Chest
Early chest involvement, Atelectasis, Haemoptysis, Pneumothorax, non-invasive ventilation, Other
Early chest involvement – detection and treatment
VanDevanter DR, Kahle JS, O’Sullivan AK, Sikirica S, Hodgkins PS. Cystic fibrosis in young children: A review of disease manifestation, progression, and response to early treatment. J Cyst Fibros. 2016 Mar;15(2):147-57. Free full text [PubMed]

Donald (Dutch) VanDevanter
The authors observe that studies have described illness associated with cystic fibrosis (CF) early in life, but there is no comprehensive accounting of the prevalence and ages of disease manifestation and progression described in individual studies. They searched for peer-reviewed English-language studies of the health of children ≤6years old with CF (published 1990-2014). Structural abnormalities and dysfunction of the digestive and respiratory systems were summarized across relevant studies by system and age group. Primary studies (125 total) from 22 countries described abnormalities, dysfunction, and disease progression in infancy and early childhood. Improved health was consistently observed in association with diagnosis via newborn screening compared with cohorts diagnosed later by symptomatic presentation.
In conclusion, they found the peer-reviewed literature to be remarkably consistent regarding all three of the three initial research questions they posed.
(1) At what ages have CF-related dysfunction and structural differences been demonstrated in young children with CF (≤ 6 years of age)? CF-associated growth impairment and airway abnormalities are reported at birth and the underlying pathology of CF directly related to reduced CFTR protein function was demonstrated in young children with CF. Abnormalities and dysfunction of the digestive and respiratory systems were reported throughout early childhood in CF.
(2) At what ages has disease progression been reported in young children with CF? Disease progression is reported in infancy and throughout childhood. The youngest age at which disease progression was reported was by the age of 6 months in both digestive (pancreatic sufficiency decline) and respiratory systems (lung function decline). Accumulation of lung damage was reported by 1 year of age, and lung structure and function worsened significantly each year of life in young children, with potentially irreversible lung damage reported by the age of 2 years.
(3) At what ages are there improved outcomes with early versus late treatment initiation in young children with CF? Earlier access to routine CF management improved subsequent health status. Earlier diagnosis (by 4–14 months) and standard-of-care treatment initiation in infancy compared with later diagnosis and subsequent treatment initiation improved long-term outcomes, including survival.
Dr Donald (Dutch) VanDevanter is an Adjunct Professor of Pediatrics, Case Western Reserve University School of Medicine, Cleveland.
– This is a valuable extensive review (143 references) of a very important topic which is attracting increasing interest as it is appreciated that damage from abnormal CFTR function occurs very early – even in utero – and is usually irreversible. It is of particular interest as more effective modulators become available for use in young children.
2016 Darrah RJ; Mitchell AL; Campanaro CK; Barbato ES; Litman P; Sattar A; Hodges CA; Drumm ML; Jacono FJ. Early pulmonary disease manifestations in cystic fibrosis mice. J Cyst Fibros 2016 May 23. [PubMed]
The authors investigated young CF mice to determine if they exhibit pulmonary pathophysiology consistent with the early CF lung phenotype. Lung histology and pulmonary mechanics were examined in 12- to 16-week-old congenic C57bl/6 F508del and R117H CF mice using a forced oscillation technique (flexiVent). RESULTS: There were no significant differences in the resistance of the large airways. However, in both CF mouse models, prominent differences in the mechanical properties of the peripheral lung compartment were identified including decreased static lung compliance, increased elastance and increased tissue damping. CF mice also had distal airspace enlargement with significantly increased mean linear intercept distances.An impaired ability to stretch and expand the peripheral lung compartment, as well as increased distances between gas exchange surfaces, were present in young CF mice carrying two independent Cftr mutations. This altered pulmonary histopathophysiology in the peripheral lung compartment, which develops in the absence of infection, is similar to the early lung
– These findings of early structural abnormalities in the absence of infection are in keeping with previously described tracheal and histological abnormalities.
Davis SD, Ratjen F, Brumback LC, Johnson RC, Filbrun AG, Kerby GS, Doumit M, Belessis Y; Stelzer-Braid S; Mallitt KA; Rawlinson W; Jaffe A. Diagnostic accuracy and distress associated with oropharyngeal suction in cystic fibrosis. J Cyst Fibros 2016; 15(4):473-8. [PubMed]
This study aimed to assess the diagnostic accuracy of oropharyngeal suction (OPS) samples in obtaining airway bacterial cultures in young children with cystic fibrosis (CF), and the level of child distress caused by obtaining OPS samples.Young children with CF undergoing broncho-alveolar lavage (BAL) as part of concurrent research or routine annual surveillance were studied. OPS was performed by stimulating a cough and suctioning the back of the oropharynx in the awake child to replicate clinical practice. BAL of the right upper, middle and lingula lobes was then performed. Samples were sent for standard bacterial culture. The child’s distress during OPS was rated using the Groningen Distress Scale (1=calm, 2=timid/nervous, 3=serious distress but still under control, 4=serious distress with loss of control, 5=panic).
There were 65 paired samples obtained from 39 children (21 boys, mean age on day of first sampling was 34.1 months, SD 19.1 months). For Pseudomonas aeruginosa, specificity, sensitivity, NPV and PPV with 95% CI were 98% (87-99), 75% (20-96), 98% (91-98) and 60% (15-93%) respectively. In all age groups combined, median level of distress was 3 (IQR 2-4), with distress highest in 2 and 3 year olds, with a median of 4 (IQR 3-4).-
The authors concluded OPS has diagnostic utility in determining the absence of organisms in the lower airway, with specificity for P. aeruginosa detection of 98%. However, a positive OPS result is not necessarily a good indicator of lower airway infection. Distress levels were high during OPS, mostly in 2 and 3 year olds. They suggest there is a need for interventions to reduce distress or to find alternative methods which are less distressing.
Lahiri T, Hempstead SE, Brady C, Cannon CL, Clark K, Condren ME, Guill MF, Guillerman RP, Leone CG, Maguiness K, Monchil L, Powers SW, Rosenfeld M, Schwarzenberg SJ, Tompkins CL, Zemanick ET, Davis SD. Clinical Practice Guidelines From the Cystic Fibrosis Foundation for Preschoolers With Cystic Fibrosis. Pediatrics. 2016 Mar 23. pii: peds.2015-1784. [Epub ahead of print] [PubMed](Available to download from CFF website) Cystic fibrosis (CF) clinical care guidelines exist for the care of infants up to age 2 years and for individuals ≥6 years of age. An important gap exists for preschool children between the ages of 2 and 5 years. This period marks a time of growth and development that is critical to achieve optimal nutritional status and maintain lung health. Given that disease often progresses in a clinically silent manner, objective and sensitive tools that detect and track early disease are important in this age group. Several challenges exist that may impede the delivery of care for these children, including adherence to therapies. A multidisciplinary committee was convened by the CF Foundation to develop comprehensive evidence-based and consensus recommendations for the care of preschool children, ages 2 to 5 years, with CF.
2016 Psoter KJ; DE Roos AJ; Wakefield J; Mayer JD; Bryan M; Rosenfeld M. Association of meteorological and geographical factors and risk of initial Pseudomonas aeruginosa acquisition in young children with cystic fibrosis. Epidemiol Infect 2016; 144(5):1075-83.[PubMed]
Meteorological and geographical factors and risk of initial Pa acquisition in young children with CF were examined using the U.S. Cystic Fibrosis Foundation Patient Registry from 2003 to 2009. The results suggest that environmental factors may play a previously unrecognized role in the aetiology of initial Pa acquisition.
– The authors concluded meteorological and geographical factors, particularly increased temperature, dew point and rainfall were found to be associated with time to initial Pa acquisition in young children with CF. They have published on this subject previously
2016 Zampoli M; Pillay K; Carrara H; Zar HJ; Morrow B.Microbiological yield from induced sputum compared to oropharyngeal swab in young children with cystic fibrosis. J Cyst Fibros 2016; 15(5): 605-10. [PubMed]
Standard respiratory sampling in young children with cystic fibrosis (CF) is by oropharyngeal swab (OPS) as they cannot spontaneously expectorate. The authors consider sputum induction (IS) has been poorly investigated in this population. They aimed to compare the bacteriological yield of OPS vs. IS in young children with CF. They confirm sputum induction is feasible, safe and superior to OPS for detecting CF-associated bacteria in young children with CF.
– A little unkind to previous paediatric studies (see paper) but a useful paper from South Africa by people with experience in diagnosing TB and other respiratory infections in young children.
Heather Zar is Head of Paediatric Pulmonology, Red Cross Children’s Hospital, Capetown.
Marco Zampoli is a consultant paediatrician in the Red Cross Children’s Hospital Capetown.
2016 Britton LJ, Oates GR, Oster RA, Self ST, Troxler RB, Hoover WC, Gutierrez HH, Harris WT. Risk stratification model to detect early pulmonary disease in infants with cystic fibrosis diagnosed by newborn screening. Pediatr Pulmonol. 2016 Nov;51(11):1168-1176. doi: 10.1002/ppul.23536. Epub 2016 Aug 24. [Pubmed]
The clinical benefit of newborn screening (NBS) for cystic fibrosis (CF) has been primarily nutritional, with less overt respiratory impact. Identification of risk factors for infant CF lung disease could facilitate targeted interventions to improve pulmonary outcomes. This retrospective study evaluated socioeconomic information, clinical data, and results from routine infant pulmonary function testing (iPFT) of infants diagnosed with CF through NBS (N = 43) at a single CF center over a 4-year period (2008-2012). A five-item composite clinical score was developed and combined with socioeconomic indicators to facilitate identification of CF infants at increased risk of early-onset respiratory impairment.
Paternal education was positively associated with lung function (P = 0.02). Clinical score <7 (on a scale of 0-10) predicted diminished pulmonary measure (P < 0.005). Retrospective risk stratification by clinical score and paternal education identified CF infants at low, intermediate, or high risk of pulmonary disease. Forced expiratory volume (FEV0.5 %, mean ± SD) averaged 115 ± 19% in the low-risk group, 97 ± 17% in the intermediate-risk group, and 90 ± 8% in the high-risk group (P < 0.005). Results were similar for mid-expiratory flows (FEF25-75 %). Multiple regression analysis confirmed the predictive value of this risk stratification model of CF infant pulmonary health.
The authors combined socioeconomic and clinical data to risk-stratify CF infants for early-onset lung disease as quantified by iPFT. Their model showed significant differences in infant pulmonary function across risk groups. The developed tool offers an easily available, inexpensive, and non-invasive way to assess risk of respiratory decline in CF infants and identify those meriting targeted therapeutic attention.
~ A useful contribution to aid identification of the substantial number of infants who develop early lung diseases despite being identified in the first weeks by newborn screening.
William T Harris, the corresponding author, is Assistant Professor and Director of the Pediatric Research Bronchoscopy Program at the Children’s of Alabama
Caudri D, Turkovic L, Ng J, de Klerk NH, Rosenow T, Hall GL, Ranganathan SC, Sly PD, Stick SM; AREST CF. The association between Staphylococcus aureus and subsequent bronchiectasis in children with cystic fibrosis. J Cyst Fibros. 2017 Dec 21. pii: S1569-1993(17)30980-3. doi: 10.1016/j.jcf.2017.12.002. [Epub ahead of print] [Pubmed] Staphylococcus aureus (S. aureus) may be related to more rapid progression of cystic fibrosis (CF) lung disease. In the AREST CF cohort study, children diagnosed with CF undergo annual bronchoscopies with bronchoalveolar lavage and ultra-low-dose, chest computed tomography (CT) up to 6-years-old. Spirometry was assessed 3-monthly from the age of 4years. Associations between de novo S. aureus acquisition before school age and CT and lung function at ages 5-7years were investigated. Models were adjusted for multiple markers of disease severity at baseline.
De novo S. aureus acquisition at 3-years-old (n/N=12/122) was associated with increased bronchiectasis score at age 5-6years. This association decreased but remained significant after adjustment for confounders. S. aureus at 3 was associated with significantly reduced FEF25-75 at age 5-7years, but not with FEV1-%-predicted. De novo S. aureus acquisition at age 3 is associated with later bronchiectasis and FEF25-75 in children with CF.
– These findings are very important and not surprising. They lend support to the, oft criticised, UK guideline recommendation for long-term flucloxacillin from birth during the early years. The unnecessarily high proportion of CF patients chronically infected with SA in many countries (amounting on average to almost 50% of patients – ECFS patient Registry 2014) compared with the very low incidence in the UK (15.48%) is a refection of the early aggressive approach to eradication and prevention of SA infection pioneered in the UK by the late Dr. David Lawson, who first advised anti-staphylococcal prophylaxis from diagnosis and it is still recommended in the UK.
2017 Cigana C, Bianconi I, Baldan R, De Simone M, Riva C, Sipione B, Rossi G, Cirillo DM, Bragonzi A. Staphylococcus aureus impacts Pseudomonas aeruginosa chronic respiratory disease in murine models. J Infect Dis. 2017 Dec 5. doi: 10.1093/infdis/jix621. [Epub ahead of print] [Pubmed]
Staphylococcus aureus and Pseudomonas aeruginosa are key bacterial pathogens of the respiratory tract in patients with cystic fibrosis. While P. aeruginosa chronic bronchial infection is associated with a poorer prognosis, the consequences of S. aureus colonization on CF outcomes are controversial. In this paper, murine models of infection resembling traits of the CF human airways disease have been revisited using an infection schedule that mimics the sequence of events of pulmonary disease in CF patients. First, mice were infected with S. aureus, embedded in agar beads; this was followed by P. aeruginosa infection and analysis of bacterial load, leukocyte infiltration, and lung tissue damage.
The authors concluded that: i) S. aureus promotes severe lesions including abscess formation, ii) S. aureus increases the risk of subsequent chronic P. aeruginosa respiratory infection, iii) once the chronic infection has been established, P. aeruginosa influences most of the inflammatory responses independent of S. aureus.
The authors suggest their findings establish the significance of S. aureus colonization per se and the impact on the subsequent P. aeruginosa infection. This would point towards a thorough assessment for the need of treatment against S. aureus.
– The need for treatment of S. aureus is clear. The organism should always be treated aggressively and eradicated whenever possible. However, if the infection has been ignored, as obviously happens not infrequently in some CF centres, it would be wise to give long term oral anti-staphylococcal therapy to limit subsequent damage.
2017 D’Sylva P, Caudri D, Shaw N, Turkovic L, Douglas T, Bew J, Keil AD, Stick S, Schultz A. Induced sputum to detect lung pathogens in young children with cystic fibrosis. Pediatr Pulmonol. 2017 Feb;52(2):182-189. doi: 10.1002/ppul.23636. Epub 2016 Nov 30. [Pubmed]
Microbiological culture results were compared between 61 paired induced sputum and bronchoalveolar lavage fluid samples from young children with cystic fibrosis. The first cohort received no airway clearance and the second cohort received airway clearance. Induced sputum was sampled within 7 days of bronchoscopy. The Median age (range) of participants was 3.3 years (0.9-6.7). Sensitivity and specificity (95%CI) of induced sputum was 36.8% (16.3, 61.6), and 69% (52.9, 82.4), respectively (N = 61). In subgroup analysis, induced sputum with (N = 31) and without airway clearance (N = 30) demonstrated sensitivity of 50% (15.7, 84.3) and 27.3% (6.0, 61.0), respectively, and specificity of 60.9% (38.5, 80.3), and 78.9% (54.4, 93.9), respectively.
– The authors concluded that induced sputum is not highly sensitive or specific as routine surveillance for detection of lower airway pathogens in young children with cystic fibrosis. It seems there is still merit in performing quite frequent cultures thus increasing the chance of identifying a significant pathogen – in some CF centres these are performed on every attendance and when any new respiratory symptoms occur.
2017 Ranganathan SC, Hall GL, Sly PD, Stick SM, Douglas TA; Australian Respiratory Early Surveillance Team for Cystic Fibrosis (AREST-CF). Early Lung Disease in Infants and Preschool Children with Cystic Fibrosis. What Have We Learned and What Should We Do about It? Am J Respir Crit Care Med. 2017 Jun 15;195(12):1567-1575. doi: 10.1164/rccm.201606-1107CI.[Pubmed] The past decade has seen significant advances in understanding of the pathogenesis and progression of lung disease in cystic fibrosis (CF). Pulmonary inflammation, infection, and structural lung damage manifest very early in life and are prevalent among preschool children and infants, often in the absence of symptoms or signs. Early childhood represents a pivotal period amenable to intervention strategies that could delay or prevent the onset of lung damage and alter the longer-term clinical trajectory for individuals with CF. This review summarises what we have learned about early lung disease in children with CF and discusses the implications for future clinical practice and research.
– This is an excellent article reviewing the present situation regarding the need for more effective early monitoring and treatment to prevent the development of bronchiectasis in up to 80% of children by the age of 5 years with the long-term consequences. The author considers an “attitudinal change within CF clinics in important with increased attention of the early years in the establishment of lung disease’ with “policies and guidelines that lead to a more unified proactive approach care in asymptomatic and apparently healthy young children rather than an acceptance of a casual or reactive approach”.
The author discuses in some detail the options which are already available multidisciplinary care at a CF centre modifiable psychological risk factors, home treatment, and adherence. Antibiotics for CF pathogens detected in both symptomatic and asymptomatic individuals. Early eradication of of P. aeruginosa. Mucolytic and the anti-inflammatory actions of macrolides and antibiotics targeting eradication of S. aureus and H. influenzae even in the absence of symptoms. Bronchoscopy is indicated when response to treatment is suboptimal. Introduction of mucolytics at an early stage. Nutritional strategies for the rapid regain of birth weight and normalising fat-soluble vitamin levels. Increased frequency of clinical review and a lower threshold for intensive multidisciplinary review and a lower threshold for admissions for intensive multidisciplinary therapy. He then discusses moving treatments into the preschool period and assessing the CFTR modulators in young children.
Associate Professor Sarath Ranganathan is a full-time specialist in paediatric respiratory medicine and director of Respiratory Medicine at the Royal Melbourne Children’s Hospital. He is an expert in the field of clinical respiratory physiology and early lung disease.
2017 Stanojevic S; Davis SD; Retsch-Bogart G; Webster H; Davis M; Johnson RC; Jensen R; Pizarro ME; Kane M; Clem CC; Schornick L; Subbarao P; Ratjen FA. Progression of Lung Disease in Preschool Patients with Cystic Fibrosis. Am J Respir Crit Care Med 2017; 195(9):1216-1225, 2017 May 01.[Pubmed]
A study to define the utility of the Lung Clearance Index (LCI), measured by multiple breath washout, as a means to track disease progression in preschool children with CF. Children with CF between the ages of 2.5 and 6 years with a confirmed diagnosis of CF and age-matched healthy control subjects were enrolled at three North American CF centers. Multiple breath washout tests were performed at baseline, 1, 3, 6, and 12 months to mimic time point chosen in clinical care and interventional trials; spirometry was also conducted. A generalised linear mixed-effects model was used to distinguish LCI changes associated with normal growth and development (i.e., healthy children) from the progression of CF lung disease.
Data were collected on 156 participants with 800 LCI measurements.
Although both LCI and spirometry discriminated health from disease, only the LCI identified significant deterioration of lung function in CF over time. The LCI worsened during cough episodes and pulmonary exacerbations, whereas similar symptoms in healthy children were not associated with increased LCI values.
The authors concluded that LCI is a useful marker to track early disease progression and may serve as a tool to guide therapies in young patients with CF.
2017 Zacharasiewicz A, Renner S, Haderer F, Weber M, Dehlink E, Szepfalusi Z, Frischer T. Early detection of lung function decrements in children and adolescents with cystic fibrosis using new reference values. Wien Klin Wochenschr. 2017 Mar 9. doi: 10.1007/s00508-017-1184-0. [Epub ahead of print] [Pubmed]
Interpretation of lung function values in children with cystic fibrosis depends on the applied reference values. The authors hypothesize that differences between the new global lung function initiative (GLI) values and the formerly used Zapletal et al. values produce significantly different clinical results. They analyzed 3719 lung function measurements of 108 children and adolescents (n = 54 male; aged 6-18 years) with CF treated between September 1991 and July 2009. Data were analysed in milliliters (ml) and % predicted (pred.) and interpreted using Zapletal and GLI reference values. Applying GLI compared to Zapletal resulted in significantly lower mean forced expiratory volume in 1s (FEV1)% pred. Zapletal 86.6% (SD 20.6), GLI 79.9% (SD 20.3) and 32% (n = 497/1543) were misclassified as normal when using Zapletal. Despite showing no overall differences in FEV1 and forced vital capacity (FVC) between concomitant Pseudomonas detection (PA+) in n = 938 and Pseudomonas negative (PA-) (n = 2781) using either reference PA+ resulted in lower FEV1 and FVC values with increasing age; however, measurement of small airway obstruction with forced expiratory flow at 75% of FVC (FEF75) values – available for Zapletal -showed significant differences. Reassurance regarding lung function when using old reference values may occur with potential clinical significance. Discrepancies in lung function interpretation underline the importance of using uniform and best available reference values.
Dr Angela Zacharasiewicz is a consultant Paediatric Pulmonologist in Vienna.
van Horck M, van de Kant K Winkens B, Wesseling G, Gulmans V, Hendriks H, van der Grinten C, Jöbsis Q, Dompeling E. Risk factors for lung disease progression in children with cystic fibrosis. Eur Respir J. 2018 Jun 7;51(6). pii: 1702509. doi: 10.1183/13993003.02509-2017. Print 2018 Jun. [Pubmed] The authors studied the longitudinal data of all children with CF (aged ≥5 years) registered in the Dutch CF Registry (2009-2014). Lung disease progression was expressed as a decline in lung function (forced expiratory volume in 1 s (FEV1) % pred) and pulmonary exacerbation rate.
In a cohort of Dutch children with CF followed for 5 years, the authors were able to identify several risk factors for future exacerbations. In particular, the association between proton pump inhibitor use and lung disease progression definitely requires further investigation.
Ahmed B, Cox MJ, Cuthbertson L, James P, Cookson WOC, Davies JC, Moffatt MF, Bush A. Longitudinal development of the airway microbiota in infants with cystic fibrosis.Sci Rep. 2019 Mar 26;9(1):5143. doi: 10.1038/s41598-019-41597-0 [Pubmed] Free PFMC Article
The pathogenesis of airway infection in cystic fibrosis (CF) is poorly understood. The authors performed a longitudinal study coupling clinical information with frequent sampling of the microbiota to identify changes in the airway microbiota in infancy that could underpin deterioration and potentially be targeted therapeutically.
Thirty infants with CF diagnosed on newborn screening (NBS) were followed for up to two years. Two hundred and forty one throat swabs were collected as a surrogate for lower airway microbiota (median 35 days between study visits) in the largest longitudinal study of the CF oropharyngeal microbiota. Streptococcus spp. and Haemophilus spp. were the most common genera (55% and 12.5% of reads respectively) and were inversely related. Only beta (between sample) diversity changed with age (Bray Curtis r2 = 0.15, P = 0.03). Staphylococcus and Pseudomonas were rarely detected. These results suggest that Streptococcus spp. and Haemophilus spp., may play an important role in early CF. Whether they are protective against infection with more typical CF micro-organisms, or pathogenic and thus meriting treatment needs to be determined.
Dr B Ahmed of National Heart and Lung Institute, Imperial College and the Department of Respiratory Paediatrics, Royal Brompton Hospital, London
– The uncertainty regarding the early bacterial content of the CF airways seems to continue
Breuer O, Schultz A, Turkovic L, de Klerk N, Keil AD, Brennan S, Harrison J, Robertson C, Robinson PJ, Sly PD, Ranganathan S, Stick SM, Caudri D; AREST CF.The Changing Prevalence of Lower Airway Infections in Young Children with Cystic Fibrosis.Am J Respir Crit Care Med. 2019 Feb 27. doi:10.1164/rccm.201810-1919OC. [Epub ahead of print] [Pubmed]
-

Osmed Breuer and daughter
- Historical studies suggest that airway infection in cystic fibrosis (CF) initiates with Staphylococcus aureus and Haemophilus influenzae with later emergence of Pseudomonas aeruginosa. Aspergillus species are regarded as relatively infrequent, late occurring infections. The authors assessed the prevalence and change in prevalence of early lower airway infections in a modern cohort of children with CF.
All infants diagnosed with CF after newborn screening, participating in the AREST-CF cohort study between 2000-2018, were included. Participants prospectively underwent bronchoalveolar lavage (BAL) at 3-6 months,1 year and annually up to 6 years of age. Lower airway infection prevalence was described. Changes in prevalence patterns were assessed longitudinally using generalized estimating equations controlling for age and repeated visits.
A total of 380 infants underwent 1,759 BALs. The overall prevalence and median age of first acquisition of the most common infections were: S. aureus 11%, 2.5yrs, P. aeruginosa 8%, 2.4yrs, Aspergillus species 11%, 3.2yrs, H. influenzae 9%, 3.1yrs. During the study, a significant decrease in prevalence of P. aeruginosa (p<0.001) and S. aureus (p<0.001) was observed with significant change towards more aggressive treatment. Prevalence of Aspergillus infections did not significantly change (p=0.669). T
The study demonstrated Aspergillus species and P. aeruginosa are commonly present in the lower airways from infancy. The decrease in prevalence of P. aeruginosa and S. aureus since 2000, coinciding with more aggressive therapeutic approach, has resulted in Aspergillus becoming the most commonly isolated pathogen in young children. Further research is warranted to understand the implication of these findings.
Dr Oded Breuer of the Pediatric Pulmonology Unit Hadassah –Hebrew University Medical Center Jerusalem currently on two year Ausimed Fellowship at the Telethon Kids Institute and Perth Children’s Hospital, Australia.
Fretzayas A, Douros K, Moustaki M, Loukou I. Applications of lung clearance index in monitoring children with cystic fibrosis. World J Clin Pediatr. 2019 Apr 9;8(2):15-22. doi: 10.5409/wjcp.v8.i2.15. eCollection 2019 Apr 9. [Pubmed]

Andreas Fretzayas
A sensitive, reproducible and feasible measure of lung function for monitoring the respiratory health is a prerequisite for the optimization of management of the patients with cystic fibrosis (CF). Spirometry has been considered the method of choice, although it is applicable only in children older than 6 years of age, as good cooperation is necessary for its proper performance. However, over the last 15 years, scientific interest in gas dilution techniques and particularly in multiple breath wash out (MBW) method has been revived. The most commonly reported index of MBW is lung clearance index (LCI). The aim of this review is to present the most recent developments in the application of LCI as a monitoring index of respiratory status of CF patients. LCI is a sensitive and reproducible marker of ventilation inhomogeneity. It is more sensitive than spirometry and, unlike spirometry; it can be performed across the whole pediatric age range. Since it is dependent on body size, until at least the age of 6 years, the relative and not the absolute changes are more appropriate for providing clinically meaningful conclusion on ventilation inhomogeneity. Until now, MBW has been mainly used as a research tool. Based on the currently available data LCI cannot safely predict high-resolution computed tomography findings in children with CF, especially in infants. It can be used as an end-point measure for the assessment of beneficial effect of interventions. However, its utility as an outcome measure for the efficacy of therapeutic interventions seems to be dependent on the pathophysiologic mechanisms that underlie each intervention. It seems that more studies, especially longitudinal ones, are required in order to fully clarify the clinical usefulness of LCI, not only in the research setting, but also in every day practice of CF clinic
Dr Andreas Fretzayas is Professor of Paediatrics, School of Medicine, Athens, Greece
Goetz D, Kopp BT Salvator A, Moore-Clingenpeel M, McCoy K, Leung DH, Kloster M, Ramsey BR, Heltshe SH, Borowitz D.Pulmonary findings in infants with cystic fibrosis during the first year of life: Results from the Baby Observational and Nutrition Study (BONUS) cohort study. Pediatr Pulmonol. 2019 Jan 22. doi: 10.1002/ppul.24261. [Epub ahead of print] [Pubmed]
-

Danielle Goetz
- To report observations about pulmonary correlates of growth and other clinical features in infants with CF. The authors analysed data from the prospective Baby Observational and Nutrition Study conducted in 28 centers across the US, including clinical features, medications, guardian diaries of respiratory symptoms, oropharyngeal swab cultures and chest radiographs (CXR) collected over the first year of life.
Cough was reported in 84% of infants in the first year. Up to 30% had clinically important cough but only 6.3% had crackles; 16.5% had wheeze. Wisconsin CXR score was above 5 in 23% (normal = 0; maximum score = 100). Pseudomonas was recovered from at least one respiratory culture in 24% of infants and was associated with crackles/wheezes and use of proton pump inhibitors (PPI) (OR = 5.47; 95%CI = 1.36, 21.92; P = 0.02) or PPI plus histamine-2 (H2) blocker (OR = 8.2; 95%CI = 2.41, 27.93; P = 0.001), but not H2 blocker alone. Hospitalization for respiratory indications occurred in 18% of infants and was associated with crackles/wheeze and abnormal CXR but not low weight, Pseudomonas or use of acid blockade.
Conclusions were that cough is common in infants with CF, but few present with crackles/wheeze or CXR changes. Pseudomonas is associated with use of PPI or PPI plus H2 blocker, but not with respiratory hospitalization. These observations cannot prove cause and effect but add to our understanding of pulmonary manifestations of CF in infants
Dr Danielle Goetz is paediatric Pulmonologist in the Dept. of Pediatrics, Jacobs School of Medicine, University of Buffalo
Hardaker KM, Panda H, Hulme K, Wong A, Coward E, Cooper P, Fitzgerald DA, Pandit C, Towns S, Selvadurai H, Robinson PD.Abnormal preschool Lung Clearance Index (LCI) reflects clinical status and predicts lower spirometry later in childhood in cystic fibrosis.J Cyst Fibros 2019 Feb 28. pii: S1569-1993(19)30025-6. doi: 10.1016/j.jcf.2019.02.007. [Epub ahead of print] [Pubmed]
-

Kate Hardaker
- Clinical and prognostic value of preschool Multiple Breath Washout (MBW) remains unclear. Initial MBW results (Exhalyzer® D, EcoMedics AG) in preschool Cystic Fibrosis (CF) subjects (age 2-6 years) at a time of clinical stability were compared to (1) concurrent clinical status measures and (2) later spirometry outcomes. Abnormal Lung Clearance Index (LCI) was defined using published reference data (Upper limit of normal for LCI 8.0).
LCI was abnormal in 56% (28/50), with mean (SD) LCI 8.61(1.85) at age 4.71(1.3) years. Abnormal LCI was associated with higher dornase alfa use, previous positive bacterial cultures and pF508.del homozygous genotype. Later spirometry (n = 44; mean (SD) 2.3(0.5) years after MBW) demonstrated that abnormal initial preschool LCI was a strong predictor of lower later spirometry outcomes.CONCLUSION:
Abnormal preschool LCI was associated with concurrent measures of clinical status and later spirometry deficits, suggesting early prognostic utility of MBW testing in this age range.
Dr. Kate Hardaker is a Respiratory Scientist at the Dept. Respiratory Medicine The Children’s Hospital at Westmead Sydney.
– Further work emphasising the importance of very early intervention in infants with CF.
Jorth P, Ehsan Z, Rezayat A, Caldwell E, Pope C, Brewington JJ, Goss CH, Benscoter D, Clancy JP, Singh PK. Direct Lung Sampling Indicates That Established Pathogens Dominate Early Infections in Children with Cystic Fibrosis. Cell Rep. 2019 Apr 23;27(4):1190-1204.e3. doi: 10.1016/j.celrep.2019.03.086. 31018133 Free full text [Pubmed]

Peter Jorth
Culture and sequencing have produced divergent hypotheses about cystic fibrosis (CF) lung infections. Culturing suggests that CF lungs are uninfected before colonization by a limited group of CF pathogens. Sequencing suggests diverse communities of mostly oral bacteria inhabit lungs early on and diversity decreases as disease progresses. The authors studied the lung microbiota of CF children using bronchoscopy and sequencing, with measures to reduce contamination. They found no evidence for oral bacterial communities in lung lavages that lacked CF pathogens. Lavage microbial diversity varied widely, but decreases in diversity appeared to be driven by increased CF pathogen abundance, which reduced the signal from contaminants. Streptococcus, Prevotella, and Veillonella DNA was detected in some lavages containing CF pathogens, but DNA from these organisms was vastly exceeded by CF pathogen DNA and was not associated with inflammation. These findings support the hypothesis that established CF pathogens are primarily responsible for CF lung infections
– This is a very detailed complex scientific article with nevertheless a straight forward conclusion that BALs from children with mild disease primarily contain established pathogens; microbiota from BALs lacking pathogens were indistinguishable from controls; rare oral organisms were found in some BALs containing abundant CF pathogens; CF pathogens strongly correlated with inflammation but oral organisms did not.
Dr Peter A Jorth is Assistant Professor, Departments of Pathology and Laboratory Medicine, Medicine and Biomedical Sciences, Cedars-Sinai Medical Center, Los Angeles.
Korten I, Kieninger E, Yammine S, Cangiano G, Nyilas S, Anagnostopoulou P, Singer F, Kuehni CE, Regamey N, Frey U, Casaulta C, Spycher BD, Latzin P; SCILD; BILD study group. Respiratory rate in infants with cystic fibrosis throughout the first year of life and association with lung clearance index measured shortly after birth. J Cyst Fibros. 2019 Jan;18(1):118-126. doi: 10.1016/j.jcf.2018.07.002. Epub 2018 Jul 27. [Pubmed]
-

Phillippe Latzin
Lung impairment in cystic fibrosis (CF) starts in infancy. However, tools to monitor early lung disease are limited. Respiratory rate (RR) as a key vital sign is easy to assess during sleep and is elevated during acute respiratory disease. Thus, elevated RR could indicate early lung impairment and potentially serve as a diagnostic tool in disease monitoring.
In a prospective cohort of infants with CF diagnosed by newborn screening and healthy controls RR was measured and respiratory symptoms reported weekly throughout infancy. Infants performed a lung function measurement within the first weeks of life.
The analyses included 5656 measurements from 153 infants (43 with CF). RR declined from 43.2 (40.5)/min at 6 weeks of age to 28.3 (24.6)/min at 50 weeks in infants with CF (healthy controls). Infants with CF had consistently higher RR than controls (mean difference: 4.15/min; (95% CI 2.86-5.44); p < .001). In both study groups, RR was increased throughout the study period in infants with higher lung clearance indices (LCI) and during episodes of respiratory infections.
The authors concluded infants with CF have a higher RR compared to healthy controls during the first year of life. The association with early LCI measurements, the current gold standard to assess physiology of peripheral airways persisted throughout the study period. This may indicate tracking of lung function by RR. It might thus be an early subtle sign of functional respiratory deficit. Further studies will show if RR can be used as a sensitive and promising marker to monitor early CF lung disease.
Dr Insa Korten Department of Pediatrics, Pediatric Respiratory Medicine, Inselspital, Bern University Hospital, University of Bern, Bern, Switzerlan
Prof. Philipp Latzin is the corresponding author.He is Head of Paediatric Pulmonology at University Children’s Hospital Bern.[BILD – Basel-Bern-Infant Lung Development cohort SCILD – Swiss Cystic Fibrosis Infant Lung development cohort]
– This is a really interesting and valuable study validating good old-fashioned clinical observations of the importance of a raised respiratory rate with the use of sophisticated modern infant respiratory function tests. The authors suggest that respiratory rate could be a simple method lung function tracking in early life – a most important time when early lung damage seems to be relatively common and a time in infancy which is receiving increasing attention.
Poncin W, Lebecque P.[Lung clearance index in cystic fibrosis]. Rev Mal Respir. 2019 Jan 24. pii: S0761-8425(18)31015-5. doi: 10.1016/j.rmr.2018.03.007. [Epub ahead of print] (French) [Pubmed]
-

William Poncin
- The multiple breath washout (MBW) test is affordable and non-invasive. Lung clearance index (LCI), which is the most used derived parameter, is reproducible and much more sensitive than spirometry in detecting small airways disease. However, MBW is operator dependent. The recent commercialization of devices assessing LCI launches MBW as a potential tool in routine clinical care, although its use currently remains mostly dedicated to research purposes. However, important differences in LCI between various equipment settings raise a number of theoretical questions. Specific algorithms should be refined and more transparent. Standardization of MBW is still an on going process. Whether other MBW derived indices can prove superior over LCI deserves further study
Ratjen F, Davis SD, Stanojevic S, Kronmal RA, Hinckley Stukovsky KD, Jorgensen N, Rosenfeld M; SHIP Study Group.Inhaled hypertonic saline in preschool children with cystic fibrosis (SHIP): a multicentre, randomised, double-blind, placebo-controlled trial. Lancet Respir Med. 2019 Jun 6. pii: S2213-2600(19)30187-0. doi: 10.1016/S2213-2600(19)30187-0. [Epub ahead of print] [Pubmed]

Felix Ratjen
A study to assess the effect of inhaled hypertonic saline on the lung clearance index (LCI2·5)-a measure of ventilation inhomogeneity-in children aged 3-6 years with cystic fibrosis. The Saline Hypertonic in Preschoolers (SHIP) Study was a randomised, double-blind, placebo-controlled trial at 25 cystic fibrosis centres in Canada and the USA. Eligible participants were aged 36-72 months; had a confirmed diagnosis of cystic fibrosis; were able to comply with medication use, study visits, and study procedures; and were able to complete at least two technically acceptable trials of multiple breath washout (MBW). Participants were randomly assigned (1:1) via a web-based data entry system that confirmed enrolment eligibility to inhaled 7% hypertonic saline or 0·9% isotonic saline nebulised twice daily (for no more than 15 min per dose) for 48 weeks. Permuted block randomisation was done separately for participants aged 36-54 months and those aged 55-72 months to ensure approximate balance by treatment group in the two age groups. The primary endpoint was the change in the LCI2·5 measured by nitrogen MBW from baseline to week 48.
Between April 21, 2015, and Aug 4, 2017, 150 participants were enrolled and randomly assigned, 76 to the hypertonic saline group and 74 to the isotonic saline group. Overall 89% of the MBW tests produced acceptable data. At 48 weeks, treatment with hypertonic saline was associated with a significant decrease (ie, improvement) in LCI2·5 compared with isotonic saline (mean treatment effect -0·63 LCI2·5 units [95% CI -1·10 to -0·15]; p=0·010). Six participants in the hypertonic saline group had ten serious adverse events and eight participants in the isotonic saline group had nine serious adverse events. The serious adverse events reported were cough (two patients [3%] in the hypertonic saline group vs three [4%] in the isotonic saline group), gastrostomy tube placement or rupture (two [3%] vs one [1%]), upper gastrointestinal disorders (one [1%] vs two [3%]), distal intestinal obstruction syndrome (one [1%] vs one [1%]), and decreased pulmonary function (none vs one [1%]). None of these serious adverse events was judged to be treatment related.
The authors concluded that inhaled hypertonic saline improved the LCI2·5 in children aged 3-6 years, and could be a suitable early intervention in cystic fibrosis.
Prof. Felix Ratjen is Chief of Respiratory Medicine and Professor at the Hospital for Sick Children, Toronto.
Ratjen F, Jensen R, Klingel M, McDonald R, Moore C, Benseler N, Wilson D, Stanojevic S.Effect of changes in tidal volume on multiple breath washout outcomes. PLoS One.2019 Jul 3;14(7):e0219309. doi: 10.1371/journal.pone.0219309. eCollection 2019. [Pubmed]
The lung clearance index (LCI), measured by multiple breath washout (MBW), reflects global ventilation inhomogeneity and is a sensitive marker of early obstructive airway disease. For the MBW test to accurately reflect a subject’s gas mixing within the lungs, the breathing pattern should represent physiologically appropriate tidal volumes (VT) and respiratory rate (RR).The authors aimed to assess whether changes in tidal volume impact MBW outcome measures with a series of prospective and retrospective studies. The LCI was lower, but not significantly different between deep breathing at 20 ml/kg body weight and uninstructed tidal breathing; whereas LCI was significantly higher during shallow breathing compared with normal tidal breathing. For the majority of subjects with CF (80%), VT ranged from 9-15mL/kg. Within the observed VT range, LCI was similar in trials with mean VT /kg below this range compared to trials with VT /kg within the range.
If subjects breathe naturally and are not instructed to use specific targets, the range of VT is within physiologically appropriate limits and normal variations observed do not impact MBW outcomes.
Goetz D, Kopp BT Salvator A, Moore-Clingenpeel M, McCoy K, Leung DH, Kloster M, Ramsey BR, Heltshe SH, Borowitz D.Pulmonary findings in infants with cystic fibrosis during the first year of life: Results from the Baby Observational and Nutrition Study (BONUS) cohort study. Pediatr Pulmonol. 2019 Jan 22. doi: 10.1002/ppul.24261. [Epub ahead of print] [Pubmed]
-

Danielle Goetz
- To report observations about pulmonary correlates of growth and other clinical features in infants with CF. The authors analysed data from the prospective Baby Observational and Nutrition Study conducted in 28 centers across the US, including clinical features, medications, guardian diaries of respiratory symptoms, oropharyngeal swab cultures and chest radiographs (CXR) collected over the first year of life.
Cough was reported in 84% of infants in the first year. Up to 30% had clinically important cough but only 6.3% had crackles; 16.5% had wheeze. Wisconsin CXR score was above 5 in 23% (normal = 0; maximum score = 100). Pseudomonas was recovered from at least one respiratory culture in 24% of infants and was associated with crackles/wheezes and use of proton pump inhibitors (PPI) (OR = 5.47; 95%CI = 1.36, 21.92; P = 0.02) or PPI plus histamine-2 (H2) blocker (OR = 8.2; 95%CI = 2.41, 27.93; P = 0.001), but not H2 blocker alone. Hospitalization for respiratory indications occurred in 18% of infants and was associated with crackles/wheeze and abnormal CXR but not low weight, Pseudomonas or use of acid blockade.
Conclusions were that cough is common in infants with CF, but few present with crackles/wheeze or CXR changes. Pseudomonas is associated with use of PPI or PPI plus H2 blocker, but not with respiratory hospitalization. These observations cannot prove cause and effect but add to our understanding of pulmonary manifestations of CF in infants
Dr Danielle Goetz is paediatric Pulmonologist in the Dept. of Pediatrics, Jacobs School of Medicine, University of Buffalo
-
- Ratjen F, Moeller A, McKinney ML, Asherova I, Alon N, Maykut R, Angyalosi G; EARLY study group.Eradication of early P. aeruginosa infection in children <7 years of age with cystic fibrosis: The early study.Collaborators (12) Cyst Fibros. 2019 Jan;18(1):78-85. doi: 10.1016/j.jcf.2018.04.002. Epub 2018 Apr 21. [Pubmed]
Antibiotic eradication treatment is the standard-of-care for cystic fibrosis (CF) patients with early Pseudomonas aeruginosa (Pa)-infection; however, evidence from placebo-controlled trials is limited. This double-blind, placebo-controlled trial randomised CF patients <7 years (N = 51) with early Pa-infection to tobramycin inhalation solution (TOBI 300 mg) or placebo (twice daily) for 28 days with an optional cross-over on Day 35. Primary endpoint was proportion of patients having throat swabs/sputum free of Pa on Day 29.
On Day 29, 84.6% patients in the TOBI versus 24.0% in the placebo group were Pa-free (p < 0.001). At the end of the cross-over period, 76.0% patients receiving TOBI in the initial 28 days were Pa-free compared to 47.8% receiving placebo initially. Adverse events were consistent with the TOBI safety profile with no differences between TOBI and placebo.The authors confirmed TOBI was effective in eradicating early Pa-infection with a favourable safety profile in young CF patients.– The first trial on early eradication of Pseudomonas was published in 1991 from Copenhagen. The introduction of early eradication therapy in N. America was surprisingly slow. Perhaps the need for trials may to the disadvantage of patients such as the children in the placebo group of this trial some of whom will be left with chronic pseudomonas infection due to delay in eradication treatment.Reece E, McClean S, Greally P, Renwick J.The prevalence of Aspergillus fumigatus in early cystic fibrosis disease is underestimated by culture-based diagnostic methods. J Microbiol Methods. 2019 Aug 3:105683. doi: 10.1016/j.mimet.2019.105683. [Epub ahead of print] [Pubmed]

Emma Reece
Aspergillus fumigatus is the most common fungus infecting/colonising people with cystic fibrosis (CF) and can negatively impact clinical status. Diagnostic laboratories rely on culture to detect A. fumigatus which is known to be less sensitive than molecular approaches. Therefore, A. fumigatus colonisation in the CF population may be underestimated.
Sputum (n = 60) from 25 children with CF were collected and A. fumigatus was detected using routine culture (CM1), enhanced culture (CM2) and ITS1 qPCR. The prevalence of A. fumigatus in this young CF population was 68% by qPCR and only 16% by CM1. CM1, CM2 and qPCR detected A. fumigatus in 8%, 22% and 53% of samples, respectively. qPCR had a 94.2% and 77.4% increased odds of detecting A. fumigatus over CM1 and CM2, respectively.Molecular methods proved superior for detecting A. fumigatus in CF sputum. A. fumigatus is likely more prevalent in early CF disease than is currently reported.
Dr Emma Reece is in the Department of Clinical Microbiology, Trinity College, Dublin.
The authors conclude that in CF, LCI is now a well-established outcome in research settings to detect early lung function abnormalities and new treatment effects, especially in patients with mild lung disease. In these patients, LCI seems an attractive tool for clinicians too. Yet, further investigation is needed to define clinically significant changes in LCI and to which extent this index can be useful in guiding clinical decisions remains to be studied.
Dr William Poncin is an expert on respiratory physiology at Universite Catholique de Louvain.
Shawcross A, Murray CS, Pike K, Horsley A. A novel method for infant multiple breath washout: First report in clinical practice. Pediatr Pulmonol. 2019 Jun 18. doi: 10.1002/ppul.24384. [Epub ahead of print] [Pubmed]
Lung clearance index (LCI), measured using multiple breath inert gas washout (MBW) is a potentially useful test in infants with respiratory disease, particularly cystic fibrosis (CF). Clinical use is limited however by the need for specialist staff and equipment. We have previously described a novel method for infant MBW suitable for use outside of specialist laboratories. This study describes its performance in vivo in infants with CF and healthy controls, including a limited comparison with the respiratory mass spectrometer. Children aged less than 2 years with CF and controls underwent MBW testing on a single occasion. The practical applicability of the system was determined by the number of successful duplicate tests and within-subject repeatability.
Twenty-five children (seven with CF, 18 healthy controls, all sedated with chloral hydrate) attempted MBW. Twenty patients (seven with CF) successfully underwent duplicate testing (80% success rate). Mean within-subject coefficient of variation for functional residual capacity (FRC) was 7.2% and for LCI 5.9%. Comparison of LCI with the mass spectrometer was limited but gave very similar values for LCI and FRC in those patients who underwent technically adequate tests with both methods.
We have described a new MBW method that is feasible and reproducible in sedated infants. Results fall within the expected range, and well within accuracy limits set by international guidelines. This could provide a more accessible alternative to previously described systems for infant MBW, and overcomes many of the technical challenges inherent in conventional MBW
Dr Anna Shawcross is Clinical Research Fellow and Specialist Trainee in Paediatric Respiratory Medicine Manchester and the Department of Paediatric Respiratory Medicine, Royal Manchester Children’s Hospital, Manchester, UK.
THE ORIGINAL PUBLICATION OF THIS METHOD –
Shawcross A, Murray CS, Goddard N, Gupta R, Watson S, Horsley. Accurate lung volume measurements in vitro using a novel inert gas washout method suitable for infants. Pediatr Pulmonol. 2016 May;51(5):491-7. doi: 10.1002/ppul.23348. Epub 2015 Dec 1 [Pubmed]
Multiple breath washout (MBW) in infants presents a number of technical challenges. Conventional MBW is based on simultaneous measurement of flow and gas concentrations. These two signals are aligned and combined to derive expired gas volumes from which lung volumes and measures of ventilation inhomogeneity are calculated. Accuracy of measurement becomes increasingly vulnerable to errors in gas signal alignment at fast respiratory rates. In this paper we describe an alternative method of performing MBW in infants. Expired gas is collected and analyzed to derive functional residual capacity (FRC) and lung clearance index (LCI). This eliminates the need for simultaneous measurement of flow, and integration of flow and gas signals, and significantly reduces deadspace. A highly accurate lung model incorporating BTPS conditions was used to generate realistic infant breathing parameters: FRC of 100-250 mls with respiratory rate of 20-60 min(-1) . In vitro accuracy of FRC measurement using the novel MBW method was assessed using the model. Overall mean error (standard deviation) of FRC measurement was -1.0 (3.3)% with 90% of tests falling within ±5%.
FRC measurement using the novel method has superior accuracy in vitro than previously described systems. By uncoupling the measurement of gas volumes from real-time flow and gas measurement, this system offers an alternative method of MBW which is well suited to infants.
Turkovic L, Caudri D, Rosenow T, Breurer O, Murray C, Tiddens HAWM, Ramanauskas F, Ranganathan SC, Hall GL, Stick SM; AREST CF. Structural determinants of long term functional outcomes in young children with cystic fibrosis. Eur Respir J. 2020 Mar 5. pii: 1900748. doi: 10.1183/13993003.00748-2019. [Epub ahead of print] [Pubmed]

Lidijat Turkovic
Accelerated lung function decline in individuals with cystic fibrosis (CF) starts in adolescence with respiratory complications being the most common cause of death in later life. Factors contributing to lung function decline are not well understood, in particular its relationship with structural lung disease in early childhood. Detection and management of structural lung disease could be an important step in improving outcomes in CF patients.
Annual chest computed tomography (CT) scans were available from 2005 to 2016 as a part of AREST CF cohort for children aged 3-months to 6-years. Annual spirometry measurements were available for 89.77% of the cohort (n=167 children at age 5-6 years) from ages 5 to 15 years through outpatient clinics at Perth Children’s Hospital and The Royal Children’s Hospital in Melbourne. (n=697 measurements, age 9.3 (2.1) years).
Findings: Children with a total CT score at 5-6 years above the median were more likely to have abnormal FEV1 (aHR 2.67 (1.06, 6.72) p=0.037) during the next 10 years compared to those below the median chest CT score. The extent of all structural abnormalities except bronchial wall thickening were associated with lower FEV1 Z scores. Mucus plugging and trapped air were the most predictive sub-score (adjusted mean change -0.17 (-0.26, -0.07) p<0.001 and -0.09 (-0.14, -0.04) p<0.001 respectively).
The authors observe that this study shows that chest CT identifies children at an early age who have adverse long-term outcomes. The prevention of structural lung damage should be a goal of early intervention and can be usefully assessed with chest CT. In an era of therapeutics that might alter disease trajectories, chest CT could provide an early readout of likely long-term success.
Dr Lidijat Turkovic was at Telethon Kids Institute, Perth, Australia and now Principal Biostatistician, IQVIA Human Data Science Company, Melbourne, Australia
– This excellent long-term data from AREST CF study provides further hard evidence that what happens in very early childhood determines the situation many years later. Once damage occurs progress is downhill even though considerably slowed by treatment during childhood.
Oudraad MCJ, Kuo W, Rosenow T, Andrinopoulou ER, Stick SM, Tiddens HAWM Assessment of early lung disease in young children with CF: A comparison between pressure-controlled and free-breathing chest computed tomography. Pediatr Pulmonol. 2020 Mar 2. doi: 10.1002/ppul.24702. [Epub ahead of print] [Pubmed]

Merel Oudraad
Chest computed tomography (CT) in children with cystic fibrosis (CF) is sensitive in detecting early airways disease. The pressure-controlled CT-protocol combines a total lung capacity scan (TLC PC-CT) with a near functional residual capacity scan (FRC PC-CT) under general anaesthesia, while another CT-protocol is acquired during free breathing (FB-CT) near functional residual capacity. The aim of this study was to evaluate the sensitivity in detecting airways disease of both protocols in two cohorts.
Routine PC-CTs (Princess Margaret Children’s Hospital) and FB-CTs (Erasmus MC-Sophia Children’s Hospital) were retrospectively collected from CF children aged 2 to 6 years. Total airways disease (%disease), bronchiectasis (%Bx), and low attenuation regions (%LAR) were scored on CTs using the Perth-Rotterdam annotated grid morphometric analysis-CF method. The Wilcoxon signed-rank test was used for differences between TLC and FRC PC-CTs and the Wilcoxon rank-sum test for differences between FRC PC-CTs and FB-CTs.
RESULTS: Fifty patients with PC-CTs (21 male, aged 2.5-5.5 years) and 42 patients with FB-CTs (26 male, aged 2.3-6.8 years) were included. %Disease was higher on TLC PC-CTs compared with FRC PC-CTs (median 4.51 vs 2.49; P < .001). %Disease and %Bx were not significantly different between TLC PC-CTs and FB-CTs (median 4.51% vs 3.75%; P = .143 and 0.52% vs 0.57%; P = .849). %Disease, %Bx, and %LAR were not significantly different between FRC PC-CTs and FB-CTs (median 2.49% vs 3.75%; P = .055, 0.54% vs 0.57%; P = .797, and 2.49% vs 1.53%; P = .448).
The authors consider their data suggest that FRC PC-CTs are less sensitive than TLC PC-CTs and that FB-CTs have similar sensitivity to PC-CTs in detecting lung disease. FB-CTs seem to be a viable alternative for PC-CTs to track CF lung disease in young patients with CF.
Dr Merel C J Oudraad was Student researcher of the Lung Analysis research group Erasmus MC and now Clinical Fellow Emergency Department Royal Infirmary Edinburgh.
Horati H, Janssens HM, Margaroli C, Veltman M, Stolarczyk M, Kilgore MB, Chou J, Peng L, Tiddens HAMW, Chandler JD, Tirouvanziam R, Scholte BJ. Airway profile of bioactive lipids predicts early progression of lung disease in cystic fibrosis. 2020 Feb 10. pii: S1569-1993(20)30034-5. doi: 10.1016/j.jcf.2020.01.010. [Epub ahead of print] [Pubmed]

Hamid N Horati

Bob Scholte
Previously, these authors showed that abnormal levels of bioactive lipids in bronchoalveolar lavage fluid (BALF) from infants with cystic fibrosis (CF) correlated with early structural lung damage. To extend these studies, BALF bioactive lipid measurement by mass spectrometry and chest computed tomography (CT, combined with the sensitive PRAGMA-CF scoring method) were performed longitudinally at 2-year intervals in a new cohort of CF children (n = 21, aged 1-5 yrs).
Results: PRAGMA-CF, neutrophil elastase activity, and myeloperoxidase correlated with BALF lysolipids and isoprostanes, markers of oxidative stress, as well as prostaglandin E2 and combined ceramide precursors (Spearman’s Rho > 0.5; P < 0.01 for all). Multiple protein agonists of inflammation and tissue remodeling, measured by Olink protein array, correlated positively (r = 0.44-0.79, p < 0.05) with PRAGMA-CF scores and bioactive lipid levels. Notably, levels of lysolipids, prostaglandin E2 and isoprostanes at first BALF predicted the evolution of PRAGMA-CF scores 2 years later. In wild-type differentiated primary bronchial epithelial cells, and in CFTR-inducible iCFBE cells, treatment with a lysolipid receptor agonist (VPC3114) enhanced shedding of pro-inflammatory and pro-fibrotic proteins.
The authors concluded their findings suggest that bioactive lipids in BALF correlate with and possibly predict structural lung disease in CF children, which supports their use as biomarkers of disease progression and treatment efficacy. Furthermore, our data suggest a causative role of airway lysolipids and oxidative stress in the progression of early CF lung disease, unveiling potential therapeutic targets.
Dr H Horati is Paediatric Resident n the Department of Pediatrics, Division of Respiratory Medicine and Allergology, Erasmus MC-Sophia Children’s Hospital, University Hospital Rotterdam, the Netherlands
Dr B J Bob Scholte is group leader and assistant professor (Gene therapy, experimental therapy of lung disease) at Erasmus MC Rotterdam since 1986, presently associated with the Pediatric Pulmonology department, and the Cell biology department (Biomedical Sciences Theme).
– The early detection of bronchial infection is an important area of research if such infection is to be identified before irreversible tissue damage occurs – often at a very early age.
Davies G, Thia LP, Stocks J, Bush A, Hoo AF, Wade A, Nguyen TTD, Brody AS, Calder A, Klein NJ, Carr SB, Wallis C, Suri R, Pao CS, Ruiz G, Balfour-Lynn IM; London Cystic Fibrosis Collaboration (LCFC). Minimal change in structural, functional and inflammatory markers of lung disease in newborn screened infants with cystic fibrosis at one year. J Cyst FIBROS 2020 Feb 7. pii: S1569-1993(20)30031-X.doi: 10.1016/j.jcf.2020.01.006. [Epub ahead of print] [Pubmed]
With the widespread introduction of newborn screening for cystic fibrosis(CF), there has been considerable emphasis on the need to develop objective markers of lung health that can be used during infancy. We hypothesised that in a newborn screened (NBS) UK cohort, evidence of airway inflammation and infection at one year would be associated with adverse structural and functional outcomes at the same age.
Infants underwent lung function testing, chest CT scan and bronchoscopy with bronchoalveolar lavage (BAL) at 1 year of age when clinically well. Microbiology cultures were also available from routine cough swabs.
65 infants had lung function, CT and BAL. Mean (SD) lung clearance index and forced expiratory volume in 0.5 s z-scores were 0.9(1.2) and -0.6(1.1) respectively; median Brody II CF-CT air trapping score on chest CT =0 (interquartile range 0-1, maximum possible score 27). Infants isolating any significant pathogen by 1 yr of age had higher LCI z-score (mean difference 0.9; 95%CI:0.4-1.4; p = 0.001) and a trend towards higher air trapping scores on CT (p = 0.06). BAL neutrophil elastase was detectable in 23% (10/43) infants in whom BAL supernatant was available. This did not relate to air trapping score on CT.
The authors concluded that in this UK NBS cohort at one year of age, lung and airway damage is much milder and associations between inflammation, abnormal physiology and structural changes were at best weak, contrary to our hypothesis and previously published reports. Continued follow-up will clarify longer term implications of these very mild structural, functional and inflammatory changes.
Dr Gwyneth Davies is a Research Associate Respiratory, Critical Care and Anaesthesia section, UCL Great Ormond Street Institute of Child Health (GOS ICH), London,
Taylor SL, Leong LEX, Ivey KL, Wesselingh S, Grimwood K, Wainwright CE, Rogers GB; Australasian Cystic Fibrosis Bronchoalveolar Lavage (ACFBAL) study group. Total bacterial load, inflammation, and structural lung disease in paediatric cystic fibrosis. J Cyst Fibros. 2020 Mar 18. pii: S1569-1993(20)30079-5. doi: 10.1016/j.jcf.2020.03.008. [Epub ahead of print] [Pubmed]
Cystic fibrosis (CF) is characterised by reduced airway clearance, microbial accumulation, inflammation, and lung function decline. Certain bacterial species may contribute disproportionately to worsening lung disease. However, the relative importance of these microorganisms compared to the absolute abundance of all bacteria is uncertain. The authors aimed to identify the characteristics of lower airway microbiology that best reflect CF airway inflammation and disease in children.
Analysis was performed on bronchoalveolar lavage (BAL) fluid from 78 participants of the Australasian CF Bronchoalveolar Lavage (ACFBAL) clinical trial, aged 4.5-5.5 years. Universal bacterial quantitative PCR (qPCR), species-specific qPCR, and 16S rRNA gene sequencing were performed on DNA extracts to determine total bacterial load, species-specific load and taxa relative abundance. Quantification of pre-specified pathogens was performed by culture-based methods. Bacteriological data were related to neutrophil counts, interleukin-8, lung function, and two computed-tomography based measures, CF-CT (as the primary measure) and PRAGMA.
Of all bacteriological measures assessed, total bacterial load determined by qPCR correlated most strongly with structural disease (CF-CT total score, rs=0.30, P=0.0095). Specifically, total bacterial load correlated with bronchiectasis, airway wall thickening, mucus plugging and parenchymal disease sub-scores. In contrast, culture-based quantification, microbiota-derived measures, and pathogen-specific qPCR-based quantification were weakly associated with total CF-CT. Regression analyses supported correlation findings, with total bacterial load explaining the greatest variance in total CF-CT (R2=0.097, P=0.0061). Correlations with PRAGMA score were comparable to CF-CT total score.
the authors concluded within the ACFBAL trial, culture-independent quantification of total bacteria provided the most clinically informative bacteriological measure in 5-year-old CF patients.
Steven Taylor is at the SAHMRI Microbiome Research Laboratory, Flinders University College of Medicine and Public Health, Adelaide, SA, Australia; Microbiome and Host Health, South Australia Health and Medical Research Institute, North Terrace, Adelaide, SA, Australia
They report a Phase I, single-dose, dose-escalating study aimed at demonstrating safety and tolerability of AeroVanc. In conclusion, AeroVanc was well tolerated and achieved high levels in sputum with a mean systemic absorption of 49%, making it a potential therapeutic strategy for respiratory infection with MRSA.
Dr Grant Waterer is Professor of Medicine, University of Western Australia is a respiratory physician at Royal Perth Hospital and is a professor of medicine at the University of Western Australia and professor of medicine at Northwestern University, Chicago, USA.
Wijker NE, Vidmar S, Grimwood K, Sly PD, Byrnes CA, Carlin JB, Cooper PJ, Robertson CF, Massie RJ, Kemner van de Corput MPC, Cheney J, Tiddens HAWM, Wainwright CE; Australasian Cystic Fibrosis Bronchoalveolar Lavage (ACFBAL) and Follow-up of the ACFBAL (CF-FAB) study groups.Early markers of cystic fibrosis structural lung disease: follow-up of the ACFBAL cohort. Eur Respir J. 2020 Apr 3;55(4). pii: 1901694. doi: 10.1183/13993003.01694-2019. Print 2020 Apr. [Pubmed]

Suzanna Vidmar

Naomi Wijker
Little is known about early predictors of later cystic fibrosis (CF) structural lung disease. This study examined early predictors of progressive structural lung abnormalities in children who completed the Australasian CF Bronchoalveolar Lavage (ACFBAL) clinical trial at age 5-years and participated in an observational follow-up study (CF-FAB). Eight Australian and New Zealand CF centres participated in CF-FAB and provided follow-up chest computed-tomography (CT) scans for children who had completed the ACFBAL study with baseline scans at age 5-years. CT scans were annotated using PRAGMA-CF scoring. Ordinal regression analysis and linear regression were used to investigate associations between PRAGMA-CF (Perth-Rotterdam Annotated Grid Morphometric Analysis for CF) outcomes at follow-up and variables measured during the ACFBAL study.
99 out of 157 ACFBAL children (mean±sd age 13±1.5 years) participated in the CF-FAB study. The probability of bronchiectasis at follow-up increased with airway disease severity on the baseline CT scan. In multiple regression (retaining factors at p<0.05) the extent of bronchiectasis at follow-up was associated with baseline atelectasis (OR 7.2, 95% CI 2.4-22; p≤ 0.001), bronchoalveolar lavage (BAL) log2 interleukin (IL)-8 (OR 1.2, 95% CI 1.05-1.5; p=0.010) and body mass index z-score (OR 0.49, 95% CI 0.24-1.00; p=0.05) at age 5 years. Percentage trapped air at follow-up was associated with BAL log2 IL-8 (coefficient 1.3, 95% CI 0.57-2.1; p<0.001) at age 5 years.
The study established that the extent of airway disease, atelectasis, airway inflammation and poor nutritional status in early childhood are risk factors for progressive structural lung disease in adolescence.
Dr Naomi E Wijker of the Departments of Pulmonology and Allergology, Erasmus Medical Center Sophia Children’s Hospital, Rotterdam, The Netherlands & Radiology and Nuclear Medicine, Erasmus Medical Center, Rotterdam, The Netherlands.
Dr Suzanna Vidmar is Senior Research Officer in the Clinical Epidemiology and Biostatistics Unit, Murdoch Children’s Research Institute, Melbourne, Australia & the Dept of Paediatrics, University of Melbourne, Melbourne, Australia
See comment below from Flume and VanDevanter
Flume PA, VanDevanter DR. Leveraging early markers of cystic fibrosis structural lung disease to improve outcomes. Eur Respir J. 2020 Apr 3;55(4). pii: 2000105. doi: 10.1183/13993003.00105-2020. Print 2020 Apr. [Pubmed] Comment on the article of Wijker NE, Vidmar S et al Eur Respir J 2020 Apr 3;55(4):ABOVE

Patrick Flume
(Précis of the article as there is no abstract) Development of a diagnostic tool for a chronic disease is a necessary first step in a longer process of testing interventions and (hopefully) demonstrating subsequent disease modification. Clarification of temporal associations between early CF lung disease manifestations and subsequent irreversible damage by CT prompts the obvious question of how intervention might be deployed to prevent or delay this process. Prescription of inhaled antipseudomonal antibiotics upon the identification of bacteria, notably Pseudomonas, has become standard of care, but what of the chronic therapies such as hypertonic saline, dornase alfa and macrolides? The data presented by WIJKER et al. suggest that earlier interventions guided by CT and inflammatory marker findings may be warranted.
Beyond hypothesising that “benefit is likely” in a subpopulation, we should feel obliged to study interventions longitudinally in that population to determine if benefit has occurred, and if so to what extent. Children with poor nutritional indices at age 3 years have lower lung function by age 6 years and the trajectory of nutritional status is associated with subsequent pulmonary function, justifying nutritional intervention in young children with poor nutritional indices. Is it time to consider subjecting all our infants with CF to MBW and/or CT imaging to identify those patients showing early signs of progression, or could we be more selective in whom we perform testing?
Ideally, we seek demonstration that a therapy can reverse or attenuate abnormal findings of diagnostic tests. WIJKER et al. have left little doubt that addressing early inflammation in the CF lung will be integral to slowing or stopping CF lung disease progression. Further, their results suggest that studies of intervention-associated change in atelectasis, airway thickening and/or IL-8 concentrations may be justified in infants with CF. Finally, they have provided the methodology for using CT to evaluate the effects of such interventions on lung disease progression in children. Many if not most subjects in this study were already receiving at least some chronic pulmonary interventions intended to mitigate obstruction and infection. It will be of great interest to observe whether early highly effective modulator therapy (HEMT) intervention will slow the development of structural disease later in life, and it appears that we will now be able to use CT to start these observations at a very early age. It may be that a decade from now, it will be possible to use the CT methodologies described by WIJKER et al to discriminate between those children with CF who enjoyed access to CFTR modulators early in life and those who did not.
As we are now in the era of highly effective modulator therapy (HEMT), with drugs that increase the activity of the cystic fibrosis transmembrane conductance regulator (CFTR) activity, this “next level” of intervention has already demonstrated considerable benefits as an “add on” to background therapy. CFTR modulators have been associated with a reduction in the rate of lung function decline, suggesting disease modification, presumably by impacting the obstructive aspects of the condition, but perhaps also reducing, or delaying, the infection and inflammatory components. It will be of great interest to observe whether early HEMT intervention will slow the development of structural disease later in life, and it appears that we will now be able to use CT to start these observations at a very early age.
Sadly, we appear to be on the cusp of a naturalistic study of CFTR modulators in very young children with CF that may inform this discussion. Although the global CF community likely concurs that there is potential for early modulator access to retard lung disease progression by improving CFTR activity in the airway, the reality is that the cost of these drugs to payers (whether public or private) has produced regional disparities in modulator access to very young children with CF. It may be that a decade from now, it will be possible to use the CT methodologies described by WIJKER et al to discriminate between those children with CF who enjoyed access to CFTR modulators early in life and those who did not.
Carzino R, Frayman KB, King L, Vidmar S, Ranganathan S; AREST CF. Regional differences in infection and structural lung disease in infants and young children with cystic fibrosis. J Cyst Fibros. 2019 Nov 6. pii: S1569-1993(19)3-6. doi: 10.1016/j.jcf.2019.10.018. [Epub ahead of print][Pubmed]

Rosemary Carzino
Both infection and inflammation are critical to the progression of cystic fibrosis (CF) lung disease. Potential anatomical differences in lower airway infection, inflammation and bronchiectasis in young children with CF raise questions regarding the pathogenesis of early structural lung disease.
A longitudinal multi-centre birth cohort study of infants newly diagnosed with CF was conducted. Paired bronchoalveolar lavage (BAL) samples were obtained from the right middle lobe (RML) and lingula bronchi. Chest computed tomography (CT) was performed biennially and analysed using the modified CF-CT scoring system.
One hundred and twenty-four children (0.11 – 7.0 years) contributed 527 BAL samples and underwent 388 CT chest scans. Pro-inflammatory microbes were detected in 279 BAL samples (53%), either in both lingula and RML samples (69%), in the lingula alone (24%), or in the RML alone in only 7% of samples. Overall, the prevalence of structural lung disease was greater in the setting of pro-inflammatory microbes. Although infection was less commonly isolated in the right lung, bronchiectasis was more commonly detected in the right lung compared with the left. No anatomical differences in the presence of air trapping were detected.
The authors concluded overall that the detection of pro-inflammatory microbes in the lower airways was associated with increased risk of both air trapping and bronchiectasis. However, the apparent discordance between commonest sites of isolation of pro-inflammatory microbes and the anatomical site of early bronchiectasis warrants further exploration.
Rosemary Carzino is Senior Research Assistant at the Respiratory Diseases Group, Murdoch Children’s Research Institute, Victoria, Australia.
Samuel T Montgomery, Dario L Frey, Marcus A Mall, Stephen M Stick, Anthony Kicic , AREST CF. Rhinovirus Infection Is Associated With Airway Epithelial Cell Necrosis and Inflammation via Interleukin-1 in Young Children With Cystic Fibrosis. Front Immunol 2020 Apr 9;11:596. doi: 10.3389/fimmu.2020.00596. eCollection 2020.[Pubmed]

Samuel T Montgomery
The responses of cystic fibrosis (CF) airway epithelial cells (AEC) to rhinovirus (RV) infection are likely to contribute to early pathobiology of lung disease with increased neutrophilic inflammation and lower apoptosis reported. Necrosis of AEC resulting in airway inflammation driven by IL-1 signalling is a characteristic finding in CF detectable in airways of young children. Being the most common early-life infection, RV-induced epithelial necrosis may contribute to early neutrophilic inflammation in CF via IL-1 signalling. As little is known about IL-1 and biology of CF lung disease, this study assessed cellular and pro-inflammatory responses of CF and non-CF AEC following RV infection, with the hypothesis that RV infection drives epithelial necrosis and IL-1 driven inflammation.
Conclusions: This study found rhinovirus (RV) infection drives necrotic cell death in CF airway epithelial cells (AEC). Furthermore, RV induced IL-1 strongly correlated with necrotic cell death in these cells. As IL-1R signalling drives airway neutrophilia and mucin production, these observations suggest RV infection early in life may exacerbate inflammation and mucin accumulation driving early CF lung disease. Since IL-1R can be targeted therapeutically with IL-1Ra, these data suggest a new anti-inflammatory therapeutic approach targeting downstream effects of IL-1R signalling to mitigate viral-induced, muco-inflammatory triggers of early lung disease.
Dr Samuel T Montgomery is at the Faculty of Health and Medical Sciences, School of Biomedical Sciences, The University of Western Australia, Crawley, WA, Australia.
Prof Geraint B Rogers is a molecular microbiologist and microbial ecologist. He is the Director, Microbiome Research at SAHMRI, leads a laboratory based within the Flinders University School of Medicine, Adelaide
Tim Rosenow, L Clara Mok, Lidija Turkovic, Luke J Berry, Peter D Sly, Sarath Ranganathan, Harm A W M Tiddens, Stephen M Stick The cumulative effect of inflammation and infection on structural lung disease in early cystic fibrosis. Eur Respir J 2019 Jul 11;54(1):1801771.doi: 10.1183/13993003.01771-2018. Print 2019 Jul. [Pubmed]

Tim Rosenow
Introduction: Pulmonary inflammation and infection are important clinical and prognostic markers of lung disease in cystic fibrosis (CF). However, whether in young children they are transient findings or have cumulative, long-term impacts on respiratory health is largely unknown. We aimed to determine whether their repeated detection has a deleterious effect on structural lung disease.
Methods: All patients aged <6 years with annual computed tomography (CT) and bronchoalveolar lavage (BAL) were included. Structural lung disease on CT (%Disease) was determined using the PRAGMA-CF (Perth-Rotterdam Annotated Grid Morphometric Analysis for CF) method. The number of times free neutrophil elastase (NE) and infection were detected in BAL were counted, to determine cumulative BAL history. Linear mixed model analysis, accounting for repeat visits and adjusted for age, was used to determine associations.
Results: 265 children (683 scans) were included for analysis, with BAL history comprising 1161 visits. %Disease was significantly associated with the number of prior NE (0.31, 95% CI 0.09-0.54; p=0.007) but not infection (0.23, 95% CI -0.01-0.47; p=0.060) detections. Reference equations were determined.
Conclusions: Pulmonary inflammation in surveillance BAL has a cumulative effect on structural lung disease extent, more so than infection. This provides a strong rationale for therapies aimed at reducing inflammation in young children
Dr Tim Rosenow is a physicist and senior research fellow at the Telethon Kids Institute, Centre for Child Health Research, University of Western Australia, Subiaco, Australia
Barreda CB, Farrell PM, Laxova A, Eickhoff JC, Braun AT, Coller RJ, Rock MJ. Newborn screening alone insufficient to improve pulmonary outcomes for cystic fibrosis. J Cyst Fibros. 2020 Jun 13:S1569-1993(20)30731-1. doi: 10.1016/j.jcf.2020.06.002. Online ahead of print.[Pubmed]

Christina Barreda
The Wisconsin Cystic Fibrosis Neonatal Screening Project was a randomized clinical trial (RCT) revealing that children receiving an early diagnosis of CF via newborn screening (NBS) had improved nutritional outcomes but similar lung disease severity compared to those who presented clinically. Because the evaluations of these subjects by protocol ended in 2012, our objective was to assess long-term pulmonary and mortality outcomes.
Retrospective analysis of the RCT cohort utilized longitudinal outcome measures obtained from the Cystic Fibrosis Foundation Patient Registry (CFFPR). Data included screening assignment, clinical characteristics, percent predicted forced expiratory volume in 1 s (ppFEV1) and mortality. A random intercept model was used to compare the ppFEV1 decline of subjects between the two groups up to age 26 years. Mortality was analyzed using the Kaplan-Meier method.
Of the 145 subjects who consented to the original study, 104 subjects met inclusion criteria and had adequate data in the CFFPR. Of 57 subjects in the screened group and 47 in the control group, the rates of ppFEV1 decline were 1.76%/year (95% CI 1.62 to 1.91%) and 1.43%/year (95% CI 1.26 to 1.60%), respectively (p<0.0002). Pseudomonas aeruginosa acquired before 2 years was partially responsible. There was no difference in mortality between the two groups
Conclusions: NBS alone does not improve pulmonary outcomes in CF, particularly when other risk factors supervene. In an era prior to strict infection control and current therapies, NBS for CF may be associated with worse pulmonary outcomes.
Dr Christina B Barreda is a paediatrician in the Department of Pediatrics, University of Wisconsin-Madison School of Medicine and Public Health.
Davies G, Thia LP, Stocks J, Bush A, Hoo AF, Wade A, Nguyen TTD, Brody AS, Calder A, Klein NJ, Carr SB, Wallis C, Suri R, Pao CS, Ruiz G, Balfour-Lynn IM; London Cystic Fibrosis Collaboration (LCFC). Minimal change in structural, functional and inflammatory markers of lung disease in newborn screened infants with cystic fibrosis at one year. J Cyst FIBROS 2020 Feb 7. pii: S1569-1993(20)30031-X.doi: 10.1016/j.jcf.2020.01.006. [Epub ahead of print] [Pubmed[]
With the widespread introduction of newborn screening for cystic fibrosis(CF), there has been considerable emphasis on the need to develop objective markers of lung health that can be used during infancy. We hypothesised that in a newborn screened (NBS) UK cohort, evidence of airway inflammation and infection at one year would be associated with adverse structural and functional outcomes at the same age.
Infants underwent lung function testing, chest CT scan and bronchoscopy with bronchoalveolar lavage (BAL) at 1 year of age when clinically well. Microbiology cultures were also available from routine cough swabs.
65 infants had lung function, CT and BAL. Mean (SD) lung clearance index and forced expiratory volume in 0.5 s z-scores were 0.9(1.2) and -0.6(1.1) respectively; median Brody II CF-CT air trapping score on chest CT =0 (interquartile range 0-1, maximum possible score 27). Infants isolating any significant pathogen by 1 yr of age had higher LCI z-score (mean difference 0.9; 95%CI:0.4-1.4; p = 0.001) and a trend towards higher air trapping scores on CT (p = 0.06). BAL neutrophil elastase was detectable in 23% (10/43) infants in whom BAL supernatant was available. This did not relate to air trapping score on CT.
The authors concluded that in this UK NBS cohort at one year of age, lung and airway damage is much milder and associations between inflammation, abnormal physiology and structural changes were at best weak, contrary to our hypothesis and previously published reports. Continued follow-up will clarify longer term implications of these very mild structural, functional and inflammatory changes.
Dr Gwyneth Davies is a Research Associate Respiratory, Critical Care and Anaesthesia section, UCL Great Ormond Street Institute of Child Health (GOS ICH), London,
Claire Nissenbaum , Gwyneth Davies , Alexander Horsley, Jane C Davies Monitoring early stage lung disease in cystic fibrosis. Curr Opin Pulm Med 2020 Sep 10. doi: 10.1097/MCP.0000000000000732.Online ahead of print. [Pubmed]

Claire Nissenbaum
Early stage lung disease has long been synonymous with infancy and childhood. As diagnosis happens earlier and conventional management improves, we are seeing larger proportions of people with cystic fibrosis) in adolescence and even adulthood with well-preserved lung health. The availability of highly effective cystic fibrosis transmembrane conductance regulator modulator drugs for a large proportion of the CF population will impact even further. Transitioning into adult care with ‘normal’ lung function will become more common. However, it is crucial that we are not blasé about this phase, which sets the scene for future lung health. It is well recognized that lung function assessed by spirometry is insensitive to ‘early’ changes occurring in the distal, small airways. Much of our learning has come from studies in infants and young children, which have allowed assessment and optimization of alternative forms of monitoring.
Here, as a group of paediatric and adult CF specialists, the authors review the evidence base for sensitive physiological testing based on multibreath washout, lung imaging, exercise and activity monitoring, assessment of infection and quality of life measures. They seek to emphasise the importance of further work in these areas, as outcome measures become widely applicable to a growing CF population.
Dr Claire Nissenbaum is in the Division of Infection, Immunity & Respiratory Medicine, Manchester University and the Manchester Adult Cystic Fibrosis Centre.
M Pollak , M Shaw , S Balkovec , D Wilson , K Kowalik , P Subbarao, F Ratjen Infant spirometry as a predictor of lung function at early childhood in cystic fibrosis patients. J Cyst Fibros. 2020 Sep 17;2116. doi: 10.1016/j.jcf.2020.09.005. Online ahead of print. [Pubmed]
Infant pulmonary function testing using the raised volume rapid thoracoabdominal compression (RVRTC) technique requires sedation and is time consuming. Many cystic fibrosis (CF) centers do not have access to equipment and the utility of routine testing remains to be determined. The authors aimed to assess whether RVRTC tests performed during infancy predict spirometry at early school age.
The RVRTC-based forced expiratory flow measures in infants were compared to the first adequately performed spirometry at school age. All tests were carried out during routine clinic visits and expressed as age related z-scores; only test occasions where patients were considered stable were included in the analysis
The infant RVRTC measures were not predictive of pulmonary function in early school age, likely due to the high proportion of measures of forced expiratory flows within the normal range at both time points.
Dr M Pollak is in the Division of Respiratory Medicine Hospital for Sick Children, Toronto, ON, Canada.
Jose Caparrós-Martín, Stephanie Flynn, F Jerry Reen, David F Woods, Patricia Agudelo-Romero, Sarath C Ranganathan , Stephen M Stick, Fergal O’Gara. The Detection of Bile Acids in the Lungs of Paediatric Cystic Fibrosis Patients Is Associated With Altered Inflammatory Patterns. Diagnostics (Basel). 2020 May 6;10(5):E282.doi: 10.3390/diagnostics10050282. [Pubmed]

Fergal Ogara

Jose Caparros-Martin
Cystic fibrosis respiratory disease starts early in life, with the detection of inflammatory markers and infection evident even before respiratory symptoms arise. Thus, identifying factors that dysregulate immune responsiveness at the earliest stages of the disease will provide novel targets for early therapeutic intervention.
The authors evaluated the clinical significance of bile acid detection in the bronchoalveolar lavage fluid of clinically stable preschool-aged children diagnosed with CF. Results: We applied an unbiased classification strategy to categorize these specimens based on bile acid profiles. We provide clear associations linking the presence of bile acids in the lungs with alterations in the expression of inflammatory markers. Using multiple regression analysis, we also demonstrate that clustering based on bile acid profiles is a meaningful predictor of the progression of structural lung disease.
The authors consider their work has identified a clinically relevant host-derived factor that may participate in shaping early events in the aetiology of CF respiratory disease.
Dr Jose A Caparrós-Martín is a Research Associate with the Human Microbiome Programme, School of Pharmacy and Biomedical Sciences, Curtin University, Perth 6102, Australia and the Curtin Health Innovation Research Institute (CHIRI), Curtin University, Perth 6102, Australia. He is senior researcher in the Human Microbiome Programme directed by Professor Fergal O’Gara.
Barry Linnane , Aaron M Walsh, Calum J Walsh, Fiona Crispie, Orla O’Sullivan, Paul D Cotter, Michael McDermott, Julie Renwick, Paul McNally. The Lung Microbiome in Young Children with Cystic Fibrosis: A Prospective Cohort Study. Microorganisms 2021 Feb 26;9(3):492.doi: 10.3390/microorganisms9030492. Free article [Pubmed]

Julie Renwick

Barry Linnane
The objective of this study was to thoroughly characterise the lower airway microbiome in pre-school children with CF. Bronchoalveolar lavage (BAL) samples were collected annually from children attending the three clinical centres. Clinical and demographic data were collated on all subjects alongside BAL inflammatory markers. Data on 292 sequenced BALs from 101 children with CF and 51 without CF show the CF lung microbiome, while broadly similar to that in non-CF children, is distinct. Alpha diversity between the two cohorts was indistinguishable at this early age. The CF diagnosis explained only 1.1% of the variation between the cohort microbiomes.
However, several key genera were significantly differentially abundant between the groups. While the non-CF lung microbiome diversity increased with age, diversity reduced in CF with age. Pseudomonas and Staphylococcus were more abundant with age, while genera such as Streptococcus, Porphyromonas and Veillonella were less abundant with age.
There was a negative correlation between alpha diversity and interleukin-8 and neutrophil elastase in the CF population. Neither current flucloxacillin or azithromycin prophylaxis, nor previous oral or IV antibiotic exposure, was correlated with microbiome diversity. Consecutive annual BAL samples over 5 years from a subgroup of children demonstrated diverse patterns of development in the first years of life.
Dr Barry Linnane is at the Centre for Interventions in Infection, Inflammation and Immunity (4i) and Graduate Entry Medical School, University of Limerick, Limerick V94 T9PX, Ireland.
Corresponding author is Dr Julie Renwick, Assistant Professor of Clinical Microbiology, School of Medicine, Trinity College, Dublin. She cofounded the Airway Microbiome in Cystic Fibrosis project
– There is a detailed full version available. There are no definite suggestions as to the practical implications of the findings
Dr Sarah E Bauer is a Fellow at Pediatrics, Indiana University, Indianapolis, IN, United States.
Katie J Bayfield , Tonya A Douglas , Tim Rosenow, Jane Carolyn Davies, Stuart J Elborn, Marcus Mall, Anthony Paproki, Felix Ratjen, Peter D Sly, Alan Robert Smyth, Stephen Stick, Claire E Wainwright, Paul D Robinson. Time to get serious about the detection and monitoring of early lung disease in cystic fibrosis.Thorax. 2021 Apr 29;thoraxjnl-2020-216085.doi: 10.1136/thoraxjnl-2020-216085. Online ahead of print. [Pubmed]

Tonya Douglas

Katie Bayfield
Structural and functional defects within the lungs of children with cystic fibrosis (CF) are detectable soon after birth and progress throughout preschool years often without overt clinical signs or symptoms. By school age, most children have structural changes such as bronchiectasis or gas trapping/hypoperfusion and lung function abnormalities that persist into later life. Despite improved survival, gains in forced expiratory volume in one second (FEV1) achieved across successive birth cohorts during childhood have plateaued, and rates of FEV1 decline in adolescence and adulthood have not slowed. This suggests that interventions aimed at preventing lung disease should be targeted to mild disease and commence in early life. Spirometry-based classifications of ‘normal’ (FEV1≥90% predicted) and ‘mild lung disease’ (FEV1 70%-89% predicted) are inappropriate, given the failure of spirometry to detect significant structural or functional abnormalities shown by more sensitive imaging and lung function techniques.
The state and readiness of two imaging (CT and MRI) and two functional (multiple breath washout and oscillometry) tools for the detection and monitoring of early lung disease in children and adults with CF are discussed in this article. Prospective research programmes and technological advances in these techniques mean that well-designed interventional trials in early lung disease, particularly in young children and infants, are possible. Age appropriate, randomised controlled trials are critical to determine the safety, efficacy and best use of new therapies in young children. Regulatory bodies continue to approve medications in young children based on safety data alone and extrapolation of efficacy results from older age groups.
Harnessing the complementary information from structural and functional tools, with measures of inflammation and infection, will significantly advance our understanding of early CF lung disease pathophysiology and responses to therapy. Defining clinical utility for these novel techniques will require effective collaboration across multiple disciplines to address important remaining research questions. Future impact on existing management burden for patients with CF and their family must be considered, assessed and minimised.
To address the possible role of these techniques in early lung disease, a meeting of international leaders and experts in the field was convened in August 2019 at the Australiasian Cystic Fibrosis Conference. The meeting entitiled ‘Shaping imaging and functional testing for early disease detection of lung disease in Cystic Fibrosis’, was attended by representatives across the range of disciplines involved in modern CF care. This document summarises the proceedings, key priorities and important research questions highlighted.
Dr Katie J Bayfield is in the Department of Respiratory Medicine, Children’s Hospital at Westmead, Westmead, New South Wales, Australia.
Dr Tonya A Douglas is Department of Respiratory and Sleep Medicine, Queensland Children’s Hospital, South Brisbane, Queensland, Australia and the Child Health Research Centre, The University of Queensland, Brisbane, Queensland, Australia.
Pedro Mondéjar-López, Alexander Horsley, Felix Ratjen, Silvia Bertolo, Helene de Vicente, Òscar Asensio de la Cruz. A multimodal approach to detect and monitor early lung disease in cystic fibrosis. Expert Rev Respir Med. 2021 Apr 12;1-12.doi: 10.1080/17476348.2021.1908131.Online ahead of print.[Pubmed]

Pedro Mondejar-López
Introduction: In the early stages, lung involvement in cystic fibrosis (CF) can be silent, with disease progression occurring in the absence of clinical symptoms. Irreversible airway damage is present in the early stages of disease; however, reliable biomarkers of early damage due to inflammation and infection that are universally applicable in day-to-day patient management have yet to be identified.
Areas covered: At present, the main methods of detecting and monitoring early lung disease in CF are the lung clearance index (LCI), computed tomography (CT), and magnetic resonance imaging (MRI). LCI can be used to detect patients who may require more intense monitoring, identify exacerbations, and monitor responses to new interventions. High-resolution CT detects structural alterations in the lungs of CF patients with the best resolution of current imaging techniques. MRI is a radiation-free imaging alternative that provides both morphological and functional information. The role of MRI for short-term follow-up and pulmonary exacerbations is currently being investigated.
Expert opinion: The roles of LCI and MRI are expected to expand considerably over the next few years. Meanwhile, closer collaboration between pulmonology and radiology specialties is an important goal toward improving care and optimizing outcomes in young patients with CF.
Dr Pedro Mondéjar-López is Pediatric Pulmonologist at the Pediatric Pulmonology and Cystic Fibrosis Unit, University Hospital Virgen de la Arrixaca, Murcia, Spain.
Daniela K Schlüter, Josh S Ostrenga, Siobhán B Carr , Aliza K Fink, Albert Faro, Rhonda D Szczesniak, Ruth H Keogh, Susan C Charman, Bruce C Marshall, Christopher H Goss, David Taylor-Robinson. Lung function in children with cystic fibrosis in the USA and UK: a comparative longitudinal analysis of national registry data. Thorax 2021 May 11;thoraxjnl-2021-216849. doi: 10.1136/thoraxjnl-2021-216849.Online ahead of print. [Pubmed]

Daniela Schlüter
Rationale: A previous analysis found significantly higher lung function in the US paediatric cystic fibrosis (CF) population compared with the UK with this difference apparently decreasing in adolescence and adulthood. However, the cross-sectional nature of the study makes it hard to interpret these results.
Conclusions: Children with CF and homozygous F508del genotype in the USA had better lung function than UK children. These differences do not appear to be explained by early growth or nutrition, but differences in the use of early treatments need further investigation
Insa Korten, Marc-Alexander Oestreich, Urs Frey, Alexander Moeller, Andreas Jung, Renate Spinas, Dominik Mueller-Suter, Daniel Trachsel, Isabelle Rochat, Ben Spycher, Philipp Latzin, Carmen Casaulta, Kathryn Ramsey, SCILD, and BILD, study group. Respiratory symptoms do not reflect functional impairment in early CF lung disease. J Cyst Fibros 2021 Jun 1;S1569-1993(21)00116-8.doi: 10.1016/j.jcf.2021.04.006.Online ahead of print. [Pubmed]

Insa Korten
Background: Lung disease can develop within the first year of life in infants with cystic fibrosis (CF). However, the frequency and severity of respiratory symptoms in infancy are not known.
Methods: We assessed respiratory symptoms in 50 infants with CF and 50 healthy matched controls from two prospective birth cohort studies. Respiratory symptoms and respiratory rate were documented by standardized weekly interviews throughout the first year. Infants performed multiple breath washout in the first weeks of life.
Results: We analyzed 4552 data points (2217 in CF). Respiratory symptoms (either mild or severe) were not more frequent in infants with CF (OR:1.1;95% CI:[0.76, 1.59]; p=0.6). Higher lung clearance index and higher respiratory rate in infants with CF were not associated with respiratory symptoms.
Conclusions: We found no difference in respiratory symptoms between healthy and CF infants. These data indicate that early CF lung disease may not be captured by clinical presentation alone
Dr Insa Korten is in the Division of Paediatric Respiratory Medicine and Allergology, Department of Paediatrics, Inselspital, Bern Unviersity Hospital, University of Bern, Switzerland.
Daniela K Schlüter is a lecturer in Public Health Data Science in the Department of Public Health, Policy and Systems, University of Liverpool, Liverpool, UK
Paul McNally, Daryl Butler, Yuliya V Karpievitch, Barry Linnane , Sarath Ranganathan, Stephen M Stick , Graham L Hall, Andre Schultz, SHIELD CF and ARESTCF. Ivacaftor and Airway Inflammation in Preschool Children with Cystic Fibrosis. Am J Respir Crit Care Med 2021 Jun 2.doi: 10.1164/rccm.202012-4332LE.Online ahead of print. [Pubmed]

Paul McNally
The authors comment – Notwithstanding certain limitations to our study, our data suggest that in stable preschool children with CF, ivacaftor does not have a significant beneficial effect on airway infection and inflammation. Therefore caution should be applied in this group of children before discontinuing, avoiding or delaying the use of the use of traditional treatments that we might typically prescribe such as airway clearance, mucoactive agents and antibiotics
Paul McNally is Associate Professor of Paediatrics at the at the RCSI, 8863, Paediatrics, Dublin, Ireland and Children’s Health Ireland, 575376, Respiratory Medicine, Dublin, Ireland; paulmcnally@rcsi.ie.
Heather N Muston, James E Slaven, Christina Tiller, Charles Clem, Thomas W Ferkol, Sarath Ranganathan, Stephanie D Davis, Clement L Ren. Hyperinflation is Associated with Increased Respiratory Rate and is a More Sensitive Measure of Cystic Fibrosis Lung Disease During Infancy Compared to Forced Expiratory Measures. Pediatr Pulmonol 2021 Jun 18.doi: 10.1002/ppul.25538. Online ahead of print. [Pubmed]

Heather Muston
Background: The goal of this study was to identify clinical features associated with abnormal infant pulmonary function tests (iPFTs), specifically functional residual capacity (FRC), in infants with cystic fibrosis (CF) diagnosed via newborn screen (NBS). We hypothesized that poor nutritional status in the first 6-12 months would be associated with increased FRC at 12-24 months.
Methods: This study utilized a combination of retrospectively and prospectively collected data from ongoing research studies and iPFTs performed for clinical indications. Demographic and clinical features were obtained from the electronic medical record. Forced expiratory flows and volumes were obtained using the raised volume rapid thoracoabdominal technique (RVRTC) and FRC was measured via plethysmography.
Results: A total of 45 CF NBS infants had iPFTs performed between 12-24 months. Mean forced vital capacity, forced expiratory volume in 0.5 second, and forced expiratory flows were all within normal limits. In contrast, the mean FRC z-score was 2.18 (95%CI=1.48, 2.88) and the mean respiratory rate (RR) z-score was 1.42 (95%CI=0.95, 1.89). There was no significant association between poor nutritional status and abnormal lung function. However, there was a significant association between higher RR and increased FRC, and a RR cut off of 36 breaths/min resulted in 92% sensitivity to detect hyperinflation with 32% specificity.
Conclusions: These results suggest that FRC is a more sensitive measure of early CF lung disease than RVRTC measurements and that RR may be a simple, non-invasive clinical marker to identify CF NBS infants with hyperinflation.
Heather N Muston is Assistant Professor of Pediatrics in the Division of Pediatric Pulmonology, Allergy and Sleep Medicine, Department of Pediatrics, Indiana University School of Medicine, Indianapolis, IN.
– This is an interesting and practically useful article confirming the value of a simple clinical sign, a raised respiratory rate, with functional residual capacity – an early measure of infant lung disease
Mirjam Stahl, Eva Steinke , Simon Y Graeber, Cornelia Joachim, Christoph Seitz, Hans-Ulrich Kauczor, Monika Eichinger, Susanne Hämmerling, Olaf Sommerburg, Mark O Wielpütz, Marcus A Mall. Magnetic Resonance Imaging Detects Progression of Lung Disease and Impact of Newborn Screening in Preschool Children with Cystic Fibrosis. Am J Respir Crit Care Med. 2021 Jul 20., oi: 10.1164/rccm.202102-0278OC.Online ahead of print. [Pubmed]

Mirjam Stahl
Rationale: Previous cross-sectional studies demonstrated that chest magnetic resonance imaging (MRI) is sensitive to detect early lung disease in infants and preschool children with cystic fibrosis (CF) without radiation exposure. However, the ability of MRI to detect progression of lung disease and the impact of early diagnosis in preschool children with CF remains unknown.
Objectives: To investigate the potential of MRI to detect progression of early lung disease and impact of early diagnosis by CF newborn screening (NBS) in preschool children with CF.
Methods: Annual MRI was performed from diagnosis over four years in a cohort of 96 preschool children with CF (age 0-4 yr) that were concurrently diagnosed based on NBS (n=28) or clinical symptoms (n=68). MRI scans were evaluated using a dedicated morphofunctional score and the relationship between longitudinal MRI scores and respiratory symptoms, pulmonary exacerbations, upper airway microbiology and mode of diagnosis were determined.
Measurements and main results: The MRI global score increased in the total cohort of children with CF during preschool years (P<0.001) which was associated with cough, pulmonary exacerbations (P<0.0001), and detection of Staphylococcus aureus and Haemophilus influenzae (P<0.05). MRI-defined abnormalities in lung morphology, especially airway wall thickening/bronchiectasis, were lower in NBS compared to clinically diagnosed children with CF throughout the observation period (P<0.01).
Conclusions: MRI detected progression of early lung disease and benefits of early diagnosis by NBS in preschool children with CF. These findings support MRI as sensitive outcome measure for diagnostic monitoring and early intervention trials in preschool children with CF.
Mirjam Stahl is at the Charité Universitätsmedizin Berlin, 14903, Department of Pediatric Pulmonology, Immunology and Critical Care Medicine, Berlin, Germany.German Center for Lung Research (DZL), associated partner site, Berlin, Germany.University of Heidelberg, Department of Translational Pulmonology, Heidelberg, Germany.German Center for Lung Research (DZL), Translational Lung Research Center Heidelberg (TLRC), Heidelberg, Germany
Bouzek DC, Abou Alaiwa MH, Adam RJ, Pezzulo AA, Reznikov LR, Cook DP, et al. Early Lung Disease Exhibits Bacterial-Dependent and -Independent Abnormalities in Cystic Fibrosis Pigs. Am J Respir Crit Care Med [online ahead of print] 25 June 2021 [Pubmed]

Drake C Bouzek
Rationale: While it is clear that cystic fibrosis airway disease begins at a very young age, the early and subsequent steps in disease pathogenesis and the relative contribution of infection, mucus, and inflammation are not well understood.
Objectives: As one approach to assessing the early contribution of infection, we tested the hypothesis that early and continuous antibiotics would decrease the airway bacterial burden. We thought that, if it does, it might reveal aspects of the disease that are more or less sensitive to decreasing infection.
Methods: Three groups of pigs were studied from birth until ~3 weeks of age: 1) wild-type, 2) cystic fibrosis, and 3) cystic fibrosis pigs treated continuously with broad-spectrum antibiotics from birth until study completion. Disease was assessed with chest computed tomography, histopathology, microbiology, and bronchoalveolar lavage.
Measurements and Main Results: Disease was present by 3 weeks of age in cystic fibrosis pigs. Continuous antibiotics from birth improved chest computed tomography imaging abnormalities and airway mucus accumulation, but not airway inflammation in the cystic fibrosis pig model. However, reducing bacterial infection did not improve two disease features already present at birth in cystic fibrosis pigs, air trapping and submucosal gland duct plugging. In the cystic fibrosis sinuses, antibiotics did not prevent the development of infection, disease, or the number of bacteria but did alter the bacterial species.
Conclusions: These findings suggest that cystic fibrosis airway disease begins immediately following birth, and that early and continuous antibiotics impact some, but not all, aspects of CF lung disease development
Dr Drake C Bouzek of the The University of Iowa Roy J and Lucille A Carver College of Medicine, 12243, Iowa City, Iowa, United States
Shiping Lu, Jay K Kolls. Early Antibiotics in Cystic Fibrosis: Lessons from the CF Pig Model. Am J Respir Crit Care Med. 2021 Aug 3.doi: 10.1164/rccm.202106-1383ED.Online ahead of print. Pubmed
(Commentary on the above article by Bouzek et al.

Jay K Kolls

Shipping Lu
Cystic fibrosis (CF) is caused by mutations in cystic fibrosis transmembrane conductance regulator (CFTR), which results in defects in ion transport. The leading causes of morbidity and mortality are respiratory symptoms and progressive pulmonary failure. Three hallmarks of this pathogenesis identified to date are abnormal mucus accumulation/tethering, chronic sinopulmonary inflammation, and recurrent infections(1). But there has been continued debate about what comes first: infection or inflammation akin to the chicken or the egg argument.
This is a detailed referenced commentary on the relationship between inflammation and infection in the CF infant. The main text finishes – “As the clinical studies continue to be performed in younger individuals, it will be critical to understand how these drugs impact both mucous clearance, airways inflammation, and infection. Although, this paper focused on the contributions of bacterial infection, we know there is a complex interplay between viral infection and bacterial infection and specifically bacterial biofilm formation and this will be an important area to model in pre-clnical models. This paper highlights the potential need to target inflammation independent of infection to have the greatest impact in preserving lung function in patients with CF”.
Dr Jay K Kolls, the corresponding author, is Professor of Medicine and Pediatrics at Tulane University School of Medicine, 12255, Medicine, New Orleans, Louisiana, United States.
Dr Shiping Lu is a Faculty Member Center for Translational Research in Infection and Inflammation Tulane University Health Sciences Center
Thomas Lahiri, Jillian S Sullivan. Recent advances in the early treatment of cystic fibrosis: Bridging the gap to highly effective modulator therapy. Pediatr Pulmonol. 2021 Sep 2.doi: 10.1002/ppul.25660. Online ahead of print. [Pubmed]
Thomas Lahiri
Highly effective modulator therapy (HEMT) for cystic fibrosis (CF) has been touted as one of the greatest advances to date in CF care. As these therapies are now available for many older children and adults with CF, marked improvement of their nutritional status, pulmonary and gastrointestinal symptoms has been observed. However, most infants and younger children are not current candidates for HEMT due to age and/or cystic fibrosis transmembrane conductance regulator (CFTR) mutation. For these young children, it is essential to provide rigorous monitoring and care to avoid potential disease sequelae while awaiting HEMT availability. The following article highlights recent advances in the care of infants and young children with CF with regard to surveillance and treatment of nutritional, pulmonary, and gastrointestinal disorders. Recent clinical trials in this population are also reviewed.
Dr Thomas Lahiri is a paediatric pulmonologist in the Divisions of Pediatric Pulmonology and Gastroenterology,
Jobst F Roehmel, Friederike J Doerfler, Cordula Koerner-Rettberg, Folke Brinkmann, Anne Schlegtendal, Martin Wetzke, Isa Rudolf, Simone Helms, Joerg Große-Onnebrink, Yin Yu, Thomas Nuesslein, Irena Wojsyk-Banaszak, Sebastian Becke, Olaf Eickmeier, Olaf Sommerburg, Heymut Omran, Mirjam Stahl, Marcus A Mall Comparison of the Lung Clearance Index in Preschool Children with Primary Ciliary Dyskinesia and Cystic Fibrosis Chest. 2022 Mar 7;S0012-3692(22)00421-4.doi: 10.1016/j.chest.2022.02.052.Online ahead of print. [Pubmed]

Jobst Roshmel
Background: Previous studies have shown that the lung clearance index (LCI) determined by multiple-breath washout (MBW) is sensitive to detect early lung disease in preschool children with cystic fibrosis (CF). In preschool children with primary ciliary dyskinesia (PCD), data on the onset and severity of lung disease and on the sensitivity of the LCI as a noninvasive quantitative outcome measure remain limited.
Research and study question: Is MBW feasible and sensitive to detect ventilation inhomogeneity in preschool children with PCD?
Study design and methods: This was a prospective cross-sectional multicenter study and included preschoolers with PCD and preschoolers with CF and healthy controls. LCI was determined using nitrogen MBW, and compared between the three groups.
Results: LCI was determined in 27 children with PCD, 34 children with CF and 30 healthy controls (mean age, 4.8 years; range, 2.2 – 6.9 years). The LCI in preschool children with PCD was increased (median, 9.1; CI 95%, 8.6-10.3) compared to healthy controls (median, 7.0; CI 95%, 6.7-7.1), (P < 0.0001), but did not differ from preschool children with CF (median, 8.6; CI 95%, 8.4-9.7), (P = 0.71). The feasibility in the PCD group was 93.1% and was similar to that in the CF group (91.9%) and in healthy controls (85.7%), (P = 0.55).
Interpretation: This study demonstrates early onset of lung disease in preschool children with PCD and indicates that lung disease severity in PCD may be similar to that in CF during preschool years. These data support a need for early diagnostic monitoring and therapy and suggest the LCI as a noninvasive diagnostic tool and as a potential endpoint in clinical trials testing early interventions in children with PCD.
Dr Jobst F Roehmel is consultant paediatrician in the Department of Pediatric Respiratory Medicine, Immunology and Critical Care Medicine, Charité – Universitätsmedizin Berlin, corporate member of Freie Universität Berlin and Humboldt-Universität zu Berlin, Berlin, Germany.
Harm A W M Tiddens, Yuxin Chen Eleni-Rosalina Andrinopoulou, Stephanie D Davis, Margaret Rosenfeld, Felix Ratjen, Richard A Kronmal, Karen D Hinckley Stukovsky, Alison Dasiewicz, Stephen Michael Stick, SHIP-CT Study Group Collaborators. The effect of inhaled hypertonic saline on lung structure in children aged 3-6 years with cystic fibrosis (SHIP-CT): a multicentre, randomised, double-blind, controlled trial. Lancet Respir Med 2022 Mar 11;S2213-2600(21)00546-4.doi: 10.1016/S2213-2600(21)00546-4. Online ahead of print [Pubmed]

Harm Tiddens
Background: In the Saline Hypertonic in Preschoolers (SHIP) study, inhaled 7% hypertonic saline improved the lung clearance index in children aged 3-6 years with cystic fibrosis, but it remained unclear whether improvement is also seen in structural lung disease. We aimed to assess the effect of inhaled hypertonic saline on chest CT imaging in children aged 3-6 years with cystic fibrosis.
Methods: Children with cystic fibrosis were enrolled in this multicentre, randomised, double-blind, controlled study at 23 cystic fibrosis centres in Spain, Denmark, the Netherlands, Italy, France, Belgium, the USA, Canada, and Australia. Eligible participants were children aged 3-6 years who were able to cooperate with chest CT imaging and comply with daily nebuliser treatment. Participants were randomly assigned 1:1 to receive inhaled 2 puffs of 100 μg salbutamol followed by 4mL of either 7% hypertonic saline or 0·9% isotonic saline twice per day for 48 weeks. Randomisation was stratified by age in North America and Australia, and by age and country in Europe. Chest CTs were obtained at baseline and 48 weeks and scored using the Perth-Rotterdam Annotated Grid Morphometric Analysis for Cystic Fibrosis (PRAGMA-CF) method. The primary outcome was the difference between groups in the percentage of total lung volume occupied by abnormal airways (PRAGMA-CF %Disease) measured by chest CT at 48 weeks. Analysis was by intention-to-treat. This study is registered withClinicaltrials.gov, NCT02950883.
Findings: Between May 24, 2016, and Dec 18, 2019, 134 children were assessed for inclusion. 18 patients were excluded (nine had incomplete or unsuccessful chest CT at enrolment visit, two could not comply with CT training, two had acute respiratory infection, two withdrew consent, two for reasons unknown, and one was already on hypertonic saline). 116 participants were enrolled and randomly assigned to hypertonic saline (n=56) or isotonic saline (n=60). 12 patients dropped out of the study (seven in the hypertonic saline group and five in the isotonic saline group). Mean PRAGMA-CF %Disease at 48 weeks was 0·88% (95% CI 0·60-1·16) in the hypertonic saline group and 1·55% (1·25-1·84) in the isotonic saline group (mean difference 0·67%, 95% CI 0·26-1·08; p=0·0092) based on a linear regression model adjusted for baseline %Disease values and baseline age. Most adverse events in both groups were rated as mild, and the most common adverse event in both groups was cough.
Interpretation: Inhaled hypertonic saline for 48 weeks had a positive effect on structural lung changes in children aged 3-6 years with cystic fibrosis relative to isotonic saline. This is the first demonstration of an intervention that alters structural lung disease in children aged 3-6 years with cystic fibrosis.
Prof. Harm A W M Tiddens is in the Department of Paediatrics, Division of Respiratory Medicine and Allergology, Sophia Children’s Hospital, Erasmus MC, Rotterdam, Netherlands; Department of Radiology and Nuclear Medicine, Erasmus MC, Rotterdam, Netherlands.
Alex R Horsley, John Belcher, Katie Bayfield, Brooke Bianco, Steve Cunningham, Catherine Fullwood , Andrew Jones, Anna Shawcross, Jaclyn A Smith, Anirban Maitra, Francis J Gilchrist. Longitudinal assessment of lung clearance index to monitor disease progression in children and adults with cystic fibrosis. Thorax 2022 Apr;77(4):357-363.doi: 10.1136/thoraxjnl-2021-216928. Epub 2021 Jul 22. Free PMC article [Pubmed]

Alex Horsley
Background: Lung clearance index (LCI) is a valuable research tool in cystic fibrosis (CF) but clinical application has been limited by technical challenges and uncertainty about how to interpret longitudinal change. In order to help inform clinical practice, this study aimed to assess feasibility, repeatability and longitudinal LCI change in children and adults with CF with predominantly mild baseline disease.
Methods: Prospective, 3-year, multicentre, observational study of repeated LCI measurement at time of clinical review in patients with CF >5 years, delivered using a rapid wash-in system
Results: 112 patients completed at least one LCI assessment and 98 (90%) were still under follow-up at study end. The median (IQR) age was 14.7 (8.6-22.2) years and the mean (SD) FEV1z-score was -1.2 (1.3). Of 81 subjects with normal FEV1 (>-2 z-scores), 63% had raised LCI (indicating worse lung function). For repeat stable measurements within 6 months, the mean (limits of agreement) change in LCI was 0.9% (-18.8% to 20.7%). A latent class growth model analysis identified four discrete clusters with high accuracy, differentiated by baseline LCI and FEV1. Baseline LCI was the strongest factor associated with longitudinal change. The median total test time was under 19 min.
Conclusions: Most patients with CF with well-preserved lung function show stable LCI over time. Cluster behaviours can be identified and baseline LCI is a risk factor for future progression. These results support the use of LCI in clinical practice in identifying patients at risk of lung function decline.
Dr Alex Horsley is in the Division of Infection, Immunity and Respiratory Medicine, The University of Manchester Faculty of Biology, Medicine and Health, Manchester, UK and the Manchester Adult Cystic Fibrosis Centre, Manchester University NHS Foundation Trust, Manchester, UK.
P Aurora, Julie Anne Duncan, S Lum, G Davies, A Wade, J Stocks, L Viviani, E Raywood, C Pao, G Ruiz, A Bush, London Cystic Fibrosis Collaboration (LCFC). Early Pseudomonas aeruginosa predicts poorer pulmonary function in preschool children with cystic fibrosis. J Cyst Fibros 2022 Apr 30;S1569-1993(22)00102-3.doi: 10.1016/j.jcf.2022.04.013.Online ahead of print.[Pubmed]

Paul Aurora
Background: We previously reported relatively normal pulmonary function (2 years of age) and computed tomography (CT, 1 year of age) in cystic fibrosis (CF) newborn screened (NBS) infants. We now report follow up of these children to preschool age.
Methods: 67 NBS children with CF and 41 healthy controls underwent pulmonary function tests in infancy (∼3 months, 1 year and 2 years) and at preschool (3-6 years). Broncho-alveolar lavage (BAL) and CT were undertaken in those with CF at 1 year. Primary outcomes at preschool were lung clearance index (LCI) and forced expired volume (FEV0.75). Risk factors for lung function impairment were identified by regression modelling, emphasising factors that could be identified or measured in the first 2 years of life.
Results: At preschool age children with CF had poorer lung function than controls, mean(95% CI) difference in LCI z-score: 1.47(0.96;1.97) and FEV0.75 z-score -0.54(-0.98; -0.10). Isolation of Pseudomonas aeruginosa before 6 months was a highly significant predictor of raised (abnormal) preschool LCI, associated with a mean (95%CI) increase of 1.69(0.43, 2.95) z-scores, compared to those with no Pseudomonas aeruginosa during the first 2 years of life. Including 2 year LCI and 1 year CT data in the predictive model increased the r2 from 13% to 61%.
Conclusions: Lung function deteriorates after 2 years in NBS children with CF. Isolation of Pseudomonas aeruginosa before 6 months and minor abnormalities of infant lung function tests and CT in infancy are associated with higher preschool LCI.
Paul Aurora is in the Department of Infection, Immunity, Inflammation Research and Teaching Department, UCL Great Ormond Street Institute of Child Health, 30 Guilford Street, London WC1N 1EH, United Kingdom; Respiratory Medicine, Great Ormond Street Hospital for Children NHS Foundation Trust, London, United Kingdom.
Amy Macdougall, Deborah Jarvis, Ruth H Keogh, Cole Bowerman, Diana Bilton, Gwyneth Davies, Siobhán B Carr, Sanja Stanojevic Trajectories of early growth and subsequent lung function in cystic fibrosis: An observational study using UK and Canadian registry data. J Cyst Fibros 2022 Sep 7;S1569-1993(22)00658-0.doi: 10.1016/j.jcf.2022.09.001.Online ahead of print. Free article [Pubmed]

Amy Macdougall Linkedin.com
Background: Understanding the pulmonary impact of changes in early life nutritional status over time in a paediatric CF population may help inform how to use nutritional assessment to guide clinical care. National registry data provides an opportunity to study patterns of weight gain over time at the level of the individual, and thus to gain detailed understanding of the relationship between early weight trajectories and later lung function in children with Cystic Fibrosis (CF).
Methods: Using data from the United Kingdom (UK) and Canadian CF Registries, a mixed effects linear regression model was used to describe children’s weight and BMI z-score trajectories from age 1 to 5 years. The intercept (weight-for-age at age 1) and slope (weight-for-age trajectory) from this model were then used as covariates in a linear regression of first lung function measurement at age 6 years.
Results: In both the UK and Canadian data, greater weight-for-age z-score at age 1 year and greater change in weight-for-age over time were associated with higher FEV1% predicted. A greater weight-for-age z-score at age 1 year was associated with a higher FEV1% predicted (UK: 3.78% (95% CI: 1.76; 4.70); Canada: 3.20% (95%CI: 1.76, 4.70)). These associations were reproduced for BMI z-scores and FVC% predicted.
Conclusions: Early weight-for-age, specifically at age 1 year, and weight-for-age trajectories across early childhood are associated with later lung function. This relationship persists after adjustment for potential confounders. Current guidelines may need to be updated to place less emphasis on a specific cut-off (such as the 10th percentile) and encourage tracking of weight-for-age over time
Dr Amy Macdougall is a research fellow is at the National Heart and Lung Institute, Imperial College London, London, United Kingdom.
Nelufa Begum, Catherine A Byrnes, Joyce Cheney, Peter J Cooper, Emmanuelle Fantino, Nicholas Gailer, Keith Grimwood, Diana GutierrezCardenas , John Massie, Colin F Robertson, Peter D Sly, Harm Awm Tiddens, Claire E Wainwright , Robert S Ware. Factors in childhood associated with lung function decline to adolescence in cystic fibrosis. Cyst Fibros. 2022 Nov;21(6):977-983. doi: 10.1016/j.jcf.2022.03.008. Epub 2022 Mar 24. pubmed.ncbi.nlm.nih.gov/35341694/
Background: Despite improvements in general health and life expectancy in people with cystic fibrosis (CF), lung function decline continues unabated during adolescence and early adult life.
Methods: We examined factors present at age 5-years that predicted lung function decline from childhood to adolescence in a longitudinal study of Australasian children with CF followed from 1999 to 2017.
Results: Lung function trajectories were calculated for 119 children with CF from childhood (median 5.0 [25%-75%=5.0-5.1]) years) to early adolescence (median 12.5 [25%-75%=11.4-13.8] years). Lung function fell progressively, with mean (standard deviation) annual change -0.105 (0.049) for forced vital capacity (FVC) Z-score (p<0.001), -0.135 (0.048) for forced expiratory volume in 1-second (FEV1) Z-score (p<0.001), -1.277 (0.221) for FEV1/FVC% (p<0.001), and -0.136 (0.052) for forced expiratory flow between 25% and 75% of FVC Z-score (p<0.001).
Factors present in childhood predicting lung function decline to adolescence, in multivariable analyses, were hospitalisation for respiratory exacerbations in the first 5-years of life (FEV1/FVC p = 0.001, FEF25-75p = 0.01) and bronchoalveolar lavage neutrophil elastase activity (FEV1/FVC% p = 0.001, FEV1p = 0.05, FEF25-75p = 0.02). No examined factor predicted a decline in the FVC Z-score.
Conclusions: Action in the first 5-years of life to prevent and/or treat respiratory exacerbations and counteract neutrophilic inflammation in the lower airways may reduce lung function decline in children with CF, and these should be targets of future research.
Dr Nelufa Begum is with the Children’s Health and Environment Program, Child Health Research Centre, The University of Queensland, 62 Graham St, South Brisbane, QLD 4101, Australia.
Lucy Perrem, Sanja Stanojevic, Melinda Solomon, Hartmut Grasemann, Neil Sweezey, Valerie Waters, Don B Sanders, Stephanie D Davis, Felix Ratjen. Evaluation of clinically relevant changes in the lung clearance index in children with cystic fibrosis and healthy controls. Thorax. 2022 Apr 15;thoraxjnl-2021-218347.doi: 10.1136/thoraxjnl-2021-218347.Online ahead of print. [Pubmed]

Lucy Perem researchgate.net
Background:The limits of reproducibility of the lung clearance index (LCI) are higher in children with cystic fibrosis (CF) compared with healthy children, and it is currently unclear what defines a clinically meaningful change.
Methods:In a prospective multisite observational study of children with CF and healthy controls (HCs), we measured LCI, FEV1% predicted and symptom scores at quarterly visits over 2 years. Two reviewers performed a detailed review of visits to evaluate the frequency that between visit LCI changes outside ±10%, ±15%, ±20% represented a clinically relevant signal. In the setting of acute respiratory symptoms, we used a generalised estimating equation model, with a logit link function to determine the ability of LCI worsening at different thresholds to predict failure of lung function recovery at follow-up.
Results:Clinically relevant LCI changes outside ±10%, ±15% and ±20% were observed at 25.7%, 15.0% and 8.3% of CF visits (n=744), respectively. The proportions of LCI changes categorised as noise, reflecting biological variability, were comparable between CF and HC at the 10% (CF 9.9% vs HC 13.0%), 15% (CF 4.3% vs HC 3.1%) and 20% (CF 2.4% vs HC 1.0%) thresholds. Compared with symptomatic CF visits without a worsening in LCI, events with ≥10% LCI increase were more likely to fail to recover baseline LCI at follow-up.
Conclusion: The limits of reproducibility of the LCI in healthy children can be used to detect clinically relevant changes and thus inform clinical care in children with CF.
Dr Lucy Perrem is involved with the Division of Respiratory Medicine, The Hospital for Sick Children, Toronto, Ontario, Canada, Postgraduate Medical Education, Royal College of Surgeons in Ireland, Dublin, Ireland. National Children’s Research Centre, Dublin, Ireland. Department of Paediatrics, The University of Toronto, Toronto, Ontario, Canada. Translational Medicine Program, SickKids Research Institute, Toronto, Ontario, Canada.
D B Sanders, U Khan, S L Heltshe, M Skalland, N E West, D R VanDevanter, C H Goss, P A Flume, STOP2 Investigators. Association of site of treatment with clinical outcomes following intravenous antimicrobial treatment of a pulmonary exacerbation. J Cyst Fibros 2022 Jul;21(4):574-580.doi10.1016/j.jcf.2021.11.009 pubmed.ncbi.nlm.nih.gov/34857494/

Don B Sanders
medicine.iu.edu
Background:In the STOP2 (Standardized Treatment of Pulmonary Exacerbations-2) study, intravenous (IV) antimicrobial treatment duration for adults with cystic fibrosis (CF) experiencing pulmonary exacerbations (PEx) was determined based on initial treatment response. The impact of home vs hospital care remains an important clinical question in CF. Our hypothesis was that STOP2 participants treated at home would have less improvement in lung function compared to those treated in the hospital.
Methods:Treating clinicians determined PEx treatment location, which was a stratification factor for STOP2 randomization. Lung function, weight, and symptom recovery were evaluated by treatment location. Propensity scores and inverse probability treatment weighting were used to test for differences in clinical response by treatment location.
Results:In all, 33% of STOP2 participants received IV antimicrobials in the hospital only, 46% both in the hospital and at home, and 21% at home only. Mean (95% CI) ppFEV1 improvement was significantly (p < 0.05) lower for those treated at home only, 5.0 (3.5, 6.5), compared with at home and in the hospital, 7.0 (5.9, 8.1), and in the hospital only, 8.0 (6.7, 9.4). Mean weight (p < 0.001) and symptom (p < 0.05) changes were significantly smaller for those treated at home only compared to those treated in the hospital only.
Conclusions:Compared to PEx treatment at home only, treatment in the hospital was associated with greater mean lung function, respiratory symptom, and weight improvements. The limitations of home IV therapy should be addressed in order to optimize outcomes for adults with CF
Don B Sanders is Associate Professor of Pediatrics at Indiana University School of Medicine, Indianapolis, IN, United States.
Don B Sanders, Ashley R Deschamp, Joseph E Hatch, James E Slaven, Netsanet Gebregziabher, Mariette Kemner-van de Corput, Harm A W M Tiddens, Tim Rosenow, Gregory A Storch, Graham L Hall, Stephen M Stick, Sarath Ranganathan, Thomas W Ferkol, Stephanie D Davis. Association between early respiratory viral infections and structural lung disease in infants with cystic fibrosis. J Cyst Fibros
. 2022 Nov;21(6):1020-1026. doi: 10.1016/j.jcf.2022.04.014. Epub 2022 May 4. pubmed.ncbi.nlm.nih.gov/35523715/

Don B Sanders
Background: Infants with cystic fibrosis (CF) develop structural lung disease early in life, and viral infections are associated with progressive lung disease. We hypothesized that the presence of respiratory viruses would be associated with structural lung disease on computed tomography (CT) of the chest in infants with CF.
Methods: Infants with CF were enrolled before 4 months of age. Multiplex PCR assays were performed on nasal swabs to detect respiratory viruses during routine visits and when symptomatic. Participants underwent CT imaging at approximately 12 months of age. Associations between Perth-Rotterdam Annotated Grid Morphometric Analysis for CF (PRAGMA-CF) CT scores and respiratory viruses and symptoms were assessed with Spearman correlation coefficients.
Results: Sixty infants were included for analysis. Human rhinovirus was the most common virus detected, on 28% of tested nasal swabs and in 85% of participants. The median (IQR) extent of lung fields that was healthy based on PRAGMA-CF was 98.7 (0.8)%. There were no associations between PRAGMA-CF and age at first virus, or detection of any virus, including rhinovirus, respiratory syncytial virus, or parainfluenza. The extent of airway wall thickening was associated with ever having wheezed (ρ = 0.31, p = 0.02) and number of encounters with cough (ρ = 0.25, p = 0.0495).
Conclusions: Infants with CF had minimal structural lung disease. We did not find an association between respiratory viruses and CT abnormalities. Wheezing and frequency of cough were associated with early structural changes.
Don B Sanders is is Associate Professor in the Department of Pediatrics, Indiana University School of Medicine, Indianapolis, IN, USA.
- A study emphasising the importance of cough as an indication of lower respiratory tract pathology in young children
Atelectasis
1953 di Sant’Agnese PA. Bronchial obstruction with lobar atelectasis and emphysema in cystic fibrosis of pancreas. Pediatrics 1953; 2:178-190. [PubMed]
This paper describes the classical right upper lobe collapse so characteristic of CF and notes bronchoscopy was usually not effective in expanding the collapsed lobe (however, only rigid bronchoscopes were available at that time). Of 211 children with CF 10% presented with collapse of one or more lobes. In the discussion there was still a lingering suggestion that vitamin A deficiency “may contribute but not a major cause”.
Harry Shwachman agreed that atelectasis worsens the prognosis but also noted “The hypothesis suggesting an imbalance of the autonomic nervous system which may affect many systems and organs is attractive”. So there was still no clear explanation for the various manifestations of the condition; some suspected the autonomic nervous system. With regard to the association of the pancreatic lesions and the pulmonary complications, di Sant’Agnese concludes that “a satisfactory understanding of this problem has not yet been attained” which seemed to sum up the situation.
1957 White R Jr, Dent JH, Derbes VJ. Asthmatic states caused by mucoviscidosis. J Louisiana St Med S 1957; 109:299-302.[PubMed]
Thirty eight of 66 children with CF from New Orleans had some degree of wheezing. The authors comment “It has been the common experience of mature pediatricians that administration of epinephrine in such circumstances has led to prompt, albeit transient, alleviation”. The mechanical factors that cause impairment of pulmonary function in asthma – bronchospastic contraction, edema of the mucous membrane and excessive secretion and retention of mucus, are present both in CF and asthma. The authors’ message from their paper being – “it is the responsibility of all physicians who treat wheezing children to exclude this disorder (i.e. cystic fibrosis)”.
Harm A W M Tiddens, Yuxin Chen Eleni-Rosalina Andrinopoulou, Stephanie D Davis, Margaret Rosenfeld, Felix Ratjen, Richard A Kronmal, Karen D Hinckley Stukovsky, Alison Dasiewicz, Stephen Michael Stick, SHIP-CT Study Group Collaborators. The effect of inhaled hypertonic saline on lung structure in children aged 3-6 years with cystic fibrosis (SHIP-CT): a multicentre, randomised, double-blind, controlled trial. Lancet Respir Med 2022 Mar 11;S2213-2600(21)00546-4.doi: 10.1016/S2213-2600(21)00546-4. Online ahead of print [Pubmed]

Harm Tiddens
Background: In the Saline Hypertonic in Preschoolers (SHIP) study, inhaled 7% hypertonic saline improved the lung clearance index in children aged 3-6 years with cystic fibrosis, but it remained unclear whether improvement is also seen in structural lung disease. We aimed to assess the effect of inhaled hypertonic saline on chest CT imaging in children aged 3-6 years with cystic fibrosis.
Methods: Children with cystic fibrosis were enrolled in this multicentre, randomised, double-blind, controlled study at 23 cystic fibrosis centres in Spain, Denmark, the Netherlands, Italy, France, Belgium, the USA, Canada, and Australia. Eligible participants were children aged 3-6 years who were able to cooperate with chest CT imaging and comply with daily nebuliser treatment. Participants were randomly assigned 1:1 to receive inhaled 2 puffs of 100 μg salbutamol followed by 4mL of either 7% hypertonic saline or 0·9% isotonic saline twice per day for 48 weeks. Randomisation was stratified by age in North America and Australia, and by age and country in Europe. Chest CTs were obtained at baseline and 48 weeks and scored using the Perth-Rotterdam Annotated Grid Morphometric Analysis for Cystic Fibrosis (PRAGMA-CF) method. The primary outcome was the difference between groups in the percentage of total lung volume occupied by abnormal airways (PRAGMA-CF %Disease) measured by chest CT at 48 weeks. Analysis was by intention-to-treat. This study is registered withClinicaltrials.gov, NCT02950883.
Findings: Between May 24, 2016, and Dec 18, 2019, 134 children were assessed for inclusion. 18 patients were excluded (nine had incomplete or unsuccessful chest CT at enrolment visit, two could not comply with CT training, two had acute respiratory infection, two withdrew consent, two for reasons unknown, and one was already on hypertonic saline). 116 participants were enrolled and randomly assigned to hypertonic saline (n=56) or isotonic saline (n=60). 12 patients dropped out of the study (seven in the hypertonic saline group and five in the isotonic saline group). Mean PRAGMA-CF %Disease at 48 weeks was 0·88% (95% CI 0·60-1·16) in the hypertonic saline group and 1·55% (1·25-1·84) in the isotonic saline group (mean difference 0·67%, 95% CI 0·26-1·08; p=0·0092) based on a linear regression model adjusted for baseline %Disease values and baseline age. Most adverse events in both groups were rated as mild, and the most common adverse event in both groups was cough.
Interpretation: Inhaled hypertonic saline for 48 weeks had a positive effect on structural lung changes in children aged 3-6 years with cystic fibrosis relative to isotonic saline. This is the first demonstration of an intervention that alters structural lung disease in children aged 3-6 years with cystic fibrosis.
Prof. Harm A W M Tiddens is in the Department of Paediatrics, Division of Respiratory Medicine and Allergology, Sophia Children’s Hospital, Erasmus MC, Rotterdam, Netherlands; Department of Radiology and Nuclear Medicine, Erasmus MC, Rotterdam, Netherlands.
Haemoptysis
1970 Holsclaw DS, Grand RJ, Shwachman H. Massive haemoptysis in cystic fibrosis. Pediatrics 1970; 75:829-838.[PubMed]
First report dealing primarily with 29 episodes of haemoptysis – a serious complication as 13 of the 19 patients died within six months. Treatment was with transfusions and supportive care and surgical resection in one patient (also reported by Lenvitsky S, et al, JAMA 1970; 213:125-127).
Arterial embolisation had not been described as yet and the technique certainly improved the prognosis – for example Stern RC et al, (Am Rev Resp Dis 1977; 117:825) had no deaths in 38 patients although 48% had recurrent episodes. Also a series of 13 patients treated by bronchial artery embolisation was reported from Shwachman’s unit (Fellows KE et al, J Pediatr 1979; 95:959-963 below).
1979 Fellows KE, Kon Taik Khaw, Schuster S, Shwachman H. Bronchial artery embolisation in cystic fibrosis; technique and long term results. J Pediatr 1979; 93:959-963. [PubMed]
This technique was first reported in other diseases (Wholey MH et al, JAMA 1976; 236: 2501) and in two patients with CF in a series of 104 with various conditions (Remy J et al, Radiology 1977; 122:33). In this present series major bleeding ceased in 12 of the 13 patients with CF although five had minor recurrences. The authors advised the procedure should be limited to life-threatening episodes (also Holsclaw DS et al, 1970; Stern et al, 1977 both above)
Flume PA, Yankaskas JR, Ebeling M, Hulsey T, Clark LL. Massive hemoptysis in cystic fibrosis. Chest 2005; 128:729-738.[PubMed]
Massive hemoptysis is a serious complication in CF patients, occurring more commonly in older patients with more advanced lung disease. Nearly 1 in 100 patients will have this complication each year. There is an attributable mortality to the complication and considerable morbidity, resulting in increased health-care utilization and a measurable decline in lung function.
2006 Vidal V. Therasse E. Berthiaume Y. Bommart S. Giroux MF. Oliva VL. Abrahamowicz M. du Berger R. Jeanneret A. Soulez G. Bronchial artery embolization in adults with cystic fibrosis: impact on the clinical course and survival. J Vasc Intervent Radiol 2006; 17:953-958 [PubMed]
Although bronchial artery embolization (BAE) is effective in the acute control of recurrent or major hemoptysis in adults with cystic fibrosis, outcomes after embolization are not well known. Of 297 patients with cystic fibrosis hospitalized from 1990 to 2004, 30 patients (mean age, 26.7+/-9.2 years) presented with major or persistent hemoptysis that required 42 BAE sessions. These patients were compared with a control group of 27 patients without hemoptysis requiring embolization who were matched for age, sex, and forced expiratory volume in 1 second (FEV1). Hemoptysis stopped within 24 hours after BAE in 96.6% of patients (n=29), and there were no major complications. The change in the slope of FEV1 after the BAE or matching date was significantly worse in the embolization group (P=.0007). At last follow-up, nine and one patients, respectively, had undergone lung transplantation in the BAE and control groups (P=.002). The 5-year survival rates without lung transplantation were 31% and 84%, respectively, in the BAE and control groups (hazard ratio, 5.95; P=.002). Sixty-two percent of patients were free of hemoptysis 5 years after BAE. The number of collateral arteries was the only factor associated with the risk of death or recurrent hemoptysis (P=.001). Despite the effectiveness of embolization in controlling recurrent or major hemoptysis, adults with cystic fibrosis who have undergone BAE for hemoptysis are at much higher risk of respiratory function aggravation, death, and the need for lung transplantation than those who have not undergone BAE for hemoptysis. They are more likely to die or to undergo lung transplantation than to present with recurrent major hemoptysis.
– This is useful extensive experience of treating haemoptysis in people with CF. As to be expected the patients with haemoptysis had more severe chest involvement and generally a worse prognosis but the procedure was successful and free of major complications with regard to the controlling the bleeding.
2011 Pestana Knight EM, Novelli PM, Joshi SM. Cerebral and systemic infarcts after bronchial artery embolization. Pediatr Neurol 2011; 45:324-327.[PubMed]
A 17-year-old girl with cystic fibrosis developed hemoptysis and underwent bilateral bronchial artery embolization with 300-500 mum and 500-700 mum microsphere particles. Afterwards, she was delirious and complained of headache, had altered mental status and general hyperreflexia. Her left fifth digit was painful and cyanotic. Neuroimaging demonstrated multiple embolic infarcts in the cerebellum, thalamus, and cerebral hemispheres. She was heterozygous for a prothrombin 20210A mutation. Her functional neurologic recovery was complete.
– This is the first pediatric case of cerebral and systemic embolism after bronchial artery embolization. Although this complication is not predictable, the authors suggest it should be suspected in patients with underlying chronic lung disease who develop acute neurologic signs after bronchial artery embolization, because these patients are prone to anomalous arterial-arterial shunt formation. Bronchial artery embolization with microspheres constitutes an effective, safe procedure for controlling hemoptysis. However, this was an alarming and previously unreported complication of pulmonary artery embolisation treatment of haemoptysis. The more usual occasional complication is embolisation of the spinal arteries with the risk of paralysis.
Megan Sheppard, Hiran Selvadurai, Paul D Robinson, Chetan Pandit, S Murthy Chennapragada, Dominic A Fitzgerald. Approaches to the management of haemoptysis in young people with cystic fibrosis Review Paediatr Respir Rev. 2022 Nov 3;S1526-0542(22)00070-7. doi: 10.1016/j.prrv.2022.10.002. Online ahead of print. pubmed.ncbi.nlm.nih.gov/36463090/
Haemoptysis occurs in up to 25 % of young people with Cystic fibrosis (CF) [1]. We undertook a literature review and described the management approach to haemoptysis in CF between 2010 and 2020 at an Australian tertiary paediatric centre, The Children’s Hospital Westmead, Sydney, New South Wales, using a retrospective review of the medical records which identified 67 episodes. Sixty episodes met inclusion criteria, including 31 patients. Using the US CF Foundation guidelines, episodes were classified as scant (53.3 %), moderate (38.3 %) or massive (8.3 %). Fifty-two percent of patients were female, mean age at presentation was 15.4 years (SD+/- 2.4) and 58 % were homozygous for the Fdel508 genotype. Twelve episodes (9 patients) required bronchial artery embolization (BAE). BAE was used in all cases of massive haemoptysis 5/5 (100 %), 6/23 (22 %) episodes of moderate and 1/32 (3 %) episode of scant haemoptysis as an elective procedure for recurrent haemoptysis. Our literature review and institutional experience highlights the need for up-to-date management guidelines in the management of haemoptysis in Cystic Fibrosis. Based on our experience, we provide a proposed algorithm to help guide the management of haemoptysis in CF.
Megan Sheppard is in the Dept.of Respiratory Medicine, The Children’s Hospital at Westmead, Sydney, NSW 2145, Australia.
OTHER
Gao Z, Wood-Baker R, Harle R, Muller K, Hauser J, Reid DW. “Bong lung” in cystic fibrosis: a case report. J Med Case Rep 2010; 4:371. [PubMed]
Marijuana or “bong” lung has been described recently. Subjects typically develop large peripheral paraseptal lung bullae and are predisposed to spontaneous pneumothoraces. A 23 year old man with CF developed large peripheral paraseptal lung bullae and was predisposed to spontaneous pneumothoraces related to using marijuana. A “Bong” is a water pipe, bubbler or moof filtration device used for smoking cannabis or other inhaled substances. The condition would be worth considering in patients who had problems with recurrent pneumothoraces.
1966 Paxton DG, Scott EP. Pneumothorax: An unusual complication in fibrocystic disease. Am J Dis Child 1966; 111:311-312.[PubMed]
The authors did not find previous reports of pneumothorax in the American literature – only in text books. However, prior to this report there had been sporadic reports of pneumothorax in CF in the literature from 1947 (Fanconi G, Metaxas-Buhler M. Helv Paediat Acta 1947; 2:289-295). Also Doershuk (1964) had one example in 96 patients.
This present report is of sudden onset of left pneumothorax in a 12 year old girl with CF whose chest showed “far advanced changes” at the age of 7.5years (figure 1). With a tube and drainage the lung expanded in 2 days (figure 2); she was discharged in 6 days but died 4 months later from her pulmonary disease.
Pneumothorax is a complication which occurs in those with more advanced chest damage and is now very rare in children with CF. For example in the 2004 UK CF Registry there were no children reported as having pneumothorax and only one in an adult with cystic fibrosis.
2017 Barry PJ, Flume PA*. Bronchodilators in cystic fibrosis: a critical analysis. Expert Rev Resp Med 11(1):13-20, 2017 Jan.[Pubmed]
The use of bronchodilators in CF remains commonplace “despite the lack of solid evidence”. The authors suggest further studies should define key endpoints to determine a role for bronchodilators in light of a substantial treatment burden endured by people with CF.
– It would seem sensible to use N=1 test and, with the patient, judge if they are obtaining benefit. Do we really need a trial for everything?
2017 Cogen JD, Oron AP Gibson RL, Hoffman LR, Kronman MP, Ong T, Rosenfeld M. Characterization of Inpatient Cystic Fibrosis Pulmonary Exacerbations. Pediatrics. 2017 Jan 26. pii: e20162642. doi: 10.1542/peds.2016-2642. [Epub ahead of print] [Pubmed]
This trial was a retrospective cross-sectional study. From 38 hospitals, 4827 individual pulmonary exacerbations were examined. Median length of stay was 10.0 days (interquartile range, 6-14.0 days). Significant variation was seen among centers in the use of hypertonic saline (11%-100%), azithromycin (5%-83%), and systemic corticosteroids (3%-61%) and in the frequency of lung function testing. Four different admission antibiotic regimens were used >10% of the time, and the most commonly used admission antibiotic regimen comprised 2 intravenous antibiotics with no additional oral or inhaled antibiotics (29%). Significant variation exists in the treatment and monitoring of pulmonary exacerbations across Pediatric Health Information System-participating Cystic Fibrosis Foundation-accredited care centers.
– The authors suggest results from this study can inform future research working toward standardised inpatient pulmonary exacerbation management to improve CF care. However, perhaps there is a case for not becoming too rigid in treating individual patients’ exacerbations? However, the great variation in such “add ons” as azithromycin, hypertonic saline and corticosteroids is interesting and would be worth discussing with selected centre directors.
Dr. Jonathan David Cogen specialises in pulmonary and sleep medicine at Seattle Children’s.
2017 Stanojevic S; McDonald A; Waters V; MacDonald S; Horton E; Tullis E; Ratjen F. Effect of pulmonary exacerbations treated with oral antibiotics on clinical outcomes in cystic fibrosis. Thorax. 72(4):327-332, 2017 Apr.[Pubmed]

Sanja Stanojevic
Despite extensive knowledge regarding the effect of pulmonary exacerbations treated with intravenous antibiotics on clinical outcomes in cystic fibrosis (CF), there is little known about the role of milder pulmonary exacerbations treated with oral antibiotics (oPEx). This was a retrospective cohort study of patients with CF followed at the Hospital for Sick Children and St. Michael’s Hospital from 2009 to 2014. The authors evaluated the effect of oPEx on short-term clinical outcomes as the proportion of oPEx events in which 100% or 90% of baseline FEV1% predicted was recovered at the end of treatment. They then examined the association of the number of oPEx events in the past 12 months on lung function (FEV1% predicted) and nutritional status (body mass index (BMI) z-score) using a mixed-effects model.
There were a total of 2608 oPEx events in 570 subjects during the study period. In over half (53.4%) of oPEx events, lung function was already at 90% or higher of baseline FEV1 at the initiation of oral antibiotic therapy and 82% were at 90% or higher of baseline FEV1 at follow-up.
In individuals with CF, one or more oPex events in the previous 12 months were associated with decreased FEV1 compared with 12 months periods without oPex events. When the cumulative effect of oPExs on lung function was examined over the entire study period, patients with six or more oPEx events had the steepest rate of FEV1 decline. oPEx events were not associated with changes in BMI.
The authors concluded pulmonary exacerbations treated with oral antibiotics are associated with short-term loss of FEV1 and have a negative effect on lung function.
Dr Sanja Stanojevic (figure) is a member of the Department of Pediatrics, Hospital for Sick Children, and the Institute of Health Policy, University of Toronto.
2017 Stephen MJ, Long A, Bonsall C, Hoag JB, Shah S, Bisberg D, Holsclaw D, Varlotta L, Fiel S, Du D, Zanni R, Hadjiliadis D. Daily spirometry in an acute exacerbation of adult cystic fibrosis patients. Chron Respir Dis. 2017 Jan 1:1479972317743756. doi: 10.1177/1479972317743756. [Epub ahead of print] [Pubmed]

Twice daily peak flow rates during treatment of a child transferred to our centre with severe exacerbation of her chest infection
To help answer the question of length of intravenous antibiotics during an acute exacerbation of cystic fibrosis (CF), we had subjects to follow daily home spirometry while on intravenous antibiotics. CF patients, 18 and older, with an acute exacerbation requiring intravenous antibiotics had a daily FEV1. The average time to a 10% increase over their initial sick FEV1 was calculated, as well as the time to a new baseline. A total of 25 subjects completed the study. Ten of the 25 subjects did not have a sustainable 10% increase in FEV1. Of the 15 subjects with a sustainable 10% increase in FEV1, it took 5.2 days (±4.5) after day 1, while a new baseline was achieved on average at 6.6 days (±4.8) after day 1. Given the wide range of time to a 10% improvement and new baseline, it is recommended there should be flexibility in length of intravenous antibiotics in CF, not by a pre-set number.
– This seems to be a helpful approach as, for a variety of reasons, patients differ in their response to antibiotic treatment. For many years in the Leeds Regional CF Centre we recorded the twice-daily Peak Expiratory Flow rates of children undergoing a course of IV antibiotic treatment (figure 54) ; this was continued until the values plateaued. Failure to improve each day would prompt a search for the reason/s. The twice-daily PFRs would usually be measured before and after a bronchodilator to note the usual reduction in bronchial lability that occurs during effective treatment.
2016 Kopp BT; Ortega-Garcia JA; Sadreameli SC; Wellmerling J; Cormet-Boyaka E; Thompson R; McGrath-Morrow S; Groner JA. The Impact of Secondhand Smoke Exposure on Children with Cystic Fibrosis: A Review. Int J Environ Res Public Health [Electronic Resource]. 13(10), 2016 Oct 12. [Pubmed

Benjamin Kopp
This review examines what is known regarding the prevalence of SHSe (second hand smoke exposure) in CF, with the majority of reviewed studies utilizing parental-reporting of SHSe without an objective biomarker of exposure. A wide range of SHSe is reported in children with CF, but under-reporting is common in studies involving both reported and measured SHSe. Additionally, the impact of SHSe on respiratory and nutritional health is discussed, with potential decreases in long-term lung function, linear growth, and weight gain noted in CF children with SHSe. Immunologic function in children with CF and SHSe remains unknown. The impact of SHSe on cystic fibrosis transmembrane conductance regulator (CFTR) function is also examined, as reduced CFTR function may be a pathophysiologic consequence of SHSe in CF and could modulate therapeutic interventions.
– This is a very interesting and extensively referenced review of the effects of second hand smoke exposure in people with CF. The full article is available via PubMed.
Benjamin T Kopp (figure) is Assistant Professor of Pediatrics at the Ohio State University College of Medicine.
Arooj P, Plant R, Doddakula K, Plant BJ. Inhaler screw-up: A real world cystic fibrosis (CF) case. Pediatr Pulmonol. 2018 Sep 18. doi: 10.1002/ppul.24158. [Epub ahead of print] [Pubmed]

Parniya Arooj
A 40-year-old male with Cystic Fibrosis developed a sudden onset choking, cough, dyspnea and hemoptysis after using his inhaler. He presented to A&E. CT scan located a foreign body in his right bronchus intermedius (RBI). Rigid bronchoscopy was performed and removed a plastic raw plug with screw from his RBI. He made a rapid recovery. On questioning he mentioned he had stored his inhaler uncapped in the same pocket he had this screw that he found at work.
The authors note that small objects can lodge in inhalers due to their design/mouthpiece uncapping. This can result in endobronchial foreign body aspiration. This case highlights the importance of replacing inhaler cap when not in use.
Dr. Parniya Arooj is a member of the Department of Respiratory Medicine, Cork University Hospital, Ireland
Sivam S, Dentice R, Reddy N, Moriarty C, Yozghatlian V, Mellis C, Torzillo P, Glanville A, Gattas D, Bye P. Use of extracorporeal membrane oxygenation in cystic fibrosis in an Australian cystic fibrosiscentre. Intern Med J. 2018 Mar;48(3):340-343. doi: 10.1111/imj.13728. 29612325 ??
Extracorporeal membrane oxygenation (ECMO) support is used in selected patients with cystic fibrosis (CF) as a bridge to transplantation. Our aim was to describe briefly treatment and outcomes of six CF patients who received ECMO. One patient received a lung transplant and another recovered from acute respiratory failure. Four died despite ECMO support. Lack of timely availability of suitable donor lungs and patient selection are contributing factors.
Carzino R, Frayman KB, King L, Vidmar S, Ranganathan S; AREST CF. Regional differences in infection and structural lung disease in infants and young children with cystic fibrosis. J Cyst Fibros. 2019 Nov 6. pii: S1569-1993(19)30933-6. doi: 10.1016/j.jcf.2019.10.018. [Epub ahead of print]. [Pubmed]

Rosemary Carzino
Both infection and inflammation are critical to the progression of cystic fibrosis (CF) lung disease. Potential anatomical differences in lower airway infection, inflammation and bronchiectasis in young children with CF raise questions regarding the pathogenesis of early structural lung disease.
A longitudinal multi-centre birth cohort study of infants newly diagnosed with CF was conducted. Paired bronchoalveolar lavage (BAL) samples were obtained from the right middle lobe (RML) and lingula bronchi. Chest computed tomography (CT) was performed biennially and analysed using the modified CF-CT scoring system.
One hundred and twenty-four children (0.11 – 7.0 years) contributed 527 BAL samples and underwent 388 CT chest scans. Pro-inflammatory microbes were detected in 279 BAL samples (53%), either in both lingula and RML samples (69%), in the lingula alone (24%), or in the RML alone in only 7% of samples. Overall, the prevalence of structural lung disease was greater in the setting of pro-inflammatory microbes. Although infection was less commonly isolated in the right lung, bronchiectasis was more commonly detected in the right lung compared with the left. No anatomical differences in the presence of air trapping were detected.
The authors concluded overall, the detection of pro-inflammatory microbes in the lower airways was associated with increased risk of both air trapping and bronchiectasis. However, the apparent discordance between commonest sites of isolation of pro-inflammatory microbes and the anatomical site of early bronchiectasis warrants further exploration.
Dr Rosemary Carzino is a Senior Research Assistant in the Respiratory Diseases Group, Murdoch Children’s Research Institute, Victoria, Australia
Cohen RWF, Folescu TW, Boechat MCB, Fonseca VM, Marques EA, Leão RS. High-resolution computed tomography findings in young infants with cystic fibrosis detected by newborn screening. Clinics (Sao Paulo). 2019 Oct 21;74:e1399. doi: 10.6061/clinics/2019/e1399. eCollection 2019.Free full text [Pubmed]
High-resolution computed tomography (HRCT) allows the early detection of pathological changes in the lung structure, and reproducible scoring systems can be used to quantify chest computed tomography (CT) findings in patients with cystic fibrosis (CF). The aim of the study was to describe early HRCT findings according to a validated scoring system in infants with CF diagnosed by newborn screening (NBS).
This cross-sectional study included infants with CF diagnosed by NBS who were born between January 2013 and January 2017 and who underwent HRCT scanning within the first year after diagnosis when they were clinically stable. The CT scans were evaluated using the modified Bhalla score.
Thirty-two subjects underwent HRCT scanning. The mean total-modified Bhalla score was 3.6±2.1, and 93.8% of the scans were abnormal. Pseudomonas aeruginosa airway colonization was associated with increased modified Bhalla score values. Bronchial wall thickening was the most common feature (90.6%), followed by bronchial collapse/consolidation (59.4%), mosaic attenuation/perfusion (50%), bronchiectasis (37.5%) and mucus plugging (15.6%). Bronchial wall thickening was diffuse in most of the patients.
Conclusion: A substantial proportion of infants diagnosed with CF after detection by NBS already showed evidence of lung disease. P. aeruginosa colonization was associated with increased Bhalla scores, highlighting the importance of this CF pathogen in early structural lung disease. The presence of bronchial wall thickening at such a young age may reflect the presence of airway inflammatory processes. The detection and quantification of structural abnormalities with the modified Bhalla score may aid in the identification of lung disease before it is clinically apparent.
Dr Renata Wrobel Folescu Cohen is in the Faculdade de Ciencias Medicas, Universidade do Estado do Rio de Janeiro, Rio de Janeiro, RJ, BR.
Mordechai Pollak, Michelle Shaw, David Wilson, Melinda Solomon, Felix Ratjen, Hartmut Grasemann. Bronchodilator responsiveness in cystic fibrosis children treated for pulmonary exacerbations. Pediatr Pulmonol 2021 Apr 8.doi: 10.1002/ppul.25409. Online ahead of print.[Pubmed]
Background: Cystic fibrosis (CF) pulmonary exacerbations (PEx) are associated with a significant drop in pulmonary function. The clinical value of measuring bronchodilator (BD) responsiveness during treatment for PEx to monitor or predict recovery of lung function is unclear.
Methods: A retrospective analysis of spirometry with BD response testing obtained during hospital admissions for PEx in pediatric CF patients. Repeated events were included for patients with BD testing during multiple admissions.
Results: Two hundred forty-nine spirometries with BD testing in 102 patients were completed around Day 7 (Days 4-10) of hospital admission for treatment of CF PEx. Median (IQR) forced expiratory volume in 1 s (FEV1 ) was 70.6% predicted (58.1, 84.6) before the PEx event (best FEV1in 6 months before admission), 54.4% (41.5, 66.9) at admission, 62.3% (48.4, 74.7) around Day 7 of admission and 67.1% predicted (53.8, 78.2) at the end of treatment. BD response around Day 7 correlated poorly with FEV1 before PEx (r = -.16, p = .02) and did not correlate with recovery to baseline FEV1 at end of treatment (r = .08, p = .22). Only 23/249 (9%) individual tests had a BD response in FEV1 of ≥12% and 200 ml. BD response was not related to age or severity of lung disease and led to an immediate change in clinical management in only four cases.
Conclusions: Significant BD response in CF patients treated for PEx is rare, shows poor correlation with baseline pulmonary function and does not correlate with the recovery of FEV1 with treatment. These data suggest that routine testing for BD response is not indicated during PEx.
Dr Mordechai Pollak is in the Division of Respiratory Medicine, Department of Paediatrics, Hospital for Sick Children, Toronto, Ontario, Canada.
Kubra M Bozkanat, Natalie E West, Sigrid Ladores, Kristina Montemayor, Maria Gabriela Tupayachi Ortiz, Mindy Christianson, Raksha Jain Catamenial haemoptysis in females with cystic fibrosis: a case series with review of management strategies. Respirol Case Rep 2021 May 7;9(6):e00755.doi: 10.1002/rcr2.755.eCollection 2021 Jun. [Pubmed]
Catamenial haemoptysis, the expectoration of blood during menses, has not been extensively reported in the cystic fibrosis (CF) literature. We describe four cases (age range: 25-34 years) of catamenial haemoptysis across four CF centres in the United States. These cases may represent thoracic endometriosis versus hormonal fluctuations in airway inflammation or infection resulting in bronchial artery bleeding. We identify common and nuanced management strategies including use of pro-coagulants, hormone contraceptives, anti-inflammatories, bronchial artery embolization, and use of the newer cystic fibrosis transmembrane conductance regulator (CFTR) modulators.
Dr Kubra M Bozkanat, is a paediatrician in the Department of Pediatrics University of Texas, Southwestern Medical Center, Dallas TX USA.
Dominic A Hughes, Olga Archangelidi, Matthew Coates, Darius Armstrong-James, Stuart J Elborn, Siobhán B Carr, Jane C Davies. Clinical characteristics of Pseudomonas and Aspergillus co-infected cystic fibrosis patients: A UK registry study. J Cyst Fibros 2021 May 3;S1569-1993(21)00117-X.doi: 10.1016/j.jcf.2021.04.007.Online ahead of print. [Pubmed]

Dominic Hughes
Background: Pseudomonas aeruginosa (Pa) and Aspergillus species (Asp) are the most common bacterial and fungal organisms respectively in CF airways. Our aim was to examine impacts of Asp infection and Pa/Asp co-infection using the UK CF Registry.Full details on PubMed.
Conclusions: Co-infection with Pa and Asp was not associated with reduced lung function compared with Pa alone, but was associated with additional use of IV antibiotics. Asp infection itself is associated with several important indicators of disease severity. Longitudinal analyses should explore the impact of co-infection on disease progression.
Dr Dominic A Hughes is a researcher at the National Heart & Lung Institute, Imperial College London, UK; Royal Brompton and Harefield Hospitals, London, UK
Giulia Spoletini, Kim Pollard , Ruth Watson, Michael J Darby, Annette Johnstone, Christine Etherington, Paul Whitaker, Ian J Clifton, Daniel G Peckham. Noninvasive Ventilation in Cystic Fibrosis: Clinical Indications and Outcomes in a Large UK Adult Cystic Fibrosis Center. Respir Care 2021 Mar;66(3):466-474.doi: 10.4187/respcare.07862. Epub 2020 Sep 8. [Pubmed]

Giulia Spoletini
Background: Noninvasive ventilation (NIV) is routinely used to treat patients with cystic fibrosis and respiratory failure. However, evidence on its use is limited, with no data on its role in disease progression and outcomes. The aim of this study was to assess the indications of NIV use and to describe the outcomes associated with NIV in adults with cystic fibrosis in a large adult tertiary center.
Methods: A retrospective analysis of data captured prospectively on the unit electronic patient records was performed. All patients with cystic fibrosis who received NIV over a 10-y period were included in the study. A priori, 2 groups were identified based on length of follow-up, with 2 subgroups identified based on duration of NIV treatment.
Results: NIV was initiated on 64 occasions. The duration of follow-up was categorized as > 6 months or < 6 months in 31 (48.4%) and 33 (51.6%) occasions, respectively. The most common indications for starting NIV were chronic (48.5%) and acute (32.8%) hypercapnic respiratory failure. Among those with a follow-up > 6 months, subjects who stopped using NIV early showed a steady median (interquartile range) decline in FEV1 (pre-NIV: -0.04 [-0.35 to 0.03] L/y vs post-NIV: -0.07 [-0.35 to 0.01] L/y, P = .51), while among those who continued using it had an improvement in the rate of decline (pre-NIV: -0.25 [-0.52 to -0.02] L/y vs post-NIV: -0.07 [-0.13 to 0.16] L/y, P = .006). No differences in intravenous antibiotic requirement or pulmonary exacerbations were noted with the use of NIV. Pneumothorax and massive hemoptysis occurred independently in 4 cases.
Conclusions: NIV is being used in cystic fibrosis as adjunct therapy for the management of advanced lung disease in a similar fashion to other chronic respiratory conditions. Adherence to NIV treatment can stabilize lung function but does not reduce pulmonary exacerbations or intravenous antibiotic requirement.
Dr Giulia Spoletini Consultant in Respiratory and Adult CF Medicine at the Leeds Regional Adult Cystic Fibrosis Centre, St James’s University Hospital, Leeds Teaching Hospital NHS Trust and the Leeds Institute of Medical Research, University of Leeds, Leeds, UK.
Christina M Mingora, Patrick A Flume. Pulmonary Complications in Cystic Fibrosis: past, present and future. Chest 2021 Jun 17;S0012-3692(21)01127-2.doi:0.1016/j.chest.2021.06.017.Online ahead of print. [Pubmed]

Christina MIngora
Cystic Fibrosis (CF) is an autosomal recessive genetic condition with multi-systemic disease manifestations, the most prominent of which occur in the respiratory system. Despite significant developments in disease understanding and therapeutics, each contributing to improved lung function and survival in persons with CF, several pulmonary complications including pneumothorax, massive hemoptysis, and respiratory failure continue to occur. In this review, we briefly describe each of these complications and their management, as well as discuss how they impact the care and disease trajectory of individuals in whom they occur. Finally, we discuss the evolving role that palliative care and cystic fibrosis transmembrane conductance regular modulator therapies play in the natural disease course and care of persons with CF.
Dr Christina M Mingora is at the Medical University of South Carolina, Charleston, SC.
– This is a clear account of the chest problems which remain a major factor affecting the lives of the majority of people with C
Sara W Carson, Kevin Psoter, Kirsten Koehler, Karen R Siklosi, Kristina Montemayor, Alexandra Toporek, Natalie E West, Noah Lechtzin, Nadia N Hansel, Joseph M Collaco, Christian A Merlo Indoor air pollution exposure is associated with greater morbidity in cystic fibrosis. J Cyst Fibros 2021 Sep 13;S1569-1993(21)01356-4.doi: 10.1016/j.jcf.2021.08.015.Online ahead of print [Pubmed]

Sara W Carson
Background: Exposure to higher levels of outdoor air pollution is associated with increased morbidity in individuals with cystic fibrosis. Limited information exist regarding the potential adverse effects of indoor air pollution on those with cystic fibrosi
Results: Of 1432 participants with data on secondhand smoke exposure, 362 (25.3%) were exposed. Of 765 individuals with data on forced hot air exposure, 491 (64.2%) were exposed. Of 1247 participants with data on wood stove exposure and 830 with data on fireplace exposure, 182 (14.6%) and 373 (44.9%) were exposed, respectively. In longitudinal analysis, pediatric individuals either exposed to secondhand smoke or to forced hot air had a 0.60% predicted/year decrease in FEV1% predicted (P=0.002) or a 0.46% predicted/year decrease in FEV1% predicted (P=0.048), respectively compared to individuals who were not exposed. Adults exposed to secondhand smoke had a 42% increased yearly risk of hospitalization compared to those who were not exposed (P=0.045).
Conclusions: Our questionnaire-based data suggest that exposure to sources of indoor air pollution increase morbidity in both the pediatric and adult cystic fibrosis populations. Future studies with quantitative indoor air quality assessments are needed.
Dr Sara W Carson is a Pulmonary and Critical Care Fellow at the Department of Medicine, Division of Pulmonary and Critical Care Medicine, Johns Hopkins University, Baltimore, USA.
Aesha Jobanputra, Sugeet Jagpal, Paula Marulanda, Maya Ramagopal, Teodoro Santiago, Sreelatha Naik . An overview of non-invasive ventilation in cystic fibrosis. Pediatr Pulmonol 2021 Nov 9.doi: 10.1002/ppul.25753. Online ahead of print. [Pubmed]

Aesha Jobanputra
Noninvasive ventilation (NIV) use was initially reported in cystic fibrosis (CF) in 1991 as a bridge to lung transplantation, and over the decades, the use of NIV has increased in the CF population. Individuals with CF are prone to various physiologic changes as lung function worsens, and they benefit from NIV for advanced lung disease. As life expectancy in CF has been increasing due to advances such as highly effective modulator therapy, people with CF may also benefit from NIV for other diagnosis beyond advanced lung disease. NIV can improve gas exchange, quality of sleep, exercise tolerance, and augment airway clearance in CF. CF providers can readily become comfortable with this therapeutic modality.In this review, we will summarize the physiologic basis for NIV use in CF, describe indications for initiation, and discuss how to order and monitor patients on NIV. We will discuss aspects unique to people with CF and the use of NIV, as well as suggestions on how to reduce risks such as infection. We hope that this serves as a resource for CF providers, in particular those who do not have dedicated training in sleep medicine as we all continue to care for the CF patient population.
Dr Aesha Jobanputra is Assistant Professor of Medicine in the Division of Pulmonary, Critical Care and Sleep Medicine, Rutgers the State University of New Jersey, New Brunswick, New Jersey, USA.
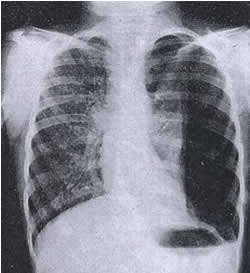
Fig. 1: Massive left sided pneumothorax.

Fig. 2: Air resolved in 2 days with tube and drainage.
2006 Hafen GM. Ukoumunne OC. Robinson PJ. Pneumothorax in cystic fibrosis: a retrospective case series. Arch Dis Child 2006; 91:924-925.[PubMed]
Pneumothorax is a known complication in cystic fibrosis (CF), associated with poor outcome. Records of CF patients with pneumothorax at the Royal Children’s Hospital, Melbourne between 1990 and 2004 were reviewed, and the characteristics, sputum culture results, lung function, treatment, and outcome for the 11 patients who had pneumothoraces were described.
– Although a small series, this is a useful report as pneumothorax is now rare in children with CF.
2010 MacDuff A, Tweedie J, McIntosh L, Innes JA. Pneumothorax in cystic fibrosis: prevalence and outcomes in Scotland. J Cyst Fibros 2010; 9:246-249.
A total of 22 episodes of pneumothorax occurred in 20 patients in 3 Scottish CF centres over a 12 year period. 2 patients died as a result of the pneumothorax. 16 pneumothoraces were treated by insertion of an intercostal drain and 8 by observation. 8 patients suffered a prolonged air leak. 5 patients were treated with pleurodesis. Pneumothorax was associated with a small decline in lung function which persisted for at least 1year. Pneumothorax can present a challenge to treat in adult CF. However successful outcomes can be achieved even in cases of prolonged air leaks. Current national guidelines help in selecting optimal pleural interventions.
– A recent account of experience with pneumothoraces is welcome and as the adult population increases in relation to children, it is likely that the increase in this complication will continue. Pneumothorax is now very rare in the children with CF as evidenced by virtually no instances in children recorded in the recent UK Annual Patient Registry reports.
2010 Gao Z, Wood-Baker R, Harle R, Muller K, Hauser J, Reid DW. “Bong lung” in cystic fibrosis: a case report. J Med Case Rep 2010; 4:371. [PubMed]
Marijuana or “bong” lung has been described recently. Subjects typically develop large peripheral paraseptal lung bullae and are predisposed to spontaneous pneumothoraces. A 23 year old man with CF developed large peripheral paraseptal lung bullae and was predisposed to spontaneous pneumothoraces related to using marijuana.
– A “Bong” is a water pipe, bubbler or moof filtration device used for smoking cannabis or other inhaled substances. The condition would be worth considering in patients who had problems with recurrent pneumothoraces
ASSISTED VENTILATION
2001 Sood N. Paradowski LJ. Yankaskas JR. Outcomes of intensive care unit care in adults with cystic fibrosis. Am J Resp Crit Care 2001; 163:335-338. [PubMed] Mechanical ventilation has been discouraged in CF because of poor outcomes, but improved survival and the availability of lung transplantation have increased the indications for care of CF patients in the intensive care unit (ICU). We studied the outcomes of all CF patients admitted to the University of North Carolina Hospitals Medical ICU from January 1990 through December 1998. Seventy-six patients, ranging in ages from 17 to 45 yr (mean: 27 yr), and of whom 53% were female, had 136 admissions for exacerbations of CF with respiratory failure (RF, n = 65), hemoptysis (n = 33), antibiotic desensitization (n = 30), pneumothorax (n = 3), or other reasons (n = 5). Eighty-six percent of the patients with hemoptysis and all of those with desensitization and pneumothorax were alive 1 yr after ICU discharge. Of the 42 patients with RF, 37 (88%) required assisted ventilation. Twenty-three (55%) of the patients with RF survived to ICU discharge and 19 (45%) died. Seventeen (40%) of the patients with RF received lung transplants and 14 were alive 1 yr later. Without transplantation, three (7%) of the patients with RF were alive and three (7%) were dead 1 yr later. Sex, body mass index, and respiratory bacteria did not correlate with survival. We conclude that ICU care for adults with CF who have reversible complications is appropriate and effective. Ventilatory support is appropriate for some transplant candidates.
– This is a useful indication of the fate of people with CF admitted to an ICU in a major CF Centre at the present time. Undoubtedly the policy of not admitting to an ICU or ventilating people with CF in no longer valid.
2006 Slieker MG. van Gestel JP. Heijerman HG. Tramper-Stranders GA. van Berkhout FT. van der Ent CK. Jansen NJ. Outcome of assisted ventilation for acute respiratory failure in cystic fibrosis. Intens Care Med 2006; 32:754-758. [PubMed]
To assess outcome of assisted ventilation in cystic fibrosis (CF) patients with acute respiratory failure (ARF), to identify risk factors associated with poor outcome and to compare long-term outcome of CF children who were mechanically ventilated for ARF with unventilated CF controls. A retrospective cohort study in two large CF centres in the Netherlands. Thirty-one CF patients required assisted ventilation for ARF between January 1990 and March 2005. All five children (under 2 years of age) and seven adults (27%) survived. CF patients younger than 2 years old, who are ventilated because of ARF, have a good prognosis and their long-term outcome seems identical to unventilated CF controls. ARF in adult CF patients still is associated with high mortality, especially among patients with acute on chronic respiratory failure.
– The resort to assisted ventilation has changed over the years now there is the possibility of transplantation; prior to the mid-Eighties, before the first successful transplantations, ventilation was usually regarded as inappropriate.
2009 McDermott S. Barry SC. Judge EE. Collins S. de Jong PA. Tiddens HA. McKone EF. Gallagher CC. Dodd JD. Tracheomalacia in adults with cystic fibrosis: determination of prevalence and severity with dynamic cine CT. Radiology 2009; 252:577- 586. [PubMed] To determine the prevalence and severity of tracheomalacia in adults with cystic fibrosis (CF) by using dynamic cine multidetector computed tomography (CT) and to correlate these findings with pulmonary function test (PFT) results and the severity of parenchymal lung disease. Tracheomalacia was demonstrated in 24 (69%) patients and no control subjects during forced expiratory maneuvers (P = .001) and in 10 (29%) patients and one (10%) control subject during coughing. There was no correlation between tracheal cross-sectional luminal reduction and either predicted FEV(1) or CT Bhalla score. Tracheomalacia depicted at dynamic cine multidetector CT is a highly prevalent finding in adults with CF.
– Clinically tracheomalacia has been observed on occasion but the present study demonstrates how common is the condition. It is interesting that similar tracheal abnormalites occur commonly in CF pigs in particular some degree of maldevelopment of the tracheal cartilage.
2011 George PM, Banya W, Pareek N, Bilton D, Cullinan P, Hodson ME, Simmonds NJ. Improved survival at low lung function in cystic fibrosis: cohort study from 1990 to 2007. BMJ 2011; 342:d1008. [PubMed]
To evaluate the survival of patients with cystic fibrosis whose lung function has deteriorated to a forced expiratory volume in one second (FEV(1)) below 30% predicted in the recent treatment era and to explore factors associated with any change in survival. 276 patients (147 (53%) male) attending the Brompton whose FEV(1) was first observed to be less than 30% predicted between 1 January 1990 and 31 December 2003. The median survival improved from 1.2 years in the 1990-1 group to 5.3 years in the 2002-3 group, with a marked improvement in survival from 1994. The use of nebulised recombinant human DNase was significantly associated with a reduced risk of death (hazard ratio 0.59, 95% confidence interval 0.44 to 0.79). Significantly increased risks were associated with a body mass index under 19 (hazard ratio 1.52, 1.10 to 2.10), long term oxygen therapy (3.52, 2.49 to 4.99), and nebulised antibiotics (1.84, 1.05 to 3.22). The authors concluded that a marked improvement has occurred in the survival of patients with cystic fibrosis with an FEV(1) less than 30% predicted. Secondary analyses suggest that some of this improvement may be due to use of recombinant human DNase.
– This is encouraging data from the UKs major adult CF centre showing a much improved survival for these severely affected patients, presumably related to improved treatment. For some years a survival;- in this study the authors suggest that the use of DNase may be a significant factor.
2013 Jones A. Bilton D. Evans TW. Finney SJ. Predictors of outcome in patients with cystic fibrosis requiring endotracheal intubation. Respirology 2013; 18:630-636. [PubMed]
Acute severe clinical deterioration of patients with cystic fibrosis (CF) may mandate endotracheal intubation. The benefits of intubation were evaluated by examining which pre-admission parameters were associated with intensive care unit (ICU) outcome and assessing the potential benefits of intubation for survivors in terms of time from ICU discharge to death. Thirty patients required intubation on 34 occasions (8 per 1000 admissions). Eleven patients died in ICU and 7 after ICU but not hospital discharge. Fifty-nine per cent of 22 patients intubated for pneumothorax and/or haemoptysis survived to hospital discharge. Of the twelve intubated for infective exacerbations, 33% survived to hospital discharge. Those who died after hospital discharge survived 447 days. There were no significant differences for survivors in reasons for intubation, colonizing organism, frequency of infective exacerbations, severity of illness or pulmonary physiology. Osteoporosis and a greater fall in body mass index over the 24 months prior were more frequent in non-survivors.
– Experience at the Royal Brompton Hospital indicated patients with CF developing haemoptysis and/or pneumothorax should be admitted to ICU and intubated promptly, should this be required. Chronic disease markers may be more relevant prognostically than rates of hospitalization or forced expiratory volume in 1s decline which should not be bars to invasive ventilation.
2014 Fischer AJ. Singh SB. Adam RJ. Stoltz DA. Baranano CF. Kao S. Weinberger MM. McCray PB Jr. Starner TD. Tracheomalacia is associated with lower FEV1 and Pseudomonas acquisition in children with CF. Pediatr Pulmonol 2014; 49:960-70.[PubMed]
Tracheomalacia (TM) occurs in approximately 1 in 2,100 children. Because the trachea develops abnormally in animal models of cystic fibrosis (CF), the authors examined the prevalence and clinical consequences of TM in children with CF. TM was defined as dynamic collapse of the trachea, and the severity was recorded.
Eighty-nine percent of children with CF had at least one bronchoscopy (n=97/109). Fifteen percent of these children had TM described in any bronchoscopy report (n=15/97 16%), eight of these had meconium ileus (P=0.003) and all were pancreatic insufficient. Pseudomonas aeruginosa infection occurred 1.3 years earlier among children with TM (P=0.01). Life-threatening episodes of airway obstruction occurred in 3 of 15 patients with CF and TM, including one leading to death.
– So tracheomalacia is significantly more common in infants and children with CF than in the general population and is associated with airway obstruction and earlier Pseudomonas acquisition.
Intractable expiratory wheeze poorly responsive to treatment related to tracheomalacia is a major problem in occasional CF infants. The findings of abnormal tracheal development, analogous to that recently described in CF animals, is obviously an explanation. Such infants may present a really difficult management problem.
2014 Sheikh SI. McCoy KS. Ryan-Wenger NA. Patel A. Kirkby S. Lobectomy in patients with cystic fibrosis. Can Respir J 2014; 21:e63-6. [PubMed]
Some patients with cystic fibrosis develop severe but localized lung disease or recurrent hemoptysis/pneumothorax refractory to conventional medical therapies. The outcomes of lung resection in patients with CF and worsening localized lung disease or recurrent hemoptysis/pneumothorax refractory to conventional therapy (n=15) were evaluated by reviewing the medical records of all patients with CF followed at the CF Center at Nationwide Children’s Hospital (Columbus, Ohio, USA), who underwent lobectomy over a 15-year period (1998 to 2012).
The median age of the 15 patients (93% Caucasian) was 20 years (range two to 41 years) and their mean forced expiratory volume in 1 s (FEV1) was 59.5% of predicted one year before surgery. Three patients died within two years after lobectomy; all three deaths occurred in patients with an FEV1 <40% of predicted before surgery. There were no significant changes in mean height, weight, body mass index, hospital admissions or antibiotic use over time. The mean FEV1 decreased over time. Compared with at surgery, decline in FEV1 in the year before surgery was -5.4% (P=0.024) and decline in the year after surgery was -1.3% (P=0.513); however, the difference in the rate of decline was not statistically significant. The authors concluded that in patients with CF and localised worsening bronchiectasis and/or recurrent hemoptysis/pneumothorax, lobectomy carried a significant risk of mortality, especially in patients with FEV1 <40% of predicted, and should only be considered when all other measures fail. – This experience in older patients differs significantly from the relatively good results for lobectomy for localised severe changes in children reported by many previous authors (see Topics -> Surgery for details of previous publications). It is not surprising that when there is extensive lung involvement in older patients lobectomy will be less beneficial as was the case in the present study.
McDermott S, Barry SC, Judge EP, Collins S, de Jong PA, Tiddens HA, McKone EF, G, Dodd JD. Tracheomalacia in adults with cystic fibrosis: determination of prevalence and severity with dynamic cine CT. Radiology. 2009; 252(2):577-86. doi: 10.1148/radiol. 25220819 56. Epub 2009 Jun 9. [PubMed]
To determine the prevalence and severity of tracheomalacia in adults with cystic fibrosis using dynamic cine multi-detector computed tomography (CT) and to correlate these findings with pulmonary function test (PFT) results and the severity of parenchymal lung disease.
Mean predicted forced expiratory volume in 1 second (FEV(1)) was 70.6% +/- 20.7, and mean Bhalla CT score was 41.8% +/- 13.6. In patients with CF, dynamic cine mean tracheal cross-sectional area reduction was 51.7% +/- 18.4 (range, 9%-89%) for forced expiratory manoeuvres and 68.8% +/- 11.7 (range, 18%-88%) for coughing (P = .001). Tracheomalacia was demonstrated in 24 (69%) patients and no control subjects during forced expiratory manoeuvres (P = .001) and in 10 (29%) patients and one (10%) control subject during coughing. For end-expiration images, mean tracheal luminal reduction was 16.1% +/- 14.0% (range, 0.0%-53.0%), with one patient demonstrating tracheal luminal reduction of more than 50%. There was no correlation between tracheal cross-sectional luminal reduction and either predicted FEV(1) or CT Bhalla score.
Tracheomalacia depicted at dynamic cine multidetector CT is a highly prevalent finding in adults with CF.
– The tendency to tracheomalacia in people with CF is well documented and at times clinically evident as a tendency to severe expiratory wheeze (Fischer AJ et al, 2014 [PubMed]). Similar tracheal abnormalities have been documented in animal CF models (Adam RJ et al. 2013.[PubMed])
2015 Diwakar A, Adam RJ, Michalski AS, Tamegnon MM, Fischer AJ, Launspach JL, Horan RA, Kao SC, Chaloner K, Meyerholz DK, Stoltz DA,. Sonographic evidence of abnormal tracheal cartilage ring structure in cystic fibrosis. Laryngoscope. 2015 Oct;125(10):2398-404. doi: 10.1002/lary.25255. Epub 2015 Mar 30. [PubMed]
Tracheal cartilage ring structural abnormalities have been reported in CF mice and pigs. Whether similar findings are present in humans with CF is unknown.
Tracheal cartilage ring size and shape were measured in adults with (n = 21) and without CF (n = 18).
Ultrasonography was used in human subjects to noninvasively assess tracheal cartilage ring structure in both the sagittal and the transverse planes. Tracheal cartilage ring thickness was also determined from histological sections obtained from newborn non-CF and CF pigs. These values were compared with human data.
Human CF tracheas had a greater width and were less circular in shape compared to non-CF subjects. CF tracheal cartilage rings had a greater midline cross-sectional area and were thicker compared to non-CF rings. Maximal tracheal cartilage ring thickness was also greater in both newborn CF pigs and human adults with CF, compared to non-CF controls.
The authors’ findings demonstrate that structural differences exist in tracheal cartilage rings in adults with CF. Comparison with newborn CF pig data suggests that some of these changes may be congenital in nature
2016 Liew Z, Mallikarjuna S, Hasan A, Gould FK, Bunn S, Thomas MF, Lordan JL, O’Brien C, Brodlie M. Successful outcome following pneumonectomy in a teenage boy with cystic fibrosis: a case report. BMC Pulm Med. 2017 Jan 13;17(1):17. doi: 10.1186/s12890-016-0350-x. Free PMC article [PubMed]
Lung resection surgery is seldom indicated in cystic fibrosis and the associated medical literature is relatively sparse. A 14 year old boy was referred for lung transplantation assessment. He had a chronic history of complete collapse and consolidation of his entire right lung. This was causing severe morbidity in terms of a continuous requirement for intravenous antibiotics over the last year, poor exercise tolerance with forced expiratory volume in 1 s of 35-40% predicted and need for home tuition. He also had significant nutritional problems and gastrointestinal symptoms following a Nissen’s fundoplication operation a year earlier.
His nutritional status was firstly improved by the institution of jejunal feeding, which also greatly improved his distressing symptoms of nausea and wretching. After thorough multidisciplinary assessment the therapeutic option of performing a right pneumonectomy was considered due to relative sparing of the left lung, which demonstrated only mild bronchiectasis on computed tomography scan. This was performed uneventfully with a smooth peri-operative course. Targeted antimicrobials were used to treat the multiresistant organisms colonising his airways. Subsequently his quality of life, nutritional status and lung function all improved significantly and requirement for lung transplantation has been delayed. A successful outcome following pneumonectomy in a teenage boy with cystic fibrosis referred for lung transplantation assessment with chronic unilateral collapse and consolidation of his right lung. Pneumonectomy can be a feasible option in this clinical situation in cystic fibrosis but the associated risks must be considered carefully on a case-by-case basis.
– The first pneumonectomy in a 14 year old boy with CF was reported as far back as 1952 from Staten Island Hospital, New York (Lloyd MS, Robitzek EH Quart Bull Sea View Hospital 1952; 13:114-124.[PubMed] also see Topics -> Surgery for more information)
2016 Reicher JJ; Mohabir P; Rad E; Gayer G. Increased prevalence of tracheal diverticula in cystic fibrosis patients. Brit J Radiol 2016; 89(1060). [PubMed]
This investigation sought to evaluate the prevalence and imaging characteristics of tracheal diverticula (TD) among patients with cystic fibrosis (CF). 113 patients with CF, with a median age of 29 years, had chest CT examinations between 2002 and 2014.Of the 113 cases reviewed, 20 (17.7%) patients were found to have 1 or more TD. The presence of TD was associated with more severe disease by imaging criteria. Pulmonary function tests demonstrated an insignificant trend towards worsening function in patients with
The authors concluded the prevalence was 17.7% – a higher prevalence in patients with CF than in the general population and associated with more severe pulmonary disease.
– Initially estimated as present in 1% of an autopsy series, more recent CT studies estimate the incidence as 2% – 3.7%. Diverticula arise from the posterior tracheal wall where the cartilage rings are incomplete. Usually asymptomatic they may cause haemoptysis, dyspnoea, and dysphagia; they may act as a reservoir for infection
