Sixties – clinical
Sixties – clinical
CF Centre care for a few people in some countries – both benefits and side effects from long term treatment. Cystic fibrosis organisations, rare paradigms of good clinical care and the increasing use of the sweat test
During the Sixties more national CF organisations were formed, usually following pressure from parents and engendering a collaborative approach between the medical community and the CF families; but few people other than those closely involved had even heard of cystic fibrosis. The US National CF Research Foundation (later the CF Foundation) had been formed in 1955 (above), and the Canadian CF Foundation in 1959 (above). Subsequently, national CF organisations formed in many countries where CF was identified; their programmes covered welfare, support, advocacy, clinical care, professional education and research, depending on the local stage of development.
Sir Robert Johnson
In 1964 the UK “Cystic Fibrosis Research Foundation Trust” was formed as a charitable organisation to raise funds for research (full account of early years by Sir Robert Johnson QC is in the “More Historical Things” section – “Some previous publications on the history of cystic fibrosis”). Sir Robert Johnson, a parent of two children with CF, was one of the founders of the UK Cystic Fibrosis Trust in 1964 and subsequently Vice Chairman. He recalls the depressing situation facing CF families in the UK in the Sixties – “the general picture here was of ignorance and distress, unmitigated by hope or practical effective action”. As a young paediatrician in the Sixties I can certainly vouch for the hopeless outlook for infants identified as having CF at that time., as more patients survived and an increasing proportion of the research funds went to support clinical care in the developing CF centres during the Eighties, the scientists on the Research and Medical Advisory Committee of the UK CF Research Trust requested the title of the organisation be amended to the “The Cystic Fibrosis Trust” as an increasing proportion of funding was going to patient care rather than research! Many years later, in the late Nineties, the CF clinicians, many with large CF clinics, complained bitterly that too great a proportion of the CF Trust’s resources was going to the scientists working on gene replacement therapy!
In 1965 the International Cystic Fibrosis (Mucoviscidosis) Association (ICFMA), the predecessor of CF Worldwide, was formed in Paris under the medical chairmanship of Paul di Sant’Agnese. In 1960, prior to his moving from New York to The National Institutes of Health, di Sant’Agnese visited Europe to meet other clinicians interested in cystic fibrosis. These included Prof. Guido Fanconi and Prof. Ettore Rossi (Switzerland), Prof. Andre Hennequet and Dr Jean Feigelson (France), Drs Archie Norman and David Lawson (England), Prof. G de Toni (Italy) and Profs. Weijers, Dicke and Van de Kamer (Holland). The aims of the ICFMA were to improve the care of children and adults who had CF, to foster research and to disseminate information. Also di Sant’Agnese notes that prior to this meeting those working in CF did not know each other except through the literature and so the ICFMA brought together physicians, paramedical personnel and lay people giving them a sense of common purpose. This was the start of the International CF (ICFMA) now CF Worldwide meetings, which occur every 4 years. It is difficult to appreciate the problems with communication and travel in the Sixties – before the days of easy air travel, photocopiers, fax machines, e-mails, internet and medical databases such as Medline and PubMed.
Niels Hoiby
In 1969, the European Working Group for Cystic Fibrosis (EWGCF) was formed to provide an annual forum where people from the various disciplines, but with a common interest in CF, could meet, present and discuss their latest findings. Since 1970, there has been an annual meeting (except every four years when there is a combined meeting of the International Cystic Fibrosis Congress) in a different European country and organised in conjunction with the local CF association. In 1997, following suggestions over a number of years by the membership, the Board decided to propose an official transformation of the EWGCF to a Society to be known as the European Society for Cystic Fibrosis (ESCF). However, subsequently it was realised that the name abbreviation was similar to that of a study group associated with the American CF Foundation (Study of Epidemiology of Cystic Fibrosis). Consequently the name of the European society was changed again at the Annual General Meeting held at the 22nd European CF Conference in Berlin, June 1998 to the European Cystic Fibrosis Society (ECFS).
An account of the history of the ECFS, based on a presentation given by Niels Hoiby at the annual ECFS Conference in 2007, is in the “Some previous publications on the history of cystic fibrosis” in the “More Historical Things” section of this website.
During the Sixties sweat tests gradually became more widely available following the publication of the pilocarpine iontophoresis method of sweat stimulation by Gibson and Cooke (1959, above). I was impressed by Dr Tom McKendrick’s sweat test study (McKendrick, 1962 below) in progress when I was a house physician at the Hospital for Sick Children, Great Ormond Street in London. So on returning to Leeds, as a Lecturer in Paediatrics, I arranged for the purchase of a sweat-testing box and our biochemist, Mr Alan Steele, soon introduced accurate sweat tests. By 1968, with our recently introduced paediatric jejunal biopsy service to identify coeliac disease, most infants and children with malabsorption problems could be accurately diagnosed. Both these services were used by many paediatricians in the Yorkshire region (population 3.6 million) and the seeds of the Leeds Regional CF Service were sown.
Paul Quinton notes that CF research in the Fifties, Sixties and Seventies, searching for the basic defect that would unify the disparate symptoms of the disease, followed numerous paths mainly based primarily on empirical observations, often completely unrelated to any known pathology – the era he described as the “Wild West” era of research (Quinton, 1999 below). So essentially, during the Sixties, there was little progress in the understanding of the basic defect in cystic fibrosis.

Beat Haddorn
Although by no means the first to perform stimulated pancreatic function tests on children with CF, the name of Beat Hadorn is closely associated with accurate stimulated pancreatic function tests in CF; he described the pancreozymin–secretin stimulation test using a triple lumen tube. Hadorn showed that in CF there was a markedly reduced volume of stimulated pancreatic juice and abnormally low bicarbonate levels even in those few people with CF who had sufficient residual pancreatic function to achieve normal fat absorption (Hadorn et al, 1968 below). However, although these tests were useful they were invasive and unpleasant for the children and required significant sedation, duodenal intubation and intravenous access. Later, non-invasive faecal chymotrypsin levels (Barbero et al, 1966 below; Brown et al, 1988 below) and more recently faecal pancreatic elastase 1 measurements have simplified the recognition of pancreatic insufficiency (Wallis et al, 1997 below; Cade et al, 2000 below). So although there had been some progress in a few clinics, particularly with regard to making the diagnosis with the sweat test, the outlook for most children with CF remained very poor with very few even reaching adolescence. Although there were reports of an improving outlook from a few large CF centres, most children in the UK did not attend a CF centre and most still died within the first few years. The nature of the basic defect remained totally obscure; also relatively few scientists were researching the problem.
CLINICAL PAPERS PUBLISHED IIN THE SIXTIES
1960 Shwachman H. Therapy of cystic fibrosis of the pancreas. Pediatrics 1960; 25:155-163. [PubMed]

Fig 1. Harry Shwachman
A review of management presented to the American Academy of Pediatrics in 1958 by Harry Shwachman, the most experienced CF clinician at the time, who urged caution “against discarding any form of therapy that offers relief” but avoiding “the use of harmful agents and needless operative procedures”.
The article is a pleasure to read and full of wise advice. For example, Harry Shwachman (figure 1) stressed the importance of early and certain diagnosis, adequate education of the parents, seeing the patient at regular intervals, also being readily accessible for advice. On the last he comments – “clinic as well as private patients may call us on the phone whenever questions arise”.
Although often accused of advising severe fat restriction, Shwachman states that fat is allowed as tolerated. Iodides were thought to be helpful in thinning the viscid secretions, intramuscular or aerosol pancreatic trypsin were not recommended nor were carbon dioxide inhalations but the mist tent, with a 10% solution of propylene glycol and 3% saline, was helpful as were “English” methods of physiotherapy. Antibiotics were central to treatment but the parenteral route was rarely used – a major difference to present day treatment. Oral chlortetracycline or oxytetracycline, at times were combined with erythromycin or a sulphonamide, and aerosol penicillin and streptomycin or neomycin and polymyxin.
It is interesting, in view of the present role of macrolides, that both Harry Shwachman and Margaret Mearns appeared to find erythromycin was helpful.
1960 Anderson CM, Freeman M. Sweat test results in normal persons of different ages compared with families with fibrocystic disease of the pancreas. Arch Dis Child 1960; 35: 581-587. [PubMed]
Charlotte Anderson (figure 2) (from Melbourne and later Birmingham UK) showed no abnormality in the sweat electrolytes from parents or siblings of people with CF nor in patients with other chronic chest diseases. A wide scatter of results was obtained in adults for example 34/100 normal adults had sweat sodium levels over 60meq/l. Anderson states that “determination of sweat sodium and chloride loses much of its value” in adults. Also intradermal mecholyl chloride was used to stimulate sweating in Anderson’s study.

Fig 2. Charlotte Anderson
This method of stimulating sweating did not become popular and we heard of one serious reaction with the method. The details of the methods used in the study were criticised by di Sant’Agnese as a different dose of mecholyl was used in the different age groups and this may have affected the rate of sweating which would influence the concentration of electrolytes (also Simmonds EJ, et al. Arch Dis Child 1989; 64:1717-1720. [PubMed]). So di Sant’Agnese considered that the conclusions drawn by Anderson and Freeman “were not warranted by their limited experience”. Fortunately during the Sixties the sweat test by the Gibson and Cooke pilocarpine iontophoresis method, first described in 1959 (above), slowly became the gold standard. Later studies from Great Ormond Street, London (McKendrick et al, 1963 below) showed the sweat electrolytes were insignificantly higher than normal in obligatory heterozygotes.
1960 Marks BL, Anderson CM. Fibrocystic disease of the pancreas in a man aged 46. Lancet 1960; i: 365-367. [PubMed]
A very detailed report from Melbourne of a middle aged man with long standing bronchial infection, bronchial damage and chronic diarrhoea with pancreatic achylia determined by detailed pancreatic function tests. The sweat sodium and chloride were 85 and 71 meq/l respectively. Spermatozoa were absent from the seminal fluid. There was a family history of deaths in childhood.
This was the oldest well-documented patient reported up to this time – with very convincing evidence for the diagnosis.
1960 Leading article. Mucoviscidosis in adults. Lancet 1960; i: 963-964. [PubMed]
This article is confusing. The writer discusses the possibility of encountering CF in older patients and mentions the Marks & Anderson 46 year-old man with CF (Marks & Anderson, 1960 above). Also there is discussion of a paper by Koch of Giessen (Koch E. Germ Med Mon 1960; 5:40) who searched for CF in an adult hospital population and reviewed “84 such cases” – presumably considered to have cystic fibrosis. He searched through healthy students, gall bladder patients, peptic ulcer patients, 88 patients with unrelated complaints and 68 close relatives of CF patients. Diagnosis was based on sweat tests and pancreatic enzymes in duodenal aspirates – the activities of one or more were depressed.
However, the findings of this particular study of Koch’s are difficult to accept. For example “of the 68 relatives of 41 cases of mucoviscidosis only 9 were free from symptoms, signs or laboratory evidence of the disease”. Also an article from the same author in 1959 entitled “Mucoviscidosis in adults, a very frequent dominant hereditary disease” (Bohn H Koch E. Die Mediz 1959; 4:1139-1149) does little to reassure one that the findings in the present paper are valid. Subsequent studies searching for undiagnosed CF in populations of patients with bronchiectasis and chronic bronchitis did not reveal patients with unrecognised cystic fibrosis (Muir et al, 1962 below). Although the findings in this paper are questionable when viewed in the light of subsequent publications, the possibility of encountering this new disease – CF – was being suggested to clinicians dealing with adults and other gastrointestinal and respiratory conditions.
1960 Green MN, Kulczycki LL, Shwachman H. Serum protein paper electrophoresis in patients with cystic fibrosis. Am J Dis Child 1960; 100:365-72. [PubMed]
Increased levels of gamma globulin, as determined by paper electrophoresis reflected the severity of the pulmonary disease. Subsequent studies confirmed the relationship of high immunoglobulin levels with severe chest involvement. The levels correlated with disease activity (Matthews WJ et al. N Eng J Med 1980; 302:245-249.[PubMed]); also a subgroup of children with lower immunoglobulin levels appeared to have a better prognosis when followed over 5 years (Wheeler WB et al. J Pediatr 1984; 104:695-699 below[PubMed]). Also later more specific qualitative immunoglobulin abnormalities were reported ascharacteristic of the condition such as low IgG2 (Garside et al, 2005; Garside et al, 2007 both below).
1960 Bruce GM, Denning CR, Spalter HF. Ocular findings in cystic fibrosis of the pancreas: a preliminary report. Arch Ophthalmol 1960; 63:391-401. [PubMed]

Fig 3. Carolyn Denning.
The authors became aware of complaints referable to impaired vision and abnormal fundal appearances in their patients in the summer of 1958 and they report the eye findings in 27 patients. Definite impairment of vision was noted in 4 of 10 patients. Characteristic findings were “varying degrees of engorgement and edema of the disc marked in some instances by haemorrhages and in others by cystic changes in the macula”. All those affected had severe pulmonary involvement and raised gammaglobulin levels in the serum and spinal fluid. A later report failed to provide an explanation for the eye changes possibilities including chronic hypoxia, hypercapnia, right heart failure, increased intracranial pressure, a bleeding tendency or some disturbance of serum globulins (Soc Pediatr Res 1960; abstract 127). In 1963 the effects of chloramphenicol were reported (Denning et al, 1963 below).
Dr Carolyn Denning (1927-2016) (figure 3) was one of the leading CF paediatricians at that time working first in New York with Dorothy Andersen and later at St Vincent’s Hospital in New York. In the figure 1 she is examining the hand print of a person with CF on a “Shwachman plate” (see N Eng J Med 1956:255:999-1001 above).
I was fortunate to visit her CF unit at St Vincent’s in the late Eighties, having been encouraged to do so by Ron Tucker the then Director of the UK CF Trust; he was very keen that I should visit her. Carolyn Denning was the first woman to chair the National Cystic Fibrosis Foundation’s Medical Advisory Council and was one of the first to organize and initiate a multidisciplinary team approach to management of the disease – this was very apparent when I visited her and her team at St Vincent’s, New York. A quote from the website “A Changing Face of Medicine” typifies her general approach – “My office visits,” she says, “are conducted in a private setting with no interruptions by telephone or office personnel with a one-hour minimum allotted to each patient. I am realistic yet optimistic, stressing the importance of hope. I am current on research activities in the field as well as other important relevant events. I follow through on all matters pertaining to the patient and his office visit and I am available by telephone at all times. I put great stress on personal integrity, ethics and moral beliefs. As director of a large, multi-disciplinary group of health professionals, I have worked hard to choose people who share the same philosophy.” It was good to see such an excellent team in action.
1960 Feigelson J. The treatment of mucoviscidosis or cystic fibrosis of the pancreas. Bull Mem Soc Med Paris 1960; 9:4-17.

Fig 4. Warren Warwick, John Dodge and Jean Feigelson. Author’s image
Jean Feigelson (1921 – 2017) (figure 4) of Paris is one of the pioneers of CF care and still a regular attendee at CF conferences in Europe and North America. He trained in paediatrics at the Sick Children’s Clinic in Oslo in 1952. In a career spanning over 45 years he has treated over 250 people with cystic fibrosis. This is Jean Feigelson’s first recorded paper on cystic fibrosis. His most recent is as a co-author of a paper on partial splenectomy, that was published in 2007 (Louis D et al, Pediatr Pulmonol 2007; 42:1173-1180). He has 48 references noted in Medline produced steadily over 40 years
“Jean Feigelson was a member of the French Resistance, war hero, Knight of the national order of the Legion of Honour, and holder of many other awards; in the times of peace he continued his fight against any injustice. He inspired doctors to fight for people suffering from cystic fibrosis, so that they could have a long and fulfilled life. He filled people with energy, self-confidence, and made them believe in the scientific potential of medicine – and this refers not only to his colleague doctors but also to patients from all over the world” (from Charitable Foundation “Ostrava”)
1960 Siegel B, Siegel S. Pregnancy and delivery in a patient with cystic fibrosis of the pancreas. Obstet Gynecol 1960; 16:438-440.
This was the first report of pregnancy in a lady with CF; the patient died six weeks after the birth. The authors concluded, “cystic fibrosis is seriously complicated by pregnancy”.
However, as the survival and condition of patients with CF improved, an increasing number of women with CF had successful pregnancies (Cohen et al, 1980 below; Gilliam et al, 2000 below; Edenborough et al, 2000 below), even some who had undergone lung transplantations (Gyi KM et al. J Cyst Fibros 2006; 5:171-175).
1960 Anderson CM. Histologic changes in duodenal mucosa in coeliac disease: Reversibility during treatment with wheat gluten free diet. Arch Dis Child 1960; 35:419-427. [PubMed]
This is the first report of per oral duodenal biopsy in 17 children with coeliac disease; 11 of whom were re-biopsied after taking a gluten free diet when all had improved histology. Eventually in patients considered to have coeliac disease and treated with a gluten free diet, it would become practice to re-biopsy to ensure the intestinal mucosa had recovered and at some stage later to re-challenge with gluten powder to ensure the gluten intolerance was permanent before committing the patient to a lifetime gluten free diet.
This report was some three years after the first report of per oral intestinal biopsy in adults by Margot Shiner (Sakula J, Shiner, M. Lancet 1957; ii: 876) and the first in children. It is an important paper both with regard to the management of coeliac disease and also important in improving the means of clearly differentiating between cystic fibrosis and coeliac disease; also rarely the coexistence of the two conditions could be identified (Hide & Burman, 1969 below). This recently introduced technique of per-oral duodenal biopsy permitted a positive diagnosis of coeliac disease for the first time (see comment on Samuel Gee,1888 above). The technique gradually became more generally available at major centres throughout the UK during the Sixties. (Please Note the author of this paper is Charlotte Anderson – not Dorothy H Andersen – the spelling is confused in more than one publication – even by the editor of a leading pediatric journal!!

Fig.5. Charlotte Anderson
Charlotte M Anderson (1915-2002) (figure 5) was the first woman to be appointed a Professor of Paediatrics in the United Kingdom. She qualified in 1945 and after hospital jobs in Melbourne she worked at the Hospital for Sick Children at Great Ormond Street, London and at the Institute of Child Health at the University of Birmingham. Her work with British colleagues on the role of gluten in coeliac disease (Anderson CM et al. Coeliac disease gastrointestinal studies and the effect of wheat flour. Lancet 1952; i: 836-842) was carried out at much the same time as that of Dicke and colleagues in Holland, and helped to establish her international renown. She started the first Australian cystic fibrosis clinic in 1953 in Melbourne and published widely on both CF and paediatric gastroenterology. She became Professor of Paediatrics at the University of Birmingham and director of the Institute of Child Health in 1968.
I was fortunate to hear Charlotte Anderson speak at the Samuel Gee 1988 Coeliac Centenary Meeting at St Bartholomew’s in London and, even more fortunate, to talk with her and Margot Shiner (the first person to perform per oral intestinal biopsy in children) over lunch time sandwiches – a memorable lunch for me!
1960 Young WF. Ototoxicity to neomycin aerosol. Lancet 1960; i: 1103.
Fig 6. Winifred Young
This letter to the Lancet from Winifred Young (1909-1969) (figure 6), of the Queen Elizabeth Hospital for Children, London, followed closely a report from the Royal National Throat, Nose and Ear Hospital, London, of two children with CF who had received nebulised neomycin for 34 months and 26 months respectively and who had become severely deaf (Fuller A. Ototoxicity of neomycin aerosol. Lancet 1960; i: 1026). Winifred Young responded that the patients were part of a series of children treated at her CF clinic at the Queen Elizabeth Hospital for Children, London and both the children had very severe chest involvement – in fact, both had since died. Dr Young and her otological colleagues “had been able to reassure herself that neomycin aerosol can be used for many months without risk of ototoxicity”.
Despite this reassurance, the use of long term nebulised neomycin was eventually abandoned due to ototoxicity – at that time it was not appreciated that inhaled antibiotics could be absorbed in significant amounts. Inhaled neomycin was first described as a treatment for CF in 1956 (Gibbs GE & Raskin J. Antibiotic Med Clin Therapy 1956; 2:332-336.). A case report of ototoxicity appeared in 1959 (Greenwood GJ. AMA Arch Otolaryngol 1959; 69:390-397) and in a number of reports in the early Sixties although most reports of ototoxicity and CF concern the aminoglycosides.
1960 Ruben BL, Crigler JF Jr, Berenberg W, Shwachman H. Hypothyroidism: a complication of iodide therapy in children with chronic respiratory involvement of cystic fibrosis. Am J Dis Child 1960; 100:721-722.
This report is of two children with CF who developed hypothyroidism whilst taking iodide therapy to improve sputum clearance – in these two patients there was no thyroid enlargement. Later Dolan TF & Gibson LE (J Pediatr 1971; 79:684-687) reported 55 patients on long term iodide therapy of whom a remarkable 85% developed goitres and also 24% had evidence of hypothyroidism. Their thyroid glands were enlarged, sometimes markedly so, usually after three years or so of iodide therapy. There was discussion as to the possibility of an intrinsic defect of thyroid function but people with CF not taking iodides were all euthyroid.
– Suggest see Endocrine section in “Topics” for further information and image)
1960 Zegarelli EV, Denning CR, Kutscher Tuoti F, di Sant’Agnese PA. Discolouration of the teeth in patients with cystic fibrosis. Pediatrics 1960; 26:1050.
There was severe discoloration of the teeth in 38 of 52 children and adolescents with CF. In 31 the deciduous teeth were involved, the permanent teeth in 18 and both in 11. The authors noted that tetracycline had been involved in animals and speculated that antibiotic therapy “might conceivably contribute to the discolouration by deposition in the teeth”. In 1959 Shwachman et al. had recognised tooth staining (Antibiot Ann 1958-1959, 692-699) (Shwachman et al, 1958 above). Subsequently Zegarelli, usually with Carolyn Denning of New York, published 11 papers on tooth discoloration. Tetracycline is deposited in growing bone and teeth by complexing with the bone mineral (Witkop CJ, Wolf RO. JAMA 1963; 185:1008-1011). Subsequently tetracyclines were avoided in children under seven years of age and also by pregnant women.
The dangers of some drugs taken by the mother during pregnancy were becoming apparent at this time – particularly the thalidomide tragedy which came to light in the early Sixties after over 10,000 infants had been born with various limb deformities between 1956 and 1962 as a result of their mothers taking the drug during pregnancy.
1961 Alagille D, Vinh Le Tan. Hepatic localizations of mucoviscidosis. Tijdschr gastro-enterol 1961; 4:435-454.

Fig. 6a Daniel Alagille EASL website
The incidence of hepatic cirrhosis varies in different reports but all agree the complication increases with age. In 200 people with CF, “cirrhosis” occurred in 1% aged less than 3 months, 6% between three and 12 months, 11% one to three years, 37% over three years of age. Histologically there was a focal biliary cirrhosis, diffuse multilobular cirrhosis and/or portal hypertension. The lesson the authors took from their findings was that “Investigation of the young cirrhotic patient is incomplete without a sweat test” – which is still sound advice today.
Daniel Alagille (1925-2005) (fig. 6a) was a distinguished French paediatrician and expert on liver disease. He published over 500 articles and several books. He was chief editor of the Revue internationale d’hépatologie (1954-1971) and Archives françaises de pédiatrie (1964-1990).Alagille’s syndrome is an inherited condition in which bile builds up in the liver because there are too few bile ducts to drain the bile. This results in liver damage.
1961 Huhnstock K, Schwarz G. On mucoviscidosis in adults and diabetes mellitus. Klinische Wochenschrift 1961; 39:854-7.[PubMed]
These authors screened 250 adults with diabetes mellitus using Shwachman plates (Shwachman et al, 1956 above) and those who were positive had sweat tests performed by the bag method. Nine of the 250 diabetic adults had positive sweat tests but no other signs of cystic fibrosis.
These findings are difficult to explain, and indeed accept, as diabetes mellitus is usually a late feature in the progression of cystic fibrosis. Also the ages of the patients (between 49 and 66 years) were quite against their having cystic fibrosis. So it is difficult to accept these findings particularly as there were no other signs of cystic fibrosis in these middle aged patients. Also, a number of authors had found some apparently healthy adults with sweat tests with values of sodium and chloride over 60 meq/l. This paper was followed by a number of publications on the relationship between established diabetics and cystic fibrosis. The first description of diabetes mellitus in cystic fibrosis is usually attributed to Shwachman & Leubner, 1955 (above).
1961 Elian E, Shwachman H, Hendren WH. Intestinal obstruction in the newborn infant; usefulness of the sweat electrolyte testing differential diagnosis. N Eng J Med 1961; 264:13-16. [PubMed]
The authors managed to perform pilocarpine iontophoresis sweat tests in the first four days of life in 37 babies- a difficult feat at this early age. Another six newborns with intestinal obstruction were tested – the four with CF were all sweat test positive and the two with negative sweat tests had respectively Hirschprung’s disease and ileal atresia.
So sweat tests were already positive in the newborn period in infants with CF but an experienced and skilful technician would be required to perform the investigation. If an urgent answer is required at the present time, a check on the infant for the presence of CF mutations would be helpful in most instances
1961 Shwachman H, Antonowicz I, Stern M. The sweat tests in cystic fibrosis. Am J Dis Child 1961; 102:769.
An interesting report where Shwachman describes performance of over 2000 “bag” sweat tests – 335 in patients with CF. The mean chloride level in people with CF was 113 meq/l and mean sodium 112meq/l compared with controls’ values of 23 and 23 respectively. The bag method was abandoned in 1958 in preference to the pilocarpine method of Gibson and Cooke (1959 above) with which the bag results were compared.
1961 Kunstadter RH, Mendelsohn RS. Norethandrolone in children with and without cystic fibrosis of the pancreas. Illinois M J 1961; 120:156-161. [PubMed]
In 1961 as the chest infection progressed and increased in severity, it was very difficult, and usually impossible, to achieve normal weight gain and growth in children with cystic fibrosis. As the available pancreatic enzyme supplements were relatively inefficient, most patients took a low fat diet to avoid very unpleasant bowel symptoms; also there was a severe catabolic wasting effect from the active and increasingly severe chest infection. However, in this report of 14 children with CF treated with anabolic steroids there were “remarkable gains in weight”.
Shwachman commented that he had used one such preparation (Nilevar) on 30 patients and found the drug “very useful but not to be used routinely”. This was the first of a number of reports that anabolic steroids had a favourable effect on weight gain in children with cystic fibrosis. The drugs were to become quite widely used as nutritional problems became increasingly severe as more children survived for longer and nutrition continued to be an increasingly significant problem. It was not until the early Eighties that there was marked improvement in the control of the intestinal malabsorption following the introduction of the acid resistant enzymes (Pancrease and later Creon); also around that time, for those with more severe nutritional problems, more aggressive nutritional interventions such as nasogastric and gastrostomy feeds, became available. So the use of anabolic steroids gradually declined (also Dooley RR et al. J Pediatr 1969; 74:95-102).The subject was reviewed in 1981 by Richard Dooley (Anabolic steroids. In 1000 years of Cystic Fibrosis. Warren Warwick (ed). University of Minnesota, 1981).
1961 Shwachman H, Kulczycki LL, Mueller HL. Nasal polyposis in patients with cystic fibrosis. Am J Dis Child 1961; 102:768-769.
An early description of nasal polyps in cystic fibrosis (also see Lurie MH, 1959 above). Of 650 patients with CF seen over the previous 4 years, 43 (7%) had nasal polyposis – 10% of those over 3 years. The effect on facial appearance, increasing the width of the nasal bridge, and the tendency to recur after removal were stressed. There was nothing characteristic about the histological appearance of the polyps. A sweat test was recommended in any child with nasal polyposis.
1962 Shwachman H. Kulczycki LL, Mueller HL, Flake CG. Nasal polyposis in patients with cystic fibrosis. Pediatrics 1962; 30: 389-401. [PubMed].

Fig. 6b Nasal polyp in CF
Nasal polyposis occurred in 50 (6.7%) of 742 patients with CF in those with allergies and those without.
-Later more accurate assessment of the incidence of polyps was possible with fibreoptic instruments indicating that 37% of patients were affected. Inhaled steroids were used with some success as local treatment – eventually many years later confirmed in a controlled trial (Hadfield et al, 2000 below). Also, as an incidental finding during a trial of oral ibuprofen for the chest infection, the nasal polyps were observed to shrink (Lindstrom et al, 2007 below).
1961 Levin S, Gordon MH, Nitowsky HM, Goldman C, di Sant’Agnese P, Gordon HH. Studies of tocopherol deficiency in infants and children. VI. Evaluation of muscle strength and effect of tocopherol administration in children with cystic fibrosis. Pediatr 1961; 27:578-588. [PubMed]
This is said to be the first randomized controlled trial in people with cystic fibrosis. A double blind placebo controlled parallel single centre randomised controlled trial in which the effect of tocopherol supplementation on muscle strength was evaluated, by means of a “hand bulb ergograph” which was squeezed to measure grip strength. There was no difference in strength noted with vitamin E supplementation – both the treated and placebo group improved.
Oppenheimer had been the first to report an infant with necrotic changes in muscle resembling those found in tocopherol deficiency (Oppenheimer. EH. Bull Johns Hopkins Hosp 1956; 98:353-358). The authors of the present studies concluded that “although the present study did not demonstrate a clinical functional effect of tocopherol therapy in patients with cystic fibrosis, its administration is recommended because of previously reported biochemical and pathological evidence of vitamin E deficiency in these subjects”.
– This very reasonable approach would be a lesson for some clinicians who would never use a treatment unless supported by a suitable randomised controlled trial – a view I have even heard expressed with regard to vitamin E supplements in CF! Here all the available reasonable information was considered before a policy was recommended that may well do good and was very unlikely to do harm to their patients.
1961 Shahidi NT, Diamond LK, Shwachman H. Anemia associated with protein deficiency. A study of 2 cases with cystic fibrosis. J Pediatr 1961; 59:533-42. [PubMed]
There was a fall in serum albumin from 4.0 to 2.6 g/dl over 30 days in an infant with CF fed a soy formula. The normal half life of 131I-labelled albumin excluded an exudative protein loosing enteropathy. The authors suggested that in CF infants soy protein absorption is more affected than cow’s milk protein.
Usually serum albumin is, rather surprisingly, within the normal range in CF unless there is significant liver involvement. However, it became apparent in a number of subsequent reports that soya based milk preparations were particularly likely to be associated with hypoproteinaemia in infants with cystic fibrosis and should be avoided. If cows milk intolerance is suspected a hyrolysed protein preparation, rather than a soy formula, should be used (Fleisher et al, 1964 below; McClean &Tripp, 1974 below; Lee et al, 1974 below)
1962 Rosan RC, Shwachman H, Kulczycki LI. Diabetes mellitus and cystic fibrosis of the pancreas. Laboratory and clinical observations. Am J Dis Child 1962; 104:625-34. [PubMed]
One of the early descriptions of diabetes mellitus in cystic fibrosis; the first was in 1955 in an article by Shwachman & Leubner (above). In the present paper 10 patients with diabetes mellitus were identified in a CF population of about 1300 patients seen since 1947 – one adult, three teenagers and the rest children. Reviewing the 10 patients – eight required insulin therapy, they noted that diabetes complicates management but does not necessarily shorten survival; it may begin at any age; four of the 10 patients were mentally retarded – an unusual occurrence in CF which was not discussed; the complication was indistinguishable from juvenile diabetes except ketosis was very rare; all were completely pancreatic insufficient.
The authors predicted that subclinical diabetes must exist in a large proportion of people with CF. This prophetic observation was absolutely correct but was a new concept at the time as there were very few adults with cystic fibrosis. There were so few patients with diabetes mellitus and CF that this paper reporting 10 patients was published.
1962 Muir D, Batten J, Simon G. Mucoviscidosis and adult chronic bronchitis. Their possible relationship. Lancet 1962; i: 181-3.[PubMed]
Fig. 6c David C F Muir RCP Museum
One hundred adults with chronic bronchitis, 42 patients with other chest diseases and 25 controls were screened with the fingerprint method for raised chloride levels in the sweat (method of Shwachman & Gahm, 1956 above). None of the patients had excessive sweat chloride levels as judged by the plate test and the authors concluded that cystic fibrosis, in the homozygous state, could not be implicated as a cause of their chronic bronchitis.
It was reasonable to search for people with CF amongst those with similar chronic disorders. However, in the Sixties survival into adult life was unusual. As in the present study, usually there were no patients with CF amongst the patients studied. Later this group, at the Royal Brompton Hospital in London, also failed to find an increase in respiratory disease amongst obligate heterozygotes for CF – that is to say the parents of people who had cystic fibrosis (Batten et al, 1963 below)
Dr David Muir (1931-2021) was at this time completing a PhD on the behaviour of fine aerosol particles in the lung. His early physiological research into airborne particles led him to a career in occupational medicine in Scotland and then McMaster university in Canada, where he became a leader in the profession.
1962 McKendrick T. Sweat sodium levels in normal subjects, in fibrocystic patients and their relatives and in chronic bronchitis patients. Lancet 1962; I: 183-186.
A study by Dr Tom McKendrick (figure 7), when a senior registrar working at Great Ormond Street, London with Dame Barbara Clayton, the chemical pathologist, and Dr Archie Norman, using the recently described Gibson and Cooke pilocarpine iontophoresis method of sweat stimulation (Gibson & Cooke, 1959 above). In normal children sweat sodium was almost always less than 60 meq/l rising from 22 to 44 in the first 14 years and rising to 55 in adults.
95% of people with CF had sodium levels over 70 and parents and siblings showed levels slightly greater than normals. The levels were normal in chronic bronchitis patients i.e. there were no people with CF amongst those considered to have chronic bronchitis.
The conclusion was that the “The wide variation of results both in single subjects and within groups of similar subjects limit the value of the test. It is useful only for confirming the diagnosis of cystic fibrosis” – for which, of course, it proved of immense value and to be a major advance, eventually becoming the “gold standard” method of sweat testing.
1962 Jensen KG. Meconium ileus equivalent in a 15-year old patient with mucoviscidosis. Acta Paediatr Scand 1962; 51:344-345. [PubMed]
This report, often incorrectly quoted as first description of “meconium ileus equivalent”, describes the condition in a boy aged 15 years – however, it was the first time the term “meconium ileus equivalent” was used. Already Levy (1951 above) and Fischer (1954 above) and others had reported post neonatal intestinal obstruction in CF children. Also Fanconi (Helvet Paediat Acta 1960; 15:566-579) had used the term “post-neonatal meconium ileus”. This present patient of Jensen’s had an ileostomy through which pancreatin was infused which relieved the obstruction.
1962 Esterly JR, Oppenheimer EH. Observations in cystic fibrosis of the pancreas. I. The gallbladder. Bull Johns Hopkins Hosp 1962; 110:247-55. [PubMed]
First description of gall bladder abnormalities noted at autopsy that were present in 24 of 72 people with cystic fibrosis. “The cystic duct may be atretic or stenotic from inspissated mucus or mucosal hyperplasia. Mucus distends the gallbladder epithelial cells and fills the lumen with a colourless secretion. The gallbladder may atrophy or persist as a thin walled cyst lined with flattened mucosa”. Radiological appearances of the gall bladder and bile ducts had been reported by Jones et al, 1958 (above).
1962 Andersen DH. Pathology of cystic fibrosis. Ann NY Acad Sci 1962; 93:500-517.
In this publication Dorothy Andersen reported that the lungs of CF infants were normal at birth. Others agreed that the lungs were “essentially normal” at birth (Zuelzer WW & Newton WA. Pediatrics 1949; 4:53-59. [PubMed]). However, others later found that there is an accumulation of mucin in the tracheobronchial glands of the fetus with CF even in the second trimester (Ornoy A et al. Am J Med Genet 1987; 28:935-947). [PubMed] and in the post natal period, even before infection occurs, changes are present in the submucosal glands (Oppenheimer EH, Esterly JR. Perspect Pediatr Pathol 1975; 2:241-278. [PubMed]). Under four months of age there is some slight dilatation of the acini of the tracheal submucosal glands but gland development and architecture are normal (Sturgess J, Imrie J. Am J Pathol 1982; 106:303-311. [PubMed]).
Despite these findings, which led to very slight hyperinflation of the lungs, for practical purposes the respiratory function is within the normal range and can be maintained in a stable state with little or no deterioration for many years provided chronic infection can be prevented by early diagnosis, careful microbiological monitoring and early aggressive antibiotic treatment.
1962 Webb WR. Clinical evaluation of a new mucolytic agent acetyl-cysteine. J Thorac Cardiovasc Surg 1962; 44:330-343. [PubMed]
Acetyl cysteine, a derivative of the amino acid cysteine, is a drug that subsequently was widely used for CF in Europe but never popular in the UK. Here experience is reported of 285 patients with a variety of suppurative pulmonary conditions and “revealed it to be extremely effective with almost no associated complications. Seven patients with CF improved over 10 months with either inhalations or sleeping in a tent with the drug nebulised with saline and propylene glycol”. (figure 8).
Apparently N-acetylcysteine and other sulphydryl compounds act by depolymerising mucus in vitro by breaking disulphide bonds of the glycoproteins thereby lowering the viscosity (Sheffner AL. Ann N Y Acad Sci 1963; 106:298-310. [PubMed]).

Fig 8. 24 hour sputum collection from a man with purulent bronchitis during the day prior to and 4 days subsequent to starting Acetyl cysteine
This paper contains a useful summary of all the many side effects of animal-derived trypsin and enzymatic treatments used to liquefy sputum – contrasted with the minimal side effects experienced with N-acetylcysteine. Interestingly there has been a renewal of interest in acetyl cysteine in the Millennium and the drug has been used both for respiratory (6.5% of USA patients with CF take inhaled acetyl cysteine) and gastrointestinal problems in CF (Lillibridge CB et al. Oral administration of n-acetyl cysteine in the prophylaxis of “meconium ileus equivalent” J Pediatr 1967; 71:887-9; Gracey M et al. Treatment of abdominal pain in cystic fibrosis by oral administration of n-acetyl cysteine. Arch Dis Child 1969; 44:404-405).
More recently the relation to glutathione, in particular, has featured in recent references as N-acetylcysteine is an effective precursor of cysteine for tissue glutathione synthesis. Apparently CFTR is responsible for glutathione transport and there may be intracellular accumulation of glutathione in cystic fibrosis (Childers M. Medical Hypotheses 2007; 68:101-102.)
1962 Denton R. Bronchial secretions in cystic fibrosis. The effects of treatment with mechanical percussion vibration. Am Rev Respir Dis 1962; 86:41-6. [PubMed]
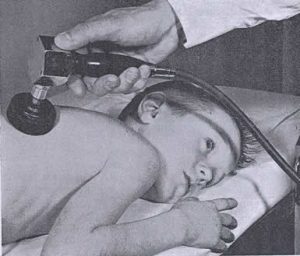
Fig 9. Percussor in use, From Denton 1962
One of many publications by Dr Robert Denton from Philadelphia. As the effect of chest clapping and vibrations was considered to be helpful in moving bronchial secretions, the effect of rapid repetitive percussion with a mechanical device was examined in 23 patients with CF who had moderate and marked pulmonary involvement.
His study with a mechanical percussor (figure 9) is complex and impressive, even involving a “control percussor” that did not vibrate. Over a 12 minute period, there was a significant increase in secretions produced with the percussor + vibrations compared to percussor with simulated vibrations and unassisted postural drainage; this was significant in 19 of the 23 patients although the vital capacity did not change significantly.
This was the first of a number of papers on mechanical percussion as an aid to chest physiotherapy. Some years later in the UK the “Salford percussor” (Maxwell & Redmond, 1979 below; Flowers et al, 1979 below) received a cool reception from the UK physiotherapists. However, the delivery of vibrations by a jacket or vest eventually became part of standard approved therapy in the USA thanks to the work of Warren Warwick (Warwick & Hansen, 1991 below). Again this more recent mechanical aid, “the Vest”, was slow to find favour with physiotherapists in the UK!
1962 Kuo PT, Huang NN, Bassett DR. The fatty acid composition of the serum chylomicrons and adipose tissue of children with cystic fibrosis of the pancreas. J Pediatr 1962; 60:394-403. [PubMed]
The first study of fatty acids in blood and tissue lipids of patients with CF. The fatty acid composition of chylomicrons and adipose tissue from children with CF who had variable degrees of fat malabsorption was compared with the values from controls. There was a relative decrease in linoleic acid and increased palmitoleic and oleic acids. Subsequently the abnormalities have been explained as related to liver disease, the basic defect and the intestinal malabsorption.
Prof. Bob Elliott and colleagues from New Zealand published several papers showing improvement in the clinical state with supplements of medium chain triglycerides even to the extent of returning the sweat electrolytes to nearer normal values (Elliott RB. Aust Paediatr J 1972; 8:217. below; Elliott RB, Robinson PG. Arch Dis Child 1975; 50:75-78; Elliot RB. 1976; 57:474-479). However, subsequent studies failed to substantiate their findings (Davidson GP et al. Aust Paediatr J 1978; 14:80-82. [PubMed] ; Chase et al. Pediatrics 1979; 59:428-432 below).
1962 Barbero GJ, Sibinga MS. Enlargement of the submaxillary glands in cystic fibrosis. Pediatrics NY 1962; 29:788-793. [PubMed]

Fig 10. Enlarged submandibular glands in cystic fibrosis
This is the first report of enlarged submandibular glands in CF – a feature which is sometimes quite marked (figure 10). During their studies on secretory activity of the salivary glands the authors noted many patients had enlarged submandibular glands. The submandibular glands of 300 normal children, 106 with CF and 20 with chronic pulmonary disease were examined. Enlarged submandibular glands were palpated in 92% of children with CF and only 2% of healthy controls and those with chronic pulmonary disorders. The presence of enlargement can be helpful when considering a diagnosis of CF.
1962 Wallman IS, Hilton HB. Teeth pigmented by tetracycline. Lancet 1962; i: 827-829. [PubMed]
A report from the Princess Margaret Hospital for Children, Perth, Australia. This is one of the early reports of “tetracycline teeth”, although the authors noted that Shwachman had described tooth discolouration in 40 of 50 children who had long term treatment with tetracycline (Antibiotics Annual. New York. 1958:692). (also Zagaralli et al, 1960 above and 1963 below).
The present authors noted pigmentation of infant’s teeth at a maternity hospital follow-up clinic; many of those affected had not been jaundiced – the usual explanation given for tooth discolouration. The co-author Hilton had previously observed skeletal pigmentation with tetracycline, so the possibility of a relation to tetracycline administration was investigated. 50 out of 64 babies had received tetracycline in the newborn period and 46 had yellow or brown pigmentation of their teeth with or without enamel hypoplasia. The more tetracycline, the greater the change in tooth colour. Earlier Buyske et al had noted bone pigmentation by tetracycline and chlortetracycline in animals (Buyske DA et al. J Pharmacol Exp Ther 1960; 130:150-156. [PubMed]).
1962 Shwachman H. The sweat test. Pediatrics 1962; 30:167-171.[PubMed]
A commentary on the relatively recently described sweat test by Harry Shwachman and the article is full of really good advice for the clinician. While the sweat test is specific for CF Shwachman emphasised that the following factors were crucially important in diagnosis. Maintaining a high degree of suspicion noting the great variability of the disease; the presence of elevated electrolytes alone does not establish the diagnosis; many factors influence the result – not least the experience of the laboratory; diagnosis should not be made lightly but only after careful appraisal of the patient, the family history and laboratory evidence. Heterozygotes cannot be detected with the sweat test.
One suspects that over diagnosis was a relatively common problem in Shwachman’s experience due false high values of sweat electrolytes – this article discusses some of the confounding and other factors that affect the test. A key publication from Charlotte Anderson’s unit in the UK first documented the frequent over diagnosis of the condition in the UK (Smalley et al, 1978 below) and was of great importance in alerting UK paediatricians to the problem.
1962 Pileggi A. Cystic Fibrosis in a negro. Del Med J 1962; March:97-98. [PubMed]
A black infant admitted with bronchopneumonia at 8 months was diagnosed by three positive sweat tests as having cystic fibrosis. He died after 37 days. At autopsy, in addition to bronchopneumonia, the pancreas showed typical changes of cystic fibrosis. The authors note that at the Babies Hospital New York only 2 children of 397 cases were black infants an incidence of approximately 0.5% (di Sant’Agnese Am J Med 1956; 21:406).
1962 Polgar G, Denton R. Cystic fibrosis in adults. Studies in pulmonary function and some physical properties of bronchial mucus. Am Rev Respir Dis 1962; 85:319-327. [PubMed]
Fig 11. George Polgar
One of many respiratory studies by George Polgar (figure 11) one of the early respiratory paediatricians. At this time only 2% of people with CF were over 20 years of age. Two of the 4 adults studied died and were autopsied. In all the recognition of CF had been only after years of illness. Interestingly the use of hypertonic saline was mentioned as causing “symptomatic improvement” – eventually, some 40 years later, this was confirmed in a large trial (Elkins et al, 2006 below). Functional abnormalities were: airway obstruction, stiffening of the lungs, increased arterial carbon dioxide and reduced arterial oxygen saturation. The authors concluded the primary cause of the respiratory disease was obstruction of the airways secondary to impaired flow of abnormal bronchial mucus. They suggested that the practical conclusion would be to search for methods that could be used for mobilisation of the mucus from the airways.
Subsequently such treatments as hypertonic saline or rhDNase (Pulmozyme) proved to be an effective means of improving and preserving lung function.
1963 Pino G, Conterno G, Colongo PG. Clinical observations on the activity of aerosol colomycin and of endobronchial instillations of colomycin in patients with pulmonary suppurations. Minerva Medica 1963; 54:2117-2122. [PubMed]
One of the early reports of colomycin, administered as an aerosol, achieving “satisfactory blood levels”. Reference is also made to Mensi E (1958) in this paper. Colomycin has had three phases of popularity in treating people with cystic fibrosis.
Phase 1.As Gram negative infections, including Pseudomonas aeruginosa (Ps. pyocyanea as it was then), became more of a problem during the Sixties, intramuscular colomycin was the only effective injectable antibiotic. Robert Stern recalls how, in the early Sixties, he first started infusions of intravenous colomycin in Cleveland prompted by the extreme pain of the intramuscular injections in an emaciated girl with CF who already had an IV infusion running for hydration purposes. The IV route gradually replaced the painful IM route particularly when carbenicillin became available in 1968. However, when gentamicin became available in 1968 this drug replaced colomycin as first line treatment for P. aeruginosa in people with cystic fibrosis.
Phase 2. Interest revived in nebulised colomycin following the short report from Leeds (Littlewood et al, 1985 below) of the successful eradication of early colonisation with P. aeruginosa in CF using nebulised colomycin – an observation later confirmed in Copenhagen (Valerius et al, 1991, below) and a number of other small studies from Europe. According to Hoiby, nebulised colomycin was also introduced into the treatment of chronically infected patients in Copenhagen in 1987 on the strength of the initial report from Leeds. It is interesting that none of these early reports were accepted in the USA (even the excellent trial of Valerius et al, 1991 with its striking results) and it was some 15 years before early eradication of P. aeruginosa became widespread in the USA.
Phase 3. As most resistant P. aeruginosa remained sensitive to colomycin, the intravenous use was again evaluated for strains of the organism which had become resistant to other antibiotics; it was found to be effective with an acceptable level of side effects (Conway et al, 1997 below).
There was a detailed multi-author ten year review of Colomycin and its role in the treatment of CF published in 2000 (Littlewood JM et al. Respir Med 2000; 94:632-640 below)
1963 Rubin LS, Barbero GJ, Chernick WS, Sibinga MS. Pupillary reactivity as a measure of autonomic balance in cystic fibrosis. J Pediatr 1963; 63:1120-1129. [PubMed]
There was considerable interest in possible abnormalities of the autonomic nervous system considered to be in some way related to the basic defect. The authors found significant differences in the pupillary reactivity between people with CF and controls.
Holzel in Manchester had found normal levels of acetyl cholinesterase in various tissues and concluded any cholinergic over-stimulation was not due to absence of the hydrolysing enzyme (Holzel A et al. Lancet 1962; i: 822-823 above). Autonomic abnormalities were later confirmed by Davies et al, (N Eng J Med 1980; 302:1453-1456 below) and more recently were reviewed by Mirakhur A et al. (J R Soc Med 2003; 96 Suppl 43:11-17. below).
Although there was considerable interest in autonomic abnormalities this knowledge does not appear to have made any contribution to either the treatment or the understanding of the basic defect. There was a later report of excessive finger wrinkling in people with CF when their fingers were immersed in warm water and this phenomenon has been related to autonomic function (Elliott, 1974 below). In recent years there has been a renewed interest in finger wrinkling in people with CF.
1963 Denning CR, Bruce GM, Spalter HF. Optic neuritis in chloramphenicol treated patients with cystic fibrosis. J Pediatr 1963; 63:878.
The first report of optic neuritis in four children with CF on long term chloramphenicol – a complication which had been reported first in 1952 by Wallstein & Snyder (1952 above) in a woman with inflammatory bowel disease who after five months developed optic neuritis and peripheral neuritis. Later a number of reports in people with CF were reviewed by Harley RD et al (Trans Am Acad Ophthalmol Otol 1970; 74:1011-103). Numbness and tingling of the peripheries preceded the ocular signs which appeared to be related to the total dose received. It was suggested that 25 mg/kg/day for not more than 3 months was relatively safe. Fortunately, visual acuity usually recovered soon after stopping the drug but the problem may recur if treatment was resumed. (Also Huang N et al. J Pediatr 1966; 68:32-44).
1963 Lobeck CC, McSherry NR. Response of sweat electrolyte concentrations to 9 alpha-fluorohydrocortisone in patients with cystic fibrosis and their families. J Pediatr 1963; 62: 393-398. [PubMed]

Fig 12. Charles Lobeck
Patients with CF failed to show a significant decrease in their sweat electrolytes after administration of oral 9-alpha fluorohydrocortisone (3.0 mg per square meter for two days). Parents, siblings of people with CF and controls all had a significant decrease in the concentration of their sweat electrolytes after this challenge – for example the fall in chloride in parents was – 40.8%, in controls – 43.6%, in siblings -35.6%, but people with CF only had -1.1% reduction in their sweat chloride level.
This was a practically useful paper when there was a problem with diagnosis and there was a marginal sweat test result – particularly pre-1989 before genetic mutations could be determined. We used the test on a number of occasions and found it to be helpful when the diagnosis was in doubt and the sweat test result borderline with chloride values of around 50 – 70 meq/l. Margaret Hodson also found the fludrocortisone suppression test useful in adults with marginal sweat test results (Hodson ME et al. BMJ 1983; 286:1381-1383.[PubMed]).
Dr Charles Lobeck (1926 -2012) (figure 12) was a distinguished paediatrician at both Wisconsin then the Missouri School of Medicine and finally back in Wisconsin. In between his administration work and clinical duties as a paediatrician, Lobeck conducted basic and clinical research on cystic fibrosis. He was instrumental in creating and leading the U.S. Cystic Fibrosis Foundation and for many years was closely involved with that organisation. Paul Sant’Agnese recalls that Lobeck was one of the few people who further explored his discovery of the sweat abnormalities and worked in this aspect with John Mangos. He had a major influence in raising the standard of CF research.
He contributed a very interesting chapter to Carl Doershuk’s book (“Center Directors Remember: Madison”. Charles C Lobeck. Chapter 24 in Cystic Fibrosis in the 20th Century. CF Doershuk Ed. AM Publishing. 2002) and was obviously a major influence in the CF scene in N. America for many years.
1963 Parkins RA, Eidelman S, Rubin CE, Dobbins WO III, Phelps PC. The diagnosis of cystic fibrosis by rectal suction biopsy. Lancet 1963; 38:851-6. [PubMed]
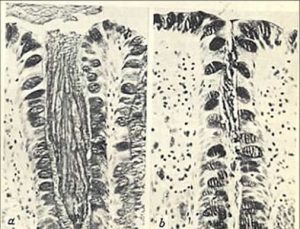
Fig 13. Rectal mucosa -left cystic fibrosis, right normal. From Parkins et al, 1963
An interesting paper by workers with extensive experience in rectal biopsy. The histological picture was characteristic of CF in many patients. When the histological picture of rectal “mucosis” is present it is specific for CF as shown here (figure 8) and it cannot be confused with any other rectal condition. It was not clear as to the proportion of cases of CF could be diagnosed with certainty – six of 11 patients with CF examined in this study showed definite diagnostic changes. Understandably, rectal biopsy never became popular as an additional diagnostic aid for CF; although ion transport abnormalities in the rectal mucosa were described in number of later studies (Veeze et al, Gatroenterology 1981; 101:398-403; Hardcastle et al, 1991 below).
1963 Batten J, Muir D, Simon G, Carter C. The prevalence of respiratory disease in heterozygotes for the gene for fibrocystic disease of the pancreas. Lancet 1963; i: 1348-1350. [PubMed]

Sir John Batten
The incidence of chronic bronchitis in parents of people with CF (obligate heterozygotes) and controls was similar to that reported for the general population – which was remarkably high at that time being 17% of men aged 40-60 years and 8% in women. The authors concluded that “the heterozygous state for fibrocystic disease of the pancreas could not be implicated as an important cause of chronic chest disease or of peptic ulceration”. These results agreed with those of Anderson et al. Med J Aust 1962; 1:965.
These results may not apply today as chronic bronchitis was remarkably common in the general population in the Sixties due to both atmospheric pollution and tobacco smoking.
1963 Lloyd AV, Grimes G, Khaw KT, Shwachman H. Chloramphenicol for long-term therapy of cystic fibrosis. JAMA 1963; 184:1001-6. [PubMed]
Report of more than three years of daily chloramphenicol in patients with CF without toxic effects in 50 patients studied and in post mortem records of 23 others. Later one fatal case of aplastic anaemia was encountered.(also Denning et al, 1963 above; Huang et al. 1966).
1963 Rick W. Untersuchung zur exokrinen function des pancreas bei zysticher pancreas-fibroses. (Pancreatic exocrine function in CF of the pancreas). Medizinische Welt 1963; 42:2158-9.
An early report of pancreatic function in CF showing reduced volume and reduced bicarbonate secretion. (Quoted by Wong LT et al, Gut 1982; 23:744-750.[PubMed]). Also pancreatic function was reported by Maddock et al, 1943 (above), Kopleman et al, 1985 (below) and Hadorn et al, 1968 (below). Hadorn’s work seemed to have had more impact (possibly as published in English) and is generally regarded as making the major contribution to pancreatic function testing in people with cystic fibrosis.
1963 Reas HW. The effect of N-acetylcysteine on the viscosity of tracheobronchial secretions in cystic fibrosis of the pancreas. J Pediatr 1963; 62:31-5. [PubMed] (Also Reas HW. South Med J. 1963; 56:1271-1278.[PubMed]).
Viscosity measurements were determined on secretions obtained via tracheotomies from 2 patients with CF with the use of N-acetylcysteine aerosol which produced a greater fall in the viscosity of the secretions than did a control aerosol (also Webb 1962 above). The authors suggest that “The combination of this safe method of mucolysis with energetic postural drainage and physiotherapy may be very rewarding in the easier removal of retained pulmonary secretions”. (Also Suddarth SB. Acetylcysteine a new and effective mucolytic agent. Bulletin – Grainger Medical Center 1963; 15:65-69 above; Meeker IA Jr, Kincannon WN. Acetyl cysteine used to liquefy inspissated meconium causing intestinal obstruction in the newborn. Surgery, St Louis 1964; 56:419-425).
– – Obviously at the time there was considerable interest in this new mucolytic agent whose free sulphydryl group reduced the disulphide linkages of mucoproteins. Subsequently it was the subject of a number of publications in liquefying sputum, improving abdominal pain and treating meconium ileus but never became popular in the UK as part of the pulmonary treatment. Although a subsequent review found no evidence of benefit (Duijvestijn YC, Brand PL. Acta Paediatr 1999; 88:38-41.[PubMed]), Ratjen et al (Eur J Pediatr 1985; 144:374-378. [PubMed]) found in a 12 week oral trial of NAC, ambroxal and placebo that “although no clinical differences could be observed between the three groups, significant impairment in the placebo group was found for trapped air and FEV1 when compared to the active groups, suggesting a therapeutic effect of ambroxal and NAC in CF”. More recently the relation to glutathione has caused renewed interest in the drug which, when given orally in high doses, provides a source of glutathione and apparently reduces airway inflammation (Tirouvanziam R, et al. Proc Nat Acad Sc 2006; 103:4628-4633.[PubMed]).
1963 Huang NN, Sproul A, Promadhattavedi V, High RH. Long-term therapy with oxacillin in patients with cystic fibrosis. Antimicrob Agent Chemother 1963; 54:667-672. [PubMed]
A short anecdotal report of long term use of oxacillin (an anti-Staphylococcal antibiotic available since 1962) in 15 patients with CF many of whom were receiving other antibiotics – mainly chloramphenicol. However, it did show that oxacillin was safe and that resistance on the part of S. aureus did not develop even after prolonged use although the organism was eliminated in only three patients – presumably because most had “advanced pulmonary involvement” and chronic entrenched infection by the time the treatment was started.
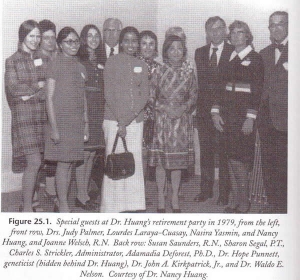
Fig 14. Nanny Huang, Lourdes Laraya-Cussay and others. With permission of Carl Doershuk
Dr Nancy Huang was a leading authority in the USA during the Fifties to the Eighties and published on a wide variety of subjects, many related to the use of antibiotics but on many other aspects of CF. Although her retirement party was held in 1979 (figure14) she was still publishing papers on CF in the late Eighties! Dr Huang and Dr Lourdes R Laraya-Cuasay have written an interesting account of their work at St Christopher’s Hospital, Philadelphia and other biographical details (Center Directors Remember: Philadelphia. In Doershuk K, editor. Cystic Fibrosis in the 20th Century. Cleveland, Ohio: AM Publishing, Ltd.2001: 294-314).
This is the first report of long term anti-Staphylococcal therapy, a treatment now recommended in the UK for all children with CF under three years of age, although its prophylactic longterm use is still the subject of debate. Essential facts which have become apparent are that resistance to the antibiotic does not develop and the frequency of S. aureus positive cultures is reduced when patients are receiving long term anti-Staphylococcal therapy. The possibility of an increased likelihood of culturing P. aeruginosa becomes less relevant when a successful policy of early Pseudomonas eradication is routine the clinic – this was not the case in North America until recently.
However, in Leeds, where lifelong long term flucloxacillin for most patients has been the policy since 1975 and early eradication of P. aeruginosa has been practiced since around 1984 – both the prevalence of chronic S. aureus infection of 14% is low (Southern et al, 1993. In: Clinical ecology of cystic fibrosis. Escobar H et al. (eds). Excerpta Medica Internat Congr Series 1034: 129-132) and chronic P. aeruginosa infection is well below average at 18.1% for the whole clinic and only 4.3% for those children less than 11 years of age (Lee et al, 2004, below).
1964 Fleisher DS, DiGeorge AM, Barness LA, Cornfeld D. Hypoproteinaemia and edema in infants with cystic fibrosis of the pancreas. J Pediatr 1964; 64:341-348. [PubMed]
Four infants with CF fed either human milk or soya milk had severe hypoproteinemia. The onset of oedema was around two months. Death was usually between 8-16 weeks. Soya was definitely contraindicated in infants thought to have CF.
Subsequent studies showed less nitrogen absorption from soya feed than from one based on evaporated milk (Fleisher DS et al. J Pediatr 1964; 64:349-356). A further instance was reported by Menton and Middleton in 1944 (above) and the first detailed report being that of Wissler & Zollinger in 1945 (above). Also Shahidi et al, 1961 (above). So soya based feeds definitely seem to be contraindicated for infants with cystic fibrosis.
1964 Doggett RG, Harrison GM, Wallis ES. Comparison of some properties of Pseudomonas aeruginosa isolated from infections in persons with and without cystic fibrosis. J Bacteriol 1964; 87:427-431. [PubMed]
One of the early papers discussing the peculiarities of this organism that was isolated with increasing frequency from people with CF, in particular the so-called “mucoid” form. There was considerable discussion about the pathogenicity of P. aeruginosa in CF which initially was questioned by some clinicians. Pseudomonas aeruginosa, isolated from the respiratory tract of a group of patients diagnosed as having CF, attained the ability to produce, in its capsule, a material which was insoluble in certain organic solvents, such as ethanol. The capsule obtained from P. aeruginosa isolated from infected individuals who did not have CF was ethanol-soluble. This alcohol-insoluble mucoid from the CF P.aeruginosa could be demonstrated to persist after sequential subcultures of the organism. (also Doggett et al, 1966 below).
1964 Schuster SR, Shwachman H, Harris GBC, Khan K-T. Pulmonary surgery for cystic fibrosis. J Thorac Cardiovasc Surg 1964; 48:750760. [PubMed]
One of a number of papers on this subject which have appeared since that of Lloyd & Robitzek in 1952 (above) most of which showed surprisingly good results of lung surgery in people with cystic fibrosis. This report concerns surgery for severely affected segments of lungs of 21 patients with CF. Two became symptom free, 13 improved and 3 had poor results including cardiac arrest, eventually fatal collapse of the remaining lung and one had fatal multiple thoracic sepsis.
Fig. 15 Sydney Gellis
Sydney Gellis (1914-2002) (figure 15), the ever-sceptical editor of the Year Book of Pediatrics (Sydney Gellis, 1965-66 Year Book of Pediatrics), commented that there were obviously some who were not “affected by the contagion of enthusiasm exhibited by those who work closely with cystic fibrosis……The discovery of the basic cause of the disorder and hopefully some form of substitution therapy must be the focus of the efforts in the disease”. One could comment that had it not been for the efforts of those “affected by the contagion of enthusiasm exhibited by those who work closely with cystic fibrosis” as Gellis put it, over the years, the impressive improvement in outlook would never have occurred! Also there was certainly a great need for such enthusiasts in the Sixties.
1964 Cystic Fibrosis. A symposium. Report of a meeting on 28th May 1964 at the Wellcome Foundation London. Chest and Heart Association.
This was one of the first, if not the first, substantial CF meeting in the UK. Chaired by Professor Douglas Hubble of Birmingham, the contributors included most of those in the UK who had significant involvement with CF at the time including Drs Winifred Young, Archie Norman, Tony Jackson, John Batten, Cedric Carter, Lynne Reid and David Lawson.
Dr Lloyd Rusby, of the Chest and Heart Association, noted that the Cystic Fibrosis Research Foundation was started in 1962 to raise funds for further research; also a group of parents based in Somerset “devoted largely to the exchange of emotive and dismal family news”.
Sir Robert Johnson describes how attempts were made to absorb this Somerset Group in the Chest and Heart Association and to make that the main Cystic Fibrosis organisation in the UK. Fortunately that failed as the charity would have been concerned with too wide a range of disabilities to give adequate emphasis to cystic fibrosis. However, these efforts gave rise to considerable concern until the Cystic Fibrosis Research Trust was formed (1964 see details below).

Fig 16. Lynne Reid
Among the presentations at this meeting, Lynne Reid (scientist) (figure 16) implied that CF resulted in an abnormality of mucus which predisposed to infection this abnormality could occur at an early stage but did not seem to be present at birth and “what is not so clear is why infection arises from impaction of uninfected mucus”. “Perhaps the proportion of the different cell types is abnormal; from this, differences in the final constitution of the final secretion may follow”.

Fig 17. Archie Norman
Archie Norman (paediatrician) (figure 17) gives a detailed account of the clinical features ending – “To sum up cystic fibrosis should be remembered as a possibility in a newborn baby who takes his feeds well and yet fails to thrive, in an older baby who develops whooping cough and in the toddler with rectal prolapse. It should be considered in any older child with clubbing of the fingers or with a cough that never quite clears up”.
John Emery (paediatric pathologist from Sheffield),(figure 18) discussing the laboratory aspects concluded – “I suggest that you do not send 24-

Fig 18. John Emery
hour specimens of stool to the laboratory for quantitative fat. A half minute scan of a drop of stool under the microscope will usually tell you much more”. 20% trichloracetic acid is advised to test meconium for the increased protein in meconium ileus and the X-ray plate method for tryptic activity. After a review of the various tests available including the sweat test Emery wisely observes “Cystic fibrosis is by no means an ‘all or none’ disease and in my opinion should never be diagnosed or excluded on a single test”.
Fig 19. Winifred Young
Winifred Young (“research clinician”) (figure 19) one of the leading CF paediatricians describes how their treatment at the Queen Elizabeth Hospital was intensified in 1955 due to their failure to arrest the incidence and progress of the pulmonary Fig 15. complications.
Tony Jackson,(consultant paediatrician),(figure 20) reviews the improvement in outlook that occurred following these changes described by Dr Young. Criteria for adequate antibiotic therapy were considered to be –
Fig 20. Tony Jackson
1.Early treatment of the first lower respiratory infection with high doses of antibiotics by aerosol and other routes until clinical recovery and elimination of Staphylococcus Pyogenes judged by three negative swabs.
2.Continuous antibiotic prophylaxis for at least three months after lower respiratory infections.
3. Prophylaxis with antibiotics intermittently during subsequent upper respiratory infections.
4. Adequate treatment of all subsequent lower respiratory infections.
Considerable emphasis was placed on maintaining adequate nutrition and nearly half their patients were above the 25th centile for weight
Fig 18. David Lawson
Dr David Lawson gave a thoughtful concluding talk on the future. As “there is as yet no wisp of smoke over the horizon of our knowledge” “we must deal with the problem as it is”.
This symposium gives an insight into the situation regarding CF as seen by the very few professionals in the UK who were familiar with the condition and experienced in treating affected children.
1964 UK CYSTIC FIBROSIS RESEARCH TRUST WAS FORMED
Fig 19. John Panchaud
The UK Cystic Fibrosis Research Trust was formed in 1964 on the initiative of the late Mr John Panchaud (figure 19) whose daughter Caroline had cystic fibrosis.
The details surrounding the formation of the CF Trust were described in 1984 by Sir Robert Johnson, also a CF parent. A full transcript of Sir Robert’s 1984 lecture is included in the “Future” section. He recalls that John Panchaud’s father-in-law was Percy Lovely, a man highly respected in the City of London and a Member of the Common Council. At this time the Chairman of the Dock Labour Board was Lord Crook who lived in Carshalton. In 1963 Lord Crook and the National Dock Labour Board gave a cocktail party at the Board’s headquarters on the Albert Embankment in London to which Lord Crook invited a friend – a neighbor from Carshalton, Dr David Lawson. David Lawson was a paediatrician at Queen Mary’s Children’s Hospital in Carshalton and himself a CF parent. Among the other guests, at what was a City function for business dignitaries, were by chance, Mr. and Mrs. Lovely. In the course of the party, Dr Lawson espied Mrs Lovely. She was apparently a lady of some elegance wearing on this occasion a particularly edible hat! Having attracted or so it seems the attention of this young Dr Lawson and finding out that he was a doctor, she poured out her heart to him about the problem of her grand daughter Caroline. It was left that she would get her son-in-law, John Panchaud, to phone David Lawson to arrange a meeting.
So it was at that cocktail party, in the unlikely setting of the National Dock Labour Board headquarters in London, that one has the origin of the Cystic Fibrosis Research Trust. The consequence was that John Panchaud went to see Dr. Lawson and together they evolved a plan. David Lawson’s first suggestion was that they should set up a medical or scientific steering committee. John Panchaud proposed that this committee should include Dr Lawson and the physician who was looking after his daughter Caroline at Great Ormond Street Hospital – Dr Archie Norman. Eventually Dr Lawson became chairman of the steering committee which included Dr Archie Norman, Dr Cedric Carter, the geneticist from GOS, Dr Winifred Young of the Queen Elizabeth’s Children’s Hospital Hackney in London and Dr Lynne Reid a scientist working at the Brompton Hospital in London; they were soon joined by Dr John Batten another physician from the Brompton.
Fig 20. Joseph levy CBE BEM First Chairman
In July 1963, John Panchaud had his solicitor draw up the necessary legal documents for the formal creation of the charity. One of the first Trustees was Mr. Percy Lovely and as a result of his and John Panchaud’s contacts in the City they got together a Board of Trustees, including as originals Mr Joseph Levy and Lord Crook. others were Lord Bossom and there were other prominent figures in the City. The inaugural meeting of the new CF Research Trust was held on February 20th 1964 in the Mansion House in the City of London, under the auspices of the Lord Mayor, Sir James Harman.
John Panchaud, Joseph Levy and Percy Lovely were the prime movers in fund raising for research into something of which scarcely anyone had heard. Initially the individual trustees organised fund raising but soon the fund raising base needed widening and the initiative was taken by Dr Archie Norman. He selected one of the mothers attending his clinic to organise the first group in London. There was increasing interest by parents in the groups and more formed around the UK.
Sir Robert Johnson looks back on those days with great emotion for suddenly there was hope. Suddenly there was something one could do to fight back. A chance even to win. For those who were involved those days still mark a turning point in their lives.
Much of the above detail has been taken from a lecture by Sir Robert Johnson, “History of Cystic Fibrosis Research Trust”, at the CF Trust’s 20th Anniversary Weekend at Brighton in June 1984. A full version of this lecture, recently approved by Sir Robert Johnson, can be found in this website in the section “Some other historical Things” – in which it is listed in “Some previous publications on the history of cystic fibrosis mentionMr Joseph Levy CBE BEM (figure 20) was Chairman of the CF Research Trust for 20 years, from soon after its formation in 1964 until 1984 when his son, Mr Peter Levy OBE succeeded him, followed by Mr Duncan Bluck CBE until I (Jim Littlewood) became chairman in 2003 to 2012. In 2012 Mr George Jenkins OBE was appointed Chairman. Many in the UK CF community, patients, parents and professionals, have reason to be grateful to Joe Levy, to Peter and the Levy family for their continuing and generous support in many areas.
The name of the organisation changed to the Cystic Fibrosis Trust in the mid Eighties at the request of the scientists on the Research & Medical Advisory Committee. They considered it was now not only a “research” Trust in view of the increasing proportion of the funds that were used for care of the increasing number of people with CF who were surviving and to support the many developing CF centres in the UK.

Fig 21. Ron Tucker OBE
Ron Tucker OBE (figure 21) was appointed the first Director of the CF Research Trust in 1965 after many years of work with youth clubs in Lancashire and London. Apparently an interview panel was assembled to appoint a new Executive. Ron Tucker, who was a friend of Joe Levy, was on the panel. There were no suitable applicants and he was asked if he was interested – fortunately he was! Ron proved to be an inspirational central figure in the development of CF care and research in the UK. He was widely respected by patients, parents and professionals throughout the UK and abroad. He was very supportive of the new CF centres which were developing during the Eighties in the UK and very supportive of any paediatricians who showed the slightest interest in CF – such as myself!. Ron was instrumental in the appointment of both a CF research fellow (doctor) and a CF Nurse Specialist in Leeds when our unit was developing during the early Eighties and subsequently also supported many other developing provincial CF centres. He also encouraged many families with CF to come to our unit in Leeds for our Comprehensive Assessments when their local care was not available or he considered it to be unsatisfactory.
1964 Sproul A, Huang N. Growth patterns in children with cystic fibrosis. J Pediatr 1964; 65:664-676.[PubMed]
An early detailed report of the poor nutritional state and growth of 50 children with CF studied serially. The significant retardation of weight gain and growth particularly in adolescent and pre-adolescent children was severe with the medians for height and weight being only between the third and tenth centiles for age. Skeletal development was delayed in 38% of children. Not surprisingly there was a significant relation between the severity of the malnutrition and the pulmonary status. Better weight gain and growth occurred when the chest was treated – improvement being most marked in infants.
Presumably a number of previously under-treated children were referred to this clinic and so the initial improvement was impressive. Unfortunately, many children deteriorated after a short period of improvement, succumbing to their advanced pulmonary disease which had been a major factor in the first place.
1964 Grossman H, Denning CR, Baker DH. Hypertrophic osteoarthropathy in cystic fibrosis. Am J Dis Child 1964; 107:1-6.[PubMed]
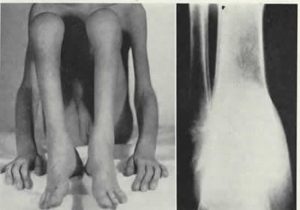
Fig 22. Clubbing of fingers and toes, swollen ankles and knees. Xray of distal tibia and fibula showing periosteal new bone formation along their shafted
An early report of pulmonary hypertrophic osteoarthropathy in a girl of nine years (figure 22) with CF and severe pulmonary disease. Often asymptomatic in the early stages there is later aching and tenderness along the shafts of the long bones and around the joints. Shwachman commenting on this report said he had seen five or six instances in patients with severe pulmonary disease. Also he notes the condition is mentioned in Harris et al, Post Grad Med 1963; 34:251.
The degree of clubbing can be quantified in various ways. Sinniah D & Omar (Arch Dis Child 1979; 54:145-146) used a shadowgram technique which we later used in the Leeds clinic (Pitts Tucker et al, Arch Dis Child 1986; 61:576-579 below).
1964 Shwachman H, Diamond LK, Oski FA, Khaw Kon-T. The syndrome of pancreatic insufficiency and bone marrow dysfunction. J Pediatr 1964; 65:645-656. [PubMed]
This is the second most frequent cause of chronic pancreatic disease in children. Six children are described with what became known as the Shwachman–Diamond Syndrome. It is one of a number of conditions eventually recognised as separate entities from cystic fibrosis. The authors advised that the condition should be considered in children at first suspected of having CF but who had repeatedly normal sweat electrolytes.
In 1967 Burke and colleagues (Burke V et al. Arch Dis Child 1967; 42:147-157.[PubMed]) reported 19 children with the condition from Royal Children’s Hospital Melbourne having published a preliminary report in 1965 (Colebatch JH et al Lancet 1965; ii: 496). Burke et al commented that in 1964 Bodian et al (Acta Paediatr Uppsala 1964; 53:282) from Great Ormond Street, London had described two children with congenital hypoplasia of the exocrine pancreas both of whom had variable neutropenia and thrombocytopenia but which “did not receive special comment” – which is not entirely true. Bodian et al did however provide a useful review of a previous 18 histologically proven cases in the literature.
This was an important paper for paediatricians dealing with children who had CF as it identified a specific condition (exocrine pancreatic insufficiency, bone marrow dysfunction, skeletal abnormalites and short stature with normal sweat tests) likely to be encountered in specialist CF centres. In fact, we identified five such children with the Shwachman-Diamond syndrome in Leeds over 20 years in the course of investigation of hundreds of children considered initially to have cystic fibrosis.
1964 Wiser WC, Beier FR. Albumin in the meconium of infants with cystic fibrosis: a preliminary report. Pediatrics 1964; 271:926-933.
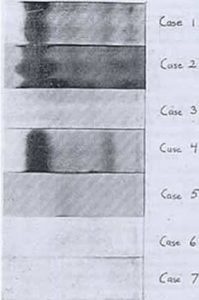
Fig 23. Electrophoresis of meconium. Wiser et al, 1964 (see text opposite for explanation)
Although an unusual protein content in the meconium of infants with meconium ileus had been described by a number of authors (Glanzmann E, Berger H. Ann Paediat 1950; 175:33 above; Buchannan & Rapoport Pediatr 1952:9:304 above; Green M et al. Pediatr 1958; 21:635 above), the present study was to determine if meconium from infants with CF who did not have meconium ileus also had an abnormal protein content as perhaps this could be “used in a predictive manner” i.e. for neonatal CF screening.
In this study, using immunoelectrophoresis, the meconium from five infants with a family history of CF (1 – 5) was examined for increased protein (figure 23). The three of these infants with CF (1,2,& 4) had obviously raised albumin levels which did not occur in the two unaffected infants (3 & 5) nor in two healthy control infants (6 & 7).
This study, from Salt Lake City, was the first to demonstrate increased albumin in the meconium of all CF infants and to suggest the finding could be used in a “predictive manner”. Later Schutt & Isles (Arch Dis Child 1968; 43:178 below) from Bristol in the UK showed that the increased albumin could be recognised very simply by using the Albustix dipstick test designed for testing urine for albumin; this method eventually formed the basis of the BM Meconium test used with variable success in several neonatal CF screening studies during the Seventies (In Europe by Stephan U, et al. Pediatrics 1975; 55:35-38 below; in Wales by Ryley HC, et al. Arch Dis Child 1979; 54:92-97 below; in the UK by Evans et al, 1983 below).
1964 Matthews LW, Doershuk CF, Wise M, Eddy G, Nudelman H, Spector S. A therapeutic regimen for patients with cystic fibrosis. J Pediatr 1964; 65:558-575. [PubMed]
Fig 23, Carl Doershuk
Dr Doershuk (figure 23) recalls that Dr William Wallace, Chairman of Pediatrics at the Babies and Children’s Hospital, Cleveland had been approached in 1957 by a parents’ organisation – the “Cousins Club” – one of whom had already lost a child with CF and had another deteriorating from the condition. They asked Dr Wallace to start a “research orientated treatment programme for CF” which they offered to fund. To develop this programme Dr Wallace appointed a young paediatrician, Dr Leroy Matthews (figure 25) to plan and initiate the “comprehensive and prophylactic (preventive) treatment programme” for the treatment of cystic fibrosis. The programme which developed eventually became the model for the CF Foundation CF centres programme (also Doershuk et al, 1964 & 1965 below).
Three important areas of treatment were the obstructive pulmonary lesion, the secondary infections and the pancreatic deficiency and nutritional state. Treatment was early and comprehensive even started before symptoms – where this group differed from others and as such were ahead of their time. This paper describes the “comprehensive therapeutic regimen” which so influenced CF care in N America.
Fig 25. LeRoy Matthews.
Veteran CF physician Dr Warren Warwick of Minnesota has “fond memories of two great stars – Harry Shwachman and Leroy Matthews”. Of Leroy Matthews he writes – “Leroy Matthews, the greatest genius CF has seen, single handedly established the value of Comprehensive Treatment, laid the ground work for Pediatric Pulmonology, and led the CF Centres as well as planning and directing excellent research. He made only two mistakes. He allowed his “Comprehensive Treatment” plan to be equated with “mist tent therapy” so when the mist tent was discredited many also felt the Comprehensive Care Program was discredited. And he tried too hard to control his diabetes and suffered hypoglycaemic brain injury and cardiovascular complications” (Warren Warwick in Doershuk CF (ed). Cystic fibrosis in the 20th Century. AM Publishing, Cleveland 2001:319)
1964 Doershuk CF, Matthews LW, Tucker AS, Nudelman H, Eddy G, Wise M, Spector S. A 5 year clinical evaluation of a therapeutic program for patients with cystic fibrosis. J Pediatr 1964; 65:677-93. [PubMed]
A detailed evaluation of the results of the Cleveland comprehensive therapeutic regimen. 96 consecutive patients were followed for 18 to 60 months (average 37 months) and evaluated using a modified Shwachman score. 82% improved, 11% remained the same, and 4% showed progression beyond their initial status and only 3% died – none were less than five years of age. Patients who were regarded as having reversible pulmonary changes were reviewed separately in 1965 (Doershuk et al, Pediatrics 1965; 36:675 below).
1965 Doershuk CF, Matthews LW, Tucker A, Spector S. Evaluation of a prophylactic and therapeutic program for patients with cystic fibrosis. Pediatrics 1965; 36:675-688. [PubMed]
Good results were reported in the group of children treated prophylactically with little progression over an average of 4.5 yrs. The early intervention and prophylactic approach was not the usual policy at this time and most clinicians waited until symptoms developed – even experts such as Paul di Sant’Agnese. In this study 98 consecutive patients had been followed for an average of 4.5 years and the clinical course of 49 were considered to be on prophylactic therapy was significantly different from the accepted natural course of the disease and from the 49 patients who had irreversible lung damage when first seen. No evidence of significant progression of the pulmonary state was seen in any of the prophylactic group. No deaths occurred in this group and the annual mortality rate was only 2% for the whole group. Their findings supported the need for early diagnosis and prophylactic treatment.
Sydney Gellis (always a sceptic regarding the treatment of CF!!) in the Year Book of Pediatrics questioned whether more mild cases had been included; also whether the improved survival could not have been due entirely to antibiotics and to none of the other methods of treatment described such as mist tents, aerosols, segmental postural drainage. di Sant’Agnese also observed that in one series of older patients (Shwachman et al, 1965) the diagnosis had not been made in many until teen age years suggesting they had a milder form of CF. Certainly patients with CF diagnosed later in childhood, who were included in some of the early adult series, undoubtedly more frequently would have had milder CF gene mutations as was confirmed in later studies (Gan K-H et al, 1995 below).
Rather surprisingly di Sant’Agnese questioned the need to start the full prophylactic programme in all patients as soon as the diagnosis is made and agrees with most other clinicians at that time that treatment is not started “until there is indication of incipient pulmonary involvement”. This is surprising and quite the opposite to modern policy. In these days of neonatal screening, failure to start early microbiological monitoring, early eradication treatment of respiratory pathogens and early nutritional intervention, would be regarded as quite unacceptable.
1965 Batten J. Cystic Fibrosis: A Review. Brit J Dis Chest 1965; 59:1-9. [PubMed]

Fig 26. Sir John Batten
In the mid Sixties Sir John Batten (figure 26) (1924 – 2013) started the first clinic in UK for adults with CF at the Royal Brompton Hospital, London. This clinic eventually became the world’s largest centre for adults with cystic fibrosis. In the UK it was the only large clinic for adults with CF until the late Eighties as there were so few adults surviving. Sir John remained closely involved in the developments of CF care in the UK and with the work of the UK CF Trust eventually becoming its Hon. President from 1986 to 2003. Sir John was physician to Her Majesty the Queen from 1974 to 1989.
1965 The International Cystic Fibrosis (Mucoviscidosis) Association was formed.
In 1965 the International Cystic Fibrosis (Mucoviscidosis) Association (the predecessor of CF Worldwide) was formed Paris under the medical chairmanship of Paul di Sant’ Agnese. Guido Fanconi was appointed Hon. Chairman, George Barrie as lay President and Prof. Rossi Vice Chairman of the Medical/Scientific Council. The aims of the association were to improve the care of children and adults who had cystic fibrosis, to foster research and to disseminate information. This was the start of the International CF (ICFMA) now CF Worldwide meetings, which take place every 4 years.
1965 Kopito L, Mahmodian A, Townley RRW, Khaw KT, Shwachman H. Studies in cystic fibrosis: analysis of nail clippings for sodium and potassium. N Engl J Med 1965; 272:504-509. [PubMed]
Abnormal electrolyte content of nails was suggested as a possible diagnostic help but the test never became popular as there was overlap between CF and non-CF and it was difficult to perform. (also Leonard PJ, Morris WP. Arch Dis Child 1972; 47:495-498)
1965 Rickham PP, Boeckman CR. Neonatal meconium obstruction in the absence of mucoviscidosis. Am J Surg 1965; 109:173 – 177. [PubMed]
Mr. Rickham, a paediatric surgeon from the Alder Hey Children’s Hospital in Liverpool, UK, reported seven infants who, although having neonatal meconium obstruction did not appear to have cystic fibrosis. Five survived and subsequently had normal sweat tests and trypsin was present in their stools; although three did show some evidence of intestinal malabsorption. The three infants that died had normal pancreatic histology further confirming they did not have CF. Also they did not have positive sweat tests and had normal routine pancreatic histology which has been found in only a minority of infants who die of meconium ileus (Oppenheimer & Esterly Arch Pathol 1973; 96:149-154). Other examples of non-CF neonatal meconium obstruction have been reported (Dolan TF, Toulon RJ. J Pediatr Surg 1974; 9:821-824; Shigemoto H, et al. J Pediatr Surg 1978; 13:475-479. [PubMed]). The fact that five of these infants survived with normal sweat tests in 1965, when many children with CF died in early childhood, provided further confirmation they did not have cystic fibrosis.
This was an important report as the presumption that an infant with meconium ileus definitely had CF on one occasion to my knowledge resulted in an incorrect diagnosis of CF – a situation overlooked for some 10 years. A child of 10 years who had been treated in the neonatal period for meconium ileus was subsequently treated in the paediatric clinic as having cystic fibrosis. In an outpatient clinic a medical student asked the consultant paediatrician the result of the sweat test. It was eventually discovered, after a search through the notes, that the child had never had a sweat test performed to confirm the diagnosis. So a sweat test was performed which proved quite negative as did all the other tests for cystic fibrosis. So the diagnosis was reversed.

Fig 27. Peter Rickham
Mr Peter Rickham (1917-2003) (figure 27) was one of the paediatric surgeons who helped to establish paediatric surgery in the UK, founding the first neonatal surgical unit at the Alder Hey Children’s Hospital in Liverpool. Peter Rickham trained in paediatric surgery at Great Ormond Street Hospital, London, and at Alder Hey. He spent a year in Boston and Philadelphia as a Harkness travelling fellow before being appointed consultant paediatric surgeon at Alder Hey in 1952. He became director of paediatric surgical studies there in 1965. In 1971 he was appointed professor of paediatric surgery at the University Children’s Hospital in Zurich, where he remained until his retirement in 1983.
He was forceful and outspoken, but passionately involved with his specialty. Apparently in the early years following his appointment in Liverpool, he became so exasperated by the local paediatricians’ use of barium to diagnose oesophageal atresia that he sent every paediatrician in his catchment area a Christmas card enclosing a radio-opaque catheter so that they could safely diagnose the condition!
1965 Mearns MB, Young W, Batten JC. Transient pulmonary infiltrations in cystic fibrosis due to allergic aspergillosis. Thorax 1965; 20:385-392.
This was the first description of allergic bronchopulmonary aspergillosis (ABPA) occurring in two children with cystic fibrosis. A subsequent study from this group showed precipitating antibody to Aspergillus to be present in 31% of 122 children with CF compared with in only 7% in 60 asthmatic children (Mearns M et al. Lancet 1967;i:538-539).(see Brueton et al, 1980 below for typical chest X-ray of ABPA).
Winifred Young (1909-1969) (figure 16) was appointed as a research clinician at the Queen Elizabeth Hospital for Children Hackney Road London in 1943 and established a cystic fibrosis clinic there in 1950. Winifred Young and Margaret Mearns (figure 19) were treating children with CF at the Queen Elizabeth Hospital for Children, Hackney, London – at the time one of the few CF clinics in the UK. Children who survived were referred from there (along with those from Archie Norman’s clinic at Great Ormond Street) to Dr John Batten’s adult CF clinic at the Royal Brompton Hospital, London.
As early as 1972, Drs Margaret Mearns and Winifred Young published encouraging results of their meticulous clinical and microbiological follow-up and treatment reflecting their care in the Sixties (Mearns, 1972 below). These were further indications that vigorous meticulous treatment of the secondary effects of the basic defect at an early stage could significantly improve prognosis. From the 1950s their young patients had received prophylactic erythromycin and nebulised neomycin and intensive physiotherapy – before 1957 they had 50 infants who, at a year, had no significant trouble and who, at 5 years, were still considered to be free of bronchitis (Mearns, 1969); this was quite atypical for the UK at that time.
It is a reflection of the much inferior medical communication systems in those times, or perhaps, more likely, the attitudes of the general paediatricians to specialsed care, that the effective treatment regimens at the few large UK CF clinics, such as this, were not more widely adopted throughout the UK.
1965 Holsclaw DS, Eckstein HB, Nixon HH. Meconium ileus. A 20-year review of 109 cases. Am J Dis Child 1965; 109:101-113.[PubMed]
Fig. 28 Douglas Holscaw Author’s image
Douglas Holsclaw (figure 28) who was a colleague of Harry Shwachman’s, reviewed experience since 1944 of 109 infants with meconium ileus from the Hospital for Sick Children, Great Ormond Street, London.
The paediatric surgeons were Mr Herbert Eckstein and Mr Harold Nixon (1918-1990) . Half the infants with uncomplicated meconium ileus, 18% with a perforation and 24% with gangrene of a loop of bowel, survived. Of those treated surgically 41% survived after primary anastomosis, compared with 72% after a Bishop-Koop procedure (Bishop & Koop, 1957 above). Only 25% of those with a double barrelled ileostomy survived. Only 20 of 46 survivors reached one year and only seven lived over five years – virtually all died of pulmonary complications. However, there seemed to be a steady improvement occurring as nine of the 10 most recent cases survived
Douglas Holsclaw published extensively over subsequent years (Kaplan et al, 1968; Holsclaw et al, 1970; Holsclaw et al, 1971; Holsclaw & Keith, 1980; Holsclaw et al, 1980 all mentioned below)
Harold Nixon (1918-1990) was a distinguished paediatric consultant surgeon at Great Ormond Street.
Mr Herbert Eckstein (figure 29) was resident surgeon at Great Ormond Street at the time.
1965 Shwachman H, Kulczycki LL, Khaw Kon-Taik. Studies in cystic fibrosis. A report of sixty-five patients over 17 years of age. Pediatrics 1965; 36:689-699. [PubMed]
Harry Shwachman had treated 1700 patients over a period of 25 years. Ten years previously he had only three patients aged over 17 years. Here he is reporting 65 patients over 17 yrs – not including the 15 who died aged over 17 yrs. As in all other series of older patients the diagnosis was made later than average. For example in this series only 8 were diagnosed in the first year and only 34 of 65 were diagnosed less than 10 years. It is almost certain, as eventually shown by mutation analysis, that many of these late diagnosed patients had milder mutations.
Shwachman considered the most important single advance in treatment (as did others) was the introduction of broad spectrum antibiotics in 1948. The authors mention many aspects of management now regarded as features of optimal care.
“A few minor changes evolved over the years that may play a greater role than we are able to quantitate. Factors that have to deal with the economic, emotional and psychological problems of parents and of growing children having a disease expensive to treat and with an unpredictable future. Our constant availability for their guidance, the close and harmonious relationship to the family physician or paediatrician and of highly skilled experts in our medical centre, our attempt to secure financial assistance and to provide continuous long-term care by the same group of individuals regardless of the age of the patient, coupled with efforts to instruct our parents and above all our positive approach undoubtedly contributes to the relative success of our programme and survival of some of these patients beyond adolescence.”
These main components of good CF care have remained much the same over the years. One particular feature stressed by a number of the successful CF paediatricians over the years has been availability of the doctor for advice and continuity of care by the same group of individuals – two features which are less readily available in the modern UK National Health Service. However, one point must be made – many paediatricians in the USA – including Shwachman – were initially slow to refer their patients to chest physicians treating adults most of whom lacked the knowledge and experience to continue providing the expert treatment the patients had received to achieve their adult status. One factor may have been the problems with medical insurance arrangements.
1966 Wilroy RS Jr, Crawford SE, Johnson W. Cystic fibrosis with extensive fatty replacement of the liver. J Pediatr 1966; 68:67-73. [PubMed]
An early description of fatty infiltration of the liver (steatosis), which can result in gross hepatomegaly and is, in part, reversible when the intestinal malabsorption is treated and the nutritional state improved. The child reported in this paper presented at two years five months with an enlarged liver which “extended to the pelvic brim” and marked generalised oedema – no manifestations of pulmonary disease were noted at the time.
1966 Barbero GJ, Siblinga MS, Marino JM, Seibel R. Stool trypsin and chymotrypsin. Value in the diagnosis of pancreatic insufficiency in cystic fibrosis. Am J Dis Child 1966; 112:536-540.[PubMed]
Fig. 29a Giulio Barbero
These are useful non-invasive tests for confirming pancreatic insufficiency used for many years – chymotrypsin being preferred to trypsin as it is the more stable. Their value was confirmed in subsequent reports (Brown et al, 1988 below). This present study used the method of Haverbach BJ, et al, (Gastroenterol 1963; 44:588-597). There was clear separation of CF and non-CF and the authors concluded it to be reliable in identifying those children with cystic fibrosis. Chymotrypsin values were : in CF < 58 ug/g and in non-CF > 75 ug/g stool and trypsin: in CF < 30 ug/g and in non-CF >80 ug/g stool.
Giulio Barbero (1923 – 1997) (Fig. 29a) was distinguished leader in the N. American CF scene. His residency was interrupted by 2 years army service with a MASH unit in Korea where he helped establish a children’s hospital in Pusan. He subsequently developed a programme of CF care at the Children’s Hospital of Pennsylvania and played an important role in the development of CF services in the USA. He was described as “a most articulate and eloquent speaker, a very dedicated and caring physician, a motivator and great humanitarian”. After various appointments in Philadelphia including the development of the Hahnemann CF programme, he recruited Dr. Holsclaw who had worked with Harry Shwachman. He eventually left to become Chairman of the Department of Pediatrics at the University Missouri-Colombia School of Medicine. In 1996 he was honoured by the award the third European Joseph Levy Lecture which was entitled “The Science and Humanity of Cystic Fibrosis”.
1966 Huang NN, Harley RD, Promadhattavedi V, Sproul A. Visual disturbances in cystic fibrosis following chloramphenicol administration. J Pediatr 1966; 68:32-44. [PubMed]
There were visual changes in nine (27%) of 33 patients with CF who had received chloramphenicol in total doses of 81-283 g. The authors mention another patient treated with 135 g of chloramphenicol over 4.5 months (Cocke JG, et al. J Pediatr 1966; 68:27). The authors state that although visual disturbances had been described in children with CF and advanced respiratory disease (Bruce et al. Arch Ophth 1960; 63:391) only advanced respiratory changes were present as an explanation; however, these authors later described four children with eye changes due to chloramphenicol (Denning et al. J Pediat 1963; 63:878) as did Huang et al. (3rd Interscience Conference Antimicrob Chemother 1963:79). Such patients with eye changes had always received prolonged treatment with chloramphenicol. The eye symptoms usually improved when the drug was stopped. Regular tests of vision were advised when the drug was used for prolonged periods.
1966 Schwartz RH. Serum immunoglobulin levels in cystic fibrosis. Am J Dis Child 1966; 111:408. [PubMed]
Raised immunoglobulin levels were noted in many people with cystic fibrosis. Subsequently the raised levels were shown to relate to the severity of the lung involvement. The levels of serum immunoglobulins were very high in patients with advanced chest involvement. They are a very useful clinical marker of the severity of the chest infection. A later study showed that children with lower immunoglobulin levels had a better prognosis (Matthews WJ et al N Eng J Med 1980; 302:245-249).
1966 Rubin LS, Barbero GJ, Chernick W. Pupillary dysfunction as a concomitant of cystic fibrosis. Pediatrics 1966; 38:865-873. [PubMed]
The authors found abnormalities in response to darkness, stress and recovery from stress. They considered at the time these findings were possibly being related to the basic defect. Autonomic abnormalities were first suggested by Roberts in 1959 (above). (Also Holzel et al, 1962 above; Rubin et al, 1963 above; Davies et al, NEJM 1980; 302:1453-1456 and more recently reviewed by Mirakhur A et al. (J R Soc Med 2003; 96 Suppl 43:11-17).
1966 Doggett RG, Harrison GM, Stillwell RN, Wallis ES. An atypical Pseudomonas aeruginosa associated with cystic fibrosis of the pancreas. J Pediatr 1966; 68:215-221.
Another of the many papers published by Doggett on the atypical “mucoid” Pseudomonas aeruginosa isolated from 43 of 62 cultures from 78 children with CF. It was a highly mucoid variant of the organism which was insoluble in ethanol-benzene (figure 30) and was impossible to eradicate once established (also Doggett et al, 1964 above). The authors observe that “until such a means of control is found … clinics that treat groups of CF children may find it good practice to separate those already having Pseudomonas from those not infected with the organism, especially those having inhalation therapy”.
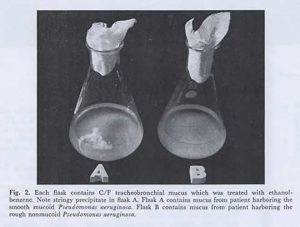
Fig 30. Details in the image. From Doggett R G et al 1966 with permission
Doggett is usually credited with recognising the significance of the mucoid form of Pseudomonas in people with CF and the conversion from non-mucoid to mucoid after acquisition of the former but not in people who do not have cystic fibrosis. Also it is interesting that, even at this stage, he was suggesting that segregation of Pseudomonas-positive from Pseudomonas-negative patients would be good practice – some 35 years before such segregation was introduced into all CF centres in the UK – in a few with great reluctance on the part of the clinicians!
1966 Keith CG, de Haller J, Young W F. Side effects to antibiotics in cystic fibrosis: 1. Ocular changes in relation to antibiotic administration and severity of pulmonary involvement. Arch Dis Child 1966; 41:262-266. [PubMed]
Experience of Winifred Young from London – only one of 42 patients had ocular changes from chloramphenicol; 425 g having been given to this patient over 15 months. Various other findings were considered unrelated to drug therapy including four with squint, nine with tortuosity of the retinal vessels, one with blurring of disk margins – appearances considered due to more severe lung disease. Eighteen children had various short course of chloramphenicol with no obvious ill-effects.
1966 Mantle DJ, Norman AP. Life tables for cystic fibrosis. BMJ 1966; 2:1238-1241. [PubMed]
First of a number of publications on survival in the UK from Dr Archie Norman’s unit at Great Ormond Street, London. Life tables for 1943-1964 showed that 80% died by 5 years and 90% by 10 years. Infants with meconium ileus, 25% died by 1 week and 75% by 3 months.
Sydney Gellis, in an editorial comment in the corresponding Year Book of Pediatrics, observed that “Despite claims to the contrary, cystic fibrosis of the pancreas continues to carry a gloomy prognosis. Present day therapy is helpful but offers relatively little, and a realistic alteration of the course of the disease will require a major breakthrough in discovering the aetiology”. Gellis, although a distinguished paediatrician was not an expert on CF and in this prediction was obviously quite wrong for the outlook improved steadily over the years long before the basic defect was identified during the Eighties.
1966 Paxton DG, Scott EP. Pneumothorax: An unusual complication in fibrocystic disease. Am J Dis Child 1966; 111:311-312. [PubMed]
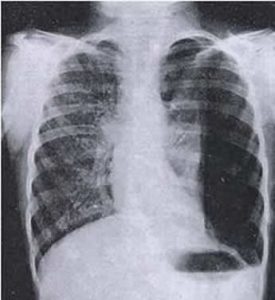
Fig 31. Massive left sided pneumothorax
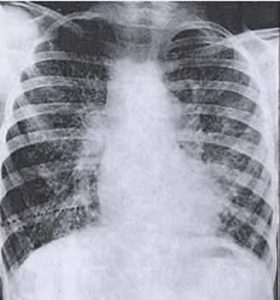
Fig 32. Pneumthorax resolved
The authors did not find previous reports of pneumothorax in the American literature – only in text books. However, prior to this report there had been sporadic reports of pneumothorax in CF in the literature from 1947 (Fanconi G, Metaxas-Buhler M. Helv Paediat Acta 1947; 2:289-295). Also Doershuk (1964) had one example in 96 patients.
This present report is of sudden onset of left pneumothorax in a 12 year old girl with CF whose chest showed “far advanced changes” at the age of 7.5years (figure 22). With a tube and drainage the lung expanded in 2 days (figure 23); she was discharged in 6 days but died 4 months later from her pulmonary disease.
Pneumothorax is a complication which occurs in those with more advanced chest damage and is now rare in children with CF. For example in the 2009 UK CF Registry there were only 2 children in 3312 less than 16 years reported as having pneumothorax but in 46 in 4065 patients over 16 years.
1966 Lawler RH, Nakielny W, Wright NA. Psychologic implications of cystic fibrosis. Canad M A J 1966; 94:1043-1046. [PubMed]
A detailed evaluation of 11 patients aged five to 17 years. Not unexpectedly extremely marked intrapsychic and interpersonal conflicts occurred in all cases. The authors considered that both children and parents required psychological treatment also the doctor-family relationships required further stud
The editor of the Year Book of Pediatrics, Sydney Gellis, felt the almost unbearable psychologic problems should be treated actively. He questioned “the support conferred by the CF Foundation which undoubtedly makes the family more knowledgeable about the condition and more capable of coping with the problems involved, but also makes parents more aware of the prognosis”. He suspected that a minister or priest would prove more helpful than a psychiatrist in assisting parents.
It was just this approach, exemplified by Gellis, that made the situation even more unbearable for the parents who usually appreciated an aggressive therapeutic approach, as adopted by paediatricians such as Shwachman, di Sant’Agnese and Leroy Matthews even if they realised that the end was inevitable. It was at the CF centres of such paediatricians that this approach resulted in a steady improvement in prognosis over the years.
Fig. 33 Sydney Gellis
Sydney Gellis (1914-2002) (figure 33) was Professor of Pediatrics at Tufts University School of Medicine and Chairman of the New England Medical Center Hospital in Boston. He was editor of the Year Book of Pediatrics from where I have obtained these comments which appear in this History of Cystic Fibrosis. He appeared to have had little time for psychiatrists or paediatricians who treated children with cystic fibrosis!! It is perhaps not surprising that not one of his 206 publications listed on Medline concerned cystic fibrosis. He was described as “the quintessential pediatric generalist who was not deterred by the growing army of “-ologists”! We all know such colleagues !!!!!! Certainly such “generalists” who failed to appreciate the advantages of specialization were a definite hindrance in the attempts to improve the outlook for many people with cystic fibrosis – this was certainly the case in the UK.
1967 Denton R, Kwart H, Litt M. N-acetylcysteine in cystic fibrosis. Mechanical and chemical factors in treatment by aerosol. Am Rev Resp Dis 1967; 95:643-651. [PubMed]
Robert Denton describes the in vitro mucolytic activity, the clinical response and the effect of oxygen and nebulisation on the stability of a 20% solution of N-acetylcysteine. In vitro dispersion is more complete than with saline. There was an improvement in drainage from the upper respiratory tract but failure to improve drainage from the lower respiratory tract. Nebulisation did not alter the chemical structure. The present method of mask administration may not affect the lower respiratory tract (also Webb 1962 above; Reas 1963 above)
– It is interesting that N-acetylcysteine is so rarely used for people with CF in the UK when some of the earlier published work is so impressive with regard to its mucolytic effect. More recently the relation to glutathione has caused renewed interest in the drug which when given orally in high doses provides a source of glutathione and apparently reduces airway inflammation (Tirouvanziam R, et al. Proc Nat Acad Sc 2006; 103:4628-4633).
1967 Swallow JN, De Haller J, Young WF. Side-effects to antibiotics in cystic fibrosis: dental changes in relation to antibiotic administration. Arch Dis Child 1967; 42: 311-318. [PubMed]
Experience from Dr Winifred Young’s unit in London where 36.5% of 63 children with CF had discoloured teeth due to tetracycline treatment (also above Shwachman H, et al, Antibiot Ann 1958-59; 692 above; Zegarelli et al, Pediatr 1960; 26:1050 above; Wallman IS, Hilton HB. Lancet 1962; i: 827 above)
1967 Young WF, Jackson AD. The prognosis of cystic fibrosis. Bibliotheca Paediatrica 1967;86:350-352.
Winifred Young and Tony Jackson were paediatricians at the Queen Elizabeth Hospital Hackney where there was one of the few CF clinics in the UK which was started by Winifred Young in 1950. Margaret Mearns joined the staff there soon after. Further data from these authors is described above in Cystic Fibrosis. A symposium. Report of a meeting on 28th May 1964 at the Wellcome Foundation London. Chest and Heart Association.
1967 Matthews LW, Doershuk CF, Spector S. Mist tent therapy of the obstructive pulmonary lesion of cystic fibrosis. Pediatrics 1967; 39:176-185.[PubMed]
This paper from Cleveland, from one of the most respected clinical groups in the USA, was considered to provide evidence of the efficacy of mist tent treatment which was by this time widely used in the USA. After three control periods the addition of mist tent therapy to an otherwise comprehensive treatment programme resulted, over the next two months, in significant decrease in functional residual capacity, residual volume and ratio of residual volume to total lung capacity – changes that were maintained over the next year.
– In commenting favourably on this paper at the time Paul di Sant’Agnese implied that clinicians with experience of treating people with CF would agree with the authors’ findings and stated – “the results reported here confirm the clinical observation of the value of mist tent therapy…it is generally accepted by almost all clinicians, who have had adequate experience with this disease, that most patients have considerable benefit from such a treatment programme”.
Di Sant’Agnese continued “we must conclude from all available clinical, physiologic and pathologic evidence that, in addition to the judicious use of antibiotic agents, all types of inhalation and physical therapy should be used in therapy of pulmonary involvement of cystic fibrosis”.
Despite this support from leading CF clinicians of the time, the treatment was later discredited and gradually abandoned by most of them in the early Seventies (See also Doershuk et al, 1968 below). Mist tent therapy was never popular in the UK. But perhaps the possible benefits of nocturnal humidification will be re-examined in the light of the low salt theory of pathogenesis of the respiratory problems?
(Suggest also read “Mist Tents” in Topics section this website.)
1967 Avery ME, Galina M, Nachman R. Mist Therapy. Pediatrics 1967; 39:160-165.[PubMed]

Fig 34. Mary Ellen Avery The National Library of Medicine
In the same issue of Pediatrics as Matthews et al, 1967 (above) paper on mist tent therapy, Mary Ellen Avery (Fig. 34) wrote a detailed critical review of mist therapy and concluded – “At present the technical advances in the generation of mists and knowledge of the deposition of particles exceeds knowledge of the role of mists in the treatment of respiratory disorders. Some evidence exists that viscous secretions can be thinned by mist; upper airway cooling and drying can be decreased by added humidity”. So the doubts about mist therapy were beginning to be expressed.
Mary Ellen Avery (1927-2011) (Fig. 34) was Professor of Pediatrics at Harvard and the first woman-in-chief at the Children’s Hospital, Boston. She had a distinguished career mentioned in the Harvard Magazine “From childhood on, she clearly had an outsized sense of self and purpose and a zest for new experiences that help explain the extraordinary list of firsts she accumulated: first to recognize the pathophysiology and cause of respiratory distress syndrome (RDS) in premature babies; first woman to chair the pediatrics department at McGill, head a major clinical department at Harvard Medical School, and become physician-in-chief at Boston Children’s Hospital; and first pediatrician to be president of the American Association for the Advancement of Science, the world’s largest multidisciplinary scientific society” (harvardmagazine.com)
1967 Warwick WJ, Manson S. Life table studies of mortality. In Cystic Fibrosis Part I. Physiology and pathophysiology of serum secretion clinical investigation and therapy. Proc 4th Int Conf on CF. Geigy Symposium Berne/Grundewald 1966 (Modern Problems in Pediatrics Vol 10) PFI p353 Ed. Rossi E, Stoll E. Karger: Basle and New York.
Fig. 34a Warren Warwick Authors’s image
In 2001 Warren Warwick (fig.34a) commented “After 10 years of grants funding the US CF Patient Registry and indirectly supporting the Canadian CF Patient Registry and the beginning of the International Registry, the CF Foundation decided the Registry should become the property of the CF Foundation. When the CF Foundation took over the operation they discovered what a bargain the $10,000 annual grant was. So after spending over $100,000 and still not finishing the analysis, they decided to give up the analysis as too expensive. They were shamed into doing the analysis when the Canadian Foundation provided funds and manpower to complete the analysis. The fallout was that the Canadian Foundation went its own way and beginning the International Registry was abandoned. All the data from the first 10 years of the US Registry, including the magnetic tapes, were transferred to the CF Foundation where they were somehow lost!”
1967 Pugh RJ, Pickup JD. Cystic fibrosis in the Leeds region: incidence and life expectancy. Arch Dis Child 1967; 42:544-545.[PubMed]
Fig 34b. Richard Pugh
This paper is included as it is one of the few reports from the UK of a survey between 1952 and 1962 from the North of England by two excellent Yorkshire paediatricians Richard Pugh of Hull (figure 34b) and Douglas Pickup of Pontefract on behalf of the Leeds Regional Paediatric Club. During this decade 132 infants were confirmed as having CF among total of 546,764 births over 13 years – an incidence of 1/4142. Fifty six infants (42%) died in the first year.
These findings would be typical of the situation in the UK at the time where virtually all children with CF were treated at local hospitals and there were no specialised CF clinics in most towns and cities – or even in most provincial teaching hospitals. So few patients survived childhood. A significant number of affected infants must have gone unrecognised in this early study for the incidence in this part of the UK was later shown to be at least 1/2500 births.
1967 Saggers BA, Lawson D, Stern J, Edgson AC. Rapid method for detection of cystic fibrosis of the pancreas in children. Arch Dis Child 1967; 42:187-189. [PubMed]
A sodium sensitive electrode was used to measure parotid saliva sodium and showed a reasonable separation between CF (12-52 meq/l – 27.2 meq/l mean) and controls (3-15 meq/l mean 5.9 meq/l) with 4% in overlap values of 12-15 meq/l.
– Unfortunately, a later paper on CF screening showed “an undesirably wide” scatter of results in neonates which narrowed by 6 weeks (Lawson et al, Arch Dis Child 1967; 42:689). The method was never used for neonatal screening as not only was it unsatisfactory but also neonatal screening was not recommended at the time in view of the relatively ineffective treatment available in most of the UK. This situation still existed in the Eighties at the time of the West Midlands and Wales trial of neonatal screening (Chatfield et al, 1991 below). Unfortunately, the considerable amount of work on salivary electrolytes never had a significant clinical application (Chernick et al, 1961 above; Chernick & Barbero, 1963 above).
1967 Waring WW, Hal Brunt C, Hilman Bettina C. Mucoid impaction of the bronchi in cystic fibrosis. Pediatrics 1967; 39:166-175.
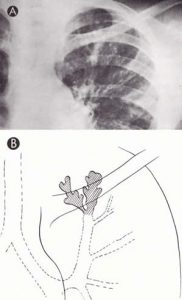
Fig 35. A. Mucoid impaction of bronchi the upper lobe. Double branched opacification with the “inverted cluster of grapes”extends up behind the clavicle in the apical posterior segment of the left upper lobe
Dr Waring noted later in 2002 that Bettina Hilman, Hal Brunt and himself were the first to report a chest radilological sign that is almost specific for CF – mucoid impaction of the bronchi – finger like branching or grape cluster opicifications in one or both lungs produced by the accumulation of radiodense mucopus in bronchiectatic bronchi. he notes that the sign is less frequently seen in recent years as pulmonary therapy improved.

Fig. 37 Bettina C Hillman The Winchester Star

Fig 36. William Waring
Dr William Waring (1923-2023) (figure 36) and Dr Bettina Hillman (1928-2023) (figure 37) were contemporaries and colleagues for many years from the 1960s in New Orleans. Both were prominent in the development of CF care and research in N. Amerca. Dr Hilman developed her own CF centre at Louisiana/Shreveport but continued close cooperation with William Waring at Tulane.
1968 Busey JF, Fenger EP, Hepper NG, Kent DC, Kilburn KH, Matthews LW, Simpson DG, Grzybowski S. The treatment of cystic fibrosis. A statement by the Committee on Therapy. Am Rev Resp Dis 1968; 97:730-734. [PubMed]
This is a concise account of present treatment recommendations by the American Thoracic Society Committee on Therapy. However, Dr LeRoy Matthews appears to be the only CF expert on the committee – in fact, the only person on the committee to have published any papers on CF according to a search of Medline! Treatment by nebulisation is one of the most effective measures where particles of liquid are deposited in the airways and is recommended three or four times a day. Also mist tent therapy is recommended “to add large amounts of water to the pulmonary secretions to liquefy them and thus promote their removal” for “all patients throughout life” and “studies have demonstrated that mist therapy is one of the most effective measures available”. There is a blunt statement that “prophylactic antibiotic therapy is of no value”. The contents are presumably influenced by the views of Leroy Matthews and as such represent a comprehensive account of current treatment with a section on Comprehensive Care. At that time Matthews was a leading supporter of mist tent therapy (Matthews et al, 1967 above).
1968 Schwarz V, Sutcliffe CH, Style PP. Some hazards of the sweat test. Arch Dis Child 1968; 43:695-701. Full article available. [PubMed]
A detailed paper dealing with many practical aspects of the sweat test. Burns and blisters at the site of the electrodes were shown to be caused by penetration of acid generated electrolytically to the vicinity of the patient’s skin. Prevention of these and other errors are discussed in detail. In particular, the rapid evaporation which can occur from the collection pad resulting in up to a twofold increase in concentration of the sweat in 30 seconds – probably this is the major cause of over diagnosis from false high results.
For some years after the Fifties sweat tests were performed in many small laboratories on an occasional basis and many mistakes were made – these were usually false positives and were due to evaporation leading to false high sweat electrolyte values. The acceptance of these results by paediatricians led to over diagnosis (Smalley et al, 1978 below).
Dr Victor Schwarz (1920-1997) of Manchester University joined the staff of the University in 1956 and rose to be Reader in chemical pathology until his retirement in 1985. Schwarz died on 22 July 1997, “remembered for developing a test for patients with cystic fibrosis”.
1968 Esterly J, Oppenheimer E. Observations in cystic fibrosis of the pancreas I: The Gallbladder. Bull Johns Hopkins Hosp 1968:110:247-254.
Reported blockage of the cystic duct by white mucous material. Previous reports on the gall bladder by Jones et al, 1958 (above) and Esterly & Oppenheimer, 1962 (above).
1968 Esterly JR, Oppenheimer EH. Cystic fibrosis of the pancreas: structural changes in peripheral airways. Thorax 1968; 23:670-675. [PubMed]
A detailed report of autopsy findings of 84 patients with CF. There was widespread dilatation of respiratory bronchioles and alveolar ducts in 29 but significant parenchymal destruction in only three patients.
The pathologists John Esterly (1933-1987) of Chicago and Ella Oppenheimer (1897-1981) (figure 25) of Johns Hopkins Baltimore made numerous contributions to the knowledge of the pathology of cystic fibrosis.
Dr. John Esterly (1933-1987), a University of Chicago professor, was an internationally famous pediatric pathologist specializing in diseases of the lungs in newborns. He also had appointments in gynecology and obstetrics and was a member of the Committee on Developmental Biology at the university. He was a quiet, reserved, scholarly type, according to Dr. Werner Kirsten, chairman of the department of pathology. He spent all of his life at universities in pediatric pathology studying the development of the lung. He studied, taught and wrote about diseases of the lung in infants, attempting to explain the pathology of such common causes of perinatal death as the lungs not expanding or filling with fluid. Dr. Esterly received the Fothergill Award from the Scientific Research Society of America.

Fig 38. Ella Oppenheimer
Dr Ella Oppenheimer (figure 38) (1897-1981) Dr Ella Oppenheimer died at the age of 83 and was working in the Department until the day before her sudden death. In her obituary it is said it was impossible to find the right superlative for her services to the Department, and eloquent tributes were paid to her at a memorial service at the School of Medicine. In her memory the departmental library was named The Ella Oppenheimer Memorial Library.
1968 Mearns MB. Simple tests of ventilatory capacity in children with cystic fibrosis. Arch Dis Child 1968; 4:528-539. [PubMed]
The first reports of respiratory function tests in children with CF had been performed by West et al, 1954 (above). In Margaret Mearns’s study from London the results of respiratory function tests were reported. Thirty three of 85 patients had normal FEV1 and FVC but the day to day variability were considered to limit the value of the respiratory function tests. Reversibility in response to bronchodilators was described. Twenty eight had minimal X-ray change, stable and normal; 16 with localised damage had greater reduction in FEV1 than FVC; extensive damage was associated with significant reductions in both. The tests were a valuable aid to clinical assessment especially in those patients with no or little radiological changes.
Margaret Mearns observed that “the present study shows that without the mist tent (given such prominence by Leroy Matthews and others in the USA during the Sixties), but using intensive treatment for acute respiratory illness and very close follow up from the time of diagnosis, children presenting without permanent lung damage can remain well and maintain good respiratory function over a period of years”. (Mist tents were never popular in the UK)
These were early days for respiratory function tests in many paediatric clinics in the UK. The Vitalograph was the first widely available bellows spirometer for non-specialist use. But most general paediatricians in the UK did not have a Vitalograph although most eventually used the Wright peak flow meter. Also few children treated in general paediatric clinics lived to an age when the results would have been reliable – say over six years.
1968 Petersen RA, Petersen VS, Robb RM. Vitamin A deficiency with xerophthalmia and night blindness in cystic fibrosis. Am J Dis Child 1968; 116:662-665. [PubMed]
The first report of night blindness in CF due to vitamin A deficiency in 16 year old girl who had been seriously under-treated and who had major social problems. Later reports showed abnormal nocturnal vision due to vitamin A deficiency (Rayner et al,1989 below) but not where vitamin levels had been monitored regularly and maintained in the normal range (Ansari et al, 1999 below).
1968 Denning CR, Sommers SC, Quigley HJ. Infertility in male patients with cystic fibrosis. Pediatrics NY 1968; 41:7-17. [PubMed]
This is the first report that men with CF were infertile. Repeated sperm analyses in 8 male patients with CF always showed aspermia with low volume and increased turbidity. All the men were in reasonable general condition. In nine patients at autopsy and in one biopsy specimen the testes showed active spermatogenesis but half the sperms had malformed heads. Various explanations for the infertility were discussed including malnutrition, vitamin deficiencies and genetic causes – but not at this stage were abnormalities of the vas deferens suggested as a cause.
– Although “transport difficulties” of the sperms due to viscid secretions in the male are mentioned there is no mention of the maldevelopment of the vas deferens which was eventually found to be the main reason for the infertility; this was described first by Kaplan et al, in 1968 (below) and also by Valman and France in 1969 (below).
1968 Kaplan E, Shwachman H, Perlmutter AD, Rule A, Khaw KT, Holsclaw DS. Reproductive failure in males with cystic fibrosis. N Eng J Med 1968; 279:65-69. [PubMed]
Histological abnormalities of the testis and structural abnormalities of the vas deferens are described; this is the first correct explanation of the male infertility. Twenty five patients aged 17 to 31 years all had aspermia. They could not identify the vas deferens in necropsy specimens from patients aged 5 to 20 years nor in 6 patients during repair of inguinal hernias. These findings provided an explanation for the previously reported infertility of men with CF (Denning et al, 1968 above). The vas deferens was represented by a thin fibrous cord or could not be located; the body of the epididymis was small or absent and the seminal vesicles were either absent, fused or represented in a dilated or bifid sac. The authors considered these were development changes rather than the result of duct obstruction as occurred in the pancreas (See Denning et al, 1968 above; Valman HB, France NE. 1969 below). Later a survey of US CF centres suggested that some 2-3% of men with CF may be fertile (Taussig LM et al. N Eng J Med 1972; 287:586-589).
Dr Elvin Kaplan (1936 – ) later recalled – “My year as a fellow with him (Harry Shwachman) was rich in clinical and personal growth. Harry expected each fellow to write a paper and he eventually suggested the topic he wanted me to explore. It was his idea, his insight and his direction that lead this paper that was published in the New England Journal of Medicine (Kaplan et al, 1968). But he insisted that I be the senior author. It was at that time quite a breakthrough in our understanding of why males were sterile, but Harry took none of the credit. I think this typified his devotion and nurturing of his staff” (Fanos JH. Am J Med Genet 2008; Part A164A:284-293).
1968 Warwick W, Pogue RE. Computer studies in cystic fibrosis. In Lawson D (ed). Proceedings of 5th international Cystic Fibrosis Conference, Cambridge 1969; 320-330. London. Cystic Fibrosis Research Trust.
Warren Warwick has pioneered databases in CF and was responsible for starting the CF Foundation Patient Registry. He maintains that US paediatricians initially only agreed to cooperate with his first CF database as they did not believe Leroy Matthews’s excellent results and thought the data may confirm their suspicion!!!(also Warwick & Manson, 1967).
1968 Hadorn B, Zoppi G, Shmerling DH, Prader A, McIntyre I, Anderson CM. Quantitative assessment of exocrine pancreatic function in infants and children. J Pediatr 1968; 73:39-50.[PubMed]

Fig. 38a Beat Haddorn
One of a number of papers by Hadorn et al on stimulated pancreatic function in CF using a triple lumen tube. The method was used in a few CF Centres, including our own in Leeds, during the Seventies, but it was a difficult test to perform and very invasive for the children. The findings in the present group of 10 children with CF were a low volume of fluid and low bicarbonate output even when the enzyme concentrations were not markedly reduced.
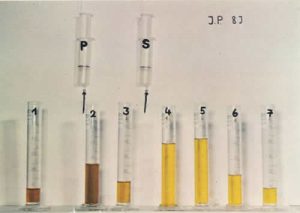
Fig 39. Pancreatic function test. Duodenal aspirate after IV pancreozymin (P) secretin (S).
After intravenous injection of pancreozymin (P) bile stained juice high in enzymes is secreted. After secretin (S) injection the volume and bicarbonate concentration is increased but the enzyme concentrations are reduced (figure 39). In CF the secretion of both is markedly reduced
Also from the same group Zoppi et al. (Helvet Paediatr Acta 1968; 6:577-590) found a higher protein content in the pancreatic juice of both CF and non-CF pancreatic insufficiency using electrophoresis
1968 Hadorn B, Johansen PG, Anderson CM. Pancreozymin secretin tests of exocrine pancreatic function in cystic fibrosis and the significance of the result for the pathogenesis of the disease. Can Med Ass J 1968; 98:377-85. [PubMed]
Thirteen of 176 children with CF in the Melbourne clinic had normal fat excretion. Ten of these pancreatic sufficient patients (PS) had pancreozymin-secretin tests confirming that the water and bicarbonate secretion from the pancreas was more severely affected than the enzyme secretion. They secreted small volumes of pancreatic juice with very low bicarbonate content and but abnormally high enzyme concentrations. Evidence was presented that the pathological features in the pancreas could result from a failure to produce an adequate amount of electrolyte containing fluid.
In the text the authors make the following important comments “it is possible that this (the extensive changes in the pancreas) is at least partially caused by the “organic fraction” which is abnormally concentrated in enzymes. Although proteolytic enzymes are originally present in an inactive form in pancreatic juice it is not unlikely that they may become activated if the flow of secretion is markedly reduced or stagnates. Furthermore, because the secretion is more concentrated and more viscous, blockage of tubules followed by dilatation of the acini may lead to their rupture, and the intraluminal material containing activated enzymes could spread into the surrounding tissue causing irritation and destruction followed by atrophy and fibrosis of parts of the pancreas or entire organ”
This is very likely to be the correct explanation for the early onset of the pancreatic damage starting with the electrolyte/fluid abnormality, now (but not then in 1968) known to be related to abnormalities of fluid and electrolyte transport across the cell membranes and analogous to the changes occurring in other organs – but earlier and more severe as the other organs do not have to contend with the damaging effects of the pancreatic enzymes. Of course, the abnormality of membrane transport had not been described at this stage.
– Pancreatic function had been studied previously by Correia JP & Barros F. (Study of the exocrine function of the pancreas with secretin and pancreozymin. Journal do Medico 1963; 52:581-92). Rick (1963, above) produced an early report of pancreatic function in CF showing reduced volume and reduced bicarbonate secretion (quoted by Wong LTK et al, Gut 1982; 23:744-750). Pancreatic function in CF had been reported first by Maddock et al, 1943 (above), and subsequently by Kopleman et al, 1985 (below). Hadorn’s work seemed to have had more impact (possibly as published in English) and is generally regarded as making the first major contribution to pancreatic function testing in CF.
1968 Doershuk CF, Matthews LW, Gillespie CT, Lough MD, Spector S. Evaluation of jet-type and ultrasonic nebulizers in mist tent therapy for cystic fibrosis. Pediatrics NY 1968; 41:723-732.[PubMed]
Mist tents were still a very popular form of treatment in the USA in the late Sixties particularly in the Cleveland clinic. Ultrasonic nebulisers were said to be better then jet nebulisers for mist tent therapy. However, towards the end of the decade the use of mist tents was increasingly questioned until eventually a number of studies failed to show benefit from the overnight treatment (Bau et al, 1971 below; Norman & Hall Practitioner, 1971; 206: 786-789 below; Motoyama et al, Pediatrics 1972; 50:299; Chang et al, Am Rev Resp Dis 1973; 107:672 below). Certainly the Mistogen compressor nebuliser system gave a very fine dense mist into the tent.
1968 Green MN, Shwachman H. Presumptive tests for cystic fibrosis based on serum protein in meconium. Pediatrics 1968; 41:989-992. [PubMed]
An early suggestion for neonatal CF screening from detection of the increased protein in meconium, a finding which was first described by Buchanan & Rapoport, 1952 (above). Wiser & Beier, 1964 (above) had described raised albumin in the meconium of infants who did not have meconium ileus. Meconium from 49 infants with CF who were siblings of 196 people known to have CF were tested and only 4 gave a negative protein reaction (trichloracetic acid ring test and a slide agglutination test); 1600 control meconium specimens were all negative.
The test was suggested as screening test for CF with 90% reliability. The authors stated – “It is strongly recommended that mass surveys be undertaken only with accompanying facilities for the clinical investigation and treatment of the patients found”. This was very sound advice and lack of centre care for infants with CF detected eventually proved to be a main reason that a large UK Wales & West Midlands neonatal screening study in the Eighties failed to show benefit for the screened infants (Chatfield et al. 1991).
1968 Harries RL, Riley HD Jr. Cystic fibrosis in the American Indian. Pediatr 1968; 41:733-738.
These were the first two children with CF in the American Indian population. Both patients had convincingly high sweat tests and clinical features and were three years eight months and one year 11 months when reported. A sibling of case one who died had the typical pancreatic changes of cystic fibrosis. Caucasian ancestry, if present, was very distant and only on one side of the family and then three generations back. It was suggested that the rarity of CF in Mongolian and American Indians may be related to their common Asian ancestry before the American Indians crossed the Bering Straits into the Western Hemisphere. [PubMed]. Mutation analysis in native American populations of the south west USA were later reported by Grebe et al. (Am J Hum Genet 1992; 51:736-740. [PubMed]).
1968 The Danish CF Centre started at Rigshospitalet in Copenhagen.
Fig 40. Erhard Winge Flensborg
Fig 41. Dr Flenborg’s 90th birthday
Erhard Winge Flensborg (figure 40) (1912-2009) diagnosed the first person with CF in Denmark in 1944. Soon after the Second World War he visited Dorothy Andersen in New York to discuss the Danish cases. Subsequently five patients were published by Flensborg in 1948 (Of the so-called congenital cystic fibrosis of the pancreas. Nord Med 1948; 39:1574). After a number of paediatric appointments Flensborg became head of the Paediatric Department TG, Rigshospitalet, Copenhagen where, in the mid-Sixties, he started the first Scandinavian CF Centre and founded the National Danish Cystic Fibrosis Association. The CF Centre in Copenhagen is today one of the leading international centres of CF research and clinical care. Flensborg retired in 1982 at the age of 69 years and had his 95th birthday in 2007 (figure 41).
The proceedings of the interesting Festschrift at Prof. Flenborg’s retirement were published (Act Paediatr Scand 1982; Suppl 301) and contains details of the 119 CF references published by members of the Danish CF centre up to 1981.
Dr Warren Warwick (Minnesota) wrote in 1982 “Beginning early in the nineteen-sixties the excellence of the work in pulmonary and cystic fibrosis research done at the Paediatrics Department TG attracted interest from around the world and cystic fibrosis (CF) researchers from everywhere began to visit Denmark to learn from Doctor Erhard Winge Flensborg. I joined that group of visitors in 1966 when I wrote to Doctor Flensborg for permission to visit his department. Like all the others, I was welcomed. The intellectual stimulation there surrounded by the sparkling hospitality of Erhard and Inga Flensborg and the doctors studying at Paediatric Department TG was so helpful that I have eagerly returned on many occasions over these past 16 years, as have others who have made a first visit to Paediatric Department TG. For each visitor a first visit was habit forming (Acta Paediatr 1982; 71 (s301):13–14).
1968 Schutt WH, Isles TE. Protein in meconium from meconium ileus. Arch Dis Child 1968; 43:178-181. [PubMed]

Fig. 41a Werner Schutt
I clearly recall this really memorable little cameo presentation by Dr Werner Schutt (1929– 2021) of Bristol at the UK Paediatric Research Society; he eventually became a distinguished paediatric neurologist. The authors state “we have found a simple side room technique helpful in detecting the presence or absence of albumin in significant quantities in meconium”. Protein in meconium of 9 infants with meconium ileus was high at 70% compared with 9% in controls infants and 22% in other cases of neonatal obstruction.
The authors proposed, for the first time, a simple test using the Albustix, a urine dipstick test that turned blue in the presence of the albumin, to detect the increased albumin in the CF meconium. A solution of a few drops of water and a little CF meconium was mixed on a white tile, and the Albustix was laid on the tile with the tip in the solution. There was an impressive blue coloration when there was excess albumin present.
The authors observed that the test “Could provide the basis for a screening test” – which it certainly did – the BM Meconium test! Wiser & Beier (above) were the first to describe the excessive amount of albumin in the meconium of CF infants who did not have meconium ileus (Pediatrics 1964; 33:115-118 above).
1968 Boxerbaum B, Doershuk CF, Pittman S, Leroy W Matthews. Efficacy and Tolerance of carbenicillin in patients with cystic fibrosis. Antimicrob Agents Ch 1968; 8:239-295. [PubMed]
The authors, from the Cleveland clinic, state that “effective therapy of P. aeruginosa has emerged as one of the principal needs to prevent further damage to the lung”. This is the first report of the use of intravenous carbenicillin in 41 people with cystic fibrosis. Pulmonary function tests improved in 80% of patients and 79% had improved X-ray appearances. There were many subsequent publications on the use of carbenicillin in CF. It is interesting that although colistin (also a polymyxin) was considered to have limited clinical value due to “renal toxicity and their disappointing activity in vivo”, colistin is now a widely used antibiotic in CF for P. aeruginosa both by inhalation and intravenously.
1968 Bhakoo ON, Kumar R, Walia BN. Mucoviscidosis of lung. Report of a case. Indian J P 1968; 35: 183-185. [PubMed]
1968 Mehta S, Wadhwa UN, Mehta SK, Chhutani PN. Fibrocystic disease of the pancreas in India. Indian Pediatr 1968; 5:185-191. [PubMed]
First two reports of cystic fibrosis in India. Reviewed by Kabra SK et al (Cystic fibrosis in India. Pediatr Pulmonol 2007; 42:1087-1094.[PubMed]).
1969 Feigelson J, Pecau Y, Shwachman H. A propos d’une paternite chez un malade attient de mucoviscidose: Tudes des fonctions genitals et de la filiation. Arch Fr Pediatr 1969; 26:937-944. [PubMed]
Jean Feigelson told me this was the first instance of proven fertility in a man with cystic fibrosis. Shwachman reviewed the details with Feigelson and agreed with the diagnosis – hence Shwachman was included as an author. It is usually stated that 2-3% of men with CF are fertile and this is more likely with particular genotypes such as 3849-10kb C->T mutation (Dryfus DH et al. Am J Resp Crit Care Med 1996; 153:858-860).
1969 THE FIRST MEETING OF EUROPEAN WORKING GROUP FOR CYSTIC FIBROSIS LATER TO BECOME THE EUROPEAN CYSTIC FIBROSIS SOCIETY (ECFS)

Fig 42. Ettore Rossi. ECFS
In 1969, following an informal meeting held at Interlaken chaired by Prof Ettore Rossi (see figure 42 below) a European Working Group for Cystic Fibrosis (EWGCF) was formally founded later that year at a satellite meeting held during the 5th International Cystic Fibrosis Conference in Cambridge. Prof Ettore Rossi was the EWGCF’s first chairman. The purpose of the EWGCF was to provide an annual forum where people from the various disciplines but with a common interest in CF could meet, present and discuss their latest findings. In 1997, the board proposed an official transformation of the EWGCF to a Society. This change together with a new constitution was approved at the Annual General Meeting held during the 21st European CF conference in Davos, June 1997. The first President of the ECFS was Prof. Niels Høiby. (Note: the Society was first called the European Society for Cystic Fibrosis (ESCF) but as the initials were the same as another group, the name was changed at the next annual conference in Berlin) (History based on information from the ECFS website)
Between 1970 and 2000, an annual conference was held in different European countries, but suspended every fourth year when there was an International CF Conference.
From 2002 to 2007 the Ettore Rossi Medal Award was presented at the annual conference to honour a person who has made an outstanding contribution to our basic understanding of cystic fibrosis or to the treatment or care of patients with cystic fibrosis. In 2008 the ECFS Award was introduced to perpetuate the tradition of the Rossi Award. I was proud to be awarded the Rossi Medal in 2004.

Fig 43. Presentation of the ECFS award to Gerd Doring by the President Stuart Elborn
Professor Stuart Elborn (figure 43) has been President of the ECFS since 2007/8 during which the size and role of the ECFS has considerably expanded
In 2004, the ECFS took over the responsibilities for another annual conference which is entirely dedicated to basic science. These conferences are characterised by active discussion of data and ideas at the forefront of research on CF and CFTR, in an informal, co-operative environment. The ECFS acknowledges the enormous contribution of Prof. Margarida Amaral (figure 44) in establishing these conferences on the international stage.
The Journal of Cystic Fibrosis (JCF) was first published in 2002 with Dr. Harry Heijerman being the first Editor-in-Chief. The JCF is the official journal of the European Cystic Fibrosis Society and is devoted to promoting the research and treatment of cystic fibrosis. The JCF has been an outstanding success.
The ECFS has been organising regular consensus meetings over a number of years. The reports culminating from these meetings are submitted for publication in the Journal of Cystic Fibrosis and published on the ECFS website. Prof Gerd Döring,(figure 43) the 2nd ECFS President, was very instrumental in initiating this tradition.

Fig 44. Mararida Amaral receiving the 2010 ECFS award . L to R David Sheppard, Amparo Sole, Stuart Elborn
EuroCareCF, an EU funded project led by Dr. David Sheppard (figure 44) from Bristol University, paved the way for two important projects for the ECFS – a European Clinical Trials Network and the further development of the European CF Patient Registry. Under the initial leadership of Prof. Kris De Boeck, the Clinical Trials Network was established in 2008.
The ECFS Patient Registry has been collecting data from both national and single centre European registries over a number of years.As one of the principle aims of the ECFS is to foster the best possible care for people with cystic fibrosis, a new Standards of Care project was established in 2011 under the direction of Dr. Carlo Castellani. The three main areas being addressed are Best Practice, Centre Framework and Quality Management.

Fig 44a. Christine Dubois
Since 2000 the affairs of the ECFS have been ably managed by Christine Dubois (figure 44a)
Professor Rossi (figure 42) (1915-1998) was Chairman of the Department of Paediatrics of the University of Berne, Switzerland from 1956 until he retired in 1985. He was one of the central figures involved in the development of very many areas of paediatrics in Europe, including cystic fibrosis.
I met Professor Rossi only briefly on a few occasions – one incident left me with a lasting impression of his kindness and humanity. At an International CF Conference, when he was chairing a plenary session, he had no hesitation in informing one very senior presenter, who had just described of a study involving children with CF in numerous annual needle biopsies of the liver, in no uncertain terms, precisely what he thought of the ethics of the study! He was obviously held in high regard by those who knew him and described as an enthusiastic teacher, a serious hard working paediatrician and a superb medical friend – “the beloved father of hundreds of paediatricians in the whole world”.
Professor Niels Hoiby delivered a lecture at the 30th ECFS Conference at Belec Turkey in 2007 on the “History of the European Working Group for Cystic Fibrosis and the European Cystic Fibrosis Society Conferences”. He kindly allowed me to use his Power point presentation as a basis for an account of his lecture which I have edited and included in the “More Historical Things” Topic of this website – listed in the subjects included at the start of that Topic
1969 McCarthy DS, Pepys J, Batten J. Hypersensitivity to fungi in Cystic fibrosis. Proceedings of the 5th International Cystic Fibrosis Conference, Cambridge. P194. Ed. Lawson D. Cystic Fibrosis Trust, London.
Positive skin test reactions to common allergens were present in 50% of 37 patients with cystic fibrosis. Many subsequent papers reported an increase in atopy in people with CF although clinical manifestations of allergy have not proved a major problem with the exception of allergic bronchopulmonary aspergillosis and more recently the frequent allergic reactions to intravenous antibiotics – which are now both major problems.(also Price et al, 1979 below).
1969 Milner AD. Blood glucose and serum insulin levels in children with cystic fibrosis. Arch Dis Child 1969; 44:351-355. [PubMed]
Fig. 44c Anthony David Milner RCPCH.ac.uk
One of the early studies on glucose metabolism from Great Ormond Street, London by Tony Milner at a time when few patients survived to an age when they developed diabetes. However, it had been predicted that this might occur as patients became older. Glucose and insulin levels were measured after oral glucose and intravenous glucose, glucagon and tolbutamide in 61 children with CF. The results suggested that the increased incidence of impaired glucose tolerance was due to a defect in the release of an glucagon-like substance from the alimentary system in addition to defective islet cell function. (also Rosan et al, 1962 above; Huhnstock K & Schwarz G, 1961 above).
Anthony (Tony) Milner (Fig. 44c) ( – 2021) eventually described as “the father of modern respiratory paediatric research” subsequently had a very distinguished career in London primarily at Guys Hospital and Great Ormond Street.
1969 Lawson D. Panel discussion on microbiology and chemotherapy of the respiratory tract in cystic fibrosis. Proc 5th Int CF Conference, Cambridge, 1969. Ed. Lawson D. London. Cystic Fibrosis Research Trust 1969:225.
Fig. 44d David Lawson
David Lawson was one of the first paediatricians to suggest long term anti-Staphylococcal prophylactic chemotherapy. Eventually this treatment was supported by a controlled trial in CF screened infants in East Anglia, UK (Weaver et al, 1994 below). Prophylactic flucloxacillin is now recommended for all CF infants in the first 3 years by the UK CF Trust’s Expert Antibiotic Group (2002 and 2009) although the findings are not accepted in North America.
I was impressed by David Lawson’s approach and from 1975 all CF children for whom I was responsible were on long term cloxacillin and later flucloxacillin from soon after birth, if screened, or from the time of diagnosis. The results of this policy were reported in 1993 by Kevin Southern at the Madrid ECFS meeting. Of 110 patients attending our unit for all their care at that time only 16 (14.5%) had chronic Staph. aureus infection – individual group prevalence in 0-4 years nil, 5-9 yrs 14.7%, 10-15 yrs 22%; furthermore some of those patients had been referred to our clinic already chronically infected with S. aureus. The Leeds CF centres still have most patients on continuous flucloxacillin and there is a very low prevalence of chronic Staphylococcal infection. It is also interesting that despite the publications suggesting anti-Staphylococcal prophylaxis leads to a higher prevalence of Pseudomonas infection, this does not occur if there is also a policy of regular cultures and early Pseudomonas eradication.
David Lawson,(1917-2004) whose daughter had CF, was one of the founders of the UK CF Research Trust in 1964. He maintained that earlier diagnosis, by improved neonatal screening, was essential for improvement of results as by the time the diagnosis was presently made lung damage was already present. In 1953, David was appointed as a consultant paediatrician and medical administrator at Queen Mary’s Hospital for Children, Carshalton, and later became a clinical tutor. He also held consultant posts at Epsom District Hospital and at the Royal Marsden Hospital.
At Queen Mary’s, he established a pioneering specialist clinic for children with cystic fibrosis. Sarah Walters, one of his patients, who went on to become a doctor and a fellow of the RCP, first met him as a child: ‘Here was a doctor who didn’t think it was a waste of time to do blood tests and X rays, to monitor my lung function and to treat the infections in my chest. Here was a doctor who wanted the very best for me, and for all his CF patients. Here was a doctor who gave me hope.’
David Lawson was one of the founders and a chairman of the Cystic Fibrosis Research Trust, and secretary of the scientific/medical committee of the International Cystic Fibrosis Association, based in New York. He wrote extensively, including papers on intra-cranial neoplastic diseases of childhood, the management of coeliac disease, meningitis and on cystic fibrosis.
1969 Valman HB, France NE. The vas deferens in cystic fibrosis. Lancet 1969; ii: 566-567.[PubMed]
Fig 45. Bernard Valman
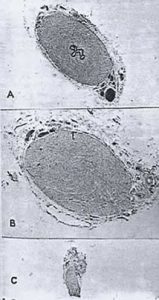
Fig 46. a.Photomicrograph of the vasa differentia to show variable changes b.normal vas c.Thin muscle cord representing distal vas. With permission
One of the early reports of the abnormalities of the vas deferens which explained the infertility first reported in detail by Denning et al – first at the CF Club 1966 and later published in 1968. Also this paper confirmed the abnormalities of the vasa differentia subsequently described by Kaplan et al, 1968 (above) as the cause of the infertility and showed the changes could be variable. Bernard Valman (figure 45) studied the post mortem appearance of the vasa differentia in 10 boys with CF. In all the boys the vasa were either absent or reduced to a fibrous or muscular band suggesting that the mesonephric duct had been obliterated during the 10th or 12th week of fetal life (figure).
1969 Phelan PD, Gracey M, Williams HE, Anderson CM. Ventilatory function in infants with cystic fibrosis. Physiological assessment of inhalation therapy. Arch Dis Child 1969; 44: 393-400. [PubMed]

Fig 47. Peter Phelan performing infant respiratory function tests. Kindly provided by Dr Sarath Ranganathan
An early (possibly the first?) study of respiratory function in CF infants (figure 47). Total gas volume, dynamic compliance and mean pulmonary resistance were measured in 18 infants less than 9 months old. Nine infants with no infection and others with infections all returned to normal when treated with intermittent inhalations of propylene glycol 10%, glycerine 2%, in 0.9% saline 2ml + 0.25 ml of 2% orciprenaline 1-4 x daily.
More recent studies of infant respiratory function show a mild but consistent degree of airways obstruction and hyperinflation even in uninfected young infants with cystic fibrosis (Ranganathan SC et al, Lancet 2001; 358:1964-1965).
1969 Lawson D. Discussion on the therapeutic and prophylactic use of mist tents. Proc 5th Int CF Conference, Cambridge, 1969. Ed. Lawson D. London. Cystic Fibrosis Research Trust 1969:149-168.
Opinions of many of the leading authorities of the time were divided but all agreed there was a need for clinical trials. The Europeans and North Americans were in favour of mist tents but UK were not. The discussion seemed to move towards nebulised antibiotics; Leroy Matthews was enthusiastic about nebulised gentamicin later used with carbenicillin by Margaret Hodson (Hodson et al, 1981 below).
1969 Hide DW, Burman D. An infant with both cystic fibrosis and coeliac disease. Arch Dis Child 1969; 44:533-535. [PubMed]
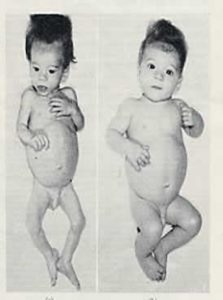
Fig 48. Infant before and after starting gluten free diet. From Hide DW, Burman D 1969. With permission
The first convincing description of both coeliac disease and CF in a marasmic infant (figure 48) from David Burman’s paediatric unit in Bristol. The sweat test was re-checked when the infant was thriving and was strongly positive. In addition to the abnormal jejunal biopsy, which showed subtotal villus atrophy, the infant reacted violently when challenged with gluten at the age of a year.
Subsequently children with both conditions were reported also by Goodchild MC, et al. Arch Dis Child 1973; 48:684-691; Katz A et al, Pediatrics 1976; 57:715). Later studies have shown a slight increase in incidence of coeliac disease in people with cystic fibrosis (Valetta EA, Mastella G. Acta Paediatr Scand 1989; 78:784-785 below).
1969 Noblett HR. Treatment of uncomplicated meconium ileus by gastrografin enema. A preliminary report. J Pediatr Surg 1969; 4: 190-197. [PubMed]
A major milestone in the treatment of meconium ileus, the first being the surgical management described by Hiatt & Wilson in 1953 (above); then the Bishop Koop ileostomy (1957 above). This is the first reported use of diatrizoate maglumine (Gastrografin) enemas for meconium ileus. Later reported from Liverpool as effective in meconium ileus equivalent in older patients when given by mouth (O’Halloran et al, 1986 below).

Fig. 48a Helen Noblett. baps.org.uk
Helen Noblett (1933-2020) Fig.48a Helen Noblett was a pioneering and innovative paediatric surgeon. She was born in South Australia she did her undergraduate medical training in Brisbane having entered on a scholarship, qualifying in 1957. She did junior hospital jobs in Brisbane, proceeding to general surgery and then paediatric surgery in Brisbane Children’s Hospital in 1962. She eventually moved to the UK where she became the consultant paediatric surgeon in Bristol. Helen Noblett deserves to be remembered as a great character and a paediatric surgeon of the highest calibre. Her other major contribution was a rectal suction biopsy device of her own invention used in the diagnosis of Hirschsprung disease.
1969 Gracey M, Burke V, Anderson CM. Treatment of abdominal pain in cystic fibrosis by oral administration of n-acetyl cysteine. Arch Dis Child 1969; 44:404-405. [PubMed]
For patients with troublesome abdominal pain, 5 ml of a 20% solution N-acetyl cysteine with 50% water was given four times daily. Five of the six patients ceased having pain within a week – the other patient refused to take the treatment. The authors were prompted to try the treatment by the first report of a 26 year old man with CF reported by Lillibridge CB et al,(J Pediatr 1967; 71:887) whose

Fig 49. Michael Gracey
abdominal pain responded impressively with N-acetylcysteine 30 ml three times daily by mouth.
A particularly useful report as the results of surgery for meconium ileus equivalent were still poor.
Dr Michael Gracey ( -2021) (figure 49) is Professor of Child Health, University of Western Australia. He published a number of papers on cystic fibrosis around the time of this paper, when he collaborated with Charlotte Anderson and Valerie Burke contributing the CF sections to their gastroenterolgy text book, also on a wide variety of gastroenterological topics and environmental health. He has travelled widely and his career has focussed on improving the health of infants and children in developing countries and of Aboriginal children in Australia. Michael Gracey was designated the Most Outstanding Paediatrician in Asia in 1997, received the Medal of Honour of the International Paediatric Association in 2001 and was made an Honoured professor of the Kazakh State Medical University in Almaty, Republic of Kazakhstan, in the same year.1969
1969 Anonymous. Inhalation and mist tents in cystic fibrosis. Lancet 1969; 2(7626):891-892. [PubMed]
A review of the increasing doubts regarding the use of mist tent therapy noting that most of the liquid was deposited in the upper respiratory tract – although breathing through a wide bore tube was more effective. Although Leroy Matthews is mentioned as producing evidence of a beneficial effect (Matthews et al, 1967 above) it was suggested that trial should be given to all sorts of inhalation therapy for the individual patient, either intermittent aerosols or mist tents. A controlled trial seemed to be indicated.
1969 Dooley RR, Moss AJ, Wright PM, Hassakis PC. Norethandrolone in cystic fibrosis of the pancreas. J Pediatr 1969; 74: 95-102. [PubMed]
Twenty eight severely affected patients were treated with the anabolic steroid norethandrolone in the 5 years up to 1968. All the patients showed immediate improvement in appetite, activity and weight gain; also their respiratory function improved. Six patients died and there were a variety of side effects side effects including virilisation (also Kunstadter et al, 1961 above). However, there was great interest in this treatment as all else had failed to achieve weight gain in some of these patients.The subject was reviewed in 1981 by Richard Dooley (Anabolic steroids. In 1000 years of Cystic Fibrosis. Warren Warwick (ed). University of Minnesota, 1981).
1969 Louria DB, Young L, Armstrong D, Smith JK. Gentamicin in the treatment of pulmonary infections. J Infect Dis 1969; 119:483-485. [PubMed]

Fig. 50 Donald B Louria
A report of the use of intravenous gentamicin in a variety of respiratory infections including 30 patients with cystic fibrosis. Intravenous gentamicin was administered over periods ranging from three weeks to 16 months and the response to treatment was classified as good in 20 patients, moderately improved in 7 and ineffective in 3. The drug was reported as often valuable in infections due to Pseudomonas aeruginosa.
Donald B Louria (1928-2021) (Fig. 50) was an expert on infectious diseases, preventive medicine and drug abuse. He had a variety of academic and national appointments finally 30 years as Chair of the Department of Preventative Medicine and Community Health in the New Jersey Medical School.



