– THIS SECTION CONTAINS A VARIETY OF PUBLICATIONS RELATING TO THE VARIOUS MODULATORS, NOT ONLY WITH REGARD TO RESPIRATORY FUNCTION BUT ALSO EFFECTS ON OTHER SYSTEMS SUCH AS THE CVS, PANCREAS, LIVER ETC.
THE ABSTRACTS ARE PRESENTED IN CHRONOLOGICAL ORDER IN TWO SECTIONS
=============================================================
– IMPORTANT TRIALS OF SPECIFIC MODULATORS OR COMBINATIONS ARE ALSO ABSTRACTED AGAIN IN THE SECTIONS ON SPECIFIC MODULATORS AS FOLLOWS
VX-770 (IVACAFTOR)
VX-809 (LUMACAFTOR)
VX-770 + VX-809 (ORKAMBI)
VX-661 (TEZACAFTOR)
VX-661 (TEZACAFTOR) + VX-770 (IVACAFTOR) (SYMDEKO)
TEZACAFTOR (VX-661) + IVACAFTOR (VX-770) + VX-440
TEZACAFTOR (VX-661) + IVACAFTOR (VX-770) + VX-659
TEZACAFTOR (VX-661) + IVACAFTOR (VX-770) + ELEXACAFTOR (VX-445) = TRIKAFTA
OTHER NEW THERAPY
=================================================================================
ALL PUBLICATIONS RELATING TO MODULATORS
IN CHRONOLOGICAL ORDER BY YEAR AND ALPHABETICAL BY FIRST AUTHOR IN INDIVIDUAL YEARS
SECTION ONE – CONTAINS REFERENCES UP TO AND INCLUDING 2020
2009 Van Goor F, Hadida S, Grootenhuis PD, Burton B, Cao D, Neuberger T, Turnbull A, Singh A, Joubran J, Hazlewood A, Zhou J, McCartney J, Arumugam V, Decker C, Yang J, Young C, Olson ER, Wine JJ, Frizzell RA, Ashlock M, Negulescu P.Rescue of CF airway epithelial cell function in vitro by a CFTR potentiator, VX-770. Proc Natl Acad Sci U S A. 2009; 106(44):18825-30. [PubMed]Free article available

Frederick van Goor
The authors describe the in vitro pharmacology of VX-770, an orally bioavailable CFTR potentiator in clinical development for the treatment of CF. In recombinant cells VX-770 increased CFTR channel open probability (P(o)) in both the F508del processing mutation and the G551D gating mutation. VX-770 also increased Cl(-) secretion in cultured human CF bronchial epithelia (HBE) carrying the G551D gating mutation on one allele and the F508del processing mutation on the other allele by approximately 10-fold, to approximately 50% of that observed in HBE isolated from individuals without CF. Furthermore, VX-770 reduced excessive Na(+) and fluid absorption to prevent dehydration of the apical surface and increased cilia beating in these epithelial cultures.
These results support the hypothesis that pharmacological agents that restore or increase CFTR function can rescue epithelial cell function in human CF airway.
2010 2010 2010
2010 Accurso FJ, Rowe SM, Clancy JP, Boyle MP, Dunitz JM, Durie PR, Sagel SD, Hornick DB, Konstan MW, Donaldson SH, Moss RB, Pilewski JM, Rubenstein RC, Uluer AZ, Aitken ML, Freedman SD, Rose LM, Mayer-Hamblett N, Dong Q, Zha J, Stone AJ, Olson ER, Ordonez CL, Campbell PW, Ashlock MA, Ramsey BW. Effect of VX-770 in persons with cystic fibrosis and the G551D-CFTR mutation. VX-770, a CFTR potentiator, has been shown to increase the activity of wild-type and defective cell-surface CFTR in vitro.New Engl J Med. 2010; 363:1991-2003. [PubMed]

Frank Accurso
39 adults with cystic fibrosis and at least one G551D-CFTR allele received oral VX-770 every 12 hours at a dose of 25, 75, or 150 mg or placebo for 14 days (in part 1 of the study) or VX-770 every 12 hours at a dose of 150 or 250 mg or placebo for 28 days (in part 2 of the study). At day 28, in the group of subjects who received 150 mg of VX-770, the median change in the nasal potential difference (in response to the administration of a chloride-free isoproterenol solution) from baseline was -3. 5 mV (range, -8. 3 to 0. 5; P=0.02 for the within-subject comparison, P=0.13 vs. placebo), and the median change in the level of sweat chloride was -59. 5 mmol per liter (range, -66. 0 to -19. 0; P=0.008 within-subject, P=0.02 vs. placebo). The median change from baseline in the percent of predicted forced expiratory volume in 1 second was 8. 7% (range, 2. 3 to 31. 3; P=0. 008 for the within-subject comparison, P=0. 56 vs. placebo). None of the subjects withdrew from the study. Six severe adverse events occurred in two subjects (diffuse macular rash in one subject and five incidents of elevated blood and urine glucose levels in one subject with diabetes). All severe adverse events resolved without the discontinuation of VX-770.
The authors concluded that this study to evaluate the safety and adverse-event profile of VX-770 showed that VX-770 was associated with within-subject improvements in CFTR and lung function. These findings provide support for further studies of pharmacologic potentiation of CFTR as a means to treat cystic fibrosis.
– The results of this phase II trial of VX-770, confirmed it to be one of the most significant advances up to the present time in increasing CFTR function and with obvious beneficial changes in respiratory function and even normalisation of the abnormal sweat electrolyte levels. Subsequent Phase III trials (below) fully confirmed that this was indeed a major advance for those people with CF who had at least one G551D mutation – in the UK 5.8% of people with CF.
The drug named Kalydeco (generic name ivacaftor, previously known as VX-770) was approved for clinical use in January 2012 in the USA although it is likely that the cost would prove a problem. Suggested annual cost could be $294,000 per year.
2011 2011 2011
2011 Ramsey BW, Davies J, McElvaney NG, Tullis E, Bell SC, Drevinek P, Griese M, McKone EF, Wainwright CE, Konstan MW, Moss R, Ratjen F, Sermet Gaudelus I, Rowe SM, Dong Q, Rodriguez S, Yen K, Ordonez C, Elborn JS. VX08-770-102 Study Group. A CFTR potentiator in patients with cystic fibrosis and the G551D mutation. New Engl J Med 2011; 365:1663-72 .[PubMed] Free article available

Bonnie Ramsey
This is the main report of a randomized, double-blind, placebo-controlled trial to evaluate Ivacaftor (VX-770), a CFTR potentiator, in subjects 12 years of age or older with CF and at least one G551D-CFTR mutation. Subjects were randomly assigned to receive 150 mg of ivacaftor every 12 hours (84 subjects, of whom 83 received at least one dose) or placebo (83, of whom 78 received at least one dose) for 48 weeks. The primary end point was the estimated mean change from baseline through week 24 in the percent of predicted forced expiratory volume in 1 second (FEV(1)).
RESULTS: The change from baseline through week 24 in the percent of predicted FEV(1) was greater by 10.6 percentage points in the Ivacaftor group than in the placebo group (P<0.001). Effects on pulmonary function were noted by 2 weeks, and a significant treatment effect was maintained through week 48. Subjects receiving Ivacaftor were 55% less likely to have a pulmonary exacerbation than were patients receiving placebo, through week 48 (P<0.001). In addition, through week 48, subjects in the ivacaftor group scored 8.6 points higher than did subjects in the placebo group on the respiratory-symptoms domain of the Cystic Fibrosis Questionnaire-revised instrument (a 100-point scale, with higher numbers indicating a lower effect of symptoms on the patient’s quality of life) (P<0.001). By 48 weeks, patients treated with Ivacaftor had gained, on average, 2.7 kg more weight than had patients receiving placebo (P<0.001). The change from baseline through week 48 in the concentration of sweat chloride, a measure of CFTR activity, with Ivacaftor as compared with placebo was -48.1 mmol per liter (P<0.001). The incidence of adverse events was similar with ivacaftor and placebo, with a lower proportion of serious adverse events with Ivacaftor than with placebo (24% vs. 42%).
The authors concluded that Ivacaftor was associated with improvements in lung function at 2 weeks that were sustained through 48 weeks. Substantial improvements were also observed in the risk of pulmonary exacerbations, patient-reported respiratory symptoms, weight, and concentration of sweat chloride.
– This is one of the most important papers of recent years, undoubtedly a “megapaper”, and represents the first successful small molecule correction of the effects of a specific CF gene mutation, G551D. It is the first such treatment of the basic defect that has significantly changed the abnormal sweat chloride concentration in addition to favourably influencing the clinical condition of the treated patients.
2011 Van Goor F, Hadida S, Grootenhuis PD, Burton B, Stack JH, Straley KS, Decker CJ, Miller M, McCartney J, Olson ER, Wine JJ, Frizzell RA, Ashlock M, Negulescu PA. Correction of the F508del-CFTR protein processing defect in vitro by the investigational drug VX-809. Proc Nat Acad Sci USA 2011; 108:18843-84. [PubMed]
The authors describe the in vitro pharmacology of VX-809, a CFTR corrector. In cultured human bronchial epithelial cells isolated from patients with CF homozygous for F508del, VX-809 improved F508del-CFTR processing in the endoplasmic reticulum and enhanced chloride secretion to approximately 14% of non-CF human bronchial epithelial cells, a level associated with mild CF. F508del-CFTR corrected by VX-809 exhibited biochemical and functional characteristics similar to normal CFTR. VX-809 represents a class of CFTR corrector that specifically addresses the underlying processing defect in F508del-CFTR.
– As DF508 is the most frequent CF mutation it is hoped that this corrector will be as therapeutically active as indicated in these studies as it is likely that even 14% of normal CFTR activity will ameliorate the main symptoms associated with complete absent CFTR activity. However, the corrector does not seem to have the same dramatic effect on DF508 as VX-770 has on the G551D mutation. However, the results of VX-770 in patients with the GF551D mutation added great impetus to the small molecule corrector research and there is now major investment in this area by pharmaceutical companies and the CF Foundation.
2012 2012 2012
2012 Clancy JP. Rowe SM. Accurso FJ. Aitken ML. Amin RS. Ashlock MA. Ballmann M. Boyle MP. Bronsveld I. Campbell PW. De Boeck K. Donaldson SH. Dorkin HL. Dunitz JM. Durie PR. Jain M. Leonard A. McCoy KS. Moss RB. Pilewski JM. Rosenbluth DB. Rubenstein RC. Schechter MS. Botfield M. Ordonez CL. Spencer-Green GT. Vernillet L. Wisseh S. Yen K. Konstan MW. Results of a phase IIa study of VX-809, an investigational CFTR corrector compound, in subjects with cystic fibrosis homozygous for the F508del-CFTR mutation. Thorax 2012; 67:12-18. [PubMed]

John Clancy
VX-809,(lumacaftor), a cystic fibrosis transmembrane conductance regulator (CFTR) modulator, has been shown to increase the cell surface density of functional F508del-CFTR in vitro. This randomised, double-blind, placebo-controlled study evaluated the safety, tolerability and pharmacodynamics of VX-809 in adult patients with cystic fibrosis (n=89) who were homozygous for the F508del-CFTR mutation. Subjects were randomised to one of four VX-809 28 day dose groups (25, 50, 100 and 200 mg) or matching placebo. The type and incidence of adverse events were similar among VX-809- and placebo-treated subjects. Respiratory events were the most commonly reported and led to discontinuation by one subject in each active treatment arm. Pharmacokinetic data supported a once-daily oral dosing regimen. Pharmacodynamic data suggested that VX-809 improved CFTR function in at least one organ (sweat gland). VX-809 reduced elevated sweat chloride values in a dose-dependent manner (p=0.0013) that was statistically significant in the 100 and 200 mg dose groups.
There was no statistically significant improvement in CFTR function in the nasal epithelium as measured by nasal potential difference, nor were there statistically significant changes in lung function or patient-reported outcomes. No maturation of immature F508del-CFTR was detected in the subgroup that provided rectal biopsy specimens.
The authors concluded that VX-809 had a similar adverse event profile to placebo for 28 days in F508del-CFTR homozygous patients, and demonstrated biological activity with positive impact on CFTR function in the sweat gland. Additional data are needed to determine how improvements detected in CFTR function secondary to VX-809 in the sweat gland relate to those measurable in the respiratory tract and to long-term measures of clinical benefit
2012 Yu H, Burton B, Huang CJ, Worley J, Cao D, Johnson JP Jr, Urrutia A, Joubran J, Seepersaud S, Sussky K, Hoffman BJ, Van Goor F. Ivacaftor potentiation of multiple CFTR channels with gating mutations. J Cyst Fibros. 2012;11:237-45. [PubMed]
Ivacaftor potentiated multiple mutant CFTR forms with defects in CFTR channel gating. These included the G551D, G178R, S549N, S549R, G551S, G970R, G1244E, S1251N, S1255P and G1349D CFTR gating mutations. The authors concluded that these in vitro data suggest that ivacaftor has a similar effect on all CFTR forms with gating defects and support investigation of the potential clinical benefit of ivacaftor in CF patients who have CFTR gating mutations beyond G551D.
2013 2013 2013
2013 Bellin MD. Laguna T. Leschyshyn J. Regelmann W. Dunitz J. Billings J. Moran A. Insulin secretion improves in cystic fibrosis following ivacaftor correction of CFTR: a small pilot study. Pediatr Diabetes 2013; 14:417-421. [PubMed]
An open-label pilot study in CF patients with the G551D mutation given new prescriptions for ivacaftor (VX-770). At baseline and 4wk after daily ivacaftor therapy, intravenous glucose tolerance tests (IVGTT) and oral glucose tolerance tests (OGTT) were performed.
Five patients aged 6-52 were studied. After 1month on ivacaftor, the insulin response to oral glucose improved by 66-178% in all subjects except one with long-standing diabetes. OGTT glucose levels were not lower in the two individuals with diabetes or the two with normal glucose tolerance (NGT), but the glucose tolerance category in the subject with impaired glucose tolerance (IGT) improved to NGT after treatment. In response to intravenous glucose, the only patient whose acute insulin secretion did not improve had newly diagnosed, untreated CFRD. The others improved by 51-346%. Acute insulin secretion was partially restored in two subjects with no measurable acute insulin response at baseline, including the one with IGT and the one with long-standing diabetes.
The authors concluded the results suggest there is a direct role of CFTR in human insulin secretion. Larger, long-term longitudinal studies are necessary to determine whether early initiation of CFTR correction, particularly in young children with CF who have not yet lost considerable beta-cell mass, will delay or prevent development of diabetes.
– These are really important results. The prevention of CF related diabetes would represent a major advance in improving the health and quality of life of the majority of adults with CF most of whom will eventually develop CF related diabetes mellitus
2013 Davies JC, Wainwright CE, Canny GJ, Chilvers MA, Howenstine MS, Munck A, Mainz JG, Rodriguez S, Li H, Yen K, Ordonez CL, Ahrens R. VX08-770-103 (ENVISION) Study Group. Efficacy and safety of ivacaftor in patients aged 6 to 11 years with cystic fibrosis with a G551D mutation. Am J Resp Crit Care 2013; 187:1219-25. [PubMed]

Jane Davies
Children received oral ivacaftor 150 mg (n = 26) or placebo (n = 26) every 12 hours for 48 weeks. Despite near-normal mean baseline values in FEV1, patients receiving ivacaftor had a significant increase in percent predicted FEV1 from baseline through Week 24 versus placebo group (treatment effect, 12.5 percentage points; P < 0.001). Effects on pulmonary function were evident by 2 weeks, and a significant treatment effect was maintained through Week 48. Patients treated with ivacaftor gained, on average, 2.8 kg more than those receiving placebo at Week 48 (P < 0.001). The change from baseline through Week 48 in the concentration of sweat chloride, a measure of CFTR activity, with ivacaftor was -53.5 mmol/L (P < 0.001) versus placebo. The incidence of adverse events was similar in the two groups.
These quite dramatic results further confirm the very significant benefit from ivacaftor even in those children with a G551D mutation who have normal or near normal respiratory function. The authors concluded that in patients who are younger and healthier than those in previously studied populations, ivacaftor demonstrated a significant improvement in pulmonary function, weight, and CFTR activity compared with placebo.
– These trials reporting the effects of ivacaftor in adults and here in children must surely be the most sensational and important publications that have appeared to date relating to the treatment of CF.
2013 Davies J, Sheridan H, Bell N, Cunningham S, Davis SD, Elborn JS, Milla CE, Starner TD, Weiner DJ, Lee PS, Ratjen F. Assessment of clinical response to ivacaftor with lung clearance index in cystic fibrosis patients with a G551D-CFTR mutation and preserved spirometry: a randomised controlled trial. Lancet Respir Med. 2013 Oct;1(8):630-8. [PubMed]
Lung clearance index (LCI) using multiple-breath washout might be an alternative to and more sensitive method than forced expiratory volume in 1 s (FEV1) to assess treatment response in the growing number of children and young adults with cystic fibrosis who have normal spirometry. The aim of the study was to assess the treatment effects of ivacaftor on LCI in patients with cystic fibrosis, a G551D-CFTR mutation, and an FEV1 >90% predicted
This phase 2, multicentre, placebo-controlled, double-blind 2×2 crossover study of ivacaftor treatment was conducted in patients with cystic fibrosis, at least one G551D-CFTR allele, and an FEV1 >90% predicted. Patients also had to have an LCI higher than 7·4 at screening, age of 6 years or older, and a weight higher than or equal to 15 kg. Eligible patients were randomly allocated to receive one of two treatment sequences (placebo first followed by ivacaftor 150 mg twice daily [sequence 1] or ivacaftor 150 mg twice daily first followed by placebo [sequence 2]) of 28 days’ treatment in each period, with a 28-day washout between the two treatment periods. Randomisation (ratio 1:1) was done with block sizes of 4, and all site personnel including the investigator, the study monitor, and the Vertex study team were masked to treatment assignment. The primary outcome measure was change from baseline in LCI. .
Between February and November, 2011, 21 patients were enrolled., Treatment with ivacaftor led to significant improvements compared with placebo in LCI (difference between groups in the average of mean changes from baseline at days 15 and 29 was -2·16 [95% CI -2·88 to -1·44]; p<0·0001).
– In patients with cystic fibrosis aged 6 years or older who have at least one G551D-CFTR allele, ivacaftor led to improvements in LCI. The authors suggest tha LCI might be a more sensitive alternative to FEV1 in detecting response to intervention in these patients with mild lung disease.
2013 Durmowicz AG. Witzmann KA. Rosebraugh CJ. Chowdhury BA. Change in sweat chloride as a clinical end point in cystic fibrosis clinical trials: the ivacaftor experience. Chest 2013; 143:14-18. [PubMed]
A clinical trial performed to support ivacaftor dose selection demonstrated a dose-response relationship between improvement in FEV(1) and decrease in sweat chloride, a measure of CFTR function. Validation of such a relationship between FEV(1) and sweat chloride would facilitate development of new drugs that target the defective CFTR. Subsequently, in phase 3 studies, ivacaftor 150 mg bid resulted in significant improvements in FEV(1) (10%-12%) and reduction in sweat chloride (approximately 50 mmol/L). However, a decrease in sweat chloride did not correlate with improvement in FEV(1), nor did there appear to be a threshold level for change in sweat chloride above which an improvement in FEV(1) was apparent.
The lack of correlation of sweat chloride with improvement in FEV(1) speaks to the multiplicity of factors, physiologic, environmental, and genetic, that likely modulate CF disease severity. Future clinical trials of drugs that are directed to the defective CFTR will need take into account the uncertainty of using even established measurements, such as sweat chloride, as clinical end points.
– Ivacaftor is the first drug to alter the abnormal sweat electrolytes in people with CF. However, the numerous variables which influence the FEV make it unlikely that this single measure will be an accurate reflection of the effect of ivacaftor.
2013 Grasemann H, Ratjen F, Solomon M. Aquagenic wrinkling of the palms in a patient with cystic fibrosis. N Engl J Med. 2013 Dec 12;369(24):2362-3. doi: 10.1056/NEJMc1308349. [PubMed]

Hatmut Grasemann
An 11-year-old patient with cystic fibrosis (CFTR genotype F508del/G551D) who received maintenance therapy with other drugs for cystic fibrosis in addition to ivacaftor. Aquagenic wrinkling of his palms was assessed by putting his left hand into a water bath at 37°C for 5 minutes before treatment and after 1 month of treatment. Although considerable wrinkling was observed at baseline, the phenomenon had resolved after treatment. In parallel, the patient’s sweat chloride concentrations decreased from 90 mmol per liter before treatment to 32 mmol per liter after treatment
– The authors comment that their findings show that CFTR-directed therapy had an effect on aquagenic wrinkling in a patient with cystic fibrosis and indicate an association of this phenomenon with CFTR dysfunction. Ivacaftor trials have shown considerable variability in treatment response when it is assessed according to the sweat chloride and nasal potential difference, two distinct measures of CFTR function. As new CFTR-directed therapies are being explored, additional measures of CFTR function could help to better capture the individual variability in response. Their observation related to ivacaftor therapy raises the potential that aquagenic wrinkling of the palms could serve as an additional and simple test of CFTR function to monitor the success of drug treatment although this seems unlikely
Helge Hebestreit, Annette Sauer-Heilborn, Rainald Fischer, Manfred Käding, Jochen G Mainz. Effects of inacaftor on severely ill patients carrying a G551D mutation. J Cyst Fibros. 2013; 12:599-603. doi: 10.1016/j.jcf.2013.05.006. Epub 2013 Jun 10.[PubMed]
Data from 14 severely affected patients with a FEV1 <40% predicted who received ivacaftor on a “named patient program” basis in Germany were analyzed. One patient took ivacaftor at a lower than recommended dose due to abundant mucus and a feeling to “suffocate.” No additional severe adverse events were reported. One further patient stopped ivacaftor due to lung transplantation, one due to perceived poor effectiveness, one due to pregnancy, and one stopped standard therapy. The remaining patients took ivacaftor regularly and did not change other therapies. FEV1 increased by more than 5% predicted in 5 of the 14 patients from baseline (average FEV1 during the year prior to ivacaftor). On average, FEV1 increased significantly by 5.2±5.6%predicted (p<0.01). The relative improvement in FEV1 was 19.7±22.1%.
– So ivacaftor was effective in many patients with poor lung function. The response was, however, variable. Although the drug appeared safe for most of these patients, increased bronchial secretions may warrant intensified physiotherapy and intravenous antibiotic treatment when ivacaftor is initiated.
2013 Harrison MJ, Murphy DM, Plant BJ. Ivacaftor in a G551D homozygote with cystic fibrosis.N Engl J Med. 2013 Sep 26;369(13):1280-2. doi: 10.1056/NEJMc1213681. [PubMed]
A report on the use of ivacaftor in a 19-year-old woman who was homozygous for the G551D mutation. After a period of progressive deterioration with recurrent infective exacerbations (seven separate courses of intravenous antibiotics in the previous 12 months), the baseline FEV1 had decreased to 24% of the predicted value, she had become dependent on oxygen, and she was referred for assessment for lung transplantation. Simultaneously, ivacaftor therapy was initiated. Within 8 weeks, the FEV1 had increased to 35% of the predicted value, continuous oxygen was discontinued with a resting oxygen saturation of 95% (it was previously 85%) while the patient was breathing ambient air, and assessment for transplantation was deferred. Prospectively, over the subsequent 12 months of therapy, she required one course of intravenous antibiotics, the FEV1 increased by 16 percentage points (from 24 to 40% of the predicted value), the sweat chloride level decreased from 92 mmol per liter to 18 mmol per liter, the 6-minute walk distance increased by 410 m (from 140 to 550 m), and the weight increased by 8.4 kg (from 42.0 to 50.4 kg). In addition, the serum albumin level increased from 3.3 g per deciliter to 4.5 g per deciliter, and the daily consumption of pancreatic-enzyme supplements decreased by approximately 60%.
In the VX08-770-105 clinical-trial cohort of patients who were heterozygous for the G551D mutation, the improvements in sweat chloride levels and the FEV1 reached a plateau after 2 weeks. To date, the authors have not found a plateau effect with ivacaftor therapy in the G551D homozygous patient. The progressive reduction and normalization of the sweat chloride level (a marker of CFTR dysfunction), coupled with the continued clinical improvements in lung function, weight, and walk distance throughout the 12-month follow-up period provide support for the increased efficacy of ivacaftor in homozygous versus heterozygous patients.
So improvement in this particular patient did not plateau after 2 weeks in this lady homozygous for G551D as is the case in heterozygotes for G551D. The results from other patients homozygous for G551D are awaited.
2013 Hebestreit H, Sauer-Heilborn A, Fischer R, Käding M, Mainz JG. Effects of ivacaftor on severely ill patients with cystic 2013 Farinha CM. King-Underwood J. Sousa M. Correia AR. Henriques BJ. Roxo-Rosa M. Da Paula AC. Williams J. Hirst S. Gomes CM. Amaral MD. Revertants, Low Temperature, and Correctors Reveal the Mechanism of F508del-CFTR Rescue by VX-809 and Suggest Multiple Agents for Full Correction. Chem Biol 2013; 20:943-55. [PubMed]
Cystic fibrosis is mostly caused by the F508del mutation, which impairs CFTR protein from exiting the endoplasmic reticulum due to misfolding. VX-809 (lumacaftor) is a small molecule that rescues F508del-CFTR localization, which recently went into clinical trial but with unknown mechanism of action (MoA). Herein, the authors assessed if VX-809 is additive or synergistic with genetic revertants of F508del-CFTR, other correctors, and low temperature to determine its MoA. They explored and integrated those various agents in combined treatments, showing how they add to each other to identify their complementary MoA upon correction of F508del-CFTR.
The authors’ experimental and modeling data, while compatible with putative binding of VX-809 to NBD1:ICL4 interface, also indicate scope for further synergistic F508del-CFTR correction by other compounds at distinct conformational sites/cellular checkpoints, thus suggesting requirement of combined therapies to fully rescue F508del-CFTR.
2013 Ivacaftor. Uncertain harm-benefit balance. [No authors listed] Prescrire Int 2013; 142:229-31.[PubMed]
Ivacaftor is described as a selective potentiator of CFTR protein. It is now licensed for the treatment of cystic fibrosis patients 6 years of age and older who carry the CFTR G551D mutation, which is the case for about 4% to 5% of cystic fibrosis patients. Two randomised placebo-controlled trials of ivacaftor have been carried out in this setting, in a total of 213 patients. The frequency of pulmonary exacerbations fell in one of the two trials during the first 48 weeks of treatment, but there was no impact on the number of hospitalisations or the use of intravenous antibiotics. In both trials, addition of ivacaftor improved FEV1 by an average of about 10% at week 24 and increased body weight by an average of about 2.5 kg after 1 year. Upper respiratory tract infections occurred in the ivacaftor groups during these trials, with more cases of bacterial contamination and, possibly, more pulmonary exacerbations in the longer term.
The authors warn that Ivacaftor carries a risk of numerous pharmacokinetic interactions that can require dose adjustment, particularly for patients with hepatic impairment and those receiving cytochrome P450 isozyme 3A inhibitors or inducers. Given the absence of data, ivacaftor should be avoided during pregnancy. In practice, in 2013, it is not possible to determine the harm-benefit balance of ivacaftor due to the high risk of drug interactions, as well as a possible increased risk of infections and liver toxicity.
– So here is a word of caution regarding the use of ivacaftor.
2013 McGarry ME. Nielson DW. Normalization of sweat chloride concentration and clinical improvement with ivacaftor in a patient with cystic fibrosis with mutation S549N.Chest 2013; 144:1376-8. [PubMed]
There are 10 known class 3 gating mutations, the most common of which is G551D. Ivacaftor is a drug that in vitro increases open time and transepithelial chloride transport in all 10 gating mutations, but it is approved for use only in patients with the G551D mutation. The authors report complete normalization of sweat chloride concentration and rapid clinical improvement over 6 weeks of treatment with ivacaftor in a patient with CF with the gating mutation S549N. They suggest that ivacaftor should be considered for use in patients with any of the known gating mutations.
2013 Polenakovik HM. Sanville B. The use of ivacaftor in an adult with severe lung disease due to cystic fibrosis (F508/G551D). J Cyst Fibros 2013; 12:530-1. [PubMed]
An adult with cystic fibrosis (F508/G551D) with severe lung disease (forced expiratory volume (FEV1) in one second 24% predicted) was admitted for a pulmonary exacerbation. He was managed with maximal medical therapy, but did not have significant improvement until after he was started on ivacaftor on hospital day 15. He subsequently had significant improvement in lung function with normalization of hypercarbia, oxygen saturation on room air, and increase in FEV1 to 36% predicted. Prior to use of ivacaftor he was being assessed for a lung transplant. However, after ivacaftor therapy for 6 months, he is no longer considering this treatment modality due to his improvement of lung function and functional status.
– One of a number of reports of impressive improvement with ivacaftor in patients with severely affected chests.
2013 Ren HY. Grove DE. De La Rosa O. Houck SA. Sopha P. Van Goor F. Hoffman BJ. Cyr DM. VX-809 corrects folding defects in cystic fibrosis transmembrane conductance regulator protein through action on membrane-spanning domain 1. Mol Biol Cell 2013; 24:3016-24. [PubMed]

Clement L Ren
CFTR contains two membrane-spanning domains (MSDs), two nucleotide-binding domains (NBDs), and a regulatory domain, and its channel assembly requires multiple interdomain contacts. The most common CF-causing mutation, F508del, occurs in NBD1 and results in misfolding and premature degradation of F508del-CFTR. VX-809 is an investigational CFTR corrector that partially restores CFTR function in people who are homozygous for F508del-CFTR. To identify the folding defect(s) in F508del-CFTR that must be repaired to treat CF, the authors explored the mechanism of VX-809 action. VX-809 stabilized an N-terminal domain in CFTR that contains only MSD1 and efficaciously restored function to CFTR forms that have missense mutations in MSD1. The action of VX-809 on MSD1 appears to suppress folding defects in F508del-CFTR by enhancing interactions among the NBD1, MSD1, and MSD2 domains. The ability of VX-809 to correct F508del-CFTR is enhanced when combined with mutations that improve F508del-NBD1 interaction with MSD2.
The authors suggest that the use of VX-809 in combination with an additional CFTR corrector that suppresses folding defects downstream of MSD1 may further enhance CFTR function in people with F508del-CFTR.
2013 Seliger V, Rodman D, Van Goor F, Schmelz A, Mueller P.The predictive potential of the sweat chloride test in cystic fibrosis patients with the G551D mutation. J Cyst Fibros. 2013; 12:706-13. doi: 10.1016/j.jcf.2013.03.004. Epub 2013 Apr 28.[PubMed]
Sweat chloride measurements at day 15 had an overall positive predictive value (PPV) of 86.3%, a negative predictive value (NPV) of 65.5%, sensitivity of 73.9%, and specificity of 80.9% for an FEV1 improvement of ≥5% from baseline at week 16. For ivacaftor patients the median FEV1 improvement was 16.7%; for placebo patients 0.4%. For patients aged 6-11 years who received ivacaftor and who had a sweat chloride decrease of ≥40 mmol/L from baseline at day 15, a median weight gain of 11.2% at week 16, compared to 6% for those with a smaller decrease was observed.
The authors suggest changes in sweat chloride concentration at day 15 following treatment with ivacaftor may have sufficient predictive potential to identify individuals that show improvement in pulmonary function and weight gain after 16 weeks of treatment.
2014 2014 2014
2014 Accurso FJ, Van Goor F, Zha J, Stone AJ, Dong Q, Ordonez CL, Rowe SM, Clancy JP, Konstan MW, Hoch HE, Heltshe SL, Ramsey BW, Campbell PW, Ashlock MA. Sweat chloride as a biomarker of CFTR activity: proof of concept and ivacaftor clinical trial data. J Cyst Fibros. 2014; 13:139-47. [PubMed]
The authors examined data from a Phase 2 trial {NCT00457821} of ivacaftor, a CFTR potentiator, in cystic fibrosis (CF) patients with a G551D mutation to evaluate standardized approaches to sweat chloride measurement and to explore the use of sweat chloride and nasal potential difference (NPD) to estimate CFTR activity. Sweat chloride and NPD were secondary endpoints in this placebo-controlled, multicenter trial. Standardization of sweat collection, processing,and analysis was employed for the first time. Sweat chloride and chloride ion transport (NPD) were integrated into a model of CFTR activity.
Within-patient sweat chloride determinations showed sufficient precision to detect differences between dose-groups and assess ivacaftor treatment effects. Analysis of changes in sweat chloride and NPD demonstrated that patients treated with ivacaftor achieved CFTR activity equivalent to approximately 35%–40% of normal.
– The authors concluded that sweat chloride is useful in multicenter trials as a biomarker of CFTR activity and to test the effect of CFTR potentiators. However, experience and opinions appear to vary on this (Barry et al, 2014 v. infra).
2014 Barry PJ, Jones AM, Webb AK, Horsley AR. Sweat chloride is not a useful marker of clinical response to Ivacaftor. Thorax. 2014 Jun;69(6):586-7. doi: 10.1136/thoraxjnl-2013-204532. Epub 2013 Nov 20.[PubMed]
Clinical trials have revealed that Ivacaftor significantly reduces sweat chloride in patients with cystic fibrosis who carry the G551D mutation. This finding has been incorporated into the commissioning guidelines in the UK with a sweat chloride reduction of 30% or below 60 mmol/L, specified as the main criteria for continued funding of Ivacaftor for individual patients.
In a cohort of 24 adults who were prescribed Ivacaftor, there was no correlation between absolute or relative reductions in sweat chloride and improvements in lung function. This questions the validity of sweat chloride as a surrogate marker of clinical efficacy.
2014 Barry PJ, Plant BJ, Nair A, Bicknell S, Simmonds NJ, Bell NJ, Shafi NT, Daniels T, Shelmerdine S, Felton I, Gunaratnam C, Jones AM, Horsley AR. Effects of Ivacaftor in cystic fibrosis patients carrying the G551D mutation with severe lung disease. Chest 2014 Feb 13. doi: 10.1378/[PubMed]
21 patients received ivacaftor for a median of 237 days. Mean FEV1 improved from 26·5% to 30·7% predicted (p=0·01), representing a 16.7% relative improvement. Median weight improved from 49·8 to 51·6kg (p=0·006). Median in-patient intravenous antibiotic days declined from 23 to 0 days per year (p=0.001) and median total intravenous treatment days decreased from 74 to 38 days per year (p=0.002) following ivacaftor. Changes in pulmonary function and intravenous antibiotic requirements were significant compared to control subjects.
Ivacaftor was clinically effective in CF patients carrying the G551D mutation with severe pulmonary disease. The reductions in treatment requirements were clinically and statistically significant and have not been described in less severe populations.
2014 Baroni D. Zegarra-Moran O. Svensson A. Moran O. Direct interaction of a CFTR potentiator and a CFTR corrector with phospholipid bilayers.Euro Biophys J 2014; 43(6-7):341-6.[PubMed]
Cystic fibrosis transmembrane conductance regulator (CFTR) potentiators and correctors are new drugs that target the basic CFTR protein defect and are expected to benefit cystic fibrosis patients. To optimise the substances so far proposed for human use, and to minimise unwanted side effects, it is essential to investigate possible interactions between the drugs and cell components. The authors used small-angle X-ray scattering with synchrotron radiation to analyse the effects of two representative drugs, the potentiator VX-770 (Ivacaftor), approved for human use, and the corrector VX-809 (Lumacaftor), on a model phospholipid membrane.
By reconstruction of the electron density profile of unilamellar vesicles treated with VX-770 or VX-809 the authors found that these drugs penetrate the phospholipid bilayer. VX-809 becomes homogeneously distributed throughout the bilayer whereas VX-770 accumulates predominantly in the internal leaflet, behaviour probably favoured by the asymmetry of the bilayer, because of vesicle curvature.
Penetration of the bilayer by these drugs, probably as part of the mechanisms of permeation, causes destabilization of the membrane; this must be taken into account during future drug development.
– It is still early days in the use of these correctors and potentiators. They have such a profound effect on those treated that it is not surprising they have a variety of other effects and such studies are welcome.
2014 Boinot C. Jollivet Souchet M. Ferru-Clement R. Becq F. Searching for combinations of small-molecule correctors to restore f508del-cystic fibrosis transmembrane conductance regulator function and processing. J Pharmacol Exp Ther 2014; 350(3):624-34. [PubMed]
The mutated protein F508del-cystic fibrosis transmembrane conductance regulator (CFTR) failed to traffic properly as a result of its retention in the endoplasmic reticulum and functions as a chloride (Cl(-)) channel with abnormal gating and endocytosis. Small chemicals (called correctors) individually restore F508del-CFTR trafficking and Cl(-) transport function, but recent findings indicate that synergistic pharmacology should be considered to address CFTR defects more clearly. The authors studied the function and maturation of F508del-CFTR expressed in HeLa cells using a combination of five correctors [miglustat, IsoLAB (1,4-dideoxy-2-hydroxymethyl-1,4-imino-l-threitol), Corr4a (N-[2-(5-chloro-2-methoxy-phenylamino)-4′-methyl-[4,5′]bithiazolyl-2′-yl]-benzamide), VX-809 [3-(6-(1-(2,2-difluorobenzo[d][1,3]dioxol-5-yl)cyclopropanecarboxamido)-3-methylpyridin-2-yl)benzoic acid], and suberoylamilide hydroxamic acid (SAHA)]. Full data in the abstract.
The authors consider their results open new perspectives for the development of a synergistic polypharmacology to rescue F508del-CFTR and show the importance of temperature on the effect of correctors and on the level of correction, suggesting that optimized combination of correctors could lead to a better rescue of F508del-CFTR function.
2014 Boyle MP. Bell SC. Konstan MW. McColley SA. Rowe SM. Rietschel E. Huang X. Waltz D. Patel NR. Rodman D. VX09-809-102 study group. A CFTR corrector (lumacaftor) and a CFTR potentiator (ivacaftor) for treatment of patients with cystic fibrosis who have a phe508del CFTR mutation: a phase 2 randomised controlled trial. Lancet Respir Med 2014; 2(7):527-38. [PubMed]
This important multicentre study tested combination treatment with lumacaftor, an investigational CFTR corrector that increases trafficking of phe508del CFTR to the cell surface, and ivacaftor, a CFTR potentiator that enhances chloride transport of CFTR on the cell surface.
The authors assessed three successive cohorts, with the results of each cohort informing dose selection for the subsequent cohort. They recruited patients from 24 cystic fibrosis centres in Australia, Belgium, Germany, New Zealand, and the USA. Eligibility criteria were: confirmed diagnosis of cystic fibrosis, age at least 18 years, and a forced expiratory volume in 1s (FEV1) of 40% or more than predicted.
Cohort 1 included phe508del CFTR homozygous patients randomly assigned to either lumacaftor 200 mg once per day for 14 days followed by addition of ivacaftor 150 mg or 250 mg every 12 h for 7 days, or 21 days of placebo.
Together, cohorts 2 and 3 included phe508del CFTR homozygous and heterozygous patients, randomly assigned to either 56 days of lumacaftor (cohort 2: 200 mg, 400 mg, or 600 mg once per day, cohort 3: 400 mg every 12 h) with ivacaftor 250 mg every 12 h added after 28 days, or 56 days of placebo.
The primary outcomes for all cohorts were change in sweat chloride concentration during the combination treatment period in the intention-to-treat population and safety (laboratory measurements and adverse events). (The study is registered with ClinicalTrials.gov, number NCT01225211, and EudraCT, number 2010-020413-90).
Cohort 1 included 64 participants. Cohort 2 and 3 combined contained 96 phe508del CFTR homozygous patients and 28 compound heterozygotes. Treatment with lumacaftor 200 mg once daily and ivacaftor 250 mg every 12 h decreased mean sweat chloride concentration by 9.1 mmol/L (p<0.001) during the combination treatment period in cohort 1.
In cohorts 2 and 3, mean sweat chloride concentration did not decrease significantly during combination treatment in any group. Frequency and nature of adverse events were much the same in the treatment and placebo groups during the combination treatment period; the most commonly reported events were respiratory. 12 of 97 participants had chest tightness or dyspnoea during treatment with lumacaftor alone. In pre-planned secondary analyses, a significant decrease in sweat chloride concentration occurred in the treatment groups between day 1 and day 56 (lumacaftor 400 mg once per day group -9.1 mmol/L, p<0.001; lumacaftor 600 mg once per day group -8.9 mmol/L, p<0.001; lumacaftor 400 mg every 12 h group -10.3 mmol/L, p=0.002). These changes were significantly greater than the change in the placebo group. In cohort 2, the lumacaftor 600 mg once per day significantly improved FEV1 from day 1 to 56 (difference compared with placebo group: +5.6 percentage points, p=0.013), primarily during the combination period. In cohort 3, FEV1 did not change significantly across the entire study period compared with placebo (difference +4.2 percentage points, p=0.132), but did during the combination period (difference +7.7 percentage points, p=0003). Phe508del CFTR heterozygous patients did not have a significant improvement in FEV1.
This trial provided evidence that combination lumacaftor and ivacaftor (Orkambi) improves FEV1 for patients with cystic fibrosis who are homozygous for phe508del CFTR, with a modest effect on sweat chloride concentration. These results support the further exploration of combination lumacaftor and ivacaftor as a treatment in this setting. The abstract of this important study and rather complex study is reproduced in full.
2014 Char JE, Wolfe MH, Cho HJ, Park IH, Jeong JH, Frisbee E, Dunn C, Davies Z, Milla C, Moss RB, Thomas EA, Wine JJ. A little CFTR goes a long way: CFTR-dependent sweat secretion from G551D and R117H-5T cystic fibrosis subjects taking ivacaftor. PLoS One. 2014 Feb 10;9(2):e88564. doi: 10.1371/journal.pone.0088564. eCollection 2014.[PubMed]
To determine if oral dosing with the CFTR-potentiator ivacaftor (VX-770, Kalydeco) improves CFTR-dependent sweating in CF subjects carrying G551D or R117H-5T mutations, the authors optically measured sweat secretion from 32-143 individually identified glands in each of 8 CF subjects; 6 F508del/G551D, one G551D/R117H-5T, and one I507del/R117H-5T. Two subjects were tested only (-) ivacaftor, 3 only (+) ivacaftor and 3 (+/-) ivacaftor (1-5 tests per condition). The total number of gland measurements was 852 (-) ivacaftor and 906 (+) ivacaftor. A healthy control was tested 4 times (51 glands). For each gland they measured both CFTR-independent (M-sweat) and CFTR-dependent (C-sweat); C-sweat was stimulated with a beta-adrenergic cocktail that elevated [cAMP]i while blocking muscarinic receptors. Absent ivacaftor, almost all CF glands produced M-sweat on all tests, but only 1/593 glands produced C-sweat (10 tests, 5 subjects). By contrast, 6/6 subjects (113/342 glands) produced C-sweat in the (+) ivacaftor condition, but with large inter-subject differences; 3-74% of glands responded with C/M sweat ratios 0.04%-2.57% of the average WT ratio of 0.265. Sweat volume losses cause proportionally larger underestimates of CFTR function at lower sweat rates. The losses were reduced by measuring C/M ratios in 12 glands from each subject that had the highest M-sweat rates. Remaining losses were estimated from single channel data and used to correct the C/M ratios, giving estimates of CFTR function (+) ivacaftor = 1.6%-7.7% of the WT average.
These authors observe that these estimates are in accord with single channel data and transcript analysis, and apparently suggest that significant clinical benefit can be produced by low levels of CFTR function.
2014 Cholon DM. Quinney NL. Fulcher ML. Esther CR Jr. Das J. Dokholyan NV. Randell SH. Boucher RC. Gentzsch M. Potentiator ivacaftor abrogates pharmacological correction of F508 CFTR in cystic fibrosis. Translational Medicine 2014; 6(246):246ra96. [PubMed]
In studies of human primary airway epithelial cells, both acute and chronic treatment with VX-770 improved CFTR function in cells with the G551D mutation, consistent with clinical studies. In contrast, chronic VX-770 administration caused a dose-dependent reversal of VX-809-mediated CFTR correction in F508 homozygous cultures. This result reflected the destabilisation of corrected F508 CFTR by VX-770, markedly increasing its turnover rate. Chronic VX-770 treatment also reduced mature wild-type CFTR levels and function.
– The authors consider their findings demonstrate that chronic treatment with CFTR potentiators and correctors may have unexpected effects that cannot be predicted from short-term studies. Combining these drugs to maximise rescue of F508 CFTR may require changes in dosing and/or development of new potentiator compounds that do not interfere with CFTR stability.
2014 De Boeck K, Munck A, Walker S, Faro A, Hiatt P, Gilmartin G, Higgins M. Efficacy and safety of ivacaftor in patients with cystic fibrosis and a non-G551D gating mutation. J Cyst Fibros. 2014 Dec;13(6):674-80. doi: 10.1016/j.jcf.2014.09.005. Epub 2014 Sep 2 [PubMed]
Ivacaftor is used to treat patients with CF and a G551D gating mutation; the KONNECTION study assessed the efficacy and safety of ivacaftor in patients with CF and a non-G551D gating mutation. Patients with CF ≥6-years- old with non-G551D gating mutations ivacaftor 150mg q12h or placebo for 8weeks in this 2-part, double-blind crossover study (Part 1) with a 16-week open-label extension (Part 2). The primary efficacy was the outcome of treatment. Eight weeks of ivacaftor resulted in significant improvements in percent predicted FEV1, BMI, sweat chloride, and CFQ-R scores that were maintained through 24weeks. Ivacaftor was generally well tolerated.
Ivacaftor was efficacious in a group of patients with CF who had selected non-G551D gating mutations
2014 Eckford PD. Ramjeesingh M. Molinski S. Pasyk S. Dekkers JF. Li C. Ahmadi S. Ip W. Chung TE. Du K. Yeger H. Beekman J. Gonska T. Bear CE. VX-809 and related corrector compounds exhibit secondary activity stabilizing active F508del-CFTR after its partial rescue to the cell surface. Chem Biol 2014; 21(5):666-78. [PubMed]
The most common mutation causing cystic fibrosis (CF), F508del, impairs conformational maturation of CF transmembrane conductance regulator (CFTR), thereby reducing its functional expression on the surface of epithelia. Corrector compounds including C18 (VRT-534) and VX-809 have been shown to partially rescue misfolding of F508del-CFTR and to enhance its maturation and forward trafficking to the cell surface.
The authors show that there is an additional action conferred by these compounds beyond their role in improving the biosynthetic assembly. In vitro studies show that these compounds bind directly to the metastable, full-length F508del-CFTR channel. Cell culture and patient tissue-based assays confirm that in addition to their cotranslational effect on folding, certain corrector compounds bind to the full-length F508del-CFTR after its partial rescue to the cell surface to enhance its function. These findings may inform the development of alternative compounds with improved therapeutic efficacy.
Adam Feuerstein. Vertex Pharma Cystic Fibrosis Combo Therapy Hits Key Endpoints in Two Pivotal Trials. A report in The Street on 24.6.14
Combination therapy of two Vertex Pharmaceuticals (VRTX_) drugs, VX-809 (lumacaftor) and Kalydeco (ivacaftor VX-770), produced a statistically significant improvement in lung function for patients with the most common form of cystic fibrosis (F508del-CFTR). The two phase III studies dubbed “TRAFFIC” and “TRANSPORT” both met their primary endpoints separately. When the studies were pooled together, cystic fibrosis patients treated with the higher of two doses of VX-809 (also known as Lumacaftor) and Kalydeco saw their lung function improve by 3.3% on an absolute basis compared to placebo.
Vertex’s combination regimen also achieved statistical significance versus placebo on two key secondary endpoints of the phase III studies — a 30% and 39% reduction in pulmonary exacerbations and improvements in weight gain (body mass index.) [Vertex shared the study results with the writer of this abstract on June 23rd under embargo.]
2014 Hayes D Jr. McCoy KS. Sheikh SI. Improvement of sinus disease in cystic fibrosis with ivacaftor therapy. Am J Resp Crit Care Med 2014; 190(4):468.[PubMed]
A 19-year old woman with CF (d508/G551D) experienced significant general improvement after 15 months ivacaftor therapy and in particular major improvement in previously troublesome sinus disease. Impressive changes in the MCT scan reproduced in the link from the abstract.
2014 Kopeikin Z. Yuksek Z. Yang HY. Bompadre SG. Combined effects of VX-770 and VX-809 on several functional abnormalities of F508del-CFTR channels. J Cyst Fibros 2014; 13:508-14.[PubMed]
VX-770, a clinically approved drug for treatment of CF patients carrying the G551D mutation, and VX-809, a corrector shown in vitro to increase membrane expression of mutant channels, are currently undergoing clinical trials, but functional data at the molecular level is still lacking. The effect of VX-770 and VX-809 (lumacaftor) on the multiple functional defects of F508del-CFTR was assessed via excised inside-out patch-clamp experiments.
VX-770 completely restores the low opening-rate of F508del-CFTR, with smaller open-time increase, in temperature-corrected and VX-809-treated channels. The shorter locked-open time of hydrolysis-deficient F508del-CFTR is also prolonged by VX-770. VX-809 does not improve channel function by itself as previously reported.
The authors concluded these studies can be interpreted as an equilibrium shift toward the open-channel conformation of F508del-CFTR channels.
2014 Reznikov LR. Abou Alaiwa MH. Dohrn CL. Gansemer ND. Diekema DJ. Stoltz DA. Welsh MJ. Antibacterial properties of the CFTR potentiator ivacaftor. J Cyst Fibros 2014; 13:515-9. [PubMed]

Leah Reznikov
As ivacaftor structurally resembles quinolone antibiotics, the authors tested the hypothesis that ivacaftor possesses antibacterial properties. Bioluminescence, colony forming unit, and minimal inhibitory concentration assays were used to assess viability of Staphylococcus aureus, Pseudomonas aeruginosa and multiple clinical microbial isolates. Ivacaftor induced a dose-dependent reduction in bioluminescence of S. aureus and decreased the number of colony forming units. There was a similar but less robust effect in P. aeruginosa following outer membrane permeabilisation. Ivacaftor inhibited the growth of respiratory isolates of S. aureus and Streptococcus pneumoniae and exhibited positive interactions with antibiotics against lab’ and respiratory strains of S. aureus and S. pneumoniae.
The authors consider these data indicate that ivacaftor exhibits antibacterial properties and raise the possibility that ivacaftor might have an antibiotic effect in people with CF.
2014 Rowe SM. Heltshe SL. Gonska T. Donaldson SH. Borowitz D. Gelfond D. Sagel SD. Khan U. Mayer-Hamblett N. Van Dalfsen JM. Joseloff E. Ramsey BW. GOAL Investigators of the Cystic Fibrosis Foundation Therapeutics Development Network. Clinical mechanism of the cystic fibrosis transmembrane conductance regulator potentiator ivacaftor in G551D-mediated cystic fibrosis. J Respir Crit Care Med 2014; 190(2):175-84.[PubMed]
Steven Rowe
To evaluate ivacaftor in a post-approval setting and determine mechanism of action and response of clinically relevant markers the authors conducted a longitudinal cohort study in 2012-2013 in G551D CF patients age 6 and older with no prior exposure to ivacaftor. Study assessments were performed at baseline, 1, 3, and 6 months after ivacaftor initiation. Substudies evaluated mucociliary clearance, beta-adrenergic sweat secretion rate, gastrointestinal pH, and sputum inflammation and microbiology
Measurements and Main Results: A total of 151 of 153 subjects were prescribed ivacaftor and 88% completed the study through 6 months. FEV1 % predicted improved from baseline to 6 months (mean absolute change, 6.7%; P < 0.001). Similarly, body mass index improved from baseline to 6 months (mean change, 0.8 kg/m(2); P < 0.001). Sweat chloride decreased from baseline to 6 months (mean change, -53.8 mmol/L; 95% confidence interval, -57.7 to -49.9; P < 0.001), reflecting augmented CFTR function. There was significant improvement in hospitalization rate (P < 0.001) and Pseudomonas aeruginosa burden (P < 0.01). Significant improvements in mucociliary clearance (P < 0.001), gastrointestinal pH (P = 0.001), and microbiome were also observed, providing clinical mechanisms underlying the therapeutic benefit of ivacaftor.
The authors concluded clinical and physiologic improvements were observed on initiation of ivacaftor in a broad patient population, including reduced infection with P. aeruginosa. Biomarker studies substantially improve the understanding of the mechanistic consequences of CFTR modulation on pulmonary and gastrointestinal physiology.
2014 Saynor ZL. Barker AR. Oades PJ. Williams CA. The effect of ivacaftor in adolescents with cystic fibrosis (G551D mutation): an exercise physiology perspective. Phys Ther 2014; 26:454-61. [PubMed]
The purpose of this report was to evaluate the influence of 12 weeks of ivacaftor treatment on the aerobic function of 2 teenage patients with cystic fibrosis (CF; F508/G551D) using a maximal cardiopulmonary exercise test. One patient, with relatively mild disease, demonstrated no clinically meaningful changes in maximal oxygen uptake (Equation is included in full-text article. O2max). However, in the second case, with more established lung disease on imaging, the O2max improved by approximately 30%.
The authors suggest cardiopulmonary exercise testing represents an important outcome measure in the functional assessment of patients with CF.
2014 Van Goor F. Yu H. Burton B. Hoffman BJ. Effect of ivacaftor on CFTR forms with missense mutations associated with defects in protein processing or function. J Cyst Fibros 2014; 13(1):29-36. [PubMed]
Ivacaftor (KALYDECO, VX-770) is a CFTR potentiator that increased CFTR channel activity and improved lung function in patients age 6 years and older with CF who have the G551D-CFTR gating mutation. The aim of this in vitro study was to evaluate the effect of ivacaftor on mutant CFTR protein forms with defects in protein processing and/or channel function.
The effect of ivacaftor on CFTR function was tested in electrophysiological studies using a panel of Fischer rat thyroid (FRT) cells expressing 54 missense CFTR mutations that cause defects in the amount or function of CFTR at the cell surface.
Ivacaftor potentiated multiple mutant CFTR protein forms that produce functional CFTR at the cell surface. These included mutant CFTR forms with mild defects in CFTR processing or mild defects in CFTR channel conductance.
The authors conclude that in vitro data indicated that ivacaftor is a broad acting CFTR potentiator and could be used to help stratify patients with CF who have different CFTR genotypes for studies investigating the potential clinical benefit of ivacaftor.
2014 Veit G. Avramescu RG. Perdomo D. Phuan PW. Bagdany M. Apaja PM. Borot F. Szollosi D. Wu YS. Finkbeiner WE. Hegedus T. Verkman AS. Lukacs GL. Some gating potentiators, including VX-770, diminish F508-CFTR functional expression. Translat Med 2014; 6(246): 246ra97. [PubMed]
Treatment of CF patients carrying the G551D gating mutation with the potentiator VX-770 (ivacaftor) largely restores channel activity and has shown substantial clinical benefit. However, most CF patients carry the F508 mutation, which impairs CFTR folding, processing, function, and stability. Studies in homozygous F508 CF patients indicated little clinical benefit of monotherapy with the investigational corrector VX-809 (lumacaftor) or VX-770, whereas combination clinical trials show limited but significant improvements in lung function.
The authors show that VX-770, as well as most other potentiators, reduces the correction efficacy of VX-809 and another investigational corrector, VX-661. To mimic the administration of VX-770 alone or in combination with VX-809, they examined its long-term effect in immortalised and primary human respiratory epithelia. VX-770 diminished the folding efficiency and the metabolic stability of F508-CFTR at the endoplasmic reticulum (ER) and post-ER compartments, respectively, causing reduced cell surface F508-CFTR density and function. VX-770-induced destabilisation of F508-CFTR was influenced by second-site suppressor mutations of the folding defect and was prevented by stabilisation of the nucleotide-binding domain 1 (NBD1)-NBD2 interface.
The authors suggest that the reduced correction efficiency of F508-CFTR, as well as of two other processing mutations in the presence of VX-770, suggests the need for further optimisation of potentiators to maximise the clinical benefit of corrector-potentiator combination therapy in CF.
2014 Wang Y. Liu J. Loizidou A. Bugeja LA. Warner R. Hawley BR. Cai Z. Toye AM. Sheppard DN. Li H. CFTR potentiators partially restore channel function to A561E-CFTR, a cystic fibrosis mutant with a similar mechanism of dysfunction as F508del-CFTR. Br J Pharmacol 2014; 171:4490-503.[PubMed]
A561E-CFTR is a CF mutation found frequently in Portugal. Using the iodide efflux assay, CFTR potentiators, including genistein and the clinically approved small-molecule ivacaftor, partially restored function to A561E-CFTR. Interestingly, ivacaftor restored wild-type levels of channel activity (as measured by open probability) to single A561E- and F508del-CFTR Cl(-) channels. However, it accentuated the thermoinstability of both mutants in cell-free membrane patches.
2014 Whiting P. Al M. Burgers L. Westwood M. Ryder S. Hoogendoorn M. Armstrong N. Allen A. Severens H. Kleijnen J. Ivacaftor for the treatment of patients with cystic fibrosis and the G551D mutation: a systematic review and cost-effectiveness analysis Technology Assessment (Winchester, England) 2014; 18(18):1-106. [PubMed]
To review the clinical effectiveness and cost-effectiveness of ivacaftor for the treatment of CF in patients aged > 6 years who have the G551D mutation.
More data in the abstract. The incremental cost-effectiveness ratio varied between £335,000 and £1,274,000 per quality-adjusted life-year gained. The total additional lifetime costs for all eligible CF patients in England ranged from £438M to £479M; the lifetime cost for standard care only was £72M.
The authors concluded that available evidence suggests that ivacaftor is a clinically effective treatment for patients with CF and the G551D mutation; the high cost of ivacaftor may prove an obstacle in the uptake of this treatment. The main priority for further research is the long-term effectiveness of ivacaftor.
This study emphasises the very high cost of ivacaftor in a UK perspective. The authors observe that the high cost may prove an obstacle – there can be no doubt that it will prove a major problem.
(From Kleijnen Systematic Reviews Ltd York UK of which Dr Jos Kleijnen is Director. KSR Ltd prepares systematic reviews and meta-analyses, rapid reviews, and health technology assessments to support policy making, licensing and reimbursement decisions (fourth hurdle processes), local decision-making about commissioning health services, economic evaluations and guideline development).
2014 Xue X, Mutyam V, Tang L, Biswas S, Du M, Jackson LA, Dai Y, Belakhov V, Shalev M, Chen F, Schacht J, J Bridges R, Baasov T, Hong J, Bedwell DM, Rowe SM. Synthetic aminoglycosides efficiently suppress cystic fibrosis transmembrane conductance regulator nonsense mutations and are enhanced by ivacaftor. Am J Respir Cell Mol Biol. 2014 ; 50:805-16. [PubMed]
New drugs are needed to enhance premature termination codon (PTC) suppression to treat the underlying cause of cystic fibrosis (CF) and other diseases caused by nonsense mutations. The authors tested new synthetic aminoglycoside derivatives expressly developed for PTC suppression in a series of complementary CF models. Using a dual-luciferase reporter system containing the four most prevalent CF transmembrane conductance regulator (CFTR) nonsense mutations (G542X, R553X, R1162X, and W1282X) within their local sequence contexts (the three codons on either side of the PTC), they found that NB124 promoted the most readthrough of G542X, R1162X, and W1282X PTCs. NB124 also restored full-length CFTR expression and chloride transport in Fischer rat thyroid cells stably transduced with a CFTR-G542XcDNA transgene, and was superior to gentamicin and other aminoglycosides tested. NB124 restored CFTR function to roughly 7% of wild-type activity in primary human bronchial epithelial (HBE) CF cells (G542X/delF508), a highly relevant preclinical model with endogenous CFTR expression. Efficacy was further enhanced by addition of the CFTR potentiator, ivacaftor (VX-770), to airway cells expressing CFTR PTCs. NB124 treatment rescued CFTR function in a CF mouse model expressing a human CFTR-G542X transgene; efficacy was superior to gentamicin and exhibited favorable pharmacokinetic properties, suggesting that in vitro results translated to clinical benefit in vivo. NB124 was also less cytotoxic than gentamicin in a tissue-based model for ototoxicity.
– These results provide evidence that NB124 and other synthetic aminoglycosides provide a 10-fold improvement in therapeutic index over gentamicin and other first-generation aminoglycosides, providing a promising treatment for a wide array of CFTR nonsense mutations. Included here as efficacy enhanced by ivacaftor.
2015 2015 2015
2015 Commentary by Scott Bell on the Alton et al publication
Bell SC. A new phase of CFTR treatment for cystic fibrosis? Lancet Respir Med 2015; 3(9):662-663. no abstract [PubMed]

Scott Bell
After mention of the developments in CFTR treatments Scott Bell reviews in some detail the UK Gene Therapy Consortium’s randomised, double-blind, placebo-controlled, phase 2b study of multi-dose nebulised gene–liposome complex (pGM169/GL67A) in patients with cystic fibrosis (FEV 1 50–90% predicted) and any combination of CFTR mutation (Alton EWFW et al, 2015). Therapy with pGM169/GL67A was well tolerated, with no excess treatment-associated adverse effects. Nasal and lower airway gene transfer analyses, showed modest concentrations of pGM169 plasmid DNA. Of the roughly one in five participants who had an improvement in FEV 1 of more than 5%, 70% had received the gene–liposome complex. Another notable finding was that patients with more severe lung disease (FEV 1 49·6–69·2% predicted) tended to have a greater treatment effect (6·4%) than those with milder lung disease (FEV 1 69·6–89·9% predicted; treatment effect 0·2%; p=0·065).
Commenting on the use of physiological saline as placebo – Bell suggested future trials should included a CFTR depleted plasma liposome placebo also effect on quality of life and pulmonary exacerbations (not an end point in this trial). He noted the increasing awareness of the complexity of the interactions between the CFTR protein and complex intracellular protein networks and suggested an even broader understanding of the cellular biology of CFTR would be necessary for successful correction of the numerous CFTR mutations.
2015 Bodewes FA; Verkade HJ; Taminiau JA; Borowitz D; Wilschanski M; Working group Cystic Fibrosis and Pancreatic Disease of the European Society for Paediatric Gastroenterology. Cystic fibrosis and the role of gastrointestinal outcome measures in the new era of therapeutic CFTR modulation. Hepatology and Nutrition (ESPGHAN). J Cyst Fibros 2015;14(2):169-77. [PubMed]
The currently available and accepted clinical endpoints, FEV1 and BMI, have limitations. The aim of this report is to draw attention to the need and the ample possibilities for the development and validation of relevant gastrointestinal clinical endpoints for scientific evaluation of CFTR modulation treatment, particularly in young children and infants. The gastrointestinal tract offers very good opportunities to measure CFTR protein function and systematically evaluate CF related clinical outcomes based on the principal clinical gastrointestinal manifestations of CF: intestinal pH, intestinal transit time, intestinal bile salt malabsorption, intestinal inflammation, exocrine pancreatic function and intestinal fat malabsorption.
The article contains a descriptive analysis of a variety of gastrointestinal outcome measures for clinical relevance, reliability, validity, responsiveness to interventions, feasibility in particular in young children and the availability of reference values.
– An attractive feature of the new drugs that directly affect CFTR function is that they act systemically and not merely on the airways. Already changes in pancreatic function and insulin production are described in patients on ivacaftor. Some form of extrapulmonary measure of change in CFTR function may be helpful particularly in young children where respiratory function tests are a problem.
2015 Bernarde C, Keravec M, Mounier J, Gouriou S, Rault G, Férec C, Barbier G, Héry-Arnaud G. Impact of the CFTR-Potentiator Ivacaftor on Airway Microbiota in Cystic Fibrosis Patients Carrying A G551D Mutation. PLoS One. 2015 Apr 8;10(4):e0124124. doi: 10.1371/journal.pone.0124124. eCollection 2015. [PubMed]
The purpose of this study was to follow the evolution of the airway microbiota in CF patients treated with ivacaftor, using quantitative PCR and pyro-sequencing of 16S rRNA amplicons, in order to identify quantitative and qualitative changes in bacterial communities. Three G551D children were followed up longitudinally over a mean period of more than one year covering several months before and after initiation of ivacaftor treatment.
129 operational taxonomy units (OTUs), representing 64 genera, were identified. There was no significant difference in total bacterial load before and after treatment. Comparison of global community composition found no significant changes in microbiota. Two OTUs, however, showed contrasting dynamics: after initiation of ivacaftor, the relative abundance of the anaerobe Porphyromonas 1 increased (p<0.01) and that of Streptococcus 1 (S. mitis group) decreased (p<0.05), possibly in relation to the anti-Gram-positive properties of ivacaftor. The anaerobe Prevotella 2 correlated positively with the pulmonary function test FEV-1 (r=0.73, p<0.05). The study confirmed the presumed positive role of anaerobes in lung function.
The authors concluded that several airway microbiota components, notably anaerobes (obligate or facultative anaerobes), could be valuable biomarkers of lung function improvement under ivacaftor, and could shed light on the pathophysiology of lung disease in CF patients. Another potentially important consequence of taking ivacaftor. It is reassuring that the various additional effects of the drug are receiving attention as well as the dramatic effects on the usual measured parameters.
2015 Carter S, Kelly S, Caples E, Grogan B, Doyle J, Gallagher CG, McKone EF. Ivacaftor as salvage therapy in a patient with cystic fibrosis genotype F508del/R117H/IVS8-5T. J Cyst Fibros. 2015 Jul; 14(4):e4-5. doi: 10.1016/j.jcf.2015.01.010. Epub 2015 Feb 16. [PubMed]
R117H-CFTR is a relatively common CFTR mutation that demonstrates an in-vitro response to ivacaftor. A clinical trial has suggested that there may be a role for ivacaftor in older patients with R117H-CFTR although this trial did not include patients with very severe CF lung disease The authors report a case demonstrating a substantial therapeutic effect of ivacaftor in a CF patient with genotype F508del/R117H and advanced lung disease. A 45-year-old male with CF (F508del/R117H/IVS8-5T/9T), was diagnosed at the age of 16 years old. His CF is complicated by advanced lung disease (FEV1 = 31% predicted, SaO2 = 95% on 1 l O2 at rest), chronic infection with Burkholderia multivorans and pancreatic insufficiency (faecal elastase = 135 mcg/g (normal > 200 mcg/g)); frequent exacerbations necessitated continuous IV antibiotic therapy. There was substantial improvement on inacaftor therapy. After 5 months of treatment, his weight is up by 4.3 kg with an increase in FEV1 to 1.50 l (42% predicted). Immediate improvements in FEV1 were seen at 2 weeks and continued up to a peak at day 75. Our patient also reports improved sputum volume and colour although is still growing B. multivorans in his sputum. Exercise capacity is much improved with an improvement in 6-minute walk test distance and decreased oxygen requirements at rest and with exercise. CRP levels have reduced to between 14 and 28 mmol/l, the lowest seen in 12 months. Faecal elastase is now in the normal range (355 mcg/g; repeat 1 month later 492 mcg/g). Sweat chloride on ivacaftor has reduced to 46 mmol/l. As a result, his continuous iv antibiotics have now been stopped and on 28th March he was taken off the active lung transplant list. To date, he continues to do well and is being followed closely by his CF team in conjunction with the lung transplant team.
– There are useful references in the paper to the various mutations that respond to ivacaftor therapy (Van Goor F et al. J Cyst Fibros 2014; 13(1):29-36) including the R117H-CFTR mutation (Moss RB et al. J Cyst Fibros 2014; 13(S2):44).
The improvement in faecal elastase is interesting and has been noted previously (Bellin et al. 2013. 23952705; Hayes D et al. 2014. 25171312) It is tempting to speculate that early ivacaftor therapy may delay or even avoid diabetes mellitus which is such a burden to people with CF.
2015 Chang EH; Tang XX; Shah VS; Launspach JL; Ernst SE; Hilkin B; Karp PH; Abou Alaiwa MH; Graham SM; Hornick DB; Welsh MJ; Stoltz DA; Zabner J. Medical reversal of chronic sinusitis in a cystic fibrosis patient with ivacaftor. Forum of Allergy & Rhinology 2015; 5(2):178-81. [PubMed]
Case report of 1 patient with long-standing chronic sinus disease and a new diagnosis of CF with a mild mutation (P205S) and a severe mutation (G551D). Clinical changes in symptoms, radiographic findings, nasal potential difference testing, and nasal pH values before and after treatment with ivacaftor are reported. The authors then developed primary sinonasal epithelial cell cultures from a biopsy of the patient to determine changes in airway surface liquid (ASL) pH and ASL viscosity after ivacaftor treatment.
Ivacaftor treatment reversed CT findings of CF sinus disease, increased nasal voltage and pH, and resolved sinus symptoms after 10 months of therapy. Ivacaftor significantly increased ASL pH and decreased ASL viscosity in primary airway cultures.
The authors state that this report documents the reversal of CF sinus disease. Based on their in vivo and in vitro results, they speculate that ivacaftor may reverse CF sinusitis by increasing ASL pH and decreasing ASL viscosity.
2015 Davies J, Sheridan H, Bell N, Cunningham S, Davis SD5, Elborn JS, Milla CE, Starner TD, Weiner DJ, Lee PS, Ratjen F. Assessment of clinical response to ivacaftor with lung clearance index in cystic fibrosis patients with a G551D-CFTR mutation and preserved spirometry: a randomised controlled trial. Lancet Respir Med. 2013 Oct;1(8):630-8. doi: 10.1016/S2213-2600(13)70182-6. Epub 2013 Sep 10.
Lung clearance index (LCI) using multiple-breath washout might be an alternative to and more sensitive method than forced expiratory volume in 1 s (FEV1) to assess treatment response in the growing number of children and young adults with cystic fibrosis who have normal spirometry. The aim of the study was to assess the treatment effects of ivacaftor on LCI in patients with cystic fibrosis, a G551D-CFTR mutation, and an FEV1 >90% predicted.
This phase 2, multicentre, placebo-controlled, double-blind 2×2 crossover study of ivacaftor treatment was conducted in patients with cystic fibrosis, at least one G551D-CFTR allele, and an FEV1 >90% predicted. Patients also had to have an LCI higher than 7·4 at screening, age of 6 years or older, and a weight higher than or equal to 15 kg. Eligible patients were randomly allocated to receive one of two treatment sequences (placebo first followed by ivacaftor 150 mg twice daily [sequence 1] or ivacaftor 150 mg twice daily first followed by placebo [sequence 2]) of 28 days’ treatment in each period, with a 28-day washout between the two treatment periods. Randomisation (ratio 1:1) was done with block sizes of 4, and all site personnel including the investigator, the study monitor, and the Vertex study team were masked to treatment assignment. The primary outcome measure was change from baseline in LCI.
Between February and November, 2011, 21 patients were enrolled, of which 11 were assigned to the sequence 1 group, and 10 to the sequence 2 group. 20 of these patients received treatment and 17 completed the trial (eight in sequence 1 group and 9 in sequence 2 group).
Treatment with ivacaftor led to significant improvements compared with placebo in LCI (difference between groups in the average of mean changes from baseline at days 15 and 29 was -2·16 [95% CI -2·88 to -1·44]; p<0·0001). Adverse events experienced by study participants were similar between treatment groups; at least one adverse event was reported by 15 (79%) of 19 patients who received placebo and 13 (72%) of 18 patients who received ivacaftor.
The authors concluded that in patients with cystic fibrosis aged 6 years or older who have at least one G551D-CFTR allele, ivacaftor led to improvements in Lung Clearance Index. They suggest that LCI might be a more sensitive alternative to FEV1 in detecting response to intervention in these patients with mild lung disease.
2015 Grasemann H, Gonska T, Avolio J, Klingel M, Tullis E, Ratjen F. Effect of ivacaftor therapy on exhaled nitric oxide in patients with cystic fibrosis. J Cyst Fibros. 2015 Jul 11. pii: S1569-1993(15)00163-0. doi: 10.1016/j.jcf.2015.07.001. [Epub ahead of print] [PubMed]

Hatmut Grasemann
Airways of patients with cystic fibrosis are deficient for nitric oxide. Low nitric oxide in cystic fibrosis has been shown to be associated with poor pulmonary function and risk of infection with certain pathogens. Fractional exhaled nitric oxide (FENO) was measured before and 4 weeks after initiation of ivacaftor therapy, in patients with cystic fibrosis and a CFTR gating mutation. The effect of ivacaftor on FENO was compared to treatment with inhaled dornase alfa or hypertonic saline for 4 weeks, respectively.
A total of 15 patients on ivacaftor therapy were studied. Pulmonary function improved significantly and mean (±SD) FENO increased from 8.5±5.0 to 16.2±15.5ppb. The effect was more pronounced in pediatric compared to adult patients. There was no linear correlation between changes in FENO, pulmonary function or sweat chloride concentration. Neither treatment with inhaled dornase alfa (n=15) or hypertonic saline (n=16) resulted in a change in FENO.
The authors suggested therapy with ivacaftor results in an increase in nitric oxide formation in cystic fibrosis airways, while dornase alfa or hypertonic saline has no effect on airway nitric oxide. Some beneficial effects of CFTR targeting therapy in CF may result from improved airway nitric oxide production.
2015 Hayes D Jr; Warren PS; McCoy KS; Sheikh SI. Improvement of hepatic steatosis in cystic fibrosis with ivacaftor therapy. J Pediatr Gastroenterol Nutr 2015; 60(5):578-9. [PubMed]

Don Hayes Jr
Treatment of liver disease, including hepatic steatosis, in patients with cystic fibrosis is limited. The authors report an adolescent with CF had significant improvement in hepatic steatosis with ivacaftor treatment.
– It is important to note that inadequate pancreatic enzyme replacement therapy can worsen steatosis. A girl with CF and gross hepatomegaly was referred to Leeds for liver biopsy that revealed severe steatosis. She had severe undertreated intestinal malabsorption. With control of the malabsorption with adequate pancreatic replacement therapy her hepatomegaly regressed.
2015 Heltshe SL; Mayer-Hamblett N; Burns JL; Khan U; Baines A; Ramsey BW; Rowe SM; GOAL (the G551D Observation-AL) Investigators of the Cystic Fibrosis Foundation Therapeutics Development Network. Pseudomonas aeruginosa in cystic fibrosis patients with G551D-CFTR treated with ivacaftor. Clin Infect Dis 2015; 60(5):703-12. [PubMed]

Sonya Heltshe
This study examines changes in CF respiratory pathogens with ivacaftor and correlates them with baseline characteristics and clinical response. Among 151 participants prescribed ivacaftor, 29% (26/89) who were culture positive for P. aeruginosa the year prior to ivacaftor use were culture negative the year following treatment; 88% (52/59) of those P. aeruginosa free remained uninfected. The authors concluded Pseudomonas aeruginosa culture positivity was significantly reduced following ivacaftor treatment. Efficacious CFTR modulation may contribute to lower frequency of culture positivity for P. aeruginosa and other respiratory pathogens, particularly in patients with less established disease.
– An encouraging study – presumably altering the physicochemical state of the airways towards normal reduced the likelihood of P. aeruginosa colonisation/infection and/or increased the ease with which the organism was eradicated by the patient.
2015 Konstan MW; Plant BJ; Elborn JS; Rodriguez S; Munck A; Ahrens R; Johnson C. Efficacy response in CF patients treated with ivacaftor: post-hoc analysis. Pediatr Pulmonol 2015; 50(5):447-55. [PubMed]

Michael Konstan
Clinical studies in patients with cystic fibrosis and G551D-CFTR showed that the group treated with ivacaftor had improved clinical outcomes. To better understand the effect of ivacaftor therapy across the distribution of individual FEV(1) responses, data from Phase 3 studies (STRIVE/ENVISION) were re-examined. In this post-hoc analysis of patients (n=209) who received 48 weeks of ivacaftor or placebo, patients were assigned to tertiles according to FEV(1) response. Across all tertiles, numerical improvements in FEV(1), sweat chloride, CFQ-R and the frequency of pulmonary exacerbations were observed in ivacaftor-treated patients: the treatment difference versus placebo was statistically significant for all outcomes in the upper tertile and for some outcomes in the lower and middle tertiles. The number needed to treat for a >5% improvement in % predicted FEV(1) was 1.90, for a >5% body weight increase was 5.74, and to prevent a pulmonary exacerbation was 3.85.
The authors concluded that this analysis suggests that the majority of patients with clinical characteristics similar to STRIVE/ENVISION patients have the potential to benefit from ivacaftor therapy.
– Further confirmation of the remarkable effect of ivacaftor in all genetically appropriate patients – as expected, response was better in the less severely affected patients.
(“Tertile”: Any of the two points that divide an ordered distribution into three parts, each containing a third of the population).
2015 Lenherr N, Lurà M, Trachsel D, Latzin P, Hammer J. Ivacaftor in a young boy with the rare gating mutation S549R – use of lung clearance index to track progress: a case report. BMC Pulm Med. 2015 Oct 16;15:123. doi: 10.1186/s12890-015-0120-1. Free PMC article [PubMed]
S549Ris a rare gating mutation considered to be less sensitive to potentiators such as ivacaftor than all other gating mutations. An 8-year-old boy with the rare S549R gating mutation treated with ivacaftor had subjective clinical improvements, the sweat chloride level and the lung clearance index decreased impressively within a few weeks of treatment while forced expiratory volume in the first and second values remained in normal range.
– The authors emphasise the value of measuring small airway function by lung clearance index as an outcome measure for new interventions targeting the correction of the CFTR defect at an age before traditional lung function parameters start to deteriorate.
2015 Matthes E, Goepp J, Carlile GW, Luo Y, Dejgaard K, Billet A, Robert R, Thomas DY, Hanrahan JW. Low free drug concentration prevents inhibition of F508del CFTR functional expression by the potentiator VX-770 (ivacaftor). Br J Pharmacol. 2015 Oct 22. doi: 10.1111/bph.13365.
The most common cystic fibrosis (CF) mutation F508del inhibits the gating and surface expression of CFTR (CF Transmembrane conductance Regulator), a plasma membrane anion channel, therefore optimal pharmacotherapies will likely require both a “potentiator” to increase channel open probability and a “corrector” that improves folding and trafficking of the mutant protein and its stability at the cell surface. Interaction between CF drugs has been reported but remains poorly understood. CFTR.
– The authors concluded chronic exposure to clinically relevant concentrations of VX-770 does not reduce F508del CFTR function when assayed at those concentrations. Therapeutic benefit of VX-770 + VX-809 (Orkambi) is probably limited by the efficacy of VX-809 rather than by an inhibitory effect of VX-770.
2015 McKone EF, Borowitz D, Drevinek P, Griese M, Konstan MW, Wainwright C, Ratjen F, Sermet-Gaudelus I, Plant B, Munck A, Jiang Y, Gilmartin G, Davies JC; VX08-770-105 (PERSIST) Study Group. Long-term safety and efficacy of ivacaftor in patients with cystic fibrosis who have the Gly551Asp-CFTR mutation: a phase 3, open-label extension study (PERSIST). Lancet Respir Med 2014 Nov; 2(11):902-10. doi: 10.1016/S2213-2600(14)70218-8. Epub 2014 Oct 9.[PubMed]

Edward McKone
Ivacaftor, a cystic fibrosis transmembrane conductance regulator (CFTR) potentiator, is approved for the treatment of patients with cystic fibrosis aged 6 years or older with Gly551Asp-CFTR. The authors assessed the safety and efficacy of ivacaftor during 96 weeks of PERSIST in patients with cystic fibrosis who completed a previous 48-week, placebo-controlled trial of the drug (STRIVE or ENVISION).
In this phase 3, open-label extension study, patients received ivacaftor 150 mg every 12 h in addition to their prescribed cystic fibrosis therapies. Patients who received placebo in their previous study initiated ivacaftor in this extension study. Patients were eligible if they had a Gly551Asp-CFTR mutation on at least one allele. The primary objective was to assess the long-term safety profile of ivacaftor as assessed by adverse events, clinical laboratory assessments, electrocardiograms, vital signs, and physical examination; secondary measures included change in forced expiratory volume in one second (FEV1), weight, and pulmonary exacerbations.
Between July 8, 2010, and April 8, 2013, 144 adolescents/adults (≥12 years) from STRIVE and 48 children (6-11 years) from ENVISION were enrolled. Across both trials, 38 (20%) patients had a serious adverse event during the first 48 weeks and 44 (23%) during the subsequent 48 weeks. Two adults (1%) and one child (<1%) discontinued because of adverse events. The most common adverse events were pulmonary exacerbation, cough, and upper respiratory tract infection.
Patients previously treated with ivacaftor had sustained improvements in FEV1, weight, and rate of pulmonary exacerbations for up to 144 weeks of treatment. Among adolescents/adults and children who previously received ivacaftor, absolute change in FEV1 at week 96 (144 weeks ivacaftor) was 9·4 and 10·3 % points and absolute increase in weight was 4·1 kg and 14·8 kg, respectively. For adolescents/adults only, the pulmonary exacerbation rate remained suppressed compared with that of patients who received placebo in the placebo-controlled study.
In summary the authors concluded at 144 weeks of treatment, ivacaftor was well tolerated, with no new safety concerns. Ivacaftor also provided durable effects for 144 weeks in patients who had received active treatment in the placebo-controlled study. Those patients who previously received placebo had improvements comparable to those of patients treated with ivacaftor in the placebo-controlled study.
2015 Moss RB, Flume PA, Elborn JS, Cooke J, Rowe SM, McColley SA, Rubenstein RC, Higgins M; VX11-770-110 (KONDUCT) Study Group. Efficacy and safety of ivacaftor in patients with cystic fibrosis who have an Arg117His-CFTR mutation: a double-blind, randomised controlled trial. Lancet Respir Med. 2015 Jul;3(7):524-33. doi: 10.1016/S2213-2600(15)00201-5. Epub 2015 Jun 9. [PubMed]
Richard Moss
Ivacaftor has been previously assessed in patients with cystic fibrosis with Gly551Asp-CFTR or other gating mutations. The authors assessed ivacaftor in patients with Arg117His-CFTR, a residual function mutation. They did a 24-week, placebo-controlled, double-blind, randomised clinical trial, which enrolled 69 patients with cystic fibrosis aged 6 years and older with Arg117His-CFTR and percentage of predicted forced expiratory volume in 1 s (% predicted FEV1) of at least 40. They randomly assigned eligible patients (1:1) to receive placebo or ivacaftor 150 mg every 12 h for 24 weeks. Randomisation was stratified by age (6-11, 12-17, and ≥18 years) and % predicted FEV1 (<70, ≥70 to ≤90, and >90).
The primary outcome was the absolute change from baseline in % predicted FEV1 through week 24. Secondary outcomes included safety and changes in sweat chloride concentrations and Cystic Fibrosis Questionnaire-Revised (CFQ-R) respiratory domain scores. An open-label extension enrolled 65 of the patients after washout; after 12 weeks, we did an interim analysis.
After 24 weeks, the treatment difference in mean absolute change in % predicted FEV1 between ivacaftor (n=34) and placebo (n=35) was 2·1 percentage points (95% CI -1·13 to 5·35; p=0·20). Ivacaftor treatment resulted in significant treatment differences in sweat chloride (-24·0 mmol/L, 95% CI -28·01 to -19·93; p<0·0001) and CFQ-R respiratory domain (8·4, 2·17 to 14·61; p=0·009). In prespecified subgroup analyses, % predicted FEV1 significantly improved with ivacaftor in patients aged 18 years or older (treatment difference vs placebo: 5·0 percentage points, 95% CI 1·15 to 8·78; p=0·01), but not in patients aged 6-11 years (-6·3 percentage points, -11·96 to -0·71; p=0·03).
In the extension study, both placebo-to-ivacaftor and ivacaftor-to-ivacaftor groups showed % predicted FEV1 improvement (absolute change from post-washout baseline at week 12: placebo-to-ivacaftor, 5·0 percentage points [p=0·0005]; ivacaftor-to-ivacaftor, 6·0 percentage points [p=0·006]). There were no new safety concerns
– Although this study did not show a significant improvement in % predicted FEV1, ivacaftor did significantly improve sweat chloride and CFQ-R respiratory domain scores and lung function in adult patients with Arg117His-CFTR, indicating that ivacaftor might benefit patients with Arg117His-CFTR who have established disease.
2015 Patel S, Sinha IP, Dwan K, Echevarria C, Schechter M, Southern KW. Potentiators (specific therapies for class III and IV mutations) for cystic fibrosis. Cochrane Database Syst Rev. 2015 Mar 26;3:CD009841. doi: 10.1002/14651858.CD009841.pub2. [PubMed]
To evaluate te effects of CFTR potentiators on clinically important outcomes in children and adults with cystic fibrosis. The authors included four randomised controlled trials (n = 378), lasting from 28 days to 48 weeks, comparing the potentiator ivacaftor to placebo. Trials differed in terms of design and participant eligibility criteria, which limited the meta-analyses. The phase 2 trial (n = 19) and two phase 3 trials (adult trial (n = 167), paediatric trial (n = 52)), recruited participants with the G551D mutation (class III). The fourth trial (n = 140) enrolled participants homozygous for the ΔF508 mutation (class II).
The authors concluded both G551D phase 3 trials (n = 219) demonstrated a clinically relevant impact of the potentiator ivacaftor on outcomes at 24 and 48 weeks, providing evidence for the use of this treatment in adults and children (over six years of age) with cystic fibrosis and the G551D mutation (class III). There is no evidence to support the use of ivacaftor in people with the ΔF508 mutation (class II) (n = 140). Trials on ivacaftor in people with different mutations are ongoing.
2015 Quon BS; Schaeffer MR; Molgat-Seon Y; Wilkie SS; Wilcox PG; Guenette JA. Physiological mechanisms of dyspnoea relief following ivacaftor in cystic fibrosis : a case report. Resp Physiol Neurobiol 2015; 205:105-8. [PubMed]

Bradley Quon
The authors performed detailed cardiopulmonary exercise testing pre- and post-initiation of ivacaftor in a 27-year old male with CF (CFTR genotype F508del/G551D) and chronic airflow obstruction (FEV1/FVC=0.44). An improvement of FEV1 (by 16%) following ivacaftor was accompanied by clinically significant improvements in exercise capacity (by 14%) and exertional dyspnea (by up to 5 Borg scale units). These improvements were attributable, at least in part, to favourable alterations in the ventilatory response to exercise, including improvements in breathing patterns (e.g., increased tidal volume and reduced breathing frequency) and dynamic operating lung volumes (e.g., increased inspiratory reserve volume and inspiratory capacity) and decreases in dynamic mechanical ventilatory constraints.
2015 Quittner A, Suthoff E, Rendas-Baum R, Bayliss MS, Sermet-Gaudelus I, Castiglione B, Vera-Llonch M. Effect of ivacaftor treatment in patients with cystic fibrosis and the G551D-CFTR mutation: patient-reported outcomes in the STRIVE randomized, controlled trial. Health Qual Life Outcomes. 2015 Jul 2; 13:93. doi: 10.1186/s12955-015-0293-6. [PubMed] Free full text
The authors evaluated how ivacaftor treatment affected CF symptoms, functioning, and well-being, as measured by the Cystic Fibrosis Questionnaire-Revised (CFQ-R), a widely-used patient-reported outcome (PRO) measure.
The results illustrate broad benefits of ivacaftor treatment across many domains: respiratory symptoms, physical and social functioning, health perceptions, and vitality, as measured by the CFQ-R. The breadth of improvements reflects the systemic mechanism of action of ivacaftor compared to other therapies. Findings support the patient-reported value of ivacaftor treatment in this patient population.
2015 Robertson SM; Luo X; Dubey N; Li C; Chavan AB; Gilmartin GS; Higgins M; Mahnke L. Clinical drug-drug interaction assessment of ivacaftor as a potentialitor of cytochrome P450 and P-glycoprotein. J Clin Pharmacol 2015; 55(1):56-62. [PubMed]
A series of in vitro experiments conducted early in the development of ivacaftor indicated ivacaftor and metabolites may have the potential to inhibit cytochrome P450 (CYP) 2C8, CYP2C9, CYP3A, and CYP2D6, as well as P-glycoprotein (P-gp). Based on these results, a series of clinical drug-drug interaction (DDI) studies were conducted to evaluate the effect inhibof ivacaftor on sensitive substrates of CYP2C8 (rosiglitazone), CYP3A (midazolam), CYP2D6 (desipramine), and P-gp (digoxin). In addition, a DDI study was conducted to evaluate the effect of ivacaftor on a combined oral contraceptive, as this is considered an important comedication in CF patients.
The results indicate ivacaftor is a weak inhibitor of CYP3A and P-gp, but has no effect on CYP2C8 or CYP2D6. Ivacaftor caused non-clinically significant increases in ethinyl estradiol and norethisterone exposure. Based on these results, caution and appropriate monitoring are recommended when concomitant substrates of CYP2C9, CYP3A and/or P-gp are used during treatment with ivacaftor, particularly drugs with a narrow therapeutic index, such as warfarin.
2015 Sawicki GS, McKone EF, Pasta DJ, Millar SJ, Wagener JS,, Johnson CA, Konstan MW. Sustained Benefit from Ivacaftor Demonstrated by Combining Clinical Trial and Cystic Fibrosis Patient Registry Data. Am J Respir Crit Care Med. 2015 Oct 1;192(7):836-42. doi: 10.1164/rccm.201503-0578OC. [PubMed]

Gregory Sawicki
A study to examine, over a 3-year period, whether ivacaftor therapy affects pulmonary function and nutritional measures in patients with CF with a G551D mutation compared with patients with CF who are homozygous for the F508del mutation.
A propensity score was used to match patients with CF greater than or equal to 6 years of age who have a G551D mutation and received ivacaftor in clinical trials for up to 144 weeks with data from patients in the U.S. Cystic Fibrosis Foundation Patient Registry who are homozygous for the F508del mutation.
The rate of lung function decline in G551D ivacaftor-treated patients was slower by nearly half. Moreover, treatment with ivacaftor is shown to improve body mass index and weight-for-age z scores for G551D patients over the 3-year analysis period. The authors conclude these findings suggest that ivacaftor is a disease-modifying therapy for the treatment of cystic fibrosis.
– Few would question the authors’ conclusions that ivacaftor is a disease modifying therapy for the treatment of CF. However this study does show that the benefits are sustained.
2015 Sheikh SI; Long FR; McCoy KS; Johnson T; Ryan-Wenger NA; Hayes D Jr. Ivacaftor improves appearance of sinus disease on computerised tomography in cystic fibrosis patients with G551D mutation. Clin Otolaryngol 2015; 40(1):16-21. [PubMed]
Twelve patients with a G551D-CFTR mutation were monitored for at least one year before and after starting ivacaftor. Patients with CF and G551D mutation, within 6 months of starting ivacaftor had significant improvements in weight, BMI and mean % FEV1. Significant lessening of underlying sinus disease measured by CT scan was noted, suggesting a disease modifying effect.
2015 Sheikh SI; Long FR; McCoy KS; Johnson T; Ryan-Wenger NA; Hayes D Jr. Computed tomography correlates with improvement with ivacaftor in cystic fibrosis patients with G551D mutation. J Cyst Fibros 2015; 14(1):84-9. [PubMed]
A single-center study was performed in CF patients receiving ivacaftor to evaluate the usefulness of high resolution computed tomography (HRCT) of the chest as a way to gauge response to ivacaftor therapy.
Ten patients with CF were enrolled for at least one year before and after starting ivacaftor. At time of enrolment, mean age was 20.9 +/- 10.8 (range 10-44) years. There were significant improvements from baseline to 6 months in mean %FVC (93 +/- 16 to 99 +/- 16) and %FEV1 (79 +/- 26 to 87 +/- 28) but reverted to baseline at one year. Mean sweat chloride levels decreased significantly from baseline to one year. Mean weight and BMI improved at 6 months. Weight continued to improve with stabilisation of BMI at one year.
Chest HRCT showed significant improvement at one year in mean modified Brody scores for bronchiectasis, mucous plugging, airway wall thickness, and total Brody scores. Elevated bronchiectasis and airway wall thickness scores correlated significantly with lower %FEV1, while higher airway wall thickness and mucus plugging scores correlated with more pulmonary exacerbations requiring IV and oral antibiotics respectively.
The authors concluded that, based on their findings, HRCT imaging is a useful tool in monitoring response to ivacaftor therapy.
2015 Stanton BA, Coutermarsh B, Barnaby R, Hogan D. Pseudomonas aeruginosa Reduces VX-809 Stimulated F508del-CFTR Chloride Secretion by Airway Epithelial Cells. PLoS One. 2015 May 27;10(5):e0127742. doi: 10.1371/journal.pone.0127742. eCollection 2015. 26018799 Free PMC article. [PubMed]
Previously, these authors demonstrated that P. aeruginosa reduced wt-CFTR Cl secretion by airway epithelial cells. Recently, a new investigational drug VX-809 (lumacaftor) has been shown to increase F508del-CFTR Cl secretion in human bronchial epithelial (HBE) cells, and, in combination with VX-770, to increase FEV1 (forced expiratory volume in 1 second) by an average of 3-5% in CF patients homozygous for the F508del-CFTR mutation. The authors propose that P. aeruginosa infection of CF lungs reduces VX-809 + VX-770 (orkambi) – stimulated F508del-CFTR Cl secretion, and thereby reduces the clinical efficacy of VX-809 + VX-770.
F508del-CFBE cells and primary cultures of CF-HBE cells (F508del/F508del) were exposed to VX-809 alone or a combination of VX-809 + VX-770 for 48 hours and the effect of P. aeruginosa on F508del-CFTR Cl secretion was measured in Ussing chambers. The effect of VX-809 on F508del-CFTR abundance was measured by cell surface biotinylation and western blot analysis. PAO1, PA14, PAK and 6 clinical isolates of P. aeruginosa (3 mucoid and 3 non-mucoid) significantly reduced drug stimulated F508del-CFTR Cl secretion, and plasma membrane F508del-CFTR.
The observation that P. aeruginosa reduces VX-809 and VX-809 + VX-770 stimulated F508del CFTR Cl secretion may explain, in part, why VX-809 + VX-770 (orkambi) has modest efficacy in clinical trials.
2015 Taylor-Cousar J, Niknian M, Gilmartin G, Pilewski JM; for the VX11-770-901 investigators. Effect of ivacaftor in patients with advanced cystic fibrosis and a G551D-CFTR mutation: Safety and efficacy in an expanded access program in the United States. J Cyst Fibros. 2015 Feb 11. pii: S1569-1993(15)00010-7. doi: 10.1016/j.jcf.2015.01.008. [Epub ahead of print][PubMed]

Jennifer Taylor-Cousar
CF patients aged ≥6years with a G551D-CFTR mutation and FEV1≤40% predicted or listed for lung transplant received ivacaftor 150mg every 12h. The primary endpoint was safety as determined by adverse events. Secondary endpoints included assessment of lung function and weight.
The rate of serious adverse events was consistent with disease severity. At 24weeks of treatment with ivacaftor, there was a mean absolute increase predicted FEV1% of 5.5 percentage points and a 3.3kg mean absolute increase in weight from baseline.
So in patients with severe lung disease, ivacaftor was well tolerated and was associated with improved lung function and weight gain.
– One of a number of reports on the beneficial effects of ivacaftor in patient with severe chest involvement.
2015 Vreede CL; Berkhout MC; Sprij AJ; Fokkens WJ; Heijerman HG. Ivacaftor and sinonasal pathology in a cystic fibrosis patient with genotype deltaF508/S1215N. J Cyst Fibros 2015; 14(3):412-3. [PubMed]
A report of a positive favourable effect of ivacaftor on the sinonasal pathology in a 17 year old patient with CF. Although there were some adverse reports of the effect of ivacaftor on the upper respiratory tract, after 5 months of ivacaftor use in this patient, the CT-sinus showed complete resolution of the opacification of the paranasal sinuses and a decrease in symptoms of sinonasal disease.
2015 Wainwright CE, Elborn JS, Ramsey BW, Marigowda G, Huang X, Cipolli M, Colombo C, Davies JC, De Boeck K, Flume PA, Konstan MW, McColley SA, McCoy K, McKone EF, Munck A, Ratjen F, Rowe SM, Waltz D, Boyle MP; TRAFFIC Study Group; TRANSPORT Study Group. Lumacaftor-Ivacaftor in Patients with Cystic Fibrosis Homozygous for Phe508del CFTR. N Engl J Med. 2015 Jul 16;373(3):220-31. doi: 10.1056/NEJMoa1409547. Epub 2015 May 17. [PubMed]

Claire Wainwright
Two phase 3, randomised, double-blind, placebo-controlled studies were designed to assess the effects of lumacaftor (VX-809), a CFTR corrector, in combination with ivacaftor (VX-770), a CFTR potentiator, (Orkambi) in patients 12 years of age or older who had cystic fibrosis and were homozygous for the Phe508del CFTR mutation. In both studies, patients were randomly assigned to receive either lumacaftor (600 mg once daily or 400 mg every 12 hours) in combination with ivacaftor (250 mg every 12 hours) or matched placebo for 24 weeks. The primary end point was the absolute change from baseline in the percentage of predicted forced expiratory volume in 1 second (FEV1) at week 24.
A total of 1108 patients underwent randomization and received study drug. The mean baseline FEV1 was 61% of the predicted value. In both studies, there were significant improvements in the primary end point in both lumacaftor-ivacaftor dose groups; the difference between active treatment and placebo with respect to the mean absolute improvement in the percentage of predicted FEV1 ranged from 2.6 to 4.0 percentage points (P<0.001), which corresponded to a mean relative treatment difference of 4.3 to 6.7% (P<0.001). Pooled analyses showed that the rate of pulmonary exacerbations was 30 to 39% lower in the lumacaftor-ivacaftor groups than in the placebo group; the rate of events leading to hospitalization or the use of intravenous antibiotics was lower in the lumacaftor-ivacaftor groups as well. The incidence of adverse events was generally similar in the lumacaftor-ivacaftor and placebo groups. The rate of discontinuation due to an adverse event was 4.2% among patients who received lumacaftor-ivacaftor versus 1.6% among those who received placebo.
These data show that lumacaftor in combination with ivacaftor provided a benefit for patients with cystic fibrosis homozygous for the Phe508del CFTR mutation.; benefit was a modest 3% improvement in FEV1 and 35% decrease in pulmonary exacerbations.
2015 Yousef S, Solomon GM, Brody A, Rowe SM, Colin AA. Improved clinical and radiographic outcomes after treatment with ivacaftor in a young adult with cystic fibrosis with the P67L CFTR mutation. Chest 2015; 147(3):e79-82. doi: 10.1378/chest.14-1198. [PubMed]
Originally approved for the G511D CFTR mutation, ivacaftor is now approved for eight additional alleles exhibiting gating defects and has also been tested in R117H, a CFTR mutation with residual function that exhibits abnormal gating. P67L is a class 4 conductance (non-gating) mutation exhibiting residual CFTR function. The authors report marked clinical improvement, normalisation of spirometry, and dramatic reduction in radiographic structural airway changes after > 1 year of treatment with ivacaftor in a young adult with the compound heterozygous genotype P67L/F508del CFTR.
The case suggests that ivacaftor may have a potential benefit for patients with CF with non-gating mutations.
2016 2016 2016
2016 Adam RJ, Hisert KB, Dodd JD, Grogan B, Launspach JL, Barnes JK, Gallagher CG, Sieren ACI. Acute administration of ivacaftor to people with cystic fibrosis and a G551D-CFTR mutation reveals smooth muscle abnormalities. Insight. 2016 Apr 7;1(4):e86183. [PubMed]
Airflow obstruction is common in cystic fibrosis (CF), yet the underlying pathogenesis remains incompletely understood. People with CF often exhibit airway hyper-responsiveness, CF transmembrane conductance regulator (CFTR) is present in airway smooth muscle (ASM), and ASM from newborn CF pigs has increased contractile tone, suggesting that loss of CFTR causes a primary defect in ASM function. The authors hypothesized that restoring CFTR activity would decrease smooth muscle tone in people with CF. To increase or potentiate CFTR function, they administered ivacaftor to 12 adults with CF with the G551D-CFTR mutation; ivacaftor stimulates G551D-CFTR function.
The authors studied people before and immediately after initiation of ivacaftor (48 hours) to minimize secondary consequences of CFTR restoration. They tested smooth muscle function by investigating spirometry, airway distensibility, and vascular tone.
The ivacaftor rapidly restored CFTR function, indicated by reduced sweat chloride concentration. Airflow obstruction and air trapping also improved. Airway distensibility increased in airways less than 4.5 mm but not in larger-sized airways. To assess smooth muscle function in a tissue outside the lung, they measured vascular pulse wave velocity (PWV) and augmentation index, which both decreased following CFTR potentiation. Finally, change in distensibility of <4.5-mm airways correlated with changes in pulse wave velocity.
Acute CFTR potentiation provided a unique opportunity to investigate CFTR-dependent mechanisms of CF pathogenesis. The rapid effects of ivacaftor on airway distensibility and vascular tone suggest that CFTR dysfunction may directly cause increased smooth muscle tone in people with CF and that ivacaftor may relax smooth muscle.
2016 Bratcher PE; Rowe SM; Reeves G; Roberts T; Szul T; Harris WT; Tirouvanziam R; Gaggar A. Alterations in blood leukocytes of G551D-bearing cystic fibrosis patients undergoing treatment with ivacaftor. J Cyst Fibros 2016; 15(1):67-73. [PubMed]

Ivacaftor improves clinical outcome by potentiation of mutant G551D CFTR. Due to the presence of CFTR in monocytes and polymorphonuclear neutrophils (PMNs), we hypothesized that ivacaftor may impact leukocyte activation. METHODS: We examined blood leukocytes from G551D CF subjects prior to and at one and six months after receiving ivacaftor. Blood leukocytes from ivacaftor-naive G551D, F508del, and healthy controls were also treated with ivacaftor ex vivo to assess mutation-specific effects.Compared to healthy controls, G551D CF subjects had significantly higher expression of active CD11b on PMNs and of CD63 on monocytes, which were normalized by in vivo ivacaftor treatment. Ex vivo exposure to ivacaftor of blood cells from G551D, but not F508del and healthy subjects, resulted in changes in CXCR2 and CD16 expression on PMNs.
The authors concluded in vivo and ex vivo exposure of G551D CF leukocytes to ivacaftor resulted in an altered activation profile, suggesting mutation-specific leukocyte modulation
Dr. Preston Bratcher is a scientist working at National Jewish Health, Denver; his research is focused on pulmonary inflammation and the innate immune system of the lung.
2016 Borowitz D, Lubarsky B, Wilschanski M, Munck A, Gelfond D, Bodewes F, Schwarzenberg SJ. Nutritional Status Improved in Cystic Fibrosis Patients with the G551D Mutation After Treatment with Ivacaftor. Dig Dis Sci. 2016 Jan;61(1):198-207. doi: 10.1007/s10620-015-3834-2. Epub 2015 Aug 7. [PubMed]

Drucy Borowitz
To further analyze improvements in weight and body mass index (BMI) in two studies of ivacaftor in patients aged ≥6years with CF and the G551D mutation.Patients were randomized 1:1 to ivacaftor 150mg or placebo every 12h for 48weeks. Primary end point (lung function) was reported previously. Other outcomes included weight and height measurements and CF Questionnaire-Revised (CFQ-R).Studies included 213 patients (aged≤20years, n=105; aged>20years, n=108).
2017 Casciaro R, Costa S, Dang P, Majo F, Ros M. Lumacaftor/ivacaftor combination therapy for cystic fibrosis: A nationwide survey among clinicians. Clin Respir J. 2017 Jul 31. doi: 10.1111/crj.12677. [Epub ahead of print] [28759146]
This was a letter the journal. Not reviewed.
2016 Davies JC; Cunningham S; Harris WT; Lapey A; Regelmann WE; Sawicki GS; Southern KW; Robertson S; Green Y; Cooke J; Rosenfeld M; KIWI Study Group. Safety, pharmacokinetics, and pharmacodynamics of ivacaftor in patients aged 2-5 years with cystic fibrosis and a CFTR gating mutation (KIWI): an open-label, single-arm study.The Lancet Respir Med 2016; 4(2):107-15.[PubMed]

Jane Davies
Ivacaftor has been shown to be a safe, effective treatment for cystic fibrosis in patients aged 6 years or older with a CFTR gating mutation. The authors aimed to assess the safety, pharmacokinetics, and pharmacodynamics of ivacaftor in children aged 2-5 years.In the two-part KIWI study, we enrolled children aged 2-5 years weighing 8 kg or more with a confirmed diagnosis of cystic fibrosis and a CFTR gating mutation on at least one allele from 15 hospitals in the USA, UK, and Canada. Participants received oral ivacaftor 50 mg (if bodyweight <14 kg) or 75 mg (if bodyweight >14 kg) every 12 h for 4 days in part A (to establish the short-term safety of doses for subsequent assessment in part B), and then for 24 weeks in part B (to assess safety and longer-term pharmacodynamics). Children could participate in both or just one part of the study. Primary outcomes were pharmacokinetics and safety, analysed in all patients who received at least one dose of ivacaftor. Secondary outcomes were absolute change from baseline in sweat chloride concentrations and bodyweight, body-mass index (BMI), and height Z scores, and pharmacokinetic parameter estimation of ivacaftor. This study is registered with ClinicalTrials.gov, number NCT01705145.
Between Jan 8, 2013, and March 1, 2013, nine patients were enrolled onto part A of the study, all of whom completed the 4 day treatment period, and eight of whom took part in part B. Between June 28, 2013, and Sept 26, 2013, 34 patients were enrolled in part B, 33 of whom completed the 24 week treatment period. All patients received at least one dose of ivacaftor. Results of ivacaftor pharmacokinetics suggested that exposure was similar to that reported in adults (median Cmin were 536 ng/mL for the 50 mg dose; 580 ng/mL for the 75 mg dose; median ivacaftor AUC values were 9840 ng x h/mL and 10 200 ng x h/mL, respectively). Common adverse events in part B included cough (in 19 [56%] of 34 patients) and vomiting (in ten [29%]). Five (15%) patients had liver function test (LFT) results that were more than eight times higher than the upper limit of normal, four of whom had study drug interrupted, and one of whom had study drug discontinued. Six (18%) of 34 patients had seven serious adverse events; a raised concentration of transaminases was the only serious adverse event regarded as related to ivacaftor and the only adverse event that resulted in study treatment discontinuation. At week 24, in patients for whom we had data, sweat chloride had changed from baseline by a mean of -46.9 mmol/L (SD 26.2, p<0.0001), weight Z score by 0.2 (0.3; p<0.0001), BMI Z score by 0.4 (0.4, p<0.0001), and height Z score by -0.01 (0.3; p=0.84).
Ivacaftor at doses of 50 mg and 75 mg seems to be safe in children aged 2-5 years with cystic fibrosis with a gating mutation followed up for 24 weeks, although the frequency of elevated LFTs suggests that monitoring should be frequent in young children, particularly those with a history of elevated LFTs. Results of an ongoing extension study assessing durability of these effects and longer-term safety are warranted.
– This study confirmed that ivacaftor was safe and effective for children aged 2-5 years. Full abstract included in view of importance.
See comment from Yammine S et al, 2016 below for comment on the dose and effect on liver function in young children taking Ivacaftor.
2016 Dryden C; Wilkinson J; Young D; Brooker RJ; Scottish Paediatric Cystic Fibrosis Managed Clinical Network (SPCFMCN). The impact of 12 months treatment with ivacaftor on Scottish paediatric patients with cystic fibrosis with the G551D mutation: a review. Arch Dis Child 2016 Jun 10. [PubMed]
The authors reviewed the impact of ivacaftor on Scottish paediatric patients with cystic fibrosis >6 years of age after 12 months of treatment. Statistically significant improvements in FEV1 and body mass index and a reduction in sweat chloride, all comparable with previously published data were observed. The findings also suggested reduced use of intravenous antibiotics and oral antibiotics. No significant adverse effects were observed but a possible association with cataract formation could not be excluded.
– This review suggests that, in the short term at least, ivacaftor is effective and safe in Scottish paediatric patients >6 years of age with G551D.
Johanna F Dekkers, Gitte Berkers, Evelien Kruisselbrink, Annelotte Vonk, Hugo R de Jonge, Hettie M Janssens, Inez Bronsveld, Eduard A van de Graaf, Edward E S Nieuwenhuis, Roderick H J Houwen, Frank P Vleggaar, Johanna C Escher, Yolanda B de Rijke, Christof J Majoor, Harry G M Heijerman, Karin M de Winter-de Groot, Hans Clevers, Cornelis K van der Ent, Jeffrey M Beekman. Characterizing responses to CFTR-modulating drugs using rectal organoids derived from subjects with cystic fibrosis. Sci Transl Med 2016 Jun 22;8(344):344ra84.doi: 10.1126/scitranslmed.aad8278. [PubMed]

Jeffrey Beekman

Johanna Dekkers
Identifying subjects with cystic fibrosis (CF) who may benefit from cystic fibrosis transmembrane conductance regulator (CFTR)-modulating drugs is time-consuming, costly, and especially challenging for individuals with rare uncharacterized CFTR mutations. We studied CFTR function and responses to two drugs-the prototypical CFTR potentiator VX-770 (ivacaftor/KALYDECO) and the CFTR corrector VX-809 (lumacaftor)-in organoid cultures derived from the rectal epithelia of subjects with CF, who expressed a broad range of CFTR mutations. We observed that CFTR residual function and responses to drug therapy depended on both the CFTR mutation and the genetic background of the subjects. In vitro drug responses in rectal organoids positively correlated with published outcome data from clinical trials with VX-809 and VX-770, allowing us to predict from preclinical data the potential for CF patients carrying rare CFTR mutations to respond to drug therapy. We demonstrated proof of principle by selecting two subjects expressing an uncharacterized rare CFTR genotype (G1249R/F508del) who showed clinical responses to treatment with ivacaftor and one subject (F508del/R347P) who showed a limited response to drug therapy both in vitro and in vivo. These data suggest that in vitro measurements of CFTR function in patient-derived rectal organoids may be useful for identifying subjects who would benefit from CFTR-correcting treatment, independent of their CFTR mutation.
Johanna F Dekkers is in the Department of Pediatric Pulmonology, University Medical Center Utrecht, Laboratory of Translational Immunology, Wilhelmina Children’s Hospital. She was awarded the first ECFS Gerd Döring award in 2015. Her description of forskolin induced swelling of intestinal organoids as a disease model for CF was the first disease model in adult stem cell cultures with great impact on CF diagnosis, drug discovery and personalised medicine.
Professor Jeffrey Beekman, the corresponding author, is affiliated with the Department of Pediatric Pulmonology and the Regenerative Medicine Center, Utrecht. He leads the research group.
2016 Elborn JS; Ramsey BW; Boyle MP; Konstan MW; Huang X; Marigowda G; Waltz D; Wainwright CE; VX-809 TRAFFIC and TRANSPORT study groups. Efficacy and safety of lumacaftor/ivacaftor combination therapy in patients with cystic fibrosis homozygous for Phe508del CFTR by pulmonary function subgroup: a pooled analysis. The Lancet Respiratory Medicine. 4(8):617-26, 2016 Aug. [PubMed]

Stuart Elborn
Lumacaftor/ivacaftor combination therapy (Orkambi) has shown clinical benefits in patients with cystic fibrosis homozygous for the Phe508del CFTR mutation; however, pretreatment lung function is a confounding factor that potentially affects the efficacy and safety of this therapy. The authors aimed to assess the efficacy and safety of lumacaftor/ivacaftor therapy in these patients, defined by specific categories of lung function. Both trials (TRAFFIC and TRANSPORT) included in this pooled analysis were multinational, randomised, double-blind, placebo-controlled, parallel-group, phase 3 studies. Eligible patients from 187 participating centres in North America, Australia, and the European Union (both trials) were aged 12 years or older with a confirmed diagnosis of cystic fibrosis, homozygous for the Phe508del CFTR mutation, and with a percent predicted FEV1 (ppFEV1) of 40-90 at the time of screening. Patients were randomly assigned with an interactive web response system (1:1:1) to receive placebo, lumacaftor (600 mg once daily) plus ivacaftor (250 mg every 12 h), or lumacaftor (400 mg every 12 h) plus ivacaftor (250 mg every 12 h) for 24 weeks. Pre-specified subgroup analyses of pooled efficacy and safety data by lung function, as measured by ppFEV1, were done for patients with baseline ppFEV1 (<40 and >40) and screening ppFEV1 (<70 and >70). The primary endpoint was the absolute change from baseline in ppFEV1 at week 24 analysed in all randomised patients who received at least one dose of study drug. Both trials are registered with ClinicalTrials.gov (TRAFFIC: NCT01807923; TRANSPORT: NCT01807949).
Both trials were done between April, 2013, and April, 2014. Of the 1108 patients included in the efficacy analysis, 81 patients had a ppFEV1 that decreased to lower than 40 between screening and baseline and 1016 had a ppFEV1 of 40 or higher at baseline. At screening, 730 had a ppFEV1 of less than 70, and 342 had a ppFEV1 of 70 or higher.
Improvements in the absolute change from baseline at week 24 in ppFEV1 were observed with both lumacaftor/ivacaftor doses in the subgroup with baseline ppFEV1 levels lower than 40 (least-squares mean difference vs placebo was 3.7 percentage points [95% CI 0.5-6.9; p=0.024] in the lumacaftor [600 mg/day]-ivacaftor group and 3.3 percentage points [0.2-6.4; p=0.036] in the lumacaftor [400 mg/12 h]-ivacaftor group). Improvements in ppFEV1 compared with placebo were also reported in the subgroup with baseline ppFEV1 levels of 40 or higher (3.3 percentage points [2.3-4.4; p<0.0001] in the lumacaftor [600 mg per day]-ivacaftor group and 2.8 percentage points [1.7-3.8; p<0.0001] in the lumacaftor [400 mg/12 h]-ivacaftor group). Similar absolute improvements in ppFEV1 compared with placebo were observed in subgroups with screening ppFEV1 levels lower than 70 and ppFEV1 levels of 70 or higher. Increases in body-mass index and reduction in number of pulmonary exacerbation events were observed in both lumacaftor/ivacaftor dose groups compared with placebo across all lung function subgroups. Treatment was generally well tolerated, although the incidence of some respiratory adverse events was higher with lumacaftor/ivacaftor than with placebo in all subgroups. In patients with baseline ppFEV1 levels lower than 40, these adverse events included cough, dyspnoea, and abnormal respiration.
The authors consider these analyses confirm that lumacaftor/ivacaftor combination therapy benefits patients with cystic fibrosis homozygous for Phe508del CFTR who have varying degrees of lung function impairment.
2016 Elborn JS, Ramsey B, Wainwright C, Boyle. Response to: ‘Lumacaftor/ivacaftor for patients homozygous for Phe508del-CFTR: should we curb our enthusiasm?’ by Jones and Barry. (Thorax 2015; 70:215-216. ). Thorax. 2016 Feb;71(2):185-6. doi: 10.1136/thoraxjnl-2015-207611. Epub 2015 Oct 27. [PubMed]
The article by Andy Jones and Peter Barry, to which Stuart Elborn and his co-authors are responding, essentially carries a cautionary message. In contrast to the impressive clinical and physiological response to ivacaftor in people with an Gly551Asp mutation, the response of patients with Phe508del mutations to the lumacaftor/ivacaftor combination is significantly less impressive, doubting “whether the results merit heralding the study as a landmark advance”. The potential problems of the two-drug combination, between which interactions have been reported, also the high cost of treatment are mentioned. Finally, with such modest results, the adverse effect of non-adherence, well described with ivacaftor, would be significant in view of the already modest effects. In conclusion the authors agree “the study represents a success for the CF community and should be welcomed as such; however, the recognition of these results should not represent the “holy grail” for Phe508del homozygote patients is equally important”
In the present response Stuart Elborn and his co-authors consider Jones and Barry’s view to be rather pessimistic. They consider the proof of principle of clinical benefit from a corrector/potentiator combination is a very significant development in CF treatment. The addition of the combination to maximal conventional therapy (as was the case) still demonstrated additional spirometric, exacerbation, quality of life and nutritional effects. The emphasise the primary goal of treatment is to restore CFTR function and they consider this combination therapy represents significant progress and should not be underestimated. The cost of treatment should not impact the interpretation of data. Pharmaceutical companies and health care commissioners must find ways to deliver sustainable funding arrangements that recognise the costs of developing new therapies. Although more effective CFTR modulators may become available, lumacaftor/ivacaftor should not be denied to patients who will benefit.
– At the time of writing (early 2019) Orkambi is still not available in the UK for people with cystic fibrosis although approved in many other European and N. American countries.Even though the improvements with Orkambi are modest the UK patients understandably feel very angry that they are denied the benefits of this treatment.
Frizzell RA, Sheppard DN, Cyr DM, Sorscher EJ, Brodsky JL, Lukacs GL. From CFTR biology toward combinatorial pharmacotherapy: expanded classification of cystic fibrosis mutations. Mol Biol Cell. 2016 Feb 1;27(3):424-33. doi: 10.1091/mbc.E14-04-0935. [PubMed]
More than 2000 mutations in the cystic fibrosis transmembrane conductance regulator (CFTR) have been described that confer a range of molecular cell biological and functional phenotypes. Most of these mutations lead to compromised anion conductance at the apical plasma membrane of secretory epithelia and cause cystic fibrosis (CF) with variable disease severity. Based on the molecular phenotypic complexity of CFTR mutants and their susceptibility to pharmacotherapy, it has been recognised that mutations may impose combinatorial defects in CFTR channel biology. This notion led to the conclusion that the combination of pharmacotherapies addressing single defects (e.g., transcription, translation, folding, and/or gating) may show improved clinical benefit over available low-efficacy mono therapies. Indeed, recent phase 3 clinical trials combining ivacaftor (a gating potentiator) and lumacaftor (a folding corrector) have proven efficacious in CF patients harbouring the most common mutation (deletion of residue F508, ΔF508, or Phe508del).This drug combination was recently approved by the U.S. Food and Drug Administration for patients homozygous for ΔF508. Emerging studies of the structural, cell biological, and functional defects caused by rare mutations provide a new framework that reveals a mixture of deficiencies in different CFTR alleles. Establishment of a set of combinatorial categories of the previously defined basic defects in CF alleles will aid the design of even more efficacious therapeutic interventions for CF patients.
– This article is distributed by The American Society for Cell Biology under license from the author(s). Two months after publication it is available to the public under an Attribution–Noncommercial–Share Alike 3.0 Unreported Creative Commons License (http://creativecommons.org/licenses/by-nc-sa/3.0).
– The beneficial effects of the drug combination of Ivacaftor and Lumacaftor (Orkambi) although approved by the FDA is less effective striking than that of Ivacaftor alone on people with G551D mutation and as yet (2019) has not been approved in the UK.
2016 Gentzsch M; Ren HY; Houck SA; Quinney NL; Cholon DM; Sopha P; Chaudhry IG; Das J; Dokholyan NV; Randell SH; Cyr DM. Restoration of R117H CFTR folding and function in human airway cells through combination treatment with VX-809 and VX-770. Am J PhysioL – Lung Cell Mol PhysioL 311(3):L550-9, 2016 Sep 1. [PubMed]
The potentiator VX-770 was the first CFTR modulator approved by the FDA for treatment of CF patients with the gating mutation G551D. Orkambi is a drug containing VX-770 and corrector VX809 and is approved for treatment of CF patients homozygous for F508del, which has folding and gating defects. At least 30% of CF patients are heterozygous for the F508del mutation with the other allele encoding for one of many different rare CFTR mutations.
Treatment of heterozygous F508del patients with VX-809 and VX-770 (Orkambi) has had limited success, so it is important to identify heterozygous patients that respond to CFTR modulator therapy. R117H is a more prevalent rare mutation found in over 2,000 CF patients. In this study the authors investigated the effectiveness of VX-809/VX-770 therapy on restoring CFTR function in human bronchial epithelial (HBE) cells from R117H/F508del CF patients. They found that VX-809 stimulated more CFTR activity in R117H/F508del HBEs than in F508del/F508del HBEs. R117H expressed exclusively in immortalized HBEs exhibited a folding defect, was retained in the ER, and degraded prematurely. VX-809 corrected the R117H folding defect and restored channel function.
The authors conclude that because R117 is involved in ion conductance, VX-770 acted additively with VX-809 to restore CFTR function in chronically treated R117H/F508del cells. Although treatment of R117H patients with VX-770 has been approved, these studies indicate that Orkambi may be more beneficial for rescue of CFTR function in these patients.
2016 Howlett C, Ronan NJ, NiChroinin M, Mullane D, Plant BJ. Partial restoration of pancreatic function in a child with cystic fibrosis. Lancet Respir Med. 2016 May;4(5):e21-2. doi: 10.1016/S2213-2600(16)30032-7. [PubMed]
The authors observed changes in fecal elastase (FE-1) in a child (aged 6·5 years) after commencing ivacaftor treatment. A female (genotype F508del/G551D ) diagnosed at 4 years and 9 months old, after hospital admission with increased respiratory effort and cough.
FE-1 was measured at diagnosis and was consistent with severe pancreatic insufficiency at less than 15 μg/g. At this time, the patient was started on four 150 mg pancreatin capsules per day. The patient started ivacaftor therapy on her sixth birthday in accordance with local regulatory guidelines.After 6 months of ivacaftor treatment, the patient reported abdominal pain and constipation. As a result, her treatment regimen was reduced by 50% to two 150 mg pancreatin capsules per day. FE-1 was measured and was in the normal range at 259 μg/g. Two subsequent FE-1 measurements were made after 7 months of treatment (118 μg/g and 121 μg/g) and were consistent with moderate pancreatic insufficiency.
The authors of the KIWI study have highlighted the potential for a partial restoration of pancreatic function in early life in some CF patients given ivacaftor (Davies JC et al, 2016). Also a significant 60% reduction in pancreatic enzyme requirement occurred in one 16 year old woman after commencing ivacaftor (Harrison MJ et al, N Eng J Med 2013;369:1280-1282. [PubMed])
– It is encouraging that specific therapy with ivacaftor appears to have a favourable effect on both endocrine and exocrine pancreatic function. Not only does the output of pancreatic enzymes improve, and the enzyme replacement requirement fall, but insulin secretion also improves and even resolution of CF related diabetes has been reported (Hayes D et al, 2014. [PubMed])
Kaminski R, Nazareth D. A successful uncomplicated CF pregnancy while remaining on Ivacaftor. J Cyst Fibros. 2016 Jan;15(1):133-4. doi: 10.1016/j.jcf.2015.11.013. Epub 2015 Dec 14. [PubMed]
A 25 year old (G551D:3272-26A>G) gravida 1, BMI 20.8kg/m2, infected with Achromobacter xylosoxidose. On Ivacaftor since 2013 following which her FEV1 rose from 85% to 95%. With the patient’s agreement, after discussion, the Ivacaftor was continued through a normal pregnancy with an FEV1 of 95% with two courses of IV antibiotics. A normal 7 lb 8oz baby girl was born at 39 weeks. The mother did not wish to breast feed for reasons unrelated to her treatment.
– This is first report of the use of Ivacaftor throughout pregnancy. Previous animal studies failed to show a risk to the fetus.
2016 Konstan MW, McKone EF, Moss RB, Marigowda G, Tian S, Waltz D, Huang X, Lubarsky B, Rubin J, Millar SJ, Pasta DJ, Mayer-Hamblett N, Goss CH, Morgan W, Sawicki GS. Assessment of safety and efficacy of long-term treatment with combination lumacaftor and ivacaftor therapy in patients with cystic fibrosis homozygous for the F508del-CFTR mutation (PROGRESS): a phase 3, extension study. Respir Med. 2016 Dec 20. pii: S2213-2600(16)30427-1. doi: 10.1016/S2213-2600(16)30427-1. [Epub ahead of print] [PubMed]
24-week safety and efficacy of lumacaftor/ivacaftor (Orkambi) combination therapy was shown in two randomised controlled trials (RCTs)-TRAFFIC and TRANSPORT-in patients with cystic fibrosis who were aged 12 years or older and homozygous for the F508del-CFTR mutation. This present study aimed to assess the long-term safety and efficacy of extended lumacaftor/ivacaftor therapy in this group of patients in PROGRESS, the long-term extension of TRAFFIC and TRANSPORT.PROGRESS was a phase 3, parallel-group, multicentre, 96-week study of patients who completed TRAFFIC or TRANSPORT in 191 sites in 15 countries. Patients were eligible if they were at least 12 years old with cystic fibrosis and homozygous for the F508del-CFTR mutation. Exclusion criteria included any comorbidity or laboratory abnormality that, in the opinion of the investigator, might confound the results of the study or pose an additional risk in administering the study drug to the participant, history of drug intolerance, and history of poor compliance with the study drug. Patients who previously received active treatment in TRANSPORT or TRAFFIC remained on the same dose in PROGRESS.
Patients who had received placebo in TRANSPORT or TRAFFIC were randomly assigned (1:1) to receive lumacaftor (400 mg every 12 h)/ivacaftor (250 mg every 12 h) or lumacaftor (600 mg once daily)/ivacaftor (250 mg every 12 h). The primary outcome was to assess the long-term safety of combined therapy. The estimated annual rate of decline in percent predicted FEV1 (ppFEV1) in treated patients was compared with that of a matched registry cohort. Efficacy analyses were based on modified intention-to-treat, such that data were included for all patients who were randomly assigned and received at least one dose of study drug.
Between Oct 24, 2013, and April 7, 2016, 1030 patients from the TRANSPORT and TRAFFIC studies enrolled in PROGRESS, and 1029 received at least one dose of study drug. 340 patients continued treatment with lumacaftor 400 mg every 12 h/ivacaftor 250 mg every 12 h; 176 patients who had received placebo in the TRANSPORT or TRAFFIC studies initiated treatment with lumacaftor 400 mg every 12 h/ivacaftor 250 mg every 12 h, the commercially available dose, for which data are presented. The most common adverse events were infective pulmonary exacerbations, cough, increased sputum, and haemoptysis. Modest blood pressure increases seen in TRAFFIC and TRANSPORT were also observed in PROGRESS. For patients continuing treatment, the mean change from baseline in ppFEV1 was 0·5 (95% CI -0·4 to 1·5) at extension week 72 and 0·5 (-0·7 to 1·6) at extension week 96; change in BMI was 0·69 (0·56 to 0·81) at extension week 72 and 0·96 (0·81 to 1·11) at extension week 96. The annualised pulmonary exacerbation rate in patients continuing treatment through extension week 96 (0·65, 0·56 to 0·75) remained lower than the placebo rate in TRAFFIC and TRANSPORT. The annualised rate of ppFEV1 decline was reduced in lumacaftor/ivacaftor-treated patients compared with matched controls (-1·33, -1·80 to -0·85 vs -2·29, -2·56 to -2·03). The efficacy and safety profile of the lumacaftor 600 mg once daily/ivacaftor 250 mg every 12 h groups was generally similar to that of the lumacaftor 400 mg every 12 h/ivacaftor 250 mg every 12 h groups.
The authors concluded the long-term safety profile of lumacaftor/ivacaftor combination therapy (Orkambi) was consistent with previous RCTs. Benefits continued to be observed with longer-term treatment, and lumacaftor/ivacaftor was associated with a 42% slower rate of FEV1 decline than in matched registry controls.
– An important review reproduced here in some detail. Although not as convincing as the response of people with G551D to ivacaftor, there is a significant fall in frequency of exacerbations which appears to be an increasing valuable endpoint.
2016 McColley SA. A safety evaluation of ivacaftor for the treatment of cystic fibrosis. Expert Opin Drug Saf. 2016 Apr 7:1-7. [Epub ahead of print] [PubMed]
This article reviews ivacaftor safety. Areas covered: Safety findings in ivacaftor clinical trials, and reported subsequently, were accessed by a PubMed search using key words “VX-770” or “ivacaftor”. Additional information was accessed via Google Search. Transaminitis (“raised transaminase coupled with non-specific hepatitis”) was noted in ivacaftor and combination lumacaftor-ivacaftor trials.
Ivacaftor was associated with cataracts in juvenile rat pups in pre-clinical studies; non-congenital cataracts have been found in children taking ivacaftor. Ivacaftor is a CYP3A substrate; CYP3A inhibitors and inducers should be avoided during its administration. Ivacaftor and its M1 metabolite may inhibit CYP3A and P-gp; therefore, ivacaftor may increase systemic exposure to drugs which are substrates of CYP3A and/or P-gp, increasing the potential for adverse events.
Expert opinion: Ivacaftor therapy may be associated with ocular and hepatic side effects; specific recommendations for monitoring are available.The authors advise potential drug interactions should be evaluated in patients taking ivacaftor. High clinical efficacy suggests that the risk benefit ratio of ivacaftor favors therapy.
2016 Milla CE, Ratjen F, Marigowda G, Liu F, Waltz D, Rosenfeld M; VX13-809-011 Part B Investigator Group. Lumacaftor/Ivacaftor in Patients Aged 6-11 Years With Cystic Fibrosis Homozygous for F508del-CFTR. Am J Respir Crit Care Med. 2016 Nov 2. [Epub ahead of print] [PubMed]
Combination lumacaftor/ivacaftor has been shown to improve lung function and other endpoints in patients aged ≥12 years with cystic fibrosis homozygous for F508del-CFTR but has not been assessed in younger patients.
This open-label phase 3 trial evaluated the safety, tolerability, pharmacodynamics, and efficacy of lumacaftor/ivacaftor combination therapy in patients aged 6-11 years with cystic fibrosis homozygous for F508del-CFTR. Patients (N = 58) received 200 mg lumacaftor/250 mg ivacaftor orally every 12 hours for 24 weeks in addition to their existing cystic fibrosis medications.
Lumacaftor/ivacaftor was well tolerated; the safety profile was generally similar to that observed in larger lumacaftor/ivacaftor trials in older patients. Four patients discontinued (two due to drug-related adverse events: elevated liver transaminases, n=1; rash, n=1). No safety concerns were associated with spirometry. No significant changes in % predicted FEV1 were observed (change from baseline at Week 24, +2.5 percentage points; 95% CI, -0.2 to 5.2; P = 0.0671). At Week 24, significant improvements from baseline were observed in sweat chloride (-24.8 mmol/L; 95% CI, -29.1 to -20.5; P < 0.0001), BMI z score (+0.15; 95% CI, 0.08 to 0.22; P < 0.0001), Cystic Fibrosis Questionnaire-Revised respiratory domain score (+5.4; 95% CI, 1.4 to 9.4; P = 0.0085), and lung clearance index 2.5 (-0.88; 95% CI, -1.40 to -0.37; P = 0.0018).
– Lumacaftor/ivacaftor was well tolerated in this young population; no new safety concerns were identified. Improvements in lung clearance index, sweat chloride, nutritional status, and health-related quality of life were observed after 24 weeks of treatment.
O’Connor MG; Seegmiller A. The effects of ivacaftor on CF fatty acid metabolism: An analysis from the GOAL study. J Cyst Fibros 2016 Jul 26.[PubMed]
Abnormalities in fatty acid metabolism have previously been shown to be a characteristic of CFTR dysfunction. The authors hypothesized that as a reflection of this clinical improvement, ivacaftor would improve plasma fatty acid levels and decrease urine prostaglandin E metabolite levels. They analyzed plasma fatty acid levels and urine prostaglandin E metabolites (PGE-M) in 40 subjects with CF participating in the G551D observational (GOAL) study who demonstrated response to the medication by a significant decrease in sweat Cl levels.
The authors showed that ivacaftor reduces inflammatory PGE without fully correcting the plasma fatty acid abnormalities of CF. Age-related differences in fatty acid levels were observed, that may be a result of other clinical factors, such as diet, clinical care, or drug response.
– Another chapter in the CF – fatty acid story!
2016 Rowe SM, McColley SA, Rietschel E, Li X, Bell SC, Konstan MW, Marigowda G, Waltz D, Boyle MP; VX09‐809‐102 Study Group.Lumacaftor/Ivacaftor Treatment of Patients with Cystic Fibrosis Heterozygous for F508del-CFTR. Ann Am Thorac Soc. 2016 Nov 29. [Epub ahead of print] [PubMed]
Lumacaftor/ivacaftor treatment (≤28 days) in patients with cystic fibrosis (CF) heterozygous for F508del-CFTR did not improve lung function. This study was to evaluate an optimised lumacaftor/ivacaftor dosing regimen with longer duration in a cohort of patients heterozygous for F508del-CFTR.
Patients age ≥18 years with a confirmed CF diagnosis and percent predicted forced expiratory volume in 1 second (ppFEV1) of 40 to 90 were randomised to lumacaftor/ivacaftor (400 mg/250 mg every 12 hours) or placebo daily for 56 days. Primary outcomes were change in ppFEV1 at day 56 and safety. Other disease markers were evaluated.Of 126 patients; 119 (94.4%) completed the study. Lumacaftor/ivacaftor was well tolerated, although chest tightness and dyspnea occurred more frequently with active treatment than with placebo (27.4% vs 14.3% and 14.5% vs 6.3%, respectively). Mean (SD) ppFEV1 at baseline was 62.9 (14.3) [active treatment] and 60.1 (14.0) [placebo]. Absolute change in ppFEV1 (least squares mean [SE]) at day 56 was -0.6 (0.8) [active treatment] and -1.2 (0.8) percentage points [placebo] (P = 0.60). CF respiratory symptom scores improved by a mean of 5.7 points versus a decrease of -0.8 for placebo (P < 0.01). No changes in body mass index (BMI) occurred. Change from baseline in sweat chloride (least squares mean [SE]) at day 56 was -11.8 (1.3) mmol/L [active treatment] and -0.8 (1.2) mmol/L [placebo] (P < 0.0001).
The authors concluded sweat chloride and respiratory symptom scores improved with lumacaftor/ivacaftor, though no meaningful benefit was seen in ppFEV1 and BMI in patients heterozygous for F508del-CFTR.
– This is a modest effect for patients heterozygous for F508del which would be unlikely to result in the treatment being recommended for patients heterozygous for F508del – certainly in the UK where the combination therapy is not even approved by NICE for patients homozygous for F508del.
Suthoff ED; Bonafede M; Limone B; O’Callaghan L; Sawicki GS; Wagener JS. Healthcare resource utilization associated with ivacaftor use in patients with cystic fibrosis.J Med Econom 2016; 19(9):845-51. [PubMed]
The objective of this analysis was to analyse the impact of ivacaftor on health resource utilisation through analysis of claims data. Ivacaftor therapy was associated with significant reductions in hospitalisations along with high rates of adherence to treatment over 12 months.
2016 Taylor-Cousar J, Niknian M, Gilmartin G, Pilewski JM; VX11-770-901 investigators. Effect of ivacaftor in patients with advanced cystic fibrosis and a G551D-CFTR mutation: Safety and efficacy in an expanded access program in the United States.J Cyst Fibros. 2016 Jan;15(1):116-22. doi: 10.1016/j.jcf.2015.01.008. Epub 2015 Feb 11 [PubMed]
Patients with severe lung disease were excluded from the randomised Phase 3 trials. This open-label study was designed to provide ivacaftor to patients in critical medical need prior to commercial product availability. CF patients aged ≥6years with a G551D-CFTR mutation and FEV1≤40% predicted or listed for lung transplant received ivacaftor 150mg every 12h. The primary endpoint was safety as determined by adverse events. Secondary endpoints included assessment of lung function and weight. The rate of serious adverse events was consistent with disease severity.
At 24 weeks of treatment with ivacaftor, there was a mean absolute increase in percent predicted FEV1 of 5.5 percentage points and a 3.3kg mean absolute increase in weight from baseline.
– The authors concluded that in patients with severe lung disease, ivacaftor was well tolerated and was associated with improved lung function and weight gain. This appears to be the reported experience of others
2016 Yammine S, Singer F, Latzin P. CFTR modulation for young children with cystic fibrosis. Lancet Respir Med. 2016 Feb;4(2):84-5. doi: 10.1016/S2213-2600 (16)00009-6. Epub 2016 Jan 21. No abstract available. [PubMed]
This is a comment on Davies JC, Cunningham S, Harris WT, et al: Safety, pharmacokinetics, and pharmacodynamics of ivacaftor in patients aged 2–5 years with cystic fibrosis and a . Lancet Respir Med 2016.(see above in this section)
In The Lancet Respiratory Medicine, Jane C Davies and colleagues reported data on safety and pharmacokinetics from an open-label, single-arm ivacaftor trial in children aged 2–5 years with at least one CFTR gating mutation. They reported a similar safety profile and pharmacokinetics as reported in adults. The most frequently reported adverse events in children were cough in 19 (56%) of 34 patients and vomiting in ten (29%). The drug has a proven efficacy and good plasma concentration, despite the high occurrence of vomiting. This finding raises the question as to whether or not the suggested dose is indeed needed to achieve therapeutic benefit. Particular attention has been paid to the rise in liver enzymes in 15% of the children, which has not been described to such an extent in patients older than 5 years. The role of ursocholic acid remains unclear, but additional monitoring of liver function in preschool children is suggested.
– Comment on the dose and effect on liver function in young children taking Ivacaftor.
2016 Zeybel GL; Pearson JP; Krishnan A; Bourke SJ; Doe S; Anderson A; Faruqi S; Morice AH; Jones R; McDonnell M; Zeybel M; Dettmar PW; Brodlie M; Ward C. Ivacaftor and symptoms of extra-oesophageal reflux in patients with cystic fibrosis and G551D mutation. J Cyst Fibrosis 2016 Jul 27. [PubMed]
Extra-oesophageal reflux (EOR) may lead to micro aspiration in patients with cystic fibrosis (CF), a probable cause of deteriorating lung function. Successful clinical trials of ivacaftor highlight opportunities to understand EOR in a real world study. METHODS: Data from 12 patients with CF and the G551D mutation prescribed ivacaftor (150mg bd) was collected at baseline, 6, 26 and 52 weeks. The changes in symptoms of EOR were assessed by questionnaire (reflux symptom index (RSI) and Hull airway reflux questionnaire (HARQ)) Six patients presented EOR at baseline (RSI >13; median 13; range 2-29) and 5 presented airway reflux (HARQ >13; median 12; range 3 to 33). Treatment with ivacaftor was associated with a significant reduction of EOR symptoms (P<0.04 versus baseline) denoted by the reflux symptom index and Hull airway reflux questionnaire.
The authors concluded ivacaftor treatment was beneficial for patients with symptoms of EOR, thought to be a precursor to micro-aspiration.
2017 2017 2017
2017 Barnaby R, Koeppen K, Nymon A, Hampton TH, Berwin B, Ashare A, Stanton B. Lumacaftor (VX-809) restores the ability of CF macrophages to phagocytose and kill Pseudomonas aeruginosa. Am J Physiol Lung Cell Mol Physiol. 2017 Nov 16:ajplung.00461.2017. doi: 10.1152/ajplung.00461.2017. [Epub ahead of print] [Pubmed]
Studies were conducted to examine the effects of lumacaftor alone and in combination with ivacaftor (i.e., Orkambi) on the ability of human CF (del508Phe/del508Phe) monocyte derived macrophages (MDMs) to phagocytose and kill P. aeruginosa. Lumacaftor alone restored the ability of CF MDMs to phagocytose and kill P. aeruginosa to levels observed in MDMs obtained from non-CF donors (WT-CFTR). This effect contrasts with the partial correction (~15%) of del508Phe Cl- secretion of airway epithelial cells by lumacaftor. Ivacaftor reduced the ability of lumacaftor to stimulate phagocytosis and killing of P. aeruginosa. Lumacaftor had no effect on P. aeruginosa-stimulated cytokine secretion by CF MDMs. Ivacaftor (5 µM) alone, or in combination with lumacaftor, reduced the secretion of several pro-inflammatory cytokines.
The authors suggest the clinical efficacy of Orkambi may be related in part to the ability of lumacaftor to stimulate phagocytosis and killing of P. aeruginosa by macrophages.
2017 Dagan A, Cohen-Cymberknoh M, Shteinberg M, Levine H, Vilozni D, Bezalel Y, Bar Aluma BE, Sarouk I, Ashkenazi M Lavie M, Tsabari R, Blau H, Kerem E, Bentur L, Efrati O, Livnat G. Ivacaftor for the p.Ser549Arg (S549R) gating mutation – The Israeli experience. Respir Med. 2017 Oct;131:225-228. doi: 10.1016/j.rmed.2017.08.026. Epub 2017 Sep 1. [Pubmed]
Information about the efficacy of ivacaftor in patients carrying the rare p.Ser549Arg (S549R) CFTR mutation is sparse. Data obtained from CF patients receiving ivacaftor for one year is reported. Eight CF patients, mean age 21 ± 10 years, received ivacaftor. After one year, significant improvement was found in FEV1, increasing from 74% to 88% (p < 0.001), FVC, 89% to 101% (p = 0.019), and FEF25-75, 59%-76% (p = 0.019). Sweat chloride concentration decreased from 116 ± 8 mmol/L to 51 ± 17 mmol/L (p < 0.001), and BMI increased from 20 ± 3 to 22 ± 4 (p = 0.003). Glucose tolerance improved in five patients. There was no significant change in bacterial colonization.
Therefore ivacaftor therapy resulted in significant clinical improvement in patients carrying the p.Ser549Arg (S549R) CFTR mutation.
2017 Dilokthornsakul P, Patidar M, Campbell JD. Forecasting the Long-Term Clinical and Economic Outcomes of Lumacaftor/Ivacaftor in Cystic Fibrosis Patients with Homozygous phe508del Mutation. Value Health. 2017 Dec;20(10):1329-1335. doi: 10.1016/j.jval.2017.06.014. Epub 2017 Aug 1.[Pubmed]
To forecast lifetime outcomes and cost of lumacaftor/ivacaftor combination therapy in patients with cystic fibrosis with homozygous phe508del mutation from the US payer perspective. A lifetime Markov model was developed from a US payer perspective. The model included five health states: 1) mild lung disease (per cent predicted forced expiratory volume in 1 second [FEV1] >70%), 2) moderate lung disease (40% ≤ FEV1 ≤ 70%), 3) severe lung disease (FEV1 < 40%), 4) lung transplantation, and 5) death. All inputs were derived from published literature. The authors estimated lumacaftor/ivacaftor’s improvement in outcomes compared with a non-CF reference population as well as CF-specific mortality estimates.
Lumacaftor/ivacaftor was associated with additional 2.91 life-years (95% credible interval 2.55-3.56) and additional 2.42 quality-adjusted life-years (QALYs) (95% credible interval 2.10-2.98). Lumacaftor/ivacaftor was associated with improvements in survival and QALYs equivalent to 27.6% and 20.7%, respectively, for the survival and QALY gaps between CF usual care and their non-CF peers. The incremental lifetime cost was $2,632,249.
Lumacaftor/ivacaftor increased life-years and QALYs in CF patients with the homozygous phe508del mutation and moved morbidity and mortality closer to that of their non-CF peers but it came with higher cost.
2017 De Boeck K, Davies JC. Where are we with transformational therapies for patients with cystic fibrosis? Curr Opin Pharmacol. 2017 Jun;34:70-75. doi: 10.1016/j.coph.2017.09.005. Epub 2017 Oct 6.[Pubmed]

Jane Davies

Kris De Boeck
Cystic fibrosis is caused by a disturbance in the synthesis or function of the CFTR anion channel. Several types of smallmolecules geared to overcome the underlying defect in specific patient groups are in the clinical pipeline. Two drugs have obtained regulatory approval. The potentiator ivacaftor brings major clinical benefit in patients with CFTR protein expression at the cell membrane; the combination ivacaftor plus corrector lumacaftor brings a modest benefit for patients homozygous for the most common mutation F508del. The busy drug pipeline puts pressure on the finite CF patient population. Improving CFTR function in patients has at times yielded unexpected findings. The initial success with ivacaftor has set high expectations, has pushed drug prices sky high and has resulted in inequity in drug access.
– This is an excellent review by Kris de Boeck and Jane Davies and can be recommended to any readers overwhelmed by the vast amount of information appearing on these new drugs – as is this writer!!!
2017 Donaldson SH, Pilewski JM, Griese M, Cooke J, Viswanathan L, Tullis E, Davies JappearingC, Lekstrom-Himes JA, Wang LT; VX11-661-101 Study Group. Tezacaftor/Ivacaftor in Subjects with Cystic Fibrosis and F508del/F508del-CFTR or F508del/G551D-CFTR. Am J Respir Crit Care Med. 2017 Sep 20. doi: 10.1164/rccm.201704-0717OC. [Epub ahead of print] [Pubmed]

Scott H Donaldson
Tezacaftor (formerly VX-661) is an investigational small molecule that improves processing and trafficking of the cystic fibrosis transmembrane conductance regulator (CFTR) in vitro, and improves CFTR function alone and in combination with ivacaftor. This is a study to evaluate safety and efficacy of tezacaftor monotherapy and tezacaftor/ivacaftor combination therapy in subjects with CF homozygous for F508del or compound heterozygous for F508del and G551D. This was a randomized, placebo-controlled, double-blind, multicenter, phase 2 study (NCT01531673). Subjects homozygous for F508del received tezacaftor (10 mg to 150 mg) qday alone or in combination with ivacaftor 150 mg q12h in a dose escalation phase, as well as in a dosage regimen-testing phase. Subjects compound heterozygous for F508del and G551D taking physician prescribed ivacaftor received tezacaftor 100 mg qday.
Primary endpoints were safety through day 56 and change in sweat chloride from baseline through day 28. Secondary endpoints included change in percent predicted FEV1 (ppFEV1) from baseline through day 28 and pharmacokinetics. The incidence of adverse events was similar across treatment arms.
Tezacaftor 100 mg qday/ivacaftor 150 mg q12h resulted in a 6.04 mmol/L decrease in sweat chloride and 3.75 percentage point increase in ppFEV¬1 in subjects homozygous for F508del and a 7.02 mmol/L decrease in sweat chloride and 4.60 percentage point increase in ppFEV¬1 in subjects compound heterozygous for F508del and G551D from baseline through day 28 (P < 0.05 for all).
The authors consider these results support continued clinical development of tezacaftor 100 mg qday in combination with ivacaftor 150 mg q12h in subjects with CF.
Dr. Scott H Donaldson is Associate Professor of Medicine, Pulmonary Diseases and Critical Care Medicine, University of North Carolina School of Medicine.
2017 Edgeworth D, Keating D, Ellis M, Button B, Williams E, Clark D, Tierney A, Heritier S, Kotsimbos T, Wilson J. Improvement in exercise duration, lung function and well-being in G551D-cystic fibrosis patients: a double-blind, placebo-controlled, randomized, cross-over study with ivacaftor treatment. Clin Sci (Lond). 2017 Jul 16;131(15):2037-2045. doi: 10.1042/CS20170995. Print 2017 Aug 1. [Pubmed]

John Wilson
The effect of ivacaftor, a CFTR-potentiator, on exercise capacity in CF is unknown. Twenty G551D-CF patients were recruited to a single-centre, double-blind, placebo-controlled, 28-day crossover study of ivacaftor. A positive treatment effect on spirometry, BMI (increased), SCT (decreased) and total and activity based CF-specific QOL measures was expected. However, the lack of discernible improvement in VO2max and VE despite other positive changes including spirometric lung function and exercise time with a 28-day ivacaftor intervention suggests that ventilatory parameters are not the sole driver of change in exercise capacity in this study cohort. Investigation over a more prolonged period may delineate the potential interdependencies of the observed discordances over time.
Prof. John Wilson is head of the Cystic Fibrosis Service at The Alfred, Melbourne.
2017 Elborn JS, Ramsey BW, Boyle MP, Konstan MW, Huang X, Marigowda G, Waltz D, Wainwright CE; VX-809 TRAFFIC and TRANSPORT study groups. Efficacy and safety of lumacaftor/ivacaftor combination therapy in patients with cystic fibrosis homozygous for Phe508del CFTR by pulmonary function subgroup: a pooled analysis. Lancet Respir Med. 2016 Aug;4(8):617-626. doi: 10.1016/S2213-2600(16)30121-7. Epub 2016 Jun 10.
Lumacaftor/ivacaftor combination therapy has shown clinical benefits in patients with cystic fibrosis homozygous for the Phe508del CFTR mutation; however, pretreatment lung function is a confounding factor that potentially affects the efficacy and safety of this therapy. We aimed to assess the efficacy and safety of lumacaftor/ivacaftor therapy in these patients, defined by specific categories of lung function.
METHODS:Both trials (TRAFFIC and TRANSPORT) included in this pooled analysis were multinational, randomised, double-blind, placebo-controlled, parallel-group, phase 3 studies. Eligible patients from 187 participating centres in North America, Australia, and the European Union (both trials) were aged 12 years or older with a confirmed diagnosis of cystic fibrosis, homozygous for the Phe508del CFTR mutation, and with a percent predicted FEV1 (ppFEV1) of 40-90 at the time of screening. Patients were randomly assigned with an interactive web response system (1:1:1) to receive placebo, lumacaftor (600 mg once daily) plus ivacaftor (250 mg every 12 h), or lumacaftor (400 mg every 12 h) plus ivacaftor (250 mg every 12 h) for 24 weeks. Prespecified subgroup analyses of pooled efficacy and safety data by lung function, as measured by ppFEV1, were done for patients with baseline ppFEV1 (<40 and ≥40) and screening ppFEV1 (<70 and ≥70). The primary endpoint was the absolute change from baseline in ppFEV1 at week 24 analysed in all randomised patients who received at least one dose of study drug.
FINDINGS: Both trials were done between April, 2013, and April, 2014. Of the 1108 patients included in the efficacy analysis, 81 patients had a ppFEV1 that decreased to lower than 40 between screening and baseline and 1016 had a ppFEV1 of 40 or higher at baseline. At screening, 730 had a ppFEV1 of less than 70, and 342 had a ppFEV1 of 70 or higher. Improvements in the absolute change from baseline at week 24 in ppFEV1 were observed with both lumacaftor/ivacaftor doses in the subgroup with baseline ppFEV1 levels lower than 40 (least-squares mean difference vs placebo was 3·7 percentage points [95% CI 0·5-6·9; p=0·024] in the lumacaftor [600 mg/day]-ivacaftor group and 3·3 percentage points [0·2-6·4; p=0·036] in the lumacaftor [400 mg/12 h]-ivacaftor group). Improvements in ppFEV1 compared with placebo were also reported in the subgroup with baseline ppFEV1 levels of 40 or higher (3·3 percentage points [2·3-4·4; p<0·0001] in the lumacaftor [600 mg per day]-ivacaftor group and 2·8 percentage points [1·7-3·8; p<0·0001] in the lumacaftor [400 mg/12 h]-ivacaftor group). Similar absolute improvements in ppFEV1 compared with placebo were observed in subgroups with screening ppFEV1 levels lower than 70 and ppFEV1 levels of 70 or higher. Increases in body-mass index and reduction in number of pulmonary exacerbation events were observed in both lumacaftor/ivacaftor dose groups compared with placebo across all lung function subgroups. Treatment was generally well tolerated, although the incidence of some respiratory adverse events was higher with lumacaftor/ivacaftor than with placebo in all subgroups. In patients with baseline ppFEV1 levels lower than 40, these adverse events included cough, dyspnoea, and abnormal respiration.
INTERPRETATION:These analyses confirm that lumacaftor/ivacaftor combination therapy benefits patients with cystic fibrosis homozygous for Phe508del CFTR who have varying degrees of lung function impairment.
2017 Fila L; Valentova Bartakova L; Grandcourtova A; Marel M; Drnek R; Bilkova A; Macek M; Drevinek P. Ivacaftor in cystic fibrosis adults: Czech experience with six years of follow-up. Biomed Pap Med Fac Univ Palacky Olomouc, Czech Republic. 160(2):276-9, 2016 Jun.[Pubmed]
Five CF adults with a median age 28.6 years (range 21.4-35.6 years) with median FEV1 45% pred. (range 16-85% pred.) were included in the study. Four subjects were also participants in the STRIVE and PERSIST studies. Altogether, twenty-four patient-years of ivacaftor treatment were analysed. The median FEV1 decline per year decreased from -4.5 to -0.9% pred. (P = 0.043). Reduction in number of days on antibiotic treatment and hospital stays was 21% (P < 0.001) and 75% (P = 0.003), respectively. Improvement and stabilisation of lung function was observed for up to six years of treatment. In a patient with severe airway obstruction, an increase in the FEV1 value (30.4% from baseline) was documented during the first twelve months of treatment.
2017 Hisert KB, Heltshe SL, Pope C, Jorth P, Wu X, Edwards RM, Radey M, Accurso FJ, Wolter DJ, Cooke G, Adam RJ, Carter S, Grogan B, Launspach JL, Donnelly SC1, Gallagher CG, Bruce JE, Stoltz DA, Welsh MJ, Hoffman LR, McKone EF, Singh PK. Restoring Cystic Fibrosis Transmembrane Conductance Regulator Function Reduces Airway Bacteria and Inflammation in People with Cystic Fibrosis and Chronic Lung Infections. Am J Respir Crit Care Med. 2017 Jun 15;195(12):1617-1628. doi: 10.1164/rccm.201609-1954OC.[Pubmed]

Katherine Hisert
Previous work indicates that ivacaftor improves cystic fibrosis transmembrane conductance regulator (CFTR) activity and lung function in people with cystic fibrosis and G551D-CFTR mutations but does not reduce density of bacteria or markers of inflammation in the airway. These findings raise the possibility that infection and inflammation may progress independently of CFTR activity once cystic fibrosis lung disease is established. (see my comments below re. Drittanti et al 1997)
To better understand the relationship between CFTR activity, airway microbiology and inflammation, and lung function in subjects with cystic fibrosis and chronic airway infections, the authors studied 12 subjects with G551D-CFTR mutations and chronic airway infections before and after ivacaftor. They measured lung function, sputum bacterial content, and inflammation, and obtained chest computed tomography scans.
Ivacaftor produced rapid decreases in sputum Pseudomonas aeruginosa density that began within 48 hours and continued in the first year of treatment. However, no subject eradicated their infecting P. aeruginosa strain, and after the first year P. aeruginosa densities rebounded. Sputum total bacterial concentrations also decreased, but less than P. aeruginosa. Sputum inflammatory measures decreased significantly in the first week of treatment and continued to decline over 2 years. Computed tomography scans obtained before and 1 year after ivacaftor treatment revealed that ivacaftor decreased airway mucous plugging.
Ivacaftor caused marked reductions in sputum P. aeruginosa density and airway inflammation and produced modest improvements in radiographic lung disease in subjects with G551D-CFTR mutations. However, P. aeruginosa airway infection persisted. Thus, measures that control infection may be required to realise the full benefits of CFTR-targeting treatments.
Dr. Katherine Hisert (figure) is based in the Division of Pulmonary and Critical Care and Sleep Medicine, Center for Lung Biology, Seattle.
– A paper by Drittanti et al, 1997 (Gene Therapy 1997; 4:1001-1003.[PubMed] in the Nineties Clinical section of this history) deals with this suggestion of inflammation eventually progressing independently of CFTR activity. Drittanti et al suggested that before the onset of chronic infection people with CF can be considered to be in the phase of “CF Disease”i.e. they have various physicochemical alterations in the electrolyte and liquid composition of the airway fluid but no tissue damage. Although they develop respiratory infections these can be eradicated, if treated early with antibiotics and their respiratory function remains stable.
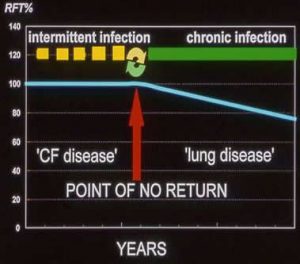
The “point of no return”
However eventually a new respiratory infection is not eradicated and chronic infection of the tissues becomes established. At this stage the patient then enters the phase of “Lung disease”where infection and chronic inflammation become established, self perpetuating and progress independently of the basic CFTR abnormality – this change is referred to as the “Point of no return”and there follows a slow deterioration in their condition, the speed of which is determined by the type and intensity of treatment they receive.
So the aim of modern treatment is to avoid passing the “Point of no return” i.e. prevent or delay for as long as possible the onset of chronic infection of the airways. I represented this concept in the illustration also in the Drittanti et al.1997 entry in this History.
2017 Hubert D, Chiron R, Camara B, Grenet D, Prévotat A, Bassinet L, Dominique S, Rault G, Macey J, Honoré I, Kanaan R, Leroy S, Desmazes Dufeu N, Burgel PR. Real-life initiation of lumacaftor/ivacaftor combination in adults with cystic fibrosis homozygous for the Phe508del CFTR mutation and severe lung disease. J Cyst Fibros 2017;16(3):388-91.[Pubmed]

Dominique Hubert
A study to investigate the short-term adverse events and effectiveness of lumacaftor/ivacaftor combination treatment in adults with cystic fibrosis (CF) and severe lung disease in a real life setting. A multicentre observational study investigated adverse events, treatment discontinuation, FEV1 and body mass index (BMI) one month and three months after lumacaftor/ivacaftor initiation in adults with CF and FEV1 below 40% predicted.
Respiratory adverse events (AEs) were reported by 27 of 53 subjects (51%) and 16 (30%) discontinued treatment. The mean absolute change in FEV1 was +2.06% after one month of treatment (P=0.086) and +3.19% after 3 months (P=0.009). BMI was unchanged.
The authors concluded treatment with lumacaftor/ivacaftor in patients with CF and severe lung disease was discontinued more frequently than reported in clinical trials, due to respiratory adverse events. Nevertheless, the patients who continued treatment had an increase in lung function comparable to what was observed in pivotal trials.
Dr. Dominique Hubert (figure) set up the CF Center at the Hospital Cochin, Paris in 1986. She is involved in the clinical and research aspects of CF and coordinates the activity of the Resource Center and Competence Center for CF.
2017 Horsley A, Barry P. Orkambi in patients with severe disease – Bumps in the road to CFTR modulation. J Cyst Fibros. 2017 May;16(3):11-312. doi: 10.1016/j.jcf.2017.04.008. Epub 2017 Apr 20.[Pubmed]
(This is a very helpful article I have covered here in some detail as there is no abstract on PubMed)

Alex Horsley
CFTR modulation therapies offer the promise to patients and clinicians that true disease modification in CF is possible. In this issue of the journal, we can examine the first published reports of the effects of lumacaftor/ivacaftor (Orkambi™) in clinical practice (Popowicz et al, 2017 [Pubmed]Hubert D et al, 2017 [Pubmed]. Two studies report on patients too ill to qualify for the pivotal phase 3 studies. Although lacking the rigour of clinical trials, these reports provide important and consistent observations that appear to differ from the trials [Wainwright et al, 2015 [Pubmed]; Boyle MP et al, 2014 [Pubmed].
The headline news is that tolerability of Orkambi in patients with FEV1 < 40% predicted is substantially worse than in the registration studies. The authors report discontinuation rates of 25 and 30% before 3 months, the majority due to adverse respiratory events. This stands in striking contrast to the discontinuation rate of 4.6% at the equivalent dose in the phase 3 trials. Hubert et al. describe respiratory adverse events in 51% of patients commencing therapy and Popowicz et al. report similar events in 83% within 24 h, which persisted in two thirds at 1 month. They also report acute deterioration in lung function, including a mean fall in FEV1 of 20% at 1 h. This is very substantial, and potentially destabilising in patients with a median FEV1 of 36% predicted at baseline. These findings raise several questions.
Could these results have been anticipated?
The consistency of both reports suggests that these findings are reflective of the true experience of this compound in clinical practice in patients with low baseline lung function.
What is the cause of these adverse events?
Similar events were not described with ivacaftor monotherapy (Wainwright CE et al, 2015 [Pubmed]; Barry PJ et al, 2014[Pubmed], so the respiratory adverse events described here are almost certainly related to lumacaftor. In the phase 2 trials, there was also a dose related decrement in FEV1 in the lumacaftor monotherapy arm [Boyle MP et al, 2014]. Interestingly, these effects appear to be worse after initiation of the medication, and may abate with time [Konstan et al, 2017 [Pubmed]. Withdrawal of therapy appears to lead to resolution of these symptoms.
Events described as dyspnoea and chest tightness were accompanied by an acute fall in FEV1. Similar decline in FEV1 has also been reported in healthy controls challenged with lumacaftor. In healthy subjects the acute FEV1 decline was attenuated by bronchodilator therapy, leading to speculation that it was caused by bronchospasm (Marigowda et al, 2017 [Pubmed]. Unfortunately, a protective effect of bronchodilators was not witnessed in the studies reported in this issue, and in the study by Popowicz additional bronchodilators did not reverse the fall in FEV1. Popowicz speculates that the phenomenon may instead be due to changing hydration of the airway mucus. Whilst this may be contributory, it doesn’t explain why the same tightness was absent in Gly551Asp patients with severe disease treated with ivacaftor [Barry et al, 2014 [Pubmed]. Nor has this featured in the early reports of the pipeline modulator VX-661 (tezacaftor), which restores CFTR function to a similar level (Pilewski J et al, 2015 [Pubmed]and in a recent press release seems to be at least as effective at improving FEV1. It would therefore appear most likely that this is an off-target effect, but without a clear explanation the treatment to mitigate it also remains uncertain.
What are the clinical implications of these findings?
To prescribe a therapy, which will likely cause adverse events in patients with severe lung disease, requires confidence that it will ultimately be effective. In the phase 3 subgroup analysis by Elborn, patients with FEV1 <40% predicted showed the greatest improvement [Elborn et al, 2016 [Pubmed].. However, these subjects had declined between screening and baseline assessment, so their improvement is at least partially regression back to true baseline. Popowicz describes high rates of ongoing symptoms at 1 month, and no change in lung function. Hubert however reports that in those who tolerate and continue treatment, similar lung function improvements to that in the clinical trials can be achieved, with an absolute increase of 5% in FEV1 seen in a third of patients. Ultimately, lung function changes may not be as important as establishing the effect on exacerbations, which was the clearest demonstration of benefit for a severe Gly551Asp cohort treated with ivacaftor [Barry P J et al, 2014 [Pubmed] The reviewers suggest that as health care professionals, we may need to temper enthusiasm to provide realistic counsel to patients. Media reports of a ‘life-saving’ therapy may mean that the common failure to tolerate therapy can be perceived as disastrous. Our mantra: this may help you feel better, but we might see very little change in lung function and you might well feel worse when you first start taking it. Now we need to quantify these observations to better predict who will benefit, and whether tolerance can be improved, for a population awaiting the realisation of hope.
Dr.Alex Horsley is Senior Lecturer and Consultant in Respiratory Medicine at The University of Manchester and Manchester Adult CF Centre.
2017 Jennings MT, Dezube R, Paranjape S, West NE, Hong G, Braun A, Grant J4, Merlo CA, Lechtzin N. An Observational Study of Outcomes and Tolerances in Patients with Cystic Fibrosis Initiated on Lumacaftor/Ivacaftor. Ann Am Thorac Soc. 2017 Nov;14(11):1662-1666. doi: 10.1513/AnnalsATS.201701-058OC.[Pubmed]
In July 2015, the U.S. Food and Drug Administration approved lumacaftor/ivacaftor for use in patients with cystic fibrosis (CF). This drug targets the primary defect in the CFTR protein that is conferred by the F508del CFTR mutation. As there is limited experience with this therapy outside of clinical trials, this study aims to examine the clinical experience of this new drug in a population with CF.
Retrospective cohort study of individuals followed at the Johns Hopkins CF Center who initiated treatment with lumacaftor/ivacaftor. Patients were followed from 1 year before drug initiation to up to 11 months postinitiation. Key exclusion criteria include previous exposure to lumacaftor/ivacaftor through participation in a clinical trial. Of 116 individuals identified who started lumacaftor/ivacaftor treatment, 46 (39.7%) reported adverse effects related to lumacaftor/ivacaftor, with the vast majority (82.2%) being pulmonary adverse effects, and 20 (17.2%) discontinued lumacaftor/ivacaftor because of adverse effects. The mean change in FEV1% predicted was 0.11% (range: -39% to +20%; P = 0.9). Nineteen individuals had an FEV1% predicted of 40% or less before treatment, and there was a higher percentage of patients in this subgroup who reported adverse effects (57.9%) and a higher percentage of patients who discontinued lumacaftor/ivacaftor (31.6%). Female sex was associated with a higher odds of drug discontinuation (adjusted odds ratio, 3.12, 95% confidence interval, 1.04-9.38).
The authors concluded their study highlights the prevalence of adverse effects in a CF population newly exposed to lumacaftor/ivacaftor and demonstrates a relatively high rate of drug intolerance.
2017 Konstan MW, McKone EF2 Moss RB, Marigowda G, Tian S, Waltz D, Huang X, Lubarsky B, Rubin J, Millar SJ, Pasta DJ, Mayer-Hamblett N, Goss CH, Morgan W, Sawicki GS. Assessment of safety and efficacy of long-term treatment with combination lumacaftor and ivacaftor therapy in patients with cystic fibrosis homozygous for the F508del-CFTR mutation (PROGRESS): a phase 3, extension study. Lancet Respir Med. 2017 Feb;5(2):107-118. doi: 10.1016/S2213-2600(16)30427-1. Epub 2016 Dec 21 [Pubmed]
The 24-week safety and efficacy of lumacaftor/ivacaftor combination therapy was shown in two randomised controlled trials (RCTs)-TRAFFIC and TRANSPORT-in patients with cystic fibrosis who were aged 12 years or older and homozygous for the F508del-CFTR mutation. We aimed to assess the long-term safety and efficacy of extended lumacaftor/ivacaftor therapy in this group of patients in PROGRESS, the long-term extension of TRAFFIC and TRANSPORT. PROGRESS was a phase 3, parallel-group, multicentre, 96-week study of patients who completed TRAFFIC or TRANSPORT in 191 sites in 15 countries. Patients were eligible if they were at least 12 years old with cystic fibrosis and homozygous for the F508del-CFTR mutation. Exclusion criteria included any comorbidity or laboratory abnormality that, in the opinion of the investigator, might confound the results of the study or pose an additional risk in administering the study drug to the participant, history of drug intolerance, and history of poor compliance with the study drug. Patients who previously received active treatment in TRANSPORT or TRAFFIC remained on the same dose in PROGRESS. Patients who had received placebo in TRANSPORT or TRAFFIC were randomly assigned (1:1) to receive lumacaftor (400 mg every 12 h)/ivacaftor (250 mg every 12 h) or lumacaftor (600 mg once daily)/ivacaftor (250 mg every 12 h). The primary outcome was to assess the long-term safety of combined therapy. The estimated annual rate of decline in percent predicted FEV1 (ppFEV1) in treated patients was compared with that of a matched registry cohort. Efficacy analyses were based on modified intention-to-treat, such that data were included for all patients who were randomly assigned and received at least one dose of study drug. This study is registered with ClinicalTrials.gov, number NCT01931839.
FINDINGS: Between Oct 24, 2013, and April 7, 2016, 1030 patients from the TRANSPORT and TRAFFIC studies enrolled in PROGRESS, and 1029 received at least one dose of study drug. 340 patients continued treatment with lumacaftor 400 mg every 12 h/ivacaftor 250 mg every 12 h; 176 patients who had received placebo in the TRANSPORT or TRAFFIC studies initiated treatment with lumacaftor 400 mg every 12 h/ivacaftor 250 mg every 12 h, the commercially available dose, for which data are presented. The most common adverse events were infective pulmonary exacerbations, cough, increased sputum, and haemoptysis. Modest blood pressure increases seen in TRAFFIC and TRANSPORT were also observed in PROGRESS. For patients continuing treatment, the mean change from baseline in ppFEV1 was 0·5 (95% CI -0·4 to 1·5) at extension week 72 and 0·5 (-0·7 to 1·6) at extension week 96; change in BMI was 0·69 (0·56 to 0·81) at extension week 72 and 0·96 (0·81 to 1·11) at extension week 96. The annualised pulmonary exacerbation rate in patients continuing treatment through extension week 96 (0·65, 0·56 to 0·75) remained lower than the placebo rate in TRAFFIC and TRANSPORT. The annualised rate of ppFEV1 decline was reduced in lumacaftor/ivacaftor-treated patients compared with matched controls (-1·33, -1·80 to -0·85 vs -2·29, -2·56 to -2·03). The efficacy and safety profile of the lumacaftor 600 mg once daily/ivacaftor 250 mg every 12 h groups was generally similar to that of the lumacaftor 400 mg every 12 h/ivacaftor 250 mg every 12 h groups.
The long-term safety profile of lumacaftor/ivacaftor combination therapy was consistent with previous RCTs. Benefits continued to be observed with longer-term treatment, and lumacaftor/ivacaftor was associated with a 42% slower rate of ppFEV1 decline than in matched registry controls.
2017 Labaste A, Ohlmann C, Mainguy C, Jubin V, Perceval M, Coutier L, Reix P. Real-life acute lung function changes after lumacaftor/ivacaftor first administration in pediatric patients with cystic fibrosis. J Cyst Fibros. 2017 Nov;16(6):709-712. doi: 10.1016/j.jcf.2017.05.002. Epub 2017 May 18. [Pubmed]
The combination of lumacaftor and ivacaftor (LUM/IVA) has been reported to induce a mean acute absolute drop of -4.1% predicted forced expiratory volume in 1s (FEV1) after a unique administration in healthy subjects. The aim of the present study was to assess acute FEV1 changes after the first dose of LUM/IVA in CF patients. A total of 32 pediatric patients were included. Respiratory manifestations occurred in only 3 patients (9.4%), but FEV1 consistently decreased (-10.4±4.6%, range: -1.5; -21.8%). FEV1 only partially resumed after salbutamol inhalation. Patients with previously known significant reversible airway obstruction and low FEV1 were more at risk of FEV1 decrease.
– A frequent significant drop in FEV1 after first inhalation lumacaftor/ivacaftor in children with CF.
2017 Loo TW, Clarke DM. Corrector VX-809 promotes interactions between cytoplasmic loop one and the first nucleotide-binding domain of CFTR. Biochem Pharmacol. 2017 Jul 15;136:24-31. doi: 10.1016/j.bcp.2017.03.020. Epub 2017 Mar 31. [Pubmed]
A large number of correctors have been identified that can partially repair defects in folding, stability and trafficking of CFTR processing mutants that cause cystic fibrosis (CF). The best corrector, VX-809 (Lumacaftor), has shown some promise when used in combination with a potentiator (Ivacaftor). Understanding the mechanism of VX-809 is essential for development of better correctors. Here, the authors tested their prediction that VX-809 repairs folding and processing defects of CFTR by promoting interactions between the first cytoplasmic loop (CL1) of transmembrane domain 1 (TMD1) and the first nucleotide-binding domain (NBD1).
Their results (which are detailed in the full summary) suggest that the mechanism by which VX-809 promotes maturation and stability of CFTR is by promoting CL1/NBD1 interactions.
2017 McColley SA. A safety evaluation of ivacaftor for the treatment of cystic fibrosis. Cardiopulmonary Comparative Physiology Expert Opin Drug Saf. 2016 May;15(5):709-15. [Pubmed]
Transaminitis (elevated transaminases) was noted in ivacaftor and combination lumacaftor-ivacaftor trials. Ivacaftor was associated with cataracts in juvenile rat pups in pre-clinical studies; non-congenital cataracts have been found in children taking ivacaftor. Ivacaftor is a CYP3A substrate; CYP3A inhibitors (Ketoconazole, Itraconazole, Fluconazole, Cimetidine, Clarithromycin, Erythromycin, Troleandomycin, Grapefruit juice) inducers should be avoided during its administration. Ivacaftor and its M1 metabolite may inhibit CYP3A and P-gp; therefore, ivacaftor may increase systemic exposure to drugs which are substrates of CYP3A and/or P-gp, increasing the potential for adverse events.
Ivacaftor therapy may be associated with ocular and hepatic side effects; specific recommendations for monitoring are available. Potential drug interactions should be evaluated in patients taking ivacaftor. High clinical efficacy suggests that the risk benefit ratio of ivacaftor favours therapy.
Susanna A McColley is Professor of Pediatrics (Pulmonary Medicine) at Northwestern University.
2017 Marigowda G, Liu F, Waltz D. Effect of bronchodilators in healthy individuals receiving lumacaftor/ivacaftor combination therapy.J Cyst Fibros. 2017 Mar;16(2):246-249. doi: 10.1016/j.jcf.2016.11.001. Epub 2016 Nov 25. 27894875 Free full text[Pubmed]
In an open-label, single-center phase 1 pharmacokinetic study in healthy subjects who received lumacaftor (LUM) in combination with ivacaftor (IVA), review of spirometry data showed a transient decline in percent predicted forced expiratory volume in 1s (ppFEV1) within 4h of drug administration. An additional cohort of healthy subjects with normal baseline ppFEV1 values was studied to evaluate the ppFEV1 response to LUM/IVA administration and assess the effect of long-acting bronchodilators (LABDs) and short-acting bronchodilators (SABDs) on ppFEV1 response. The ppFEV1 decline observed at 4h was attenuated following administration of an LABD and reversed following administration of an SABD. Concomitant administration of LUM/IVA with bronchodilators was well tolerated.
These data show that a transient decline in ppFEV1 was observed in healthy subjects following administration of LUM/IVA combination therapy, which can be ameliorated with LABDs or SABDs.
2017 Milla CE, Ratjen F, Marigowda G, Liu F, Waltz D, Rosenfeld M; VX13-809-011 Part B Investigator Group. Lumacaftor/Ivacaftor in Patients Aged 6-11 Years with Cystic Fibrosis and Homozygous for F508del-CFTR. Am J Respir Crit Care Med. 2017 Apr 1;195(7):912-920. doi: 10.1164/rccm.201608-1754OC [Pubmed]
Combination lumacaftor/ivacaftor has been shown to improve lung function and other endpoints in patients aged 12 years and older with cystic fibrosis and homozygous for F508del-CFTR, but it has not been assessed in younger patients. In this open-label phase III trial, we evaluated the safety, tolerability, pharmacodynamics, and efficacy of lumacaftor/ivacaftor combination therapy in patients aged 6-11 years with cystic fibrosis who were homozygous for F508del-CFTR. Patients (N = 58) received 200 mg lumacaftor/250 mg ivacaftor orally every 12 hours for 24 weeks in addition to their existing cystic fibrosis medications.
Lumacaftor/ivacaftor was well tolerated; the safety profile was generally similar to that observed in larger lumacaftor/ivacaftor trials with older patients. Four patients discontinued (two because of drug-related adverse events: elevated liver transaminases, n = 1; rash, n = 1). No safety concerns were associated with spirometry. No significant changes in percent predicted FEV1 were observed (change from baseline at Week 24, +2.5 percentage points; 95% confidence interval [CI], -0.2 to 5.2; P = 0.0671). At Week 24, significant improvements from baseline were observed in sweat chloride (-24.8 mmol/L; 95% CI, -29.1 to -20.5; P < 0.0001), body mass index z score (+0.15; 95% CI, 0.08 to 0.22; P < 0.0001), Cystic Fibrosis Questionnaire-Revised respiratory domain score (+5.4; 95% CI, 1.4 to 9.4; P = 0.0085), and lung clearance index based on lung volume turnover required to reach 2.5% of starting N2concentration (-0.88; 95% CI, -1.40 to -0.37; P = 0.0018).
CONCLUSIONS:
Lumacaftor/ivacaftor was well tolerated in this young population; no new safety concerns were identified. Improvements in lung clearance index, sweat chloride, nutritional status, and health-related quality of life were observed after 24 weeks of treatment.
2017 McGarry ME, Illek B, Ly NP, Zlock L, Olshansky S, Moreno C, Finkbeiner WE, Nielson DW. In vivo and in vitro ivacaftor response in cystic fibrosis patients with residual CFTR function: N-of-1 studies. Pediatr Pulmonol. 2017 Apr;52(4):472-479. doi: 10.1002/ppul.23659. Epub 2017 Jan 9. Full article.[Pubmed]

Megan McGarry
Some CF patients have CFTR in the epithelium with residual CFTR function. The effect of ivacaftor in these patients is unknown. This was a series of randomized, crossover N-of-1 trials of ivacaftor and placebo in CF patients ≥8 years old with potential residual CFTR function (as indicated by intermediate sweat chloride concentration, pancreatic sufficient, or mild bronchiectasis on chest CT). Human nasal epithelium (HNE) was obtained via nasal brushing and cultured. Sweat chloride concentration change was the in vivo outcome. Chloride current change in HNE cultures with ivacaftor was the in vitro outcome.
Three subjects had decreased sweat chloride concentration (-14.8 to -40.8 mmol/L, P < 0.01). Two subjects had unchanged sweat chloride concentration. Two subjects had increased sweat chloride concentration (+23.8 and +27.3 mmol/L, P < 0.001); both were heterozygous for A455E and pancreatic sufficient. Only subjects with decreased sweat chloride concentration had increased chloride current in HNE cultures.
The authors concluded some CF patients with residual CFTR function have decreased sweat chloride concentration with ivacaftor. Increased chloride current in human nasal epithelium cultures among subjects with decreased sweat chloride concentrations may predict clinical response to ivacaftor. Ivacaftor can increase sweat chloride concentration in certain mutations with unclear clinical effect.
Dr. Meghan McGarry (figure) is assistant professor and pediatric pulmonologist at the University of California, San Francisco.
2017 McKinzie CJ, Goralski JL, Noah TL, Retsch-Bogart GZ, Prieur MB. Worsening anxiety and depression after initiation of lumacaftor/ivacaftor combination therapy in adolescent females with cystic fibrosis. J Cyst Fibros. 2017 Jul;16(4):525-527. doi: 10.1016/j.jcf.2017.05.008. Epub 2017 Jun 8.[Pubmed]

Cameron J McKinzie
In both phase III studies of lumacaftor/ivacaftor, as well as an extension study, worsening of mental health was not reported as a common side effect. Here the authors describe five cases in adolescent female patients that suggest a worsening of anxiety or depression associated with its use. In these five patients, two experienced suicidal ideation and three made suicide attempts that resulted in psychiatric hospitalizations
Dr. Cameron Jordan McKinzie (figure) is a Clinical Specialist, Pediatric Pulmonology, Pharmacy Department, University of North Carolina Children’s Hospital.
2017 Milla CE, Ratjen F, Marigowda G, Liu F, Waltz D, Rosenfeld M; VX13-809-011 Investigator Group. Lumacaftor/Ivacaftor in Patients Aged 6-11 Years with Cystic Fibrosis and Homozygous for F508del-CFTR. Am J Respir Crit Care Med. 2017 Apr 1;195(7):912-920. doi: 10.1164/rccm.201608-1754OC. [Pubmed]

Carlos Milla
Combination lumacaftor/ivacaftor has been shown to improve lung function and other endpoints in patients aged 12 years and older with cystic fibrosis and homozygous for F508del-CFTR, but it has not been assessed in younger patients.
In this open-label phase III trial, the authors evaluated the safety, tolerability, pharmacodynamics, and efficacy of lumacaftor/ivacaftor combination therapy in patients aged 6-11 years with cystic fibrosis who were homozygous for F508del-CFTR. Patients (N = 58) received 200 mg lumacaftor/250 mg ivacaftor orally every 12 hours for 24 weeks in addition to their existing cystic fibrosis medications.
Lumacaftor/ivacaftor was well tolerated; the safety profile was generally similar to that observed in larger lumacaftor/ivacaftor trials with older patients. Four patients discontinued (two because of drug-related adverse events: elevated liver transaminases, n = 1; rash, n = 1). No safety concerns were associated with spirometry. No significant changes in percent predicted FEV1 were observed (change from baseline at Week 24, +2.5 percentage points; 95% confidence interval [CI], -0.2 to 5.2; P = 0.0671). At Week 24, significant improvements from baseline were observed in sweat chloride (-24.8 mmol/L; 95% CI, -29.1 to -20.5; P < 0.0001), body mass index z score (+0.15; 95% CI, 0.08 to 0.22; P < 0.0001), Cystic Fibrosis Questionnaire-Revised respiratory domain score (+5.4; 95% CI, 1.4 to 9.4; P = 0.0085), and lung clearance index based on lung volume turnover required to reach 2.5% of starting N2 concentration (-0.88; 95% CI, -1.40 to -0.37; P = 0.0018).
The authors concluded Lumacaftor/ivacaftor was well tolerated in this young population; no new safety concerns were identified. Improvements in lung clearance index, sweat chloride, nutritional status, and health-related quality of life were observed after 24 weeks of treatment.
Dr. Carlos Milla is Professor of Pediatrics (Pulmonary Medicine) at the Lucile Salter Packard Children’s Hospital, Sanford.
2017 Peleg AY, Choo J, Langan K, Edgeworth D, Keating D, Wilson J. Antibiotic exposure and interpersonal variance mask the effect of ivacaftor on respiratory microbiota composition. J Cyst Fibros. 2017 Oct 14. pii: S1569-1993(17)30837-8. doi: 10.1016/j.jcf.2017.08.002. [Epub ahead of print][Pubmed]
Anton Peleg
Ivacaftor effect on the airway microbiome remains poorly characterised. Twenty CF patients with at least one G551D mutation from a single centre were recruited to a 4-month double-blind, placebo-controlled, crossover study of ivacaftor with 28 days of active treatment. No significant difference in microbiota composition was observed in subjects following ivacaftor treatment or placebo (PERMANOVA P=0.95, square root ECV=-4.94, 9479 permutations). Microbiota composition variance was significantly greater between subjects, than within subjects over time (P<0.0001, Mann Whitney U test), and an additional within-patient paired assessment of microbiota similarity was therefore performed. Again, change in microbiota composition was not significantly greater during treatment with ivacaftor compared to placebo (Wilcoxon test, P=0.51). A significant change in microbiota composition was however associated with any change in antibiotic exposure, regardless of whether ivacaftor or placebo was administered (P=0.006). In a small, subgroup analysis of subjects whose antibiotic exposure did not change within the study period, a significant reduction in total bacterial load was observed during treatment with ivacaftor (P=0.004, two-tailed paired Student’s t-test).
The authors concluded the short-term impact of ivacaftor therapy on sputum microbiota composition in patients with G551D mutations are modest compared to those resulting from antibiotic exposure, and may be masked by changes in antibiotic treatment regimen.
Anton Peleg (figure) is Professor of Infectious Diseases and Microbiology, Monash University and Infectious Disease Physician, Alfred Hospital, Melbourne.
~ This is the expected result as when the airways are chronically infected, the progressive inflammatory state in the lungs is less dependent on the disturbed CFTR function, which is influenced by ivacaftor, than the chronic bacterial inflammation (See Drittanti L et al in 1997 Cinical section of this history for a suggested explanation) i.e. when the patient has passed from the “CF Disease” phase to the “Lung Disease” phase.
Iwona M Pranke, Aurélie Hatton, Juliette Simonin, Jean Philippe Jais, Françoise Le Pimpec-Barthes, Ania Carsin, Pierre Bonnette, Michael Fayon, Nathalie Stremler-Le Bel, Dominique Grenet, Matthieu Thumerel, Julie Mazenq, Valerie Urbach , Myriam Mesbahi, Emanuelle Girodon-Boulandet, Alexandre Hinzpeter, Aleksander Edelman, Isabelle Sermet-Gaudelus. Correction of CFTR function in nasal epithelial cells from cystic fibrosis patients predicts improvement of respiratory function by CFTR modulators. Sci Rep 2017 Aug 7;7(1):7375.doi: 10.1038/s41598-017-07504-1. Free PMC article [Pubmed]

Isabelle Sremet-Gaudelius
Clinical studies with modulators of the Cystic Fibrosis Transmembrane conductance Regulator (CFTR) protein have demonstrated that functional restoration of the mutated CFTR can lead to substantial clinical benefit. However, studies have shown highly variable patient responses.
The objective of this study was to determine a biomarker predictive of the clinical response. CFTR function was assessed in vivo via nasal potential difference (NPD) and in human nasal epithelial (HNE) cultures by the response to Forskolin/IBMX and the CFTR potentiator VX-770 in short-circuit-current (∆IscF/I+V) experiments. CFTR expression was evaluated by apical membrane fluorescence semi-quantification. Iscmeasurements discriminated CFTR function between controls, healthy heterozygotes, patients homozygous for the severe F508del mutation and patients with genotypes leading to absent or residual function. ∆IscF/I+V correlated with CFTR cellular apical expression and NPD measurements. The CFTR correctors lumacaftor and tezacaftor significantly increased the ∆IscF/I+V response to about 25% (SEM = 4.4) of the WT-CFTR level and the CFTR apical expression to about 22% (SEM = 4.6) of the WT-CFTR level in F508del/F508del HNE cells. The level of CFTR correction in HNE cultures significantly correlated with the FEV1 change at 6 months in 8 patients treated with CFTR modulators.
Iwona M Pranke is a post-doctoral cell biologist at Inserm U1151 – CNRS UMR 8253 – team 2, Faculté de Médecine Paris Descartes, Paris, France.
Isabelle Sermet-Gaudelus MD, PhD, IS Professor of Pediatrics and Head of the Pediatric Cystic Fibrosis Center. Hopital Necker-Enfants Malades
2017 Ratjen F, Hug C, Marigowda G, Tian S, Huang X, Stanojevic S, Milla CE, Robinson PD, Waltz D, Davies JC; VX14-809-109 investigator group. Efficacy and safety of lumacaftor and ivacaftor in patients aged 6-11 years with cystic fibrosis homozygous for F508del-CFTR: a randomised, placebo-controlled phase 3 trial. Lancet Respir Med. 2017 Jul;5(7):557-567. doi: 10.1016/S2213-2600(17)30215-1. Epub 2017 Jun 9. [Pubmed]

Felix Ratjen
Lumacaftor and ivacaftor combination treatment showed efficacy in patients aged 12 years or older with cystic fibrosis homozygous for F508del-cystic fibrosis transmembrane conductance regulator (CFTR) in placebo-controlled studies and for patients aged 6-11 years with cystic fibrosis homozygous for F508del-CFTR in an open-label study. The authors report efficacy and safety of lumacaftor and ivacaftor in patients with cystic fibrosis aged 6-11 years homozygous for F508del-CFTR.
In this phase 3, randomised, double-blind, placebo-controlled, multicentre study, patients were enrolled at 54 hospitals and medical centres in nine countries (the USA, Australia, Belgium, Canada, Denmark, France, Germany, Sweden, and the UK). Eligible patients weighed at least 15 kg, with a confirmed diagnosis of cystic fibrosis, per cent predicted forced expiratory volume in 1 s (FEV1) of 70 or more, and lung clearance index 2·5 (LCI 2·5) of 7·5 or more at screening (values less than these thresholds were permitted at day 1). All patients were tested for CFTR genotype at screening; eligible patients had to have the F508del-CFTR mutation on both alleles. Exclusion criteria included any comorbidity or laboratory abnormality that might confound the study results or pose additional risk to the patient. Patients were stratified by weight (<25 kg vs. ≥25 kg) and ppFEV1 severity (<90 vs. ≥90) determined at the screening visit, and randomly assigned 1:1 to treatment using an interactive web response system to receive 200 mg lumacaftor and 250 mg ivacaftor every 12 hours or placebo for 24 weeks. The primary endpoint was the mean absolute change in LCI 2·5 from all on-treatment study visits up to and including week 24. All randomly assigned patients who were exposed to any amount of study drug, with treatment assignment as assigned were included in primary and other efficacy analyses. All patients who were exposed to any amount of study drug, with treatment assignment as treated, were included in the safety analysis. This study was registered with ClinicalTrials.gov, number NCT02514473.
Between July 23, 2015, and Sept 20, 2016, a total of 206 patients were enrolled and randomly assigned to receive lumacaftor and ivacaftor (n=104) or placebo (n=102). Two randomly assigned patients were never dosed with study drug (one in the placebo arm due to ineligibility arising from a streptococcal throat infection and one in the lumacaftor and ivacaftor arm due to withdrawal based on refusal to provide blood tests) and were not included in the analyses.
103 patients received at least one dose of lumacaftor and ivacaftor and 101 patients received at least one dose of placebo. For the primary endpoint, the average absolute change in LCI2·5 from baseline over all study visits up to and including the week 24 visit, least squares mean difference was -1·09 units (95% CI -1·43 to -0·75, p<0·0001) for lumacaftor and ivacaftor versus placebo. For the key secondary endpoint of sweat chloride concentration, the least squares mean difference versus placebo was -20·8 mmol/L (95% CI -23·4 to -18·2, average absolute change at day 15/week 4; p<0·0001). The least squares mean difference compared with placebo in absolute change in ppFEV1 from all on-treatment study visits until week 24 was 2·4 (95% CI 0·4-4·4, p=0·0182). 196 (96%) of 204 patients reported adverse events, most of which were mild (87 [43%]) or moderate (98 [48%]). Treatment was discontinued due to adverse events in three (3%) of 103 patients in the lumacaftor and ivacaftor group and two (2%) of 101 patients in the placebo group. Serious adverse events were reported in 13 (13%) of 103 patients in the lumacaftor and ivacaftor group and 11 (11%) of 101 patients in the placebo group.
The authors concluded that treatment with lumacaftor and ivacaftor was associated with statistically significant improvements in lung function, as measured by LCI2·5 and ppFEV1, versus placebo in patients aged 6-11 years with cystic fibrosis homozygous for F508del-CFTR. The overall safety profile was consistent with previous phase 3 studies of lumacaftor and ivacaftor.
– The first important major study on lumacaftor/ivacaftor children aged 6 to 11 years.
2017 Rowe SM, Daines C, Ringshausen FC, Kerem E, Wilson J, Tullis E, Nair N, Simard C, Han L, Ingenito EP, McKee C, Lekstrom-Himes J, Davies JC. Tezacaftor-Ivacaftor in Residual-Function Heterozygotes with Cystic Fibrosis. N Engl J Med. 2017 Nov 23;377(21):2024-2035. doi: 10.1056/NEJMoa1709847. Epub 2017 Nov 3. [Pubmed]Free PMC Article
A randomized, double-blind, placebo-controlled, phase 3, crossover trial to evaluate the efficacy and safety of ivacaftor alone or in combination with tezacaftor, a CFTR corrector, in 248 patients 12 years of age or older who had cystic fibrosis and were heterozygous for the Phe508del mutation and a CFTR mutation associated with residual CFTR function. Patients were randomly assigned to one of six sequences, each involving two 8-week intervention periods separated by an 8-week washout period. They received tezacaftor-ivacaftor, ivacaftor monotherapy, or placebo. The primary end point was the absolute change in the percentage of predicted forced expiratory volume in 1 second (FEV1) from the baseline value to the average of the week 4 and week 8 measurements in each intervention period.
The number of analysed intervention periods was 162 for tezacaftor-ivacaftor, 157 for ivacaftor alone, and 162 for placebo. The least-squares mean difference versus placebo with respect to the absolute change in the percentage of predicted FEV1 was 6.8 percentage points for tezacaftor-ivacaftor and 4.7 percentage points for ivacaftor alone (P<0.001 for both comparisons). Scores on the respiratory domain of the Cystic Fibrosis Questionnaire-Revised, a quality-of-life measure, also significantly favoured the active-treatment groups. The incidence of adverse events was similar across intervention groups; most events were mild or moderate in severity, with no discontinuations of the trial regimen due to adverse events for tezacaftor-ivacaftor and few for ivacaftor alone (1% of patients) and placebo (<1%).
CFTR modulator therapy with tezacaftor-ivacaftor or ivacaftor alone was efficacious in patients with cystic fibrosis who were heterozygous for the Phe508del deletion and a CFTR residual-function mutation.(EXPAND ClinicalTrials NCT02392234).
From the Division of Pulmonary, Allergy, and Critical Care Medicine, University of Alabama at Birmingham, Birmingham (S.M.R.);
2017 Rowe SM, McColley SA, Rietschel E, Li X, Bell SC, Konstan MW, Marigowda G, Waltz D, Boyle MP; VX09-809-102 Study Group. Lumacaftor/Ivacaftor Treatment of Patients with Cystic Fibrosis Heterozygous for F508del-CFTR. Ann Am Thorac Soc. 2017 Feb;14(2):213-219. doi: 10.1513/Annals ATS.201609-689OC.[Pubmed]
Steven Rowe
In a prior study, lumacaftor/ivacaftor treatment (≤28 d) in patients with cystic fibrosis (CF) heterozygous for F508del-CFTR did not improve lung function. This present study was to evaluate an optimized lumacaftor/ivacaftor dosing regimen with a longer duration in a cohort of patients heterozygous for F508del-CFTR. Lumacaftor/ivacaftor (400 mg/250 mg every 12 h) or placebo daily for 56 days. Sweat chloride and respiratory symptom scores improved with lumacaftor/ivacaftor, though no meaningful benefit was seen in ppFEV1 or body mass index in patients heterozygous for F508del-CFTR.
Dr. Steven Rowe (figure) is a pulmonologist in Birmingham, Alabama and is affiliated with University of Alabama at Birmingham Hospital
2017 Ronan NJ, Einarsson GG, Twomey M, Mooney D, Mullane D, NiChroinin M, O’Callaghan G, Shanahan F, Murphy DM, O’Connor OJ, Shortt CA, Tunney MM, Eustace JA, Maher MM, Elborn JS, Plant BJ. CORK study in CF: Sustained improvements in ultra-low dose chest CT scores post CFTR modulation with ivacaftor. 10.1016/j.chest.2017.10.005. [Epub ahead of print] [Pubmed]

Nicola J Ronan
Ivacaftor produces significant clinical benefit in patients with cystic fibrosis (CF) with the G551D mutation. Prevalence of this mutation at Cork CF Centre is 23%. This study assessed the impact of CFTR modulation on multiple modalities of patient assessment.
Thirty-three patients with the G551D mutation were assessed at baseline and prospectively three monthly for one year post initiation of ivacaftor. Change in ultra-low dose chest CT, blood inflammatory mediators, and sputum microbiome were assessed.
Significant improvements in FEV1, BMI and sweat chloride were observed post-ivacaftor. Improvement in ultra-low dose CT scores was observed after treatment with significant mean reductions in total Bhalla score (p< 0.01), peri-bronchial thickening (p = 0.035) and extent of mucus plugging (p< 0.001). The greatest improvements on chest CT were in the extent of mucus plugging. This is consistent with in vitro studies where ivacaftor enhanced airway surface liquid and ciliary beat frequency. Established lung damage was not reversible. Reductions in circulating inflammatory markers, including IL-1β, IL-6, and IL-8 were demonstrated. There was a 30% reduction in the relative abundance of Pseudomonas spp. and an increase in the relative abundance of bacteria associated with more stable community structures. Post-treatment community richness increased significantly (p = 0.03).
The authors concluded early and sustained improvements on ultra-low-dose CT scores suggest it may be a useful method of evaluating treatment response. It was paralleled improvement in symptoms, circulating inflammatory markers, and changes in the lung microbiota.
– Interestingly somewhat different findings to Peleg study described in 2017 section but these Irish patients appeared to be at an earlier stage where the change in CFTR activity and physicochemical conditions within the airways would have an effect on the bacterial content.
Nicola Ronan (figure) is a pulmonologist at Cork University Hospital, Ireland.
2016 Tsabari R; Elyashar HI; Cymberknowh MC; Breuer O; Armoni S; Livnat G; Kerem E; Zangen DH. CFTR potentiator therapy ameliorates impaired insulin secretion in CF patients with a gating mutation. J Cyst Fibros 2016; 15(3):e25-7.[PubMed] To investigate the effect of treatment with ivacaftor on insulin secretion in patients with cystic fibrosis (CF) (DELTAF508\S549R) having CFRD/impaired insulin secretion. A standard OGTT was performed before and after 16weeks of treatment with ivacaftor in 2 sibling patients with CF carrying the S549R gating mutation. The area under the curve (AUC) for glucose and insulin was calculated using the trapezoidal estimation.Before treatment, the OGTT of case 1 showed indeterminate glycemia; the OGTT of case 2 indicated CFRD. After ivacaftor treatment the OGTT demonstrated improved insulin secretion pattern mainly by increased first phase early insulin secretion, resulting in reduction of the AUC of glucose in both cases. The authors concluded the treatment with ivacaftor in patients with CF carrying a gating mutation can ameliorate impaired insulin secretion and suggested further studies and larger cohorts are needed to evaluate the impact of ivacaftor.
2017 Talamo Guevara M, McColley SA. The safety of lumacaftor and ivacaftor for the treatment of cystic fibrosis. Expert Opin Drug Saf. 2017 Nov;16(11):1305-1311. doi: 10.1080/14740338.2017.1372419. Epub 2017 Sep 21. [Pubmed]
This article reviews safety of this therapy. Areas covered: Safety findings in ivacaftor, lumacaftor and combined therapy trials, and reported subsequently through post-approval evaluation, were accessed by PubMed and Google searches using key words ‘VX-770’, ‘ivacaftor’, ‘VX-809’, and ‘lumacaftor’. Transaminitis was seen in ivacaftor and combination trials. Non-congenital cataracts were seen in pre-clinical animal studies and in children taking ivacaftor and combined therapy. Dyspnea occurs in some patients taking lumacaftor and combined therapy and usually resolves without stopping treatment. Lumacaftor is a strong inducer of CYP3A while ivacaftor is a CYP3A sensitive substrate. Combination therapy can decrease systemic exposure of medications that are substrates of CYP3A, decreasing therapeutic effect. Co-administration of lumacaftor-ivacaftor with sensitive CYP3A substrates or CYP3A substrates with narrow therapeutic index is not recommended. Expert opinion: Lumacaftor-ivacaftor therapy may be associated with ocular and hepatic side effects. Specific recommendations for monitoring are available. Dyspnea occurs, especially during initiation of treatment. Potential drug interactions should be evaluated in patients taking combination therapy. The risk benefit ratio of lumacaftor-ivacaftor favours therapy.
– A comprehensive summary of the potential problems with these drugs.
2017 Taylor-Cousar JL, Jain M, Barto TL, Haddad T, Atkinson J, Tian S, Tang R, Marigowda G, Waltz D, Pilewski J; VX14-809-106 Investigator Group.Lumacaftor/ivacaftor in patients with cystic fibrosis and advanced lung disease homozygous for F508del-CFTR. J Cyst Fibros. 2017 Nov 7. pii: S1569-1993(17)30891-3. doi: 10.1016/j.jcf.2017.09.012. [Epub ahead of print] [Pubmed]
A study to evaluate the safety, tolerability, and efficacy of lumacaftor/ivacaftor in patients with cystic fibrosis (CF) with severe lung disease. Patients with CF 12 years of age and older, homozygous for F508del-CFTR, with percent predicted forced expiratory volume in 1 second (ppFEV1) <40 received lumacaftor 400 mg/ivacaftor 250mg every 12h (full dose) for 24weeks in an open-label, prospective study. Dose modification to half dose for 1-2weeks (including at initiation) was permitted. Safety and tolerability were the primary outcome measures; clinical outcomes were also assessed.
Compared with patients with higher lung function, respiratory events were more common in patients with ppFEV1<40; aside from these events, the lumacaftor/ivacaftor safety profile was consistent with previous studies. Results suggest that patients with ppFEV1<40 may benefit from treatment initiation at a lower dose with augmented monitoring before increasing to the full dose.
Taylor-Cousar JL, Munck A, McKone EF, van der Ent CK, Moeller A, Simard C, Wang LT, Ingenito EP, McKee C, Lu Y, Lekstrom-Himes J, Elborn JS.Tezacaftor-Ivacaftor in Patients with Cystic Fibrosis Homozygous for Phe508del. N Engl J Med. 2017 Nov 23;377(21):2013-2023. doi: 10.1056/NEJMoa1709846. Epub 2017 Nov 3. [Pubmed]

Jennifer Taylor-Cousar
In this phase 3, randomized, double-blind, multicenter, placebo-controlled, parallel-group trial, the authors evaluated combination therapy with tezacaftor and ivacaftor in patients 12 years of age or older who had cystic fibrosis and were homozygous for the CFTR Phe508del mutation. Patients were randomly assigned in a 1:1 ratio to receive either 100 mg of tezacaftor once daily and 150 mg of ivacaftor twice daily or matched placebo for 24 weeks. The primary end point was the absolute change in the percentage of the predicted forced expiratory volume in 1 second (FEV1) through week 24 (calculated in percentage points); relative change in the percentage of the predicted FEV1 through week 24 (calculated as a percentage) was a key secondary end point.
Of the 510 patients who underwent randomization, 509 received tezacaftor-ivacaftor or placebo, and 475 completed 24 weeks of the trial regimen. The mean FEV1 at baseline was 60.0% of the predicted value. The effects on the absolute and relative changes in the percentage of the predicted FEV1 in favour of tezacaftor-ivacaftor over placebo were 4.0 percentage points and 6.8%, respectively (P<0.001 for both comparisons). The rate of pulmonary exacerbation was 35% lower in the tezacaftor-ivacaftor group than in the placebo group (P=0.005). The incidence of adverse events was similar in the two groups. Most adverse events were of mild severity (in 41.8% of patients overall) or moderate severity (in 40.9% overall), and serious adverse events were less frequent with tezacaftor-ivacaftor (12.4%) than with placebo (18.2%). A total of 2.9% of patients discontinued the assigned regimen owing to adverse events. Fewer patients in the tezacaftor-ivacaftor group than in the placebo group had respiratory adverse events, none of which led to discontinuation.The authors concluded the combination of tezacaftor and ivacaftor was efficacious and safe in patients 12 years of age or older who had cystic fibrosis and were homozygous for the CFTR Phe508del mutation.
Dr Jennifer Taylor-Cousar (figure) is a paediatrician and adult pulmonologist in Denver, Colorado.
2017 Thomassen JC, Mueller MI, Alejandre Alcazar MA, Rietschel E, van Koningsbruggen-Rietschel S. Effectof Lumacaftor/Ivacaftor on glucose metabolism and insulin secretion in Phe508del homozygous cystic fibrosis patients. J Cyst Fibros. 2017 Dec 15. pii: S1569-1993(17)30973-6. doi: 10.1016/j.jcf.2017.11.016. [Epub ahead of print] [Pubmed]A study to investigate the effect of Lumacaftor/Ivacaftor on glucose metabolism and insulin secretion in patients with cystic fibrosis (CF) (Phe508del/Phe508del). After investigating 5 patients these authors concluded the investigation could not demonstrate that treatment with Lumacaftor/Ivacaftor had a consistent impact on glucose tolerance and insulin secretion.
2017 Zeybel GL, Pearson JP, Krishnan A, Bourke SJ, Doe S, Anderson A, Faruqi S, Morice AH, Jones R, McDonnell M, Zeybel M, Dettmar PW, Brodlie M, Ward C. Ivacaftor and symptoms of extra-oesophageal reflux in patients with cystic fibrosis and G551D mutation. J Cyst Fibros. 2017 Jan;16(1):124-131. doi: 10.1016/j.jcf.2016.07.004. Epub 2016 Jul 27. 27475719 Free PMC Article[Pubmed]
Oesophageal reflux (EOR) may lead to micro aspiration in patients with cystic fibrosis (CF), a probable cause of deteriorating lung function. Successful clinical trials of ivacaftor highlight opportunities to understand EOR in a real world study. Data from 12 patients with CF and the G551D mutation prescribed ivacaftor (150mg bd) was collected at baseline, 6, 26 and 52 weeks. The changes in symptoms of EOR were assessed by questionnaire (reflux symptom index (RSI) and Hull airway reflux questionnaire (HARQ)). Six patients presented EOR at baseline (RSI >13; median 13; range 2-29) and 5 presented airway reflux (HARQ >13; median 12; range 3 to 33). Treatment with ivacaftor was associated with a significant reduction of EOR symptoms (P<0∙04 versus baseline) denoted by the reflux symptom index and Hull airway reflux questionnaire. – Ivacaftor treatment appeared to improve the symptoms of gastroesophageal reflux although no objective evidence was obtained.
2018 2018 2018
Nikhil T Awatade, Sharon L Wong, Chris K Hewson, Laura K Fawcett, Anthony Kicic, Adam Jaffe, Shafagh A Waters Human Primary Epithelial Cell Models: Promising Tools in the Era of Cystic Fibrosis Personalized Medicine. Front Pharmacol 2018 Dec 7;9:1429.doi: 10.3389/fphar.2018.01429. eCollection 2018. Free PMC article (very detailed fully referenced) [Pubmed]

Nikhil T Awatade
Cystic fibrosis (CF) is an inherited disorder where individual disease etiology and response to therapeutic intervention is impacted by CF transmembrane regulator (CFTR) mutations and other genetic modifiers. CFTR regulates multiple mechanisms in a diverse range of epithelial tissues.
In this Review, we consolidate the latest updates in the development of primary epithelial cellular model systems relevant for CF. We discuss conventional two-dimensional (2-D) airway epithelial cell cultures, the backbone of in vitro cellular models to date, as well as improved expansion protocols to overcome finite supply of the cellular source. We highlight a range of strategies for establishment of three-dimensional (3-D) airway and intestinal organoid models and evaluate the limitations and potential improvements in each system, focusing on their application in CF. The in vitro CFTR functional assays in patient-derived organoids allow for preclinical pharmacotherapy screening to identify responsive patients. It is likely that organoids will be an invaluable preclinical tool to unravel disease mechanisms, design novel treatments, and enable clinicians to provide personalized management for patients with CF.
Nikhil T Awatade is a Post-Doctoral Fellow in the Faculty of Medicine, School of Women’s and Children’s Health and the Molecular and Integrative Cystic Fibrosis Research Centre, School of Medical Sciences, Faculty of Medicine, University of New South Wales, SydneyAustralia.
2018 Abou Alaiwa MH, Launspach JL, Grogan B, Carter S, Zabner J, Stoltz DA, Singh PK, McKone EF, Welsh MJ Ivacaftor-induced sweat chloride reductions correlate with increases in airway surface liquid pH in cystic fibrosis.JCI Insight. 2018 Aug 9;3(15). pii: 121468. doi: 10.1172/jci.insight.121468. [Epub ahead of print] [Pubmed]Free PMC Article
Compared with that in the newborn period, ASL pH increased by 6 months of age. In people with CF bearing G551D or R117H mutations, ivacaftor did not change the average ASL pH; however reductions in sweat Cl- concentration correlated with elevations of ASL pH. Reductions in sweat Cl- concentration also correlated with improvements in pulmonary function.
– These results suggest that CFTR-independent mechanisms increase ASL pH in people with CF. the authors speculate that CF airway disease, which begins soon after birth, is responsible for the adaptation.
2018 Bessonova L, Volkova N, Higgins M, Bengtsson L, Tian S, Simard C, Konstan MW, Sawicki GS, Sewall A, Nyangoma S, Elbert A, Marshall BC, Bilton D.Data from the US and UK cystic fibrosis registries support disease modification by CFTR modulation with ivacaftor.Thorax. 2018 Aug;73(8):731-740. doi: 10.1136/thoraxjnl-2017-210394. Epub 2018 May 10.Free full text. [Pubmed]

Leona Bessanova
This on going, observational, post-approval safety study evaluates clinical outcomes and disease progression in ivacaftor-treated patients using data from the US and the UK CF registries following commercial availability. Results from the 2014 analyses (2 and 3 years following commercial availability in the UK and USA, respectively) are presented here.
Analyses included 1256 ivacaftor-treated and 6200 comparator patients from the USA and 411 ivacaftor-treated and 2069 comparator patients from the UK. No new safety concerns were identified based on the evaluation of clinical outcomes included in the analyses. As part of safety evaluations, ivacaftor-treated US patients were observed to have significantly lower risks of death (0.6% vs. 1.6%, p=0.0110), transplantation (0.2% vs. 1.1%, p=0.0017), hospitalisation (27.5% vs. 43.1%, p<0.0001) and pulmonary exacerbation (27.8% vs. 43.3%, p<0.0001) relative to comparators; trends were similar in the UK. In both registries, ivacaftor-treated patients had a lower prevalence of CF-related complications and select microorganisms and had better preserved lung function.
The authors concluded that while general limitations of observational research apply, analyses revealed favourable results for clinically important outcomes among ivacaftor-treated patients, adding to the growing body of literature supporting disease modification by CFTR modulation with ivacaftor.
Dr Leona Bessonova and Dr Nataliya Volkova are from Vertex Pharmaceuticals, Boston Massachusetts
2018 Bruch BA, Singh SB, Ramsey LJ, Starner TD. Impact of a cystic fibrosis transmembrane conductance regulator (CFTR) modulator on high-dose ibuprofen therapy in pediatric cystic fibrosis patients. Pediatr Pulmonol. 2018 May 1. doi: 10.1002/ppul.24024. [Epub ahead of print] [Pubmed]
This study was undertaken to determine if a clinically relevant drug-drug interaction occurred between ibuprofen and lumacaftor/ivacaftor. Peak ibuprofen plasma concentrations were measured prior to and after lumacaftor/ivacaftor initiation. The authors showed a clinically relevant drug-drug interaction exists between ibuprofen and lumacaftor/ivacaftor. Lumacaftor may cause sub-therapeutic ibuprofen plasma concentrations due to the induction of CYP enzymes and increased metabolism of ibuprofen. Based on this analysis, they have modified their use of ibuprofen in several patients after evaluation of this drug-drug interaction.
2018 Byrnes LJ, Xu Y, Qiu X, Hall JD, West GM.Sites associated with Kalydeco binding on human Cystic Fibrosis Transmembrane Conductance Regulator revealed by Hydrogen/Deuterium Exchange. Sci Rep. 2018 Mar 16;8(1):4664. doi: 10.1038/s41598-018-22959-6. Free PMC Article[Pubmed]

Laura Jean Byrnes
Cystic Fibrosis (CF) is caused by mutations in the Cystic Fibrosis Transmembrane Conductance Regulator (CFTR). Mutations associated with CF cause loss-of-function in CFTR leading to salt imbalance in epithelial tissues. Kalydeco (also called VX-770 or ivacaftor) was approved for CF treatment in 2012 but little is known regarding the compound’s interactions with CFTR including the site of binding or mechanisms of action. In this study we use hydrogen/deuterium exchange (HDX) coupled with mass spectrometry to assess the conformational dynamics of a thermostabilized form of CFTR in apo and ligand-bound states. We observe HDX protection at a known binding site for AMPPNP and significant protection for several regions of CFTR in the presence of Kalydeco. The ligand-induced changes of CFTR in the presence of Kalydeco suggest a potential binding site
Dr. Laura Jean Byrnes is a scientist at Pfizer, Cornell University
2018 Barnaby R, Koeppen K, Nymon A, Hampton TH, Berwin B, Ashare A, Stanton BA. Lumacaftor (VX-809) restores the ability of CF macrophages to phagocytose and kill Pseudomonas aeruginosa. Am J Physiol Lung Cell Mol Physiol. 2018 Mar 1;314(3):L432-L438. doi: 10.1152/ajplung.00461.2017. Epub 2017 Nov 16. [Pubmed]
Although ivacaftor (VX-770) alone and ivacaftor in combination with lumacaftor (VX-809) improve lung function in CF patients with the Gly551Asp and del508Phe mutations, respectively, the effects of these drugs on the function of human CF macrophages are unknown. Thus studies were conducted to examine the effects of lumacaftor alone and lumacaftor in combination with ivacaftor (i.e., ORKAMBI) on the ability of human CF ( del508Phe/ del508Phe) monocyte-derived macrophages (MDMs) to phagocytose and kill Pseudomonas aeruginosa.
Lumacaftor alone restored the ability of CF MDMs to phagocytose and kill P. aeruginosa to levels observed in MDMs obtained from non-CF (WT-CFTR) donors. This effect contrasts with the partial (~15%) correction of del508Phe Cl– secretion of airway epithelial cells by lumacaftor. Ivacaftor reduced the ability of lumacaftor to stimulate phagocytosis and killing of P. aeruginosa. Lumacaftor had no effect on P. aeruginosa-stimulated cytokine secretion by CF MDMs. Ivacaftor (5 µM) alone and ivacaftor in combination with lumacaftor reduced secretion of several proinflammatory cytokines. The clinical efficacy of ORKAMBI may be related in part to the ability of lumacaftor to stimulate phagocytosis and killing of P. aeruginosa by macrophages.
From the Department of Microbiology and Immunology, Geisel School of Medicine at Dartmouth, Hanover, New Hampshire.
2018 Carlile GW, Yang Q, Matthes E, Liao J, Radinovic S, Miyamoto C, Robert R, Hanrahan JW, Thomas DY.A novel triple combination of pharmacological chaperones improves F508del-CFTR correction. Sci Rep. 2018 Jul 30;8(1):11404. doi: 10.1038/s41598-018-29276-yFree PMC Article [Pubmed]
Pharmacological chaperones (e.g. VX-809, lumacaftor) that bind directly to F508del-CFTR and correct its mislocalization are promising therapeutics for Cystic Fibrosis (CF). However to date, individual correctors provide only ~4% improvement in lung function measured as FEV1, suggesting that multiple drugs will be needed to achieve substantial clinical benefit. Here we examine if multiple sites for pharmacological chaperones exist and can be targeted to enhance the rescue of F508del-CFTR with the premise that additive or synergistic rescue by multiple pharmacological chaperones compared to single correctors indicates that they have different sites of action. First, we found that a combination of the pharmacological chaperones VX-809 and RDR1 provide additive correction of F508del-CFTR. Then using cellular thermal stability assays (CETSA) we demonstrated the possibility of a third pharmacologically important site using the novel pharmacological chaperone tool compound 4-methyl-N-[3-(morpholin-4-yl) quinoxalin-2-yl] benzenesulfonamide (MCG1516A). All three pharmacological chaperones appear to interact with the first nucleotide-binding domain (NBD1). The triple combination of MCG1516A, RDR1, and VX-809 restored CFTR function to >20% that of non-CF cells in well differentiated HBE cells and to much higher levels in other cell types. Thus the results suggest the presence of at least three distinct sites for pharmacological chaperones on F508del-CFTR NBD1, encouraging the development of triple corrector combinations.
2018 Carlile GW, Yang Q, Matthes E, Liao J, Radinovic S, Miyamoto C, Robert R, Hanrahan JW, Thomas DY.A novel triple combination of pharmacological chaperones improves F508del-CFTR correction..
Sci Rep.2018Jul 30;8(1):11404. doi: 10.1038/s41598-018-29276-y.Free PMC Article [Pubmed]
Pharmacological chaperones (e.g. VX-809, lumacaftor) that bind directly to F508del-CFTR and correct its mislocalization are promising therapeutics for Cystic Fibrosis (CF). However to date, individual correctors provide only ~4% improvement in lung function measured as FEV1, suggesting that multiple drugs will be needed to achieve substantial clinical benefit. Here we examine if multiple sites for pharmacological chaperones exist and can be targeted to enhance the rescue of F508del-CFTR with the premise that additive or synergistic rescue by multiple pharmacological chaperones compared to single correctors indicates that they have different sites of action. First, we found that a combination of the pharmacological chaperones VX-809 and RDR1 provide additive correction of F508del-CFTR. Then using cellular thermal stability assays (CETSA) we demonstrated the possibility of a third pharmacologically important site using the novel pharmacological chaperone tool compound 4-methyl-N-[3-(morpholin-4-yl) quinoxalin-2-yl] benzenesulfonamide (MCG1516A). All three pharmacological chaperones appear to interact with the first nucleotide-binding domain (NBD1).
The triple combination of MCG1516A, RDR1, and VX-809 restored CFTR function to >20% that of non-CF cells in well differentiated HBE cells and to much higher levels in other cell types. Thus the results suggest the presence of at least three distinct sites for pharmacological chaperones on F508del-CFTR NBD1, encouraging the development of triple corrector combinations.
2018 Cho DY, Zhang S, Lazrak AGrayson JW, Peña Garcia JA, Skinner DF, Lim DJ, Mackey C, Banks C, Matalon S, Woodworth BA. Resveratrol and ivacaftor are additive G551D CFTR-channel potentiators: therapeutic implications for cystic fibrosis sinus disease. Int Forum Allergy Rhinol. 2018 Aug 27. doi: 10.1002/alr.22202. [Epub ahead of print][Pubmed]
Do-Yeon Cho
Ivacaftor is a CFTR potentiator that improves Cl– transport in CF patients with at least 1 copy of the G551D mutation. Resveratrol is also a potent CFTR potentiator that increases determinants of mucociliary transport. The objective of this study is to determine whether resveratrol and ivacaftor improve Cl– secretion in G551D CFTR over either agent alone. In G551D Fisher rat thyroid cells there was improvement in G551D CFTR-mediated Cl– secretion suggests that resveratrol could enhance ivacaftor therapy in these patients and improve CF-related rhino sinusitis.
Dr. Do-Yeon Cho is Director of Otolaryngology Research, Department of Otolaryngology, University of Alabama, Birmingham Alabama
2018 Clancy JP, Cotton CU,Donaldson SH, Solomon GM, VanDevanter DR, Boyle MP, Gentzsch M, Nick JA, Illek B, Wallenburg JC, Sorscher EJ, Amaral MD, Beekman JM, Naren AP, Bridges RJ, Thomas PJ, Cutting G, Rowe S, Durmowicz AG, Mense M, Boeck KD, Skach W, Penland C, Joseloff E, Bihler H, Mahoney J, Borowitz D, Tuggle KL. CFTR modulator theratyping: Current status, gaps and future directions. J Cyst Fibros. 2018 Jun 19. pii: S1569-1993(18)30585-X. doi: 10.1016/j.jcf.2018.05.004. [Epub ahead of print]Free full text [Pubmed]
The Cystic Fibrosis Foundation (CFF) assembled a workshop of international experts to discuss the use of preclinical model systems to examine the nature of CF-causing variants in CFTR and the role of in vitro CFTR modulator testing to inform in vivo modulator use. The theme of the workshop was centred on CFTR theratyping, a term that encompasses the use of CFTR modulators to define defects in CFTR in vitro, with application to both common and rare CFTR variants.
Several preclinical model systems were identified in various stages of maturity, ranging from the expression of CFTR variant cDNA in stable cell lines to examination of cells derived from CF patients, including the gastrointestinal tract, the respiratory tree, and the blood. Common themes included the on going need for standardization, validation, and defining the predictive capacity of data derived from model systems to estimate clinical outcomes from modulator-treated CF patients.
The authors concluded CFTR modulator theratyping is a novel and rapidly evolving field that has the potential to identify rare CFTR variants that are responsive to approved drugs or drugs in development
Clancy JP.Rapid therapeutic advances in CFTR modulator science.Pediatr Pulmonol. 2018 Nov;53(S3):S4-S11. doi: 10.1002/ppul.24157.[Pubmed]

John Clancy
Established CF therapies treat the downstream consequences of CFTR dysfunction and have led to steady improvements in patient survival. A class of drugs termed CFTR modulators has recently entered the CF therapeutic landscape. These drugs differ fundamentally from prior therapies in that they aim to improve the function of disease-causing CFTR variants. This review summarizes the science behind CFTR modulators, including their targets, mechanism of action, clinical benefit, and future directions in the field. CFTR modulators have dramatically changed how CF is treated, validated CFTR as a therapeutic target, and opened the door to truly personalized therapies and treatment regim
Dr. John Clancy from the Department of Pediatrics, Cincinnati Children’s Hospital Medical Center, Cincinnati, Ohio.
2018 Davies JC, Moskowitz SM, Brown C, Horsley A, Mall MA, McKone EF, Plant BJ, Prais D, Ramsey BW, Taylor-Cousar JL, Tullis E, Uluer A, McKee CM, Robertson S, Shilling RA, Simard C, Van Goor F, Waltz D, Xuan F, Young T, Rowe SM; VX16-659-101 Study Group.VX-659-Tezacaftor-Ivacaftor in Patients with Cystic Fibrosis and One or Two Phe508del Alleles.N Engl J Med. 2018 Oct 25;379(17):1599-1611. doi: 10.1056/NEJMoa1807119. Epub 2018 Oct 18.[Pubmed]
The next-generation cystic fibrosis transmembrane conductance regulator (CFTR) corrector VX-659, in triple combination with tezacaftor and ivacaftor (VX-659-tezacaftor-ivacaftor), was developed to restore the function of Phe508del CFTR protein in patients with cystic fibrosis.The effects of VX-659-tezacaftor-ivacaftor on the processing, trafficking, and function of Phe508del CFTR protein were investigated using human bronchial epithelial cells. A range of oral VX-659-tezacaftor-ivacaftor doses in triple combination were then evaluated in randomized, controlled, double-blind, multicenter trials involving patients with cystic fibrosis who were heterozygous for the Phe508del CFTR mutation and a minimal-function CFTR mutation (Phe508del-MF genotypes) or homozygous for the Phe508del CFTR mutation (Phe508del-Phe508del genotype). The primary end points were safety and the absolute change from baseline in the percentage of predicted forced expiratory volume in 1 second (FEV1).
RESULTS:(Trial numbers NCT03224351 and NCT03029455) VX-659-tezacaftor-ivacaftor significantly improved the processing and trafficking of Phe508del CFTR protein as well as chloride transport in vitro. In patients, VX-659-tezacaftor-ivacaftor had an acceptable safety and side-effect profile. Most adverse events were mild or moderate. VX-659-tezacaftor-ivacaftor resulted in significant mean increases in the percentage of predicted FEV1 through day 29 (P<0.001) of up to 13.3 points in patients with Phe508del-MF genotypes; in patients with the Phe508del-Phe508del genotype already receiving tezacaftor-ivacaftor, adding VX-659 resulted in a further 9.7-point increase in the percentage of predicted FEV1. The sweat chloride concentrations and scores on the respiratory domain of the Cystic Fibrosis Questionnaire-Revised improved in both patient populations.
The authors concluded robust in vitro activity of VX-659-tezacaftor-ivacaftor targeting Phe508del CFTR protein translated into improvements for patients with Phe508del-MF or Phe508del-Phe508del genotypes. VX-659 triple-combination regimens have the potential to treat the underlying cause of disease in approximately 90% of patients with cystic fibrosis.
Elie Dolgin. In utero intervention to stem the damage of cystic fibrosis. Nature 2020 Jul; 583(7818): S6-S7.doi: 10.1038/d41586-020-02108-8. [Pubmed]

Elie Dolgin
There is no abstract with article so the text is summarised as follows –
The author reviews the past and present situation regarding intrauterine treatment of the CF genetic defect now that specific modulator treatments are increasingly available since 2012. Organ damage or maldevelopment occurs in utero to many organs such as the pancreas, liver, male genital tract and others and is present and irreversible after birth. Animal evidence suggests this damage is preventable by antenatal use of appropriate modulators such as ivacaftor. Promising animal research in CF mice along these lines by Janet Larson team 20 years ago using intrauterine gene therapy with viruses encoding for CFTR showed promise. However, the death of an 18-year-old undergoing gene therapy for another unrelated condition in 1999 set progress back years, caused funding to dry up. Also two prominent UK groups failed to reproduce Larson’s findings.
More recently precise techniques for gene editing such as CRISPR allow more precise correction of the genetic defect and have revived interest in the intrauterine approach. The precise gene fixing technology could repair F508del CFTR mutation in mice and human cells. Apparently, treatment during a limited critical period in utero will prevent some prenatal damage.
Also, an antenatal blood test is now available which can identify a number of genetic disease including CF by 10 weeks’ gestation and also identify the exact mutation. Also, identifying the exact mutation would enable the mother to take the specific modulator effective against the foetal mutation. Present experience seems to indicate modulators are safe during pregnancy. Treatment of ferrets with CFTR mutations susceptible to ivacaftor are protected from widespread organ damage before birth.
2018 Donaldson SH, Pilewski JM, Griese M, Cooke J, Viswanathan L, Tullis E, Davies JC, Lekstrom-Himes JA, Wang LT5; VX11-661-101 Study Group. Tezacaftor/Ivacaftor in Subjects with Cystic Fibrosis and F508del/F508del-CFTR or F508del/G551D-CFTR.Am J Respir Crit Care Med. 2018 Jan 15;197(2):214-224. doi: 10.1164/rccm.201704-0717OC.[Pubmed]

Scott H Donaldson
A study to evaluate the safety and efficacy of tezacaftor (formerly VX-661) monotherapy and of tezacaftor/ivacaftor combination therapy in subjects with cystic fibrosis homozygous for F508del or compound heterozygous for F508del and G551D. This was a randomized, placebo-controlled, double-blind, multicenter, phase 2 study. Subjects homozygous for F508del received tezacaftor (10 to 150 mg) every day alone or in combination with ivacaftor (150 mg every 12 h) in a dose escalation phase, as well as in a dosage regimen testing phase. Subjects compound heterozygous for F508del and G551D, taking physician-prescribed ivacaftor, received tezacaftor (100 mg every day).
Primary endpoints were safety through Day 56 and change in sweat chloride from baseline through Day 28. Secondary endpoints included change in per cent predicted FEV1 (ppFEV1) from baseline through Day 28 and pharmacokinetics. The incidence of adverse events was similar across treatment arms. Tezacaftor (100 mg every day)/ivacaftor (150 mg every 12 h) resulted in a 6.04 mmol/L decrease in sweat chloride and 3.75 percentage point increase in ppFEV1 in subjects homozygous for F508del, and a 7.02 mmol/L decrease in sweat chloride and 4.60 percentage point increase in ppFEV1 in subjects compound heterozygous for F508del and G551D from baseline through Day 28 (P < 0.05 for all).
The authors considered these results support continued clinical development of tezacaftor (100 mg every day) in combination with ivacaftor (150 mg every 12 h) in subjects with cystic fibrosis.
2018 Dryden C, Wilkinson J, Young D, Brooker RJ; Scottish Paediatric Cystic Fibrosis Managed Clinical Network (SPCFMCN). The impact of 12months treatment with ivacaftor on Scottish paediatric patients with cystic fibrosis with the G551D mutation: a review. Arch Dis Child. 2018 Jan;103(1):68-70. doi: 10.1136/archdischild-2015-310420. Epub 2016 Jun 10.[Pubmed]

Carol Dyden
Statistically significant improvements in FEV1 and body mass index and a reduction in sweat chloride, all comparable with previously published data were observed. The findings also suggested reduced use of intravenous antibiotics and oral antibiotics. No significant adverse effects were observed but a possible association with cataract formation could not be excluded. This review suggests that, in the short term at least, ivacaftor is effective and safe in paediatric patients ≥6 years of age with G551D.
Dr. Carol Dryden is consultant in Department of Paediatrics, Wishaw General Hospital, Wishaw, UK.
2018 Flume PA, Wainwright CE, Elizabeth Tullis D, Rodriguez S, Niknian M, Higgins M, Davies JC, Wagener JS.Recovery of lung function following a pulmonary exacerbation in patients with cystic fibrosis and the G551D-CFTR mutation treated with ivacaftor. J Cyst Fibros. 2018 Jan;17(1):83-88. doi: 10.1016/j.jcf.2017.06.002. Epub 2017 Jun 24.[Pubmed]

Patrick Flume
Pulmonary exacerbations (PEx) are associated with acute loss of lung function that is often not recovered after treatment. We investigated lung function recovery following PEx for ivacaftor- and placebo-treated subjects. Short- and long-term pulmonary function recovery data after PEx were summarized from a placebo-controlled trial in 161 cystic fibrosis patients≥12years old with the G551D-CFTR mutation (NCT00909532). Short-term recovery was measured 2 to 8 weeks after treatment, and long-term recovery was determined at the end-of-study, both compared with baseline measured just prior to the PEx. Fewer patients receiving ivacaftor experienced a PEx than patients receiving placebo (33.7% vs. 56.4%; P=0.004) and had a lower adjusted incidence rate of PEx (0.589 vs. 1.382; P<0.001). The proportion of PEx followed by full short-term recovery of per cent predicted forced expiratory volume in 1s was similar (ivacaftor vs. placebo, 57.1% vs. 53.7), as was the proportion of patients having long-term recovery (46.4% vs. 47.7%).Ivacaftor treatment reduces the frequency of PEx but does not improve on the rate of complete lung function recovery after PEx when compared with place
2018 Graeber SY, Dopfer C, Naehrlich L, Gyulumyan L, Scheuermann H, Hirtz S, Wege S, Mairbäurl H, Dorda M, Hyde R, Bagheri-Hanson A, Rueckes-Nilges C, Fischer S, Mall MA, Tümmler B. Effects of Lumacaftor/Ivacaftor Therapy on CFTR Function in Phe508del Homozygous Patients with Cystic Fibrosis. Am J Respir Crit Care Med. 2018 Jan 12. doi: 10.1164/rccm.201710-1983OC. [Epub ahead of print] [Pubmed]

Simon Graeber
The phase 3 trials of lumacaftor examined clinical outcomes, but did not evaluate the CFTR function in patients. This study examines the effect of lumacaftor-ivacaftor on biomarkers of CFTR function in Phe508del homozygous treated CF patients aged 12 years and older. A total of 53 patients were enrolled in the study and 52 patients had baseline and follow up measurements. After initiation of lumacaftor-ivacaftor sweat chloride concentrations were reduced by 17.8 mmol/L (IQR -25.9 to -6.1; p<0.001), NPD showed partial rescue of CFTR function in nasal epithelia to a level of 10.2% (IQR 0.0 to 26.1; p<0.011), and ICM showed functional improvement in rectal epithelia to a level of 17.7% of normal (IQR 10.8 to 29.0; p<0.001). All patients improved in at least one CFTR biomarker, but no correlations were found between CFTR biomarker responses and clinical outcomes.
So lumacaftor-ivacaftor results in partial rescue of Phe508del CFTR function to levels comparable to the lower range of CFTR activity found in patients with residual function mutations. Functional improvement was detected even in the absence of short-term improvement of FEV1 % predicted and BMI.
Dr Simon Graeber (figure) is a paediatric pulmonologist at the University of Heidelberg.
– The authors observe that “adverse outcome attributed to pulmonary exacerbations occur even when addressing the underlying cause of CF and improving CFTR function in the host”. This is to be expected as most of these patients had past “the point of no return” when rescued CFTR function had been overshadowed by chronic inflammation less dependent on CFTR function. Emphasising the great importance of treatment before the stage of chronic inflammation is reached.
2018 Guimbellot JS, Acosta EP, Rowe SM. Sensitivity of ivacaftor to drug-drug interactions with rifampin, a cytochrome P450 3A4 inducer. Pediatr Pulmonol. 2018 May;53(5):E6-E8. doi: 10.1002/ppul.23971. Epub 2018 Feb 28.[Pubmed]
The CFTR potentiator ivacaftor is responsible for significant clinical improvements among a subset of patients with cystic fibrosis. Because it is a substrate of the cytochrome P450 system, specifically CYP3A4/5, ivacaftor is subject to significant drug-drug interactions, including due to commonly used antimicrobials such as rifampin. While the interaction of rifampin and ivacaftor has been examined in vitro, severe adverse events resulting from this interaction have not been reported in the literature. In this report, the authors describe the termination of steady, long-term improvement in a patient taking ivacaftor, resulting from the use of rifampin and precipitating a significant pulmonary exacerbation.
2018 Guimbello J, Solomon GM, Baines A, Heltshe SL, VanDalfsen J, Joseloff E, Sagel SD, Rowe SM; GOALe(2) Investigators. Effectiveness of ivacaftor in cystic fibrosis patients with non-G551D gating mutations.2018 Apr 21. pii: S1569-1993(18)30090-0. doi: 10.1016/j.jcf.2018.04.004. [Epub ahead of print] [Pubmed]
Seven Rowe
The authors report the results of an observational study investigating its effects in CF patients with non-G551D gating mutations. Patients with non-G551D gating mutations were recruited to an open-label study evaluating ivacaftor. Primary outcomes included: lung function, sweat chloride, weight gain, and quality of life scores. Twenty-one subjects were enrolled and completed 6 months follow-up on ivacaftor; mean age was 25.6 years with 52% <18. Baseline ppFEV1 was 68% and mean sweat chloride 89.6 mEq/L. Participants experienced significant improvements in ppFEV1 (mean absolute increase of 10.9% 95% CI = [2.6,19.3], p = 0.0134), sweat chloride (-48.6 95% CI = [-67.4,-29.9], p < 0.0001), and weight (5.1 kg, 95% CI = [2.8, 7.3], p = 0.0002)A retrospective observational multicentre study collected clinical data in the year before and the 2years after ivacaftor initiation in patients with CF and a Gly551Asp-CFTR mutation. Fifty-seven patients were included. Mean absolute change in FEV1% predicted improved from baseline to Year 1 (8.4%; p<0.001) and Year 2 (7.2%; p=0.006). Statistically significant benefits were observed with increased body mass index, fewer Pseudomonas aeruginosa (56.2-41.3%) and Staphylococcus aureus (75%-58.7%) positive cultures, and decreased IV antibiotics (12.7-5.4 days) and maintenance treatment prescriptions (including azithromycin (47.4-31.3%), Dornase alpha (56.1-39.6%) and nutritional supplements ( 28.1-14.6%). No significant adverse events were reported. The clinical benefits of ivacaftor reported in previous clinical trials were confirmed in a real-world setting two years post-initiation, also reducing treatment burden.
– Useful information with “real world” results. The use of pancreatic enzymes remained unchanged (89.5-87.5%) as one would expect. The unusually high proportion of patients initially infected by S. aureus (75%) and the many receiving inhaled corticosteroids (63.2%) is interesting. The authors speculate as to whether use of ivacaftor could lead to a reduction in other long-term therapies.
The authors concluded patients with non-G551D gating mutations experienced improved lung function, nutritional status, and quality of life. This study supports on going use of ivacaftor for patients with these mutations.
Dr. Steven Rowe is Professor and Director, Gregory Fleming James Cystic Fibrosis Research Center, University of Alabama at Birmingham.
2018 Hammond JA, Connett GJ.The use of lumacaftor/ivacaftor to treat acute deterioration in paediatric cystic fibrosis.
Paediatr Respir Rev. 2018 Jun;27:16-17. doi: 10.1016/j.prrv.2018.05.008. Epub 2018 May 19.

Gary Connett
The authors describe the use of lumacaftor/ivacaftor to treat an 8 year old girl with an unusually severe exacerbation of CF lung disease and review the potential of lumacaftor/ivacaftor as a rescue therapy in the paediatric CF population.
The patient was homozygous for the Phe508del genotype. Her background included cleft palate repair for Pierre Robin sequence, gastrostomy for poor nutrition and fundoplication for severe reflux. She had previously received three courses of intravenous (IV) antibiotics for increased respiratory symptoms, but remained free of chronic infection with Pseudomonas aeruginosa. She was on regular rhDNase and enjoyed normal levels of physical activity. Before her acute severe illness FEV1s were >80%predicted. She presented with a two week history of deteriorating chest infection FEV1 44%. Despite intensive investigation and treatment at 4 months with an FEV1 of 31% she was referred for transplant assessment and lumacaftor/ivacaftor started.
Within two weeks of commencement there were significant clinical improvements. Oxygen saturations became normal in air and she was discharged within two weeks after discontinuing IV antibiotics. No other changes were made to her treatment. Her FEV1 continued to improve to 80% predicted 1 month after starting treatment and has been maintained at this level for a further 6 months.
Prof. Gary Connett, the corresponding author, was appointed as a paediatric respiratory consultant in Southampton in 1995. He is visiting professor to University Hospitals of Latvia (2009) and Singapore (2011) and has held a personal chair as professor of paediatrics at the University of Southampton since 2018.
– This is remarkable story. Professor Connett kindly informed me (in December 2018) that the child has made good progress maintaining an FEV1 between 60-70% predicted and having three monthly courses of intravenous and antibiotics. She has a relatively good quality of life attending school and participating in sporting activities. She does however feel precarious and at risk of further deterioration.
2018 Hubert D, Dehillotte C, Munck A, David V, Baek J, Mely L, Dominique S, Ramel S, Danner Boucher I, Lefeuvre S, Reynaud Q, Colomb-Jung V, Bakouboula P, Lemonnier L.Retrospective observational study of French patients with cystic fibrosis and a Gly551Asp-CFTR mutation after 1 and 2years of treatment with ivacaftor in a real-world setting.J Cyst Fibros. 2018 Jan;17(1):89-95. doi: 10.1016/j.jcf.2017.07.001. Epub 2017 Jul 12. [PubMed].

Dominique Hubert
A retrospective observational multicentre study collected clinical data in the year before and the 2years after ivacaftor initiation in patients with CF and a Gly551Asp-CFTR mutation. Fifty-seven patients were included. Mean absolute change in FEV1% predicted improved from baseline to Year 1 (8.4%; p<0.001) and Year 2 (7.2%; p=0.006). Statistically significant benefits were observed with increased body mass index, fewer Pseudomonas aeruginosa (56.2-41.3%) and Staphylococcus aureus (75%-58.7%) positive cultures, and decreased IV antibiotics (12.7-5.4 days) and maintenance treatment prescriptions (including azithromycin (47.4-31.3%), Dornase alpha (56.1-39.6%) and nutritional supplements ( 28.1-14.6%). No significant adverse events were reported. The clinical benefits of ivacaftor reported in previous clinical trials were confirmed in a real-world setting two years post-initiation, also reducing treatment burden.
– Useful information with “real world” results. The use of pancreatic enzymes remained unchanged (89.5-87.5%) as one would expect. The unusually high proportion of patients initially infected by S. aureus (75%) and the many receiving inhaled corticosteroids (63.2%) is interesting. The authors speculate as to whether use of ivacaftor could lead to a reduction in other long-term therapies.
2018 Keating D, Marigowda G, Burr L, Daines C, Mall MA, McKone EF, Ramsey BW, Rowe SM, Sass LA, Tullis E, McKee CM, Moskowitz SM, Robertson S, Savage J, Simard C, Van Goor F, Waltz D, Xuan F, Young T, Taylor-Cousar JL; VX16-445-001 Study Group. VX-445-Tezacaftor-Ivacaftor in Patients with Cystic Fibrosis and One or Two Phe508del Alleles N Engl J Med. 2018 Oct 25;379(17):1612-1620. doi: 10.1056/NEJMoa1807120. Epub 2018 Oct 18. [Pubmed]

Dominic Keating
VX-445 is a next-generation cystic fibrosis transmembrane conductance regulator (CFTR) corrector designed to restore Phe508del CFTR protein function in patients with cystic fibrosis when administered with tezacaftor and ivacaftor (VX-445-tezacaftor-ivacaftor). The authors evaluated the effects of VX-445-tezacaftor-ivacaftor on Phe508del CFTR protein processing, trafficking, and chloride transport in human bronchial epithelial cells. On the basis of in vitro activity, a randomized, placebo-controlled, double-blind, dose-ranging, phase 2 trial was conducted to evaluate oral VX-445-tezacaftor-ivacaftor in patients heterozygous for the Phe508del CFTR mutation and a minimal-function mutation (Phe508del-MF) and in patients homozygous for the Phe508del CFTR mutation (Phe508del-Phe508del) after tezacaftor-ivacaftor run-in. Primary end points were safety and absolute change in percentage of predicted forced expiratory volume in 1 second (FEV1) from baseline.
Results. In vitro, VX-445-tezacaftor-ivacaftor significantly improved Phe508del CFTR protein processing, trafficking, and chloride transport to a greater extent than any two of these agents in dual combination. In patients with cystic fibrosis, VX-445-tezacaftor-ivacaftor had an acceptable safety and side-effect profile. Most adverse events were mild or moderate. The treatment also resulted in an increased percentage of predicted FEV1 of up to 13.8 points in the Phe508del-MF group (P<0.001). In patients in the Phe508del-Phe508del group, who were already receiving tezacaftor-ivacaftor, the addition of VX-445 resulted in an 11.0-point increase in the percentage of predicted FEV1 (P<0.001). In both groups, there was a decrease in sweat chloride concentrations and improvement in the respiratory domain score on the Cystic Fibrosis Questionnaire-Revised.
The authors concluded the use of VX-445-tezacaftor-ivacaftor to target Phe508del CFTR protein resulted in increased CFTR function in vitro and translated to improvements in patients with cystic fibrosis with one or two Phe508del alleles. This approach has the potential to treat the underlying cause of cystic fibrosis in approximately 90% of patients. (Clinical trials NCT03227471 ; and EudraCT number, 2017-000797-11)
Dominic T Keating is Respiratory Physician at the Alfred Hospital · Department of Allergy, Immunology & Respiratory Medicine (AIRmed) Australia, Melbourne
2018 Andrea Kelly, Diva D De Leon , Saba Sheikh , Devaney Camburn , Christina Kubrak , Amy J Peleckis , Darko Stefanovski , Denis Hadjiliadis , Michael R Rickels , and Ronald C Rubenstein Islet Hormone and Incretin Secretion in Cystic Fibrosis Following 4-months of Ivacaftor Therapy. Am J Respir Cri Care 2018 Aug 21. https://doi-org.rsm.idm.oclc.org/10.1164/rccm.201806-1018OC [Pubmed

Andrea Kelly
Diabetes is associated with worse cystic fibrosis (CF) outcomes. The CFTR potentiator ivacaftor is suggested to improve glucose homeostasis in individuals with CF. Objective: The authors tested the hypothesis that clinically-indicated ivacaftor would be associated with improvements in glucose tolerance and insulin and incretin secretion. Methods: Oral glucose tolerance tests, mixed meal tolerance tests, and glucose-potentiated arginine tests were compared pre- and 16-weeks post-ivacaftor initiation in CF participants with at least one CFTR gating or conductance mutation. Meal-related 30- (early-phase) and 180-min incremental area under the curves were calculated as responses for glucose, insulin, C-peptide, and incretin hormones, glucagon-like peptide-1 and glucose-dependent insulinotropic polypeptide. First-phase insulin secretion, glucose-potentiation of arginine-induced insulin secretion, and disposition index were characterized by glucose-potentiated arginine tests. Results: Twelve subjects (6M/6F; 7 normal/5 abnormal glucose tolerance [AGT], oral glucose tolerance test one-hour glucose>155 and two-hour glucose<200 mg/dL) of median [min-max] age: 13.8y [6.0-42.0], BMI-Z: 0.66 [-2.4-1.9], and FEV1%-predicted: 102 [39-122] completed the study. Glucose tolerance normalized in one AGT subject. Ivacaftor treatment did not alter meal responses except for an increase in early-phase C-peptide (P=0.04). First-phase (P=0.001) and glucose-potentiation of arginine-induced (P=0.027) insulin secretion assessed by acute C-peptide responses improved after ivacaftor treatment. Consistent with an effect on β-cell function, the disposition index relating the amount of insulin secreted for insulin sensitivity also improved (P=0.04).
Authors concluded insulin secretion improved following four months of clinically-indicated ivacaftor therapy in this relatively young group of CF patients with normal to mildly impaired glucose tolerance, while incretin secretion remained unchanged.
2018 Kim J, Davies Z, Dunn C, Wine JJ, Milla C. Ivacaftor restores CFTR-dependent sweat gland fluid secretion in cystic fibrosis subjects with S945L alleles. J Cyst Fibros. 2018 Mar;17(2):179-185. doi: 10.1016/j.jcf.2017.12.005. Epub 2017 Dec 24.[Pubmed]

Carlos Milla
A study to determine in vivo effects of CFTR modulators on mutation S945L. The authors measured effects of CFTR modulators on CFTR-dependent sweating (‘C-sweat’) in two pancreatic sufficient cystic fibrosis (CF) subjects. S1 (S945L/G542X) took ivacaftor and S2 (S945L/F508del) took ivacaftor+tezacaftor. Sweating was stimulated pharmacologically to produce sequentially both CFTR-independent (methacholine stimulated) M-sweat and C-sweat; and the ratio of these was compared. Sweat secretion was measured with two methods: real time secretory rate quantitative recording and by optically measuring the growth of sweat bubbles under oil from multiple identified glands.
Using the quantitative recorder, they saw zero C-sweat secretion off-drug, but when on-drug the C-sweat responses for both subjects were comparable to those seen in carriers. The on-drug response was further quantified using the sweat bubble method. Each subject again showed robust C-sweat responses, with C-sweat/M-sweat ratios~half of the ratio determined for a cohort of 40 controls tested under identical conditions.
These in vivo results, consistent with prior in vitro findings, indicate that the drug treatments restore near-normal function to S945L-CFTR, and support the use of ivacaftor as a treatment for CF patients who carry this allele.
Corresponding author is Professor Carlos Milla at the Lucille Salter Packard Children’s Hospital, Stanford University.
2018 Kirwan L, Fletcher G, Harrington M, Jeleniewska P, Zhou S, Casserly B, Gallagher CG, Greally P, Gunaratnam C, Herzig M, Linnane B, McElvaney NG.McKone EF, McNally P, Mullane D, Ní Chróinín M, O’Mahony M, Plant BJ, Jackson AD.Longitudinal Trends in Real-World Outcomes Following Initiation of Ivacaftor: A Cohort Study from the Cystic Fibrosis Registry of Ireland.Ann Am Thorac Soc. 2018 Nov 14. doi: 10.1513/AnnalsATS.201802-149OC. [Epub ahead of print]. Pubmed]

Laura Kirwan
The authors used cystic fibrosis (CF) registry data to assess outcomes following the initiation of ivacaftor, a cystic fibrosis transmembrane conductance regulator (CFTR) potentiator approved for the treatment of CF with a defective gating CFTR mutation.
Longitudinal trends were examined using mixed effects regression analysis in 80 ivacaftor-treated CF patients aged 6-56 years registered with the CF Registry of Ireland with ≥36 month’s pre- and post-commencement data. The effects of ivacaftor treatment on percentage-predicted forced expiratory volume in 1s (ppFEV1), body mass index (BMI), hospitalisation for pulmonary exacerbation, oral and IV antibiotic usage were assessed.
In the 36 months after ivacaftor initiation, ppFEV1 improved by 2.26% per annum [95% CI (0.23 to 4.29), p=0.03] for patients aged <12 years, remained unchanged for 12-<18 years olds [95% CI (-1.87 to 2.88), p=0.67] and declined in adults by 1.74% per annum [95% CI (-3.08 to -0.39), p=0.01]. BMI in adults increased 0.28 kg m-2 per annum [95% CI (0.03 to 0.52), p=0.027] and there was no significant decline in BMI z score in children, [95% CI (-0.01 to 0.13), p=0.08]. In the year after ivacaftor initiation, IV antibiotic treatment reduced by 46% [95% CI (-62.5% to -23.3%), p<0.01], oral antibiotic treatment by 49% [95% CI (-61.1% to -32.1%), p<0.01], and there was no significant reduction in hospitalisation [95% CI (-59.2% to 9.7%), p=0.11].
The authors concluded that in this study of real-world CF registry data, clinical outcomes improved and healthcare resource utilisation reduced after commencing ivacaftor.
Dr Laura Kirwan is Research Statistician at the Cystic Fibrosis Registry of Ireland
2018 Norris AW. Is Cystic Fibrosis Related Diabetes Reversible? New Data on CFTR Potentiation and Insulin Secretion. Am J Respir Crit Care Med. 2018 Sep 7. doi: 10.1164/rccm.201808-1501ED. [Epub ahead of print] [Pubmed]

Andrew Norris
A discussion on the recent publication of Kelly et el 2018 abstracted above[Pubmed]
“The Kelly et al (7) result provides hope that restoration of CFTR function might treat and prevent CFRD. However, given the current limited understanding of CFRD pathogenesis, there remains considerable uncertainty. It is possible that the fixed defects in the pancreas might prove too great a burden for the endocrine pancreas to maintain sufficient long term function. Since pancreatic disease begins in utero, it could be envisioned that CFTR restoration may need to begin before birth in order to minimize lifetime CFRD risk. Longer term clinical studies, including in patients with CFRD, will help clarify whether such an intensive approach is needed. Likewise, mechanistic study of the early life determinants of CFRD in relevant CF animal models will help unravel the fixed versus reversible underpinnings of diabetes
2018 Kissner D, LeFlore Y, Narayan SB, Marigowda G, Simard C, Le Camus C.False-positive cannabinoid screens in adult cystic fibrosis patients treated with lumacaftor/ivacaftor. J Cyst Fibros.2018 Sep 11. pii: S1569-1993(18)30754-9. doi: 10.1016/j.jcf.2018.08.006. [Epub ahead of print] Full full text available[Pubmed]

Dana Kissner
It is important that clinicians and patients be aware that false-positive cannabinoid results on urine immunoassay may occur in people taking LUM/IVA, as such results may have negative ramifications for patients in the context of home-, school-, or workplace-related drug screening and eligibility for organ transplantation.
Dr. Dana Kissner is Associate Professor, Internal Medicine at Wayne State University School of Medicine. She was named the 2018 William Stead Tuberculosis Clinician of the Year at the National Tuberculosis Controllers Association annual conference.
Dr. Andrew Norris is Professor of Biochemistry and Pedaitrics – Endocrinology and Diabetes, University of Iowa, Iowa City, Iowa.
Kirby T. Tezacaftor-ivacaftor is safe and efficacious in patients with cystic fibrosis with Phe508del mutations. Lancet Respir Med. 2018 Jan;6(1):13-14. doi: 10.1016/S2213-2600(17)30439-3. Epub 2017 Dec 14.[Pubmed]
Two phase 3 double blind, randomised, placebo-controlled trials published in the New England Journal of Medicine show that treatment with the combination of tezacaftor-ivacaftor in patients with cystic fibrosis aged 12 years and older who have the common cystic fibrosis transmembrane conductance regulator ( CFTR ) gene mutation, Phe508del, is both safe and efficacious.
– This is a useful brief update by a medical journalist on the present trials and position regarding the recent tezacaftor-ivacaftor combinations with mention of encouraging developments in the triple combination therapy.
– For details of the trial in Phe508del heterozygotes see Rowe et al. N Eng J Med 2017; 377:2024-35 ([Pubmed]); for that in Phe508del homozygotes see Taylor-Cousar et al. N Eng J Med 2017; 377:2013-23 ([Pubmed] both abstracted in the 2017 section of this History.
2018 Kim J, Davies Z, Dunn C, Wine JJ, Milla C.Ivacaftor restores CFTR-dependent sweat gland fluid secretion in cystic fibrosis subjects with S945L alleles.J Cyst Fibros. 2018 Mar;17(2):179-185. doi: 10.1016/j.jcf.2017.12.005. Epub 2017 Dec 24.[Pubmed]
A study to determine in vivo effects of CFTR modulators on mutation S945L. The authorsmeasured effects of CFTR modulators on CFTR-dependent sweating (‘C-sweat’) in two pancreatic sufficient cystic fibrosis (CF) subjects. S1 (S945L/G542X) took ivacaftor and S2 (S945L/F508del) took ivacaftor+tezacaftor. Sweating was stimulated pharmacologically to produce sequentially both CFTR-independent (methacholine stimulated) M-sweat and C-sweat; and the ratio of these was compared. Sweat secretion was measured with two methods: real time secretory rate quantitative recording and by optically measuring the growth of sweat bubbles under oil from multiple identified glands.
Using the quantitative recorder, they saw zero C-sweat secretion off-drug, but when on-drug the C-sweat responses for both subjects were comparable to those seen in carriers. The on-drug response was further quantified using the sweat bubble method. Each subject again showed robust C-sweat responses, with C-sweat/M-sweat ratios~half of the ratio determined for a cohort of 40 controls tested under identical conditions.
The authors concluded these in vivo results, consistent with prior in vitro findings, indicate that the drug treatments restore near-normal function to S945L-CFTR, and support the use of ivacaftor as a treatment for CF patients who carry this allele.
From the Cystic Fibrosis Research Laboratory, Stanford University, Stanford, CA, USA.
2018 Laselva O, Molinski S, Casavola VBear CE. Correctors of the major Cystic Fibrosis mutant interact through membrane spanning domains. Mol Pharmacol. 2018 Apr 4. pii: mol.118.111799. doi:10.1124/mol.118.111799. [Epub ahead of print]Full text [Pubmed]

Laselva Onofrio
The most common cystic fibrosis causing mutation is deletion of phenylalanine 508 (F508del), a mutation that leads to protein misassembly with defective processing. Small molecule correctors compounds: VX-809 or Corr-4a (C4) partially restore processing of the major mutant. These two prototypical corrector compounds cause an additive effect on F508del-CFTR processing and hence were proposed to act through distinct mechanisms: VX-809 stabilizing the first membrane spanning domain 1 (MSD1) and C4, acting on the second half of the molecule (consisting of MSD2 and/or nucleotide binding domain 2 (NBD2)). The authors confirmed the effect of VX-809 in enhancing the stability of MSD1 and showed that it also allosterically modulates MSD2 when co-expressed with MSD1. They showed for the first time that C4 stabilizes the second half of the CFTR protein through its action on MSD2. Given the allosteric effect of VX-809 on MSD2- they were prompted to test the hypothesis that the two correctors interact in the full length mutant protein. They did see evidence supporting their interaction in the full-length F508del-CFTR protein bearing secondary mutations targeting domain:domain interfaces. Disruption of the MSD1:F508del-NBD1 interaction (R170G) prevented correction by both compounds pointing to the importance of this interface in processing. On the other hand, stabilization of the MSD2: F508del-NBD1 interface (by introducing R1070W) led to a synergistic effect of the compound combination on the total abundance of both the immature and mature form of the protein. Together- these findings suggest that the two correctors interact in stabilizing the complex of MSDs in F508del-CFTR.
Dr. Onofrio Laselva (figure) is a post doctoral Research Scientist at the Hospital for Sick Children Toronto.
– The full text is available for the scientists who require more detail.
2018 LeGrys VA, Moon TC, Laux J, Rock MJ, Accurso F. Analytical and biological variation in repeated sweat chloride concentrations in clinical trials for CFTR modulator therapy. J Cyst Fibros. 2018 Jan;17(1):43-49. doi: 10.1016/j.jcf.2017.07.008. Epub 2017 Jul 22 [Pubmed]

Vicky A LeGrys
Using sweat chloride as a biomarker for CFTR modifying drugs requires knowledge of analytical and biological variation. 979 sweat chloride concentrations from 128 subjects enrolled in the placebo arm of 2 multicentre, investigational drug trials were analysed to determine coefficients of variation (CV) as well as reference change value (RCV) and index of individuality (II). For these populations, calculated values for the two studies were: analytical variation (3.9, 4.1%); within-subject variation (4.4, 6.0%); between-subject variation (8.9, 7.0%); RCV (13.7, 17.0%) and II (0.7, 1.0). Sweat chloride variation was not affected by sex, collection site or sample weight; but was slightly affected by age in one of the two studies.2018
Through determination of analytical as well as between- and within-subject variation, and with a larger sample size, their data allows improved estimates of the RCV and II, and can contribute to future trials of CFTR modulators and inform the design and interpretation of n of 1 trials in both research and clinical settings.
Dr. Vicky A LeGrys (figure) is a scientist in the Department of Allied Sciences, University of North Carolina. She is an expert on all aspects of sweat testing.
2018 Li H,Pesce E,Sheppard DN,Singh AK,Pedemonte N.Therapeutic approaches to CFTR dysfunction: From discovery to drug development.J Cyst Fibros.2018Mar;17(2S):S14-S21. doi: 10.1016/j.jcf.2017.08.013. Epub 2017 Sep 12 [Pubmed]
Cystic fibrosis (CF) mutations have complex effects on the cystic fibrosis transmembrane conductance regulator (CFTR) protein. They disrupt its processing to and stability at the plasma membrane and function as an ATP-gated Cl– channel. Here, the authors review therapeutic strategies to overcome defective CFTR processing and stability. Because CF mutations have multiple impacts on the assembly of CFTR protein, combination therapy with several pharmacological chaperones is likely to be required to rescue mutant CFTR expression at the plasma membrane. Alternatively, proteostasis regulators, proteins that regulate the synthesis, intracellular transport and membrane stability of CFTR might be targeted to enhance the plasma membrane expression of mutant CFTR. Finally, they consider an innovative approach to bypass CFTR dysfunction in CF, the delivery of artificial anion transporters to CF epithelia to shuttle Cl– across the apical membrane. The identification of therapies or combinations of therapies, which rescue all CF mutations, is now a priority.
– A neat summary of the present situation from Professor David Sheppard’s team in Bristol.
2018 Murer C, Huber LC, Kurowski T, Hirt A, Robinson CA, Bürgi U, Benden C. First experience in Switzerland in Phe508del homozygous cystic fibrosis patients with end-stage pulmonary disease enrolled in a lumacaftor-ivacaftor therapy trial – preliminary results.Swiss Med Wkly. 2018 Feb 16;148:w14593. doi: 10.4414/smw.2018.14593. eCollection 2018.Free full text[Pubmed]
Patients with FEV1 <40% predicted were excluded from previous studies. The authors used LUM/IVA on a “compassionate use” basis in cystic fibrosis patients with end-stage pulmonary disease. All patients from the Adult Cystic Fibrosis Centre at the University Hospital Zurich were included who were Phe508del homozygous genotype and a predicted FEV1 <40% or being evaluated or already listed for LTX.
Twenty patients were on trial with LUM/IVA; at the cut-off date, 6-month follow-up was complete for 10 patients. Respiratory related adverse events (RAEs) were severe and occurred early. The dropout rate due to RAE or lack of clinical success was 20%. Median acute exacerbation rate (AER) decreased from 2.5 in the 6 months pre-treatment to 1 during the observation period. FEV1 increased from 32 to 34.5% predicted, p = 0.292. The 6-MWD increased by a median 33 m (p = 0.6086). Sweat chloride decreased significantly by a median of 25 mmol/l (p = 0.0003). Median BMI increased from 19 to 19.9 kg/m2 (p = 0.1488). At the cut-off, three previously listed patients were paused on the transplant waiting list.
The authors concluded Phe508del homozygous cystic fibrosis patients with end-stage pulmonary disease tolerated LUM/IVA, although RAEs occurred early and were severe. This positive finding was probably due to the stepwise dose increases. There was clinical benefit mainly from reduction in AER and stabilisation of lung function. They propose that all suitable Phe508del homozygous cystic fibrosis patients with end-stage pulmonary disease should have a trial of LUM/IVA treatment in experienced centres.
Dr Christian Benden is Medical Director Lung Transplantation and CF Center Director,Division of Pulmonology, University Hospital Zurich, Switzerland
2018 McColley SA, Konstan MW, Ramsey BW, Stuart Elborn J, Boyle MP, Wainwright CE, Waltz D.Vera-Llonch M, Marigowda G, Jiang JG, Rubin JL.Lumacaftor/Ivacaftor reduces pulmonary exacerbations in patients irrespective of initial changes in FEV1. J Cyst Fibros. 2018 Aug 23. pii: S1569-1993(18)30719-7. doi: 10.1016/j.jcf.2018.07.011. [Epub ahead of print] Free full text[Pubmed]

Susanna McColley
Improved lung function and fewer pulmonary exacerbations (PEx) were observed with lumacaftor/ivacaftor (LUM/IVA) in patients with cystic fibrosis homozygous for F508del. It is unknown whether PEx reduction extends to patients without early lung function improvement.Post hoc analyses of pooled phase 3 data (NCT01807923, NCT01807949) categorized LUM/IVA-treated patients by per cent predicted forced expiratory volume in 1 s (ppFEV1) change from baseline to day 15 into threshold categories (absolute change ≤0 vs >0; relative change <5% vs ≥5%) and compared PEx rates vs placebo.
LUM (400 mg q12h)/IVA (250 mg q12h)-treated patients (n = 369) experienced significantly fewer PEx vs placebo, regardless of threshold category. With LUM/IVA, PEx rate per patient per year was 0.60 for those with absolute change in ppFEV1 > 0 and 0.85 for those with absolute change ≤0 (respective rate ratios vs placebo [95% CI]: 0.53 [0.40-0.69; P < .0001], 0.74 [0.55-0.99; = .04]
The authors concluded LUM/IVA significantly reduced PEx, even in patients without early lung function improvement.
2018 Millar BC, McCaughan J, Rendall JC, Downey DG, Moore JE. Pseudomonas aeruginosa in cystic fibrosis patients with c.1652G›A (G551D)-CFTR treated with ivacaftor-Changes in microbiological parameters. J Clin Pharm Ther. 2018 Feb;43(1):92-100. doi: 10.1111/jcpt.12616. Epub 2017 Sep 22[Pubmed]

Bronagh Millar
This study shows that microbiological parameters with patients on ivacaftor (IVA) therapy were not detrimentally affected, as there was a lower requirement IV antibiotic therapy and a reduction in the rate and density of mucoid Pseudomonas aeruginosa (M‐PA). Examination of antibiotic susceptibility, as expressed by Relative Resistance Index, against four classes of antibiotic in (a) total PA, (b) Non‐mucoid PA (NM‐PA) and (c) M‐PA, isolated from patients before and after commencement of ivacaftor therapy, showed no reduction in antibiotic susceptibility. Overall, this study suggests an improvement in the microbiology status of patients on IVA therapy.
Following commencement of IVA therapy, patients required less iv antibiotic courses but no change in number of oral antibiotics courses. There was significant reduction in both the rate of isolation and density of M-PA (P = .02; P = .006, respectively). In contrast, there was no significant reduction in both the rate of isolation and density of NM-PA (P = .90; P = .07, respectively). Antimicrobial susceptibility in NM-PA and M-PA was not significantly reduced within any of the antibiotics classes or individual antibiotics examined. Increased susceptibility was noted in the beta-lactam class for NM-PA and M-PA, in particular with ceftazidime.Overall, (i) the requirement for less iv antibiotic therapy,(ii) a reduction in the rate and density of M- PA and (iii) no reduction in antibiotiDr.
Bronagh Millar (figure) is a Research Fellow at the School of Mechanical and Aerospace Engineering, Queens University, Belfast.
2018 Pranke I, Bidou L, Martin N, Blanchet S, Hatton A, Karri S, Cornu D, Costes B, Chevalier B, Tondelier D, Girodon E, Coupet M, Edelman A, Fanen P, Namy O, Sermet-Gaudelus I, Hinzpeter A. Factors influencing readthrough therapy for frequent cystic fibrosis premature termination codons. ERJ Open Res.2018 Feb 23;4(1). pii: 00080-2017. doi: 10.1183/23120541.00080-2017. eCollection 2018 Jan.Full text available [Pubmed]
Premature termination codons (PTCs) are generally associated with severe forms of genetic diseases. Readthrough of in-frame PTCs using small molecules is a promising therapeutic approach. Nonetheless, the outcome of preclinical studies has been low and variable. Treatment efficacy depends on: 1) the level of drug-induced readthrough, 2) the amount of target transcripts, and 3) the activity of the recoded protein.
The aim of the present study was to identify, in the cystic fibrosis transmembrane conductance regulator (CFTR) model, recoded channels from readthrough therapy that may be enhanced using CFTR modulators. First, drug-induced readthrough of 15 PTCs was measured using a dual reporter system under basal conditions and in response to gentamicin and negamycin. Secondly, exon skipping associated with these PTCs was evaluated with a minigene system. Finally, incorporated amino acids were identified by mass spectrometry and the function of the predicted recoded CFTR channels corresponding to these 15 PTCs was measured. Non-functional channels were subjected to CFTR-directed ivacaftor-lumacaftor treatments. The results demonstrated that CFTR modulators increased activity of recoded channels, which could also be confirmed in cells derived from a patient. In conclusion, this work will provide a framework to adapt treatments to the patient’s genotype by identifying the most efficient molecule for each PTC and the recoded channels needing co-therapies to rescue channel function.
– A helpful review of the present situation regarding PTCs from a leading French group
Dr. Iwona Pranke is Post Doctoral Researcher at the Institut Necker, Paris.
2018 Popowicz N, Wood J, Tai A, Morey S, Mulrennan S.Immediate effects of lumacaftor/ivacaftor administration on lung function in patients with severe cystic fibrosis lung disease.J Cyst Fibros. 2017 May;16(3):392-394. doi: 10.1016/j.jcf.2017.02.009. Epub 2017 Mar 15. [Pubmed]
Safety-data for lumacaftor/ivacaftor (LUM/IVA) combination therapy in patients with severe lung disease (percent predicted forced expiratory volume in 1s [ppFEV1] <40) remain limited. The authors report immediate post-dose respiratory-related adverse events in 12 patients with severe cystic fibrosis (CF) lung disease (median [IQR] ppFEV1: 34 [31-36]) prescribed LUM/IVA. All patients experienced a decline in ppFEV1 from baseline at 2-hours (median [IQR] relative change: -19 [-21 to -11]%, p<0.001) that persisted at 24-hours but recovered in most patients at 1-month. No pre- and post-differences in bronchodilator response were observed. Ten (83.3%) patients reported non-severe respiratory-related adverse events within 24-hours of LUM/IVA initiation. At 1-month, eight (67%) patients had persistent symptoms and six (50%) were treated for a pulmonary exacerbation.
– The authors suggest their results highlight that LUM/IVA respiratory-related adverse events are common in patients with a ppFEV1<40. They recommend close assessment of adverse events. Further studies are required to evaluate the efficacy of LUM/IVA in patients with severe lung disease.
2018 Ren CL, Morgan RL, Oermann C, Resnick HE, Brady C, Campbell A, DeNagel R, Guill M, Hoag J, Lipton A, Newton T, Peters S, Willey-Courand DB, Naureckas ET.Cystic Fibrosis Foundation Pulmonary Guidelines: Use of CFTR Modulator Therapy in Patients with Cystic Fibrosis. Ann Am Thorac Soc. 2018 Jan 17. doi: 10.1513/AnnalsATS.201707-539OT. [Epub ahead of print[Pubmed]

Clement L Ren
A multidisciplinary committee of CF caregivers and patient representatives was assembled. A systematic review was conducted to find relevant publications. The systematic review yielded 6 publications applicable to our clinical questions.
In summary their recommendations were as follows – “For adults and children aged 6 years and older with CF due to gating mutations other than G551D or R117H,(i.e G178R, S549N, S549R, G551S, G1244E, S1251N, S1255P, or G1349D)the guideline made a conditional recommendation for treatment with ivacaftor (IVA) for 1) adult aged 18 years and older and 2) for children aged 6-17 years with an FEV1 of less than 90% predicted. For those with the R117H mutation, the guideline made a conditional recommendation against treatment with IVA for 1) children aged 2-17 years with an FEV1 greater than 90% predicted and 2) children less than 6 years of age. Among those with two copies of F508del the guideline panel made a strong recommendation for treatment with ivacaftor/lumacaftor for 1) adults and children 12 years and older with an FEV1 greater than 90% predicted and 2) children aged 6-11 years”.
The authors suggest that these recommendations will be of help to CF clinicians, patients, and their families in guiding decisions regarding use of these medications.
Clement L Ren is professor of Clinical Paediatrics in the Section of Paediatric Pulmonolgy, Allergy and Sleep Medicine, Indiana University School of Medicine.
2018 Ronan NJ, Einarsson GG, Twomey M, Mooney D, Mullane D, NiChroinin M, O’Callaghan G, Shanahan F, Murphy DM, O’Connor OJ, Shortt CA, Tunney MM, Eustace JA, Maher MM, Elborn JS, Plant BJ. CORK Study in Cystic Fibrosis: Sustained Improvements in Ultra-Low-Dose Chest CT Scores After CFTR Modulation With Ivacaftor.Chest. 2018 Feb;153(2):395-403.doi: 10.1016/j.chest.2017.10.005. Epub 2017 Oct 14 [Pubmed]
Ivacaftor produces significant clinical benefit in patients with cystic fibrosis (CF) with the G551D mutation. Prevalence of this mutation at the Cork CF Centre is 23%. This study assessed the impact of cystic fibrosis transmembrane conductance regulator modulation on multiple modalities of patient assessment. Thirty-three patients with the G551D mutation were assessed at baseline and prospectively every 3 months for 1 year after initiation of ivacaftor. Change in ultra-low-dose chest CT scans, blood inflammatory mediators, and the sputum microbiome were assessed. Significant improvements in FEV1, BMI, and sweat chloride levels were observed post-ivacaftor treatment. Improvement in ultra-low-dose CT imaging scores were observed after treatment, with significant mean reductions in total Bhalla score (P < .01), peribronchial thickening (P = .035), and extent of mucous plugging (P < .001). Reductions in circulating inflammatory markers, including interleukin (IL)-1β, IL-6, and IL-8 were demonstrated. There was a 30% reduction in the relative abundance of Pseudomonas species and an increase in the relative abundance of bacteria associated with more stable community structures. Post treatment community richness increased significantly (P = .03).
The authors concluded early and sustained improvements on ultra-low-dose CT scores suggest it may be a useful method of evaluating treatment response. It paralleled improvement in symptoms, circulating inflammatory markers, and changes in the lung microbiota.
2018 Rosenfeld M,Wainwright CE,Higgins M,Wang LT,McKee C,Campbell D,Tian S,Schneider J,Cunningham S,Davies JC;ARRIVAL study group.Ivacaftor treatment ofcystic fibrosisin children aged 12 to <24 months and with a CFTR gating mutation (ARRIVAL): a phase 3 single-arm study. Lancet Respir Med.2018Jun 6. pii: S2213-2600(18)30202-9. doi: 10.1016/S2213-2600(18)30202-9. [Epub ahead of print] [Pubmed]

Margaret Rosenfield
The ARRIVAL study is a phase 3, single-arm, two-part, multicentre study. Eligible children were aged 12 to <24 months at enrolment and had a confirmed diagnosis of cystic fibrosis and a CFTR gating mutation on at least one allele and could participate in one or both parts of the study.
Children received 50 mg (bodyweight 7 to <14 kg) or 75 mg (bodyweight ≥14 to <25 kg) ivacaftor orally every 12 h. In study part A, children received ivacaftor for 3 days plus one morning. In study part B, children received 24 weeks of treatment. Seven children were enrolled in part A, of whom five received 50 mg and two received 75 mg ivacaftor. All completed treatment. Of 19 children enrolled in part B, including one from part A, all received 50 mg ivacaftor and 18 completed treatment (one withdrew because of difficulty with blood draws). All children received at least one dose of ivacaftor. Pharmacokinetics indicated exposure was similar to that in children aged 2 to <6 years and adults. No children discontinued because of adverse events or safety findings. In part A, three (43%) of seven children had treatment-emergent adverse events, all of which were mild and deemed not to be or unlikely to be related to ivacaftor. By 24 weeks in part B, treatment-emergent adverse events had been reported in 18 (95%) of 19 children, of which most were mild or moderate and the most frequent was cough (14 [74%] children). Two children in part B had four serious adverse events: one had constipation (possibly related to ivacaftor), distal intestinal obstruction syndrome, and eczema herpeticum, and one had persistent cough, all needing hospital admission. In five (28%) of 18 children aspartate or alanine aminotransferase concentrations rose to more than three times the upper limit of normal (to more than eight times in two children with concurrent infections). At week 24, the mean absolute change from baseline in sweat chloride concentration was -73·5 (SD 17·5) mmol/L. Growth parameters for age were normal at baseline and at week 24. At week 24, concentrations of faecal elastase-1 had increased and concentrations of immunoreactive trypsinogen had decreased from baseline. Mean serum lipase and amylase were raised at baseline and rapidly decreased after treatment was started.
The authors concluded that ivacaftor was generally safe and well tolerated in children aged 12 to <24 months for up to 24 weeks and was associated with rapid and sustained reductions in sweat chloride concentrations. Improvements in biomarkers of pancreatic function suggest that ivacaftor preserves exocrine pancreatic function if started early. The study is continuing in infants younger than 12 months.
2018 Sharma D, Xing S, Hung YT, Caskey RN, Dowell ML, Touchette DR.Cost-effectiveness analysis of lumacaftor and ivacaftor combination for the treatment of patients with cystic fibrosis in the United States.Orphanet J Rare Dis.2018Sep 29;13(1):172. doi: 10.1186/s13023-018-0914-3. Free PMC Article[Pubmed]
The objective of this study was to assess the cost-effectiveness of lumacaftor/ivacaftor combination (Orkambi) for the treatment of CF homozygous for F508del CF Transmembrane Conductance Regulator (CFTR) mutation. Under the base-case, Lumacaftor/ivacaftor resulted in higher QALYs (7.29 vs 6.84) but at a very high cost ($1,778,920.88) compared to usual care ($116,155.76) over a 10-year period. The ICER for base-case and worst-case scenarios were $3,655,352 / QALY, and $8,480,265/QALY gained, respectively. In the base-case, lumacaftor/ivacaftor was cost-effective at a threshold of $150,000/QALY-gained when annual drug costs were lower than $4153. The results were not substantially affected by the sensitivity analyses.
The intervention produces large QALY gains but at an extremely high cost, resulting in an ICER that would not typically be covered by any insurer. Lumacaftor/ivacaftor’s status as an orphan drug complicates coverage decisions.
From the Department of Pharmacy Systems, Outcomes & Policy, College of Pharmacy, University of Illinois at Chicago, Chicago, IL, USA.
2018 Sala MA, Jain M. Tezacaftor for the treatment of cystic fibrosis. Expert Rev Respir Med. 2018 Sep;12(9):725-732. doi: 10.1080/17476348.2018.1507741. Epub 2018 Aug 9. [Pubmed]
Cystic fibrosis (CF) is the most common, life-limiting autosomal recessive disease in Caucasians, and is caused by defects in production of the CFTR ion channel. Until recently, there were no available treatments targeting the disease-causing defects in CFTR but newly developed CFTR modulators are changing the course of disease in CF. The newest modulator, tezacaftor, is a CFTR corrector that was recently approved by the FDA to be used in combination with the first approved CFTR potentiator, ivacaftor. Areas covered: A detailed review of the clinical trials and published literature, focusing on safety and efficacy, leading to the approval of tezacaftor in CF. Expert commentary: Recent trials have demonstrated that the combination of tezacaftor-ivacaftor is a slightly superior combination to its predecessor, lumacaftor-ivacaftor, with respect to an increase in FEV1, adverse event profile, and drug-drug interactions. It is also approved for a large number of non-F508del, residual function mutations that are predicted to respond based on in vitro testing. The horizon for continued improvements in CFTR-targeted treatments is promising, with three-drug combinations currently in Phase 3 clinical trials, and other drugs with novel mechanisms of action being studied. Within the next 5 years, the vast majority of patients with CF are expected to have a modulator approved for their genotype.
2018 Sawicki GS, Fink AK, Schechter MS, Loeffler DR, Mayer-Hamblett N.Rate and predictors of prescription of lumacaftor – Ivacaftor in the 18 months following approval in the United States. J Cyst Fibros.2018Sep 7. pii: S1569-1993(18)30755-0. doi: 10.1016/j.jcf.2018.08.007. [Epub ahead of print][Pubmed]

Gregory Sawicki
Lumacaftor-ivacaftor (LUM-IVA) was approved in the US in 2015 for patients with CF aged >12 homozygous for the delF508 mutation, and patients aged 6 to 12 in 2016. The authors examined the rate of initial LUM-IVA prescriptions following approval. They compared patients eligible for LUM-IVA in the CF Foundation Patient Registry with and without prescriptions in 2015-2016.
5534 (53%) eligible patients had reported prescriptions. Prescription rate in children ages 6-11 was 19% and 61% among patients ≥12 years old. Individuals ≥12 with prescriptions more likely observed among those with private insurance, clinical trial participation, ages 18-30, FEV1 < 90%, more pulmonary exacerbations, and more use of chronic medications.
The authors concluded LUM-IVA uptake was less rapid than what was previously observed for ivacaftor, a CFTR modulator approved for a different population. Age, insurance status, disease severity and use of other therapies differed in those prescribed LUM-IVA in the initial post-approval period.
Gregory Sawicki is Director of the Cystic Fibrosis Center, Boston Children’s Hospital and Assistant Professor of Pediatrics, Harvard Medical School.
2018 Southern KW,Patel S, Sinha IP, Nevitt SJ.Correctors (specific therapies for class II CFTR mutations) for cystic fibrosis.Cochrane Database Syst Rev. 2018 Aug 2;8:CD010966. doi: 10.1002/14651858.CD010966.pub2. [Epub ahead of print] [Pubmed]

Kevin Southern
After a detailed consideration of the available published evidence (please see full abstract for details)the authors concluded there was insufficient evidence that monotherapy with correctors has clinically important effects in people with CF who have two copies of the F508del mutation. Combination therapies (lumacaftor-ivacaftor and tezacaftor-ivacaftor) each result in similarly small improvements in clinical outcomes in people with CF; specifically improvements quality of life (moderate-quality evidence), in respiratory function (high-quality evidence) and lower pulmonary exacerbation rates (moderate-quality evidence). Lumacaftor-ivacaftor is associated with an increase in early transient shortness of breath and longer-term increases in blood pressure (high-quality evidence). These adverse effects were not observed for tezacaftor-ivacaftor. Tezacaftor-ivacaftor has a better safety profile, although data are not available for children younger than 12 years. In this age group, lumacaftor-ivacaftor had an important impact on respiratory function with no apparent immediate safety concerns, but this should be balanced against the increase in blood pressure and shortness of breath seen in longer-term data in adults when considering this combination for use in young people with CF.
Professor Kevin Southern is Professor of Paediatrics at the Alder Hey Children’s Hospital and Liverpool University.
2018 Stallings VA, Sainath N, Oberle M, Bertolaso C, Schall JI. Energy Balance and Mechanisms of Weight Gain with Ivacaftor Treatment of Cystic FibrosisGating Mutations. J Pediatr. 2018 Oct;201:229-237.e4. doi: 10.1016/j.jpeds.2018.05.018. Epub 2018 Jul 18. [Pubmed]

Virginia Stallings
A study to determine if ivacaftor treatment results in weight gain and improved pulmonary function in people with cystic fibrosis transmembrane conductance regulator gating mutations. Children and adults with cystic fibrosis and at least 1 cystic fibrosis transmembrane conductance regulator gating mutation were evaluated in this observational study before and after 3 months of ivacaftor treatment. Body size and composition, total energy expenditure, resting energy expenditure (REE%) as percent predicted, coefficient of fat absorption (CFA%), fecal calprotectin, fecal elastase, and quality of life were assessed. Some outcomes were explored by pancreatic status.
There were 23 patients (5-61 years of age) who completed the study; 70% had pancreatic insufficiency (PI). Patients gained 2.5 ± 2.2 kg (P < .001) with increased (P < .05) fat-free mass (0.9 ± 1.9 kg) and fat mass (1.6 ± 1.5 kg). REE% decreased by 5.5 ± 12.0% (P < .05), fecal calprotectin decreased by 30 ± 40 µg/g stool (P < .01), and total energy expenditure was unchanged. Improvements were greater for PI than patients who were pancreatic-sufficient. CFA% increased significantly only with PI. The change (Δ) in weight was positively correlated with the percent change in forced expiratory volume at 1 second (r = 0.46; P = .028) and ΔCFA% (r = 0.47; P = .032) and negatively with ΔREE% (r = -0.50; P = .017). Together, ΔREE%, ΔCFA%, and the percent change in forced expiratory volume at 1 second explained 58% of the variance in weight gain (adjusted R2 = 0.579; P = .0007). Growth status and muscle strength improved, as did quality of life in several domains. Fecal elastase increased in most patients with pancreatic sufficiency, with no change in those with PI.
The authors’ identified mechanisms for ivacaftor-associated weight gain were decreased resting energy expenditure, gut inflammation, and fat malabsorption.
Dr Virginia A Stallings is a nutrition paediatrician and Jean A. Cortner Endowed Chair in the Division of Gastroenterology, Hepatology and Nutrition at Children’s Hospital of Philadelphia. She is the Research Director in the Nutrition Center.
2018 Thomassen JC, Mueller MI, Alejandre Alcazar MA, Rietschel E, van Koningsbruggen-Rietschel S. Effect of Lumacaftor/Ivacaftor on glucose metabolism and insulin secretion in Phe508del homozygous cystic fibrosis patients. J Cyst Fibros. 2018 Mar;17(2):271-275. doi: 10.1016/j.jcf.2017.11.016. Epub 2017 Dec 15. [Pubmed]

Silke van Koningsbruggen
A study to investigate the effect of Lumacaftor/Ivacaftor on glucose metabolism and insulin secretion in patients with cystic fibrosis(CF) (Phe508del/Phe508del). A standard oral glucose tolerance test (OGTT) and an intravenous glucose tolerance test (IVGTT) were performed to investigate glucose metabolism and insulin secretion before and after 6-8weeks of treatment with Lumacaftor/Ivacaftor in 5 Phe508del-homozygous CF patients. The area under the curve (AUC) for glucose and insulin levels was calculated using the trapezoidal approximation. 5 participants were investigated. Treatment with Lumacaftor/Ivacaftor was followed by an improvement of the 2h glucose levels in 3 patients and worsening in 2 patients. Analysis of the time course of blood glucose levels during OGTT revealed an increase of the AUC in 3 of 5 patients. In response to IVGTT, acute insulin secretion improved in 2 patients and worsened in three.
The authors concluded their investigation could not demonstrate that treatment with Lumacaftor/Ivacaftor had a consistent impact on glucose tolerance and insulin secretion. They suggested further adequately-powered studies examining glucose metabolism are needed.
Dr Silke van Koningsbruggen is at the Cystic Fibrosis Center University Hospital Cologne.
2018 Trimble AT, Donaldson SH. Ivacaftor withdrawal syndrome in cystic fibrosis patients with the G551D mutation. J Cyst Fibros.2018Mar;17(2):e13-e16. doi: 10.1016/j.jcf.2017.09.006. Epub 2017 Oct 24. [Pubmed]

Aaron Trimble
Ivacaftor use can lead to dramatic health improvements in cystic fibrosis (CF) patients with gating mutations.
Here, we report five instances of dramatic clinical decline following withdrawal of ivacaftor in three individuals with the G551D-CFTR mutation. In each case, the patient’s lung function and symptoms rapidly deteriorated after cessation of treatment. Awareness of this phenomenon should inform both clinical practices as well as the design of future clinical trials of highly active CFTR modulator
Dr. Aaron Trimble is in the Division of Pulmonary & Critical Care Medicine, Division of Medicine, University of North Carolina School of Medicine, Chapel Hill,
Vadagam P, Kamal KM, Covvey JR, Giannetti V, Mukherjee KCost-Effectiveness and Budget Impact of Lumacaftor/Ivacaftor in the Treatment of Cystic Fibrosis. J Manag Care Spec Pharm.2018Oct;24(10):987-997. doi: 10.18553/jmcp.2018.24.10.987. Free full text [Pubmed]
A cost-effectiveness analysis (CEA) of lumacaftor/ivacaftor (Orkambi) to understand the overall effectiveness of the drug compared with its costs and (b) conduct a budget impact analysis (BIA) to understand the potential financial effect of introducing a new drug in a health plan. The annual cost of therapy per patient for lumacaftor/ivacaftor was $379,780. The ACER for lumacaftor/ivacaftor was $151,912, while the ICER for lumacaftor/ivacaftor compared with placebo was $95,016 per FEV1% predicted. The annual total budget impact due to the inclusion of lumacaftor/ivacaftor on the health plan formulary was $266,046.
In patients with CF, lumacaftor/ivacaftor (Orkambi) has demonstrated better clinical effectiveness compared with placebo alongside an increased drug acquisition cost. However, the therapy may be a viable alternative to existing standard therapy over a short time horizon. Health care payers, both private and public, need to evaluate the cost-effectiveness and the financial effect when considering expansion of new drug coverage in CF management.
– More details in the PubMed abstract and free Full text
2018 Vadagam P, Kamal KM, Covvey JR, Giannetti V, Mukherjee K. Cost-Effectiveness and Budget Impact of Lumacaftor/Ivacaftor in the Treatment of Cystic Fibrosis. J Manag Care Spec Pharm. 2018 Oct;24(10):987-997. doi: 10.18553/jmcp.2018.24.10.987. Free full text [Pubmed]
A cost-effectiveness analysis (CEA) of lumacaftor/ivacaftor (Orkambi) to understand the overall effectiveness of the drug compared with its costs and (b) conduct a budget impact analysis (BIA) to understand the potential financial effect of introducing a new drug in a health plan. The annual cost of therapy per patient for lumacaftor/ivacaftor was $379,780. The ACER for lumacaftor/ivacaftor was $151,912, while the ICER for lumacaftor/ivacaftor compared with placebo was $95,016 per FEV1% predicted. The annual total budget impact due to the inclusion of lumacaftor/ivacaftor on the health plan formulary was $266,046. In patients with CF, lumacaftor/ivacaftor (Orkambi) has demonstrated better clinical effectiveness compared with placebo alongside an increased drug acquisition cost. However, the therapy may be a viable alternative to existing standard therapy over a short time horizon. Health care payers, both private and public, need to evaluate the cost-effectiveness and the financial effect when considering expansion of new drug coverage in CF management.
– More details in the PubMed abstract and free Full text
Pratyusha Vadagam is in the Division of Pharmaceutical, Administrative and Social Sciences, Duquesne University School of Pharmacy, Pittsburgh, Pennsylvania.
Wang Y, Cai Z, Gosling M, Sheppard DN.Potentiation of the cystic fibrosis transmembrane conductance regulator Cl– channel by ivacaftor is temperature-independent.Am J Physiol Lung Cell Mol Physiol. 2018 Aug 23. doi: 10.1152/ajplung.00235.2018. [Epub ahead of print][Pubmed]
Ivacaftor is the first drug to target directly defects in the cystic fibrosis transmembrane conductance regulator (CFTR), which cause cystic fibrosis (CF). To understand better how ivacaftor potentiates CFTR channel gating, here we investigated the effects of temperature on its action. As a control, we studied the benzimidazolone UCCF-853, which potentiates CFTR by a different mechanism. Using the patch-clamp technique and cells expressing recombinant CFTR, we studied the single-channel behavior of wild-type and F508del-CFTR, the most common CF mutation. Raising the temperature of the intracellular solution from 23 to 37 °C increased the frequency, but reduced the duration of wild-type and F508del-CFTR channel openings. While the open probability (Po) of wild-type CFTR increased progressively as temperature was elevated, the relationship between Po and temperature for F508del-CFTR was bell-shaped with a maximum Po at ~30 °C. For wild-type CFTR and, to a greatly reduced extent, F508del-CFTR, the temperature-dependence of channel gating was asymmetric with the opening rate demonstrating greater temperature sensitivity than the closing rate. At all temperatures tested, ivacaftor and UCCF-853 potentiated wild-type and F508del-CFTR. Strikingly, ivacaftor, but not UCCF-853, abolished the asymmetric temperature-dependence of CFTR channel gating. At all temperatures tested, Po values of wild-type CFTR in the presence of ivacaftor were approximately double those of F508del-CFTR, which were equivalent to or greater than those of wild-type CFTR at 37 °C in the absence of the drug.
The authors concluded that the principal effect of ivacaftor is to promote channel opening to abolish the temperature-dependence of CFTR channel gating.
2018 Wu HX, Zhu M, Xiong XF, Wei J, Zhuo KQ, Cheng DY. Efficacy and Safety of CFTR Corrector and Potentiator Combination Therapy in Patients with Cystic Fibrosis for the F508del-CFTR Homozygous Mutation: A Systematic Review and Meta-analysis. Adv Ther. 2019 Feb;36(2):451-461. doi: 10.1007/s12325-018-0860-4. Epub 2018 Dec 15. [Pubmed]
The authors performed a systematic review and meta-analysis of randomized controlled trials (RCTs) to evaluate the efficacy and safety of combination therapy on lung function, nutritional status, clinical score and safety in CF for the F508del-CFTR homozygous mutation.
Five RCTs, including a total of 1637 participants with the F508del-CFTR homozygous mutation who accepted CFTR corrector and potentiator combination therapy along with basic treatment were enrolled in this analysis. Primary analysis revealed that combination therapy improved the percent of predicted FEV1 (ppFEV1) (MD 2.38, 1.62-3.15, P < 0.00001), Cystic Fibrosis Questionnaire-Revised (CFQ-R) respiratory domain score (MD 2.59, 0.96-4.22, P = 0.002) and body-mass index (BMI) (MD 0.21, 0.03-0.39, P = 0.02). In the secondary analysis, combination therapy had no impact on the number of participants reporting adverse events (OR 0.88, 0.58-1.33, P = 0.53), but increased the proportion of discontinued treatments due to adverse events (OR 2.71, 1.3-5.63, P = 0.008).
The authors concluded potentiator combination therapy effectively improves lung function, nutritional status and clinical score in CF patients with the F508del-CFTR homozygous mutation, and has an acceptable safety profile.
From the Department of Respiratory and Critical Care Medicine, West China Hospital, Sichuan University, Chengdu, China.
2019 2019 2019
Akshintala VS, Kamal A, Faghih M, Cutting GR, Cebotaru L, West NE, Jennings MT, Dezube R, Whitcomb DC, Lechtzin N, Merlo CA, Singh VK.Cystic fibrosis transmembrane conductance regulator modulators reduce the risk of recurrent acute pancreatitis among adult patients with pancreas sufficient cystic fibrosis. Pancreatology. 2019 Sep 28. pii: S1424-3903(19)30735-5. doi: 10.1016/j.pan.2019.09.014. [Epub ahead of print] [Pubmed]
Approximately 1 in 5 patients with pancreas sufficient cystic fibrosis (PS-CF) will develop acute pancreatitis (AP). It is not known whether ivacaftor alone or in combination with other CFTR (cystic transmembrane regulator) modulators (tezacaftor or lumacaftor) can reduce the risk of AP in patients with PS-CF and AP history.
The authors retrospectively queried the CF registry at our institution for adult patients with PS-CF, a documented history of AP and initiation of CFTR modulators for pulmonary indications. Patient characteristics including demographics, CFTR genotype, pancreatitis risk factors, pancreatic exocrine function and other relevant laboratory, imaging parameters were obtained from the time of the sentinel AP episode through the follow-up period.
A total of 15 adult CF patients were identified with mean age of 44.1 years (SD ± 13.8). In the 24 months preceding CFTR modulator initiation, six of these patients had at least 1 episode of AP with median of 2 episodes [1.75, 2.5]. None of the patients had evidence of pancreatic calcifications or exocrine pancreas insufficiency at the time of CFTR modulator initiation. The mean duration of follow-up after CFTR modulator initiation was 36.7 months (SD ± 21.5). None of the patients who remained on CFTR modulators developed an episode of AP or required hospitalisation for AP related abdominal pain during follow-up.
The authors concluded CFTR modulators, alone or in combination, substantially reduce the risk of recurrent AP over a mean follow-up period of 3 years in adult patients with PS-CF and a history of prior AP. These data suggest that any augmentation of CFTR function can reduce the risk of pancreatitis.
From the Pancreatitis Center, Division of Gastroenterology, Johns Hopkins Medical Institutions, Baltimore, MD, USA
Dr Valentine Sergeev is in the Faculty of Medicine, University of British Columbia, Vancouver, BC, Canada
Dr Bradley S Quon, the corresponding author, is at the Centre for Heart Lung Innovation, Vancouver.
– This is a very useful comprehensive referenced review of the many extra-pulmonary effects of CFTR modulators reported to the present time. The full article can be downloaded (https://www.researchgate.net/profile/Valetnine_Sergeev).
Aksit MA, Bowling AD, Evans TA, Joynt AT, Osorio D, Patel S, West N, Merlo C, Sosnay PR, Cutting GR, Sharma N. Decreased mRNA and protein stability of W1282X limits response to modulator therapy. J Cyst Fibros. 2019 Feb 22. pii: S1569-1993(19)30027-X. doi: 10.1016/j.jcf.2019.02.009. [Epub ahead of print] [Pubmed]
Cell-based studies have shown that W1282X generates a truncated protein that can be functionally augmented by modulators. However, modulator treatment of primary cells from individuals who carry two copies of W1282X generates no functional CFTR. To understand the lack of response to modulators, we investigated the effect of W1282X on CFTR RNA transcript levels.qRT-PCR and RNA-seq were performed on primary nasal epithelial (NE) cells of a previously studied individual who is homozygous for W1282X, her carrier parents and control individuals without nonsense variants in CFTR.
CFTR RNA bearing W1282X in NE cells shows a steady-state level of 4.2 ± 0.9% of wild-type (WT) CFTR RNA in the mother and 12.4 ± 1.3% in the father. NMDI14, an inhibitor of nonsense-mediated mRNA decay (NMD), restored W1282X mRNA to almost 50% of WT levels in the parental NE cells. RNA-seq of the NE cells homozygous for W1282X showed that CFTR transcript level was reduced to 1.7% of WT (p-value: 4.6e-3). Negligible truncated CFTR protein was generated by Flp-In 293 cells stably expressing the W1282X EMG even though CFTR transcript was well above levels observed in the parents and proband. Finally, we demonstrated that NMD inhibition improved the stability and response to correctors of W1282X-CFTR protein expressed in the Flp-In-293 cells.
The authors concluded their results show that W1282X can cause substantial degradation of CFTR mRNA that has to be addressed before efforts aimed at augmenting CFTR protein function can be effective.
From the McKusick-Nathans Institute of Genetic Medicine, Johns Hopkins University School of Medicine, Baltimore, MD, United States.
Amico G, Brandas C, Moran O, Baroni D. Unravelling the Regions of Mutant F508del-CFTR More Susceptible to the Action of Four Cystic Fibrosis Correctors. Int J Mol Sci.2019 Nov 1;20(21). pii: E5463. doi: 10.3390/ijms20215463. Free full text [Pubmed]

Debora Baroni
Cystic fibrosis (CF) is a genetic disease associated with the defective function of the cystic fibrosis transmembrane conductance regulator (CFTR) protein that causes obstructive disease and chronic bacterial infections in airway epithelia. The most prevalent CF-causing mutation, the deletion of phenylalanine at position 508 (F508del), leads to CFTR misfolding, trafficking defects and premature degradation. A number of correctors that are able to partially rescue F508del-CFTR processing defects have been identified. Clinical trials have demonstrated that, unfortunately, mono-therapy with the best correctors identified to date does not ameliorate lung function or sweat chloride concentration in homozygous F508del patients. Understanding the mechanisms exerted by currently available correctors to increase mutant F508del-CFTR expression is essential for the development of new CF-therapeutics.
The authors investigated the activity of correctors on the mutant F508del and wild type (WT) CFTR to identify the protein domains whose expression is mostly affected by the action of correctors, and we investigated their mechanisms of action.
They found that the four correctors under study, lumacaftor (VX809), the quinazoline derivative VX325, the bithiazole compound corr4a, and the new molecule tezacaftor (VX661), do not influence either the total expression or the maturation of the WT-CFTR transiently expressed in human embryonic kidney 293 (HEK293) cells. Contrarily, they significantly enhance the expression and the maturation of the full length F508del molecule. Three out of four correctors, VX809, VX661 and VX325, seem to specifically improve the expression and the maturation of the mutant CFTR N-half (M1N1, residues 1-633). By contrast, the CFTR C-half (M2N2, residues 837-1480) appears to be the region mainly affected by corr4a. VX809 was shown to stabilize both the WT- and F508del-CFTR N-half isoforms, while VX661 and VX325 demonstrated the ability to enhance the stability only of the mutant F508del polypeptide.
Corresponding author is Dr Debora Baroni of the Istituto di Biofisica, Consiglio Nazionale delle Ricerche, 16149 Genova, Italy.
Barry P J, Jones AM, After the Celebrations: Lessons from the New Era of Cystic Fibrosis Transmembrane Conductance Regulator Modulator Therapy. Ann Am Thorac Soc 2019; 16(2):189-190. [Pubmed]

Peter J Barry
Peter Barry and Andrew Jones of Manchester, in an editorial discuss this paper. They note that the use of national and international registries has become increasingly commonplace. They discuss the potential problems of patient inclusion including the accuracy of registry recorded data. Registry data willl have less strict monitoring than in clinical trials. The headline results of this present study are that the significant benefits ivacaftor therapy seen in clinical trials are replicated in real life practice in patients aged 6 years and over. They discuss the reduced need for intravenous antibiotics on ivacaftor but caution against considering time on IV antibiotics as synonymous with pulmonary exacerbations and suggest this may be related to a number of different factors including a change in patient and physician thresholds for treatment. The reduced rate of decline appears to be encouraging in children and adolescents but in adults the initial improvement appears to progress after ivacaftor introduction in contrast to the findings in the initial trails. The possible reasons are discussed including the inevitable progression in lungs already significantly damaged or could the reduced need for antibiotics be related. They consider it essential that such studies are are continued and honed to ensure the maximum benefits of CFTR modulator therapy in the wider context of CF clinical care.
Bell SC, Mainz JG, MacGregor G, Madge S, Macey J, Fridman M, Suthoff ED, Narayanan S, Kinnman N. Patient-reported outcomes in patients with cystic fibrosis with a G551D mutation on ivacaftor treatment: results from a cross-sectional study. BMC Pulm Med. 2019 Aug 13;19(1):146. doi: 10.1186/s12890-019-0887-6.Free article[Pubmed]

Scott Bell
Clinical studies demonstrate that ivacaftor (IVA) improves health-related quality of life (HRQoL) in patients aged ≥6 years with cystic fibrosis (CF). The real-world impact of IVA and standard of care (SOC) in groups of patients with G551D and F508del mutations, respectively, was assessed using a survey comprising disease-specific and generic HRQoL measures. Patients with CF aged ≥12 years, or aged 6-11 years with caregiver support, with either (1) a G551D mutation and receiving IVA (G551D/IVA) for ≥3 months, or (2) homozygous for F508del and receiving SOC before lumacaftor/IVA availability (F508del/SOC), were eligible to participate in a cross-sectional survey. Demographic and clinical characteristics, and HRQoL measures were compared between patient groups, and multiple regression analyses were conducted. After differences in patient demographic and clinical characteristics were controlled for, significantly better scores were observed in the G551D/IVA group than in the F508del/SOC group on multiple domains of the validated Cystic Fibrosis Questionnaire-Revised and the EuroQol 5-dimensions 5-level questionnaire.
The authors concluded G551D/IVA patients reported better HRQoL than F508del/SOC patients on generic and disease-specific measures in a real-world setting
Dr Scott Bell is in the Department of Thoracic Medicine, The Prince Charles Hospital and QIMR Berghofer Medical Research Institute, Brisbane, QLD, Australia.
Bell SC, Mall MA, Gutierrez H, Macek M, Madge S, Davies JC, et al.The future of cystic fibrosis care: a global perspective.Lancet Respir Med. 2019 Sep 27. pii: S2213-2600(19)30337-6. doi: 10.1016/S2213-2600(19)30337-6. [Epub ahead of print] [Pubmed]
This is an important review by 39 international experts in cystic fibrosis. The past six decades have seen remarkable improvements in health outcomes for people with cystic fibrosis, which was once a fatal disease of infants and young children. However, although life expectancy for people with cystic fibrosis has increased substantially, the disease continues to limit survival and quality of life, and results in a large burden of care for people with cystic fibrosis and their families. Furthermore, epidemiological studies in the past two decades have shown that cystic fibrosis occurs and is more frequent than was previously thought in populations of non-European descent, and the disease is now recognised in many regions of the world. The Lancet Respiratory Medicine Commission on the future of cystic fibrosis care was established at a time of great change in the clinical care of people with the disease, with a growing population of adult patients, widespread genetic testing supporting the diagnosis of cystic fibrosis, and the development of therapies targeting defects in the cystic fibrosis transmembrane conductance regulator (CFTR), which are likely to affect the natural trajectory of the disease. The aim of the Commission was to bring to the attention of patients, health-care professionals, researchers, funders, service providers, and policy makers the various challenges associated with the changing landscape of cystic fibrosis care and the opportunities available for progress, providing a blueprint for the future of cystic fibrosis care. The discovery of the CFTR gene in the late 1980s triggered a surge of basic research that enhanced understanding of the pathophysiology and the genotype-phenotype relationships of this clinically variable disease. Until recently, available treatments could only control symptoms and restrict the complications of cystic fibrosis, but advances in CFTR modulator therapies to address the basic defect of cystic fibrosis have been remarkable and the field is evolving rapidly. However, CFTR modulators approved for use to date are highly expensive, which has prompted questions about the affordability of new treatments and served to emphasise the considerable gap in health outcomes for patients with cystic fibrosis between high-income countries, and low-income and middle-income countries (LMICs). Advances in clinical care have been multifaceted and include earlier diagnosis through the implementation of newborn screening programmes, formalised airway clearance therapy, and reduced malnutrition through the use of effective pancreatic enzyme replacement and a high-energy, high-protein diet. Centre-based care has become the norm in high-income countries, allowing patients to benefit from the skills of expert members of multidisciplinary teams. Pharmacological interventions to address respiratory manifestations now include drugs that target airway mucus and airway surface liquid hydration, and antimicrobial therapies such as antibiotic eradication treatment in early-stage infections and protocols for maintenance therapy of chronic infections. Despite the recent breakthrough with CFTR modulators for cystic fibrosis, the development of novel mucolytic, anti-inflammatory, and anti-infective therapies is likely to remain important, especially for patients with more advanced stages of lung disease. As the median age of patients with cystic fibrosis increases, with a rapid increase in the population of adults living with the disease, complications of cystic fibrosis are becoming increasingly common. Steps need to be taken to ensure that enough highly qualified professionals are present in cystic fibrosis centres to meet the needs of ageing patients, and new technologies need to be adopted to support communication between patients and health-care providers.
In considering the future of cystic fibrosis care, the Commission focused on five key areas, which are discussed in this report: the changing epidemiology of cystic fibrosis (section 1); future challenges of clinical care and its delivery (section 2); the building of cystic fibrosis care globally (section 3); novel therapeutics (section 4); and patient engagement (section 5). In panel 1, they summarise key messages of the Commission. The challenges faced by all stakeholders in building and developing cystic fibrosis care globally are substantial, but many opportunities exist for improved care and health outcomes for patients in countries with established cystic fibrosis care programmes, and in LMICs where integrated multidisciplinary care is not available and resources are lacking at present. A concerted effort is needed to ensure that all patients with cystic fibrosis have access to high-quality health care in the future.
– This is a quite awesome overview of the present situation and future for people with cystic fibrosis. The paper runs to 60 pages with 521 references. Scott Bell and Felix Ratjen coordinated the Commission and reviewed and edited all sections of the paper; also they coauthored the Executive Summary. They are to be congratulated on the result.
Burgel PR, Munck A, Durieu I, Chiron R, Mely L, Prevotat A, Murris-Espin M, Porzio M, Abely M, Reix P, Marguet C, Macey J, Sermet-Gaudelus, Corvol H, Bui S, Lemonnier L, Dehilotte C, Da Silva J, Paillasseur JL, Hubert D; French Cystic Fibrosis Reference Network study group.Real-Life Safety and Effectiveness of Lumacaftor-Ivacaftor in Patients with Cystic Fibrosis.Am J Respir Crit Care Med. 2019 Oct 11. doi: 10.1164/rccm.201906-1227OC. [Epub ahead of print] [Pubmed]

Pierre Regis Burgel
A study to evaluate the safety and effectiveness of lumacaftor-ivacaftor in adolescents (≥12 years) and adults (≥18 years) in a real-life post-approval setting. Among the 845 patients (292 adolescents, 553 adults) who initiated lumacaftor-ivacaftor, 18.2% (154 patients) discontinued treatment due to respiratory (48.1%, 74 patients) or non-respiratory (27.9%, 43 patients) adverse events. In multivariable logistic regression, factors associated with increased rates of discontinuation included adult age group, percent predicted forced expiratory volume in 1 sec (ppFEV1)<40% and numbers of intravenous antibiotic courses during the year prior to lumacaftor-ivacaftor initiation.Dr Pierre-Régis Burgel currently works at the Faculty of Medicine, Paris Descartes, CPSC. He does research in Pulmonology and Cell Biology.
Patients with continuous exposure to lumacaftor-ivacaftor showed an absolute increase in ppFEV1 (+3.67%), an increase in body mass index (+0.73 kg/m2), and a decrease in intravenous antibiotic courses by 35%. Patients who discontinued treatment had significant decrease in ppFEV1, without improvement in BMI or decrease in intravenous antibiotic courses.
The authors concluded treatment with Lumacaftor-ivacaftor was associated with improvement in lung disease and nutritional status in patients who tolerated treatment. Adults who discontinued lumacaftor-ivacaftor, often due to adverse events, were found at high risk of clinical deterioration.
Dr Pierre-Régis Burgel currently works at the Faculty of Medicine, Paris Descartes, CPSC. He does research in Pulmonology and Cell Biology.
Chouchane I, Stremler-Lebel N, Reix P.Lumacaftor/ivacaftor initiation in two liver transplantation patients under tacrolimus and antifungal azoles. Clin Case Rep. 2019 Feb 17;7(4):616-618. doi: 10.1002/ccr3.2053. eCollection 2019 Apr. [Pubmed]
The authors report the initiation of CFTR modulator lumacaftor/ivacaftor combination (LUM/IVA) in two adolescents with cystic fibrosis who were treated with antifungal azoles (AZO) and tacrolimus (TCS) for liver transplantation. Despite multiple drug-drug interactions, maintaining therapeutic TCS levels was achievable. During the following year, LUM/IVA was well tolerated, providing clinical benefits.
From Service de pédiatrie, Hôpital Mère Enfant Centre Hospitalier Universitaire, Hôpital Dupuytren Limoges France.
Christian F, Thierman A, Shirley E, Allen K, Cross C, Jones K.Sustained Glycemic Control With Ivacaftor in Cystic Fibrosis-Related Diabetes.Author information. J Investig Med High Impact Case Rep. 2019 Jan-Dec;7:2324709619842898. doi: 10.1177/2324709619842898. Full article available on Journal website [Pubmed]

Francis Christian
Recent small studies have shown improvement in endogenous insulin secretion with a short period of ivacaftor therapy in primarily pediatric patients with cystic fibrosis transmembrane conductance regulator mutations amenable to potentiation. In this article, the authors present the case of a 34 year old adult who had CFRD from the age of 20 years who developed sustained improvement in glycemic control after initiation of ivacaftor; also stabilisation of a declining FEV1.
Dr Francis Christian from the University of Oklahoma Health Sciences Center, Oklahoma City, OK, USA.
John Paul Clancy, Calvin U Cotton, Scott H Donaldson, George M Solomon, Donald R VanDevanter, et al. CFTR modulator theratyping: Current status, gaps and future directions. J Cyst Fibros 2019 Jan;18(1):22-34.doi: 10.1016/j.jcf.2018.05.004. Epub 2018 Jun 20. Free PMC article [Pubmed]

John Clancy
Background: New drugs that improve the function of the cystic fibrosis transmembrane conductance regulator (CFTR) protein with discreet disease-causing variants have been successfully developed for cystic fibrosis (CF) patients. Preclinical model systems have played a critical role in this process, and have the potential to inform researchers and CF healthcare providers regarding the nature of defects in rare CFTR variants, and to potentially support use of modulator therapies in new populations.
Methods: The Cystic Fibrosis Foundation (CFF) assembled a workshop of international experts to discuss the use of preclinical model systems to examine the nature of CF-causing variants in CFTR and the role of in vitro CFTR modulator testing to inform in vivo modulator use. The theme of the workshop was centered on CFTR theratyping, a term that encompasses the use of CFTR modulators to define defects in CFTR in vitro, with application to both common and rare CFTR variants.
Results: Several preclinical model systems were identified in various stages of maturity, ranging from the expression of CFTR variant cDNA in stable cell lines to examination of cells derived from CF patients, including the gastrointestinal tract, the respiratory tree, and the blood. Common themes included the ongoing need for standardization, validation, and defining the predictive capacity of data derived from model systems to estimate clinical outcomes from modulator-treated CF patients.
Conclusions: CFTR modulator theratyping is a novel and rapidly evolving field that has the potential to identify rare CFTR variants that are responsive to approved drugs or drugs in development.
Davies JC, Drevinek P, Elborn JS, Kerem E, Lee T; European CF Society (ECFS) Strategic Planning Task Force on ‘Speeding up access to new 4 drugs for CF’.Speeding up access to new drugs for CF: Considerations for clinical trial design and delivery.J Cyst Fibros. 2019 Jul 11. pii: S1569-1993(19)30815-X. doi: 10.1016/j.jcf.2019.06.011. [Epub ahead of print]. [Pubmed]

Jane Davies
The last decade has witnessed developments in the CF drug pipeline which are both exciting and unprecedented, bringing with them previously unconsidered challenges. The Task Force group was brought together to consider these challenges and possible strategies to address them. Over the last 18 months, we have discussed internally and gathered views from a broad range of individuals representing patient organisations, clinical and research teams, the pharmaceutical industry and regulatory agencies. In this and the accompanying article, we discuss two main areas of focus: i) optimising trial design and delivery for speed and efficiency; ii) drug development for patients with rare CFTR mutations. We propose some strategies to tackle the challenges ahead and highlight areas where further thought is needed. We see this as the start of a process rather than the end and hope herewith to engage the wider community in seeking solutions to improved treatments for all patients with CF
De Jong E, Garratt LW, Looi K, Lee AHY, Ling KM, Smith ML, Falsafi R, Sutanto EN, Hillas J, Iosifidis T, Martinovich KM, Shaw NC, Montgomery ST, Kicic-Starcevich E, Lannigan FJ, Vijayasekaran S, Hancock REW, Stick SM, Kicic A; WAERP, Arest CF. Ivacaftor or lumacaftor/ivacaftor treatment does not alter the core CF airway epithelial gene response to rhinovirus. J Cyst Fibros. 2020 Jul 17:S1569-1993(20)30796-7. doi: 10.1016/j.jcf.2020.07.004. Online ahead of print. [Pubmed]

Emma De Jong
Background: Aberrant responses by the cystic fibrosis airway epithelium during viral infection may underly the clinical observations. Whether CFTR modulators affect antiviral responses by CF epithelia is presently unknown. We tested the hypothesis that treatment of CF epithelial cells with ivacaftor (Iva) or ivacaftor/lumacaftor (Iva/Lum) would improve control of rhinovirus infection.
Methods: Nineteen CF epithelial cultures (10 homozygous for p.Phe508del as CFTR Class 2, 9 p.Phe508del/p.Gly551Asp as Class 3) were infected with rhinovirus 1B at multiplicity of infection 12 for 24 h. Culture RNA and supernatants were harvested to assess gene and protein expression respectively.
Results: RNA-seq analysis comparing rhinovirus infected cultures to control identified 796 and 629 differentially expressed genes for Class 2 and Class 3, respectively. This gene response was highly conserved when cells were treated with CFTR modulators and were predicted to be driven by the same interferon-pathway transcriptional regulators (IFNA, IFNL1, IFNG, IRF7, STAT1). Direct comparisons between treated and untreated infected cultures did not yield any differentially expressed genes for Class 3 and only 68 genes for Class 2. Changes were predominantly related to regulators of lipid metabolism and inflammation, aspects of epithelial biology known to be dysregulated in CF. In addition, CFTR modulators did not affect viral copy number, or levels of pro-inflammatory cytokines produced post-infection.
Conclusions: Though long-term clinical data is not yet available, results presented here suggest that first generation CFTR modulators do not interfere with core airway epithelial responses to rhinovirus infection. Future work should investigate the latest triple modulation therapies
Emma de Jong is at Senior Research Officer at the Telethon Kids Institute Respiratory Research Centre, Nedlands, 6009, Western Australia, Australia.
Frost FJ, Nazareth DS, Charman SC, Winstanley C, Walshaw MJ. Ivacaftor Is Associated with Reduced Lung Infection by Key Cystic Fibrosis Pathogens: A Cohort Study Using National Registry Data. Ann Am Thorac Soc. 2019 Jul 19. doi: 10.1513/AnnalsATS.201902-122OC. [Epub ahead of print] [Pubmed] Retrospective cohort study utilising data from the United Kingdom CF Registry 2011-2016. Primary outcome was the annual prevalence ratios for key CF pathogens between ivacaftor users and their contemporaneous comparators. Multivariate log-binomial regression models were designed to adjust for confounders. Changes in Pseudomonas aeruginosa status were compared between groups using non-parametric maximum likelihood estimate for the purposes of Kaplan-Meier approximation.
Ivacaftor use was associated with early and sustained reduction in P. aeruginosa rates (2016 Adjusted Prevalence Ratio [95% CI] 0.68 [0.58, 0.79], p<0.001) via a combination of increased clearance in those with infection (Ivacaftor: 33/87 [37.9%] vs. Non ivacaftor: 432/1872 [22.8%], p<0.001) and reduced acquisition in those without infection (33/134 [24.6%] vs. 1157/2382 [48.6%], p=0.01). The improved prevalence of P. aeruginosa infection was independent of reduced sampling in the ivacaftor cohort. Ivacaftor was also associated with reduced prevalence of Staphylococcus aureus and Aspergillus spp. but not Burkholderia cepacia complex.
The authors concluded that in this study, long-term ivacaftor use was associated with reduced infection with important CF pathogens including P. aeruginosa. These findings have implications for antibiotic stewardship and the need for on-going chronic antimicrobial therapy in this cohort.
– Expected results confirmed with UK CF Registry data.
- Martin Walshaw
- Craig Winstaley
- Susan Charman
- Dilip Nazareth
- Freddy frost
Dr Freddy Frost is an MD student at the Institute of Infection and Global Health, Liverpool.
Dr Dilip Nazareth is Consultant Pulmonologist, Liverpool.
Dr Susan Charman is Senior Statistician at the UK Cystic Fibrosis Trust Registry. Professor Graig Winstanley is Professor of Clinical Infection, Microbiology and Immunology, Liverpool. Professor Martin Walshaw is pulmonologist and Director (and founder) of the Regional Liverpool Adult CF Centre
Garg V, Shen J, Li C, Agarwal S, Gebre A, Robertson S, Huang J, Han L, Jiang L, Stephan K, Wang LT, Lekstrom-Himes J.Pharmacokinetic and Drug-Drug Interaction Profiles of the Combination of Tezacaftor/Ivacaftor.Clin Transl Sci. 2019 Jan 29. doi: 10.1111/cts.12610. [Epub ahead of print] [Pubmed]
Drug-drug interaction (DDI) studies are described for tezacaftor/ivacaftor, a new cystic fibrosis transmembrane conductance regulator modulator therapy for the treatment of cystic fibrosis. Three phase I DDI studies were conducted in healthy subjects to characterize the DDI profile of tezacaftor/ivacaftor with cytochrome P450 (CYP)3A substrates, CYP3A inhibitors, and a permeability glycoprotein (P-gp) substrate. The effects of steady-state tezacaftor/ivacaftor on the pharmacokinetics (PKs) of digoxin (a P-gp substrate), midazolam, and ethinyl estradiol/norethindrone (CYP3A substrates) were evaluated. Effects of strong (itraconazole) and moderate (ciprofloxacin) CYP3A inhibitors on tezacaftor/ivacaftor PKs were also determined. Tezacaftor/ivacaftor increased digoxin area under the curve (AUC) by 30% but did not affect midazolam, ethinyl estradiol, or norethindrone exposures. Itraconazole increased the AUC of tezacaftor 4-fold and ivacaftor 15.6-fold. Ciprofloxacin had no significant effect on tezacaftor or ivacaftor exposure. Coadministration of tezacaftor/ivacaftor may increase exposure of sensitive P-gp substrates. Tezacaftor/ivacaftor is unlikely to impact exposure of drugs metabolized by CYP3A, including hormonal contraceptives. Strong CYP3A inhibitors significantly increase the exposures of tezacaftor and ivacaftor.
– An important paper from Vertex
Ferrera L, Baroni D, Moran O. Lumacaftor-rescued F508del-CFTR has a modified bicarbonate permeability.J Cyst Fibros. 2019 Feb 6. pii: S1569-1993(18)30927-5. doi: 10.1016/j.jcf.2019.01.012. [Epub ahead of print] [Pubmed]

Loretta Ferrera
Deletion of phenylalanine at position 508, F508del, the most frequent mutation among Cystic fibrosis (CF) patients, destabilizes the protein, thus causing both a folding and a trafficking defect, resulting in a dramatic reduction in expression of CFTR. In vitro treatment with lumacaftor produces an enhancement of anion transport in cells. We studied the permeability properties of the CFTR mutant F508del treated with the corrector lumacaftor, showing that the rescued protein has selectivity properties different than the wild type CFTR, showing an augmented bicarbonate permeability. This difference would indicate a diverse conformation of the rescued F508del-CFTR, that is plausibly reflected on an improper regulation of the airway surface liquid, lessening the efficacy of the corrector. Our findings rather support the idea that a combination of correctors would be required to address the CFTR-dependent bicarbonate permeability.
Loretta Ferrera is at the Istituto Giannina Gaslini, U.O.C. Genetica Medica, Genova, Italy.
The authors suggest these findings indicate that early CF lung disease is characterized by an increased mucus burden and inflammatory markers without infection or structural lung disease and suggest that mucolytic and anti-inflammatory agents should be explored as preventive therapy.
– An interesting combined contribution to the increasing work to understand early lung changes in CF .
Charles R Esther Jr of the Division of Paediatric Pulmonology and Marsico Lung Institute, University of N. Carolina
Garbuzenko OB, Bah N, Kuzmov A, Pogrebnyak N, Pozharov V, Minko T.Inhalation treatment of cystic fibrosis with lumacaftor and ivacaftor co-delivered by nanostructured lipid carriers. J Control Release. 2019 Jan 21;296:225-231. doi: 10.1016/j.jconrel.2019.01.025. [Epub ahead of print] [Pubmed]
-

Olga Garbuzenko
- Based on their extensive experience in inhalation delivering of drugs by different nanocarriers, the authors selected nanostructured lipid carriers (NLC) for the delivery both drugs directly to the lungs by inhalation and tested NLC loaded with drugs in vitro (normal and CF human bronchial epithelial cells) and in vivo (homozygote/homozygote bi-transgenic mice with CF). The results show that the designed NLCs demonstrated a high drug loading efficiency and were internalized in the cytoplasm of CF cells. It was found that NLC-loaded drugs were able to restore the expression and function of CFTR protein. As a result, the combination of lumacaftor and ivacaftor delivered by lipid nanoparticles directly into the lungs was highly effective in treating lung manifestations of cystic fibrosis
Gifford AH, Mayer-Hamblett N, Pearson K, Nichols DP.Answering the call to address cystic fibrosis treatment burden in the era of highly effective CFTR modulator therapy.J Cyst Fibros. 2019 Nov 21. pii: S1569-1993(19)30971-3. doi: 10.1016/j.jcf.2019.11.007. [Epub ahead of print] [PubMed]

Alex H Gifford
The authors recognise an unprecedented opportunity to study the effects of withdrawing one or more chronic treatments in people with CF (PwCF) who benefit greatly from CFTR modulator therapy, but feasibility and acceptance of such a study within the community is unknown. They surveyed PwCF, their families, and their acquaintances between November 16, 2018, and December 2, 2018, and CF clinicians between December 19, 2018, and January 2, 2019, about treatment withdrawal research. They sought feedback from these groups about their level of interest in this research, the consistency with which they were taking modulator and non-modulator treatments, the ways in which they conceptualized health changes, and what chronic non-modulator treatments they were most interested in stopping. We also asked for stakeholder perspectives on the design of a treatment withdrawal trial, but we intend to report these perspectives elsewhere.
Eighty percent (541/675) of CF community respondents and 95% (206/218) of CF clinicians said that a trial of treatment simplification should be performed in the context of highly effective modulator therapy. Most current CFTR modulator users (292/359, 81%) have not stopped another chronic treatment. Worsening lung function by spirometry or increased daily symptoms were important health indicators. PwCF, their families, and/or their acquaintances ranked airway clearance techniques and inhaled antibiotics as the most burdensome treatments.
There is considerable support among the CF community and CF clinicians in the U.S. for controlled trials to assess the safety and impact of treatment simplification in patients taking highly effective modulator therapy.Alex H Gifford is Associate Professor of `Medicine and Director of the Adult Cystic Fibrosis program at Dartmouth-Hitchcock Medical Center, NH, Lebanon, USA; The Dartmouth Institute for Health Policy and Clinical Practice, NH, Lebanon, USA.
– This is an interesting time and it is timely to discuss treatment withdrawl which will require considerable thoughtand individual variation. PwCF who have already passed the “point of no return” and whose lungs have now entered a slow but relentless deterioration due chronic infection and established damaging inflammation irrespective of CFTR activity will be less likely to be appropriate for stopping some conventional treatments. Further experience is awaited with interest
Guimbellot J, Solomon GM, Baines A, Heltshe SL, VanDalfsen J, Joseloff E, Sagel SD, Rowe SM; GOALe(2) Investigators. Effectiveness of ivacaftor in cystic fibrosis patients with non-G551D gating mutations. J Cyst Fibros. 2019 Jan;18(1):102-109. doi: 10.1016/j.jcf.2018.04.004. Epub 2018 Apr 21. [Pubmed]
-

Jennifer Guimbellot
- Patients with non-G551D gating mutations were recruited to an open-label study evaluating ivacaftor. Primary outcomes included: lung function, sweat chloride, weight gain, and quality of life scores. Twenty-one subjects were enrolled and completed 6 months follow-up on ivacaftor; mean age was 25.6 years with 52% <18. Baseline ppFEV1 was 68% and mean sweat chloride 89.6 mEq/L. Participants experienced significant improvements in ppFEV1 (mean absolute increase of 10.9% 95% CI = [2.6,19.3], p = 0.0134), sweat chloride (-48.6 95% CI = [-67.4,-29.9], p < 0.0001), and weight (5.1 kg, 95% CI = [2.8, 7.3], p = 0.0002).
The authors concluded patients with non-G551D gating mutations experienced improved lung function, nutritional status, and quality of life. This study supports ongoing use of ivacaftor for patients with these mutations.
Dr Jennifer Guimbellot is a paediatric pulmonologist at the Gregory Fleming James Cystic Fibrosis Research Center, University of Alabama at Birmingham (UAB), Birmingham, AL, USA; Department of Pediatrics, Division of Pulmonary and Sleep Medicine, UAB, Birmingham, AL, USA
Hamilton JL, Zobell JT, Robson J. Pancreatic insufficiency converted to pancreatic sufficiency with ivacaftor. Pediatr Pulmonol. 2019 Jul 21. doi: 10.1002/ppul.24454. [Epub ahead of print] [Pubmed]

Jennifer Hamilton
A six‐year‐old female with cystic fibrosis (CF), genotype Phe508del/G551D, who we follow at our pediatric CF Center. Shortly after her CF diagnosis (through newborn screening), her fecal elastase was noted to be 83 µg/g (normal range >201 µg/g), and she was started on pancreatic enzyme replacement therapy (PERT). This child was started on ivacaftor at 2 years of age, as soon as it was approved by the United States Food and Drug Administration and commercially available for her age and mutations.
She had recurrent bouts of periumbilical abdominal pain extensively investigated with essentially negative findings. Since the serum lipase was mildly elevated and abdominal pain was continuing, a decision was made to investigate exocrine pancreatic function with fecal elastase‐1 testing. The patient’s fecal elastase was shown to have normalized (465 µg/g) at that check and 2 months later it was more than 500 µg/g. On the basis of these results, PERT was discontinued. Since discontinuing PERT, she has had no signs or symptoms of malabsorption. Her abdominal pain eventually improved, with clear precipitating source never identified, and we are monitoring her for recurrence of pancreatitis.
Jennifer Hamilton is at the College of Nursing, University of Utah Health Sciences, and the Paediatric Pulmonary and Sleep Medicine Division of the University of Uta
Harris JK, Wagner BD, Zemanick ET, Robertson CE, Stevens MJ, Heltshe SL, Rowe SM, Sagel SD4; GOAL Investigators of the Cystic Fibrosis Foundation Therapeutics Development Network.Changes in Airway Microbiome and Inflammation with Ivacaftor Treatment in Patients with Cystic Fibrosis and the G551D Mutation.Ann Am Thorac Soc. 2019 Oct 11. doi: 10.1513/AnnalsATS.201907-493OC. [Epub ahead of print][Pubmed]
Modulation of the cystic fibrosis transmembrane conductance regulator (CFTR) protein improves clinical outcomes in patients with cystic fibrosis (CF) and specific CFTR genetic mutations. It remains unclear how improving CFTR function modifies existing airway infection and inflammation. A study to compare sputum microbiome and markers of inflammation before and after 6 months of ivacaftor treatmentThe cohort that spontaneously expectorated sputum had a lower FEV1, higher proportion with Pseudomonas aeruginosa infection,In this multicenter cohort, six months of ivacaftor treatment were not associated with significant changes in airway microbial communities or measures of inflammation.
These data suggest that concomitant antimicrobial and anti-inflammatory treatments will still be needed to manage airway disease in CF patients treated with highly effective CFTR modulator therapy, especially in older patients with more advanced disease.
Dr J K Harris is from the University of Colorado, Pediatrics, Aurora, Colorado, United States
Heijerman HGM, McKone EF, Downey DG, Van Braeckel E, Rowe SM, Tullis EMall MA, Welter JJ, Ramsey BW, McKee CM, Marigowda G, Moskowitz SM, Waltz D, Sosnay PR, Simard C, Ahluwalia N, Xuan F, Zhang Y, Taylor-Cousar JL, McCoy KS; VX17-445-103 Trial Group.Efficacy and safety of the elexacaftor plus tezacaftor plus ivacaftor combination regimen in people with cystic fibrosis homozygous for the F508del mutation: a double-blind, randomised, phase 3 trial. Collaborators (45).Lancet. 2019 Oct 30. pii: S0140-6736(19)32597-8. doi: 10.1016/S0140-6736(19)32597-8. [Epub ahead of print] Full copy available [Pubmed]

Harry Heijerman
Cystic fibrosis transmembrane conductance regulator (CFTR) modulators correct the basic defect caused by CFTR mutations. Improvements in health outcomes have been achieved with the combination of a CFTR corrector and potentiator in people with cystic fibrosis homozygous for the F508del mutation. The addition of elexacaftor (VX-445), a next-generation CFTR corrector, to tezacaftor plus ivacaftor further improved F508del-CFTR function and clinical outcomes in a phase 2 study in people with cystic fibrosis homozygous for the F508del mutation.
This phase 3, multicentre, randomised, double-blind, active-controlled trial of elexacaftor in combination with tezacaftor plus ivacaftor was done at 44 sites in four countries. Eligible participants were those with cystic fibrosis homozygous for the F508del mutation, aged 12 years or olderwith stable disease, and with a percentage predicted forced expiratory volume in 1 s (ppFEV1) of 40-90%, inclusive. After a 4-week tezacaftor plus ivacaftor run-in period, participants were randomly assigned (1:1) to 4 weeks of elexacaftor 200 mg orally once daily plus tezacaftor 100 mg orally once daily plus ivacaftor 150 mg orally every 12 h versus tezacaftor 100 mg orally once daily plus ivacaftor 150 mg orally every 12 h alone. The primary outcome was the absolute change from baseline (measured at the end of the tezacaftor plus ivacaftor run-in) in ppFEV1 at week 4. Key secondary outcomes were absolute change in sweat chloride and Cystic Fibrosis Questionnaire-Revised respiratory domain (CFQ-R RD) score. This study is registered with ClinicalTrials.gov, NCT03525548.
Between Aug 3 and Dec 28, 2018, 113 participants were enrolled. Following the run-in, 107 participants were randomly assigned (55 in the elexacaftor plus tezacaftor plus ivacaftor group and 52 in the tezacaftor plus ivacaftor group) and completed the 4-week treatment period. The elexacaftor plus tezacaftor plus ivacaftor group had improvements in the primary outcome of ppFEV1 (least squares mean [LSM] treatment difference of 10·0 percentage points [95% CI 7·4 to 12·6], p<0·0001) and the key secondary outcomes of sweat chloride concentration (LSM treatment difference -45·1 mmol/L [95% CI -50·1 to -40·1], p<0·0001), and CFQ-R RD score (LSM treatment difference 17·4 points [95% CI 11·8 to 23·0], p<0·0001) compared with the tezacaftor plus ivacaftor group. The triple combination regimen was well tolerated, with no discontinuations. Most adverse events were mild or moderate; serious adverse events occurred in two (4%) participants receiving elexacaftor plus tezacaftor plus ivacaftor and in one (2%) receiving tezacaftor plus ivacaftor.
The authors concluded Elexacaftor plus tezacaftor plus ivacaftor provided clinically robust benefit compared with tezacaftor plus ivacaftor alone, with a favourable safety profile, and shows the potential to lead to transformative improvements in the lives of people with cystic fibrosis who are homozygous for the F508del mutation.
Dr Harry Heijerman is at the Department of Pulmonology, University Medical Center Utrecht, Utrecht, Netherlands.
De la Hoz D, Villamil Osorio M, Restrepo-Gualteros SM.Cystic fibrosis transmembrane conductance regulator modulators: Present and future in cystic fibrosis treatment. A review. Arch Argent Pediatr. 2019 Apr 1;117(2):e131-e136. doi: 10.5546/aap.2019.eng.e131. Free full text [Pubmed]
Cystic fibrosis transmembrane conductance regulator (CFTR) modulators are the present and future of drug management for patients with cystic fibrosis. The objective of this article is to review this therapeutic option. Scientific articles were reviewed by searching the MedLine database, which is available through the Cystic Fibrosis Foundation’s official website, from 2009 to 2018, in English. Twelve articles about the current status of research in CFTR modulators were selected without restrictions regarding the type of study. To date, the United States Food and Drug Administration has approved three modulators: ivacaftor, lumacaftor + ivacaftor, and tezacaftor + ivacaftor, while other 11 drugs are being studied in different investigation phases. CFTR modulator therapy is a developing reality aimed at the highest goal of personalized medicine and promises to improve the quality of life of cystic fibrosis patients.
From Universidad Nacional de Colombia, Departamento de Pediatría, Bogotá DC, Colombia. dcdeg@unal.edu.co.
– The full text is a very readable summary of the major facts and leading references regarding CFTR modulators.The first author’s previous publications appear to have concerned various aspects of acetylcholinesterase.
Joshi D, Ehrhardt A, Hong JS, Sorscher EJ.Cystic fibrosis precision therapeutics: Emerging considerations.Pediatr Pulmonol. 2019 Nov;54 Suppl 3:S13-S17. doi: 10.1002/ppul.24547. [Pubmed] Small molecules that address fundamental defects underlying cystic fibrosis (CF), including modulators such as the approved drugs ivacaftor, lumacaftor, tezacaftor, and elexacaftor, have advanced dramatically over the past few years and are transforming care and prognosis among individuals with this disease. The new treatment strategies are predicated on established scientific insight concerning pathogenesis, and applying “personalized” or “precision” interventions for specific abnormalities of the cystic fibrosis transmembrane conductance regulator (CFTR). Even with the advent of highly effective triple drug combinations-which hold great promise for the majority of patients with CF worldwide-barriers to precision therapy remain. These include refractory CFTR variants (premature truncation codons, splice defects, large indels, severe missense mutations, and others) not addressed by available modulators, and access to leading-edge therapeutic compounds for patients with ultrarare forms of CF. In addition to describing the remarkable progress that has occurred regarding CF precision medicine, this review outlines some of the remaining challenges. The CF experience is emblematic of many conditions for which personalized interventions are actively being sought.
From the Department of Pediatrics, Emory University School of Medicine and Children’s Healthcare of Atlanta, Atlanta, Georgia.
Kelly A, De Leon DD, Sheikh S, Camburn D, Kubrak C, Peleckis AJ, Stefanovski D, Hadjiliadis D, Rickels MR, Rubenstein RC. Islet Hormone and Incretin Secretion in Cystic Fibrosis after Four Months of Ivacaftor Therapy.
Am J Respir Crit Care Med.2019 Feb 1;199(3):342-351. doi: 10.1164/rccm.201806-1018OC. [Pubmed]
-

Andrea Kelly
- Diabetes is associated with worse cystic fibrosis (CF) outcomes. The CFTR potentiator ivacaftor is suggested to improve glucose homeostasis in individuals with CF. To test the hypothesis that clinically indicated ivacaftor would be associated with improvements in glucose tolerance and insulin and incretin secretion.
Oral glucose tolerance tests, mixed-meal tolerance tests, and glucose-potentiated arginine tests were compared pre-ivacaftor initiation and 16 weeks post-ivacaftor initiation in CF participants with at least one CFTR gating or conductance mutation. Meal-related 30-minute (early phase) and 180-minute incremental area under the curves were calculated as responses for glucose, insulin, C-peptide, and incretin hormones; glucagon-like peptide-1; and glucose-dependent insulinotropic polypeptide. First-phase insulin secretion, glucose potentiation of arginine-induced insulin secretion, and disposition index were characterized by glucose-potentiated arginine stimulation tests.
Twelve subjects completed the study: six male/six female; seven normal/five abnormal glucose tolerance (oral glucose tolerance test 1-h glucose ≥155 and 2-h glucose <200 mg/dl); of median (minimum-maximum) age (13.8 yr [6.0-42.0]), body mass index-Z of 0.66 (-2.4 to 1.9), and FEV1% predicted of 102 (39-122). Glucose tolerance normalized in one abnormal glucose tolerance subject. Ivacaftor treatment did not alter meal responses except for an increase in early phase C-peptide (P = 0.04). First-phase (P = 0.001) and glucose potentiation of arginine-induced (P = 0.027) insulin secretion assessed by acute C-peptide responses improved after ivacaftor treatment. Consistent with an effect on β-cell function, the disposition index relating the amount of insulin secreted for insulin sensitivity also improved (P = 0.04).
The authors concluded insulin secretion improved following 4 months of clinically indicated ivacaftor therapy in this relatively young group of patients with CF with normal to mildly impaired glucose tolerance, whereas incretin secretion remained unchanged.
Dr Andrea Kellyis attending physician in the Division of Endocrinology and Diabetes and Division of Pulmonary Medicine and Cystic Fibrosis Center, Department of Pediatrics, Children’s Hospital of Philadelphia, Philadelphia, Pennsylvania.
Kerem E, Oren YS, Kerem B. Take it personally: how personal we reach when we are so different from each other? J Cyst Fibros. 2019 Jan;18(1):6-7. doi: 10.1016/j.jcf.2018.12.009. [Pubmed]
-

Eitan Kerem

Batsheva Kerem
Discussing the variable response to Kalydeco and Orkambi among patients carrying the same genotype was shown the authors note that since these drugs are extremely expensive, it could be argued that only patients that show clinical benefit should take them. Therefore, in-vitro cellular models and genetic tools are needed to predict patient-specific clinical outcomes.
The authors discuss three papers in the present issue of JCF (below) that describe cellular systems that can be or are already used to predict response to therapy in vivo. They note that more studies are needed to correlate the response in the different in vitro systems to clinical response, since other genes, most of them unknown yet, can modify the response in vivo. The SLC29A6 gene was suggested to modify response to Kalydeco by modulating the airway response to CFTR directed therapies. The cost of the CFTR modifier therapies, and the possible need to take several in combination in order to achieve full CFTR correction of function, emphasizes the need for various, complementary cellular systems and clinical data that may together enlarge the basis for predicting CFTR drug response in a patient-specific manner.
– Clancy, J.P., Cotton, C.U., Donaldson, S.H., Solomon, G.M., VanDevanter, D.R., Boyle, M.P. et al. CFTR modulator theratyping: Current status, gaps and future directions. J Cyst Fibros. 2019; 18: 22–34. [Pubmed]
– Eckford, P.D.W., McCormack, J., Munsie, L., He, G., Stanojevic, S., Pereira, S.L. et al. The CF Canada-Sick Kids Program in individual CF therapy: A resource for the advancement of personalized medicine in CF. J Cyst Fibros. 2019; 18: 32–40. [Pubmed]
– Jennings, S., Ng, H.P., and Wang, G. Establishment of a ΔF508-CF promyelocytic cell line for cystic fibrosis research and drug screening. J Cyst Fibros. 2019; 18: 41–50. [Pubmed]
Kim J, Davies Z, Dunn C, Wine JJ, Milla C. Ivacaftor restores CFTR-dependent sweat gland fluid secretion in cystic fibrosis subjects with S945L alleles. J Cyst Fibros. 2018 Mar;17(2):179-185. doi: 10.1016/j.jcf.2017.12.005. Epub 2017 Dec 24.[Pubmed]
A study to determine in vivo effects of CFTR modulators on mutation S945L. The authors measured effects of CFTR modulators on CFTR-dependent sweating (‘C-sweat’) in two pancreatic sufficient cystic fibrosis (CF) subjects. S1 (S945L/G542X) took ivacaftor and S2 (S945L/F508del) took ivacaftor+tezacaftor. Sweating was stimulated pharmacologically to produce sequentially both CFTR-independent (methacholine stimulated) M-sweat and C-sweat; and the ratio of these was compared. Sweat secretion was measured with two methods: real time secretory rate quantitative recording and by optically measuring the growth of sweat bubbles under oil from multiple identified glands.
Using the quantitative recorder, we saw zero C-sweat secretion off-drug, but when on-drug the C-sweat responses for both subjects were comparable to those seen in carriers. The on-drug response was further quantified using the sweat bubble method. Each subject again showed robust C-sweat responses, with C-sweat/M-sweat ratios~half of the ratio determined for a cohort of 40 controls tested under identical conditions.
The authors concluded these in vivo results, consistent with prior in vitro findings, indicate that the drug treatments restore near-normal function to S945L-CFTR, and support the use of ivacaftor as a treatment for CF patients who carry this allele.
From the Cystic Fibrosis Research Laboratory, Stanford University, Stanford, CA, USA.
Optimal care of patients with CF requires a multidisciplinary care team that includes respiratory therapists, dieticians, social workers, psychologists, pharmacists, and physicians who have expertise in the treatment of this complex, multisystem disorder.
– This is still a very important message. For example an instance many years ago involved admission of a person with CF to an ICU for a respiratory indication. Omission of the pancreatic enzyme therapy led to meconium ileus equivalent intestinal obstruction, subsequent treatment of this complication proved fatal. A CF expert should be part of the ICU team.
Kirwan L, Fletcher G, Harrington M, Jeleniewska P, Zhou S, Casserly B, Gallagher CG, Greally P, Gunaratnam C, Herzig M, Linnane B, McElvaney NG, McKone EF, McNally P, Mullane D, Ní Chróinín M, O’Mahony M, Plant BJ, Jackson AD. Longitudinal Trends in Real-World Outcomes after Initiation of Ivacaftor. A Cohort Study from the Cystic Fibrosis Registry of Ireland. Ann Am Thorac Soc. 2019 Feb;16(2):209-216. doi: 10.1513/AnnalsATS.201802-149OC.[Pubmed]
-

Laura Kirwan
The authors used cystic fibrosis (CF) registry data to assess outcomes after the initiation of ivacaftor, a CF transmembrane conductance regulator (CFTR) potentiator approved for the treatment of CF with a defective gating CFTR mutation. Longitudinal trends were examined using mixed-effects regression analysis in 80 ivacaftor-treated patients with CF aged 6 to 56 years registered with the CF Registry of Ireland with at least 36 months of before and after commencement data. The effects of ivacaftor treatment on forced expiratory volume in 1 second (FEV1) % predicted, body mass index (BMI), hospitalization for pulmonary exacerbation, and oral and intravenous antibiotic use were assessed.
In the 36 months after ivacaftor initiation, FEV1% predicted improved by 2.26% per annum (95% confidence interval [CI], 0.2 to 4.3) for patients aged younger than 12 years, remained unchanged for 12- to younger than 18-year-olds (95% CI, -1.9 to 2.9), and declined in adults by 1.74% per annum (95% CI, -3.1 to -0.4). BMI in adults increased 0.28 kg/m2 per annum (95% CI, 0.03 to 0.5), and there was no significant change in BMI z-score in children (95% CI, -0.01 to 0.1). In the year after ivacaftor initiation, intravenous antibiotic treatment reduced by 46% (95% CI, -62.5% to -23.3%, oral antibiotic treatment reduced by 49% (95% CI, -61.1% to -32.1%), and there was no significant reduction in hospitalization (95% CI, -59.2% to 9.7%).
In this study of real-world CF registry data, clinical outcomes improved and healthcare resource utilization decreased after commencing ivacaftor.
Dr Laura Kirwan is Research Statistician at the Cystic Fibrosis Registry of Ireland.
Kopp BT, Fitch J, Jaramillo L, Shrestha CL, Robledo-Avila F, Zhang S, Palacios S, Woodley F, Hayes D Jr, Partida-Sanchez S, Ramilo O, White P, Mejias A. Whole-blood transcriptomic responses to lumacaftor/ivacaftor therapy in cystic fibrosis.J Cyst Fibros. 2019 Aug 29. pii: S1569-1993(19)30868-9. doi: 10.1016/j.jcf.2019.08.021. [Epub ahead of print] [Pubmed]
Cystic fibrosis (CF) remains without a definitive cure. Novel therapeutics targeting the causative defect in the cystic fibrosis transmembrane conductance regulator (CFTR) gene are in clinical use. Lumacaftor/ivacaftor is a CFTR modulator approved for patients homozygous for the CFTR variant p.Phe508del, but there are wide variations in treatment responses preventing prediction of patient responses. We aimed to determine changes in gene expression related to treatment initiation and response.
Whole-blood transcriptomics was performed using RNA-Seq in 20 patients with CF pre- and 6 months post-lumacaftor/ivacaftor (drug) initiation and 20 non-CF healthy controls. Correlation of gene expression with clinical variables was performed by stratification via clinical responses.They identified 491 genes that were differentially expressed in CF patients (pre-drug) compared with non-CF controls and 36 genes when comparing pre-drug to post-drug profiles. Both pre- and post-drug CF profiles were associated with marked overexpression of inflammation-related genes and apoptosis genes, and significant under-expression of T cell and NK cell-related genes compared to non-CF. CF patients post-drug demonstrated normalized protein synthesis expression, and decreased expression of cell-death genes compared to pre-drug profiles, irrespective of clinical response. However, CF clinical responders demonstrated changes in eIF2 signaling, oxidative phosphorylation, IL-17 signaling, and mitochondrial function compared to non-responders. Top overexpressed genes (MMP9 and SOCS3) that decreased post-drug were validated by qRT-PCR. Functional assays demonstrated that CF monocytes normalized calcium (increases MMP9 expression) concentrations post-drug.
The authors concluded transcriptomics revealed differentially regulated pathways in CF patients at baseline compared to non-CF, and in clinical responders to lumacaftor/ivacaftor.
Dr Benjamin Kopp is a Paediatric Pulmonologist, Division of Pulmonary Medicine, Nationwide Children’s Hospital, Columbus, Ohi
Li A, Vigers T, Pyle L, Zemanick E, Nadeau K, Sagel SD, Chan CL. Continuous glucose monitoring in youth with cystic fibrosis treated with lumacaftor-ivacaftor. J Cyst Fibros.2019 Jan;18(1):144-149. doi: 10.1016/j.jcf.2018.07.010. Epub 2018 Aug 10. [Pubmed]
-

Christine Chan
- The effects of lumacaftor-ivacaftor therapy on glycemia have not been thoroughly investigated. Continuous glucose monitoring (CGM) provides detailed information about glycemic patterns and detects glucose abnormalities earlier than traditional screening tools for diabetes. CGM measures, HbA1c, and oral glucose tolerance test (OGTT) results were collected and within-subject results compared in F508del homozygous youth with CF before and after initiation of lumacaftor-ivacaftor using the Wilcoxon signed-rank test.
Nine youths with CF (6 males, median age 12.7 years) were enrolled. CGM was performed in all participants before (median 26 weeks) and after lumacaftor-ivacaftor (median 29 weeks). HbA1c and fasting plasma glucose increased (p = .02) after lumacaftor-ivacaftor initiation. No changes in OGTT 1 h or 2 h glucose nor CGM measures were observed overall. When analyzed by sex, males showed lower glycemic variability, as reflected by the mean amplitude of glycemic excursions, on the post-treatment CGM.
The authors concluded glycemic abnormalities persisted in CF patients treated with lumacaftor-ivacaftor, although sex-dependent differences in glycemic response to treatment may exist.
Dr A Li of University of Colorado School of Medicine, University of Colorado Anschutz medical Campus Aurora
Dr Christine Chan is a paediatric endocrinologist in Aurora Colorado
Liu F, Zhang Z, Levit A, Levring J, Touhara KK, Shoichet BK, Chen J. Structural identification of a hotspot on CFTR for potentiation. Science. 2019 Jun 21;364(6446):1184-1188. doi: 10.1126/science.aaw7611. [Pubmed]
Cystic fibrosis is a fatal disease caused by mutations in the cystic fibrosis transmembrane conductance regulator (CFTR). Two main categories of drugs are being developed: correctors that improve folding of CFTR and potentiators that recover the function of CFTR. Here, we report two cryo-electron microscopy structures of human CFTR in complex with potentiators: one with the U.S. Food and Drug Administration (FDA)-approved drug ivacaftor at 3.3-angstrom resolution and the other with an investigational drug, GLPG1837, at 3.2-angstrom resolution. These two drugs, although chemically dissimilar, bind to the same site within the transmembrane region. Mutagenesis suggests that in both cases, hydrogen bonds provided by the protein are important for drug recognition.The molecular details of how ivacaftor and GLPG1837 interact with CFTR may facilitate structure-based optimization of therapeutic compounds.
Laboratory of Membrane Biophysics and Biology, The Rockefeller University, New York, NY 10065, USA
– Further potential way to improve the function of the CFTR modulators
Lommatzsch ST, Taylor-Cousar JL.The combination of tezacaftor and ivacaftor in the treatment of patients with cystic fibrosis: clinical evidence and future prospects in cystic fibrosis therapy. Ther Adv Respir Dis. 2019 Jan-Dec;13:1753466619844424. doi: 10.1177/1753466619844424. [Pubmed]

Steve Lommatzsch
Years of tremendous study have dawned a new era for the treatment of cystic fibrosis (CF). For years CF care was rooted in the management of organ dysfunction resulting from the mal-effects of absent anion transport through the CF transmembrane regulator (CFTR) protein. CFTR, an adenosine triphosphate binding anion channel, has multiple functions, but primarily regulates the movement of chloride anions, thiocyanate and bicarbonate across luminal cell membranes. Additional roles include effects on other electrolyte channels such as the epithelial sodium channel (ENaC) and on pulmonary innate immunity. Inappropriate luminal anion movement leads to elevated sweat chloride concentrations, dehydrated airway surface liquid, overall viscous mucous production, and inspissated bile and pancreatic secretions. As a result, patients develop the well-known CF symptoms and disease-defining complications such as chronic cough, oily stools, recurrent pulmonary infections, bronchiectasis, chronic sinusitis and malnutrition. Traditionally, CF has been symptomatically managed, but over the past 6 years those with CF have been offered a new mode of therapy; CFTR protein modulation. These medications affect the basic defect in CF: abnormal CFTR function. Ivacaftor, approved for use in the United States in 2012, is the first medication in CF history to improve CFTR function at the molecular level. Its study and approval were followed by two additional CFTR modulators, lumacaftor/ivacaftor and tezacaftor/ivacaftor. To effectively use currently available CF therapies, clinicians should be familiar with the side effects of the drugs and their impacts on patient outcomes. As many new modulators are on the horizon, this information will equip providers to discuss the benefits and shortcomings of modulator therapy especially in the context of limited healthcare resources.eDr Steven E Lommatzsch is a pulmonologist at National Jewish Health, Denver
Loureiro CA, Santos JD, Matos AM, Jordan P, Matos P, Farinha CM, Pinto FR. Network Biology Identifies Novel Regulators of CFTR Trafficking and Membrane Stability. Front Pharmacol. 2019 Jun 4;10:619. doi: 10.3389/fphar.2019.00619. eCollection 20 [Pubmed] Free PMC Article
In cystic fibrosis, the most common disease-causing mutation is F508del, which causes not only intracellular retention and degradation of CFTR, but also defective channel gating and decreased membrane stability of the small amount that reaches the plasma membrane (PM). Thus, pharmacological correction of mutant CFTR requires targeting of multiple cellular defects in order to achieve clinical benefit. Although small-molecule compounds have been identified and commercialized that can correct its folding or gating, an efficient retention of F508del CFTR at the PM has not yet been explored pharmacologically despite being recognised as a crucial factor for improving functional rescue of chloride transport. In ongoing efforts to determine the CFTR interactome at the PM, we used three complementary approaches: targeting proteins binding to tyrosine-phosphorylated CFTR, protein complexes involved in cAMP-mediated CFTR stabilisation at the PM, and proteins selectively interacting at the PM with rescued F508del-CFTR but not wt-CFTR. Using co-immunoprecipitation or peptide-pull down strategies, we identified around 400 candidate proteins through sequencing of complex protein mixtures using the nano-LC Triple TOF MS technique. Key candidate proteins were validated for their robust interaction with CFTR-containing protein complexes and for their ability to modulate the amount of CFTR expressed at the cell surface of bronchial epithelial cells. Here, the authors describe how they explored the above-mentioned experimental datasets to build a protein interaction network with the aim of identifying novel pharmacological targets to rescue CFTR function in cystic fibrosis (CF) patients. They identified and validated novel candidate proteins that were essential components of the network but not detected in previous proteomic analyses.
– BioISI-Biosystems & Integrative Sciences Institute, Faculty of Sciences, University of Lisbon, Lisbon, Portugal. Multidisciplinary/Interdisciplinary Research; Life and HealthSciences; Biomedicine; Exact Sciences & Engineering; Physics; Natural Science & Environment; Bio-based Product Technology or Food Sciences . Scientific Director is Professor Margarida Amaral
Corresponding author Francisco Pinto, Department of Chemistry and Biochemistry, Faculty of Sciences, University of Lisbon, Lisbon, Portugal
Masson A, Schneider-Futschik EK, Baatallah N, Nguyen-Khoa T, Girodon E, Hatton A, Flament T, Le Bourgeois M, Chedevergne F, Bailly C, Kyrilli S, Achimastos D, Hinzpeter A, Edelman A, Sermet-Gaudelus I. Predictive factors for lumacaftor/ivacaftor clinical response.J Cyst Fibros. 2019 May;18(3):368-374. doi: 10.1016/j.jcf.2018.12.011. Epub 2018 Dec 28[Pubmed]
Ivacaftor-lumacaftor combination therapy corrects the F508 del-CFTR mutated protein which causes Cystic Fibrosis. The clinical response of the patients treated with the combination therapy is highly variable. This study aimed to determine factors involved in the individual’s response to lumacaftor-ivacaftor therapy.
Sweat test was assessed at baseline and after 6 months of ivacaftor-lumacaftor treatment in 41 homozygous F508del children and young adults. β-adrenergic peak sweat secretion, nasal potential difference (NPD) and intestinal current measurements (ICM) were performed in patients accepting these tests. Serum level of lumacaftor and ivacaftor were determined and additional CFTR variant were searched.
Results: Sweat chloride concentration significantly decreased after treatment, whereas the β-adrenergic peak sweat response did not vary in 9 patients who underwent these tests. The average level of F508del-CFTR activity rescue reached up to 15% of the normal level in intestinal epithelium, as studied by ICM in 12 patients (p = .03) and 20% of normal in the nasal epithelium in NPD tests performed in 21 patients (NS). There was no significant correlation between these changes and improvements in FEV1 at 6 months. Serum drug levels did not correlate with changes in FEV1, BMI-Z score or other CFTR activity biomarkers. Additional exonic variants were identified in 4 patients. The F87L-I1027T-F508del-CFTR complex allele abolished the lumacaftor corrector effect.
Conclusion: This observational study investigates a number of potential factors linked to the clinical response of F508del homozygous patients treated with lumacaftor-ivacaftor combination therapy. Lumacaftor and ivacaftor blood levels are not associated with the clinical response. Additional exonic variants may influence protein correction.
Alexandra Masson is at the Centre Maladie Rare Mucoviscidose, Hôpital Necker-Enfants Malades, Assistance-Publique Hôpitaux de Paris
McColley SA, Konstan MW, Ramsey BW, Stuart Elborn J, Boyle MP, Wainwright CE, Waltz D, Vera-Llonch M, Marigowda G, Jiang JG, Rubin JL. Lumacaftor/Ivacaftor reduces pulmonary exacerbations in patients irrespective of initial changes in FEV1. J Cyst Fibros. 2019 Jan;18(1):94-101. doi: 10.1016/j.jcf.2018.07.011. Epub 2018 Aug 23. Free full text [Pubmed]
Improved lung function and fewer pulmonary exacerbations (PEx) were observed with lumacaftor/ivacaftor (LUM/IVA) in patients with cystic fibrosis homozygous for F508del. It is unknown whether PEx reduction extends to patients without early lung function improvement. This was a post hoc analyses of pooled phase 3 data (NCT01807923, NCT01807949) categorized LUM/IVA-treated patients by percent predicted forced expiratory volume in 1 s (ppFEV1) change from baseline to day 15 into threshold categories (absolute change ≤0 vs >0; relative change <5% vs ≥5%) and compared PEx rates vs placebo. The LUM (400 mg q12h)/IVA (250 mg q12h)-treated patients (n = 369) experienced significantly fewer PEx vs placebo, regardless of threshold category. With LUM/IVA, PEx rate per patient per year was 0.60 for those with absolute change in ppFEV1 > 0 and 0.85 for those with absolute change ≤0 (respective rate ratios vs placebo [95% CI]: 0.53 [0.40-0.69; P < .0001], 0.74 [0.55-0.99; P = .04]).
The authors concluded LUM/IVA significantly reduced PEx, even in patients without early lung function improvement.
McCormick J, Cho DY, Lampkin B, Richman J, Hathorne H, Rowe SM, Woodworth BA. Ivacaftor improves rhinologic, psychologic, and sleep-related quality of life in G551D cystic fibrosis patients.Int Forum Allergy Rhinol. 2019 Mar;9(3):292-297. doi: 10.1002/alr.22251. Epub 2018 Nov 24 [Pubmed]
The purpose of this study is to evaluate the impact of ivacaftor on chronic rhinosinusitis (CRS) symptoms in this population.The G551D Observational (GOAL) study was a multicenter prospective cohort study enrolling CF patients ≥6 years with at least 1 G551D mutation. Subjects were provided 20-item Sino-Nasal Outcome Test (SNOT-20) questionnaires prior to ivacaftor therapy and at 1, 3, and 6 months afterward. The impact on rhinologic (R), psychological (P), sleep (S), and ear/facial (E) quality of life (QOL) domains was evaluated separately. Of 153 subjects, 129 (84%) completed all questionnaires.
Ivacaftor improves QOL in the R, P, and S domains in G551D CF patients, although QOL instruments validated for CRS may not translate well to CF CRS patients because symptom burden was surprisingly low.
Norris AW. Is Cystic Fibrosis-related Diabetes Reversible? New Data on CFTR Potentiation and Insulin Secretion.Am J Respir Crit Care Med. 2019 Feb 1;199(3):261-263. doi: 10.1164/rccm.201808-1501ED. [Pubmed]
Andrew Norris discusses the question as to whether the new molecular therapies will treat or even prevent cystic fibrosis related diabetes. In a clear detailed review of the effect of the new therapies on the treatment and even prevention CFRD. He discusses the study of Kelly et al (abstracted below) and concludes that Kelly and colleagues’s results provide hope that restoration of CFTR function might treat or even prevent CFRD, although there remains considerable uncertainty. He mentions the severity of pancreatic involvement and even the fact that pancreatic damage occurs in utero.
McNamara JJ, McColley SA, Marigowda G, Liu F3 Tian S, Owen CA, Stiles D, Li C, Waltz D, Wang LT, Sawicki GS. Safety, pharmacokinetics, and pharmacodynamics of lumacaftor and ivacaftor combination therapy in children aged 2-5 years with cystic fibrosis homozygous for F508del-CFTR: an open-label phase 3 study.Lancet Respir Med.2019 Jan 24. pii: S2213-2600(18)30460-0. doi: 10.1016/S2213-2600(18)30460-0. [Epub ahead of print] [Pubmed]
-

John MacNamara
- The efficacy, safety, and tolerability of lumacaftor and ivacaftor are established in patients aged 6 years and older with cystic fibrosis, homozygous for the F508del-CFTR mutation. We assessed the safety, pharmacokinetics, pharmacodynamics, and efficacy of lumacaftor and ivacaftor in children aged 2-5 years.
In this multicentre, phase 3, open-label, two-part study, we enrolled children aged 2-5 years, weighing at least 8 kg at enrolment, with a confirmed diagnosis of cystic fibrosis who were homozygous for the F508del-CFTR mutation. Children received lumacaftor 100 mg and ivacaftor 125 mg (bodyweight <14 kg) or lumacaftor 150 mg and ivacaftor 188 mg (bodyweight ≥14 kg) orally every 12 h for 15 days in part A (to assess pharmacokinetics and safety) and for 24 weeks in part B (to assess safety, pharmacokinetics, pharmacodynamics, and efficacy). Children could participate in part A, part B, or both. Children were enrolled into part A at five sites in the USA and into part B at 20 sites in North America (USA, 17 sites; Canada, three sites). The primary endpoints of the study were the pharmacokinetics (part A) and safety (part B) of lumacaftor and ivacaftor; all analyses were done in children who received at least one dose of lumacaftor and ivacaftor. Secondary endpoints in part A were safety and pharmacokinetics of the metabolites of lumacaftor and ivacaftor, and in part B included pharmacokinetics in children who received at least one dose of lumacaftor and ivacaftor and absolute changes from baseline in sweat chloride concentration, growth parameters, and markers of pancreatic function. This study is registered with ClinicalTrials.gov, number NCT02797132.
The study was done from May 13, 2016, to Sept 8, 2017. 12 children enrolled in part A, 11 of whom completed the 15-day treatment period and enrolled in part B. 60 children enrolled in part B, 56 of whom completed the 24-week treatment period. Safety and pharmacokinetics were consistent with the well characterised safety profile of lumacaftor and ivacaftor. In part B, most children (59 [98%] of 60 children) had one or more treatment-emergent adverse events; most events were mild to moderate in severity. The most common adverse events were cough (38 [63%] of 60), vomiting (17 [28%]), pyrexia (17 [28%]), and rhinorrhoea (15 [25%]). Serious adverse events occurred in four children: infective pulmonary exacerbation of cystic fibrosis (n=2), gastroenteritis viral (n=1), and constipation (n=1). Three (5%) of 60 children discontinued treatment because of elevated serum aminotransferase concentrations. Mean sweat chloride concentrations decreased by 31·7 mmol/L, biomarkers of pancreatic function improved (fecal elastase-1 concentrations increased and serum immunoreactive trypsinogen concentrations decreased), and growth parameters increased at week 24.
Lumacaftor and ivacaftor were generally safe and well tolerated in children aged 2-5 years with cystic fibrosis for 24 weeks. Efficacy findings also suggest that early intervention with lumacaftor and ivacaftor has the potential to modify the course of the disease
Middleton PG, Mall MA, Drevinek P, Lands LC, McKone EF, Polineni D, Ramsay BW, Taylor0Cousar JL, Tullis E, Vermeulen F, marifwada G, Mosowski SM, Nair N, Savage J, Simard C, Tian S, Waltz D, Xuan F, Jain Rassha for the VX17-445-i102 Study Group.Elexacaftor-tezacaftor-iavacaftor for cystic fibrosis with a single The 508del allele. N Eng J Med 2019; 381:1809-19. [Pubmed]

Peter Middleton
Cystic fibrosis is caused by mutations in the gene encoding the cystic fibrosis transmembrane conductance regulator (CFTR) protein, and nearly 90% of patients have at least one copy of the Phe508del CFTR mutation. In a phase 2 trial involving patients who were heterozygous for the Phe508del CFTR mutation and a minimal- function mutation (Phe508del–minimal function genotype), the next-generation CFTR corrector elexacaftor, in combination with tezacaftor and ivacaftor, improved Phe508del CFTR function and clinical outcomes.
the authors conducted a phase 3, randomised, double-blind, placebo-controlled trial to confirm the efficacy and safety of elexacaftor–tezacaftor–ivacaftor in patients 12 years of age or older with cystic fibrosis with Phe508del–minimal function geno- types.Patients were randomly assigned to receive elexacaftor–tezacaftor–ivacaftor or placebo for 24 weeks. The primary end point was absolute change from baseline in percentage of predicted forced expiratory volume in 1 second (FEV1) at week 4.
A total of 403 patients underwent randomisation and received at least one dose of active treatment or placebo. Elexacaftor–tezacaftor–ivacaftor, relative to placebo, resulted in a percentage of predicted FEV1 that was 13.8 points higher at 4 weeks and 14.3 points higher through 24 weeks, a rate of pulmonary exacerbations that was 63% lower, a respiratory domain score on the Cystic Fibrosis Questionnaire– Revised (range, 0 to 100, with higher scores indicating a higher patient-reported quality of life with regard to respiratory symptoms; minimum clinically important difference, 4 points) that was 20.2 points higher, and a sweat chloride concentration that was 41.8 mmol per litre lower (P<0.001 for all comparisons). Elexacaftor– tezacaftor–ivacaftor was generally safe and had an acceptable side-effect profile. Most patients had adverse events that were mild or moderate. Adverse events leading to discontinuation of the trial regimen occurred in 1% of the patients in the elexacaftor–tezacaftor–ivacaftor group.
Conclusion – Elexacaftor–tezacaftor–ivacaftor was efficacious in patients with cystic fibrosis with Phe508del–minimal function genotypes, in whom previous CFTR modulator regimens were ineffective. (VX17-445-102 ClinicalTrials.gov number, NCT03525444.)
Professor Peter Middleton is Clinical Professor of Respiratory and Sleep Medicine Westmead Hospital and CF Research Group, Ludwig Engel Centre for Respiratory Research, University of Sydney.
Paterson SL, Barry PJ, Horsley AR. Tezacaftor and ivacaftor for the treatment of cystic fibrosis. Expert Rev Respir Med. 2019 Oct 18. doi: 10.1080/17476348.2020.1682998. [Epub ahead of print] [Pubmed]
Cystic fibrosis (CF) is a complex, multi-system, genetic disease affecting over 70,000 people worldwide. The underlying defect is a mutation in the CFTR gene. Dysfunctional CFTR protein results in abnormal anion movement across epithelial membranes in affected organs. There has been a paradigm shift in CF treatment over the last decade with the advent of CFTR modulation, treatments which target this underlying genetic defect and have the potential to change the course of CF clinical disease.
Available CFTR modulators in current clinical practice are reviewed in this article, with a direct comparison and summary of relevant pivotal clinical trials. The approval of ivacaftor and subsequent development of lumacaftor and tezacaftor dual combinations represent an exciting development in CF management in recent years.
Tezacaftor/ivacaftor (tez/iva) appears to have a more favourable adverse event and drug-drug interaction profile than lumacaftor/ivacaftor. Tez/iva has been approved, alongside Phe508del, for a large number of ‘residual function’ CFTR mutations, with some based on response to in vitro culture. Dual therapy with tez/iva has paved the way for triple CFTR modulation currently in clinical trials with an ultimate view to provide modulation therapy to the majority of CF genotypes in the future.
From the Division of Infection Immunity & Respiratory Medicine, Faculty of Biology Medicine and Health, University of Manchester , Manchester Adult Cystic Fibrosis Centre, Manchester NHS Foundation Trust, Wythenshawe Hospital , Southmoor Road, Wythenshawe , M23 9LT.
Pascucci C, De Biase RV, Savi D, Quattrucci S, Gnessi L, Lubrano C, Lenzi A. Impact of CFTR-modulating drugs on GH-IGF-1 axis impairment in adult patients with cystic fibrosis. Endocrinol Invest. 2019 Apr 20. doi: 10.1007/s40618-019-01051-4. [Epub ahead of print] [Pubmed]
A new class of drugs in the treatment of cystic fibrosis (CF) includes two agents: lumacaftor, which corrects CFTR channel protein, and ivacaftor, which increases CFTR channel activity. In a previous study the authors recruited 50 stable adults with CF and 16 of them showed growth hormone deficit (GHD): 7 patients severe and 9 patients partial GHD (PubMed 29098662). So they decided to re-evaluate ten patients with the GHRH + arginine test of whom only five were treated with lumacaftor/ivacaftor. All CF patients in therapy with lumacaftor/ivacaftor showed a marked improvement in GHD. Two patients moved from a severe GHD to a normal response to the GH/IGF-1 axis test, and three patients who had partial GHD moved to normal response. The authors concluded the pituitary gland may be damaged by CF disease and could benefit fromf the action of correcting drugs.
Dr Chiara Pascucci is from the Section of Medical Pathophysiology, Endocrinology, Department Experimental Medicine, Sapienza University of Rome, Italy
Perrem L, Ratjen F. Anti-inflammatories and mucociliary clearance therapies in the age of CFTR modulators. Pediatr Pulmonol. 2019 Nov;54 Suppl 3:S46-S55. doi: 10.1002/ppul.24364.[Pubmed]

Lucy Perrem
Cystic fibrosis (CF) is a genetic and life-limiting disease caused by mutations in the CF transmembrane conductance regulator (CFTR) gene. This multi-system disease is characterized by progressive lung disease and pancreatic insufficiency amongst other manifestations. CFTR primarily functions as a chloride channel that transports ions across the apical membrane of epithelial cells but has other functions, including bicarbonate secretion and inhibition of sodium transport. Defective CFTR disrupts these functions, causing viscous and dehydrated mucus to accumulate, compromising the airway lumen and contributing to obstructive pulmonary disease. The combination of CFTR dysfunction, mucus obstruction, and infection drive an exaggerated and dysfunctional inflammatory response, which contributes to irreversible airway destruction and fibrosis. CFTR modulators, an exciting new class of drugs, increase the expression and/or function of CFTR variant protein and improve multiple clinical endpoints, such as lung function, pulmonary exacerbation rates, and nutritional status. However, these genotype-specific drugs are not universally available, the clinical response is variable, and lung function still declines over time when bronchiectasis is established. Consequently, even in the age of CFTR modulators, we must target other important aspects of the CF airway disease, such as inflammation and mucociliary clearance. This review highlights the mechanisms of inflammation and mucus accumulation in the CF lung and discusses anti-inflammatory and mucociliary clearance agents that are currently in development focusing on compounds for which clinical trial data have recently become available.
Dr Lucy Perrem is in the Division of Respiratory Medicine, The Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada.
– Another article discussing the impact of the new modulators therapies and warning that even in the age of modulators other problems such as inflammation and mucociliary clearance must continue to receive attention.
Rosenfeld M, Cunningham S, Harris WT, Lapey A, Regelmann WE, Sawicki GS, Southern KW, Chilvers M, Higgins M, Tian S, Cooke J, Davies JC; KLIMB study group.An open-label extension study of ivacaftor in children with CF and a CFTR gating mutation initiating treatment at age 2-5 years (KLIMB) J Cyst Fibros. 2019 Apr 30. pii: S1569-1993(19)30061-X. doi: 10.1016/j.jcf.2019.03.009. [Epub ahead of print]Free full text [Pubmed]
KIWI (NCT01705145) was a 24-week, single-arm, pharmacokinetics, safety, and efficacy study of ivacaftor in children aged 2 to 5 years with cystic fibrosis (CF) and a CFTR gating mutation. Here, the authors report the results of KLIMB (NCT01946412), an 84-week, open-label extension of KIWI.Children received age- and weight-based ivacaftor dosages for 84 weeks. The primary outcome was safety. Other outcomes included sweat chloride, growth parameters, and measures of pancreatic function.
All 33 children who completed KIWI enrolled in KLIMB; 28 completed 84 weeks of treatment. Most adverse events were consistent with those reported during KIWI. Ten (30%) children had transaminase elevations >3 × upper limit of normal (ULN), leading to 1 discontinuation in a child with alanine aminotransferase >8 × ULN. Improvements in sweat chloride, weight, and body mass index z scores and fecal elastase-1 observed during KIWI were maintained during KLIMB; there was no further improvement in these parameters.
The authors concluded Ivacaftor was generally well tolerated for up to 108 weeks in children aged 2 to 5 years with CF and a gating mutation, with safety consistent with the KIWI study. Improvements in sweat chloride and growth parameters during the initial 24 weeks of treatment were maintained for up to an additional 84 weeks of treatment. Prevalence of raised transaminases remained stable and did not increase with duration of exposure during the open-label extension.
Dr Rosenfield is at the Seattle Children’s Hospital
– With regard to the elevated LFTs the authors note that the lack of a placebo arm made interpretation difficult as to the cause – the ivacaftor itself, ascertainment bias due to increased monitoring or the natural tendency to elevated LFTs in this age group.
Rubin JL, O’Callaghan L, Pelligra C, Konstan MW, Ward A, Ishak JK, Chandler C, Liou TG. Modeling long-term health outcomes of patients with cystic fibrosis homozygous for F508del-CFTR treated with lumacaftor/ivacaftor. Ther Adv Respir Dis.2019 Jan-Dec;13:1753466618820186. doi: 10.1177/1753466618820186.Free PMC Article[Pubmed]
Long-term survival benefits of lumacaftor/ivacaftor (LUM/IVA) cannot yet be quantified. Simulation models can provide predictions about long-term health outcomes. In this study, we aimed to project long-term health outcomes of LUM/IVA plus standard care (SC) in patients with CF homozygous for F508del-CFTR.
This modelling study was an individual patient simulation in US patients aged ⩾6 years with CF, homozygous for F508del-CFTR. The primary outcome was projected survival among (a) a cohort of patients who ever initiated LUM/IVA, accounting for treatment discontinuations, and (b) a cohort of patients who remain on continuous LUM/IVA. (Patient characteristics and model parameters were derived from clinical trials: VX14-809-109, VX13-809-011B, TRAFFIC/TRANSPORT, and PROGRESS; published literature; and the US CF Foundation Patient Registry)
Lumacaftor/ivacaftor + SC is expected to increase median survival by 6.1 years versus SC alone, accounting for treatment discontinuations. The incremental median predicted survival versus SC assuming initiation of LUM/IVA at ages 6, 12, 18, and 25 years was 17.7, 12.6, 8.0, and 3.8 years, respectively. Assuming lifetime treatment with LUM/IVA, incremental median survival was predicted to be 7.8 years longer in the LUM/IVA + SC cohort. Initiating LUM/IVA at ages 6, 12, 18, and 25 years and assuming lifetime treatment resulted in incremental median predicted survival of 23.4, 18.2, 11.0, and 4.8 years, respectively.
Lumacaftor/ivacaftor is projected to increase survival for patients with CF. Initiation at an early age and treatment persistence result in further increments in projected survival.
– A paper from the staff at Vertex
Singh SB, McLearn-Montz AJ, Milavetz F, Gates LK, Fox C, Murry LT, Sabus A, Porterfield HS, Fischer AJ.Pathogen acquisition in patients with cystic fibrosis receiving ivacaftor or lumacaftor/ivacaftor.Pediatr Pulmonol. 2019 Apr 22. doi: 10.1002/ppul.24341. [Epub ahead of print] [Pubmed]
A single-center cohort of patients with CF was studied during two time periods (2008-2011, Era 1) and (2012-2015, Era 2) based on the January 2012 approval of ivacaftor. Using Kaplan-Meier analysis, we compared the time to any new infection with P. aeruginosa, methicillin-resistant S. aureus (MRSA), or methicillin-sensitive S. aureus (MSSA) that was absent during a 2-year baseline. We stratified the analysis based on whether patients received ivacaftor or lumacaftor/ivacaftor during Era 2. The authors used the log-rank test and considered P < 0.05 statistically significant.
For patients receiving ivacaftor or lumacaftor/ivacaftor in Era 2, there was a statistically significant delay in the time to new bacterial acquisition in Era 2 vs. Era 1 ( P = 0.008). For patients who did not receive CFTR modulators, there was a trend toward slower acquisition of new bacterial infections in Era 2 compared to Era 1, but this was not statistically significant ( P = 0.10).
The authors concluded patients receiving ivacaftor or lumacaftor/ivacaftor for CF had significantly delayed acquisition of P. aeruginosa and S. aureus after these drugs were released. They suggest this method for analysing incident infections may be useful for future studies of CFTR modulators and bacterial acquisition in CF registry cohorts.
Dr S B Singh is at the Stead Family Department of Pediatrics, University of Iowa Carver College of Medicine, Iowa.
Salvatore D, Carnovale V, Iacotucci P, Braggion C, Castellani C, Cimino G, Colangelo C, Francalanci M, Leonetti G, Lucidi V, Manca A, Vitullo P, Ferrara N.Effectivenesss of ivacaftor in severe cystic fibrosis patients and non-G551D gating mutations.Pediatr Pulmonol. 2019 Jun 25. doi: 10.1002/ppSul.24424. [Epub ahead of print][Pubmed]
Ivacaftor is a significant innovation in the treatment of cystic fibrosis (CF) with gating mutations. A substantial percentage of patients with CF have severe lung involvement, but these patients are usually excluded from phase III clinical trials. Thus, the effectiveness of ivacaftor in this population has not been fully determined.
Data were collected from Italian CF centers with patients enrolled in an ivacaftor compassionate use programme (percent predicted [pp] forced expiratory volume in 1 second [FEV1 ] < 40%, or on lung transplant waiting list, or with a fast worsening trend of lung function). Data were collected for 1 year before and 1 year after ivacaftor commencement.
Thirteen patients received ivacaftor for a median of 320 days. Mean (SD) ppFEV1 increased from 35.1% (14.3%) before treatment to 46.6% (18.8%) after 12 months of treatment (absolute increase 11.5%, relative increase 32.8%). Mean distance of the 6-minute walking test improved significantly, from 535.1 m before to 611.6 m after 12 months of treatment (P = .002). The number of pulmonary exacerbations decreased significantly, from 57 during the year before ivacaftor to 28 in the year following ivacaftor (P = .0048). Five of the 13 patients (38.5%) had no exacerbations during the 12 months after starting ivacaftor. Median weight increased significantly, from 52.7 kg to 55.6 kg (P = .0031). Mean (SD) sweat chloride concentration decreased significantly, from 99.5 (22.8) mmol/L to 39.3 (15.8) mmol/L (P < .0001). No safety concerns were registered.
The authors concluded Ivacaftor was safe and effective in patients with CF with severe lung disease and non-G551D gating mutations.
Dr Donatello Salvatore is Director of the Cystic Fibrosis Center, Hospital San Carlo, Potenza, Italy.
Taylor-Cousar JL, Mall MA, Ramsey BW, McKone EF, Tullis E, Marigowda G, McKee CM, Waltz D, Moskowitz SM, Savage J, Xuan F, Rowe SM.Clinical development of triple-combination CFTR modulators for cystic fibrosis patients with one or two F508del alleles.ERJ Open Res. 2019 Jun 17;5(2). pii: 00082-2019. doi: 10.1183/23120541.00082-2019. eCollection 2019 Apr.Free PMC Article[Pubmed]
Cystic fibrosis (CF) is caused by mutations in the CF transmembrane conductance regulator gene (CFTR) that result in diminished quantity and/or function of the CFTR anion channel. F508del-CFTR, the most common CF-causing mutation (found in ∼90% of patients), causes severe processing and trafficking defects, resulting in decreased CFTR quantity and function. CFTR modulators are medications that increase the amount of mature CFTR protein (correctors) or enhance channel function (potentiators) at the cell surface. Combinations of CFTR correctors and potentiators (i.e. lumacaftor/ivacaftor, tezacaftor/ivacaftor) have demonstrated clinical benefit in subsets of patients. However, none are approved for patients with CF heterozygous for F508del-CFTR and a minimal function mutation, i.e. a mutation that produces either no protein or protein that is unresponsive to currently approved CFTR modulators. Next-generation CFTR correctors VX-659 and VX-445, each in triple combination with tezacaftor and ivacaftor, improve CFTR processing, trafficking and function in vitro and have demonstrated clinical improvements in phase 2 studies in patients with CF with one or two F508del–CFTR alleles. Here, we present the rationale and design of four randomised phase 3 studies, and their open-label extensions, evaluating VX-659 (ECLIPSE) or VX-445 (AURORA) plus tezacaftor and ivacaftor in patients with one or two F508del–CFTR alleles.
Corresponding author Dr Steven Rowe Gregory Flemming james Cystic Fibrosis Research Center, University of Alabama at Birmingham.
Rowe SM, Daines C, Ringshausen FC, Kerem E, Wilson J, Tullis E, Nair N, Simard C, Han L, Ingenito EP, McKee C, Lekstrom-Himes J, Davies JC. Tezacaftor-Ivacaftor in Residual-Function Heterozygotes with Cystic Fibrosis. N Engl J Med. 2017 Nov 23;377(21):2024-2035. doi: 10.1056/NEJMoa1709847. Epub 2017 Nov 3.[Pubmed]Free PMC Article
A randomized, double-blind, placebo-controlled, phase 3, crossover trial to evaluate the efficacy and safety of ivacaftor alone or in combination with tezacaftor, a CFTR corrector, in 248 patients 12 years of age or older who had cystic fibrosis and were heterozygous for the Phe508del mutation and a CFTR mutation associated with residual CFTR function. Patients were randomly assigned to one of six sequences, each involving two 8-week intervention periods separated by an 8-week washout period. They received tezacaftor-ivacaftor, ivacaftor monotherapy, or placebo. The primary end point was the absolute change in the percentage of predicted forced expiratory volume in 1 second (FEV1) from the baseline value to the average of the week 4 and week 8 measurements in each intervention period.
The number of analysed intervention periods was 162 for tezacaftor-ivacaftor, 157 for ivacaftor alone, and 162 for placebo. The least-squares mean difference versus placebo with respect to the absolute change in the percentage of predicted FEV1 was 6.8 percentage points for tezacaftor-ivacaftor and 4.7 percentage points for ivacaftor alone (P<0.001 for both comparisons). Scores on the respiratory domain of the Cystic Fibrosis Questionnaire-Revised, a quality-of-life measure, also significantly favoured the active-treatment groups. The incidence of adverse events was similar across intervention groups; most events were mild or moderate in severity, with no discontinuations of the trial regimen due to adverse events for tezacaftor-ivacaftor and few for ivacaftor alone (1% of patients) and placebo (<1%).
CFTR modulator therapy with tezacaftor-ivacaftor or ivacaftor alone was efficacious in patients with cystic fibrosis who were heterozygous for the Phe508del deletion and a CFTR residual-function mutation. (EXPAND ClinicalTrials.gov number, NCT02392234 .).
Also CFTR Modulator Therapy for Cystic Fibrosis. [N Engl J Med. 2017] PMID:PMCID: PMC6472479 DOI: 10.1056/NEJMoa1709847
From the Division of Pulmonary, Allergy, and Critical Care Medicine, University of Alabama at Birmingham, Birmingham (S.M.R.);
Rubin JL, O’Callaghan L, Pelligra C, Konstan MW, Ward A, Ishak JK, Chandler C, Liou TG. Modeling long-term health outcomes of patients with cystic fibrosis homozygous for F508del-CFTR treated with lumacaftor/ivacaftor.
Ther Adv Respir Dis. 2019 Jan-Dec;13:1753466618820186. doi: 10.1177/1753466618820186. Free PMC Article [Pubmed]
Long-term survival benefits of lumacaftor/ivacaftor (LUM/IVA) cannot yet be quantified. Simulation models can provide predictions about long-term health outcomes. In this study, we aimed to project long-term health outcomes of LUM/IVA plus standard care (SC) in patients with CF homozygous for F508del-CFTR.
This modelling study was an individual patient simulation in US patients aged ⩾6 years with CF, homozygous for F508del-CFTR. The primary outcome was projected survival among (a) a cohort of patients who ever initiated LUM/IVA, accounting for treatment discontinuations, and (b) a cohort of patients who remain on continuous LUM/IVA. Patient characteristics and model parameters were derived from clinical trials: VX14-809-109, VX13-809-011B, TRAFFIC/TRANSPORT, and PROGRESS; published literature; and the US CF Foundation Patient Registry.
Lumacaftor/ivacaftor + SC is expected to increase median survival by 6.1 years versus SC alone, accounting for treatment discontinuations. The incremental median predicted survival versus SC assuming initiation of LUM/IVA at ages 6, 12, 18, and 25 years was 17.7, 12.6, 8.0, and 3.8 years, respectively. Assuming lifetime treatment with LUM/IVA, incremental median survival was predicted to be 7.8 years longer in the LUM/IVA + SC cohort. Initiating LUM/IVA at ages 6, 12, 18, and 25 years and assuming lifetime treatment resulted in incremental median predicted survival of 23.4, 18.2, 11.0, and 4.8 years, respectively.
Lumacaftor/ivacaftor is projected to increase survival for patients with CF. Initiation at an early age and treatment persistence result in further increments in projected survival.
– A paper from the staff at Vertex
Ruan J, Hirai H, Yang D, Ma L, Hou X, Jiang H, Wei H, Rajagopalan C, Mou H, Wang G, Zhang J, Li K, Chen YE, Sun F, Xu J. Efficient Gene Editing at Major CFTR Mutation Loci.Mol Ther Nucleic Acids. 2019 Feb 16;16:73-81. doi: 10.1016/j.omtn.2019.02.006. [Epub ahead of print] Free full text [Pubmed]
Nuclease-mediated precise gene editing (PGE) represents a promising therapy for CF, for which an efficient strategy that is free of viral vector, drug selection, and reporter enrichment (VDR free) is desirable. Here the authors compared different transfection methods (lipofectamine versus electroporation) and formats (plasmid DNA versus ribonucleoprotein) in delivering the CRISPR/Cas9 elements along with single-stranded oligodeoxynucleotides (ssODNs) to clinically relevant cells targeting major CFTR mutation loci. They demonstrate that, among different combinations, electroporation of CRISPR/Cas9 and guide RNA (gRNA) ribonucleoprotein (Cas9 RNP) is the most effective one. By using this VDR-free method, 4.8% to 27.2% efficiencies were achieved in creating dF508, G542X, and G551D mutations in a wild-type induced pluripotent stem cell (iPSC) line. When it is applied to a patient-derived iPSC line carrying the dF508 mutation, a greater than 20% precise correction rate was achieved. As expected, genetic correction leads to the restoration of CFTR function in iPSC-derived proximal lung organoids, as well as in a patient-derived adenocarcinoma cell line CFPAC-1. The present work demonstrates the feasibility of gene editing-based therapeutics toward monogenic diseases such as CF.
– This is a comprehensive review of the position regarding gene editing and cystic fibrosis. The full free text is recommended.
From the Center for Advanced Models for Translational Sciences and Therapeutics, University of Michigan Medical Center, University of Michigan Medical School, 2800 Plymouth Road, Ann Arbor, MI 48109, USA; Key Lab of Swine Genetics and Breeding of Ministry of Agriculture and Rural Affairs, College of Animal Sciences & Technology, Huazhong Agricultural University, Wuhan, China.
Salvatore D, Carnovale V, Iacotucci P, Braggion C, Castellani C, Cimino G, Colangelo C, Francalanci M, Leonetti G, Lucidi V, Manca A, Vitullo P, Ferrara N. Effectivenesss of ivacaftor in severe cystic fibrosis patients and non-G551D gating mutations. Pediatr Pulmonol. 2019 Jun 25. doi: 10.1002/ppSul.24424. [Epub ahead of print] [Pubmed]

Donatello Salvatore
Ivacaftor is a significant innovation in the treatment of cystic fibrosis (CF) with gating mutations. A substantial percentage of patients with CF have severe lung involvement, but these patients are usually excluded from phase III clinical trials. Thus, the effectiveness of ivacaftor in this population has not been fully determined. Data were collected from Italian CF centers with patients enrolled in an ivacaftor compassionate use programme (percent predicted [pp] forced expiratory volume in 1 second [FEV1 ] < 40%, or on lung transplant waiting list, or with a fast worsening trend of lung function). Data were collected for 1 year before and 1 year after ivacaftor commencement.
Thirteen patients received ivacaftor for a median of 320 days. Mean (SD) ppFEV1 increased from 35.1% (14.3%) before treatment to 46.6% (18.8%) after 12 months of treatment (absolute increase 11.5%, relative increase 32.8%). Mean distance of the 6-minute walking test improved significantly, from 535.1 m before to 611.6 m after 12 months of treatment (P = .002). The number of pulmonary exacerbations decreased significantly, from 57 during the year before ivacaftor to 28 in the year following ivacaftor (P = .0048). Five of the 13 patients (38.5%) had no exacerbations during the 12 months after starting ivacaftor. Median weight increased significantly, from 52.7 kg to 55.6 kg (P = .0031). Mean (SD) sweat chloride concentration decreased significantly, from 99.5 (22.8) mmol/L to 39.3 (15.8) mmol/L (P < .0001). No safety concerns were registered.
The authors concluded Ivacaftor was safe and effective in patients with CF with severe lung disease and non-G551D gating mutations.
Dr Donatello Salvatore is Director of the Cystic Fibrosis Center, Hospital San Carlo, Potenza, Italy.
Saiman L. Improving outcomes of infections in cystic fibrosis in the era of CFTR modulator therapy. Pediatr Pulmonol. 2019 Nov;54 Suppl 3:S18-S26. doi: 10.1002/ppul.24522. [Pubmed]

Lisa Saiman
Currently, available single and dual-combination cystic fibrosis transmembrane conductance regulator (CFTR) modulator therapies have favorably altered the life course of individuals with cystic fibrosis (CF) by decreasing morbidities and increasing survival. However, even with CFTR modulator use, questions and challenges remain to optimize the management of lung infections. This review (a) identifies these ongoing challenges and discusses the current understanding of the potential impact of CFTR modulator therapy on infections; (b) describes ongoing research to optimize detection, diagnosis, and treatment of CF microorganisms; and (c) discusses strategies to develop new anti-infective therapies. The CF Foundation has launched the Infection Research Initiative to fund research that will improve our understanding of the complex microbial ecology within the CF lung, improve detection of CF pathogens, optimize current treatment, including long-term chronic therapies, and develop new anti-infective therapies. Ongoing clinical trials to determine the optimal duration of treatment of pulmonary exacerbations and to diagnose and treat nontuberculous mycobacteria represent clinical research paradigms that could be used to answer other complex treatment questions. The anti-infective pipeline includes both existing anti-infective and non-anti-infective agents, many of which are proposed to have unique mechanisms of action in CF. Future studies plan to evaluate short- and long-term clinical effectiveness and impact on infections, of the next generation of CFTR modulator therapy, the highly effective triple-combination therapy, for individuals with CF, homozygous or heterozygous for F508del.
Dr Lisa Saiman, is a Professor of Pediatrics at Columbia University Medical Center and an attending physician at New York-Presbyterian (NYP) Morgan Stanley Children’s Hospital.
– What will be the impact of the new modulators in individuals who already have chronic lung disease? It is likely that all CF individuals whatever the sate of their lung disease will require carful “monitoring of their microbiology and anti-microbial therapy remains a cornerstone of treatment for CF”. There was a decrease in the proportion of G551D patients with positive cultures for P.aeruginosa significantly after starting ivacaftor noted by a number of authors. A number of studies suggest that existing CFTR modulators have a favourable effect on the microbiology. The effect of modulator therapy on the microbiome is discussed. The author hopes that studies will allow careful assessment of the risks and benefits of withdrawing antimicrobial therapies as may appear attractive to some individuals. An interesting review of the microbiology by an expert as treatment of CF enters a new “modulator era”.
Shiferaw D, Faruqi S. Profile of tezacaftor/ivacaftor combination and its potential in the treatment of cystic fibrosis.Ther Clin Risk Manag. 2019 Aug 22;15:1029-1040. doi: 10.2147/TCRM.S165027. eCollection 2019.[Pubmed] Free PMC Article
Cystic fibrosis (CF) is a life-limiting autosomal recessive disease caused by dysfunction of the cystic fibrosis transmembrane conductance regulator (CFTR) ion channel. Management of CF has traditionally relied upon managing complications of CFTR protein dysfunction and this has led to a steady improvement in survival of CF patients. However, the landscape of CF care has changed substantially over the last decade with the discovery of CFTR modulators that aim to increase or potentially restore the function of the disease-causing CFTR protein. This narrative review summarises the development of CFTR therapies so far with emphasis on tezacaftor/ivacaftor combination therapy. We have also summarised the Phase II results of triple combination therapy which promises an effective CFTR modulator therapy for more than 90% of CF patients.
– Rather nice review of the present situation from Drs Dejene Shiferaw and Shoaib Faruqui of the Department of Respiratory Medicine, Hull University Teaching Hospitals NHS Trust, Hull
The experienced degree and source of emotional distress are drivers for self-management decisions in patients with cystic fibrosis who experience a pulmonary exacerbation. The authors consider their data provide new understanding that will be essential to informing clinical practice, future patient-reported outcomes measures and intervention development.
Gabriela Schmid-Mohler, of the Centre for Clinical Nursing Zurich is an expert in advanced practice nursing and patient education
Sergeev V, Chou FY, Lam GY, Hamilton CM, Wilcox PG, Quon BS. The Extra-pulmonary Effects of CFTR Modulators in Cystic Fibrosis. Ann Am Thorac Soc. 2019 Oct 29. doi: 10.1513/AnnalsATS.201909-671CME. [Epub ahead of print] Full article can be downloaded from (https://www.researchgate.net/profile/Valetnine_Sergeev) .[Pubmed]

Valentine Sergeev
The effects of CFTR modulators on lung function, pulmonary exacerbations, and quality of life have been well documented.

Bradley Quon
However, CF is a multi-organ disease and therefore an evidence base is emerging on the systemic effects of CFTR modulators beyond the pulmonary system. This is of great clinical importance as many of these studies provide proof-of-concept that CFTR modulators might be used one day to prevent or treat extra-pulmonary manifestations stemming from CFTR dysfunction. In this concise review of the literature, the authors summarize the results of key publications that have evaluated the effects of CFTR modulators on weight and growth, pancreatic function, the gastrointestinal and hepatobiliary systems, sinus disease, bone disease, exercise tolerance, fertility, mental health, and immunity. While many of these studies have reported beneficial extra-pulmonary effects related to the use of ivacaftor (IVA) in CF patients with at least one gating mutation, most of the evidence is low or very low quality given the limited number of patients evaluated and the lack of a control group. Based on an even smaller number of studies evaluating the extra-pulmonary effects of lumacaftor-ivacaftor (LUM-IVA), the benefits are less clear. While limited, these studies may provide the basis for future clinical trials to evaluate CFTR modulators on the extra-pulmonary manifestations of CF
Dr Valentine Sergeev is in the Faculty of Medicine, University of British Columbia, Vancouver, BC, Canada
Dr Bradley S Quon, the corresponding author, is at the Centre for Heart Lung Innovation, Vancouver.
Singh SB, McLearn-Montz AJ, Milavetz F, Gates LK, Fox C, Murry LT, Sabus A, Porterfield HS, Fischer AJ.Pathogen acquisition in patients with cystic fibrosis receiving ivacaftor or lumacaftor/ivacaftor.Pediatr Pulmonol. 2019 Apr 22. doi: 10.1002/ppul.24341. [Epub ahead of print] [Pubmed]
A single-center cohort of patients with CF was studied during two time periods (2008-2011, Era 1) and (2012-2015, Era 2) based on the January 2012 approval of ivacaftor. Using Kaplan-Meier analysis, we compared the time to any new infection with P. aeruginosa, methicillin-resistant S. aureus (MRSA), or methicillin-sensitive S. aureus (MSSA) that was absent during a 2-year baseline. We stratified the analysis based on whether patients received ivacaftor or lumacaftor/ivacaftor during Era 2. The authors used the log-rank test and considered P < 0.05 statistically significant.
For patients receiving ivacaftor or lumacaftor/ivacaftor in Era 2, there was a statistically significant delay in the time to new bacterial acquisition in Era 2 vs. Era 1 ( P = 0.008). For patients who did not receive CFTR modulators, there was a trend toward slower acquisition of new bacterial infections in Era 2 compared to Era 1, but this was not statistically significant ( P = 0.10).
The authors concluded patients receiving ivacaftor or lumacaftor/ivacaftor for CF had significantly delayed acquisition of P. aeruginosa and S. aureus after these drugs were released. They suggest this method for analysing incident infections may be useful for future studies of CFTR modulators and bacterial acquisition in CF registry cohorts.
Dr S B Singh is from the Sread Family Department of Pediatrics, UNiversity of Iowa Carver College of Medicine, Iowa.
– This is a very useful comprehensive referenced review of the many extra-pulmonary effects of CFTR modulators reported to the present time. The full article can be downloaded (https://www.researchgate.net/profile/Valetnine_Sergeev).
Taylor-Cousar JL, Mall MA, Ramsey BW, McKone EF, Tullis E, Marigowda G, McKee CM, Waltz D, Moskowitz SM, Savage J, Xuan F, Rowe SM.Clinical development of triple-combination CFTR modulators for cystic fibrosis patients with one or two F508del alleles.ERJ Open Res. 2019 Jun 17;5(2). pii: 00082-2019. doi: 10.1183/23120541.00082-2019. eCollection 2019 Apr. [Pubmed] Free PMC Article

Jennifer Taylor-Cousar
Cystic fibrosis (CF) is caused by mutations in the CF transmembrane conductance regulator gene (CFTR) that result in diminished quantity and/or function of the CFTR anion channel. F508del-CFTR, the most common CF-causing mutation (found in ∼90% of patients), causes severe processing and trafficking defects, resulting in decreased CFTR quantity and function. CFTR modulators are medications that increase the amount of mature CFTR protein (correctors) or enhance channel function (potentiators) at the cell surface. Combinations of CFTR correctors and potentiators (i.e. lumacaftor/ivacaftor, tezacaftor/ivacaftor) have demonstrated clinical benefit in subsets of patients. However, none are approved for patients with CF heterozygous for F508del-CFTR and a minimal function mutation, i.e. a mutation that produces either no protein or protein that is unresponsive to currently approved CFTR modulators. Next-generation CFTR correctors VX-659 and VX-445, each in triple combination with tezacaftor and ivacaftor, improve CFTR processing, trafficking and function in vitro and have demonstrated clinical improvements in phase 2 studies in patients with CF with one or two F508del–CFTR alleles. Here, we present the rationale and design of four randomised phase 3 studies, and their open-label extensions, evaluating VX-659 (ECLIPSE) or VX-445 (AURORA) plus tezacaftor and ivacaftor in patients with one or two F508del–CFTR alleles.
Corresponding author Dr Steven Rowe, Gregory Flemming James Cystic Fibrosis Research Center, University of Alabama at Birmingham.A very comprehensive review of triple-combination CFTR modulators
Toprak D, Davis C, Rosenfeld M. Treating the Airway Consequences of Cystic Fibrosis Transmembrane Conductance Regulator Dysfunction. Semin Respir Crit Care Med. 2019 Oct 28. doi: 10.1055/s-0039-1698462. [Epub ahead of print][Pubmed]

Demet Toprak
In cystic fibrosis (CF), absent or dysfunctional CF transmembrane conductance regulator (CFTR) on the surface of airway epithelial cells causes abnormal mucociliary clearance, leading to chronic endobronchial infection and inflammation, in turn resulting in life-shortening progressive obstructive lung disease and structural airway damage. Fortunately, CF-specific therapies have been developed that improve lung function and reduce pulmonary exacerbations, contributing significantly to improved survival over the past 4 decades. Therapies not originally developed for CF, such as bronchodilators and corticosteroids, are also widely used by people living with CF. Therapies to be reviewed in this article include mucolytics, airway surface liquid hydrators, anti-inflammatory medications, bronchodilators, inhaled and oral antibiotics, and airway clearance techniques. Determining which therapies to utilize can be challenging, as there is variable evidence for each treatment, differing national guidelines, few head-to-head studies, potential for drug-drug interactions, and synergistic toxicities, as well as issues with burden of care. In this review, the authors summarize the mechanism of action and available evidence, and compare national guidelines for each major medication used to treat the airway consequences of CFTR dysfunction.
Dr Demet Toprak is an Assistant Professor in the Department of Pediatrics, Division of Pulmonary and Sleep Medicine, SeattleChildren’s Hospital, Seattle, Washington.
van Koningsbruggen-Rietschel S, Conrath K, Fischer R, Sutharsan S, Kempa A, Gleiber W, Schwarz C, Hector A, Van Osselaer N, Pano A, Corveleyn S, Bwirire D, Santermans E, Muller K, Bellaire S, Van de Steen O. GLPG2737 in lumacaftor/ivacaftor-treated CF subjects homozygous for the F508del mutation: A randomized phase 2A trial (PELICAN). J Cyst Fibros. 2019 Oct 5. pii: S1569-1993(19)30890-2. doi: 10.1016/j.jcf.2019.09.006. [Epub ahead of print] [Pubmed]

Silke van Koningsbruggen
Triple combinations of cystic fibrosis (CF) transmembrane conductance regulator (CFTR) modulators demonstrate enhanced clinical efficacy in CF patients with F508del mutation, compared with modest effects of dual combinations. GLPG2737 was developed as a novel corrector for triple combination therapy. This multicenter, randomized, double-blind, placebo-controlled, phase 2a study evaluated GLPG2737 in F508del homozygous subjects who had been receiving lumacaftor 400mg/ivacaftor 250mg for ≥12weeks. The primary outcome was change from baseline in sweat chloride concentration. Other outcomes included assessment of pulmonary function, respiratory symptoms, safety, tolerability, and pharmacokinetics.
Between November 2017 and April 2018, 22 subjects were enrolled and randomized to oral GLPG2737 (75mg; n=14) or placebo (n=8) capsules twice daily for 28days. A significant decrease from baseline in mean sweat chloride concentration occurred at day 28 for GLPG2737 versus placebo (least-squares-mean difference-19.6mmol/L [95% confidence interval (CI) -36.0, -3.2], p=.0210). The absolute improvement, as assessed by least-squares-mean difference in change from baseline, in forced expiratory volume in 1s (percent predicted) at day 28 for GLPG2737 versus placebo was 3.4% (95% CI -0.5, 7.3). Respiratory symptoms in both groups remained stable. Mild/moderate adverse events occurred in 10 (71.4%) and 8 (100%) subjects receiving GLPG2737 and placebo, respectively. Lower exposures of GLPG2737 (and active metabolite M4) were observed than would be expected if administered alone (as lumacaftor induces CYP3A4). Lumacaftor and ivacaftor exposures were as expected.
GLPG2737 was well tolerated and yielded significant decreases in sweat chloride concentration versus placebo in subjects homozygous for F508del receiving lumacaftor/ivacaftor, demonstrating evidence of increased CFTR activity when added to a potentiator-corrector combination.
Dr Silke van Koningsbruggen-Rietschel is at the Cystic Fibrosis Center, Children’s Hospital, University of Cologne, Faculty of Medicine and University Hospital Cologne, Germany. Electronic address: Silke.vanKoningsbruggen@uk-koeln.de.
Walker S, Flume P, McNamara J, Solomon M, Chilvers M, Chmiel J, Harris RS, Haseltine E, Stiles D, Li C, Ahluwalia N, Zhou H, Owen CA, Sawicki G; VX15-661-113 Investigator Group. A phase 3 study of tezacaftor in combination with ivacaftor in children aged 6 through 11 years with cystic fibrosis. J Cyst Fibros. 2019 Jun 25. pii: S1569-1993(19)30813-6. doi: 10.1016/j.jcf.2019.06.009. Free full text [Epub ahead of print] [Pubmed
 Tezacaftor/ivacaftor is a new treatment option in many regions for patients aged ≥12 years who are homozygous (F/F) or heterozygous for the F508del-CFTR mutation and a residual function (F/RF) mutation. This Phase 3, 2-part, open-label study evaluated the pharmacokinetics (PK), safety, tolerability, and efficacy of tezacaftor/ivacaftor in children aged 6 through 11 years with these mutations.
Tezacaftor/ivacaftor is a new treatment option in many regions for patients aged ≥12 years who are homozygous (F/F) or heterozygous for the F508del-CFTR mutation and a residual function (F/RF) mutation. This Phase 3, 2-part, open-label study evaluated the pharmacokinetics (PK), safety, tolerability, and efficacy of tezacaftor/ivacaftor in children aged 6 through 11 years with these mutations.
Part A informed weight-based tezacaftor/ivacaftor dosages for part B. The primary objective of part B was to evaluate the safety and tolerability of tezacaftor/ivacaftor through 24 weeks; the secondary objective was to evaluate efficacy based on changes from baseline in percentage predicted forced expiratory volume in 1 s (ppFEV1), growth parameters, sweat chloride, and the Cystic Fibrosis Questionnaire-Revised (CFQ-R) respiratory domain score.
After PK analysis in part A, 70 children received ≥1 dose of tezacaftor/ivacaftor in part B; 67 children completed treatment. Exposures in children aged 6 through 11 years were within the target range for those observed in patients aged ≥12 years. The safety profile of tezacaftor/ivacaftor was generally similar to prior studies in patients aged ≥12 years. One child discontinued treatment for a serious adverse event of constipation. Tezacaftor/ivacaftor treatment improved sweat chloride levels and CFQ-R respiratory domain scores, mean ppFEV1 remained stable in the normal range, and growth parameters remained stable over 24 weeks.
Tezacaftor/ivacaftor was generally safe and well tolerated, and improved CFTR function in children aged 6 through 11 years with CF with F/F and F/RF genotypes, supporting tezacaftor/ivacaftor use in this age group. NCT02953314.Tezacaftor/ivacaftor treatment improved SwCl levels and CFQ-R respiratory domain child version scores, and lung function and normal growth were maintained over 24 weeks. These results support tezacaftor/ivacaftor as an alternative treatment option to CFTR modulators previously approved in children aged 6 through 11 years with CF and F/F and F/RF genotypes in the United States. These results also support tezacaftor/ivacaftor as a new treatment option for children aged 6 through 11 years with CF and F/RF genotypes in regions that currently lack a CFTR modulator for the treatment of this population.
Dr Seth Walker (figure) is a pulmonologist affiliated with University Hospitals of Cleveland, Cleveland Medical Center, Rainbow Babies and Children’s Hospital,
Welsner M, Straßburg S, Taube C, Sutharsan S. Use of ivacaftor in late diagnosed cystic fibrosis monozygotic twins heterozygous for F508del and R117H-7T – a case report. BMC Pulm Med. 2019 Apr 11;19(1):76. doi: 10.1186/s12890-019-0840-8.[Pubmed] Free PMC Article
CFTR modulator therapy with ivacaftor is a treatment option for Cystic Fibrosis (CF) patients with at least one copy of a R117H-7T mutation in the CFTR gene. Desirable effects of this therapy are improvement of lung function, decrease in exacerbation rate, normalization or reduction of sweat chloride and weight gain. Monogenetic CF-twins carry identical genetic information, so therapy response and side effects are expected to be nearly identical under this specific therapy.
In monozygotic twins, at the age of 55, two pathogenic variants in the CFTR gene (F508del and R117H-7T) were detected. Both patients presented with a borderline sweat test (30-59 mmol/L) and despite the same genetic information and similar life circumstances the disease proceeds completely different. While one patient has severe pulmonary involvement with chronic P. aeruginosa infection, her twin sister is almost unimpaired. Liver or pancreatic involvement was not seen in either patient. Due to the presence of one copy of a R117H-7T mutation, CFTR modulator therapy with ivacaftor was initiated in both. Response and side effects were significantly different. In the less affected patient, we observed an improvement in lung function and a normalization of sweat chloride. In the severely affected patient, no functional response to treatment was seen, but stabilization of the disease state with a decrease in exacerbation and hospitalization rate and weight gain as well as a normalization of sweat chloride. There was an increase in liver enzymes in the less affected patient, which normalized after halving the dose of ivacaftor, while the therapeutic effect was maintained.
Despite nearly identical genetic information, as in monogenetic twins, therapy response and onset of side effects of CFTR modulating therapy are very different. In patients with late diagnosis and severe pulmonary involvement, ivacaftor does not seem to improve lung function, whereas in patients with late diagnosis and low disease severity a relevant therapy response was obtained. In addition to lung function, additional clinical parameters such as reduction of exacerbation and hospitalization rate and weight gain should be used to assess therapy response, especially in severely affected patients.
From the Department of Pulmonary Medicine, University Hospital Essen – Ruhrlandklinik, Adult Cystic Fibrosis Center, University of Duisburg-Essen, Tueschener Weg 40, 45329, Essen, Germany. matthias.welsner@rlk.uk-essen.de. Department of Pulmonary Medicine, University Hospital Essen – Ruhrlandklinik, Adult Cystic Fibrosis Center, University of Duisburg-Essen, Tueschener Weg 40, 45329, Essen, Germany.
Wu HX, Zhu M, Xiong XF, Wei J, Zhuo KQ, Cheng DY. Efficacy and Safety of CFTR Corrector and Potentiator Combination Therapy in Patients with Cystic Fibrosis for the F508del-CFTR Homozygous Mutation: A Systematic Review and Meta-analysis. Adv Ther. 2019 Feb;36(2):451-461. doi: 10.1007/s12325-018-0860-4. Epub 2018 Dec 15. [Pubmed]
The authors performed a systematic review and meta-analysis of randomized controlled trials (RCTs) to evaluate the efficacy and safety of combination therapy on lung function, nutritional status, clinical score and safety in CF for the F508del-CFTR homozygous mutation. Five RCTs, including a total of 1637 participants with the F508del-CFTR homozygous mutation who accepted CFTR corrector and potentiator combination therapy along with basic treatment were enrolled in this analysis. Primary analysis revealed that combination therapy improved the percent of predicted FEV1 (ppFEV1) (MD 2.38, 1.62-3.15, P < 0.00001), Cystic Fibrosis Questionnaire-Revised (CFQ-R) respiratory domain score (MD 2.59, 0.96-4.22, P = 0.002) and body-mass index (BMI) (MD 0.21, 0.03-0.39, P = 0.02). In the secondary analysis, combination therapy had no impact on the number of participants reporting adverse events (OR 0.88, 0.58-1.33, P = 0.53), but increased the proportion of discontinued treatments due to adverse events (OR 2.71, 1.3-5.63, P = 0.008).
The authors concluded potentiator combination therapy effectively improves lung function, nutritional status and clinical score in CF patients with the F508del-CFTR homozygous mutation, and has an acceptable safety profile.
From the Department of Respiratory and Critical Care Medicine, West China Hospital, Sichuan University, Chengdu, China.
Kimberly Altman is a Cystic Fibrosis Dietitian at the Gunnar Esiason Adult Cystic Fibrosis and Lung Center, New York Presbyterian/Columbia University Medical Center, New York, New York, United States.
Also CFTR Modulator Therapy for Cystic Fibrosis. [N Engl J Med. 2017] PMID:PMCID: PMC6472479 DOI: 10.1056/NEJMoa1709847
From the Division of Pulmonary, Allergy, and Critical Care Medicine, University of Alabama at Birmingham, Birmingham (S.M.R.)
PLEASE GO TO NEXT SECTION FOR ALL FURTHER ABSTRACTS ON ALL PUBLICATIONS RELATING TO MODULATORS FROM 2020 ONWARDS






