Osteoporosis, Clubbing, Gout, Joint disease, Joints, Spine and teeth
1949 Lowe CU, May CD, Reed SC. Fibrosis of pancreas in infants and children: statistical study of clinical and hereditary features. Am J Dis Child 1949; 78:349-374. [PubMed]
These authors from the University of Minnesota reviewed the hereditary aspects of 134 patients with CF seen over 10 years at the Infant’s and Children’s Hospital, Boston where previously May had worked. There were 118 sibships and the authors concluded that the condition was determined by a recessive gene as had Andersen and Hodges (Andersen & Hodges, 1946 above). They noted good weight gain before first symptoms and fair gains thereafter in those who survived. In discussing the clinical features they noted 44 children showed osteoporosis and retarded bone age. They questioned the importance of vitamin A deficiency in the pathogenesis as had others.
This is one of the earliest mentions of osteoporosis in people with CF – a complication that was to become a major problem for adults with CF in the years to come.
1978 Erkkila JC, Warwick WJ, Bradford DS. Spine deformities and cystic fibrosis. Clin Orthop Relat Res 1978; 131:146-150. [PubMed]
Of 203 patients with CF 21.5% had more than 35 degrees of kyphosis – the prevalence increasing with age. The prevalence of significant scoliosis with curves greater than 10 degrees was similar to the general population. (Kumar N, et al. 2004 below found an increased prevalence of 15.6% of scoliosis in Leeds patients – some 20 times expected in people of similar age).
1979 Newman AJ, Ansell BM. Episodic arthritis in children with cystic fibrosis. J Pediatr 1979; 594-595. [PubMed]
Barbara Ansell was the leading UK authority on joint disease in children. Referred to her were five children aged two to 10 years with CF who developed transient episodic arthritis. Although polyarticular in distribution, only one joint may be involved during each attack. There was no radiological or laboratory evidence of juvenile chronic arthritis and no permanent joint limitation occurred.
Further reports followed of arthritis in people with CF (Vaze D. J Pediatr 1980; 96:346.[PubMed]73611714) including one with rheumatoid arthritis (Sagransky DM, et al, Am J Dis Child 1980; 134:319-320. [PubMed]).
We later reported a clear relationship between the joint problems and the activity of the chest infection in children with CF – the problem obviously worsening during exacerbations of respiratory infection and quite obviously improving during a course of intravenous antibiotic treatment for the exacerbation (Bowler I & Littlewood J. Lancet 1992; 340:244.[PubMed]).
1979 Mischler EH, Chesney PJ, Chesney RW, Mazess RB. Demineralization in cystic fibrosis detected by direct photon absorptiometry. Am J Dis Child 1979; 133:632-635.[PubMed]
Bone mineral content, bone width, and their ratio were measured in patients with CF using monoenergetic photon absorptiometry. Serial measurements of the radius and ulna were made in 27 patients with CF and were compared with 968 age-matched controls. Demineralization was found in 37% of the boys and 63% of the girls. Patients under age 10 years had normal bone mineral content and nine of 15 patients aged 13 or older were demineralised (P<0.01). Demineralization correlated with the extent of weight reduction in patients (P<0.001). Patients most likely to be demineralised were adolescent girls.
This appears to be the first study of bone mineral status of children with CF indicating that a sizable proportion of people with CF may be demineralised without having overt rickets. In 1979 most people with CF were children or adolescents.
1979 Sinniah D, Omar A. Quantitation of digital clubbing by shadowgram technique. Arch Dis Child 1979; 54:145-146. [PubMed]
Finger clubbing was quantified from the magnified silhouette of the right index finger in controls and in patients with clubbing; using a simple shadowgram technique obtained using an overhead projector and screen. There was good correlation between clinical assessment and measurement of both the profile angle and the hyponychial angle. The hyponychial angle appeared to be a more accurate indicator of clubbing than the profile angle.
We used this technique in Leeds to examine the fingers of a series of children with CF (Pitts-Tucker et al. 1986 below)
1986 Pitts-Tucker TJ, Miller MG, Littlewood JM. Finger clubbing in cystic fibrosis. Arch Dis Child 1986; 61:576-579. [PubMed]
We were interested in physical signs which may be useful and were impressed by the study of Sinniah & Omar, using the shadowgram, outlying the finger as a silouette on a screen using an overhead projector, to quantitate finger clubbing (1979 above) . Finger clubbing was measured in 73 of 105 patients with CF undergoing full Comprehensive Assessment at the Leeds Regional Paediatric CF Unit. Predictably, the degree of clubbing correlated well with the chest x-ray score, indices of pulmonary function and infection but not with weight, height, age, liver function, or degree of fat malabsorption. The presence of clubbing in a person with CF suggests appreciable pulmonary involvement. Most probably progression indicates deterioration in pulmonary state. In both instances increased efforts should be made to treat the infection.
This study was first presented by our CF Research Fellow Dr Mike Miller at the European CF Working Group Meeting in Israel. There was much hilarity that we people in Leeds had just realised clubbing was associated with chest problems! However, despite the hilarity it was one of the most discussed presentations of the session. People seemed hungry for some clinical signs that would be helpful in their work. Others later observed that finger clubbing regressed in some patients after successful lung transplantation.
1988 Gibbens DT, Gilsanz V, Boechat MI, Dufer D, Carlson ME, Wang CI. Osteoporosis in cystic fibrosis. J Pediatr 1988; 113:295-300. [PubMed]
Although osteoporosis had been noted in a number of previous publications, this was one of the early papers mainly dealing with osteoporosis, a complication which would become an increasingly common problem as the average age of people with CF increased. Vertebral bone density of 57 CF patients (aged 3-21 yrs) was compared with 57 matched controls. The bone density in people with CF was 10% less than in controls and worse in those with in a poor nutritional state. (For earlier mention of osteoporosis Mischler et al, 1979 above).
1998 Aris RM, Renner JB, Winders AD, Buell HE, Riggs DB, Lester GE, Ontjes DA. Increased rate of fractures and severe kyphosis: sequelae of living into adulthood with cystic fibrosis. Ann Int Med 1998; 128:186-193. [PubMed]
Bone mineral density was measured with dual-energy x-ray absorptiometry, patient-reported fracture events were confirmed by radiography, and kyphosis angles were measured by using the Cobb method. Mean bone mineral densities for the spine, femur, and total body were severely depressed in patients with cystic fibrosis, averaging 2 SDs below those of age-matched normal controls (P<0.001). Patient interviews showed that 54 fractures had occurred over 1410 patient-years, and chest radiographs showed evidence of 14 additional rib and 62 additional vertebral compression fractures. The database (which covered 1410 patient-years) showed that fracture rates were approximately twofold greater in women with cystic fibrosis aged 16 to 34 years (P = 0.015) and men with cystic fibrosis aged 25 to 45 years (P = 0.04) than in the general population. Vertebral compression and rib fractures were 100- and 10-fold more common than expected, respectively (P<0.001 for both comparisons). The mean kyphosis angle (+/- SD) for this group was markedly abnormal (44 +/- 14 degrees; 62% > or = 40 degrees) and probably contributed to diminished stature (mean height loss, 5.8 cm in men with CF and 5.9 cm in women with cystic fibrosis). Cumulative prednisone dose, body mass index, and age at puberty were the strongest predictors of bone mineral density.
Although osteoporosis had been mentioned in a number of previous reports, this was the first major study on osteoporosis in adults with cystic fibrosis. The study drew attention to the fact that osteoporosis is almost universal in adults with late-stage CF and its complications include increased fracture rates and severe kyphosis. The findings stimulated a great deal of research into osteoporosis in adults with cystic fibrosis. Later the subject was reviewed in many publications and in a consensus document from the UK Cystic Fibrosis Trust (Bone Mineralisation in Cystic Fibrosis. UK Cystic Fibrosis Trust Bone Mineralisation Working Group. February 2007. Full text available on the UK CF Trust website www.cftrust.org.uk) .
1999 Howarth CS, Selby PL, Webb AK, Dodd AK, Musson H, McL Niven R, Economu G, Horrocks AW, Freemont AJ, Mawer EB, Adams EJ. Low bone density in adults with cystic fibrosis. Thorax 1999; 54:961-967. [PubMed]
An early detailed study of a population of 151 adults aged 15-52 ears with CF from Manchester using DEXA and quantitative computed tomography and biochemical markers of bone turnover. 34% of adults with CF had BMD Z scores of -2 or less at one or more skeletal sites. The respiratory function and physical activity were related to the BMD Z scores. Markers of bone turnover were negatively related and vitamin D positively related to the BMD Z scores despite supplementation with vitamin D.
2001 Haworth CS, Selby PL, Adams JE, Mawer EB, Horrocks AW, Webb AK. Effect of intravenous pamidronate on bone mineral density in adults with cystic fibrosis. Thorax 2001; 56:314-316. [PubMed]
The aim of this study was to assess the effect of intravenous pamidronate on BMD in these subjects. Intravenous pamidronate increases axial BMD in adults with cystic fibrosis, but the high incidence of bone pain associated with this treatment might limit its use.
2002 Elkin SL. Vedi S, Bord S, Garrahan NJ, Hodson ME, Compston JE. Histomorphometric analysis of ,one biopsies from the iliac crest of adults with cystic fibrosis. Am J Respir Crit Care 2002; 166:1470-4.[PubMed]
This study reports the results of quantitative analysis of iliac bone histology in adults with cystic fibrosis (CF) and low bone mineral density (BMD). Twenty patients with CF had bone biopsies taken after double tetracycline labeling. Histomorphometric measurements were made by image analysis, and data were compared with those of healthy control subjects. Cancellous bone area was lower in the patients with CF (p = 0.003), and there was a trend towards a decrease in cancellous bone connectivity. Bone formation rate at tissue level was significantly lower in patients with CF (p = 0.0002). Wall width, representing the amount of bone formed within individual remodeling units, was decreased (p < 0.0001), as was mineralizing perimeter and mineral apposition rate. Analysis of resorption cavities revealed lower cavity area, reconstructed surface lengths, and cavity depths (p < 0.003) in patients with CF, whereas eroded surface area was higher (p = 0.0004). Our results demonstrate low cancellous bone volume in adult patients with CF with low BMD, the main cause of which appears to be low bone formation at tissue and cellular level. Osteomalacia was diagnosed in one patient. This condition should be excluded as a cause of low bone mineral density in patients with CF and vitamin D insufficiency corrected.
2002 Garske LA, Bell SC, Pamidronate results in symptom control of hypertrophic pulmonary osteoarthropathy in cystic fibrosis. Chest 2002; 121:1363-4. [PubMed]
Hypertrophic pulmonary osteoarthropathy (HPOA) may complicate the advanced lung disease that is associated with cystic fibrosis, resulting in severe joint pain and early-morning stiffness. Symptoms are usually controlled with the administration of non-steroidal anti-inflammatory drugs, physiotherapy, and, on occasions, oral corticosteroids. This report describes a case of refractory HPOA with complete remission following the administration of IV pamidronate, which is a potent inhibitor of osteoclastic bone resorption. Symptom relief resulted for up to 3 months, but repeated courses of pamidronate have been required to maintain symptom control.
This is a practically useful report of a treatment for hypertrophic pulmonary osteoarthropathy where other measures have failed.
2004 Haworth CS, Jones AM, Adams JE, Selby PL, Webb AK. Randomised double blind placebo controlled trial investigating the effect of calcium and vitamin D supplementation on bone mineral density and bone metabolism in adult patients with cystic fibrosis. J Cyst Fibros 2004; 3:233-236. [PubMed]
Patients were invited to participate if they had a BMD Z score of -1 or less in the lumbar spine, proximal femur or distal forearm. Patients were randomised to receive calcium 1 g+vitamin D 800 IU or placebo daily, in addition to their regular vitamin D supplements (900 IU/day). Calcium and vitamin D supplementation reduced the rate of bone turnover and bone loss in adult patients with cystic fibrosis, but these changes did not reach statistical significance. These data suggest that a longer term trial of this simple intervention would be justified.
2004 Amital H, Applbaum YH, Vasiliev L, Rubinow A. Hypertrophic pulmonary osteoarthropathy: control of pain and symptoms with pamidronate. Clin Rheumatol 2004; 23:330-332. [PubMed]
This case presents a patient with hypertrophic osteoarthropathy of the lower extremities that developed secondary to congenital cyanotic heart disease. The major clinical manifestation was severe bilateral leg pain. The pain that was debilitating in nature completely resolved following a single administration of 60 mg pamidronate. Hypertrophic osteoarthropathy (HOA) is an acquired, uncommon disorder of obscure etiology. It has been described mainly in association with chronic suppurative pulmonary diseases, bronchogenic carcinoma and lung metastases, cystic fibrosis, and cyanotic congenital malformations of the heart.
Although this was not a patient with CF it is possible that this treatment may be helpful in some patients with CF.
2005 Aris RM, Merkel PA, Bachrach LK, Borowitz DS, Boyle MP, Elkin S, Guise TA, Hardin DS, Haworth CS, Hollick MF, JosephM, O’Brien K, Tullis E, Watts NB, White TB.Consensus statement: Guide to bone health and disease in cystic fibrosis. J Clin Endocrinol Metab 2005; 90:1888-1896. [PubMed]
National guidelines
2007 Bone mineralisation in cystic fibrosis. Report of the UK Cystic Fibrosis Trust Bone Mineralisation Working Group. London. Cystic Fibrosis Trust, February 2007. Conway S (Chairman), Compston J, Cunliffe H, Dodd M, Elkin S, Haworth C, Jaffe A, Morton A, Redfern J, Truscott J. (below
National guidelines
2000 Conway SP, Morton AM, Oldroyd B, Truscott JG, White H, Smith AH, Haigh I. Osteoporosis and osteopenia in adults and adolescents with cystic fibrosis: prevalence and associated factors. Thorax 2000; 55:798-804.[PubMed]
Sixty six percent of 114 patients attending the Leeds Regional CF Centre had osteopenia or osteoporosis. The clinical score correlated significantly with bone mineral density (BMD) at the lumbar spine and femoral neck, and with total body BMD. Oral steroid use was significantly associated with reduced BMD at the lumbar spine and femoral neck.
Following the first extensive report by Aris et al (1998 above), there was increasing interest in osteoporosis as more people with CF reached adulthood and many of them had osteoporosis. This present study and others confirmed that osteopenia and osteoporosis were common findings in adults with CF, particularly those with severe disease and particularly those who had used significant amounts of corticosteroids.
2004 Conway SP, Oldroyd B, Morton A, Truscott JG, Peckham DG. Effect of oral bisphosphonates on bone mineral density and body composition in adult patients with cystic fibrosis: a pilot study. Thorax 2004; 59:699-703.[PubMed]
Approximately two thirds of adult patients with CF have reduced bone mineral density and up to a quarter have osteoporosis at one or more sites. Patients attending the Leeds Regional Adult Cystic Fibrosis Unit with either osteopenia or osteoporosis on dual energy X-ray absorptiometry (DXA) scanning were offered treatment with oral bisphosphonates after exclusion of abnormal vitamin D, calcium, or phosphate levels, abnormal thyroid function, or hypogonadism. The medians of the differences in annual changes in bone parameters between treatment and control groups showed significant differences in bone mineralisation in favour of the treatment group.
The authors concluded that treatment with oral bisphosphonates may improve bone mineralisation in adult patients with CF and suggested a randomised controlled trial.
2004 Kumar N, Balachandran S, Millner PA, Littlewood JM, Conway SP, Dickson RA. Scoliosis in cystic fibrosis: is it idiopathic? Spine 2004; 29:1990-1995. [PubMed]
This is a retrospective study of all the patients registered with the Leeds Regional Adult and Paediatric Cystic Fibrosis units from 1982 to 1997 carried out by Mr Kumar, an orthopaedic surgeon who, at the time, he was working with Professor Bob Dickson (an authority on scoliosis) at St James’s University in Leeds. Of the 316 patients, there were 184 adults (age 17 years and above) and 132 children (age 0-6 years). In the 4- to 16-year age group, the prevalence of scoliosis was 15.6%, which is 20 times the prevalence in 15,793 school children with a similar age and sex distribution from the same geographic area. The majority of curves were single-thoracic, apical around T6-T8 with no side predilection. In the adult population (above 16 years), the prevalence was 9.8%, which is higher than that of the general population. These curves were thoracic, apical around T7-T8, and approximately two thirds of them were right-sided.
The study shows a high prevalence of scoliosis in people with cystic fibrosis. These are benign short midthoracic curves, apical between T6-T8 with no side predilection. Some of these patients from the Eighties were more severely affected with chest and nutritional problems that would be the case in more recent years.
2004 Festini F, Ballarin S, Codamo T, Doro R, Loganes C. Prevalence of pain in adults with cystic fibrosis. J Cyst Fibros 2004; 3:51-57.[PubMed]
This study was aimed at evaluating the prevalence of pain symptoms in adult CF patients, if they are noticed and treated, and the influence of pain symptoms on patients’ life. Using a questionnaire, 239 adults with CF there was a high prevalence of painful episodes among CF adult patients, as for both intensity and frequency. In a 2 months period 32.6% of patients experienced episodes of pain described as intense to severe, and 29.7% had more than 10 occurrences of pain in the same location. Headache, gastric pain and backache were the most frequently reported kind of pain. 59.8% of subjects perceived pain episodes as the cause of unfavorable effects on their life. Only 42.6% of those with pain asked a CF center physician for help and another 3.5% a general practitioner.
Painful symptoms are surprisingly common in adults with CF a fact that this study from Italy confirms. Recurrent pains are a definite cause of a worsening of the quality of life for adults with CF.
2005 Doyen V, Fournier C, Bautin N, Cortet B, Flipo RM, Wallaert B. Rheumatoid arthritis and cystic fibrosis. [French] Revue des Maladies Respiratoires. 2005; 22:667-671.[PubMed] Inflammatory arthropathies are rare complications of cystic fibrosis (CF). We describe three cases of rheumatoid arthritis (RA) occurring in patients with this disease. Among the 100 patients under the care of the adult CF centre in Lille 3 presented with RA. This developed at the ages of 17, 44 and 19 years with a FEV1 of 53%, 42% and 94% respectively. Rheumatoid factor and/or anti CCP antibodies were positive. The appearance and progression of RA were associated with exacerbations of bronchial infection and deterioration of respiratory function. In 2 patients the RA was continuously progressive despite intensive treatment involving high dose cortico-steroids, methotrexate (ineffective) followed by leflunomide (complicated by intractable respiratory infection).
There is an increased incidence of RA in the patient population with CF. The evolution of the two diseases is related and seems to be dependent on the level of infection leading to therapeutic problems.
2005 Conway SP, Wolfe SP, Brownlee KG, White H, Oldroyd B, Truscott JG, Harvey JM, Shearer MJ. Vitamin K status among children with cystic fibrosis and its relationship to bone mineral density and bone turnover. Pediatrics 2005; 115:1325-1331.[PubMed]
The aim of this study was to assess vitamin K status in an unselected population of children with CF and to investigate any vitamin K effect on bone turnover and bone mineral status. One hundred and six children entered the study. Vitamin K1 deficiency was common (70%) and the authors suggested that routine supplements should be considered.
Through its role in the carboxylation of osteocalcin, vitamin K deficiency may be associated with an uncoupling of the balance between bone resorption and bone formation. However, a cause-effect relationship between vitamin K deficiency and low bone mass has not been proved.
2006 Stephenson A. Jamal S. Dowdell T. Pearce D. Corey M. Tullis E. Prevalence of vertebral fractures in adults with cystic fibrosis and their relationship to bone mineral density. Chest 2006; 130:539-544.[PubMed]
The objectives of this study were to determine the prevalence of morphometric vertebral fractures in a large cohort of adult cystic fibrosis (CF) patients, and to examine the association between fractures and bone mineral density (BMD). DESIGN: Cross-sectional retrospective study. SETTING: A tertiary care academic hospital. Seven percent of adult patients with CF had vertebral fractures as determined by morphometry. Subjects in the fracture group had both clinically and statistically higher BMD as measured by DXA.
These findings raise the intriguing possibility that BMD may not be useful in identifying CF patients with fractures.
2007 Bone mineralisation in cystic fibrosis. Cystic Fibrosis Trust Bone Mineralisation Working Group. Conway S (Chairman), Compston J, Cunliffe H, Dodd M, Elkin S, Haworth C, Jaffe A, NMorton A, Redfern J, Truscott J. London. Cystic Fibrosis Trust, February 2007.
A detailed review of the whole subject of bone mineralisation as it applies to cystic fibrosis. Bone mineral density (BMD) is usually normal in children with CF who have well preserved lung function and nutrition. Reduction in BMD Z-scores may appear around puberty and approximately one third of adults with CF have low BMD. The full text is available on the CF Trust website (www.cftrust.org.uk).
2008 Koch AK, Brömme S, Wollschläger B, Horneff G, Keyszer G. Musculoskeletal manifestations and rheumatic symptoms in patients with cystic fibrosis (CF) no observations of CF-specific arthropathy. J Rheumatol 2008; 35:1882-1891.[PubMed]
In CF patients, the prevalence of rheumatic symptoms increases with age and CF severity. Our data suggest an association of infections with P. aeruginosa and A. fumigatus with the occurrence of rheumatic symptoms. However, no association of CF with definite inflammatory joint or connective tissue diseases was observed, and no CF-specific pattern of musculoskeletal symptoms was seen.
We also reported a definite association between the severity of the joint pains and severity of the chest infection as they definitely improved during a course of intravenous antibiotics (Bowler IM, Littlewood JM. Episodic arthritis in cystic fibrosis. lancet 1992; 340:244.[PubMed]).
2010 Mandrusiak A, Giraud D, MacDonald J, Wilson C, Watter P. Muscle length and joint range of motion in children with cystic fibrosis compared to children developing typically. Physiotherapy Canada 2010; 62:141-146. [PubMed]
Thirty eight children with CF had significantly shorter pectoralis minor, pectoralis major, and gastrocnemius-soleus muscles and significantly greater range of shoulder horizontal abduction than matched controls. The altered range of movement identified in these children with CF, strengthened the rationale to support proactive physiotherapy management of the musculoskeletal system, aiming to optimize function across the increasing lifespan.
This is another area where consideration is being given to an abnormality which may cause problems in the distant future in view of the steadily increasing length of survival of the majority of patients.
2010 Bronckers A, Kalogeraki L, Jorna HJ, Wilke M, Bervoets TJ, Lyaruu DM, Zandieh-Doulabi B, Denbesten P, de Jonge H. The cystic fibrosis transmembrane conductance regulator (CFTR) is expressed in maturation stage ameloblasts, odontoblasts and bone cells. Bone 2010; 46:1188-1196.[PubMed]
Patients with cystic fibrosis (CF) have mild defects in dental enamel. The authors tested the hypothesis that Cftr channels are present and operating in the plasma membranes of mouse ameloblasts. Tissue sections of young mouse jaws and fetal human jaws were immunostained with various anti-Cftr antibodies. Specificity of the antibodies was validated in Cftr-deficient murine and human tissues. Immunostaining for Cftr was obtained in the apical plasma membranes of mouse maturation ameloblasts of both incisor and molar tooth germs. A granular intracellular immunostaining of variable intensity was also noted in bone cells and odontoblasts. In Cftr-deficient mice the incisors were chalky white and eroded much faster than in wild type mice. Histologically, only maturation ameloblasts of incisors were structurally affected in Cftr-deficient mice. Some antibody species gave also a positive cytosolic staining in Cftr-deficient cells. Transcripts of Cftr were found in maturation ameloblasts, odontoblasts and bone cells. Similar data were obtained in forming human dentin and bone.
The authors concluded that Cftr protein locates in the apical plasma membranes of mouse maturation ameloblasts. In mouse incisors Cftr is critical for completion of enamel mineralization and conceivably functions as a regulator of pH during rapid crystal growth. They speculate that the osteopenia found in CF patients as well as in Cftr-deficient mice is likely associated with defective Cftr operating in bone cells.
2011 Haworth CS, Sharples L, Hughes V, Elkin SL, Hodson ME, Conway SP. Etherington C, Elborn JS, Rendall J, Wheaton E, Kadri E, Elliott J, Barker HC, Bearcroft PW, Hlaing T, Compston JE. Multicentre trial of weekly risedronate on bone density in adults with cystic fibrosis. J Cyst Fibros 2011; 10:470-476.[PubMed]
The aim of this study was to assess the efficacy, tolerability and safety of risedronate in adults with CF. Patients with a lumbar spine (LS), total hip (TH) or femoral neck (FN) bone mineral density (BMD) Z-score of -1 or less were randomised to receive risedronate 35mg weekly or placebo, and calcium (1g)+vitamin D(3) (800IU). At baseline, BMD Z-scores in the risedronate (n=17) and placebo (n=19) groups were similar. By 24months, 7/17 (41%) risedronate patients vs 0/19 placebo patients stopped the study medication due to bone pain. After 24months treatment, the mean difference (95% CI) in change in LS, TH and FN BMD between the risedronate vs placebo groups was 4.3% (0.4, 8.2) p=0.03; 4.0% (-0.5, 8.6) p=0.08; and 2.4% (-3.5, 8.2) p=0.41. The authors concluded that after two years treatment there was a significant increase in LS BMD with weekly risedronate compared to placebo.
Bone problems have become one of the many problems encountered as people with CF grow older. Although risedronate was not tolerated by a significant proportion of patients (41%), there did seem to be a positive effective as evidenced by improvement in the bone density of the lumbar spine.
2011 Chang EH, Lacruz RS, Bromage TG, Bringas P Jr, Welsh MJ, Zabner J, Paine ML. Enamel pathology resulting from loss of function in the cystic fibrosis transmembrane conductance regulator in a porcine animal model. Cells Tissues Organs 2011; 194(2-4):249-254.[PubMed]
Mice null for Cftr and mice null for Slc4a2 have enamel defects, and there are some case reports of enamel anomalies in patients with CF. In this study the authros demonstrate that both Cftr and AE2 expression increased significantly during the rat enamel maturation stage versus the earlier secretory stage (5.6- and 2.9-fold, respectively). These qPCR data im- ply that there is a greater demand for Cl(-) and bicarbonate (HCO3-) transport during the maturation stage of enamel formation, and that this is, at least in part, provided by changes in Cftr and AE2 expression. In addition, the enamel phenotypes of 2 porcine models of CF, CFTR-null, and CFTR-DF508 have been examined using backscattered electron microscopy in a scanning electron microscope. The enamel of newborn CFTR-null and CFTRl DeltaF508 animals is hypomineralized. Together, these data provide a molecular basis for interpreting enamel disease associated with disruptions to CFTR and AE2 expression
The CF pig model providing evidence for the cause of enamel defects reported in CF patients
2011 Horsley A, Helm J, Brennan A, Bright-Thomas R, Webb K, Jones A. Gout and hyperuricaemia in adults with cystic fibrosis. J R Soc Med 2011; 104 Suppl 1:S36-9.[PubMed]
Gout has not been described previously as a complication in cystic fibrosis (CF). Nine CF patients presented with symptoms of acute gout – an estimated prevalence of around 2.5% in the adult CF clinic population, compared to a previously described prevalence in the non-CF population of just over 1%. Serum urate is measured routinely at the annual review in this unit. Mean (SD) serum urate was 0.40 (0.09) mmol/L in male CF patients (n = 108) and 0.31 (0.08) mmol/L in female patients (n = 74). This was significantly greater than in historical controls. Thirty-seven percent of male CF patients and 36% of female patients had serum urate levels above the upper limit of normal.
Although hyperuricemia has been described by a number of authors in people with CF since 1978 (Davidson GP et al, J Pediatr 1978; 93:976-8. [PubMed] ; Sack J et al, 1980 Isr J Med Sci 1980: 417-9. [PubMed]) perhaps surprisingly, these authors did not report having observed any individuals with clinical gout. This is in marked contrast to the nine affected patients in the present report from Manchester. Much of the previous discussion has concerned the possible renal effects. It was usually considered that the older less refined pancreatic enzyme preparations were more likely to cause problems, however these patients were receiving Creon – perhaps other factors in their treatment or lifestyle (diet, alcohol, medical treatment, etc) were contributory.
2011 Sermet-Gaudelus I, Bianchi ML, Garabedian M, Aris RM, Morton A, Hardin DS, Elkin SL, Compston JE, Conway SP, Castanet M, Wolfe S, Haworth CS. European cystic fibrosis bone mineralisation guidelines. J Cyst Fibros 2011;10 Suppl 2:S16-23. [PubMed]
Patients with cystic fibrosis (CF) are at risk of developing low bone mineral density (BMD) and fragility fractures. This paper presents consensus statements that summarises current knowledge of the epidemiology and pathophysiology of CF-related skeletal deficits and provides guidance on its assessment, prevention and treatment. The statements were validated using a modified Delphi methodology.
These are European guidelines available on the ECFS website.
2013 Fainardi V. Koo SD. Padley SP. Lam SH. Bush A. Prevalence of scoliosis in cystic fibrosis. Pediatr Pulmonol 2013; 48:553-5. [PubMed]
The prevalence of idiopathic scoliosis in the general pediatric population is reported to be between 0.5% and 3.2%. Previous studies have reported an increased prevalence of scoliosis in children with cystic fibrosis. Chest X-rays of 319 patients attending the Royal Brompton CF Centre were reviewed. CF patients showed a similar prevalence of scoliosis as in the normal population (2.2% vs. 0.5-3.2%). There was the same gender (female) and side (right-sided) predilection as in normal population.
Also a recent comment – Acquisition bias may have led to acceptance of the false null hypothesis that prevalence off scoliosis is the same in cystic fibrosis as the general population (Hathorn C, et al. 2014 Pediatr Pulmonol 2014; 49:201.[PubMed]).
In a previous Leeds study (Kumar N et al, 2004 above) the incidence of scoliosis in the 132 CF children in the study was 15.6% – 20 times the prevalence in local non-CF children. However, these were children referred to Leeds since 1982 when chest involvement in many children was severe at the time of referral which presumably was a major contributory factor.
2014 Dean NC. Van Boerum DH. Liou TG. Rib plating of acute and sub-acute non-union rib fractures in an adult with cystic fibrosis: a case report. Research Notes 2014; 7: 681.[PubMed]
A-37-year old white male with cystic fibrosis with a pulmonary exacerbation had an acute 5th rib fracture and chronic non-united 6th and 7th right rib fractures. Under general anaesthesia, he had a successful open reduction and internal fixation of the right 5th, 6th and 7th rib fractures with a Synthes Matrix rib set, although the immediate post-op period required close attention and care.
The authors suggest repair of rib fractures may be of benefit in selected CF patients who have suffered multiple rib fractures that were healing poorly.
2015 Hutchins JL; Jacobs RA. Thoracic paravertebral catheter placement for acute rib pain in a pregnant patient with cystic fibrosis. A & A Case Reports. 2015; 4(3):31-2. [PubMed]
A 30-year-old woman with cystic fibrosis at 33 weeks, 4 days’ gestation sustained a rib injury during an acute pulmonary exacerbation, resulting in noncompliance with her chest wall oscillation therapy and worsening of her respiratory status with concern for inducing labor early. Insertion of an ultrasound-guided thoracic paravertebral catheter produced immediate pain relief, eliminating the need for further opioids, and she was able to tolerate her chest wall oscillation treatment. She was discharged home after 7 days and was able to deliver a healthy baby at 38 weeks via spontaneous vaginal delivery.
– A successful practical solution to an unusual but potentially very serious problem. (See also Cutshall C, Hutchins J. A & A Case Reports 2015; 4(3):29-30. [PubMed])
2016 Callemeyn J, van Haecke P; Peetermans WE; Blockmans D. Clubbing and hypertrophic osteoarthropathy: insights in diagnosis, pathophysiology, and clinical significance. Acta Clinica Belgica 2016; 71(3):123-30. [PubMed]
This article reviews clinical criteria and pathophysiology of clubbing and hypertrophic osteoarthropathy (HOA). A diagnostic algorithm is proposed, based on etiology and current insights. The prognostic impact on associated diseases is discussed. The Internet databases Medline and Embase were searched. Articles were selected based on relevance of abstract, article type and impact of the journal.
Diagnostic criteria include Lovibond’s profile sign, distal/interphalangeal depth ratio and Schamroth’s sign. Three pathophysiological causes of clubbing can be distinguished: hypoxia, chronic inflammation and aberrant vascularization. A prominent role for vascular endothelial growthfactor is suggested. Associated symptoms and clinical signs should guide the initial diagnostic evaluation. Finally, clubbing is a negative prognostic factor in certain pulmonary disorders, including cystic fibrosis.
Roehmel JF, Kallinich T, Staab D, Schwarz C.Clinical manifestations and risk factors of arthropathy in cystic fibrosis. Respir Med. 2019 Feb;147:66-71. doi: 10.1016/j.rmed.2019.01.003. Epub 2019 Jan 17.[Pubmed]
-

Jobst Roehmel
- An observational study to assess the clinical manifestations, frequency, and risk factors of CF associated arthropathy. Of 186 patients (Demographics: Mean age 27 years, female gender 104/186 (57%), CFTR F508del homozygous 82/186 (44%) included in the study, 54/186 (29%) had experienced joint symptoms. Joint pain and swelling were the most frequent symptoms. The joints of the hands (JOH) followed by the joints of the feet were most affected. No specific pattern of autoantibodies was discovered. The level of total serum IgG, age, female gender, and pulmonary exacerbations per year were significant risk factors for arthropathy in the study cohort. Pulmonary exacerbations and elevated levels of total serum IgG may reflect chronic inflammation in patients with CF and may lead to a specific arthropathy associated with this condition.
The authors concluded that joint symptoms in CF are a frequent and clinically relevant phenomenon with a distinct clinical pattern. Pulmonary exacerbations and elevated levels of total serum IgG may reflect chronic inflammation in patients with CF and may lead to a specific arthropathy associated with this condition.
From the CF Center / Charité – Universitätsmedizin Berlin, A
– The relationship to inflammation, presumably pulmonary, is supported by our earlier report of clearing of joint symptoms during intravenous antibiotic treatment of respiratory exacerbations in cystic fibrosis (Bowler IM, Littlewood JM. Episodic arthritis in cystic fibrosis. Lancet 1992;340(8813):244)
Melanie M Beasley, Clare K Remy. Can we identify cystic fibrosis (CF) from skeletal remains?: A proposed differential diagnosis. Anat Rec (Hoboken) 2020 Dec 5. doi: 10.1002/ar.24576. Online ahead of print. [Pubmed]
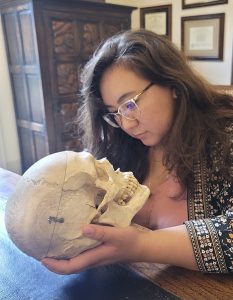
Clare Remy

Melanie Beasley
With recent medical advancement, the life span of CF patients has been extended by decades and bone disease has been observed as a common complication of long-term survivors. In addition to bone disease and associated bone fracturing, living CF patients have a unique etiology of chronic sinusitis, which manifests as a medial bulge in the lateral walls of the nasal aperture, distinct from non-CF chronic sinusitis. We suggest that available data from medical literature is sufficient evidence to indicate that CF can be identified during skeletal analysis, but future work is needed to quantify the sensitivity of the lesions for confirming a CF diagnosi
Dr Melanie M Beasley is Assistant Professor in the Dept of Anthropology, Purdue University, West Lafayette, Indiana.
Dr Clare K Remy is Supplemental Instructor and Tutor in the Dept of Anthropology, University of Tennessee-Knoxville, Knoxville, Tennessee.
– This is interesting and the apparently characteristic medial bulging of the lateral sinonasal sidewall could be used to identify CF bones
Melissa S Putman, Logan B Greenblatt, Michael Bruce, Taisha Joseph, Hang Lee, Gregory Sawicki, Ahmet Uluer, Leonard Sicilian, Isabel Neuringer, Catherine M Gordon, Mary L Bouxsein, Joel S Finkelstein. The Effects of Ivacaftor on Bone Density and Microarchitecture in Children and Adults with Cystic Fibrosis. J Clin Endocrinol Metab. 2020 Dec 1:dgaa890. doi: 10.1210/clinem/dgaa890. Online ahead of print [Pubmed]

Melissa Putman
Context: Cystic fibrosis transmembrane conductance (CFTR) dysfunction may play a role in CF-related bone disease (CFBD). Ivacaftor is a CFTR potentiator effective in improving pulmonary and nutritional outcomes in patients with the G551D-CFTR mutation. The effects of ivacaftor on bone health are unknown.
Objective: To determine the impact of ivacaftor on bone density and microarchitecture in children and adults with CF.
Design: Prospective observational multiple cohort study.
Setting: Outpatient clinical research center within a tertiary academic medical center.
Patients or other participants: Three cohorts of age-, race-, and gender-matched subjects were enrolled: 26 subjects (15 adults and 11 children) with CF and the G551D-CFTR mutation who were planning to start or had started treatment with ivacaftor within three months (Ivacaftor cohort); 26 subjects with CF were not treated with ivacaftor (CF Control cohort); and 26 healthy volunteers.
Interventions: All treatments, including ivacaftor, were managed by the subjects’ pulmonologists.
Main outcome measures: Bone microarchitecture by high resolution peripheral quantitative computed tomography (HR-pQCT), areal bone mineral density (aBMD) by dual-energy X-ray absorptiometry (DXA) and bone turnover markers at baseline, 1, and 2 years.
Results: Cortical volume, area, and porosity at the radius and tibia increased significantly in adults in the Ivacaftor cohort. No significant differences were observed in changes in aBMD, trabecular microarchitecture, or estimated bone strength in adults or in any outcome measures in children.
Conclusions: Treatment with ivacaftor was associated with increases in cortical microarchitecture in adults with CF. Further studies are needed to understand the implications of these findings.
Dr Melissa S Putman is a paediatric and adult endocrinologist in the Endocrine Unit, Department of Medicine, Massachusetts General Hospital, Boston, MA. and the Division of Endocrinology, Boston Children’s Hospital, Boston, MA.
Amanda Traylor, Denee DiPilla-George, Pornchai Tirakitsoontorn. An Unusual Presentation of Chest Pain in a Patient With Cystic Fibrosis: A Case Report. Pediatr Phys Ther 2021 Apr 1;33(2):E99-E102.doi: 10.1097/PEP.0000000000000790. [Pubmed]
This case report describes the identification and treatment of costochondritis with suspected neural entrapment in a 14-year-old individual diagnosed with cystic fibrosis. The individual discussed in this report had resolution of his chest pain with additional improvement in pulmonary function test results.
Statement of conclusion and recommendations for clinical practice: This case supports the need for musculoskeletal and neuromuscular screening and intervention for patients with cystic fibrosis. The success of the intervention suggests that when traditional approaches to treatment of costochondritis fail, use of myofascial release at the accessory muscles of breathing could be beneficial.
From the Departments of Rehabilitation (Drs Traylor and DiPilla-George) and Pulmonology (Dr Tirakitsoontorn), CHOC Children’s Hospital of Orange County, Orange, California.
Claudia Grehn, A-M Dittrich, J Wosniok, F Holz, S Hafkemeyer, L Naehrlich, C Schwarz, Registry working group of the German CF Registry. Risk factors for cystic fibrosis arthropathy: Data from the German cystic fibrosis registry. J Cyst Fibros 2021 May 22;S1569-1993(21)00130-2.doi: 10.1016/j.jcf.2021.05.003.Online ahead of print. [Pubmed]

Claudia Grehn
Background: Epidemiology and potential risk factors for cystic fibrosis arthropathy (CFA) were studied in a relevant cystic fibrosis (CF) patient cohort.
Methods: Cohort study of patients included in the German CF registry in 2016-2017. Descriptive analysis, exploratory tests and multivariable logistic regression were used to assess prevalence of CFA and associated potential risk factors for adult patients with/without chronic Pseudomonas aeruginosa infection.
Results: 6069 CF patients aged from 0 to 78 years were analysed. CFA was observed in 4.9% of the patients. Prevalence was significantly higher in adult patients (8.4%) compared to patients <18 years (0.7%; p<0.0001). Logistic regression analyses in adult patients (n=3319) showed that CFA was significantly associated with increasing age (OR=1.04; 95% CI: 1.02-1.05; p<0.0001), female gender (OR=2.10; 95%CI:1.52-2.90; p<0.0001), number of hospitalizations (OR=1.24; 95%CI:1.12-1.36; p<0.0001), chronic P. aeruginosa infection (OR=1.83; 95%CI:1.28-2.61; p=0.0009), CF-related diabetes (OR=1.69; 95%CI:1.23-2.33; p=0.0013), pancreatic insufficiency (OR=2.39; 95%CI:1.28-4.46; p=0.0060) and sinusitis/polyps (OR=1.91; 95%CI:1.39-2.62; p<0.0001). In a subgroup analysis of adults without chronic P. aeruginosa infection (n=1550) CFA was also significantly associated with increasing age, female gender, increasing number of hospitalizations, pancreatic insufficiency as well as sinusitis/polyps; antimycotic treatment associated only in this subgroup while association with CF-related diabetes was not significant.
Conclusion: CFA is a frequent and clinically relevant co-morbidity particularly in adult CF patients. CFA is significantly more common in patients with chronic P. aeruginosa colonization but associations with other indicators for a more severe disease course were identified regardless of P. aeruginosa colonization status.
Dr Claudia Grehn is in the Department of Pediatric Pneumology, Immunology and Intensive Care Medicine, Charité – Universitätsmedizin, Berlin, Germany. Electronic address: claudia.grehn@charite.de.
Jagdeesh Ullal, Katherine Kutney, Kristen M Williams, David R Weber. Treatment of cystic fibrosis related bone disease. J Clin Transl Endocrinol 2021 Dec 21;27:100291.doi: 10.1016/j.jcte.2021.100291.eCollection 2022 Mar. [Pubmed]

Jagdeesh Ullal
The advent of highly effective CFTR modulator therapies has slowed the progression of pulmonary complications in people with cystic fibrosis. There is increased interest in cystic fibrosis bone disease (CFBD) due to the increasing longevity of people with cystic fibrosis. CFBD is a complex and multifactorial disease. CFBD is a result of hypomineralized bone leading to poor strength, structure and quality leading to susceptibility to fractures. The development of CFBD spans different age groups. The management must be tailored to each group with nuance and based on available guidelines while balancing therapeutic benefits to risks of long-term use of bone-active medication. For now, the mainstay of treatment includes bisphosphonates. However, the long-term effects of bisphosphonate treatment in people with CF are not fully understood. We describe newer agents available for osteoporosis treatment. Still, the lack of data behooves trials of monoclonal antibodies treatments such as Denosumab and Romozosumab and anabolic bone therapy such as teriparatide and Abaloparatide. In this review, we also summarize screening and non-pharmacologic treatment of CFBD and describe the various options available for the pharmacotherapy of CFBD. We address the prospect of CFTR modulators on bone health while awaiting long-term trials to describe the effects of these medications on bone health.
Dr Jagdeesh Ullal is at the UPMC Center for Diabetes and Endocrinology, University of Pittsburgh Medical Center, Pittsburgh, PA 15213, USA.
Kristen M Williams, Amy Darukhanavala, Rebecca Hicks, Andrea Kelly. An update on methods for assessing bone quality and health in Cystic fibrosis. J Clin Transl Endocrinol 2021 Dec 6;27:100281.doi:10.1016/j.jcte.2021.100281.eCollection 2022 Mar. Free PMC article [Pubmed]

Kristen M Williams
With increasing life expectancy in people with Cystic fibrosis (CF), the focus of clinical care has shifted to management and prevention of non-pulmonary comorbidities. CF related bone disease, defined by low bone mineral density (BMD), is prevalent across all age groups and acknowledges the increased fractures rates that negatively impact lung function and quality of life. Dual energy X-ray absorptiometry (DXA) measurement of bone mineral content (BMC) and “areal” BMD (aBMD) is recommended for identifying and monitoring bone health in children and adults due to its low cost, low radiation exposure, and widespread availability. Recent studies in children and adolescents with chronic illness focus on adjustment of BMC and aBMD measurements for height due to the effects of short stature and delayed maturation on bone size. Expanded reference databases for alternate imaging sites such as the ultradistal radius and hip present opportunities for research and long-term monitoring. As the two-dimensional nature of DXA imposes limitations, we highlight other imaging modalities including peripheral quantitative computed tomography QCT (pQCT), magnetic resonance imaging, and quantitative ultrasound (QUS). These tools, while primarily used in a research setting, can impart information on true volumetric bone density and bone microarchitecture as well as contribute to fracture assessment and prediction. Due to the high morbidity and mortality associated with vertebral and hip fracture, we will present on vertebral fracture assessment (VFA) in both children and adults as well as applied analyses including hip structural analysis (HSA), trabecular bone score (TBS), and fracture risk assessment (FRAX) for high risk groups. Questions remain on the future clinical applicability and accessibility of these assessment and prediction tools, longitudinal monitoring through adolescence and adulthood, and how outcome measures may guide bone modifying therapies.
Dr Kristen M Williams is a Pediatric endocrinologist at the Division of Pediatric Endocrinology, Diabetes, and Metabolism, Columbia University Irving Medical Center, 1150 St Nicholas Avenue, New York, NY, USA
Rosara M Bass, Babette S Zemel Virginia A Stallings, Mary B Leonard Jaime Tsao AndreaKelly. Bone accrual and structural changes over one year in youth with cystic fibrosis. J Clin Transl Endocrinol 2022 Mar 25;28:100297.doi: 10.1016/j.jcte.2022.100297.eCollection 2022 Jun.[Pubmed]

Rosara Bass
Background: Pediatric bone accrual governs peak bone mass and strength. Longitudinal studies of bone health in youth with cystic fibrosis (CF) may provide insight into CF-related bone disease (CFBD), a prevalent co-morbidity in adults with CF.
Methods: This one-year longitudinal study of youth with pancreatic insufficient CF, enrolled in a nutrition intervention study [n = 62 (36 M/26F)] 1) examined dual-energy x-ray absorptiometry (DXA)-defined lumbar spine (LS) and total body less head (TBLH) bone accrual and 2) compared their changes in peripheral quantitative computed tomography (pQCT) cortical and trabecular tibial bone density and geometry to those of a healthy reference group [n = 143 (68 M/75F)].Main outcome measures were 1) DXA: lumbar spine areal bone mineral density (LSaBMD) and total body less head bone mineral content (TBLH-BMC), sex- and pubertal status-specific, height velocity (HV)-adjusted or HV and lean body mass velocity (HV-LBMV)-adjusted annualized velocity-Z scores and 2) pQCT: age, sex, pubertal status and, when appropriate, tibial length adjusted Z-scores for bone architecture measures.DXA velocity-Z were compared to expected mean of 0 and correlations with clinical parameters (age, BMI-Z and FEV1%-predicted) tested. Within-subject comparisons of HV-adjusted and LBMV-HV-adjusted DXA velocity-Z were conducted in CF.pQCT Z-scores were compared between the two groups over one year using longitudinal models. Longitudinal relationships between measures of bone health and clinical parameters (age, BMI-Z and FEV1%-predicted) were examined in individuals with CF.
Results: DXA velocity-Z were higher than normal in females (p < 0.05) but not males with CF. HV-adjusted and LBMV-HV-adjusted velocity-Z did not differ for LSaBMD or TBLH-BMC.In males with CF, both HV-adjusted and LBMV-HV-adjusted LSaBMD velocity-Z scores correlated negatively with age (HV rho: -0.35; p = 0.045 and LBMV-HV rho: -0.47; p = 0.0046). In males with CF BMI-Z correlated positively with HV-adjusted LSaBMD velocity-Z (rho: 0.37; p = 0.034), but this relationship did not persist for LBMV-HV (rho: 0.14; p = 0.42). In females with CF, no correlations between LSaBMD velocity-Z scores and age or BMI-Z were found (all p > 0.05). No correlations between LSaBMD velocity-Z scores and FEV1%-predicted were seen in either sex (all p > 0.12). TBLH-BMC velocity Z-scores were not correlated with clinical parameters in either sex (all p > 0.1).At baseline, multiple pQCT parameters were lower in CF (p < 0.05). pQCT Z-scores did not differ between baseline and one-year in either CF or reference group. In a longitudinal model comparing pQCT-Z changes in CF and reference, multiple pQCT-Z outcomes remained lower in CF, but the changes in parameters did not differ in CF vs reference (all p > 0.26). Lower pQCT outcomes in CF were largely restricted to males (CF group*female sex interaction beta coefficients > 0). In this combined longitudinal model, of both CF and reference, BMI-Z was positively associated with pQCT-Z parameters(p < 0.001).Multiple pQCT-Z outcomes positively correlated with both BMI-Z and FEV1%-predicted in males with CF, and with FEV1%-predicted in females with CF (p < 0.05). Age was negatively associated with section modulus (p = 0.001) in males and with cortical density-Z in females (p < 0.001).
Conclusions: With improved longevity, bone health in CF is of increasing importance. On average, bone accrual was preserved in youth with CF, and while deficits in bone geometry and strength were found, these deficits did not worsen over the one-year study. Lower LS bone accrual with increasing age suggests emerging adulthood is a period of vulnerability in CF while the role of LBM in bone health is underscored by the lack of relationship between LBMV-adjusted accrual and BMI. These findings may be useful in targeting screening practices and interventions.
Keywords: BMC, Bone mineral content; Bone accrual; Bone health; CF, Cystic Fibrosis; Cystic fibrosis; DXA velocity; DXA, Dual energy x-ray densiometry; FEV1, Forced expiratory volume in one second; HAZ, height-for-age-z-score adjusted; HV, height velocity; LBM, lean body mass; LS, lumbar spine; Peripheral quantitative computed tomography; TBLH, total body less head; Vel-Z, velocity-Z; Z-score; aBMD, areal bone mineral density; pQCT, peripheral quantitative tomography.
Rosara M Bass is in the Division of Gastroenterology, Hepatology and Nutrition, The Children’s Hospital of Philadelphia, Philadelphia, PA 19146 USA and the Department of Pediatrics, The University of Pennsylvania, Philadelphia, PA 19146, USA.
