Nose, Sinuses, Smell
1959 Lurie MH. Cystic fibrosis of the pancreas and the nasal mucosa. Ann Otol Rhinol Laryngol 1959; 68:478.[PubMed]
An early description of nasal polyps (figure 1) which are remarkably common in both children and adults with CF (6-48% in various series). In this paper three illustrative cases were described at an ENT meeting. (also Shwachman et al. 1962 below; Complete filling of the nasal sinuses was described by Pennington CL. AMA Arch Otolaryng 1956; 63:576; Bodian describes changes in the sinuses, (1952 above). Nasal polyposis may be the presenting feature of CF, the first evidence of CF being nasal polyps so large they are appearing at the external nares as occured in one of our Leeds children.
1961 Shwachman H, Kulczycki LL, Mueller HL. Nasal polyposis in patients with cystic fibrosis. Am J Dis Child 1961; 102:768-76
An early description of nasal polyps (also Lurie MH, 1959 above). Of 650 patients with CF seen over the previous 4 years, 43 had nasal polyposis – 10% of those over 3 years. The effect on facial appearance, increasing the width of the nasal bridge, and the tendency to recur after removal were stressed. There was nothing characteristic about the histological appearance of the polyps. A sweat test was recommended in any child with nasal polyposis. (also Shwachman H. Kulczycki LL, Mueller HL, Flake CG. Nasal polyposis in patients with cystic fibrosis. Pediatrics 1962; 30: 389-401. [PubMed]). Nasal polyposis occurring in 50 (6.7%) of 742 patients with CF in those with allergies and those without).
– Later more accurate assessment of the incidence of polyps was possible with fibreoptic instruments indicating 37% of patients were affected. Inhaled steroids were used with some success as local treatment – eventually many years later confirmed as effective in a controlled trial (Hadfield et al, 2000 below). Also as an incidental finding during a trial of oral ibuprofen for the chest infection, the nasal polyps were observed to shrink in patient receiving this drug (Lindstrom et al, 2007 below).
Wang X. Moylan B. Leopold DA. Kim J. Rubenstein RC. Togias A. Proud D. Zeitlin PL. Cutting GR. Mutation in the gene responsible for cystic fibrosis and predisposition to chronic rhino sinusitis in the general population. JAMA 2000; 284:1814-1819. [PubMed]
Eleven of 147 chronic rhino sinusitis (CRS) patients (7.5%) were found to have a CF mutation (DeltaF508, n = 9; G542X, n = 1; and N1303K, n = 1). Diagnostic testing excluded CF in 10 of these patients and led to CF diagnosis in 1. Excluding this patient from the analyses, the proportion of CRS patients who were found to have a CF mutation (7%) was significantly higher than in the control group (n = 2 [2%]; P =.04, both having DeltaF508 mutations). Furthermore, 9 of the 10 CF carriers had the polymorphism M470V, and M470V homozygotes were over represented in the remaining 136 CRS patients (P =.03).
These data indicate that mutations in the gene responsible for CF may be associated with the development of chronic rhinosinusitis in the general population. Another study suggesting that CF heterozygotes or even atypical patients with CF may be over represented in a condition with similar clinical features to CF.
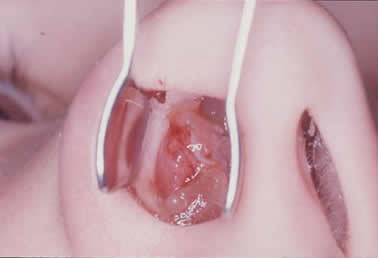
Nasal polyps in cystic fibrosis
2000 Hadfield PJ, Rowe-Jones JM, Mackay IS. The prevalence of nasal polyps in adults with cystic fibrosis. Clin Otolaryngol Allied Sci 2000; 25:19-22.[PubMed]
The prevalence of nasal polyps in this endoscopic study of 211 adults with CF was 37%. The commonest nasal symptoms were discharge, headache and obstruction. Intranasal endoscopy usually demonstrated mucosal oedema and thin, clear discharge. The prevalence of allergy, as diagnosed by skin prick testing, was almost twice that of the general population. Tympanometry showed that middle ear effusion was uncommon in these patien
The first prospective, randomised, double-blind trial of the treatment of nasal polyps in cystic fibrosis. Use of betamethasone nasal drops showed a statistically significant reduction in polyp size in comparison to placebo treatment.
This is the first trial of topical steroid treatment of nasal polyps, a complication that can prove a troublesome and recurring problem for the patient. Inhaled steroids appeared to have some effect but they had never been the subject of a clinical trial. The recurrence rate after surgery is very high.
In a more recent study of the non-steroidal anti-inflammatory ibuprofen for CF lung disease, the drug had a favourable and quite unexpected effect on the nasal polyps which was noted as an incidental finding (Lindstrom D R, et al. J Otolaryngol 2007; 36:309-314. below [PubMed]).
2003 Bateman ND, Fahy C, Woolford TJ. Nasal polyps: still more questions than answers. J Laryngol Otol 2003; 117:1-9.[PubMed].
Nasal polyps are common, affecting one to four per cent of the population. Their cause, however, remains unknown and it is possible that it is not the same in all patients. They have a clear association with asthma, aspirin sensitivity and cystic fibrosis. Histologically they demonstrate large quantities of extracellular fluid, mast cell degranulation and an infiltrate of inflammatory cells, usually eosinophils. The authors believe that an endoscopic approach using a microdebrider facilitates accurate removal of polyps with preservation of normal anatomy.
– This is a detailed review of polyps in general with no new information.
2007 Lindstrom DR, Conley SF, Splaingard ML, Gershan WM. Ibuprofen therapy and nasal polyposis in cystic fibrosis patients. J Otolaryngol 2007; 36:309-314.[PubMed]
Twelve of 22 patients with CF were treated with high-dose ibuprofen therapy to benefit their pulmonary function. Twelve had nasal polyposis and all 12 patients had observed absence of nasal polyps at some point during their ibuprofen course; nasal polyps were present in five patients during ibuprofen therapy, and all resolved with increased ibuprofen doses. Polyps occurred in six of eight patients after ibuprofen therapy ceased. Five of the 12 patients required endoscopic sinus surgery for polyposis.
This is an interesting incidental finding that oral ibuprofen improves nasal polyposis. This could prove very helpful in patients with severe and recurring nasal polyposis which can be a very difficult problem.
2009 Buyukozturk S. Gelincik A. Aslan I. Aydin S. Colakoglu B. Dal M. Methotrexate: can it be a choice for nasal polyposis in aspirin exacerbated respiratory disease?. J Asthma 2009; 46:1037-1041. [PubMed].
A report of two patients with asthma whose nasal polyps dramatically reduced in size after a course of methotrexate therapy administered as an additional treatment for their steroid- dependent asthma. Although these patients had asthma and not CF it is interesting that they responded to methotrexate – it is possible that the minority of people with severe recurring nasal polyps may also respond.
2010 Rickert S, Banuchi VE, Germana JD, Stewart MG, April MM. Cystic fibrosis and endoscopic sinus surgery: Relationship between nasal polyposis and likelihood of revision endoscopic sinus surgery in patients with cystic fibrosis. Arch Otolaryngol 2010; 136:988- 992. [PubMed] The authors graded the extent of nasal polyposis endoscopically in a cystic fibrosis population before the first surgical intervention, they observed the patients prospectively and recorded the need for revision endoscopic sinus surgery, and compared this among the individual polyp grading groupings. There were significant differences depending on the polyp grading – more polyps more recurrent surgery required.
Although the findings were to be expected they are included as there is relatively little published on sinus and polyp problems although they are a major chronic problem for many people with CF.
2013 Lavin J. Bhushan B. Schroeder JW Jr. Correlation between respiratory cultures and sinus cultures in children with cystic fibrosis. Int J Pediatr Otorhi 2013; 77:686-9.[PubMed]
Previous studies have had varying results on the correlation between respiratory and sinus cultures so further investigation is warranted. Bacterial growth from preoperative sputum, bronchoalveolar lavage, and oropharyngeal cultures were compared to the bacterial growth from intraoperative sinus cultures in patients with cystic fibrosis undergoing endoscopic sinus surgery.
In the patients over eight years of age, 16 of 26 sputum cultures matched sinus cultures (p=0.4). When sputum cultures with normal flora and no growth were eliminated, 16 of 21 matched sinus cultures (p=0.02). No statistically significant associations were found for sputum cultures in patients under eight years of age. No statistically significant associations were found between oropharyngeal or bronchoalveolar lavage cultures and intraoperative sinus cultures from patients of any age. When Staphylococcus aureus was cultured from sputum in patients over eight years of age the positive and negative predictive values that S. aureus would be cultured from the sinuses were 100% and 75% respectively. The positive and negative predictive values for Pseudomonas aeruginosa were 73% and 86% respectively.
The authors concluded that in children with CF who are over eight years of age, organisms grown from sputum cultures are similar to organisms grown from sinus cultures when bacterial growth is present.
2013 Lindig J. Steger C. Beiersdorf N. Michl R. Beck JF. Hummel T. Mainz JG. Smell in cystic fibrosis. Eur Arch Oto-Rhino-L 2013; 270:915-921. [PubMed]
In CF-associated smelling deficiencies are reported in between 12 and 71 % of patients. The aim of this study was to assess olfactory and gustatory function in relation to sinonasal symptoms and sinonasal colonization, and lung function and nutrition. Thirty-five CF patients of different ages were compared to 35 age-matched healthy controls. Olfactory function was assessed by ‘Sniffin’Sticks’, gustatory qualities by “Taste-strips”, and symptoms by sino-nasal outcome test 20 (SNOT-20).
Normosmia was found in 62.8 % of healthy controls but only in 28.6 % of CF patients. In contrast the majority of CF patients exhibited a smell loss; almost 62.9 % of them were hyposmic, and 8.6 % functionally anosmic. Importantly, reduced olfactory function only affected odor thresholds, which were significantly increased in CF, not odor identification. This suggests that the olfactory dysfunction in CF results from the olfactory periphery due to either problems in conduction and/or a functional lesion due to the inflammatory process. SNOT-20 scores increased continuously from normosmic to hyposmic and anosmic CF patients (means 7.2/11.1/28.3 points). Neither sinonasal pathogen colonization, gender, pulmonary function, nor allergy or sinonasal surgery appeared to have significant effects on olfactory function and taste.
Olfactory disorders are considerably more frequent in CF patients than in age-matched healthy controls. Assessing these parameters within CF-routine care should be considered because of their importance to nutrition and, thus, overall therapy outcome.
This problem may be very relevant in people with CF and a contributory factor to poor appetite and inadequate dietary intake. As the condition in the upper respiratory tract nor treatment had a signifcant effect it is difficult to see how the situation could be improved. As more CF patients had reduced rather than absent sense, which affected only 8.6%, increasing the olfactory stimuli from food etc would presumably be a first step in improving the situation. However, a previous study found that nutritional status was unrelated to the sensation of smell (Aitken ML et al. Sensation of smell does not determine nutrional status in patients with cystic fibrosis.Pediatr Pulmonol 1997; 24:52-56. [PubMed]).
2013 Aanaes K. Johansen HK. Poulsen SS. Pressler T. Buchwald C. Hoiby N. Secretory IgA as a diagnostic tool for Pseudomonas aeruginosa respiratory colonization. J Cyst Fibros 2013; 12: 81-87. [PubMed]
Pseudomonas aeruginosa sinusitis may be the focus for intermittent lung colonization in patients with cystic fibrosis (CF). The sinusitis may induce elevated IgA levels in nasal secretion and saliva against P. aeruginosa. 120 CF patients chronically infected, intermittently colonized or without P. aeruginosa in the lungs participated in this cross-sectional study. IgA and IgG against P. aeruginosa sonicate and alginate were measured in nasal secretions, saliva, and in serum by ELISA. The intermittently colonized patients had significantly higher IgA levels in nasal secretions and saliva than those without P. aeruginosa in the lungs, indicating that P. aeruginosa sinusitis may precede intermittent colonization and chronic infection of the lungs.
The authors conclude specific IgA against P. aeruginosa in nasal secretions and saliva can contribute to differentiation between patients chronically infected, intermittently colonized, and without P. aeruginosa in the lungs. The diagnostic value of the IgA ELISA awaits a prospective study.
– The upper respiratory tract is receiving more attention as a source of organisms invading the lower airways – particularly P. aeruginosa. ELISA determined antibodies to P. aeruginosa have been used by some units for many years, including our own in Leeds, and found to be valuable in indicating the presence of Pseudomonas.
Summary of Kasper Aanaes’s Doctoral Thesis on this subject has been published and is fully referenced and liberally illustrated – “Bacterial sinusitis can be a focus for initial lung colonisation and chronic lung infection in patients with cystic fibrosis. Aanaes K. J Cyst Fibros 2013; 12 (Suppl 2):S1-S20.
2013 Berkhout MC. Rijntjes E. El Bouazzaoui LH. Fokkens WJ. Brimicombe RW. Heijerman HG. Importance of bacteriology in upper airways of patients with Cystic Fibrosis. J Cyst Fibros 2013; 12:525-529. [PubMed]
Recently the influence of the upper airways (UAW) on the general health of a patient with Cystic Fibrosis (CF) has been acknowledged. Surprisingly the microbiology of the upper compartment of the airways receives barely any attention in the treatment of CF. The aim of the present study was to investigate the microbiology of the upper airways in adult patients with CF, to correlate these findings with cultures from the lower airways (LAW) and with clinical characteristics. In this cross-sectional study bacteriological and clinical data were gathered from 104 adult patients with CF. UAW samples for culture were collected by nasal lavage and middle meatal swabs; LAW cultures were performed on expectorated sputum or cough swabs. Each patient performed the Rhinosinusitis Outcome Measure (RSOM-31).
In 72 patients (69.2%) UAW cultures yielded micro organisms other than normal nasal flora and in 50 patients (48.1%) Pseudomonas aeruginosa grew from the UAW cultures. Similarity between UAW and LAW cultures was determined in 50.0% of these 72 patients. In 3 patients P. aeruginosa was cultured from the UAW after successful eradication of P. aeruginosa from the LAW. P. aeruginosa in the UAW did not influence symptoms of sinonasal disease compared to other micro organisms.
The authors concluded comparison of UAW and LAW cultures in adult patients with CF showed one or more concordant micro organism in 50.0% of the patients. P. aeruginosa was most frequently cultured from the UAW. P. aeruginosa can be cultured from the UAW after eradication therapy which may suggest persistence of P. aeruginosa in the UAW. We feel this is may be a motive to include the UAW in eradication therapy in Cystic Fibrosis.
– Undoubtedly the upper airways are now receiving more attention as a potential reservoir of infection. The relationship between the cultures from the upper and lower airways is not surprising but the persistence even after P. aeruginosa eradication therapy certainly suggests more active measures would be appropriate. However, some years ago decontamination of the upper respiratory tract was attempted with regular polymyxin/tobramycin/amphotericin gel to treat patients newly colonised by P. aeruginosa infection but did not prove to be successful (Dalzell AM et al, 1990. [PubMed]).
2014 Di Cicco M. Alicandro G. Claut L. Cariani L. Luca N. Defilippi G. Costantini D. Colombo C. Efficacy and tolerability of a new nasal spray formulation containing hyaluronate and tobramycin in cystic fibrosis patients with bacterial rhinosinusitis. J Cyst Fibros 2014; 13(4):455-60. [PubMed]
A small study to assess the tolerability and efficacy of a nasal spray formulation containing 0.2% sodium hyaluronate and 3% tobramycin compared to a control formulation containing 0.2% sodium hyaluronate alone in the treatment of bacterial rhinosinusitis in patients with CF.
The formulation containing hyaluronate and tobramycin was more effective than hyaluronate alone in improving the status of the nasal mucosa, in reducing the mucopurulent secretion at the level of the osteomeatal complex and in improving ENT symptoms (hyposmia/anosmia and headache/facial pain).
The authors suggest that the present study suggests that the combination therapy with hyaluronate plus tobramycin was more effective than hyaluronate alone in the treatment of bacterial rhinosinusitis in CF.
2014 Hayes D Jr. McCoy KS. Sheikh SI. Improvement of sinus disease in cystic fibrosis with ivacaftor therapy. Am J Resp Crit Care Med 2014; 190(4):468. [PubMed]
A 19-year old woman with CF (d508/G551D) experienced significant general improvement after 15 months ivacaftor therapy and in particular major improvement in previously troublesome sinus disease. Impressive changes in the MCT scan reproduced in the link from the abstract.
2014 Lourenco BM. Costa KM. da Silva Filho M. Voice disorder in cystic fibrosis patients. ONE [Electronic Resource]. 9(5):e96769, 2014 [PubMed]
The authors tested vocal parameters, using both objective physical measures and the GRBAS subjective evaluation method, in male and female cystic fibrosis patients undergoing conventional treatment and compared them to age and sex matched controls. They found that cystic fibrosis patients had a significantly lower vocal intensity and harmonic to noise ratio, as well as increased levels of jitter and shimmer. In addition, cystic fibrosis patients also showed higher scores of roughness, breathiness and asthenia, as well as a significantly altered general grade of dysphonia. When they segregated the results according to sex, we observed that, as a group, only female cystic fibrosis patients had significantly lower values of harmonic to noise ratio and an abnormal general grade of dysphonia in relation to matched controls, suggesting that cystic fibrosis exerts a more pronounced effect on vocal parameters of women in relation to men.
Overall, the dysphonic characteristics of CF patients can be explained by dysfunctions in vocal fold movement and partial upper airway obstruction, potentially caused by the accumulation of mucus and chronic cough characteristic of CF symptomatology. These results show that CF patients exhibit significant dysphonia and suggest they may potentially benefit from voice therapy as a parallel treatment strategy.
With the intrinsic mucosal abnormalities and long term inhalation therapy advised, it is not surprising there are minor voice abnormalities in many people with CF.
2014 Mainz JG. Schien C. Schiller I. Schadlich K. Koitschev A. Koitschev C. Riethmuller J. Graepler-Mainka U. Wiedemann B. Beck JF. Sinonasal inhalation of dornase alfa administered by vibrating aerosol to cystic fibrosis patients: a double-blind placebo-controlled cross-over trial. J Cyst Fibros 2014; 13:461-70. [PubMed]
Either dornase alfa (Pulmozyme) or isotonic saline were inhaled for 28 days with the Pari-Sinus and after 28 days (wash-out) crossed over to the alternative treatment. Primary nasal symptoms improved significantly with dornase alfa compared with no treatment, while small improvements with isotonic saline did not reach significance.
Vibrating sinonasal inhalation of dornase alfa reduces rhino sinusitis symptoms in CF and also incidentally improved lung function.
2015 Al-Malky G; Dawson SJ; Sirimanna T; Bagkeris E; Suri R. High-frequency audiometry reveals high prevalence of aminoglycoside ototoxicity in children with cystic fibrosis. J Cyst Fibros 2015; 14(2):248-54.[PubMed]
Intravenous aminoglycoside (IV AG) antibiotics have ototoxic complications in some patients. Audiological monitoring, if performed, uses only standard pure-tone audiometry (PTA). This study determined the most appropriate audiological tests and to identify possible risk factors. Auditory assessment was performed using standard pure tone audiometry (PTA), extended high-frequency (EHF) audiometry and distortion-product otoacoustic emissions (DPOAE). 70 CF children, mean (SD) age 10.7 (3.5) years, were recruited. Of the 63 children who received IV AG, 15 (24%) children had ototoxicity detected by EHF audiometry and DPOAE. Standard PTA only detected ototoxicity in 13 children. Eleven of these children had received at least 10 courses of IV AG courses. A 25 to 85 dBHL hearing loss (mean+/-SD: 57.5+/-25.7 dBHL) across all EHF frequencies and a significant drop in DPOAE amplitudes at frequencies 4 to 8 kHz were detected. However, standard PTA detected a significant hearing loss (>20 dBHL) only at 8 kHz in 5 of these 15 children and none in 2 subjects who had significantly elevated EHF thresholds. The number of courses of IV AG received, age and lower lung function were shown to be risk factors for ototoxicity. CF children who had received at least 10 courses of IV AG had a higher risk of ototoxicity.
Extended high frequency audiometry identified 2 more children with ototoxicity than standard PTA and depending on facilities available, should be the test of choice for detecting ototoxicity in children with CF receiving IV aminoglycosides.
2015 Farzal Z, Kou YF, St John R, Shah GB, Mitchell RB. The role of routine hearing screening in children with cystic fibrosis on aminoglycosides: A systematic review. Laryngoscope. 2015 Jul 7. doi: 10.1002/lary.25409. [Epub ahead of print] [PubMed]
Study to review the role of routine hearing screening for sensorineural hearing loss (SNHL) in children with cystic fibrosis (CF) who have been on aminoglycoside therapy. Twelve studies (1979-2014) were reviewed. The study population included 762 children (5 months-20 years). Hearing screening measures included pure-tone audiometry (PTA) at standard ± high frequency threshold (HFPTA) (12/12), distortion product otoacoustic emissions (DPOAE) (4/12), transient-evoked otoacoustic emissions (1/12), and automated auditory brainstem response (1/12).
The overall prevalence of sensory neural hearing loss ranged from 0% to 29%. However, on subset analysis of children with greater than 10 courses of intravenous (IV) aminoglycosides, up to 44% had sensory neural hearing loss. Eight studies recommended hearing screening in CF children on aminoglycosides; of these, two studies recommended screening even without aminoglycoside exposure, and four studies made no recommendations. HFPTA was the most commonly recommended screening measure followed by DPOAEs.
– This systematic review supports a recommendation for clinicians to arrange for routine hearing screening in children with CF during and after aminoglycoside exposure based on the high prevalence of sensorineural hearing loss this population. They suggest future studies should define the optimal timing for hearing screening during and after aminoglycoside therapy in children with CF.
2015 Willis J, Michael DD, Boyer H, Misono S. Prevalence and Severity of Dysphonia in Patients with Cystic Fibrosis: A Pilot Study. Otolaryngol Head Neck Surg. 2015 Jul;153(1):88-93.[PubMed] A study to assess the prevalence and severity of dysphonia in patients with cystic fibrosis sinusitis. Cystic fibrosis sinusitis appeared to be associated with worse vocal function as measured by patient self-report as well as auditory-perceptual evaluation of voice compared with patients with non-CF sinusitis and healthy controls.
2015 Mainz JG, Gerber A, Lorenz M, Michl R, Hentschel J, Nader A, Beck JF, Pletz MW, Mueller AH. Pseudomonas aeruginosa Acquisition in Cystic Fibrosis Patients in Context of Otorhinolaryngological Surgery or Dentist Attendance: Case Series and Discussion of Preventive Concepts. Case Rep Infect Dis 2015;2015:438517. [PubMed]
For their almost regular sinonasal involvement, CF patients often require otorhinolaryngological (ORL) attendance. Despite some fields around ORL-procedures with comparable risk for acquisition of P. aeruginosa as dental procedures, such CF cases have not yet been reported. The authors present four CF patients, who primarily acquired P. aeruginosa around ORL surgery, and one around dentist treatment. Perils include contact to pathogen-carriers in waiting rooms, instrumentation, suction, drilling, and flushing fluid, when droplets containing pathogens can be nebulized. Postsurgery mucosal damage and debridement impair sinonasal mucociliary clearance, facilitating pathogen proliferation and infestation.
They suggest that sinonasal surgery and dentist treatment of CF patients without chronic P. aeruginosa colonisation must be linked to repeated microbiological assessment. Further studies must elaborate whether all CF patients undergoing ORL-surgery require anti-pseudomonal prophylaxis, including nasal lavages containing antibiotics. Altogether, this underestimated risk requires structured prevention protocols.
– There is increasing interest in the upper respiratory tract and its relation to lower airways infection, in particular as a source of infection.The risks from dental equipment have been known for many years first from Copenhagen (Jensen ET et al. J Hosp Infect 1997; 36(2): 117-122. [PubMed]) but the the possibility of other upper respiratory tract procedures determining the onset of P. aeruginosa infection is obviously important.
2015 Lo DK, Hurley MN, Muhlebach MS, Smyth AR. Interventions for the eradication of methicillin-resistant Staphylococcus aureus (MRSA) in people with cystic fibrosis. Cochrane Database Syst Rev. 2015 Feb 24;2:CD009650. doi: 10.1002/14651858.CD009650.pub3. [PubMed] Methicillin-resistant Staphylococcus aureus (MRSA) has emerged as a potentially harmful pathogen in cystic fibrosis, and has been increasing steadily in prevalence internationally. Chronic pulmonary infection with MRSA is thought to confer cystic fibrosis patients with a worse overall clinical outcome and, in particular, result in an increased rate of decline in lung function. Clear guidance for the eradication of MRSA in cystic fibrosis, supported by robust evidence from good quality trials, is urgently needed.
To evaluate the effectiveness of treatment regimens designed to eradicate MRSA and to determine whether the eradication of MRSA confers better clinical and microbiological outcomes for people with cystic fibrosis. There were no eligible trials for inclusion. Although the results of several non-randomised studies would suggest that, once isolated, the eradication of MRSA is possible; whether this has a significant impact on clinical outcome is still unclear.
Update of Interventions for the eradication of methicillin-resistant Staphylococcus aureus (MRSA) in people with cystic fibrosis. [Cochrane Database Syst Rev. 2013]
2016 Alanin MC; Aanaes K; Hoiby N; Pressler T; Skov M; Nielsen KG; Taylor-Robinson D; Waldmann E; Krogh Johansen H; von Buchwald C. Sinus surgery postpones chronic Gram-negative lung infection: cohort study of 106 patients with cystic fibrosis. Rhinology 2016; 54(3):206-13. [PubMed

Mikkel Alanin
In patients with cystic fibrosis (CF) the sinuses are a bacterial reservoir for Gram-negative bacteria (GNB). From the sinuses the GNB can repeatedly migrate to the lungs. In a one-year follow-up study, endoscopic sinus surgery (ESS) with adjuvant therapy (2 weeks IV antibiotics and 6 months antibiotic nasal irrigations) reduced the frequency of pulmonary samples positive for GNB (Aanaes K et al, 2013).(See comment below for detail) The authors investigated whether the effect is sustained.They report the effect of ESS and adjuvant therapy three years postoperatively in a CF cohort participating in this prospective clinical follow-up study. The primary endpoint was the lung infection status defined by Leeds criteria.
One hundred and six CF patients underwent ESS; 27 had improved lung infection status after three years. The prevalence of patients free of lung colonization with GNB significantly increased from 16/106 patients (15%) preoperatively to 35/106 patients (33%) after three years. The total cohort had decreasing lung function during follow-up; however, in 27 patients with improved lung infection status lung function was stable. Revision surgery was performed in 31 patients (28%).
The authors concluded ESS with adjuvant therapy significantly improves the lung infection status for at least three years in our cohort of patients with CF and may postpone chronic lung infection with GNB and thus stabilize lung function.
– The procedure is a major undertaking and described in their previous paper (Aaneas K et al, 2013. 23943728). After BAL under general anesthetic, the paranasal sinuses were ventilated and drained to make these accessible for postoperative instrumental cleansing and irrigation with saline and antibiotics. More extensive surgery of the frontal and ethmoid sinuses was undertaken based on the basis of preoperative CT scan and operative findings. As a standard unicinectomy, an anterior ethmoidectomy and medial antrostomy, leaving a relatively large maxillary ostium involving more than half the medial maxillary wall. Any intramucosal abscesses were resected along with other inflamed mucosal tissue when accessible. Following the surgical procedure, the opened and now accessible sinuses were irrigated with saline and colistimethate sodium. After 2 weeks intravenous antibiotics twice daily sinus irrigations with saline and antibiotics were carried out for six monthsauthors concluded ESS with adjuvant therapy significantly improves the lung infection status for at least three years in our cohort of patients with CF and may postpone chronic lung infection with GNB and thus stabilize lung function.
Dr Mikkel Alalnin works in the Otorrhinolaryniology Dept of the Rigshospitalet Copenhagen.
2016 Doumit M, Belessis Y; Stelzer-Braid S; Mallitt KA; Rawlinson W; Jaffe A. Diagnostic accuracy and distress associated with oropharyngeal suction in cystic fibrosis. J Cyst Fibros 2016; 15(4):473-8. [PubMed] This study aimed to assess the diagnostic accuracy of oropharyngeal suction (OPS) samples in obtaining airway bacterial cultures in young children with cystic fibrosis (CF), and the level of child distress caused by obtaining OPS samples.Young children with CF undergoing broncho-alveolar lavage (BAL) as part of concurrent research or routine annual surveillance were studied. OPS was performed by stimulating a cough and suctioning the back of the oropharynx in the awake child to replicate clinical practice. BAL of the right upper, middle and lingula lobes was then performed. Samples were sent for standard bacterial culture. The child’s distress during OPS was rated using the Groningen Distress Scale (1=calm, 2=timid/nervous, 3=serious distress but still under control, 4=serious distress with loss of control, 5=panic).
There were 65 paired samples obtained from 39 children (21 boys, mean age on day of first sampling was 34.1 months, SD 19.1 months). For Pseudomonas aeruginosa, specificity, sensitivity, NPV and PPV with 95% CI were 98% (87-99), 75% (20-96), 98% (91-98) and 60% (15-93%) respectively. In all age groups combined, median level of distress was 3 (IQR 2-4), with distress highest in 2 and 3 year olds, with a median of 4 (IQR 3-4).-
The authors concluded OPS has diagnostic utility in determining the absence of organisms in the lower airway, with specificity for P. aeruginosa detection of 98%. However, a positive OPS result is not necessarily a good indicator of lower airway infection. Distress levels were high during OPS, mostly in 2 and 3 year olds. They suggest there is a need for interventions to reduce distress or to find alternative methods which are less distressing.
El Khoury J; Habre S; Nasr M; Hokayem N. Botulinum Neurotoxin A for Parotid Enlargement in Cystic Fibrosis: The First Case Report. J Oral Maxil Surg 2016; 74(9):1771-3. [PubMed]

parotid swellings in CF
The literature on submaxillary gland involvement has failed to address the parotid gland and any specific treatment

parotid swellings reduced
of salivary gland manifestations of CF. Treatment is mainly symptomatic, consisting of analgesics, gustatory stimulation, and massage. Salivary secretion has clearly been linked to parasympathetic and sympathetic signals through intracellular calcium release. CF alters salivary composition with increased calcium and phosphorus concentrations and causes histologic changes (duct enlargement, dilation of acini, and abnormal mucous plug
This study investigated whether botulinum toxin injected into the parotid gland during an acute exacerbation of CF-associated salivary gland disease could alleviate pain and control future exacerbations. A 19-year-old woman with CF had severe parotid enlargement 3 times a year for 2 years usually at the times of respiratory exacerbations. The pain and swelling resolved dramatically over a week after injection of abobotulinumtoxin A at three points of the gland. This is the first description of this treatment.
– There are impressive before and afer treatment illustrations in the article. Barbero and Sibinga first reported this complication in 1962 [see Sixties section]. Although the submandibular glands are often easily palpable symptoms are unusual.
2016 Mainz JG, Schumacher U, Schädlich K, Hentschel J, Koitschev C, Koitschev A, Riethmüller J, Prenzel F, Sommerburg O, Wiedemann B, Staab D, Gleiber W, Fischer R, Beck JF, Arnold C. Sino nasal inhalation of isotonic versus hypertonic saline (6.0%) in CF patients with chronic rhinosinusitis – Results of a multicenter, prospective, randomized, double-blind, controlled trial. J Cyst Fibros. 2016 Jun 4. pii: S1569-1993(16)30052-2. doi: 10.1016/j.jcf.2016.05.003. [Epub ahead of print] [PubMed]
Sixty nine CF patients with chronic rhino-sinusitis in eleven German CF centers were randomized to receive sinonasal vibrating inhalation of either NaCl 6.0% or NaCl 0.9% for 28days. After 28days of washout, patients crossed over to the alternative treatment. The primary outcome parameter was symptom score in the disease-specific quality of life Sino-Nasal Outcome Test-20 (SNOT-20). Additionally, pulmonary function was assessed, as well as rhinomanometry and inflammatory markers in nasal lavage (neutrophil elastase, interleukin (IL)-1β, IL-6, and IL-8) in a subgroup.Both therapeutic arms were well tolerated and showed slight improvements in SNOT-20 total scores (NaCl 6.0%: -3.1±6.5 points, NaCl 0.9%: -5.1±8.3 points, ns). In both treatment groups, changes of inflammatory parameters in nasal lavage from day 1 to day 29 were not significant. We suppose that the irritating properties of NaCl 6.0% reduced the suitability of the SNOT-20 scores as an outcome parameter. Alternative primary outcome parameters such as MR-imaging or the quantity of sinonasal secretions mobilised with both saline concentrations were, however, not feasible.
The authors concluded sinonasal inhalation with NaCl 6.0% did not lead to superior results vs. NaCl 0.9%, but recall in a previous study dornase alfa had been significantly more effective than NaCl 0.9%.
2016 Mika M, Korten I, Qi W, Regamey N, Frey U, Casaulta C, Latzin P, Hilty M; SCILD study group. The nasal microbiota in infants with cystic fibrosis in the first year of life: a prospective cohort study. Lancet Respir Med. 2016 Aug;4(8):627-35. doi: 10.1016/S2213-2600(16)30081-9. Epub 2016 May 11. [PubMed]
Between Feb 1, 2011, and May 31, 2014, the authors enrolled 30 infants with a diagnosis of cystic fibrosis. Microbiota characterisation was done with 16S rRNA gene pyrosequencing and oligotyping of nasal swabs collected every 2 weeks from the infants with cystic fibrosis. They compared these data with data for an age-matched cohort of 47 healthy infants. They additionally investigated the effect of antibiotic treatment on the microbiota of infants with cystic fibrosis.
FINDINGS. The microbiota of infants with cystic fibrosis differed compositionally from that of healthy infants (p=0·001). This difference was also found in exclusively antibiotic-naive samples (p=0·001). The disordering was mainly, but not solely, due to an overall increase in the mean relative abundance of Staphylococcaceae in infants with cystic fibrosis compared with healthy infants. Oligotyping analysis enabled differentiation between Staphylococcus aureus and coagulase-negative Staphylococci. Whereas the analysis showed a decrease in S. aureus at and after antibiotic treatment, coagulase-negative Staphylococci increased.
The authors suggest their findings could be used to inform future studies of the effect of antibiotic treatment on the microbiota in infants with cystic fibrosis, and could assist in the prevention of early disease progression in infants with this disorder.
– This study confirms a reduction in S. aureus with antibiotic treatment being supportive of the (controversial to some) recommendations of the UK CF Trust Antibiotic Group for long term flucloxacillin for the first 3 years.
2016 Prevaes SM; de Winter-de Groot KM; Janssens HM; de Steenhuijsen Piters WA; Tramper-Stranders GA; Wyllie AL; Hasrat R; Tiddens HA; van Westreenen M; van der Ent CK; Sanders EA; Bogaert D. Development of the Nasopharyngeal Microbiota in Infants with Cystic Fibrosis. Am J Resp Crit Care 2016; 193(5):504-15. [PubMed]
A study to investigate the development of nasopharyngeal microbiota profiles in infants with CF compared with those of healthy control subjects during the first 6 months of life. A prospective cohort study, from the time of diagnosis onward, in which the authors collected questionnaires and 324 nasopharynx samples from 20 infants with CF and 45 age-matched healthy control subjects. In infants with CF, early Staphylococcus aureus and, to a lesser extent, Corynebacterium spp. and Moraxella spp. dominance were followed by a switch to Streptococcus mitis predominance after 3 months of age. In control subjects, Moraxella spp. enrichment occurred throughout the first 6 months of life. In a multivariate analysis, S. aureus, S. mitis, Corynebacterium accolens, and bacilli were significantly more abundant in infants with CF, whereas Moraxella spp., Corynebacterium pseudodiphtericum and Corynebacterium propinquum and Haemophilus influenzae were significantly more abundant in control subjects, after correction for age, antibiotic use, and respiratory symptoms. Antibiotic use was independently associated with increased colonization of gram-negative bacteria such as Burkholderia spp. and members of the Enterobacteriaceae bacteria family and reduced colonization of potential beneficial commensals. From diagnosis onward, the authors observed distinct patterns of nasopharyngeal microbiota development in infants with CF under 6 months of age compared with control subjects and a marked effect of antibiotic therapy leading toward a gram-negative microbial composition.
2016Abusamra R, McShane D. Is deafness mutation screening required in cystic fibrosis patients? Paediatr Respir Rev. 2016 Aug;20 Suppl:24-6. doi: 10.1016/j.prrv.2016.06.010. Epub 2016 Jun 15.[PubMed]
Aminoglycosides are widely used in cystic fibrosis management. The m.1555A>G mutation predisposes to aminoglycoside ototoxicity. It may cause later onset hearing loss in the absence of aminoglycosides use and gradual hearing loss may be an inevitable consequence of the mutation. Given that aminoglycoside therapy forms the backbone of IV protocols in CF, these authors recommend screening for this mutation to allow informed decision-making prior to aminoglycoside administration, to avoid preventable deafness.
~Severe ototoxicity with aminoglycosides has been described in children with CF. However, it has been suggested, on the basis of only one of two children with CF and repeated aminoglycoside exposure in one series being affected, that penetrance of this pharmacologic interaction may have been overestimated (Al-Malky G et al, 2014) [Pubmed]
Janhsen WK, Arnold C, Hentschel J, Lehmann T, Pfister W, Baier M, Böer K, Hünniger K, Kurzai O, Mainz JG. Colonization of CF patients’ upper airways with S. aureus contributes more decisively to upper airway inflammation than P. aeruginosa. Microbiol Immunol 2016 Oct;205(5):485-500. doi: 10.1007/s00430-016-0463-0. Epub 2016 Jul 4.[Pubmed] In cystic fibrosis (CF) patients’ airways, inflammatory processes decisively contribute to remodelling and pulmonary destruction. The aims of this study were to compare upper airway (UAW) inflammation in the context of Staphylococcus aureus and Pseudomonas aeruginosa colonization in a longitudinal setting, and to examine further factors influencing UAW inflammation. The results indicate that UAW colonization with S. aureus significantly impacts the concentration of all measured inflammatory mediators in NL fluid except TIMP-1, whereas these effects were not significant for P. aeruginosa. Patients with S. aureus colonization of both the UAW and LAW showed significantly increased concentrations of IL-1β, IL-6, IL-8, MMP-9, and slightly elevated concentrations of NE in NL fluid compared to non-colonized patients. This work elaborates a survey on S. aureus’ virulence factors that may contribute to this underestimated pathology. Serial assessment of epithelial lining fluid by NL reveals that colonization of the UAW with S. aureus contributes more to CF airway inflammatory processes than hitherto expected.
– These results are not surprising remembering that for many years S. aureus was the main pathogen leading to fatal destruction of the lungs in children who succumbed to CF. I certainly remember such children who died in the Sixties and Seventies where S. aureus appeared to be the only pathogen. It is surprising that the presence of S. aureus is tolerated in so many CF units – but not all – for example in Copenhagen and Leeds. S. aureus can and should always be eradicated but, as in the case of Pseudomonas, this is not possible once the infection becomes chronic and well established.
Prevaes SM, de Steenhuijsen Piters WA, de Winter-de Groot KM, Janssens HM, Tramper-Stranders GA, Chu ML, Tiddens HA, van Westreenen M, van der Ent CK, Sanders EA, Bogaert D. Concordance between upper and lower airway microbiota in infants with cystic fibrosis. Eur Respir J. 2017 Mar 29;49(3). pii: 1602235. doi: 10.1183/13993003.02235-2016. Print 2017 Mar.[Pubmed]

Sabine Prevaes
Nasopharyngeal and oropharyngeal samples are commonly used to direct therapy for lower respiratory tract infections in non-expectorating infants with cystic fibrosis (CF). The authors aimed to investigate the concordance between the bacterial community compositions of 25 sets of nasopharyngeal, oropharyngeal and bronchoalveolar lavage (BAL) samples from 17 infants with CF aged ∼5 months (n=13) and ∼12 months (n=12) using conventional culturing and 16S-rRNA sequencing. Clustering analyses demonstrated that BAL microbiota profiles were in general characterised by a mixture of oral and nasopharyngeal bacteria, including commensals like Streptococcus, Neisseria, Veillonella and Rothia spp. and potential pathogens like Staphylococcus aureus, Haemophilus influenzae and Moraxella spp. Within each individual, however, the degree of concordance differed between microbiota of both upper respiratory tract niches and the corresponding BAL
The authors conclude the inconsistent intra-individual concordance between microbiota of the upper and lower respiratory niches suggests that the lungs of infants with CF may have their own microbiome that seems seeded by, but is not identical to, the upper respiratory tract microbiome.
Sabine M P J Prevaes MD, PhD, (figure) is Fellow in Pediatric Pulmonology, Clinical Researcher, University Medical Center, Utrecht, Division of Pediatrics. She has published extensively on the bacteriological aspects of cystic fibrosis.
McCormick J, Cho DY, Lampkin B, Richman J, Hathorne H, Rowe SM, Woodworth BA. Ivacaftor improves rhinologic, psychologic, and sleep-related quality of life in G551D cystic fibrosis patients.Int Forum Allergy Rhinol. 2018 Nov 24. doi: 10.1002/alr.22251. [Epub ahead of print] [Pubmed]
Ivacaftor is a cystic fibrosis transmembrane conductance regulator (CFTR) potentiator that improves pulmonary function in cystic fibrosis (CF) patients with at least 1 copy of the G551D CFTR mutation. The purpose of this study is to evaluate the impact of ivacaftor on chronic rhinosinusitis (CRS) symptoms in this population. A prospective cohort study enrolling CF patients ≥6 years with at least 1 G551D mutation. Subjects were provided 20-item Sino-Nasal Outcome Test (SNOT-20) questionnaires prior to ivacaftor therapy and at 1, 3, and 6 months afterward. The impact on rhinologic (R), psychological (P), sleep (S), and ear/facial (E) quality of life (QOL) domains was evaluated separately.
Of 153 subjects, 129 (84%) completed all questionnaires. Typical baseline symptom burden was low (75% with scores <1) and degree of improvement (ie, reduced scores) was greater with higher baseline scores. SNOT-20 decreased, reflecting improvement, at all follow-up intervals (1 month: [mean change ± standard deviation] -0.25 ± 0.53, p < 0.01; 3 months; -0.29 ± 0.58, p < 0.01; 6 months: -0.21 ± 0.58, p = 0.02), but less than the prespecified minimal clinically important difference (0.8). Significant improvement was observed at 1, 3, and 6 months in the R domain (1 month: -0.24, p < 0.01; 3 months: -0.34, p < 0.01; 6 months: -0.25, p < 0.01) and P domain (1 month: -0.25, p < 0.01; 3 months: -0.32, p < 0.01; 6 months: -0.26, p < 0.01), and 1 and 3 months in the S domain (1 months: -0.35, p < 0.01; 3 months: -0.32, p < 0.01; 6 months: -0.18, p = 0.07). There was no improvement in the E domain at any time point.
Ivacaftor improves QOL in the R, P, and S domains in G551D CF patients, although QOL instruments validated for CRS may not translate well to CF CRS patients because symptom burden was surprisingly low.
Choi KJ, Cheng TZ, Honeybrook AL, Gray AL, Snyder LD, Palmer SM, Abi Hachem R, Jang DW.Correlation between sinus and lung cultures in lung transplant patients with cystic fibrosis. Int Forum Allergy Rhinol. 2018 Mar;8(3):389-393. doi: 10.1002/alr.22067. Epub 2017 Dec 14. [Pubmed]
Infection of transplanted lungs can lead to serious complications, including graft failure and death. Although many of these patients have concurrent sinusitis, it is unclear whether bacteria from the sinuses can infect the allograft.
This is a single-institution retrospective study of all patients who underwent lung transplantation for cystic fibrosis from 2005 to 2015 at Duke University Hospital. Pre- and post-transplant nasal and pulmonary cultures obtained via nasal endoscopy and bronchoalveolar lavage (BAL), respectively, were analyzed. A total of 141 patients underwent 144 lung transplants. Sinus cultures were available for 76 patients (12 pre-transplant, 42 post-transplant, 22 both pre- and post-transplant). Pre-transplant BAL cultures were available for 139 patients, and post-transplant BAL cultures were available for all patients. Pseudomonas aeruginosa (PsA) and methicillin-resistant Staphylococcus aureus (MRSA) were the most common organisms cultured. There was a significant correlation between pre-transplant sinus and post-transplant BAL cultures for PsA (p = 0.003), MRSA (p = 0.013), and Burkholderia cepacia (p = 0.001).
There was a high correlation between pre-transplant sinus cultures and post-transplant BAL cultures for PsA, MRSA, and Burkholderia sp. This suggests that the paranasal sinuses may act as a reservoir for allograft colonization in patients with cystic fibrosis. Further studies are needed to determine whether treatment of sinusitis affects allograft colonization and transplant outcomes.
DiMango E, Overdevest J, Keating C, Francis SF, Dansky D, Gudis D. Effect of highly effective modulator treatment on sinonasal symptoms in cysticfibrosis. J Cyst Fibros. 2020 Jul 18:S1569-1993(20)30794-3. doi: 10.1016/j.jcf.2020.07.002. Online ahead of print. [Pubmed]

Emily DiMango
Elexacaftor-tezacaftor-ivacaftor is a highly effective modulator for cystic fibrosis (CF) patients homozygous or heterozygous for F508del. Effects of the drug on sinonasal symptoms have not been studied Adult participants were prospectively evaluated at baseline and after three months of treatment using validated questionnaires assessing sinonasal symptoms (SNOT-22) and CF-related quality of life (CFQ-R).
Results: Forty-three participants completed the study; 23 were taking other CF transmembrane conductance (CFTR) modulators at the time of study participation. There was a significant improvement in mean SNOT-22 from 34.8 (29.4-40, 95% confidence interval) to 24.4 (19.9-29.0) (p = 0.000003) and in the Respiratory domain of the CFQR from 60.6 (57.1-64.1) to 83.3 (79.4-87.2) (p = 0.0000002), both achieving a minimal clinically important difference. Patients previously taking CFTR modulators experienced a greater benefit in sinonasal and respiratory symptoms.
Conclusions: Elexacaftor-tezacaftor-ivacaftor is associated with significant improvement in sinonasal symptoms; previous use of CFTR modulators is associated with greater benefit
Dr Emily DiMango is Professor of Medicine at Columbia University Medical Center; Director, John Edsall-John Wood Asthma Center; Director, Adult Cystic Fibrosis Program
Dr Maarten Geurts is a PhD student at the Hubrecht Institute, Royal Netherlands Academy of Arts and Sciences (KNAW) and University Medical Center Utrecht, the Netherlands and working in the Clevers Group
Professor Hans Clevers is leader of the Clevers Group and Chief Scientific Officer/Director Research of the Princess Máxima Center for pediatric oncology, Utrecht
Gostelie R, Stegeman I, Berkers G, Bittermann J, Ligtenberg-van der Drift I, Kipshagen PV, de Winter-de Groot K, Speleman L. The impact of ivacaftor on sinonasal pathology in S1251N-mediated cysticfibrosis patients. PLoS One. 2020 Jul 20;15(7):e0235638. doi: 10.1371/journal.pone.0235638. eCollection 2020 Free article. [Pubmed]
Eight patients with cystic fibrosis with an S1251N mutation, treated with the potentiator ivacaftor were investigated. Ivacaftor (Kalydeco, VX-770) therapy. Computed tomography imaging of paranasal sinuses. Nasal nitric oxide concentration measurements and nasal endoscopy. Primary outcome is opacification of paranasal sinuses examined with computed tomography scan analysis and scaled by the modified Lund-Mackay score before and one year after treatment. Secondary outcomes are nasal nitric oxide concentration levels, sinonasal symptoms and nasal endoscopic findings before and approximately two months and in some cases one year after treatment.
Results: Computed tomography scan analysis showed a significant decrease in opacification of the majority of paranasal sinuses comparing the opacification score per paranasal sinus before and after one year of treatment with ivacaftor. Median nasal nitric oxide levels significantly improved from 220.00 (IQR:136.00-341.18) to 462.84 (IQR:233.17-636.25) (p = 0.017) parts per billion. Likewise, the majority of sinonasal symptoms and nasal endoscopic pathology decreased or resolved at two months after the use of ivacaftor.
Conclusion and relevance: Ivacaftor appears to improve sinonasal outcome parameters and thereby sinonasal health in patients with cystic fibrosis with an S1251N mutation.
Fromm the University Medical Center, Utrecht University, Utrecht, The Netherlands.
Cristina de Manuel Gómez, Ana Cecilia Morales Palacios, Olga de la Serna Blázquez, Pablo Vicente Morillo Carnero, María Elena Pérez Arenas, Sonia Milkova Ivanova, Marta Ruiz de Valbuena Maiz. Ethmoidal mucocele causing proptosis in a pediatric patient with cystic fibrosis: A case report. J Cyst Fibros 2022 Mar 1;S1569-1993(22)00048-0.doi: 10.1016/j.jcf.2022.02.016. Online ahead of print.35246383
In cystic fibrosis (CF) patients, Ear Nose Throat (ENT) pathology is often undiagnosed despite its high prevalence and its possible life-threatening complications. We present the case of an ethmoidal mucocele leading to ocular manifestations in a 2-year-old girl with cystic fibrosis with no previous serious complications. She progressively developed non-axial proptosis, limitation of the adduction and exotropia of her left eye. Paranasal sinus magnetic resonance image (MRI) showed a left ethmoidal mucocele causing displacement of the ocular globe, compression of the medial rectus and the optic nerve. Eye fundus revealed disc edema and diffuse vascular congestion. Endoscopic sinus surgery was performed to remove the mass. The mucocele was drained and the discharge was sent for microbiology assessment. Escherichia coli (E. coli) was found in the culture and treated with cefotaxime and dexamethasone with complete resolution of non-axial proptosis and disc edema.
Cristina de Manuel Gómez is in the Pediatric Pulmonology and Cystic Fibrosis Unit, Hospital Universitario La Paz, Madrid.
Amanda L Stapleton, Adam J Kimple, Jennifer L Goralski, S Mehdi Nouraie, Barton F Branstetter, Amber D Shaffer, Joseph M Pilewski, Brent A Senior, Stella E Lee, Anna C Zemke. Elexacaftor-Tezacaftor- Ivacaftor improves sinonasal outcomes in cystic fibrosis. J Cyst Fibros 2022 Mar 14;S1569-1993(22)00051-0.doi: 10.1016/j.jcf.2022.03.002.Online ahead of print. Free article [Pubmed]

Amanda Stapleton
Background: Many individuals with cystic fibrosis (CF) have chronic rhinosinusitis resulting in nasal obstruction, sinus infections, and repeated surgeries. Elexacaftor-tezacaftor-ivacaftor is a highly effective modulator therapy approved for individuals aged 6 years or older with CF who have at least one F508del allele or other responsive mutation. The current study tests the hypothesis that ELX/TEZ/IVA improves sinonasal disease in CF.
Methods: The study was a pre/post, observational cohort study conducted at two sites. Participants underwent a study visit prior to starting ELX/TEZ/IVA and a second visit at a median of 9 months on therapy. Each visit included sinus CT scan, rigid nasal endoscopy, and sweat chloride measurement. Symptoms were measured with the 22 item Sinonasal Outcome Test at scheduled intervals during the study. Regression models were used to test for improvement in symptoms, endoscopy, and CT scales.
Results: The study enrolled 34 individuals, with a median age of 27 years (range 12-60). Symptoms improved within 7 days of therapy and plateaued by day 28. Endoscopic crusting resolved and nasal polyposis improved, with a decrease in size or resolution of polyps. Sinus opacification and mucosal thickening improved on CT radiographs with treatment.
Conclusions: Sinonasal symptoms improved rapidly and durably for at least 180 days on ELX/TEZ/IVA therapy. Objective measures of disease including endoscopic and CT findings improved with ELX/TEZ/IVA.
Dr Amanda L Stapleton is Associate Professor in the Department of Otolaryngology – Head and Neck Surgery, University of Pittsburgh, United States.
Lena Wucherpfennig, Simon M F Triphan, Sabine Wege, Hans-Ulrich Kauczor, Claus P Heussel, Niclas Schmitt, Felix Wuennemann, Victoria L Mayer, Olaf Sommerburg, Marcus A Mall, Monika Eichinger, Mark O WielpützMagnetic resonance imaging detects improvements of pulmonary and paranasal sinus abnormalities in response to elexacaftor/tezacaftor/ivacaftor therapy in adults with cystic fibrosis. J Cyst Fibros 2022 Apr 7;S1569-1993(22)00088-1.: 10.1016/j.jcf.2022.03.011.Online ahead of print.[Pubmed]

Lena Wucherpfennig
Background: Therapy with Elexacaftor/Tezacaftor/Ivacaftor (ETI) was recently approved for adult cystic fibrosis (CF) patients with at least one F508del mutation. However, its effects on structural and functional lung abnormalities and chronic rhinosinusitis have not been studied by imaging.
Methods: 19 adults with CF (mean age 31±9y, range 19-55y) underwent standardized chest magnetic resonance imaging (MRI), and nine also same-session sinonasal MRI, before (MRI1) and after (MRI2) at least one month (mean duration 5 ± 3mon) on ETI. 24 control CF patients (30±7y, range 20-44y) without ETI underwent longitudinal chest MRI, and eleven also sinonasal MRI, twice (mean interval 40±15mon). MRI was assessed using the validated chest MRI score and chronic rhinosinusitis (CRS)-MRI score. Forced expiratory volume in 1 s percent predicted (FEV1%) was measured in all patients.
Results: In controls, the chest MRI global score and CRS-MRI sum score were stable from MRI1 to MRI2. In patients under ETI, the chest MRI global score improved (-11.4 ± 4.6, P<0.001), mainly due to reduction of bronchiectasis/wall thickening and mucus plugging subscores (-3.3 ± 2.2 and -5.2 ± 1.5, P<0.001, respectively). The improvement in chest MRI score correlated well with improved FEV1% (r=-0.703, P<0.001). The CRS-MRI sum score also improved in patients under ETI (-6.9 ± 3.0, P<0.001), mainly due to a reduction of mucopyoceles in the maxillary and ethmoid sinus (-50% and -39%, P<0.05, respectively).
Conclusions: MRI detects improvements of chest MRI and CRS-MRI scores in adult CF patients who first received ETI, demonstrating reversibility of structural lung and paranasal sinus abnormalities in patients with established disease.
Dr Lena Wucherpfennig is in the Department of Diagnostic and Interventional Radiology, Subdivision of Pulmonary Imaging, University Hospital Heidelberg, Im Neuenheimer Feld 420, 69120 Heidelberg, Germany; Translational Lung Research Center Heidelberg (TLRC), German Center for Lung Research (DZL), Im Neuenheimer Feld 156, 69120 Heidelberg, Germany; Department of Diagnostic and Interventional Radiology with Nuclear Medicine, Thoraxklinik at University Hospital Heidelberg, Röntgenstr. 1, 69126 Heidelberg, Germany.
