Bronchoscopy
Introduction
Flexible bronchoscopy is a useful technique to obtain lower airway specimens from children who are unable to expectorate (Brownlee & Crabbe, 1997). Pathogens may be found in bronchoalveolar lavage (BAL) fluid that were not present on cough swab specimens (Armstrong et al, 1996). However, we do not recommend either frequent or regular bronchoscope examinations because for the majority of children a general anaesthetic is required and we are concerned that even minor trauma to the airway epithelium caused by the scope may increase susceptibility to chronic airway infection.
Bronchoscopy is reserved for:
i. Patients who have new or increased symptoms or signs of infection, who have no identifiable pathogens on induced cough swab or sputum specimens and who have not responded to oral and intravenous antibiotic treatments
ii. Atypical mycobacteria cannot be detected from cough swab specimens, so if this infection is suspected on the basis of symptoms or chest x-ray (CXR) changes in a child who is unable to expectorate, a bronchoscopy and BAL are performed
iii. Immunocompromised children with CF following transplant or immunosuppressive therapy who develop respiratory symptoms or signs or CXR changes should have early bronchoscopy to exclude atypical infection
iv. Lobar or segmental collapse in children with CF requires rapid and intensive investigation and treatment. Bronchoscopy and lavage is recommended at an early stage to obtain samples for microbiology, to remove mucus plugging and exclude unsuspected foreign bodies. Collapse can be persistent but full reinflation of affected lobes can occur after repeated bronchoscopy, even several months after the initial collapse (see figure 1)
The role of bronchoscopy in adults with cystic fibrosis
Bronchoscopy is not often carried out in adult patients with CF. However there are certain situations where the procedure can provide additional diagnostic information:
i. Identification of atypical infections
ii. Monitoring rejection post lung transplant (taking tissue samples and washings)
iii. Identification of localised bleeding (but not massive haemoptysis)
iv. Clearance of secretions in lobar or segmental collapse with direct instillation of rhDNase into the affected airways, e.g. with complications of ABPA (figure 2)
v. Tissue biopsy in cases of atypical lung disease e.g. cryptogenic organizing pneumonia
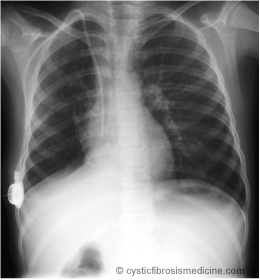
Figure 1a: Right lower lobe collapse

Figure 1b: Reinflated after sequential bronchoscopies and antifungal treatment
Figure 2a: Right upper lobe collapse t
Figure 2b: Reinflated after sequential bronchial lavage, steroids and antifungal treatment.
The procedure
In adult patients bronchoscopy is carried out using a thin flexible fibreoptic bronchoscope (the diameter of a pen). Following consent, the throat is numbed with a fine spray of local anaesthetic. This also prevents the gag reflex. A small amount of anaesthetic gel is inserted into the nose. A sedative called midazolam is administered intravenously to make the patient feel sleepy.
The bronchoscope is passed either through the nose or mouth down to the back of the throat. Further local anaesthetic is sprayed onto the vocal cords through the bronchoscope. The scope is then passed into the main trachea (windpipe) and bronchi (figure 3).
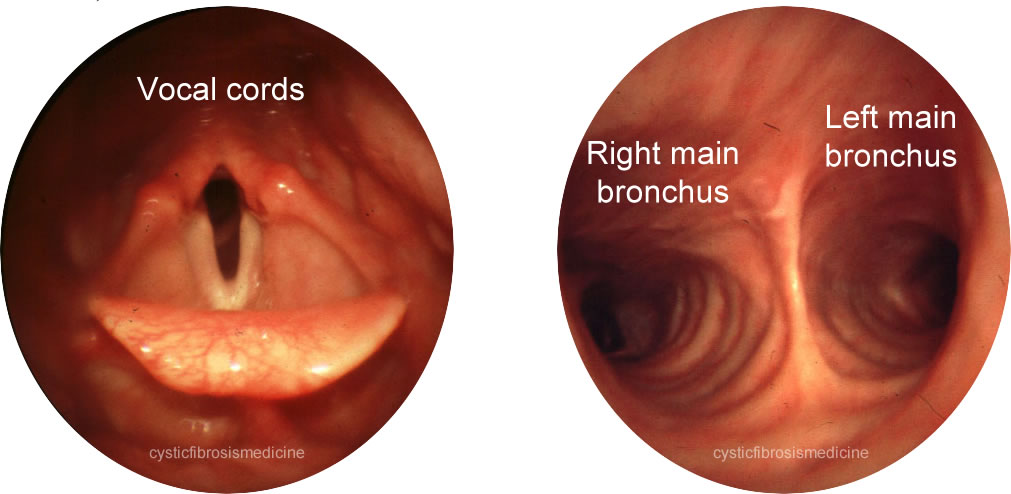
Figure 3. Bronchoscopy view
How long does it take and will it hurt?
A bronchoscopy usually only takes 10-30 minutes and is not painful. A full explanation of the procedure and related complications will always be discussed prior to consent.
Bronchoalveolar lavage (BAL)
Samples can be taken from the alveolar and bronchial airspaces by wedging the scope into a bronchus and flushing the airways with sterile 0.9% saline. Samples are then aspirated via the scope and collected for examination.
Key points
• Flexible bronchoscopy is a useful technique to obtain lower airway specimens from children who are unable to expectorate and adults where atypical infection is thought likely
• Most children will require a general anaesthetic
• Bronchoscopy should only be performed when specific criteria have been met
• Bronchoscopy is often used to monitor rejection post lung transplant
• Bronchoscopy and lavage is recommended at an early stage to obtain samples for microbiology, to remove mucus plugging and exclude unsuspected foreign bodies
• Sequential bronchoscopy to remove mucus plugging in lobar or segmental collapse can prove effective when cobined with medical therapy
References
Armstrong DS, Grimwood K, Carlin JB, et al. Bronchoalveolar lavage or oropharyngeal cultures to identify lower respiratory pathogens in infants with cystic fibrosis. Pediatr Pulmonol 1996; 21: 267-275. [PubMed]
Brownlee KG, Crabbe DCG. Paediatric bronchoscopy. Arch Dis Child 1997; 77: 272-275. [PubMed]
