thirties. The account of his numerous clinical observations and eventual collaboration with van de Kamer and Weijers, which eventually led to the discovery, is described in a fascinating article (Pioneer in the gluten free diet: Willem-Karel Dicke 1905-1962, over 50 years of gluten free diet. Van Berge-Henegouwen GP, Mulder CJJ. Gut 1993; 34:1473-1475.[PubMed]. Full article is available).
In 1953, although CF had been clearly described as one cause of the coeliac syndrome, the sweat electrolyte abnormality was not generally known at this time. So the diagnosis of CF was still a problem and rested on demonstrating low trypsin levels in the duodenal fluid or faeces of a child with intestinal malabsorption. Also the characteristic subtotal villous atrophy of the small bowel in coeliac disease had not been described; this was first identified by Paulley in 1954 in full thickness specimens of small bowel obtained at laparotomy from adults (Paulley J. BMJ 1954; ii: 1318-1321. [PubMed]). Small bowel subtotal villous atrophy was identified in vivo by per oral biopsy by Margot Shiner in 1957 (Sakula J, Shiner M. Lancet 1957; ii: 876. [PubMed]); also Charlotte Anderson showed the small bowel changes in children with coeliac disease were reversible after gluten withdrawal (Anderson CM. Arch Dis Child 1960; 35:419-27.[PubMed]) (see the entry of Gee 1888 in the Early Years section of this History for more details and images). During the late Sixties jejunal small bowel biopsy for children gradually became more generally available in the UK.
In Leeds I provided a jejunal biopsy service for Yorkshire paediatricians from 1968 (Littlewood JM. Coeliac Disease in Childhood. In: Howdle PD (ed.): Coeliac Disease. London: Bailliere Tindal, 1996:295-328. [PubMed]) and ultimately in our unit we performed over 1000 jejunal biopsies, in later years using the fibreoptic endoscope. The accurate diagnosis of gluten induced coeliac disease was of great importance in the evaluation of children with malabsorption syndrome and thus in the differential diagnosis of cystic fibrosis and an important part of our service. . With the availability of both jejunal biopsies and sweat tests in the Sixties, predictably, children who had both CF and coeliac disease were described (Hide and Burman, 1969 below); later children with CF were reported who also had intestinal mucosal damage due to cow’s milk protein intolerance (Hill et al, 1989 below).
So during the late Fifties and Sixties, with the introduction the sweat test and the jejunal biopsy, CF and coeliac disease could be diagnosed confidently in the majority of cases in centres where the two investigations were available and, of great importance, also reliable!
1953 Webster R, Williams H. Hepatic cirrhosis associated with fibrocystic disease of the pancreas: clinical and pathological reports of 5 patients. Arch Dis Child 1953; 28:343-350.[PubMed]
This is the first comprehensive paper on liver involvement in CF describing “an unusual type of multilobular portal cirrhosis”; three were identified at autopsy and two on liver biopsy. The authors considered that protein deficiency, due mainly to pancreatic dysfunction, was the cause of the liver damage.
However, di Sant’Agnese observed that CF was a generalised disease and offered a more likely explanation that it could affect the liver as well as the pancreas, lungs and sweat glands. In commenting on this paper, di Sant’Agnese described six similar cases at the Babies Hospital New York – representing some two percent of the total CF clinic.
1953 di Sant’Agnese PA. Bronchial obstruction with lobar atelectasis and emphysema in cystic fibrosis of pancreas. Pediatrics 1953; 2:178-190. [PubMed]
This paper describes the classical right upper lobe collapse so characteristic of CF and notes bronchoscopy was usually not effective in expanding the collapsed lobe (however, only rigid bronchoscopes were available at that time). Of 211 children with CF 10% presented with collapse of one or more lobes. In the discussion it is obvious that there was still a lingering suggestion that vitamin A deficiency “may contribute but not a major cause”.
Harry Shwachman agreed that atelectasis worsens the prognosis but also noted – “The hypothesis suggesting an imbalance of the autonomic nervous system which may affect many systems and organs is attractive”. So there was still no clear explanation for the various manifestations of the condition and some suspected abnormal function of the autonomic nervous system. With regard to the association of the pancreatic lesions and the pulmonary complications, di Sant’Agnese concludes that “a satisfactory understanding of this problem has not yet been attained” which seemed to sum up the situation.
1954 May CD. Cystic Fibrosis of the Pancreas in Infants and Children. Charles C Thomas. Springfield, Illinois. 1954.
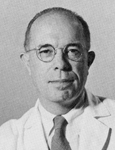
Fig. 25 Charles May medicine.uiowa.edu
A 93 page monograph reviewing the current knowledge on cystic fibrosis. Charles May (Fig.25) acknowledges many years of shared experience with Dr Charles Upton Lowe (1921-2012),(fig. 26) at the time associate Professor of Pediatrics at Buffalo.
There is an interesting dedication at the beginning – “To the practitioners, Margaret Harper (1938 above) of Sydney, Australia and Arthur H Parmelee of Chicago, Illinois (1935 above) who recognised the salient clinical features of patients found to have cystic fibrosis of the pancreas, published the first papers indicating the frequency and importance of the disease, and clearly set it apart from celiac disease against the prevalent practice”. Interestingly Dorothy Andersen is not mentioned in this context! In fact May recalls how Blackfan was steadily preoccupied during the Thirties with the problem of recognising infants who had cystic fibrosis of the pancreas culminating in his report of 1938 (Blackfan & May, 1938 above).
In the Chapter III,”Historical”, of this book May writes “Thus the history of the discovery of cystic fibrosis of the pancreas in infants is a revealing example of the gradual accumulation of observations from a variety of independent sources which may be required to attain a clear conception of a disease, even though its manifestations clinically and pathologically are flagrant. That recognition of this disease was delayed until the most recent times should serve as a reminder of the continuing need for critical clinical observation in this age of overwhelming dependence on the laboratory” – this written in 1954!! Although this is wise advice, it was only through observations in the laboratory of the characteristic pancreatic histological changes that CF was identified as a distinct clinical entity by Dorothy Andersen. Also it is interesting that there was no mention of Dorothy Andersen except that “Andersen’s original paper should be consulted for the most adequate illustrations of progressive stages in the development of this (pancreatic) lesion”.
In the “Treatment” chapter diet and the use of pancreatin precede the treatment of the chest. The important relationship between the activity of the chest infection and nutritional state is mentioned. There is a rather unenthusiastic approach to pancreatin therapy which is considered to dampen the appetite with only modest benefit on absorption so “if the infant or child does not accept pancreatin readily or if the expense is prohibitive one need not feel badly if this form of therapy must be abandoned”.
Fig. 26 Charles Upton Lowe
Dr Charles D May (1908-1992) (Fig. 26) was a graduate of Harvard College, He received his medical degree from the Harvard Medical School in 1935. In World War II he served in the Army Medical Corps during which time he delivered a lecture on CF at the Royal Society of Medicine (Proc R Soc Med 1944; 37:311-3). After the war he returned to research at Harvard Medical School in 1946. He was an associate professor of pediatrics at the University of Minnesota from 1947 to 1952, when he joined the medical faculty at the University of Iowa College of Medicine as professor and chairman of the pediatrics department. In 1957 Dr. May was appointed a clinical professor of pediatrics at the Columbia University College of Physicians and Surgeons, and joined the New York University school of medicine at the same position in 1961. In 1970 he was named to a joint appointment on the faculty of the University of Colorado Medical School and the National Jewish Hospital in Denver. Dr May published extensively on many aspects of nutrion and cystic fibrosis. He retired in 1980 (www.myheritage.com/archives).
Dr Charles Upton Lowe (1921-2012) (fig.14) mentioned by Charles May was a distinguished paediatrician who held various academic paediatric appointments finishing as Scientific Director of the National Institute of Child Health and Human Development, NIH, Bethesda. He had a wide breadth of interests and described the sex-linked metabolic disorder now known as Lowe Syndrome (oculo-cerebro-renal syndrome).
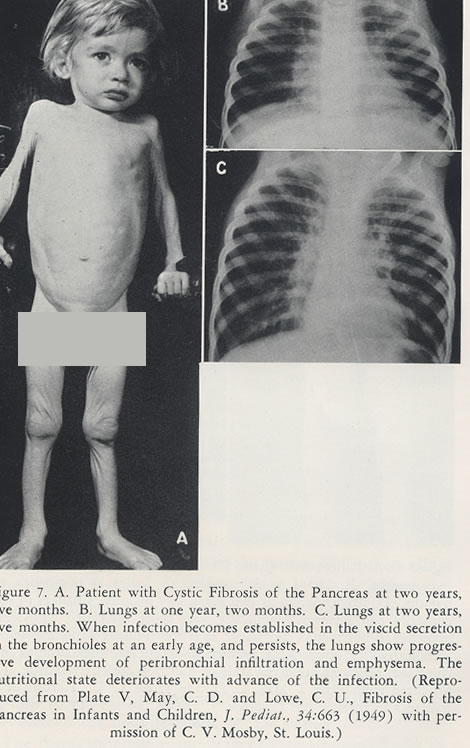
Fig.27 An illustration from C D May’s book of a typical child with CF in the Fifties. Originally from May CD, Lowe CU. Fibrosis of the pancreas in Infants and Children. J Pediat 1949; 34:663 with permission of C V Mosby, St Louis.
1954 West JR, Levin MS, di Sant’Agnese PA. Studies of pulmonary function in cystic fibrosis of the pancreas. Pediatrics 1954; 13:155-164. [PubMed]
These were the first pulmonary function tests reported in children with cystic fibrosis. Most children find pulmonary function tests using a spirometer difficult to perform before the age of six years or so. But as more patients survived through early childhood to an age when they could perform lung function, of a number of studies were reported. The findings in six patients aged 12 to 14 years clearly identified most of the important features of impaired lung function found in cystic fibrosis i.e. essentially there was difficulty moving air in and out of the lungs.
These abnormalities in respiratory function were confirmed in later studies e.g. the increase in residual volume in relation to total lung capacity as early changes and reduced total lung capacity and CO2 retention as late features; also noted were abnormal pulmonary gas mixing and other features of non-uniform distribution of alveolar ventilation as a result of bronchial obstruction.
1954 Olim CB, Ciuti A. Meconium ileus: new method of relieving obstruction. Ann Surg 1954; 140:736-740. [PubMed]
Unusual success was reported with local rectal instillation of hydrogen peroxide in removing the inspissated meconium in two infants. Robert Gross, a paediatric surgeon, commenting on the paper was “so impressed with the authors’ report that I shall certainly try the technique”. Local instillation of hydrogen peroxide appeared to be a popular method of relieving bowel blockages and was recommended for severe constipation with obstruction. However, the method did not appear to become popular for treating meconium ileus as there were problems with colonic injuries. The practice was gradually abandoned.
1954 Fisher OD. Intestinal obstruction as a late complication of fibrocystic disease of pancreas (Mucosis). Arch Dis Child 1954; 29:262-264. [PubMed]
From the Royal Belfast Children’s Hospital, the second report of late obstruction (first was Levy, 1951 above), on this occasion in an infant aged 13 months with CF, which closely followed cessation of pancreatin therapy the supply of which had run out five days before admission. The whole bowel was intermittently obstructed by masses of putty-like material and material like liquid rubber was removed via an incision, pancreatin was restarted and the infant recovered. Fisher observed rather strangely “Suggesting use of pancreatin as a form of replacement therapy”.
Shwachman commented he had seen six such patients already, three of whom were surgically treated. He mentions the presence of a palpable abdominal mass in lower right quadrant and material which was “rock-like” – the right iliac fossa hard mass was later recognised as a relatively common feature of children and adults with distal intestinal obstruction syndrome (DIOS) as more older children and adults attended CF clinics.
1954 McIntosh R. Cystic fibrosis of the pancreas. Patients over 10 years of age. Acta Paediatr 1954; (Supp.100): 467.[PubMed]
From 1931 Dr Rustin McIntosh (1894-1986) (fig. 27), a distinguished general paediatrician, was Chairman of the Babies Hospital, New York where Dorothy Andersen and Paul di Sant’Agnese developed their CF service. Out of a large group of their patients McIntosh describes 27 who were over the age of 10 years (four of whom had died) from the Colombia Presbyterian Medical Center in New York. It is of note that all the patients already had severe respiratory involvement although all retained an optimistic outlook for the future. Fatty foods were avoided because of symptoms and only half took pancreatic enzymes and they did equally well without them. The report was mentioned by Shwachman in 1958 as the largest series of older patients so far published.
Fig.28 Rustin McIntosh
1954 Shwachman H, Catzel P, Patterson PR, Stoppelman MRH. Mucoviscidosis: an evaluation of continuous and prolonged antibiotic therapy. Am J Dis Child 1954; 88: 380-382. (Meeting presentation by invitation)
One hundred and twenty three patients had received continuous antibiotic therapy (Aureomycin or Terramycin) for six months to over six years. Broad spectrum antibiotics had been introduced first in 1949. The results were least satisfactory in advanced cases. There was no evidence therapy prevented onset of chest disease but it could control symptoms for prolonged periods. The age of onset of cough influenced survival – the outlook was bad if the onset was at less than three months. Fifty six showed progressive changes (33 were alive and 23 had died), 24 were unchanged and five improved during the period of antibiotic therapy. Between 1945-54 the average age of death was 45.2 months; up to 1949 the age of death had been only 12.8 months.
The discussion at this meeting ranged from concerned speculation of patients surviving and “breeding” which one speaker observed would be “disastrous” (!), to whether the patients would have done as well with discontinuous therapy. Had Shwachman more “survivors” in his series one questioner asked? In reply Shwachman contrasts his figures with the UK Great Ormond Street, London figures reported in 1952 by Martin Bodian which reflect the impressive results achieved by Shwachman and his colleagues as follows-
BODIAN SERIES vs. SHWACHMAN SERIES
Total patients: 116 vs. 123
Dead: 68 (57%) vs. 22 (18%);
Alive: 47 (41%) vs. 101 (87%);
>5 years: 15 (13%) vs. 61 (50%)
1954 Stoppelman MR, Shwachman H. Effect of antibiotic therapy on mucoviscidosis: bacteriologic study on 140 patients. N Eng J Med 1954; 251:759-763.[PubMed]
A review of the beneficial effects of antibiotic therapy in CF – treatment which had then been available for about 10 years since the mid-Forties. Mildly affected children had chlortetracycline or oxytetracycline; the worst affected had sulphadiazine, chloramphenicol or erythromycin. The worst affected patients also had short courses of penicillin and streptomycin aerosol therapy. Most patients still had S. aureus as the main pathogen – mostly still sensitive to penicillin but resistant to chlortetracycline and oxytetracycline.
A major difference from modern CF therapy was that intravenous (IV) antibiotic therapy was rarely used as venous access in small children, and particularly repeated venous access, was still a major technical problem. In this reviewer’s experience in the Fifties single episodes where IV access was required were often managed by cutting down on a vein at the ankle and inserting a metal cannula which was tied in; this would last for a few days at the most. Of course, the vein was lost for future use as it had been ligated, so the method was quite unsuitable for repeated venous access for which other techniques were developed subsequently e.g. scalp vein needles, venous long lines and eventually totally implantable venous access devices – the latter not for some years.
1955 Gatzimos CD, Jowitt RH. Jaundice in mucoviscidosis (fibrocystic disease of the pancreas). Report of four cases. Am J Dis Child 1955; 89:182. [PubMed]
In contrast to laboratory and pathological evidence of liver disease, clinical jaundice in people with CF is uncommon even in those with abnormal liver function tests. From 1922 to 1954, 6741 autopsies were performed at Indianapolis University Medical Centre; 3517 were children and 14 had CF in four of whom jaundice had been the main complaint. The four of 14 with CF is a higher incidence of clinical jaundice than in previous series (Andersen, 1938 above; May & Lowe, 1949 above; Bodian, 1952 above). These authors suggested that CF should always be considered in the differential diagnosis of jaundice in infants.
Subsequent experience has confirmed the advice that CF should always be excluded particularly when a small infant with obstructive jaundice is suspected of having congenital biliary atresia, as on occasion an infant suspected of having congenital biliary atresia has been treated with a Kasai operation (a major procedure anastomosing the underside of the liver to the bowel in an attempt to overcome biliary atresia) only to discover later that the infant had CF with severe neonatal cholestatic jaundice (Perkins WG. et al. Cystic fibrosis mistaken for idiopathic biliary atresia. Clin Pediatr 1985; 24:107-109.[PubMed]).
1955 Allen RA, Baggenstoss AH. Pathogenesis of fibrocystic disease of the pancreas: study of ducts by serial sections. Am J Path 1955; 31:337-351. [PubMed]
The authors note the current theories of pathogenesis are 1) vitamin A deficiency 2) imbalance of sympathetic nervous system 3) altered secretions of the glandular structures including the pancreas 4) inflammation 5) congenital atresia or stenosis of the pancreatic duct. They consider that their detailed histological findings lend support to the theory that the fundamental defect lies in maldevelopment of the pancreatic duct system.
A pertinent comment on this paper by J M Craig was that the authors ignored the considerable clinical and pathological evidence of involvement of other organ systems. This paper also emphasises the fact that, at the time, the cause of CF was still totally obscure other than the condition was inherited in a Mendelian recessive manner.
1955 Denton R. The clinical use of continuous nebulization in bronchopulmonary disease. Dis Chest 1955; 28:123-140.[PubMed]
Robert Denton was a scientist and his wife, Wynne Sharples was a paediatrician. He observed that their two children with CF appeared to improve when they slept in tents into which was nebulised 3% saline or a dilute 10% propylene glycol solution. However, although the concept of continuous nebulisation was described as a new technique, its use for children with CF was not mentioned in this particular paper.
Harry Shwachman had used nocturnal mist tent therapy for children with CF from 1958 and initially was impressed by its effectiveness in patients with CF who had thick bronchial secretions. The experience of authorities such as Leroy Matthews, Robert Denton and Harry Shwachman led to the incorporation of nocturnal mist tent therapy into CF treatment programmes including the Cleveland Comprehensive Treatment Programme (Matthews et al, 1964 below). Eventually the mist tent was recommended by the US CF Foundation through the Sixties until a number of studies failed to confirm the impression that the treatment was of benefit (see Topic on Mist tents).
Shwachman (somewhat changing his ground!) later recalled that “a group of doctors in Cleveland (Matthews et al, 1964) started using the mist tent. Because they were enthusiastic over it and thought it was good we tried it. But after 5 or 6 years we asked our parents if they noticed any improvement and they said no. We tried it on and off and decided it didn’t help”. Although mist tents were widely used in North America for people with CF they were never popular in the UK and eventually their use was abandoned after trials in the late Sixties failed to show significant deposition of fluid in the lower airways or clinical benefit.
Robert Denton published nearly 40 papers mostly on mechanical factors in airway secretion from the early Fifties including nebulisation, effects of mechanical percussion, rheology of sputum and the mucolytic acetyl cysteine. His wife Wynne Sharples was also involved with the CF Foundation in the early years.
[See also the Topic on Mist Tents]
1955 Keats TE. Generalized pulmonary emphysema as an isolated manifestation of early cystic fibrosis of the pancreas. Radiology 1955; 65:223-226. [PubMed]
Commonly attributed to infection and secondary obstruction, the presence of hyperinflation before infection suggested an intrinsic abnormality of the composition of the airway secretion causing some degree of obstruction. This is now known to be the case since the availability of infant respiratory function studies. Paul di Sant’Agnese confirmed that he had seen isolated emphysema as the only early manifestation of CF when infection had been “held in check” by antibiotics.
Modern paediatricians will have seen this in infants with CF diagnosed following neonatal CF screening who have not yet acquired infection or where infection has been prevented by prophylactic flucloxacillin. In all these infants there is some slight airway obstruction in the smaller airways due to the abnormal airway secretions and this is reflected as some over inflation evident on the chest X-ray; some degree of airway obstruction is also evident on infant respiratory function testing (Ranganathan al. 2001 below)
1955 Harris R, Norman AP, Payne WW. The effect of pancreatin therapy on fat absorption and nitrogen retention in children with fibrocystic disease of the pancreas. Arch Dis Child 1955; 30:424-427. [PubMed]
A classic study from Dr Archie Norman’s unit at the Hospital for Sick Children, Great Ormond Street Hospital, London showing a modest improvement in the absorption of fat and nitrogen with pancreatin enzyme therapy (powdered pancreatin triple strength treated to form enteric coated granules). Fat absorption increased from 46% to 71% of intake and faecal nitrogen was reduced by 50% from 23.10 gm to 10.27 gm per day.
These improvements in absorption with pancreatin are modest by present standards as with modern acid resistant enzymes many patients will achieve more than 90% absorption of ingested fat (normal being over 95%). In the previous year Charles May had claimed that better nutritional results were obtained by the administration of a generous high protein diet without pancreatin which he believed impaired the appetite. So May was asked to comment on this particular paper (Pediatric Year Book, 1955) and he mentioned the negative nitrogen balance (due to the increased energy requirement which was later established in a number of studies (Pencharz et al. J Ped Gastro Nutr 1984; 3 (Suppl 1):S147-S153 below; Buchdahl RM et al. 1988; 64:1810-1816 below). He considered that the sensible approach was to try pancreatin in adequate dosage and judge by the clinical response taking pains not to attribute the improvement in weight, which may resulted from treating the chest infection, as due to the action of pancreatin. He observed that a more effective and less expensive means of pancreatic enzyme substitution therapy was sorely needed.

Fig.17 Milton and Evelyn Graub and their children Lee, Pearl and Kathy. With permission.
1955 THE NATIONAL CF RESEARCH FOUNDATION FORMED IN THE USA
The first national CF organisation was formed in the USA; later it became the US Cystic Fibrosis Foundation. National organizations have been central to clinical services and research. Evelyn and Milton Graub (figure 18) describe the early forming of small groups of parents in Philadelphia in 1952 when the disease was virtually unknown and visiting every new family personally and running the first fund raising event in 1954 where Dr Wynne Sharples, mother of two children with CF, a local socialite and non-practicing paediatrician, was the guest speaker. She was married to Dr Robert Denton who was involved in mucus chemistry and later with the use of mist tent treatment. There were many abortive attempts by the Graubs to raise the profile and awareness of CF – they were even accused of trying to steal their colleagues’ patients!
In 1955 a Charter was obtained and the CF Foundation was formed after a Founders’ Meeting in New York. The initial proposal by Dr Sharples, the first President, was for local Chapters to raise funds without having any central representation but after the Graubs objected the local Chapters were given 50% representation. So in 1955 the National Cystic Fibrosis Foundation was formed. The first Scientific Meeting was held in 1955 in Iowa where Dr Charles May was Chairman of the Department of Pediatrics. The meeting was attended by many of the well known names in CF at the time including Harry Shwachman, Paul di Sant’Agnese, Leroy Matthews, Paul Patterson, Gordon Gibbs, Giulio Barbero, Warren Warwick, Wynne Sharples, and Milton Graub (who apparently invited himself!). The Foundation wisely declined offers to merge with other organization such as the Polio Foundation
Subsequently the organization grew, many new Chapters started and the network of CF Centres was established in 1961 under the direction of Dr Kenneth Landauer. The Centres were to be located only at teaching hospitals and devoted to care, teaching and research; there were 2 centres in 1961, and 30 by 1962. The patient Data Registry was started in 1966. (Further details in Cystic Fibrosis in the 20th Century. People Events and Progress. Doershuk CF (Ed). A M Publishing Ltd, Cleveland, Ohio. 2001 – with the author’s permission).
Dr Robert Beall PhD
Fig. 18 Robert (Bob) Beall
Robert Beall (figure 18) the President and Chief Executive Officer of the CF Foundation to 2015, retired from his position after 21 years having first joined the CFF in 1980. During his 35 years of work at the CFF, substantial progress was made in CF research and drug development, resulting in an increase in patient life expectancy from 18 year to many patients living well into their 40s.
di Sant’Agnese wrote in 2001 “After the move to Bethesda, we were lucky to get Dr Robert Beall to accept the post of Medical/Scientific Director. At first he was very reluctant to accept this position and I worked quite hard to persuade him to make up his mind. I felt he was the best qualified for this position with his background at the NIH extramural programs and therefore was knowledgeable about grants and had contact with many people. He later became Vice President in charge of medical affairs and then President and CEO of the Foundation. Under the present leadership and with the discovery of the gene for CF and of its innumerable mutations, which helped to propel CF into the limelight, the Foundation has become one of the best organised and most successful medical and health organisations in the United States” ( In Doershuk CF. Cystic Fibrosis in the 20th Century. 2001 below).
Dr Preston Campbell III (fig. 18a) previously Executive Vice President for Medical Affaires succeeded Bob Beall as Chief Executive Officier of the CF Foundation in 2015. He qualified at the University of Virginia Medical School, completed his pediatric residency as chief resident at Vanderbilt University School of Medicine, earned a diploma from the Liverpool (England) School of Tropical Medicine and served as Director of Pediatrics at the Centre Medical Beraca, LaPointe, Haiti. He returned to Vanderbilt to complete his pulmonary training, joined the faculty and served as the Director of the Cystic Fibrosis Center at Vanderbilt. In 1998, Dr. Campbell joined the CF Foundation as the executive vice president for medical affairs, overseeing clinical research, the CF Foundation’s network of specialty care centers and training programs. Dr. Campbell has received numerous awards, including recognition in The Best Doctors in America At the end 2019 Preston Campbell retired as CEO and was succeeded by Michael Boyle
Fig. 19 Michael Boyle
Michael Boyle, MD, (Fig.19) is now president and chief executive officer of the Cystic Fibrosis Foundation. Prior to his appointment as president and CEO, Dr. Boyle served as the Foundation’s senior vice president, therapeutics development from 2015-2019. In that role, Dr. Boyle shaped the Foundation’s clinical research strategy, overseeing the clinical development programs of new treatments for the CF Foundation, as well as the Foundation’s Therapeutics Development Network of 90 academic research centers.

Fig 20 Bruce Marshall
Dr Bruce C Marshall (fig. 20) is the Executive Vice President & Chief Medical Officer at Cystic Fibrosis Foundation based in Bethesda, Maryland. Previously, Bruc Bruce Marshall qualified at the Maryland School of Medicine. in Baltimore. He is closely involved with all matters clinical at the CF Foundation including clinical trials, working parties, guidelines and medical publications including the patient registry.
Further information on the CF Foundation available from the website (www.cff.org).
1955 Shwachman H, Leubner H. Advan Pediat 1955; 7:249-323. [PubMed]
The paper contains the first detailed report of symptomatic diabetes mellitus and CF in a white boy aged 5 years from Kaloa, Hawaii – considered to be the superimposition of one serious disease on another. The authors note that “mucoviscidosis is so well established today that we seldom see individual case reports except in areas where interest in the disease is awakening (for example South Africa, Canada and Germany). Rather we look forward to monographs such as Bodian’s (1952 above) and May’s (May CD. Cystic fibrosis of the pancreas in infants and children. Springfield Ill: Charles C Thomas. Publisher, 1954 above) where accumulated experience is recorded”.
They note that in Bodian’s book Cedric Carter, the geneticist, combined the data from Andersen and Hodges, Lowe, May and Reed with his own to confirm the expected probability of 1 in 4 children being affected. The importance of di Sant’Agnese’s recent (1953) description of the sweat electrolyte abnormality is mentioned particularly its importance in the recognition of the 5 – 10% of people with CF without clinical pancreatic insufficiency – but the tryptic activity of duodenal juice was still of great importance in diagnosis. Shwachman describes their experience of inducing sweating in 300 children by placing the child in a plastic suit bag for 30-90 minutes with pieces of covered gauze on the back. Values of over 80 meq/l were considered diagnostic of cystic fibrosis.
The beneficial effect of controlling infection with antibiotics in contrast to the relatively unsuccessful attempts with various inhalations including trypsin and oral iodides was stressed – “early recognition of the disease and prompt antibiotic therapy may be so encouraging that parents as well as doctor begin to question the original diagnosis”!
Finally, Shwachman notes that the average age of death from 1940-48 was 12.8 months and from 1949-53 was 45.2 months – the broad spectrum antibiotics came into use in 1949 and were considered likely to be one of the reasons for the improvement.
This 74 page paper, with 142 references, is a very detailed review of the current knowledge of CF up to that time by Harry Shwachman, written with the assistance of Hugo Leubner of the WHO and Pincus Catzel, then a research fellow. It makes very interesting reading.
1955 Bille Bo SV, Vahlquist Bo. Idiopathic hypoproteinemia versus hypoproteinemia due to pancreatic dysfunction. Acta Paediatr 1955; 44:435-443. [PubMed]
Two siblings with hypoproteinemia and oedema, one aged four months, who rapidly improved on pancreatic replacement therapy, were considered to have cystic fibrosis. Twenty two reported cases of hypoproteinaemia and oedema were reviewed and the most constant finding was abnormal pancreatic function.
Charles May commented on the rarity of this complication in CF despite severe wasting. A child with this complication is more likely to have cor pulmonale or liver cirrhosis – this also applies to a child with CF. In Leeds our findings were similar; in a detailed assessments of over 600 children with CF, we found that hypoproteinaemia was unusual unless there was also significant liver involvement.
1955 di Sant’Agnese PA. Fibrocystic disease of the pancreas with normal or partial pancreatic function: current views on pathogenesis and diagnosis. Pediatrics 1955; 15:683-697.[PubMed]
Another early report of “pancreatic sufficient” patients i.e. defined as those who had sufficient remaining pancreatic function (probably around 10%) to achieve normal intestinal fat absorption without enzyme replacement therapy. On testing, six had partial pancreatic deficiency and 3 normal pancreatic function.
These patients provide further evidence that the secretory activity of many and perhaps all exocrine glands, mucus producing and others, is affected rather than the clinical manifestations being due primarily to pancreatic disease and secondary malnutrition e.g. vitamin A deficiency. (See also Gibbs et al, 1950 above; Shwachman et al, 1956 below).
1956 Dooley RR, Guilmette F, Leubner H. Patterson PR, Shwachman H, Weil C. Cystic fibrosis of the pancreas with varying degrees of pancreatic insufficiency. J Dis Child 1956; 92:347-368. [PubMed]
A further 17 patients and an estimate that some 10-15% of patients were “pancreatic sufficient” i.e. had sufficient residual exocrine pancreatic function to achieve normal fat absorption. Chest disease may develop before malabsorption occurs thus supporting the original hypothesis of Wolbach and Farber of a generalised disease if modified to include disturbance of sweat glands as an almost constant feature – in contrast to the belief that the problems were secondary to pancreatic malabsorption and malnutrition e.g. vitamin A or other deficiencies. Only one patient had a sweat test performed and that was positive – the sweat abnormality having only been described recently in 1953 (also Gibbs et al. 1950 above; Di Sant’Agnese, 1955 above).
1956 Nitowsky HM, Gordon HH, Tildon JT. Studies of tocopherol deficiency in infants and children IV. Effects of alpha tocopherol on creatinuria in patients with cystic fibrosis of the pancreas and biliary atresia. Bull Johns Hopkins Hosp 1956; 98:361-71. [PubMed]
There are numerous studies of vitamin E deficiency in CF as the vitamin is always very low in untreated and even in some treated but inadequately supplemented, patients. Five children with CF and two with biliary atresia had abnormal haemolysis of erythrocytes in hydrogen peroxide decreased by relatively large doses of intravenous or oral vitamin E. Creatinuria was decreased only in the CF children.
Fig. 21 Collection of sweat in a plastic bag tied loosely around the neck
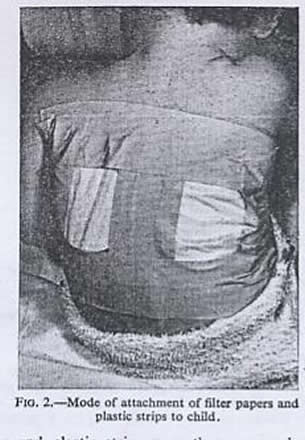
Fig. 22. Gauze applied to the back under plastic strips to collect the sweat. – Figures from Webb et al, 1956 with permission of BMJ Publishing Group
1956 Webb BW, Flute PT, Smith MJH. The electrolyte content of the sweat in fibrocystic disease of the pancreas. Arch Dis Child 1957; 32:82-84. [PubMed]
An early UK study from the Departments of Chemical Pathology and Paediatrics, Kings College Hospital, London – the first UK study since di Sant’ Agnese’s description of the sweat abnormality (di Sant’ Agnese et al, 1953 above). Twelve patients with CF, aged between 11 months and six years, and 20 controls had sweat electrolytes estimated which confirmed the findings of di Sant’Agnese et al, 1953. Controls had sweat sodium of 27 (4-32) meq/l and chloride of 23 (9-40) meq/l and the CF children sodium values of 125 (72-157) and chloride values of 127 (68-148) meq/l.
The patient was “placed in a plastic bag tied loosely around the neck (fig. 21) and allowed to lie in a cot or bed covered with three or four blankets. The sweat was collected on weighed filter papers which were applied to the back (figures 22). “In some instances the children were restive at first but quickly became used to the conditions”.
Subsequently there were a number of complications with this method of sweat testing in some hospitals, as a result of over-heating small debilitated CF infants in this manner, including at least one fatality (Misch & Holden, 1958 below).
Dr Bertie Webb
Dr Brian Wykeman Webb (1921-2017) was a distinguished and very popular English paediatrician, appointed in the year following this paper as the only consultant paediatrician in Somerset – a county containing some 60,000 children. He had a major influence on paediatric developments in the SW of England during the course of a very busy career. There are two obituaries on the internet which are both informative and one very amusing – written by the late Peter Dunn of Bristol, a friend and colleague who knew him well..
1956 Shwachman H, Gahm N. Studies in cystic fibrosis. Simple test for detection of excessive chloride on the skin. N Eng J Med 1956; 255:999-1001.[PubMed]
Due to the high level of chloride in the sweat, people with CF produce white fingerprints compared to a non-CF person on plates impregnated with silver nitrate and potassium chromate (figures 23 and 24). Dr Kulczycki (long time colleague of Harry Shwachman’s) performed 1443 control tests at an institution for the mentally handicapped.
The authors suggested “the plate test” as a screening test for CF but it never became popular. When the sweat test became more readily available in the early Sixties following the publication of Gibson and Cooke (1959 below), the result was so important that it was preferred to the semi-quantitative plate test. Subsequently Kulczycki (Am J Dis Child 1960; 100:174-180) screened 3036 school children with the plate test. There were 2% false positives on first test and no children with CF were identified. Authors suggested it would be better to use the test at an earlier age in well-baby clinics.

Fig. 23 Hand print of a non-CF child

Fig. 24 Print of a person with CF
Although the total heating of the child to induce sweating was obviously causing serious problems at times, the Gibson & Cooke iontophoresis method was soon to be reported in 1959. Subsequent screening tests using chloride electrodes, paper strips, salivary electrolytes, meconium albumin and faecal trypsin have all been relative failures with the exception of blood immunoreactive trypsin in neonates which has become internationally accepted as the basis of neonatal screening programmes (Crossley et al, 1979 above).
1956 Johnston W H. Salivary electrolytes in fibrocystic disease of the pancreas. Arch Dis Child 1956; 31: 477-480. [PubMed]
A study from Great Ormond Street Hospital in London showing elevated sodium and chloride in the stimulated saliva of 31 patients with CF compared with 63 controls. However the separation was not such that the test had diagnostic value and also the values depended on the rate of flow. Prader & Gautier (Helv Paediat Acta 1955; 10:56-62.[PubMed]) had found the saliva sodium was increased in cystic fibrosis. Unfortunately these various studies of the electrolyte content of CF saliva did not prove helpful in either the diagnosis or the understanding of the nature of the CF basic defect (also Lawson et al. 1956. below).
The studies were a natural follow-on from the recently described sweat electrolyte abnormalities – estimation of the electrolyte content of the finger nails was still to come ! (Kopito et al, 1965 below).
1956 Blanc WA, di Sant’Agnese PA. A distinctive type of biliary cirrhosis of the liver associated with cystic fibrosis of the pancreas: recognition through signs of portal hypertension. Pediatrics 1956; 18: 387-409.[PubMed]
Bodian (1952 above) recognised that foci of biliary fibrosis occurred commonly as a necropsy finding.

Fig. 25 Liver of a young person with CF removed by Prof. Geoff Giles at the time of liver transplantation in Leeds
Andersen (1938 above) reported three cases from the literature and one of her own where there was liver involvement. Here the progression of the early changes to a distinctive type of biliary cirrhosis (an example figure 19) accompanied by severe and at times fatal manifestations is reported. Seven patients, aged four to 10 years, are reported; three died; four had raised portal pressures. The absence of jaundice was noted and the lack of consistency of “so-called” liver function tests. An infective or nutritional insult to an already abnormal liver was suggested. In these young patients the condition was first recognised by the appearance of signs of portal hypertension. The authors correctly predicted that “it is possible that symptoms due to failure of liver function may appear subsequently after prolonged survival”.(also Webster et al, 1953 above; Craig et al, 1957 below; Mieles et al, 1989 below).
1956 Gibbs GE, Raskin J. Neomycin aerosol in the pulmonary complication of cystic fibrosis of the pancreas. Antibiot Med Clin Ther 1956; 2:332-336. [PubMed]
The first report of the use of inhaled neomycin in CF; eventually it was recognised as ototoxic and its use abandoned (Young, 1960 below).
1957 Fyfe W M. The stool proteolytic activity in the diagnosis of fibrocystic disease of the pancreas. Scot Med J 1957; 2:66 – 68. [PubMed]
Probably the first paper on CF from Scotland – Royal Hospital for Sick Children Glasgow – testing Shwachman’s earlier suggestion that measurement of stool proteolytic activity could replace duodenal intubation in the diagnosis of cystic fibrosis (Shwachman et al, 1949 above). Both duodenal and stool proteolytic activity were examined in 50 infants; 14 infants had absent proteolytic activity and were considered to have CF – confirmed at autopsy in eight. Fyfe concluded that liquefaction of the 1 ml of 7.5% gelatin by a 1:40 or higher dilution of stool was a reliable indication of normal duodenal proteolytic activity.
The author thanks Prof. Stanley Graham and Dr (later Prof) James Hutchinson for help and permission to study their cases – both were leading Scottish general paediatricians in the UK at the time.
1957 Hennequet A, Girault M, Debris P, Marie J. Anomalies of the sweat glands in mucoviscidosis or fibrocystic disease of the pancreas. Sem Hop 1957; 33:3130 – 38P [PubMed]
1957 Hennequet A, Girault M, Debris P, Marie J, Study of the sweat test for a method used in the analysis of total sweat. Sem Hop 1957; 33(56/10):3310-21P.[PubMed] These are early publications of Andre Hennequet of France on the subject of cystic fibrosis. Hennequet was heavily involved in CF and also published on a wide variety of subjects other than CF – unfortunately virtually always in a French publication. He was one of the few leading European paediatricians who met with Paul di Sant’Agnese when he visited Europe in 1960.
1957 MacFarlane JCW, Norman AP, Stroud CE. Fingerprint sweat test in fibrocystic disease of the pancreas. BMJ 1957; (5039):274-5. [PubMed]
The finger print test, devised by Shwachman & Gahm, 1956, (above) was tried in view of the difficulties, and even dangers, of collecting sweat by heating the whole patient, in the years before the Gibson and Cooke iontophoresis method was described in 1959. In fact, children were known to have died due to overheating in an attempt to obtain sweat (Misch & Holden, 1958 below).
The 54 children with CF in this study were all strongly positive with the finger print test. The authors suggested the test was useful and safe – but they considered it needed further evaluation. However, within 2 years the pilocarpine iontophoresis method of sweat stimulation of Gibson and Cooke (1959 below) would be described and this would become the standard method of sweat stimulation at the Hospital for Sick Children, London – although considerably more time-consuming and also open to serious errors if performed infrequently by an inexperienced operator as was later documented (Smalley et al, 1978 below).
Subsequently a study confirming the value of the Gibson and Cooke test was performed at the Great Ormond Street Hospital by Tom McKendrick, a Senior Registrar there at the time (McKendrick, 1962 below).
1957 Craig J, Haddad M, Shwachman H. The pathological changes in the liver in cystic fibrosis of the pancreas. Am J Dis Child 1957; 93:357-369. [PubMed]
Description of the typical CF liver changes by Blanc and Craig (Blanc & di Sant’Agnese, 1956 above).
1957 Gibson JB, Rodgers HW. Portal hypertension in fibrocystic disease of the pancreas. Arch Dis Child 1957; 32:355-358. [PubMed]
Good results from removal of a large spleen which reached the level of the umbilicus and weighed 710 g in a boy aged nine years. The liver showed marked fibrosis and the authors considered the liver changes were not likely to be due solely to the pancreatic damage, but suggest that focal obstruction of the bile ductules was the prime lesion – an explanation which proved to be correct. They considered the main danger from liver disease in this condition was portal hypertension.
Subsequent reports confirmed the benefit of splenectomy where the size of the organ was an embarrassment in terms of abdominal space even interfering with respiration and the descent of the diaphragm.
In 1988 a Leeds boy aged 16 years with CF had a massive spleen (3.2 kg) removed by the late Prof. Geoff Giles after which his FEV1 improved by 30% and he returned to normal sporting activities (Gilbert J, et al. Scand J Gastroenterol 1988; 23 Suppl 143:177).
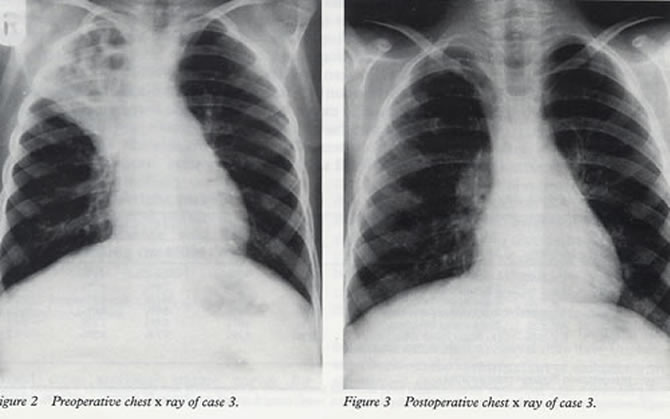
Fig. 26.A typical excellent result after resection of bronchiectatic right upper lobe. From Lucas et al, Arch Dis Child 1996; 74:449-45. With permission from BMJ Publishing Group
1957 Kulczycki LL, Craig JM, Shwachman H. Resection of pulmonary lesions associated with cystic fibrosis of the pancreas. N Eng J Med 1957; 257:203-208. [PubMed]
One of the first of many reports of the beneficial effect of resection of areas of major lung damage in CF (figure 26) – the first being the remarkable pneumonectomy reported in 1952 by Milton Lloyd (Lloyd & Robitzek, 1952 above). All the subsequent reports supported the removal of localised severely damaged areas of lung in people with CF (Mearns MB et al. Arch Dis Child 1972; 47:499-508. [PubMed] ; Feigelson J. Pulmonary resections in cystic fibrosis. Acta Paediatr Scand 1989; 78:317-318. [PubMed] ; Smith et al, J Pediatr Surg 1991; 26: 655-659 [PubMed] ; Marmon L, et al. J Pediatr Surg 1983; 18:811-815.[PubMed]; Lucas J et al. Arch Dis Child 1996; 74:449-451.
1957 di Sant’Agnese PA, Dische Z, Danilczenko A. Physicochemical difference of mucoproteins in duodenal fluid of patients with cystic fibrosis of the pancreas and controls. Pediatrics 1957; 19:252-260. [PubMed]
Mucopolysaccharides from duodenal contents had an abnormal physico-chemical behaviour and were easily denatured and rendered insoluble. Further studied by Dische Z et al (Pediatrics 1959; 24:74-91.[PubMed]) by fractional precipitation; considered possibly related to changes in distribution of sialic acid and fucose. There was a suggestion that the change in solubility of the muco-proteins may be in some way related to the obstruction in such organs as the pancreas.
1957 White R Jr, Dent JH, Derbes VJ. Asthmatic states caused by mucoviscidosis. J Louisiana St Med S 1957; 109:299-302. [PubMed]
Thirty eight of 66 children with CF from New Orleans had some degree of wheezing. The authors comment “It has been the common experience of mature pediatricians that administration of epinephrine in such circumstances has led to prompt, albeit transient, alleviation”. The mechanical factors that cause impairment of pulmonary function in asthma – bronchospastic contraction, edema of the mucous membrane and excessive secretion and retention of mucus, are present both in CF and asthma.
The authors’ wise message from their paper being – “it is the responsibility of all physicians who treat wheezing children to exclude this disorder (i.e. cystic fibrosis)”.
1957 Bishop HC, Koop CE. Management of meconium ileus, resection, Roux-en-Y anastomosis and ileostomy irrigation with pancreatic enzymes. Ann Surg 1957; 50:835-36. [PubMed]
This was a major surgical advance in the management of meconium ileus where mortality at the time was still over 50%. After resection of the most dilated portion of the ileum an end-to-side proximal-to-distal ileo-ileal roux-en-Y anastomosis is performed and the free end of the distal ileum brought out onto the abdominal wall as an Ileostomy (figure 27). The stoma acts as a safety valve and can be used to instil fluids, drugs or detergents.
Later the surgeons at the Queen Elizabeth Hospital, London reported an improvement in survival from 30% to 70% after adopting this procedure (McPartlin et al, Arch Dis Child 1972; 47:207-210).[PubMed]
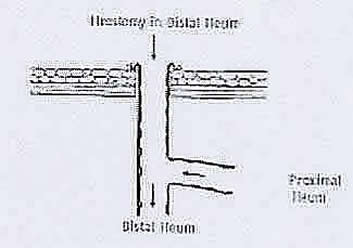
Fig. 27. Bishop Koop ileostomy
1958 Green MN, Clarke JT, Shwachman H. Studies in cystic fibrosis of the pancreas: protein pattern in meconium ileus. Pediatrics 1958: 21:635-641. [PubMed]
This study confirmed the presence of large amounts of protein in the meconium from patients with meconium ileus. The meconium of subsequent newborn siblings of known patients with CF was examined in a later study (Green & Shwachman, 1968 below).
1958 Shwachman H, Kulczycki LL. Long-term study of 105 cystic fibrosis patients. Am J Dis Child 1958; 96:6-15.[PubMed]

Harry Shwachman
This is a frequently-quoted paper of studies made over a five to fourteen year period after diagnosis –“survival beyond childhood is being noted with increasing frequency”. Ninety five patients were still living and 10 had died; 41 were over 10 years. Details of therapy are described and also the details of the Shwachman/Kulczycki clinical score which became the standard method of scoring a patients clinical condition. In the score equal weight given to the general activity, physical examination, nutritional status and X-ray chest. The authors emphasise “the value of pursuing a vigorous therapeutic programme in a disease which is still so little understood”. With regard to treatment, prior to 1948 sulphonamides, penicillin and streptomycin were the only agents available – the latter two used mainly for exacerbations. In September 1948 Aureomycin was used and very effective and Terramycin in early 1950 was equally effective. Chloramphenicol and erythromycin were used liberally since 1955 and novobiocin sparingly for one year. Wide spectrum agents in prophylactic dosage or in therapeutic dosage when pulmonary infection was well established. Complex mixtures of antibiotics, propylene glycol and detergents were used for short term inhalation therapy. A few patients were treated in mist tents at night. Patients received a liberal high protein diet with an effort to reduce the fat intake. All had pancreatin (Viokase) and vitamins.
These results were extraordinarily good for the time – certainly in most of the UK at this time there were only very exceptional patients who reached adolescence. There was no requirement for adult clinics as there were virtually no adults in most of the UK – the only clinic for adults with CF was at the Royal Brompton Hospital in London and this did not start until the mid-Sixties.
1958 Misch KA, Holden HM. Sweat test for diagnosis of fibrocystic disease of the pancreas. Arch Dis Child 1958; 33:179-180.[PubMed]
Fatal collapse of a patient having “Shwachman sweat test” which involved the whole body being enclosed in a plastic bag as a method of heating the patient to obtain an adequate sample of sweat. This boy aged 13 months was heated for 3 hours and developed hyperpyrexia, vomited copiously, became comatose and he died after 14 hours.
Shwachman commented that in his unit 1900 tests had been performed by the bag method with only one serious untoward reaction of hyperpyrexia and convulsions – the patient recovered and did not have cystic fibrosis. In the UK there were a number of serious reactions which never appeared in journals, before the Gibson & Cooke pilocarpine method of inducing sweating was described in 1959.
1958 Kulczycki LL, Shwachman H. Studies in cystic fibrosis of the pancreas: occurrence of rectal prolapse. N Eng J Med 1958; 259:409-412. [PubMed]

Fig. 28. Rectal prolapse in a young child.
Rectal prolapse (figure 28) occurred in 22.6% of 386 patients with CF. It appeared to be related to combination of steatorrhoea, poor musculature and chronic coughing. Most frequently between three and six years and more common when the diagnosis is made later. In 16 (4%) patients prolapse was the presenting sign and the authors advised that CF should be excluded in any child with a rectal prolapse.
In a later study Zempsky WT & Rosenstein (Am J Dis Child 1988;142:338-339. [PubMed]) found of 54 children seen for rectal prolapse over 10 years the causes were constipation in 15, acute diarrhoea 11, neurological abnormalities 13 and cystic fibrosis in only six children (11%).
– Rectal prolapse in patients with CF virtually always resolves after treatment with pancreatic enzymes. I only recall one adolescent girl, in over 600 patients, who reported occasional persisting problems with prolapse, although it is possible other older patients were reluctant to report that rectal prolapse was persisting.
1958 Blanc WA, Reid JD, Andersen DH. Avitaminosis E in cystic fibrosis of the pancreas: a morphologic study of gastrointestinal and striated muscle. Pediatrics 1958; 22: 494-506.[PubMed]
Ceroid pigment was present in the smooth muscle fibres of the gastrointestinal tract of patients with cystic fibrosis. It was first seen in those dying during the second year of life and present in all after 5 years of age, the amount increasing with age. The only other condition where this pigment is found is biliary atresia and cirrhosis. It was considered as probably due to prolonged and severe vitamin E deficiency. However, alterations in striated muscle are rare and minimal in CF but common in severe vitamin E deficiency (Martin AJP, Moore T. Some effects of prolonged vitamin E deficiency. J Hyg 1939; 39:643; Human occurrence in one case of CF by Pappenheimer AM, Victor J. Am J Path 1946; 22:395).
1958 Shwachman H, Fekete E, Kulczycki LL, Foley GE. Effect of long term antibiotic therapy in patients with cystic fibrosis of the pancreas. Antibiot Ann 1958-59; 692-699. [PubMed]

Fig. 29. Teeth stained by tetracycline.
An early (possibly the first) report of severe yellow discolouration of the teeth due to tetracycline (fig. 29) , an antibiotic which had become available between 1948-1950. Discolouration of the teeth was present in 80% of young children with CF receiving long term tetracycline prophylaxis; many subsequent reports have confirmed the problem (Zegarelli EV et al. Oral Surg Oral Med Oral Pathol 1962; 15:929-933; Appelbaum E et al ibid 1964; 17: 366-367; Witkop CJ, Wolf RO. JAMA 1963; 185:1008-1011). Tetracycline is deposited in growing bone by forming complexes with the bone mineral.
1958 Jones MD, Sakai H, Rogerson AG. Cholangiography in children with fibrocystic disease of the pancreas; a pilot study. J Pediatr 1958; 53:172-179.[PubMed]
Seventeen children with CF (aged 19 months to 11 years) had intravenous Cholografin and the bile ducts were visualised in 12; in 13 the gallbladder was opacified.
1958 Andersen DH. Cystic fibrosis of the pancreas. A review. J Chron Dis 1958; 7:58-90. [PubMed]

Fig. 30. Copy of original kindly sent to me by Archie Norman. 50 pages of text, 15 pages of the 231 references. No computers, copiers, printers or PubMed!!
A wide ranging and very comprehensive review of CF by Dorothy Andersen containing 231 references. A carbon copy of the original text was kindly given to me by Dr Archie Norman who I suspect reviewed the original paper. Before the days of PubMed, internet and photocopiers!
Andersen writes “From obscure origins as an esoteric disease, cystic fibrosis of the pancreas has in twenty years become one of the most intensively studied and widely discussed maladies in pediatrics”. The introduction sums up the situation at that time – “Cystic fibrosis of the pancreas can be defined as a congenital familial disease characterised by dysfunction of many of the exocrine glands. The most obvious effects are pancreatic deficiency with characteristic morphologic changes in that organ, susceptibility to chronic bronchitis, and a high concentration of electrolytes in the sweat. Other exocrine glands may give functional and morphological evidence of abnormality. The basic defect is unknown. Death occurs in infancy or childhood in the majority of cases”.
This paper provides a detailed review of CF up to the end of the Fifties, in particular, a very detailed review of the pathology. Andersen’s observation that “the disease has proved to be of varied expression requiring the informed attention of a number of branches of medicine including radiology, surgery, otolaryngology, obstetrics and internal medicine” has certainly proved to be correct – even more so as the average age of the CF population increases and more complications become apparent.
1958 di Sant’Agnese PA, Grossman H, Darling RC, Denning CR. Saliva, tears and duodenal contents in cystic fibrosis of the pancreas. Pediatrics 1958; 22:507-514. [PubMed]
Higher mean values of sodium and chloride but similar potassium levels were present in saliva of people with CF than in controls, as previous studies had shown. Also electrolytes were increased in the tears of people with CF but there was considerable overlap with normals in both tears and saliva. The concentrations of ions were similar in duodenal contents of CF and controls and not related to variations in proteolytic activity. At this stage di Sant’Agnese noted that three abnormalities in CF need explanation – an abnormality of mucus secretion, high electrolyte concentrations in sweat saliva and tears and an increased rate of secretion in parotid glands (also Lawson 1956 above; Barbero & Chernick, 1958 below).
1958 Barbero GJ, Chernick W. Function of the salivary gland in cystic fibrosis of the pancreas. Pediatrics 1958; 22: 945-952. [PubMed]
Children with CF had greater unstimulated salivary flow and the concentration of sodium and chloride was elevated compared with controls as had been shown by others. Response to mecholyl injection greater but potassium did not differ between CF and controls. This suggested an increased parasympathomimetic sensitivity in cystic fibrosis.
1959 Di Sant’Agnese PA, Andersen DH. Cystic fibrosis of the pancreas in young adults. Ann Intern Med 1959; 50:1321-1330.[PubMed]
A review article intended to bring CF to the attention of adult physicians. There are interesting statistics – between 1939 and 1958 there were 550 children with CF seen at the Babies Hospital, New York. One hundred and six survived beyond the age of 10 years, the oldest was aged 24 years and 85 were still alive. The authors mention abdominal masses in the right iliac fossa as being not infrequent; some explored surgically had proved to be of faecal in origin. Appendix abscesses, where the symptoms have been masked by antibiotics given for the chest, had been seen in two patients both of whom recovered – but “important to keep in mind”.
The authors conclude that “Cystic fibrosis is breaking out of the paediatric bounds to which it had been limited by its high mortality rate in infancy and childhood. It is now invading the domain of diseases of the adult individual.”
This paper has been quoted as containing first description of appendix abscesses in CF and the difficulties of their recognition in people with CF (also Holsclaw & Habboushe. J Pediatr Surg 1976; 11:217-221.[PubMed]).
1959 Lurie MH. Cystic fibrosis of the pancreas and the nasal mucosa. Ann Otol Rhinol Larygol 1959; 68:478-486. [PubMed]
An early description of nasal polyps (fig. 32) which are remarkably common in both children and adults with CF (6-48% in various series). In this paper three illustrative cases were described at an ENT meeting. (also Shwachman et al. 1962 below; Complete filling of the nasal sinuses was described by Pennington CL. AMA Arch Otolaryng 1956; 63:576. [PubMed]; Bodian describes changes in the sinuses, (1952 above).
Nasal polyposis may be the presenting feature of CF, the first evidence of CF being nasal polyps so large they are appearing at the external nares as occurred in one of our Leeds children.
Fig.32. Nasal polyps in cystic fibrosis
1959 Holman RL, Blanc WA, Andersen D. Decreased aortic atherosclerosis in cystic fibrosis of the pancreas. Pediatrics 1959; 24:34-39. [PubMed]
At autopsy 21 non-CF control patients had four times the incidence of aortic atheroma (average percentage of the intimal surface involved with fatty streaks) than did 18 patients with CF aged six to 13 years. The reasons were unknown and the authors did not think the simple explanation of fat malabsorption was the whole reason as other children dying from chronic malnutrition do not have this decreased incidence of atheroma. (also Moss TJ et al. J Pediatr 1979; 94:32-37. [PubMed])
1959 Gibson LE, Cooke RE. A test for concentration of electrolytes in sweat in cystic fibrosis of the pancreas utilising pilocarpine electrophoresis. Pediatrics 1959; 23:545-549.[PubMed]
This classic paper described the pilocarpine iontophoresis method for stimulating sweating to obtain sweat for analysis. It was a major advance, as prior to this these frail infants were often heated in blankets or plastic bags. The pilocarpine iontophoresis method is still used by most laboratories for stimulating localised sweating (fig. 33).
Dr Lewis E Gibson (1928-2008) was a paediatrician and researcher who developed the pilocarpine iontphoresis sweat test after he moved to the NIH in 1955. He recalls seeing his physiology teacher raising a hive on his own arm by iontophoresing histamine into the skin with an electric current. The difficulties in obtaining sweat by heating (“a few babies had died in sweat bags”) stimulated his further interest in iontphoresis of pilocarpine to stimulate sweating. in 1957 Gibson returned to Johns Hopkins where the Chairman of Pediatrics, Dr Robert E Cooke, had worked with CF and had some experience of iontophoresis. They combined on the present publication which apparently became a Current Contents classic. There is an interesting chapter by Dr Gibson in Dr Carl Doeshuk’s book (Cystic Fibrosis in the 20th Century. Ed. Doershuk CF. AM Publishing Ltd Cleveland, Ohio. 2002).

Fig. 33. Electrodes applied to infant’s forearm as pilocarpine is iontophoresed painlessly into the skin; later the sweat is collected from the treated area on weighed gauze and the weight and electrolyte content estimated in the laboratory. Most importantly, an experienced biochemist (here Dr Shapiro at St James University Hospital in Leeds) is carrying out the procedure.
Fig. 34. Robert E Cooke. Portrait by Larry Wheeler from Medical Archives of The Johns Hopkins Medical Institutions
Dr Robert E Cooke (fig. 34) was Chairman of the Department of Pediatrics at Johns Hopkins from 1956 to 1973 and involved many areas of paediatrics and child health other than CF on both a local and national level including programmes that brought better care to inner city mothers and their children, the Kennedy Program for Research into the Etiology of Mental Retardation and eventually as Director of the Kennedy Institute for Handicapped Children.
Subsequently, as more laboratories performed the test caution was expressed as when performed by inexperienced operators mistakes occurred. These mistakes often resulted in CF being over diagnosed when the sweat result was falsely high which could happen if the sweat specimen was allowed to evaporate. Also, there were reports of burns under the electrodes. The first report of such major diagnostic errors in the UK was from Birmingham (Smalley et al, Lancet 1978; ii: 415-417 below) from Prof. Charlotte Anderson’s unit but soon others followed (David TJ & Phillips BM. Lancet 1982; ii: 1204-1205. [PubMed] ).
In Leeds we found that 7 (4%) of the first 179 children referred for Comprehensive Assessment of their CF from various parts of the UK did not have the condition (Shaw NJ & Littlewood JM. Arch Dis Child 1987; 62:1271-1273. [PubMed]). The consequences of a false diagnosis of CF frequently had disastrous socio-medical consequences e.g. one mother had been sterilised to avoid having another child with CF as it was mistakenly thought her first child had CF. Many parents had avoided having further children; some parents took legal action against the paediatrician involved in the mistaken diagnosis.
So the sweat test is an excellent test if carried out correctly by experienced laboratory staff but can be disastrous if performed by inexperienced staff as an occasional procedure. Also the result should not be accepted uncritically by the paediatrician and should be considered with all the other clinical and laboratory evidence when making a diagnosis of cystic fibrosis. In recent years the diagnosis in the majority of people with CF can, and should, be confirmed by determining their CF mutations. A report of the oedema and hypoproteinaemia in an infant with CF (also Lee PA et al, JAMA 1974;228:585-588.; Gunn T et al, Am J Dis Child 1978;132:317-318. below). Also infants with CF presenting in this manner may have a false negative sweat test.
Fig. 34. Donna and Doug Summerhayes. From Candid Facts. Summer/Fall 2013.
1959 CANADIAN CYSTIC FIBROSIS FOUNDATION FORMED
Cystic Fibrosis Canada originated in the late 1950s, with an historic meeting of concerned and anxious parents at the Hospital for Sick Children in Toronto organised by Douglas and Donna Summerhayes (fig. 34) following the diagnosis of their daughter Pamela. They attended the International Research Conference in Washington in 1959 where they met Dr Wynne Sharples, a socially and politically well-connected paediatrician who had two children with CF. She had led the formation of the National Cystic Fibrosis Research Foundation in the USA and offered the Summerhayes great support during the early years of the Canadian Foundation. Douglas Summerhayes became the first President, Donna the first secretary and Robert (Bob) Ivey the first treasurer. The Summerhayes produced the first newsletter at their kitchen tables – Candid Facts; it was printed on Bob Ivey’s press and mailed out at his expense.
Candid Facts now reaches tens of thousands of people on Line (www.cystic fibrosis.ca) and through email. The Summerhayes were awarded the Order of Canada for their efforts in establishing what is now known as Cystic Fibrosis Canada.
The months that followed these early meetings were hectic, but productive. By the early 1960s the original Board of Directors had drafted by-laws for the Foundation and its Chapters, and had moved to create a strong medical committee. At first they met with obstacles for obtaining federal status. But their persistence paid off, and on July 15, 1960, the Canadian Cystic Fibrosis Foundation was incorporated by Federal Letters Patent.

Fig. 35. Cathleen Morrison. The previous Chief Executive Officer of the Canadian CF Foundation. From www.cysticfibrosis.ca
Cathleen Morrison (fig. 35) the previous CEO has written an interesting account of the formation of the various CF Associations (Morrison C, Morrison R. national and International Cystic Fibrosis Associations. In Cystic Fibrosis – Current Topics. Dodge JA, Brock DJH, Widdicombe JH (eds). John Wiley & Sons. Chichester 1993, 319-346). Cathleen was appointed CEO of the CCFA in 1980 and retired in 2010.
I am grateful to the Donna and Doug Summerhayes’s daughter Heather Cariou for information relating to these early years, described in her acclaimed book “Sixty Five Roses: A Sister’s Memoir” for which Celine Dione wrote the forward.
1959 Gandevia B, Anderson CM. The effect of bronchodilator aerosol on ventilatory capacity in fibrocystic disease of the pancreas. Arch Dis Child 1959; 34:511-515. [PubMed]
An early report, from the Royal Children’s Hospital Melbourne, of the favourable effect of bronchodilators in some people with cystic fibrosis. A 1/1000 solution of isoprenaline was used for its potency and rapidity of action. One third of 16 children with CF showed impressive improvement in their respiratory function tests after the bronchodilator, most marked in the moderately affected group rather than the severely or mildly affected patients. The authors note that there are only two previous references to bronchodilator therapy in CF – West et al, 1954 (above) who found no improvement in six patients during their early respiratory function studies and Royce 1956 (above) who noted improvement in one child. White et al, 1957 (above) reported some degree of wheezing in 38 of 66 children with CF which was relieved by epinephrine. Subsequently Landau & Phelan measured the maximum expiratory flow volumes and cautioned on the use of bronchodilators as they may impair respiratory function (Landau & Phelan. Pediatr 1973; 82:863, below).
Note this present paper is by Charlotte Anderson – at the time a paediatrician from Melbourne, Australia where she started the CF clinic. She eventually was appointed Professor of Paediatrics in Birmingham, UK (not Dorothy Andersen the pathologist from New York who described the disease in 1938 – above).
1959 Douglas WAC. Acute salt depletion in fibrocystic disease of the pancreas. Med J Australia 1959; 46:962-963.[PubMed]
The Australian climate provides the requisite conditions for acute salt depletion but up to this time no cases of this complication in people with CF had been reported from there. These are the first two children to be reported from Queensland – a girl aged four years who quickly recovered with intravenous (IV) fluids and a girl aged 10 months admitted in a collapsed state but who also recovered with IV fluids. Climate temperature was over 100°F in both instances. Both were discharged on a 4 g salt supplement daily. “The association of pink lips with peripheral circulatory collapse is most unusual” – a sign also noted by Rendle-Short (1956 above). The normal daily sodium chloride requirement is approximately half a gramme per year of age per day up to a total of 5 grammes (4 grammes= a level teaspoonful). In warm conditions this daily salt supplement is recommended.
Recently it has been suggested that using the current UK guidelines many cases of sodium depletion may be overlooked. Some infants require more than the recommended 1-2 mmol/kg/day. The urine sodium:creatinine ratio is a useful non-invasive measure to monitor sodium depletion (Coates AJ et al. 2009; 8:382-385. [PubMed]).
Fig. 36. Barbara Doyle. From Doyle B, 1959
1959 Doyle B. Physical therapy in treatment of cystic fibrosis. Phys Therapy Rev 1959; 39:24 – 27. (Prepared under the direction of Harry Shwachman). [PubMed]
An early report of physical therapy for the chest in cystic fibrosis. Shwachman mentions that active physical therapy was instituted in his clinic in 1957 and considers it to be one of the more important introductions into the treatment regimen. Barbara Doyle (figure) was a physical therapist from Eire who received her physical therapy preparation at Dublin School of Physiotherapy and was a member of the Chartered Physiotherapy Society of Great Britain. From 1956-1958 she was an exchange visitor in the United States and worked at the Children’s Medical Center, Boston. She used the so-called “English” methods (Reid JMW in Physiotherapy for Chest Diseases. In Marshall G, Perry KMA. (Eds.) Diseases of the Chest. St Louis: Butterworth & Company. 1952; 2:395-413). This report describes the current physiotherapy treatment for people with CF as done in Shwachman’s clinic in Boston and based on the experience with various chest conditions at the Hospital for Sick Children, Great Ormond Street, London
Louise Lannefors (fig. 37) of the Lund CF Centre, Sweden and physiotherapists Brenda Button and Maggie Mcllwaine published an excellent review of CF physiotherapy (Lannefors L et al. (J R Soc Med 2004; 97 (Suppl 44):8-25.[PubMed]Full text available).
They note the first reference to the use of postural drainage was by Ewart in 1901 (Ewart W. Lancet 1901; ii: 70) who referred to it as “empty bronchus treatment by posture in bronchiectasis of children”. Although few children with CF would have survived infancy at that time, bronchiectasis as an after effect of pneumococcal pneumonia, whooping cough or measles was relatively common in the pre-antibiotic era. Ewart advocated continuous drainage for hours at a time with the patient sleeping in the various positions. Later the detailed anatomy of the various lobes was described (Nelson HP. BMJ 1934; 11:251-255) and in 1949 the nomenclature of the anatomy was agreed (Anonymous. Nomenclature of broncho-pulmonary anatomy; an international nomenclature accepted by the Thoracic Society. Thorax 1950; 5: 222-228).

Fig. 37 Louise Lannefors.
1959 di Sant’Agnese PA. Recent observations on the pathogenesis of cystic fibrosis of the pancreas. Pediatrics 1959; 24: 313-321. [PubMed]
An interesting review, by a leader in the field, on the possibilities – a deficiency in function of the autonomic nervous system (also mentioned by Shwachman as a possibility and obviously popular at the time), an absence of an enzyme or some other metabolic error or according to Cooke RE & Gochberg SH “a shortage of energy for secretory activity” (Pediatrics 1956; 18:701-15. ). The author noted that the recognition of many variations in the clinical picture had been possible since the sweat tests became available after 1953. More than 550 patients had attended the Babies Hospital in New York since 1939 and only 9 (2%) had liver cirrhosis and these occurred in recent years as the age increased. Of 213 patients seen in last 5 years 34 (16.4%) had only reduced or normal pancreatic activity. The proportion of patients who are “pancreatic sufficient” varies between 5% and 15% in various reports – in part, the variation will be related to the gene mutations present in the population described.
1959 Chernick WS, Barbero GJ. Composition of tracheobronchial secretions in cystic fibrosis of the pancreas and bronchiectasis. Pediatrics 1959; 24:739-45. [PubMed]
The first of a number of studies in CF examining the composition of secretions in the airways although airway secretions had been studied in other conditions – the authors reviewed the literature. CF secretions, obtained via a bronchoscope, contained twice the organic material found in non-CF bronchiectasis and this was related to their increased viscosity. The amounts of nitrogen, carbohydrate, hexosamine and lipids were similar but the DNA content was higher. “The fluid component is related to the percentage of sodium and chloride ions in the secretions – the lowest levels being in the CF secretions”.
These are very pertinent observations in view of the present “low salt” theory caused by the excessive absorption of sodium and reduced secretion of chloride into the airways as a result of defective or absent CFTR. The depletion of the airway surface liquid is now regarded as being of major importance in the pathogenesis of the lung disease. These authors with a very accurate prediction prophetically observed at the end of their paper – “an alteration in the ionic concentration may be responsible for the peculiar characteristics observed in the tracheobronchial secretions of patients with cystic fibrosis”!! Also the increased amount of DNA present in CF sputum was relevant when the effect of enzymes was investigated (Chernick et al, 1961 below) – eventually leading to the development of the most effective mucolytic rhDNase in the Nineties.
1959 Hsia DY. Birth weight in cystic fibrosis of the pancreas. Ann Hum Genet 1959; 23:289-299. [PubMed]
The mean birth weight of CF infants of 2.9kg was below that for the USA which was 3.3 kg. It was suggested that this was due to the “intrauterine insult” of the condition. John Lloyd-Still found a similar reduction in the birth weight of CF infants (Pediatrics 1974; 54:306-311). Margaret Mearns found the mean birth weight of her 257 patients to be 3.18kg boys and 3.04kg for girls – below the 3.37 and 3.25kg for unaffected infants (In Hodson et al.(eds.) Cystic Fibrosis. Bailliere Tindall, London 1983;183-196). This was not evident in Leeds screened infants with CF whose mean birth weight of 3.3 kg was similar to that of the general local North of England population (Simmonds EJ et al. A review of infant feeding practices at a regional cystic fibrosis unit. J Hum Nutr Diet 1994; 7:31-38). Also Holliday K& Allen J found the birth weights to be normal (J Pediatr 1991; 118:77-79). However, a more recent report, in addition to noting that CF infants had a significantly lower length (-1.24SD) and weight (-0.72 SD) than normal, also noted they had a smaller head circumference (-1.82 SD) than controls. However, this series was from Sheffield Children’s Hospital and contained 34.6% who had meconium ileus, for which the hospital was a referral centre. Meconium ileus may have been associated with poor intrauterine growth for which there is some evidence (Ghosal S et al. Arch Dis Child 1996; 75:191-193.[PubMed]). For example in Toronto, 158 patients with meconium ileus had lower birth weight (3026 +/- 610 gm) than patients with no meconium ileus (3169 +/- 534 gm; p< 0.008) (Kerem E, et al. J Pediatr 1989; 114:767-73. [PubMed]).
1959 Cook CD, Helliesen PJ, Kulczycki L, Barrie H, Freidlander L, Agathon S, Harris GB, Shwachman H. Studies of respiratory physiology in children. II. Lung volumes and mechanics of respiration in 64 patients with cystic fibrosis of the pancreas. Pediatrics 1959; 24:181-193.[PubMed]
Detailed respiratory function on 64 patients aged 6 to 25 years. (Previous reports of West et al, 1954 above and Royce et al, 1958 are mentioned). Tidal volume and respiratory rate were abnormal in only the worst affected patients. The most frequent finding was an increased residual volume (46%) and functional residual capacity (21%). Vital capacity was reduced in 34%. The RV/TLC ratio was increased in 70% (figure). There was a definite correlation between respiratory function tests and clinical condition of the patients.
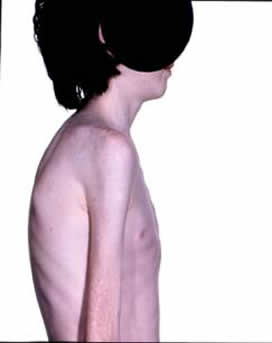
Fig. 38. A young man with CF showing the typical appearance associated with pulmonary involvement – an over inflated chest, severe kyphosis and very poor nutritional state typical of CF at the time.
1959 Roberts GB. Fundamental defect in fibrocystic disease of the pancreas. Lancet 1959; ii: 964. [PubMed]
A suggestion that autonomic abnormality could be related to the basic defect. Subsequently this was investigated and the suggestion supported by others (Mitchell I, et al. J Pediatr 1978;744-748.[PubMed]; Davis PB et al. Pediatr Res 1978; 12:703-707.[PubMed] ; Rubin et al, J Pediatr 1963; 63:1120). Autonomic abnormalities have been the subject of a recent review (Mirakhur A. Walshaw MJ. Autonomic dysfunction in cystic fibrosis. J R Soc Med 2003; 96 Suppl 43:11-17. .[PubMed]) although the findings have had no practical application in the treatment of the patients
1959 Grove SS. Fibrocystic disease of the pancreas in the Bantu. S Afr J Lab Clin Med 1959; 5: 113-119. [PubMed]
The first report from Durban of CF in a Bantu infant who died on the first day of life with meconium ileus. Detailed autopsy confirmed classical histological changes of CF in many organs including typical pancreatic changes. The author speculates that many Bantu children die of respiratory illness either before or soon after medical advice is sought. He hoped that knowing that the condition occurred in the Bantu would raise awareness of the condition. After submitting the paper a further infant with CF was seen by the author with typical pathological changes.
1959 Wright BM, McKerrow CB. Maximum expiratory flow rate as a measure of ventilatory capacity – with a description of a new portable instrument for measuring it. Brit Med J 1959; 2:1041-1947. [PubMed]
Basil Martin Wright (1912-2001) was a British bioengineer who invented several notable medical instruments, including the peak flow meter and syringe driver. The “alcolmeter” he developed won a Queen’s Award for Industry and is the breathalyser most often used at the road-side in the United Kingdom.
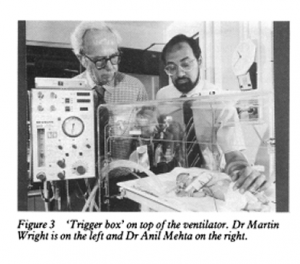
Fig. 39. Martin Wright. Tribute from the Independent (16.3.2001) to the inventor of the Wright Respirometer, Peak Flow Meter and numerous other devices used around the world
Writing about this original paper later in 1981 Dr Martin Wright (1912-2001) (fig. 39 ) says “I think the paper has been cited so much because it describes a test and an instrument which are practical and useful. In those days there was also room to put in a decent historical review and quite a bit of useful discussion and useful detail. Some years ago I noticed that although the peak flow meter (PFM) was mentioned and as often the key to the whole work, there was no longer any reference to our paper. It was evidently assumed that the PFM had been created by God. I have never got any award or honour but the Minimeter, a sort of paperback version (Wright B M. BMJ 1978; 2:1627-1628. [PubMed] ), got a design award and is selling hundreds of thousands because it can be used by patients at home. My reward is knowing that I have made a substantial contribution to clinical medicine”.

Fig. 40. Wright’s Peak Flow Meter – first model introduced in 1959.
This reviewer remembers the first Wright Peak Flow Meter (fig. 40) being purchased for our ward in the early Sixties and it was undoubtedly a major advance allowing useful repeated measurements of the patient’s respiratory function at any time and anywhere without the use of a large spirometer. Standard values of peak flow rates soon became available for adults and children.

Fig. 41 Minimeter peak flow meter.
Subsequently the advent of the Minimeter (Fig. 41) allowed patients to use it in the home and chart their own respiratory function. This was a major step forward in the management of both asthma, cystic fibrosis and other respiratory conditions.
Dr Wright says that “physiologists were a bit sniffy about the PFM holding that the proper way to measure flow is by volume and time but Colin McKerrow and Margery McDermott kindly did a very thorough calibration study”. Academic respiratory paediatricians remained, “a bit sniffy” about the peak flow meter but we paediatricians and the parents found the peak flow meters of immense value in practical management of both children with CF and asthma.


