Eighties science
Eighties -science
The Eighties was a remarkable time for both CF research and clinical care.
At the start of the decade scientists knew very little about the CF gene save for the fact it was not on one of the sex chromosomes; yet by 1985 the gene was localised to chromosome 7 and finally identified in 1989. In the early Eighties it was known that there was some problem with ion transport at cell membranes but it was not clear if this was an intrinsic abnormality of the membrane or some alteration of the function of a normal membrane caused by a circulating substance – perhaps one of the many so-called “CF factors” that had been studied so extensively during the previous decade.
In 1980, at the 8th International CF Congress in Toronto, there was a poster suggesting that abnormal epithelial electrolyte transport may reflect the primary defect – “the existence of an extraordinarily active sodium absorption could explain some of the clinical findings of CF e.g. hyper viscous mucus as being caused by excessive absorption of NaCl and water” (Hopfer et al, 1980 below). Eventually regulation of sodium absorption as well as chloride transport was identified as one of the important functions of the gene product – cystic fibrosis transmembrane regulator (CFTR), malfunction of which results in excessive viscosity of the airway secretions.
In 1981, Michael Knowles, Richard Boucher and colleagues, from the University of North Carolina, USA, demonstrated an abnormally high potential difference in the nasal mucosa of patients with CF thus providing more direct evidence of epithelial dysfunction (Knowles et al, 1981 below). There was a defect in the ability of chloride to move across CF cells, chloride permeability was not activated by beta-agonists (as it is in non-CF subjects) and there was an excessively rapid absorption of sodium. The abnormality was also present in newborns with CF indicating a primary abnormality rather being secondary to circulating CF factors or other substances.
In 1983 Paul Quinton, who himself has CF, showed that the chloride impermeability he had demonstrated in sweat glands was the basis for the raised sweat electrolytes in patients with cystic fibrosis (Quinton, 1983 below). These were the most important advances to date in understanding the basic defect as a membrane electrolyte transport problem since the discovery of the abnormal salt content of the sweat by Paul di Sant’Agnese in 1953.
From the early Eighties various research groups, including Professor Bob Williamson’s at St Mary’s Hospital in London, attempted to identify the CF gene by using ‘reverse genetics’, as the protein was unknown. They studied families with more than one affected child and in 1985 with this technique Hans Eiberg and co-workers, in Copenhagen, demonstrated a linkage between a liver enzyme marker paraoxinase, which exists in two forms but was present in the same form in 90% of CF siblings (Eiberg et al, 1985 below). In the same year, Professor Lap Chi Tsui from Toronto, in conjunction with Collaborative Research Inc. in Boston, in a series of mouse hybrid experiments, demonstrated a marker on chromosome 7 linked to both paraoxinase and cystic fibrosis (Tsui et al, 1985 below). Two other markers, known to be on chromosome 7, were closely linked to CF, the Met oncogenes, Met H and Met D reported by Dr Ray White in Salt Lake City (White et al, 1985) and the DNA probe pJ3.11 from Bob Williamson’s laboratory in London (Wainwright et al, 1985 below). These important findings were published in the same edition of Nature on the 29th November 1985.
In 1989 the CF gene was eventually identified by teams headed by Professor Lap-Chi Tsui, Dr Francis Collins and Professor Jack Riordan and termed the cystic fibrosis transmembrane conductance regulator (Kerem et al, 1989; Rommens et al, 1989; Riordan et al, 1989 all below). These workers were awarded the Paul di Sant’Agnese Prize of the CF Foundation at a memorable ceremony at the 1989 North American CF Conference. Although not the first to identify the gene Bob Williamson and his team at St Mary’s Hospital in London made a major contribution to the eventual identification of the gene by their work during the Eighties.
Publications during the Eighties in chronological order
1980 Katz S, Ansah TA. (Mg 2++ Ca 2+)-ATPase activity in plasma membrane enriched preparations of human skin fibroblasts: decreased activity in fibroblasts derived from cystic fibrosis patients. Clin Chim Acta 1980; 100:245-252. [PubMed]
There were ATPase differences between normals and CF plasma membrane enriched preparations obtained from cultured human skin fibroblasts. The (Mg2+ + Ca2+)-ATPase activity of both crude and plasma membrane enriched preparations of cultured fibroblasts from CF patients was significantly reduced compared to controls. The authors noted that this study corroborated their previous observations made in crude homogenate preparations of CF fibroblasts and indicated yet another cell type where (Mg2+ + Ca2+)-ATPase activity may be altered in cystic fibrosis.
1980 Manson JC, Brock DJH. Development of a quantitative immunoassay for the cystic fibrosis gene. Lancet 1980; i: 330-331. [PubMed]
Further work from Edinburgh pursuing the elusive “CF Factor”. An antiserum raised in guinea pigs to the CF factor showed positive immuno-electrophoretic reaction with sera from 16 of 17 patients with CF, eight of nine obligate heterozygotes, but only one of 15 normal subjects. The antiserum appeared to be specific to the CF protein described by Wilson and colleagues (1973; 1976; 1977 above). Precipitin peaks were larger with sera from CF homozygotes than from heterozygotes, suggesting the possibility of a new quantitative biochemical assay for cystic fibrosis.
Later David Brock’s group achieved 94% identification of sera from patients, heterozygotes and controls and regarded this as the best they could achieve in the present state of knowledge (Bullock S. et al. Quantitative immunoassays for diagnosis and carrier detection in cystic fibrosis. Clin Genet. 1982; 21:336-341).[PubMed]
1980 Davis PB, Shelhamer JR, Kaliner M. Abnormal adrenergic and cholinergic sensitivity in cystic fibrosis. N Eng J Med 1980; 302:1453-1456. [PubMed]

Fig 1. Pamela Davis
The authors noted “abnormal responses to all these agents and conclude that there is a lesion in cystic fibrosis at or beyond the level of the autonomic receptors”. Pam Davis also suggested, somewhat prophetically, that the defect may be symptomatic of a more generalised membrane dysfunction (Davis and di Sant’Agnese Pediat Res 1980; 14:83-78) – remembering this was the year before Dr Michael Knowles demonstrated the membrane electrolyte transport abnormality (Knowles et al, 1981 below).
There had been previous suggestions that there was an abnormality of the autonomic nervous system including the finding of abnormal pupillary reactions (Rubin L S et al, 1963 above), abnormal finger skin wrinkling in water (Elliott RB, 1974 above) and even that changes of CF in the pancreas may cause a state of “autonomic dyskinesia” causing more or less persistent bronchospasm and bronchorrhoea reflex abnormal pulmonary function from the pancreatic abnormality (Ayers WB et al. 1951 above). There is a later detailed review of the autonomic manifestations (Mirakhur A, Walshaw MJ. J R Soc Med 2003; 96:11-17. below).
Dr Pamela Davis (fig. 1) has been a leader in CF care and research since she trained with Dr Paul di Sant’Agnese with whom she combined in many studies. She has remained in the vanguard of CF patient clinical care and scientific research since the time of her first publications with Paul di Sant’Agnese in the Seventies. Her appointment as Professor of Pediatrics, Medicine, Physiology & Biophysics and Microbiology & Molecular Biology at Case Western Reserve University School of Medicine, Cleveland Ohio, gives some indication of the breadth of her interests.
Her views are summarised in her chapter on Patient Care and Research in Carl Doershuk’s book (Doershuk 2001 below) – “We cannot let patients pass some figurative “point of no return” because of insurance pressure or complacency. Vigorous prosecution of conventional treatment should be the order of the day. Just as we cannot let up on research to develop cures of tomorrow, so too we cannot neglect the meticulous care of the patient today”.
Pamela Davis considers “gene therapy still offers the best opportunity to “cure” patients with CF….it seems to me that it is likely in the next five years that nontoxic gene therapy approaches will come to clinical trial that will impact on the electrophysiology of the airway epithelium, demonstrate gene transfer unequivocally, and correct some of the downstream manifestations of CF in the airways. It may require additional effort and time to produce high level, long lasting correction but once the principle is established this reduces to a technical problem”. However, it would be 23 years before the first multidose gene therapy trial started in the UK.
In 2006 Pamela Davis received the Paul di Sant’Agnese Award of the CF Foundation.
1980 Hopfer U, Will PC, Dearborn DG. Cystic fibrosis: A secondary endocrine or target tissue sensitivity problem in epithelial electrolyte transport. In Sturgess JM (ed.): Perspectives in Cystic Fibrosis: Proceedings of the Eighth International Congress on CF Toronto. Canadian CF Foundation. 1980.

Fig. 1a Ulrich Hopfer
In this poster Ulrich Hopfer and the authors suggested that abnormal epithelial transport may reflect the basic defect. Certainly at that time it was suspected that there was some kind of a problem at epithelial surfaces but it was not clear if this was an intrinsic problem in the cell membranes or developed in the membranes secondary to circulating substances or the much-studied “CF factor”.
These authors suggested that abnormal epithelial electrolyte transport may reflect the primary defect – “the existence of an extraordinarily active sodium absorption could explain some of the clinical findings of CF e.g. hyperviscous mucus as being caused by excessive absorption of NaCl and water”. This is extraordinarily close to the low salt theory of pathogenesis championed by Richard Boucher and colleagues which is now widely accepted as playing a significant role in the pathogenesis of cystic fibrosis.
1981 Wilson GB, Fudenberg HH, Parise MT, Floyd E. Cystic fibrosis ciliary dyskinesia substances and pulmonary disease. Effects of ciliary dyskinesia substances on neutrophil movement in vitro. J Clin Invest 1981; 68:171-183. [PubMed]
Cultured mononuclear cells (MNC) from individuals homozygous or heterozygous CF individuals were reported to synthesize three unusual “mediators” termed ciliary dyskinesia substances (CDS), which markedly affect tracheal mucociliary systems in vitro. Mononuclear cell cultures from normal healthy controls do not accumulate any CDS, whereas MNC cultures from non-CF patient controls with pulmonary disease synthesized at least one CDS. This study sought to determine whether the CDS could be chemoattractants for polymorphonuclear neutrophils (PMN) and showed excessive chemoattractant activity in MNC cultures from CF genotypes and patient controls due to several different substances produced by monocytes. The authors concluded that all of the CDS can potentially play a role in the pathophysiology of lung disease.
– Wilson and co-workers wrote many papers on CF factor and dyskinesia factors between 1973 and 1984, the last being in 1984 (Wilson GB, et al. Controlled comparison of plasma and serum for cystic fibrosis protein. Clin Genet 1984; 26:331-338). However, interest on CF factors gradually waned during the Eighties as the prospect of identifying the gene became a real possibility and the evidence for a primary abnormality of membrane function gradually accumulated.
1981 Breslow JL, McPherson J, Epstein J. Distinguishing homozygotes and heterozygous cystic fibrosis fibroblasts from normal cells by differences in sodium transport. N Eng J Med 1981; 304:1. [PubMed]
Cultured fibroblasts from patients with CF accumulate less 22Na in the presence of ouabain than do normal cells. The differences between CF homozygotes or heterozygotes and normal subjects were highly significant, but there was considerable overlap between CF homozygotes and heterozygotes. This abnormality of sodium transport was considered to provide “an unequivocal in vitro test that distinguishes normal cells from cells derived from CF homozygotes or heterozygotes”. VIDE INFRA
It was suggested that it would be useful for the identification of carriers of the CF gene. (See also 1977 and 1978). However, a few months later there was a letter of denial from the authors refuting their previous findings (Breslow JL. McPherson J. Sodium transport in cystic-fibrosis-fibroblast not different from normal. N Eng J Med 1981; 305: 98).
1981 Knowles MR, Gatzy JT, Boucher RC. Increased bioelectric potential difference across respiratory epithelia in cystic fibrosis. N Eng J Med 1981; 305:1489-1495. [PubMed]

Fig 2. Michael Knowles
Undoubtedly this was a major landmark paper. Michael Knowles from North Carolina describes how they developed a technique that measured a single parameter of epithelial function – the transepithelial potential difference (PD); this they used to define salt (ion) transport properties of nasal and lower respiratory epithelium in normal humans in vivo and then in patients with CF whose transepithelial PD they showed was markedly higher than normal – a feature apparently present within hours of birth suggesting a primary genetic epithelial defect rather than due to any circulating “CF factor” or effect from infection.
– Knowles and colleagues eventually identified a defect in the ability of Cl to move across CF cells, the Cl permeability of the airway epithelium was not activated by beta-agonists and there was a very rapid absorption of salt and water. This led to the theory that CF airway epithelium has an excessive rate of NaCl and water absorption leading to dehydration of the secretions, reduced clearance of mucus predisposing to chronic airway infection – a theory which increased in popularity and was championed particularly by Knowles’s colleague Richard Boucher.
Michael Knowles (fig. 2) is Professor of Pulmonary and Critical Care Medicine at the University of North Carolina. he has over three decades of clinical research experience that spans across the disciplines of biology, physiology and design of clinical trials. He was honoured with an award from the CF Foundation at the 2008 Annual North American CF Conference. He and Richard Boucher are certainly two of the outstanding North American CF clinicians and researchers of the era.
1982 Chow CW, Landau LI, Taussig LM. Bronchial mucus glands in newborn with cystic fibrosis. Eur J Pediatr 1982; 139:240-243. [PubMed]
Bronchial glands of 21 CF infants who died aged less than 3 weeks from meconium ileus were not different from those of 28 controls. Absence of mucus gland hyperplasia at birth suggests that mucous obstruction is not primarily responsible for the susceptibility to infection.
– A vast amount of research had been done over the previous years to determine intrinsic abnormalities of mucus caused by the basic defect without any definite repeatable conclusions. However, this paper was useful in suggesting that intrinsic abnormalities in the structure of CF mucus were probably not a major factor in the pathogenesis of the lung infections. The findings of Knowles et al 1981 (above) supported the view that salt and water abnormalities leading to dehydration of the airway secretions were a more likely reason for alteration in the viscosity of the airway secretions predisposing to chronic infection than were intrinsic abnormalities in the structure of the mucus.
1983 Quinton PM. Chloride impermeability in cystic fibrosis. Nature 1983; 301:421-422. [PubMed]

Fig 3. Paul Quinton
Another landmark paper in the understanding the CF defect. Paul Quinton later recalls (Quinton, 1999 below) that Mike Knowles (1981 above) reported a significantly larger than normal electronegative potential across the nasal epithelium, along with the fact that NaCl absorption was inhibited in the CF sweat ducts and also that sodium was relatively more absorbed than chloride. Apparently this gave Quinton the idea that the basic defect in the CF duct had to be due to an anion impermeability and not defective anion exchange.
Using a series of microperfusion experiments of sweat glands (it is said from his own forearms) he measured the electrolytes by “energy dispersive X-ray analysis”. The chloride impermeability he had shown in sweat glands was the basis for the raised sweat electrolytes and provided a physiological explanation for the high salt content of CF sweat and also “provided the first description of a basic cellular defect that has since proven to be uniformly inherent in all CF affected cells”.
Dr Paul Quinton (figure 3) is a Professor of Pediatrics at University of California, San Diego, and a Professor of Biomedical Sciences at University of California, Riverside. Dr. Quinton’s interest in CF stems from his own diagnosis of the condition when he was 19 years old – he is now well into his sixties. Dr. Quinton is recognized for his recognition the basic defect in the CF sweat duct had to be due to an anion impermeability and not defective anion exchange – now accepted as one of the major advances in understanding of the basic defect.
1984 Sato K, Sato F. Defective beta adrenergic response of cystic fibrosis sweat glands in vivo and in vitro. J Clin Invest 1984; 73:1763-1771. [PubMed]
Abnormal sodium chloride absorption from the ducts of the sweat glands had been known as the only defect in CF sweat glands. These authors fortuitously found that the secretory portion of CF sweat glands is also abnormal in that it failed to show a sweating response to beta adrenergic stimulation (isoproterenol) both in vivo and in vitro. Their data, after detailed study of the sweat glands, suggested that beta adrenergic regulation was abnormal in CF sweat glands and justified further investigations into the mechanism of beta adrenergic regulation of the eccrine sweat gland in both normal and CF subjects.
Subsequently it was shown that the insensitivity was due to the fact that in the sweat gland b-adrenergically stimulated fluid secretion was coupled with the same chloride channel as was altered in salt absorption.
1985 Kopleman H, Durie P, Gaskin K, Weizman Z, Forstner G. Pancreatic fluid secretion and protein hyperconcentration in cystic fibrosis. N Eng J Med 1985; 312:329-334. [PubMed]
Using the expertise in pancreatic function testing developed in Toronto by Peter Durie and his colleagues, the secretion of pancreatic protein and water was studied in 28 patients with CF and 21 controls matched for pancreatic acinar function as defined by trypsin secretion, using a quantitative-marker perfusion technique and continuous intravenous secretin-pancreozymin stimulation. Secretions from the patients with CF contained significantly higher concentrations of protein than those from the controls and their fluid secretion was significantly decreased.
Somewhat analogous to the situation in the airways, the authors concluded that fluid secretion in patients with CF may be a rate-limiting factor in protein output and that a limited flow of hyperconcentrated protein secretions may predispose to protein precipitation and ductal obstruction in the pancreas. (also Kopleman et al, 1988 below).
1985 Eiberg H, Mohr J, Schmiegelow K, Nielsen LS. Linkage relationships of paraoxinase (PON) with other markers: evidence of PON-cystic fibrosis synteny? Clin Genet 1985; 28:265-271. [PubMed]
Fig 4. Hans Eiberg
This was the first positive move towards narrowing down the location of the CF gene. The linkage relationships of the serum arylesterase paraoxonase (PON) was examined in normal Danish families and in Danish and English CF families by Professor Hans Eiberg (fig. 4). The highest correlation was found between the inheritance of paraoxinase and cystic fibrosis. Linkage studies for PON against 64 other polymorphic marker systems did not give such a close relationship. By the present screening about 2/3 of the genome could tentatively be excluded as the region of PON and cystic fibrosis. (Synteny = the presence together on the same chromosome of two or more gene loci).
Prof. Hans Eiberg (1945-) (fig. 4) is a Danish geneticist, known for the discovery of the genetic mutation causing blue eyes. Together with Professor Jan Mohr he established the Copenhagen Family Bank in 1972, a store of DNA samples, comprising about 1000 large Danish families. Hans Eiberg has contributed to the mapping of the human genome, and he has succeeded in finding important genetic markers for several serious illnesses in addition to cystic fibrosis.
1985 Tsui L, Buchwald M, Barker D, Braman JC, Knowlton R, Schumm JW, Eiberg H, Mohr J, Kennedy D, Plavsic N, et al. Cystic fibrosis locus defined by a genetically linked polymorphic DNA marker. Science 1985; 230:1054-1057. [PubMed]

Fig 5. Lap Chi Tsui
Lap Chi Tsui (fig. 5) and co-workers used a restriction fragment to localise the gene to the long arm of chromosome 7. In a set of 39 families, a polymorphic DNA marker was genetically linked to the autosomal recessive gene that causes cystic fibrosis. The DNA marker (called D0CRI-917) was also linked to the paraoxinase locus, which by independent evidence was linked to the CF locus (Eiberg et al, 1985 above). The location of the CF gene was now narrowed to about 1 percent of the human genome (about 30 million base pairs). This was the first step in molecular analysis of the CF gene. Localising the CF gene to chromosome 7 was a major step forward.
Apparently Lap Chi Tsui encountered several problems when working with the pharmaceutical firm, Collaborative Research Inc. The firm had already invested $10 million in the project and they could see the commercial opportunities of developing markers for antenatal and carrier diagnosis. The problems are well described by Leslie Roberts (Science 1988; 240:141-144 [PubMed] & 282-285 [PubMed]). Essentially Collaborative Research Inc. wanted to delay publication of the location of the gene on chromosome 7 until more markers could be identified and patents could be applied for. Meanwhile other groups, Williamson’s in London (Wainwright et al, 1985 below) and Ray White’s in Utah (White et al, 1985 below) were said to know of the findings that the CF gene was on chromosome 7 and had already identified other markers very close to the CF gene.
1985 White R, Woodward S, Leppert M, O’Connell P, Hoff M, Herbst J, Lalouel JM. Dean M. Vande Woude G. A closely linked genetic marker for cystic fibrosis. Nature 1985; 318:382-384.[PubMed]
Fig.5a Ray Leslie White. www.cell.com
Ray White (1943-2018) and co-workers in Utah describe evidence for tight linkage between the CF locus and a DNA sequence polymorphism at the met oncogene locus. They state that this evidence, combined with the physical localisation data for the met locus presented in the accompanying paper, places the CF locus in the middle third of the long arm of chromosome 7, probably between bands q21 and q31.
1985 Wainwright BJ, Scambler PJ, Schmodtke J, Watson EA, Law H, Farrall M, Cooke HJ, Eiberg H, Williamson R. Localization of cystic fibrosis locus to human chromosome 7cen-q22. Nature 1985; 318:384-385. [PubMed]

Fig. 6 Brandon Wainwright UQ Researchers
This paper from Brandon Wainwright,(at the time working with Bob Williamson’s St Mary’s research group in London,) noted that Eiberg et al. had reported a genetic linkage between the CF locus and a polymorphic locus controlling activity of the serum aryl esterase paraoxonase (PON). The chromosomal location of PON, however, was not known at the time. Linkage to a DNA probe, DOCR1-917, was also recently found at a genetic distance of approximately 15 centimorgans (L.-C. Tsui and H. Donnis-Keller of Collaborative Research Inc.) but no chromosomal localization was given. In this paper the St Mary’s group report tight linkage between the CF locus and an anonymous DNA probe, pJ3.11, which has been assigned to chromosome 7cen-q22.
Professor Brandon Wainwright (fig. 6) is now Director of the Institute of Molecular Bioscience, University of Queensland. He was a member Cystic Fibrosis Trust’s UK Gene Therapy Consortium Scientific Advisory Committee. Professor Wainwright was appointed Director of the Institute for Molecular Bioscience in December 2006. Previously, he was Deputy Director (Research) of the IMB. Professor Wainwright joined the University of Queensland in 1990 as a Senior Lecturer in the Centre for Molecular and Cellular Biology and the Department of Biochemistry.
1985 Knowlton RG, Cohen-Hagenhauer O, Van Cong N, Frezal J, Brown VA, Barker D, Braman JC, Schumm JW, Tsui LC, Buchwald M, et al. A polymorphic DNA marker inked to cystic fibrosis is located on chromosome 7. Nature 1985; 318:681-693. [PubMed]
Two markers which had recently been identified were genetically linked to CF: one was a genetic variation in serum level of activity of the enzyme paraoxonase, and the other a restriction fragment length polymorphism (RFLP) identified with a randomly isolated DNA probe. These authors report that the genetic locus DOCRI-917 defined by the cloned DNA probe is located on chromosome 7.
Robert G Knowlton in the Dept. of Human Genetics, Collaborative Research Inc. Lexington, Massachusetts.
1986 Higgins CF, Hiles ID, Salmond GP, Gill DR, Downie JA, Evans IJ, Holland IB, Gray L, Buckel SD, Bell AW, et al. A family of related ATP-binding subunits coupled to many distinct biological processes in bacteria. Nature 1986; 323(6087):448-450. [PubMed]

Fig 7. Chris Higgins
Many biological processes are coupled to ATP hydrolysis. Professor Chris Higgins ( -1955) (fig. 7) and his colleagues describe a class of closely related ATP-binding proteins, from several bacterial species, which are associated with a variety of cellular functions including membrane transport, cell division, nodulation in Rhizobium and haemolysin export. These proteins mediate the transport of molecules across the cell membrane and CFTR was later found to belong to this family of proteins.
Prof Chris Higgins (fig. 7) was the first to describe these ATP binding proteins which are of obvious relevance in CF. He was involved in work on the scientific aspects of CF during the Eighties and Nineties when at Oxford and Imperial College particularly during the early planning and execution of the gene therapy studies. Later he was involved in an advisory capacity to the Gene Therapy Consortium and UK CF Trust on the Scientific Advisory Committee until his appointment as Vice-Chancellor of Durham University.
1986 Frizzell RA, Rechkemmer G, Shoemaker RL. Altered regulation of airway epithelial cell chloride channels in cystic fibrosis. Science 1986; 233(4763):558-560. [PubMed]
Fig 8. Raymond Frizzell. cfrc.pitt.edu
In many epithelial cells the chloride conductance of the apical membrane increases during the stimulation of electrolyte secretion. Single-channel recordings from human airway epithelial cells showed that beta-adrenergic stimulation evoked apical membrane chloride channel activity, but this response was absent in cells from patients with cystic fibrosis (also Sato et al, 1984 above). However, when membrane patches were excised from CF cells into media containing sufficient free calcium (approximately 180 nanomolar), chloride channels were activated. So the chloride channels of CF cells were similar to those of normal cells as judged by their current-voltage relations, ion selectivity, and kinetic behaviour.
These findings demonstrate the definite presence of chloride channels in the apical membranes of CF airway cells. Their regulation by calcium appears to be intact, but cyclic adenosine monophosphate (cAMP)-dependent control of their activity is defective.
Raymond Frizzell (fig. 8) is Professor and Director of the Cystic Fibrosis Research Center, Children’s Hospital and the Department of Cell Biology and Physiology, School of Medicine, University of Pittsburgh. His group is interested in the mechanisms of chloride and sodium transport across absorptive and secretory epithelial cells of the lung and kidney, in the biogenesis and quality control pathways that influence ion channel expression, and in the membrane trafficking mechanisms that govern channel density at the cell surface. This work focuses primarily on the anion channel CFTR.
1987 Dorin JR, Novak M, Hill RE, Brock DJ, Secher DS, van Heyningen V. A clue to the basic defect in cystic fibrosis from cloning the CF antigen gene. Nature 1987; 326(6113):614-617.[PubMed]
Fig 9. Victoria van Heyningen
Elevated levels of a serum protein in CF homozygotes and obligate heterozygotes had been described by Julia Dorin and Veronica van Heyningen (fig. 9) from Edinburgh. As heterozygotes are clinically unaffected, any consistently observed abnormality in these individuals is a likely pointer to the aetiology of the disease. The gene for this serum protein, called cystic fibrosis antigen, has been mapped to chromosome 1. It is not the gene that is mutant in CF because that is known to be on chromosome 7. CF antigen is a product of normal and leukemic granulocytes and is inducible in the promyelocytic cell line HL60. Abnormal accumulation of such a protein in CF is a clue which they intended to pursue now that evidence was gathering that the basic defect in CF was in pathways controlling chloride channel activity.
The MRC note later that this protein was also found useful in studying other inflammatory diseases and it has been useful in determining the effect of gene therapy. See also in relation to HL60 and CF (below).
1987 Harris A, Coleman LJ. Establishment of a tissue culture system for epithelial cells derived from human pancreas: a model for the study of cystic fibrosis. Cell Sci 1987; 87(Pt 5):695-703.[PubMed]

Fig. 10. Ann Harris northwestern.edu
A tissue culture system for epithelial cells derived from human foetal pancreas was established. The cultured cells show many ultrastructural features of interlobular duct cells. Immunocytochemical and histochemical evidence is presented in support of the view that these cells are ductal in origin. They are likely to be one of the few cell types that express the basic defect of cystic fibrosis in vitro. The cells may be passaged and sufficient material obtained to permit biochemical and molecular biological analysis.
Ann Harris (fig. 10) is now Professor in Pediatrics-Human Molecular Genetics, Northwestern University Feinberg School of Medicine. Originally from UK where she was involved in CF research at Guys Hospital in London and later at Oxford before moving to Northwestern in 2005 as Director of the Human Genetics Programme. I remember her as an enthusiastic and important member of the CF Trust’s Research and Medical Advisory Committee during the Eighties.
By 2013 Ann states her research interests were in 2 areas: 1. Tissue-specific regulation of gene expression, chromatin structure and modification in the context of the CFTR gene, which when mutated causes the common inherited disease Cystic Fibrosis. We identified and are characterizing intronic and extragenic elements that control CFTR gene expression, modulate the 3D structure of the locus and mediate tissue specificity. Our latest work applies whole genome analysis of cis-regulatory elements and their trans-interacting factors to elucidate the differentiated functions of primary human airway and epididymis epithelial cells. 2. Pancreas Cancer. We are investigating the role of secreted proteoglycans (collagen XV and the MUC6 mucin) in initiation, invasion and metastasis of human pancreatic adenocarcinoma.
1988 Taylor CJ, Baxter PS, Hardcastle J, Hardcastle PT. Failure to induce secretion in jejunal biopsies from children with cystic fibrosis. Gut 1988; 29:957-962. [PubMed]

Fig 11. Jacqueline & P T Hardcastle with Chris Taylor Author’s photo
In this study by Prof. Chris Taylor (fig. 11) and colleagues from Sheffield, the secretory activity of jejunal biopsies from children with CF was investigated using a modified Ussing chamber technique. The results showed that the defect in chloride transport observed in other epithelia in CF also exists in the jejunum and could contribute to the intestinal effects of the disease.
Similar findings were obtained in a study from Chapel Hill (Berschneider HM, et al. Altered intestinal chloride transport in cystic fibrosis. FASEB Journal 1988; 2:2625-9. [PubMed])with the same suggestion that the existence of these abnormalities may contribute to the intestinal problems, such as meconium ileus, distal intestinal obstruction and chronic abdominal pain which are by no means all controlled even with the more effective acid resistant enzyme preparations such as Pancrease and Creon.
Chris Taylor (fig. 11) is one of the UK’s leading authorities on CF generally but particularly with regard to the gastroenterological and nutritional aspects. He and the Hardcastles, his scientific colleagues in Sheffield, have made major contributions to the scientific aspects of CF concerning membrane function.
1988 Goldstein JL, Nash NT, al-Bazzaz F, Layden TJ, Rao MC. Rectum has abnormal ion transport but normal cAMP-binding proteins in cystic fibrosis. Am J Physiol 1988; 254: C719-24. [PubMed]
In keeping with the small intestinal and colonic electrolyte transport abnormalities in CF, when the authors compared in vivo transrectal potential difference (PD) in CF, the base-line PD was different in normal and CF subjects and was eliminated by amiloride in both groups. However, in response to a Cl-free solution with amiloride, all six CF subjects exhibit less of a change in potential difference. They concluded that the rectum is also an involved epithelium in CF in which the aberration may lie at a point beyond the binding of cAMP to its protein kinase.
– This is not an unexpected finding as there are obvious and characterisitic histological abnormalities of the rectal epithelium in CF (Parkins et al, 1963 above).
1988 Kopelman H, Corey M, Gaskin K, Durie P, Weizman Z, Forstner G. Impaired chloride secretion, as well as bicarbonate secretion, underlies the fluid secretory defect in the cystic fibrosis pancreas. Gastroenterology 1988; 95:349-355. [PubMed]

Fig 12.Peter Durie
Pancreatic fluid and electrolyte secretion was assessed in 56 patients with CF and 56 non-CF control subjects undergoing stimulated pancreatic function tests. The CF subjects secreted significantly less fluid than control subjects caused by impaired chloride, as well as bicarbonate, secretion. Paul Quinton, commenting on this and the 1985 paper (Kopleman et al, 1985 above) from Toronto, noted that both studies showed that bicarbonate and volume outputs were abnormally low in CF and that chloride impermeability had a pronounced negative effect on exocrine bicarbonate transport…. Without sufficient fluid and bicarbonate digestive proenzymes stagnated and activated prematurely in the pancreatic ducts… resulting in micro autolysis, focal injury, inflammation, infiltration, calcification, plugged ducts, fibrosis, and scarring until the entire parenchyma of the pancreas like the lung, but from a seemingly different cause, was destroyed. This seemed a very reasonable explanation as to why the lungs are virtually normal at birth and the pancreas already severely damaged in many infants (also Kopleman et al, 1985 above).
Peter Durie ( -2018) (figure 12) has made major contributions to CF research and clinical care for many years during his time in Toronto. He was Professor in the Department of Paediatrics, Faculty of Medicine, University of Toronto and holds a number research and clinical appointments at the Hospital for Sick Children in Toronto relating to nutrition and gastroenterology. Since his first contributions with Gordon Forstner nearly 30 years ago he has published widely on CF and many other subjects. Most clinicians will remember the work on pancreatic function which he directed. He is an expert on the disorders of the exocrine pancreas in children and has researched on the various gastrointestinal aspects of CF and other inherited disorders of the pancreas.
1989 Gray MA, Harris A, Coleman L, Greenwell JR, Argent BE. Two types of chloride channel on duct cells cultured from human fetal pancreas. Am J Physiol 1989; 257(2 Pt 1):C240-51.[PubMed]
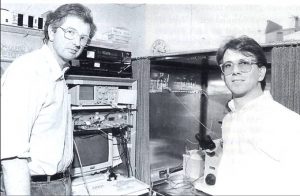
Fig 13. Mike Gray and Barry Argent in their laboratory. CF Trust photo

Fig 14. Michael Gray in recent times. Author’s photo.
Using the patch-clamp technique, two types of chloride channel were identified on duct cells from human fetal pancreas. The channel observed most frequently exhibited slight outward rectification, had a conductance of 4-7 pS in cell-attached patches, and was present on the apical plasma membrane where it usually occurred in clusters. Its open-state probability was not markedly voltage dependent but was increased up to threefold by exposing duct cells to secretin (10 nM), dibutyryl cyclic AMP (1 mM), or forskolin (1 microM). The other type of chloride channel was only rarely observed. Its current-voltage relationship exhibited marked outward rectification, giving chord conductances of 19 pS for inward currents and 53 pS for outward currents. Although this channel could be activated by sustained depolarization of excised patches, once activated the open state probability was not voltage dependent. While the physiological role of these channels is not firmly established, the small-conductance channel might function in parallel with a Cl- -HCO-3 exchanger to provide a mechanism for electrogenic bicarbonate secretion from the duct cell.
This paper was from a number of the UK’s leading scientific CF researchers – senior members being Michael Gray (Fig.14) and Barry Argent (fig. 13 left) from Newcastle.
Dr Michael Gray (figure 12, 13) is Reader in Cellular Physiology in the University of Newcatle on Tyne. He has remained involved in the CF research and also in providing advice to the CF Trust in various capacities. His major research interest of is to understand the cellular mechanisms that orchestrate epithelial ion, fluid and mucus secretion in differentiated adult epithelial tissues, and how epithelial dysfunction impacts on the pathogenesis of chronic diseases such as cystic fibrosis and asthma.
Fig. 14a. Jeffrey Wine
Professor Jeffrey Wine (Fig.14a) commented in 2010 as follows – ” I was happy to see that you do indeed include Mike Gray and Barry Argent in your account of the Eighties-but you may want to burnish the account of their work. That time was a very bad time for me, because of a bitter controversy concerning the identity of the chloride channel responsive for cystic fibrosis. Our work suggested it wasn’t the large, outwardly rectifying channel that everyone else was focused on, and so when their 1989 paper appeared it was an enormous comfort to me and a great step forward for the field. Here is their last paragraph: I have italicized the prophetic words of the final sentence–another excellent example of British understatement, like the famous “It has not escaped our notice. . .”
“Finally, the identification of chloride channels on human duct cells may provide an explanation for the reduced pancreatic bicarbonate secretion that occurs in the inherited disease cystic fibrosis. In airway epithelium the underlying genetic defect is expressed as abnormal regulation of the secretory chloride channel by CAMP , and here we report a similar, outwardly rectifying chloride channel on human pancreatic duct cells. However, because we detected this channel so infrequently and obtained no evidence for its regulation by CAMP or Ca2+, its role in ductal anion transport must remain uncertain. We believe a stronger candidate for involvement in the pancreatic pathology of cystic fibrosis is the CAMP-regulated, small-conductance chloride channel located on the apical membrane of the ductal cells.”
See also 1991 Ward, C. L., M. E. Krouse, D. C. Gruenert, R. R. Kopito and J. J. Wine.
“Cystic fibrosis gene expression is not correlated with rectifying Cl- channels.” Proc Natl Acad Sci U S A 88(12): 5277-81. [PubMeD]
1991 Wine, J. J., D. J. Brayden, G. Hagiwara, M. E. Krouse, T. C. Law, U. J. Muller, C. K. Solc, C. L. Ward, J. H. Widdicombe and Y. Xia. “Cystic fibrosis, the CFTR, and rectifying Cl- channels.” Adv Exp Med Biol 290: 253-69. [PubMed]
1989 Baxter PS, Wilson AJ, Read NW, Hardcastle J, Hardcastle PT, Taylor CJ. Abnormal jejunal potential difference in cystic fibrosis. Lancet 1989; i: 464-466. [PubMed]

Fig 15. Peter Baxter. Author’s photo
Further work from Chris Taylor’s Sheffield team that had already described failure to induce secretion from CF jejunal biopsies (Taylor et al, 1988 above). Here the transmucosal potential difference (PD) and intraluminal pressure were recorded from the same jejunal site in 15 healthy adult controls and 4 adults with cystic fibrosis. In the controls, runs of contractions were associated with wave-like changes in PD that were absent in patients with cystic fibrosis. Intraluminal boluses of 4 mg pilocarpine, or 0.1 mg prostaglandin E2, caused changes of -4.6 mV and -4.5 mV, respectively, in controls; these responses were not seen in patients with cystic fibrosis. There were no significant differences in basal PD and PD changes caused by altered concentrations of infused saline or glucose between patients and controls.
Dr Peter Baxter (fig. 15) at the time was CF Research Fellow and was later a Consultant Paediatric Neurologist at Sheffield Children’s Hospital.
1989 The following three historic papers, reporting the identification of the CF gene, represented a high point of CF research in the Eighties. The picture is the cover of the edition of Science in which the papers appeared (figure 16).
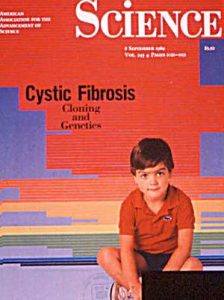
Fig 16. Cover of Science Vol 245, September 1989
1989 Kerem B-S, Rommens JM, Buchanan JA, Markiewicz D. Cox TK. Chakravarti A. Buchwald M. Tsui LC. Identification of the cystic fibrosis gene: genetic analysis. Science 1989; 245:1073-1080. [PubMed]

Fig 17. Batsheva Kerem
Approximately 70 percent of the mutations in cystic fibrosis patients correspond to a specific deletion of three base pairs, which results in the loss of a phenylalanine residue at amino acid position 508 of the putative product of the cystic fibrosis gene. Extended haplotype data based on DNA markers closely linked to the putative disease gene locus suggest that the remainder of the cystic fibrosis mutant gene pool consists of multiple, different mutations. A small set of these latter mutant alleles (about 8 percent) may confer residual pancreatic exocrine function in a subgroup of patients who are pancreatic sufficient. The ability to detect mutations in the CF gene at the DNA level had important implications for genetic diagnosis.
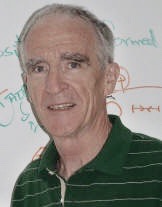
Fig 18. Jack Riordan
1989 Riordan JR, Rommens JM, Kerem B-S, Alon N. Rozmahel R. Grzelczak Z. Zielenski J. Lok S. Plavsic N,Chou JL. et al. Identification of the cystic fibrosis gene: cloning and characterization of the complementary DNA. Science 1989; 245:1066-1073. [PubMed]
Overlapping complementary DNA clones were isolated from epithelial cell libraries with a genomic DNA segment containing a portion of the putative CF locus, which is on chromosome 7. Transcripts, approximately 6500 nucleotides in size, were detectable in the tissues affected in patients with CF. The predicted protein consists of two similar motifs, each with (i) a domain having properties consistent with membrane association and (ii) a domain believed to be involved in ATP (adenosine triphosphate) binding. A deletion of three base pairs that results in the omission of a phenylalanine residue at the center of the first predicted nucleotide-binding domain was detected in CF patients.
1989 Rommens JM, Iannuzzi MC, Kerem B-S, Alon N. Rozmahel R. Grzelczak Z. Zielenski J. Lok S. Plavsic N. Chou JL. et al. Identification of the cystic fibrosis gene: chromosome walking and jumping. Science 1989; 245:1059-1065. [PubMed]

Fig 19. Lap Chi Tsui
An understanding of the basic defect in the inherited disorder cystic fibrosis requires cloning of the cystic fibrosis gene and

Fig 20 Francis Collins
definition of its protein product. In the absence of direct functional information, chromosomal map position is a guide for locating the gene. Chromosome walking and jumping and complementary DNA hybridization were used to isolate DNA sequences, encompassing more than 500,000 base pairs, from the cystic fibrosis region on the long arm of human chromosome 7. Several transcribed sequences and conserved segments were identified in this cloned region. One of these corresponds to the cystic fibrosis gene and spans approximately 250,000 base pairs of genomic DNA

Fig 21. 1989 at the presentation of the Paul di Sant’Agnese award to the leaders of the teams (in italics type) who identified the CF gene. from left to right – Lap-Chi Tsui, Paul di Sant’Agnese,Evelyn Graub, Milto Grau (past President of the CF Foundation, Francis Collins and Jack Riordan
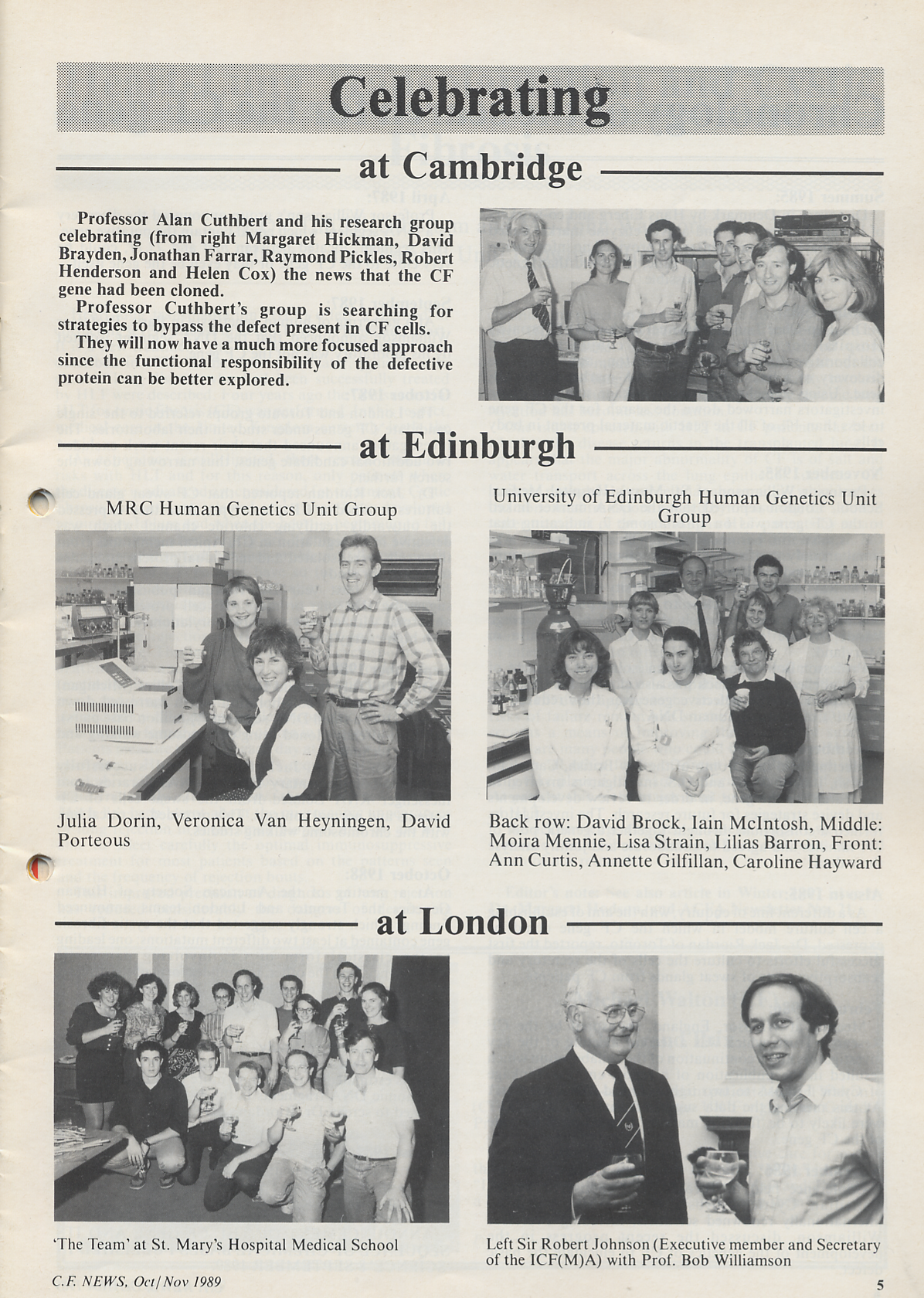
There were also celebrations in the UK by the various groups who had been fully occupied in the search for the GENE